Abstract
SARS-COV2 infection has swiftly become a pandemic disease of historic relevance and widely variable outcomes. This variable prognosis is related both to uneven damage, among others, to lungs, heart and kidneys, and to a multisystemic inflammatory reaction. All these factors are known to disrupt water balance and potentially induce hyponatraemia or hypernatraemia. Water balance disorders are known mortality and morbidity risk factors in several clinical scenarios and their proper management, though often complex and hazardous, can reduce mortality and length of hospitalization. Clinical uncertainty over COVID-19 outcome, the variety of organs involved in both the infection and water balance and difficulties in clinical examination due to risk of contagion might obstruct proper management of dysnatremic disorders. Thus, the Acqua Neuroendocrinology Group of the Spanish Society for Endocrinology (SEEN) has endeavoured to provide evidence and expert based recommendations on the management of hyponatraemia and hypernatraemia in COVID-19 patients.
Keywords: COVID-19, SARS-COV2, Hyponatraemia, Hypernatraemia, Dysnatremia
On January 30th 2020, the World Health Organization officially declared SARS-COV2 infection(COVID-19) as a pandemic disease. As of today, over 84 million cases have been confirmed, including over 1.848.000 deaths reported to WHO [1] . COVID-19 is a disease with widely variable outcomes, among which 19% develop severe disease [2].Adverse clinical outcome correlates with multi-organ injury, maladaptive functions of the renin-angiotensin-aldosterone system and thirst and appetite abnormalities, all of which potentially disrupt water homeostasis [3]. A number of case reports describing hyponatraemia of various etiologies was initially published [4–7]. Later, a descriptive study of 16 patients with COVID-19-related hospitalization found 50% of them had hyponatraemia [8], whereas the HOPE study, an international registry of 4664 hospitalized COVID-19 patients, found that 20.5% and 3.7% had hyponatraemia and hypernatraemia, respectively [9]: both hyponatraemia and hypernatraemia were generally mild (130–134 mEq/l in 16.7%), severe hyponatraemia (<120 mEq/l) was found only in 0.4%. Multivariable logistic regression analysis showed that male sex and age > 70 years were independently associated with hyponatraemia at admission, whereas smoking, tachypnea and serum creatinine >1.5 mg/dl bore a positive, independent association with admission hypernatraemia. Finally, the HOPE registry revealed that hyponatraemia was an independent risk factor for mortality (OR 1.5, 95% CI 1.08–2.09; p = 0.016) and sepsis (OR 1.87, 95% CI 1.23–2.66; p < 0.001), as was the case also for hypernatraemia (Mortality OR 2.38, 95% CI 1.18–4.78; p = 0.015. Sepsis OR 3.78, 95% CI. 1.98–7.22; p < 0.001) [9].
Patients with chronic disorders of water homeostasis, such as diabetes insipidus (DI) or chronic hyponatraemia (CH) are prone to suffering exacerbations of water imbalance during COVID-19 pandemic, either due to the loss of follow-up in non-infected patients with DI or chronic hyponatraemia or the impact of SARS-COV2 infection on water homeostasis. Thus, the European Society of Endocrinology published expert-based recommendations on the management of diabetes insipidus and hyponatraemia in the time of COVID-19 [10]. However, published literature on COVID-19 and its related complications increases swiftly; meanwhile, further waves and incidence peaks are expected in the near future, and these recommendations were based on preliminary data on the disease and require further coverage on practical aspects of fluid and electrolyte balance in these patients.
According to published data and clinical expertise, patients with DI or CH present additional challenges upon COVID-19 infection:
COVID-19 induced hyponatraemia or hypernatraemia, present in 20.5% and 3.7% respectively of hospitalized COVID-19 patients without underlying water balance disorders [9]
Challenges in the management of DI or CH during COVID-19 infection
Limitations for the clinical evaluation due to risk of contagion
Pharmacological interactions between sodium directed therapies (i.e. tolvaptan, desmopressin) and COVID-19 treatments (i.e. tocilizumab)
Management of patients with chronic water balance disorders during COVID-19 pandemic requires careful consideration of two opposing paradigms:
Careful follow-up and treatment of DI and CH patients, who might worsen their water balance homeostasis if SARS-COV2 infection occurs
Reducing clinic attendance and non-urgent tests where possible to avert patient’s risk of infection
Thus, the Neuroendocrinology Group of the Spanish Society for Endocrinology (SEEN) has endeavoured to provide recommendations both for the chronic management of DI and CH during this pandemic and for the evaluation of new-onset water balance disorders in COVID-19 patients. Where possible we have attempted to develop evidence-based guidelines, whereas expert-based consensus was provided when evidence was lacking.
Specific risks in patients with chronic hyponatraemia or diabetes insipidus and COVID-19
Mismanagement of water balance disorders during acute illness can worsen morbidity and mortality [11, 12]. Thus, adequate evidence-based treatment of CH or DI, as previously described in European and American Hyponatraemia Guidelines [13, 14] and in the European Society for Endocrinology statement on the management of these disorders during COVID-19 pandemic [10], may improve outcomes, including risk of hospitalization and therefore SARS-COV2 exposure.
COVID-19, particularly in severe forms, can induce numerous electrolyte abnormalities that might be particularly severe in patients with chronic water balance abnormalities [2]. According to published literature, these are some of the most common alterations that might complicate the management of patients with wáter balance abnormalities and SARS-COV2 infection:
Complications linked to the COVID-19 pandemic that might worsen the outcome of patients with either DI or CH:
COVID-19--related electrolyte abnormalities: hyponatraemia, hypernatraemia, hypokalemia, mixed alcalosis (respiratory alcalosis due to hyperventilation, metabolic alcalosis linked to hypovolaemia)
Loss of follow-up of CH or DI due to patient’s and/or health care worker fear of contagion or work overload by the health care worker during COVID-19 outbreaks.
Difficulties accessing water due to psychosocial factors, such as social isolation during confinement and anxiety or depression linked to outbreaks, can be particularly harmful in CH and DI patients. Futhermore, water intake can activate mesolimbic reward circuits in the central nervous system, which could lead to psychogenic polydipsia in these patients and ultimately worsen water balance [15].
-
b.
DI-specific risks during COVID-19 pandemic:
Loss of follow-up during the pandemic might lead to undetected hyponatraemia due to desmopressin overdose, particularly when administered through intranasal route [16]. SARS-COV2 infection might also increase antidiuresis. However, larger series with more in-depth description of volume status and serum and urine electrolytes are required.
During SARS-COV2 infection, extrarenal water loses might increase due to hyperpyrexia, hyperventilation and/or diarrhoea and cause hypernatraemia. This could worsen further if either the patient or health care workers do not ensure timely administration of desmopressin and monitorization of sodium levels take place regularly in patients with DI [17].
Patients with central DI often suffer as well from adrenal insufficiency and hypothyroidism. Timely administration of thyroid hormones and glucocorticoid replacement is paramount, increasing the dose of glucocorticoids during intercurrent illnesses as described in clinical guidelines [18].
Obesity is common in patients with central DI, particularly when other pituitary hormonal deficiencies or hypersecretion syndromes (i.e. Cushing’s disease) are present. Obese patients suffer from worse COVID-19 related prognosis [19], which highlights the need to reduce contagion risk in these patients.
Metabolic comorbidities in patients with central DI that could worsen COVID-19 prognosis: diabetes mellitus, hypertension, obstructive sleep apnea
Increased risk of thrombosis in DI due to hypernatraemia, which might worsen during SARS-COV2 infection, also associated with hypercoagulability, or in non-infected patients due to confinement, increased weight and lack of physical activity [20, 21]. Therefore, thromboprophylaxis should be systematically considered in COVID-19 patients with chronic DI.
c. Chronic hyponatraemia specific risks during COVID-19 pandemic:
Patients with chronic SIADH might suffer from decompensated hyponatraemia during COVID-19 infection due to thirst abnormalities during acute illness, lack of treatment adherence (i.e. tolvaptan, urea...) and/or treatment monitorization.
Changes in volume status during intercurrent illness, i.e. hypovolaemia caused by vomiting or hyperpirexia with increased perspiration. Both tolvaptan and urea are licensed for use during euvolemic hyponatraemia due to SIADH, but patients with hyponatraemia might change volume status during acute illness.
-
iii.
Chronic comorbidities common in patients with SIADH that might worsen COVID-19 prognosis: cancer, respiratory disorders, central nervous system disorders...
Management of patients with DI during COVID-19 pandemic
Non-infected patients:
Outpatient follow-up according to clinical guidelines [11]. If patients have preserved thirst sensation and are capable of regulating water intake and maintain treatment adherence, follow up could be performed through telemedicine (phone contact, videocalls...) with lab tests as required.
More stringent follow-up is indicated in the following scenarios: adipsic DI, neurocognitive impairment that concerns water intake or previous episodes of hyponatraemia due to desmopressin overdose.
-
b.
COVID-19 in patients with chronic DI:
Cooperation between health care workers dealing with COVID-19 and clinicians with expertise in water balance disorders is paramount in this scenario. Some aspects of DI treatment may vary according to COVID-19 severity [2, 22]and water balance status on presentation.
Mild or moderate COVID-19
Outpatients with chronic DI and mild to moderate COVID-19 should at least have one blood and urine test measuring osmolality, sodium, creatinine and potassium during the acute phase and whenever the medical team has identified significant changes in factors influencing water balance (fever, loss of thirst sensation, hyperventilation...)
Hospital admission of COVID-19 patients with chronic DI, besides following COVID-19 evolution, should be implemented if there are significant changes in plasma sodium levels, loss of thirst or new-onset neurocognitive impairment that hinders outpatient management (see section on “severe COVID-19”)
Inpatient management: if admission is required for the treatment of COVID-19,conscious patients with intact thirst may maintain their usual desmopressin replacement regime with daily monitoring of plasma and urine sodium, potassium, creatinine and osmolality during the acute phase of COVID-19 as inpatients. Samples should be extracted one hour before the morning doseof desmopressin. It is strongly recommended that subjects with chronic DI wear medical alert bracelets or cards and duly inform their medical team of their condition at first contact. An example of medical alert card for diabetes insipidus created by our group is provided in Fig. 1.
Fig. 1.

Medical alert card for patients with diabetes insipidus
Severe COVID-19 in patients with chronic DI
It is mandatory to check daily fluid balance: oral and parenteral fluid administration (including fluids needed to administer parenteral drugs), diuresis and extrarenal fluid losses (i.e. diarrhea, vomiting, fever...).
- Daily monitoring of plasma and urine sodium, potasium, creatinine and osmolality
- Parenteral desmopressin administration should be first choice in severe COVID-19 patients to ensure stable and predictable desmopressin activity; conversion to parenteral doses should consider the pharmacokinetic bioequivalence among different administration routes: 1 mcg of parenteral desmopressin equals 10 mcg of intranasal and 100 mcg of oral desmopressin; thus, a patient on chronic treatment with intranasal desmopressin 10 mcg bd should be initially changed to 1 mcg parenteral DDAVP bd. It is advisable to ensure osmotic homeostasis is maintained through at least daily monitoring of plasma and urine osmolality [17]
- If intercurrent illness or underlying chronic conditions impair the patient’s ability to cover daily water, electrolytes and/or nutrients needs through oral intake, osmotic balance and nutritional status should be maintained using parenteral route. Standard fluid requirements include 25–30 ml/kg-day of water, 1 mmol/kg-day of potassium, sodium and chloride and 100–150 g/day of glucose. If extrarenal water loss increases, corrections should be implemented accordingly (diarrhea, vomiting...); i.e. daily water administration should increase by 100 ml for each temperature degree above 37 °C)
- If the patient needs enteral or parenteral nutritional support according to stablished guidelines, water, electrolyte and glucose replacement should be included in nutritional formulations [23].
- In obese patients with normal nutritional status, water, glucose and electrolyte requirements will be tailored to the patient’s ideal weight. Obesity often does not preclude malnutrition, which should be equally screened and treated.
- If a patient with chronic DI develops hyponatraemia during COVID-19, three underlying factors should be identified and treatment:
Desmopressin overdose, that can be corrected reducing the dose of DDAVP and monitoring clinical evolution (consciousness, gait, speech…) and biochemical evolution
Secondary adrenal insufficiency, common in patients with central DI and whose under-replacement might lead to hyponatraemia. To our knowledge, no case of adrenal insufficiency due to SARS-COV2 infection has been published so far.
Patients with hypopituitarism often suffer from metabolic comorbidities that make them prone to developing stress-induced hyperglycemia during COVID-19. Hyperglycemia might provoke increased osmotic diuresis and disturb water balance, particularly in patients with chronic DI. This situation should be dealt with treating hyperglycemia according to evidence-based guidelines and covering fluid losses orally or parenterally. Desmopressin dose, however, should not be modified if osmotic diuresis is the only factor altering water balance unless hypernatraemia develops.
Management of patients with chronic SIADH in COVID-19
Non-infected patients:
Patients with chronic SIADH should regularly receive clinical examination that includes the assessment of internal jugular vein pressure. These data are needed to appraise dose changes and even interruption of hyponatraemia pharmacotherapy (tolvaptan, urea...). Thus, patients with pharmacologically treated and chronic hyponatraemia are not fit for telemedicine follow-up appointments wherever this is problem is concerned.
- Patients with chronic SIADH usually suffer from malnutrition as well due to common precipitating factors (multimorbidity). Malnutrition is an absolute contraindication for water restriction as a treatment for hyponatraemia, as water-restricted dieting might worsen nutritional outcomes. In patients with SIADH and without malnutrition, confinement and/or loss of social interaction might also hinder adherence to water restriction; in this situation pharmacotherapy for hyponatraemia should also be considered according to stablished guidelines [9, 10].
- New-onset hyponatraemia and COVID-19:
Hyponatraemia, whatever the underlying causes, represents a risk factor for mortality and increased length of hospitalization. Therefore, hyponatraemia should be identified and treated accordingly in COVID-19 patients [12]
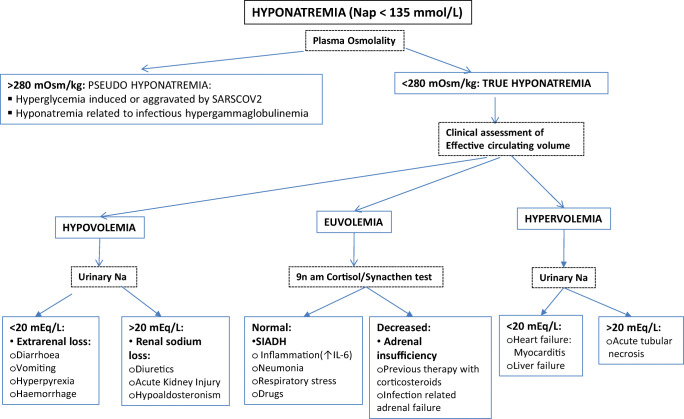
Diagnosis of new-onset hyponatraemia in COVID-19 patients should initially include plasma and urine osmolality, sodium and potassium and clinical assessment of volume status. Further etiological tests should be guided by the patient’s underlying conditions and risk factors, volume status and evolution. COVID-19 might be associated with multiple underlying disorders that might precipitate or aggravate hyponatraemia (Fig. 2). Among those etiologies, endocrinological assessment should include free thyroxine and thyroid stimulating hormone measurement, as COVID-19 can be associated with thyroid dysfunction [24], as well as diagnostic tests for adrenal insufficiency (9 am cortisol and/or synacthen test). Adrenal failure might be elicited by direct SARS-COV2 infiltration of adrenal cells or by dexamethasone-induced adrenal suprression [18, 25].
Patients suffering from COVID-19 should not be water-restricted in order to treat hyponatraemia. SARS-COV2 infection is often associated with malnutrition, increased perspiration and hyperventilation, and these factors may aggravate the adverse effects of water restriction. [2, 3, 23].
- Monitoring of COVID-19 patients with hyponatraemia should include daily measurements of plasma and urine sodium, potassium, creatinine and osmolality and clinical assessment of volume status (measurement of internal jugular vein pressure, intraocular pressure...). More intensive monitoring could be required in patients with severe hyponatraemia or those with rapidly evolving hyponatraemia.
- Hyponatraemia pharmacotherapy during COVID-19:
-
i.Indications for hyponatraemia pharmacotherapy in COVID-19 patients: euvolemic hyponatraemia with plasma sodium >120 mEq/l, after excluding adrenal insufficiency and hypothyroidism. Most COVID-19 patients will not be suitable candidates for water restriction as a treatment for hyponatraemia due to malnutrition, loss of thirst and increased extraurinary water loss. These patients should therefore be treated with tolvaptan or urea according to clinical guidelines [13, 14].
-
ii.Treatment interactions between hyponatraemia and SARS-COV2 pharmacotherapy: described in Table 1 and for each drug in its specific section.
-
i.
Fig. 2.
Hyponatraemia diagnostic algorithm in COVID-19 patients
Table 1.
| Hyponatraemia drug | Lopinavir/ritonavir | Tocilizumab | Remdesivir | Hydroxychloroquine | Dexamethasone |
|---|---|---|---|---|---|
| Tolvaptan |
↑Tolvaptan concentrations (CYP3A4 inhibition) |
↓Tolvaptan concentrations (CYP3A4 activation) |
↑Tolvaptan concentrations (CYP3A4 inhibition) |
None | None |
| Urea | No clinical experience published in COVID-19 | ||||
| Furosemide | – | – | – | – | Corticosteroids may ↑hypokalemia |
Patients with plasma sodium <120 mEq/l regardless of their clinical status or > 120 mEq/l with severe neurological symptoms should be treated with hypertonic saline serum according to published evidence-based guidelines [13, 14]
Euvolemic or hypervolemic hyponatraemia, particularly with urine osmolality >350 mOsm/kg, may be treated with loop diuretics after an oral load of 4–5 g of NaCl [26]
Hypovolaemic hyponatraemia may be treated with isotonic saline fluids, no more than 30 ml/kg-day to avoid hypercorrection [27].
c.1 Tolvaptan in COVID-19 patients:
Initialdose: 7.5 mg/day
Contraindicated if severe liver or kidney failure (Child C orGFR <30 ml/min).
- Precautions:
- Treatment with lopinavir/ritonavir inhibits CYP3A4, a potent pharmacological interaction with tolvaptan that increases plasma levels of the latter and could increase its acuaretic effect. Simultaneous use of both compounds should be closely monitored [28]
- Tocilizumab enhances CYP3A4 activity, which could decrease tolvaptan’s circulating levels and its acuaretic effect [29]
- No significant interactions have been described between hydroxychloroquine and any drug licensed for use in hyponatraemia
c.2 Urea in COVID-19:
No clinical experience has been published with urea in SARS-COV2 infected patients with hyponatraemia
- Warnings:
- Urea may decrease thirst, treated patients should be monitored, measuring intake and loss of fluids, changes in thirst, urine volume and new-onset nocturia.
c.3 Furosemide in COVID-19 patients:
Management of hypernatraemia in COVID-19
Hypernatraemia is a common laboratory abnormality in COVID-19 patients, found in 3,7% of patients hospitalised due to COVID-19 in the HOPE registry [9]. Similarly to hyponatraemia, increased plasma sodium levels are an adverse prognostic factor in non-COVID patients although this awaits confirmation in COVID-19 series. Hypernatraemia in COVID-19 develops due to an inbalance between increased water loss (hyperpyrexia, diarrhoea, vomiting, polyuria due to hyperglycemia or acute kidney injury...) and decreased water supply (anorexia with adipsia, altered consciousness, insufficient parenteral replacement...) [31, 32].
Diabetes insipidus as a direct consequence of SARS-COV2 has not been pathophysiologically described so far. Therefore, while awaiting descriptive studies of hypernatraemia in this population, it could be safely assumed that COVID-19 patients with hypernatraemia mostly suffer increased extrarenal water loss.
Treatment of hypernatraemia in COVID-19 patients is similar to that described in the general population, based on parenteral fluid replacement [31].
General recommendations:
Thrombosis prevention: hypernatraemia and SARS-COV2 infection are both independent thrombosis risk factors. If no contraindication is found, low weight heparine profilaxis should be initiated on admission.
Plasma and urine sodium measurement every 12–24 h
Objective: reduction of sodium levels <10 mEq/l every 24 h to reduce the risk of cerebral edema
- Severe hypernatraemia with loss of consciousness
- Dextrose 5% serum at 1.35 ml/kg-hour
- If there is clinical hypovolaemia, administer isotonic serum (saline serum 0,9% or Ringer) parallel to dextrose at 30 ml/kg/day to increase effective circulating volume. Patients with increased risk of cerebral edema (liver failure, heart failure) may receive instead saline serum 0,45% at 30 ml/kg-day.
Data availability
not applicable.
Compliance with ethical standards
Conflict of interest
none relevant to the article.
Ethics approval
not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO Coronavirus Disease dashboard [Internet]. Available from: https://covid19.who.int. Accessed 3 Oct 2020.
- 2.Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020. [DOI] [PubMed]
- 3.Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, Bikdeli B, Ahluwalia N, Ausiello JC, Wan EY, Freedberg DE, Kirtane AJ, Parikh SA, Maurer MS, Nordvig AS, Accili D, Bathon JM, Mohan S, Bauer KA, Leon MB, Krumholz HM, Uriel N, Mehra MR, Elkind MSV, Stone GW, Schwartz A, Ho DD, Bilezikian JP, Landry DW. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 4.De La Flor Merino JC, Mola Reyes L, Linares Gravalos T, Roel Conde A, Rodeles Del Pozo M. An unusual case of severe acute hyponatraemia in patient with COVID-19 infection. Nefrol Publicacion Of Soc Espanola Nefrol. 2020;40(3):356–358. doi: 10.1016/j.nefro.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mansoor E, Khoudari G, Abou Saleh M, Elfadawy N, Cooper GS, Katz J, et al. The many faces of COVID-19: atypical presentation of COVID-19 in a patient with Crohn’s disease with acute diarrhea leading to severe hypovolemic Hyponatraemia-a case report. Am J Gastroenterol. 2020 Aug;19. [DOI] [PMC free article] [PubMed]
- 6.Tee LY, Yap B, Sidhu GK, Goh KS, Rosario BH. Atypical presentation of COVID-19 in an older adult: lethargy and vomiting from severe hypovolemic Hyponatraemia. Geriatr Gerontol Int. 2020 Jul;8. [DOI] [PMC free article] [PubMed]
- 7.Khan AA, Ata F, Munir W, Yousaf Z. Fluid replacement versus fluid restriction in COVID-19 associated Hyponatraemia. Cureus. 2020;12(7):e9059. doi: 10.7759/cureus.9059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aggarwal S, Garcia-Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): early report from the United States. Diagn Berl Ger. 2020;7(2):91–96. doi: 10.1515/dx-2020-0046. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz-Sánchez JG, Núñez-Gil IJ, Cuesta M, Rubio MA, Maroun-Eid C, Arroyo-Espliguero R, et al. Prognostic Impact of Hyponatraemia and Hypernatraemia in COVID-19 Pneumonia. A HOPE-COVID-19 (Health Outcome Predictive Evaluation for COVID-19) Registry Analysis. Front Endocrinol [Internet]. 2020 [cited 2021 Jan 6]; 11. Available from: 10.3389/fendo.2020.599255/full. [DOI] [PMC free article] [PubMed]
- 10.Christ-Crain M, Hoorn EJ, Sherlock M, Thompson CJ, Wass JAH. ENDOCRINOLOGY IN THE TIME OF COVID-19: management of diabetes insipidus and hyponatraemia. Eur J Endocrinol. 2020;183(1):G9–15. doi: 10.1530/EJE-20-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baldeweg, S.E., Ball, S B, Brooke, A, Gleeson, H.K.G., Levy, M. J., Prentice, M., et al. Society for Endocrinology Clinical Guidance: Inpatient Management of Cranial Diabetes Insipidus. Endocrine connections. 2018. [DOI] [PMC free article] [PubMed]
- 12.Cuesta M, Garrahy A, Slattery D, Gupta S, Hannon AM, McGurren K. Mortality rates are lower in SIAD, than in hypervolaemic or hypovolaemic hyponatraemia: Results of a prospective observational study. Clin Endocrinol. et al., 2017. [DOI] [PubMed]
- 13.Verbalis J. Goldsmith, Gd, Greenberg, mark, Schrier, sterns, Rh S. Hyponatraemia treatment guidelines 2007: expert panel recommendations. Am J Med. 2007;126(10 Suppl 1):S1–42. doi: 10.1016/j.amjmed.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Spasovski G, Vanholder R, Allolio B, Djillali A, Ball S, Bichet D, et al. Clinical practice guideline on diagnosis and treatment of Hyponatraemia. Eur J Endocrinol. 2014;170(3):G1–47. doi: 10.1530/EJE-13-1020. [DOI] [PubMed] [Google Scholar]
- 15.Hew-Butler T, Smith-Hale V, Pollard-McGrandy A, VanSumeren M. Of mice and men-the physiology, psychology, and pathology of Overhydration. Nutrients. 2019;11(7):1539. doi: 10.3390/nu11071539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kataok Y, Nishida S, Hirakawa A, Oiso Y, Arima H. Comparison of incidence of hyponatraemia between intranasal and oral desmopressin in patients with central diabetes insipidus. Endocr J. 2015;62(2):195–200. doi: 10.1507/endocrj.EJ14-0368. [DOI] [PubMed] [Google Scholar]
- 17.Lamas C, del Pozo C, Villabona C. Clinical guidelines for management of diabetes insipidus and syndrome of inappropriate antidiuretic hormone secretion after pituitary surgery. Endocrinol Nutr Organo Soc Espanola Endocrinol Nutr. 2014;61(4):15–24. doi: 10.1016/j.endonu.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Arlt W, Baldeweg SE, Pearce SHS, Simpson HL. ENDOCRINOLOGY IN THE TIME OF COVID-19: management of adrenal insufficiency. Eur J Endocrinol. 2020;183(1):G25–G32. doi: 10.1530/EJE-20-0361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caci G, Albini A, Malerba M, Noonan DM, Pochetti P, Polosa R. COVID-19 and Obesity: Dangerous Liaisons. J Clin Med. 2020;9(8). [DOI] [PMC free article] [PubMed]
- 20.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miljic D, Miljic P, Doknic M, Pekic S, Stojanovic M, Petakov M, et al. Adipsic diabetes insipidus and venous thromboembolism (VTE): recommendations for addressing its hypercoagulability. Horm Athens Greece. 2014;13(3):420–423. doi: 10.14310/horm.2002.1496. [DOI] [PubMed] [Google Scholar]
- 22.Gandhi RT, Lynch JB, del Rio C. Mild or Moderate Covid-19. N Engl J Med. 2020. [DOI] [PubMed]
- 23.Arkin N, Krishnan K, Chang M, Bittner E. Nutrition in critically ill patients with COVID-19: challenges and special considerations. Clin Nutr Edinb Scotl. 2020;39(7):2327–2328. doi: 10.1016/j.clnu.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scappaticcio L, Pitoia F, Esposito K, Piccardo A, Trimboli P. Impact of COVID-19 on the thyroid gland: an update. Rev Endocr Metab Disord. 2020;25:1–13. doi: 10.1007/s11154-020-09615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferraù F, Ceccato F, Cannavò S, Scaroni C. What we have to know about corticosteroids use during Sars-Cov-2 infection. J Endocrinol Investig. 2020;28:1–9. doi: 10.1007/s40618-020-01384-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ortola A, Crespo I, Ruiz-Gracia T, Gomez-Hoyos E, Cuesta M, Penso R, et al. The use of an oral salt load followed by furosemide in the treatment of euvolemic SIADH-induced hyponatraemia. In BioScientifica; 2015 [cited 2020 Aug 30]. Available from: https://www.endocrine-abstracts.org/ea/0037/ea0037ep672
- 27.Ruiz-Sánchez JG, Meneses D, Álvarez-Escolá C, Cuesta M, Calle-Pascual AL, Runkle I. The Effect of the Dose of Isotonic Saline on the Correction of Serum Sodium in the Treatment of Hypovolemic Hyponatremia. Journal of Clinical Medicine. 2020;9(11):3567.https://www.researchgate.net/publication/329923614_Hyponatraemia_hipovolemica_dosis_umbral_de_suero_salino_fisiologico_para_evitar_sobrecorreccion [DOI] [PMC free article] [PubMed]
- 28.Shoaf SE, Bricmont P, Mallikaarjun S. Effects of CYP3A4 inhibition and induction on the pharmacokinetics and pharmacodynamics of tolvaptan, a non-peptide AVP antagonist in healthy subjects. Br J Clin Pharmacol. 2012;73(4):579–587. doi: 10.1111/j.1365-2125.2011.04114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S. Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther. 2011;89(5):735–740. doi: 10.1038/clpt.2011.35. [DOI] [PubMed] [Google Scholar]
- 30.Tomasoni D, Italia L, Adamo M, Inciardi RM, Lombardi CM, Solomon SD, et al. COVID 19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail. 2020;15. [DOI] [PMC free article] [PubMed]
- 31.Muhsin SA, Mount DB. Diagnosis and treatment of hypernatraemia. Best Pract Res Clin Endocrinol Metab. 2016;30(2):189–203. doi: 10.1016/j.beem.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 32.Rondon-Berrios H, Argyropoulos C, Ing TS, Raj DS, Malhotra D, Agaba EI, Rohrscheib M, Khitan ZJ, Murata GH, Shapiro JI, Tzamaloukas AH. Hypertonicity: clinical entities, manifestations and treatment. World J Nephrol. 2017;6(1):1–13. doi: 10.5527/wjn.v6.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Widmer P, Maibach R, Künzi UP, Capaul R, Mueller U, Galeazzi R, et al. Diuretic-related hypokalaemia: the role of diuretics, potassium supplements, glucocorticoids and beta 2-adrenoceptor agonists. Results from the comprehensive hospital drug monitoring programme, berne (CHDM) Eur J Clin Pharmacol. 1995;49(1–2):31–36. doi: 10.1007/BF00192355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
not applicable.