Abstract
Precision immunotherapy is a crucial approach to improve the efficacy of anti-cancer treatments, particularly in the metastatic setting. In this respect, accurate patient selection takes advantage of the multidimensional integration of patients’ clinical information and tumour-specific biomarkers status. Among these biomarkers, programmed death-ligand 1, tumour-infiltrating lymphocytes, microsatellite instability, mismatch repair and tumour mutational burden have been widely investigated. However, novel tumour-specific biomarkers and testing methods will further improve patients’ outcomes. Here, we discuss the currently available strategies for the implementation of a precision immunotherapy approach in the clinical management of metastatic solid tumours and highlight future perspectives.
Keywords: biomarkers, immunotherapy, PD-L1, TILs, mismatch repair, TMB
Introduction
Immune checkpoint inhibition has been increasingly applied in several solid tumours, with significant survival benefits, providing a precise patient selection [1–3]. Hence, not all the patients, even in the presence of similar clinical characteristics, would respond in the same way to the same immunotherapy protocol [4]. Furthermore, the toxicity and adverse events of such agents are not uncommon and should be taken into account while assessing the patient’s eligibility [5, 6]. In this scenario, the application of tailored immunotherapy schemes is of great importance.
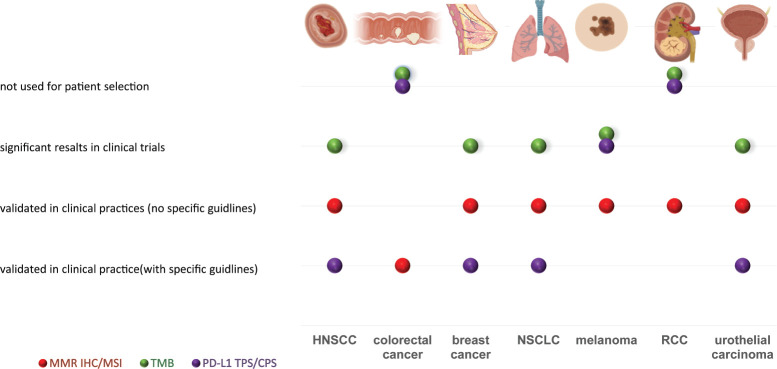
In this era of histology-agnostic approvals, the identification of tumour-specific biomarkers and interpretation guidelines is a growing opportunity [7, 8]. Currently, the most studied immune-related biomarkers include programmed death-ligand 1 (PD-L1), tumour-infiltrating lymphocytes (TILs), microsatellite instability (MSI), mismatch repair (MMR) and tumour mutational burden (TMB) [9]. The level of approval of these tests is shown in Figure 1. There are currently multiple lines of evidence on the overall better response rate of TMB-high, MSI-high and PD-L1POS tumours treated with immunotherapy [10, 11]. Additionally, there are several indications that candidate complementary and/ or surrogate biomarkers (e.g. phosphatase and tensin homologue ) may contribute to an optimal patient selection [12–16]. Novel means of mutation measurement as comprehensive genomic profiling (CGP) are currently being explored in this setting [17].
Figure 1. Schematic representation of the main fields of applications of MMR/MSI, PD-L1, TMB testing in patients’ selection for immunotherapy. Tumours are depicted in the columns, while the application of the test in the rows. The colour-coded circles refer to the selected testing method provided on the bottom left legend. The circles are distributed among different anatomical sites based on their clinical utility, as reported on the column placed on the left. MMR, mismatch repair; MSI, microsatellite instability; PD-L1, programmed cell death ligand 1; TMB, tumour mutational burden; IHC, immunohistochemistry; HNSCC, head and neck squamous cell carcinoma; NSCLC, non-small cell lung cancer; RCC, renal cell carcinoma.
Tumour-specific biomarkers, coupled with companion diagnostics (CDx), may enhance the process of precise patients’ selection, leading to a higher probability of reaching satisfying clinical outcomes [18]. In this review article, we illustrate the impacts and gaps of biomarkers suggested by previous clinical trials and translational research studies in immuno-oncology treatments. A particular focus will be given on the hopes and facts behind the concept of ‘precision immunotherapy’.
Immunotherapy in clinical practice
Cancer cells can evade the immune system through downregulation or loss of tumour antigens and alterations in the expression of costimulatory and coinhibitory molecules [19, 20]. Under normal conditions, antigens conjugated with major histocompatibility complex (MHC) molecules are presented on the surface of cancer cells. These antigens can be recognised by T cells possessing the same MHC alleles through T-cell receptors–antigen/MHC interactions [21]. For an optimal T cell response, a second signal mediated by co-stimulatory molecules is required. CD28 binds to CD80 and/or CD86, which are present on the surface of activated antigen-presenting cells [22]. Cytotoxic T-lymphocyte antigen 4 (CTLA4) is homologous to CD28 and similarly binds to CD80 or CD86, preventing the attachment of CD28 to these surface proteins. In other words, CTLA4 is a negative regulatory molecule of T cell activation [22, 23]. The pharmacologic inhibition of CTLA4 is one of the possible approaches employed in cancer immunotherapy [22]. The checkpoint axis programmed cell death protein 1 (PD-1)/PD-L1 is another widely explored target [24]. When PD-1 binds to its ligands named as PD-L1 and PD-L2, T cells undergo a negative regulatory process referred to as immune checkpoint [25]. Antibodies that block PD-1 or PD-L1 lead to activation of T cells which can subsequently recognise and attack cancer cells [26]. The therapeutic antibody ipilimumab, targeting CTLA-4, is the first approved checkpoint inhibitor for clinical use in melanoma [27]. Additionally, anti-PD-1 molecules for the management of malignancies such as non-small cell lung cancer (NSCLC), renal cell carcinoma (RCC), Hodgkin lymphoma, melanoma, urothelial carcinoma, metastatic colorectal cancer and hepatocellular carcinoma are Food and Drugs Administration (FDA)-consented to be prescribed [28], as summarised in Table 1. Clinical use of immune checkpoint inhibitors (ICPis) may bring along undesired side effects termed as immune-related adverse events (irAEs) [29]. Reportedly, anti-CTLA-4 therapy often results in more severe side effects comparing to other immunotherapy agents [30]. Organs such as intestine, liver, lung, skin and endocrine glands are frequently affected by immunotherapy toxicity [31]. Around 13%–17% of NSCLC patients treated with anti-PD-1 experienced grade 3 or higher toxicities [32]. Yet, less than 20% of patients show high-grade toxicity when treated with anti-PD-1 and/or anti-PD-L1 [33]. Most of the side effects are tackled by corticosteroids and other adjunctive medications effectively [34].
Table 1. Summary of immune checkpoint blockade therapies which have been approved by the FDA for being applied in clinical practices. https://www.fda.gov/.
| Antibody | Immunotherapy | Trading name | Cancer type | Indications | Date of approval |
|---|---|---|---|---|---|
| anti–PD-L1 | Durvalumab |
O IMFINZI, AstraZeneca + etoposide and either carboplatin or cisplatin |
Extensive-stage small cell lung cancer (ES-SCLC) | First-line treatment | March 30, 2020 |
| O IMFINZI, AstraZeneca Inc. | Unresectable stage III non-small cell lung cancer (NSCLC) |
Disease should not be progressed following concurrent platinum-based chemotherapy and radiation therapy | February 16, 2018 | ||
| O IMFINZI, AstraZeneca UK Limited) | locally advanced or metastatic urothelial carcinoma |
disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy | May 1, 2017 | ||
| Avelumab |
O BAVENCIO, EMD Serono Inc. + axitinib |
Advanced renal cell carcinoma (RCC) | First-line treatment | May 14, 2019 | |
| O BAVENCIO, EMD Serono, Inc. | Locally advanced or metastatic urothelial carcinoma | Progressed disease during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant platinum-containing chemotherapy | May 9, 2017 | ||
| O BAVENCIO, EMD Serono, Inc. | Metastatic Merkel cell carcinoma (MCC). | The first FDA-approved product to treat this type of cancer. For 12 years and older |
March 23, 2017 | ||
| Atezolizumab | O TECENTRIQ®, Genentech Inc. | Metastatic non-small cell lung cancer (NSCLC) | first-line treatment adults with high PD-L1 expression (PD-L1 stained ≥ 50% of tumour cells [TC ≥ 50%] or PD-L1 stained tumour-infiltrating immune cells [IC] covering ≥ 10% of the tumour area [IC ≥ 10%]), with no EGFR or ALK genomic tumour aberrations. |
May 18, 2020 | |
|
O TECENTRIQ, Genentech Inc. + paclitaxel protein-bound and carboplatin |
Metastatic non-squamous non-small cell lung cancer (NSCLC) | First-line treatment for adults (with no EGFR or ALK genomic tumour aberrations) |
December 3, 2019 | ||
|
O TECENTRIQ, Genentech Inc. + carboplatin and etoposide |
Extensive-stage small cell lung cancer (ES-SCLC) | First-line treatment for adults | March 18, 2019 | ||
|
O TECENTRIQ, Genentech Inc. + paclitaxel protein-bound |
Unresectable locally advanced or metastatic triple-negative breast cancer | PD-L1 (SP142) positive | March 8, 2019 | ||
| O TECENTRIQ, Genentech, Inc. + bevacizumab, paclitaxel, and carboplatin |
Metastatic non-squamous, non-small cell lung cancer (NSq NSCLC) | First-line treatment of patients with no EGFR or ALK genomic tumour aberrations. | December 6, 2018 | ||
| O TECENTRIQ, Genentech Inc. | Locally advanced or metastatic urothelial carcinoma | Not eligible for cisplatin-containing chemotherapy, and whose tumours express PD-L1 (PD-L1 stained tumour-infiltrating immune cells [IC] covering ≥5% of the tumour area) Or Not eligible for any platinum-containing therapy regardless of level of tumour PD-L1 expression |
August 16, 2018. | ||
| O TECENTRIQ, Genentech Oncology | Metastatic non-small cell lung cancer (NSCLC) | Progressed disease during or following platinum-containing chemotherapy EGFR or ALK genomic tumour aberrations with disease progression |
October 18, 2016 | ||
| O TECENTRIQ, Genentech Inc. | Locally advanced or metastatic urothelial carcinoma | Disease progression during or following platinum-containing chemotherapy or Progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy |
May 18, 2016 | ||
| anti–PD-1 |
Nivolumab | O OPDIVO, Bristol-Myers Squibb Company. | Metastatic small cell lung cancer (SCLC) | Progression after platinum-based chemotherapy and at least one other line of therapy | August 16, 2018 |
| O OPDIVO, Bristol-Myers Squibb Company | Melanoma | Adjuvant treatment with involvement of lymph nodes or with metastatic disease who have undergone complete resection. |
December 20, 2017 | ||
| O OPDIVO, Bristol-Myers Squibb Co. | Hepatocellular carcinoma (HCC) | Previously treated with sorafenib. | September 22, 2017 | ||
| O OPDIVO, Bristol-Myers Squibb Co. | Metastatic colorectal cancer | -12 years and older -Mismatch repair deficient (dMMR) and microsatellite instability high (MSI-H) -Malignancy progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan |
August 1, 2017 | ||
| O OPDIVO, Bristol-Myers Squibb Co. | Locally advanced or metastatic urothelial carcinoma | Progression during or following platinum-containing chemotherapy or Have disease progression within 12 months of neoadjuvant or adjuvant treatment with a platinum-containing chemotherapy |
February 2, 2017 | ||
| O OPDIVO, Bristol-Myers Squibb Co. | Recurrent or metastatic squamous cell carcinoma of the head and neck (SCCHN) | Progression on or after a platinum-based therapy | November 10, 2016 | ||
| O OPDIVO, Bristol-Myers Squibb Co | Advanced renal cell carcinoma | Patients who have received prior anti-angiogenic therapy | November 23, 2015 | ||
| O OPDIVO, Bristol-Myers Squibb Co | Metastatic non-small cell lung cancer (NSCLC) | Progression on or after platinum-based chemotherapy. EGFR or ALK genomic tumour aberrations should have disease progression on FDA-approved therapy for these aberrations prior to therapy |
October 9, 2015 | ||
| O OPDIVO, Bristol-Myers Squibb Co | Unresectable or metastatic melanoma | Progression following ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor | December 22, 2014 | ||
| pembrolizumab | O KEYTRUDA, Merck & Co. Inc | New dosing regimen | 400 mg every 6 weeks for pembrolizumab across all currently approved adult indications, in addition to the current 200 mg every three weeks dosing regimen. | April 28, 2020 | |
| O KEYTRUDA, Merck & Co. Inc. | Bacillus Calmette-Guerin (BCG)-unresponsive, high-risk, non-muscle invasive bladder cancer (NMIBC) | With carcinoma in situ (CIS) with or without papillary tumours who are ineligible for or have elected not to undergo cystectomy. | January 8, 2020 | ||
|
O KEYTRUDA, Merck + lenvatinib (LENVIMA, Eisai) |
Advanced endometrial carcinoma | That is not microsatellite instability high (MSI-H) or mismatch repair deficient (dMMR) Have disease progression following prior systemic therapy but are not candidates for curative surgery or radiation. |
September 17, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Advanced esophageal squamous cell cancer | Tumour PD-L1 expression (Combined Positive Score [CPS] ≥10), determined by an FDA-approved test Disease progression after one or more prior lines of systemic therapy. |
July 30, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Metastatic small cell lung cancer (SCLC) | Disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy. | June 17, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Metastatic small cell lung cancer (SCLC) | Disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy. | June 17,2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Metastatic or unresectable recurrent head and neck squamous cell carcinoma (HNSCC) | First-line treatment |
June 10, 2019 | ||
|
O KEYTRUDA, Merck & Co. Inc. + axitinib |
Advanced renal cell carcinoma (RCC) | First-line treatment |
April 19, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Stage III non-small cell lung cancer (NSCLC) | First-line treatment -Not candidates for surgical resection or definitive chemoradiation or metastatic NSCLC. -Patients’ tumours must have no EGFR or ALK genomic aberrations and express PD-L1 (Tumour Proportion Score [TPS] ≥1%) determined by an FDA-approved test. |
April 11, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Melanoma | Adjuvant treatment -With involvement of lymph node(s) following complete resection. |
February 15, 2019 | ||
| O KEYTRUDA, Merck & Co. Inc. | Recurrent locally advanced or metastatic Merkel cell carcinoma (MCC) | Adult and pediatric patients | December 19, 2018 | ||
| O KEYTRUDA, Merck & Co. Inc. | Hepatocellular carcinoma (HCC) | Previously treated with sorafenib | November 9, 2018 | ||
|
O KEYTRUDA, Merck & Co. Inc. + carboplatin and either paclitaxel or nab-paclitaxel |
Metastatic squamous non-small cell lung cancer (NSCLC) | First-line treatment | October 30, 2018 | ||
|
O KEYTRUDA, Merck & Co. Inc. + Pemetrexed,platinum |
Metastatic, non-squamous non-small cell lung cancer (NSqNSCLC) | First-line treatment with no EGFR or ALK genomic tumour aberrations |
August 20, 2018 | ||
| O KEYTRUDA, Merck & Co. Inc | Locally advanced or metastatic urothelial cancer |
PD-L1 levels evaluation in tumour tissue who are cisplatin-ineligible. PD-L1 expression CPS ≥ 10 as determined by an FDA-approved test Or not eligible for any platinum-containing chemotherapy regardless of PD-L1 status |
August 16, 2018 | ||
| O KEYTRUDA, Merck & Co. Inc | Refractory primary mediastinal large B-cell lymphoma (PMBCL) | Treatment of adult and pediatric patients, relapsed after two or more prior lines of therapy. |
June 13, 2018 | ||
| O KEYTRUDA, Merck & Co. Inc | Recurrent or metastatic cervical cancer | Disease progression on or after chemotherapy PD-L1 expression (CPS ≥1) as determined by an FDA-approved test |
June 12, 2018 | ||
| O KEYTRUDA, Merck & Co. Inc | Recurrent locally advanced or metastatic, gastric or gastroesophageal junction adenocarcinoma | PD-L1 expression as determined by an FDA-approved test Disease progression on or after two or more prior systemic fluoropyrimidine- and platinum-containing chemotherapy and, HER2/neu-targeted therapy |
September 22, 2017 |
||
| O KEYTRUDA, Merck & Co. Inc | Unresectable or metastatic colorectal cancer | Adult and pediatric patients unresectable or metastatic, MSI-H or dMMR solid tumours progressed following prior treatment with no satisfactory alternative treatment options or MSI-H or dMMR colorectal cancer that has progressed following treatment with a fluoropyrimidine, oxaliplatin, and irinotecan. |
May 23, 2017 | ||
| O KEYTRUDA, Merck & Co. Inc | Locally advanced or metastatic urothelial carcinoma | Disease progression during or following platinum-containing chemotherapy or within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. | May 18, 2017 | ||
|
O KEYTRUDA, Merck & Co. Inc + pemetrexed and carboplatin |
Metastatic non-squamous non-small cell lung cancer (NSCLC) | Previously untreated | May 10, 2017 | ||
| O KEYTRUDA, Merck & Co. Inc | Metastatic non-small cell lung cancer (NSCLC) | Tumours express PD-L1 as determined by an FDA-approved test | October 24, 2016 | ||
| O KEYTRUDA, Merck & Co. Inc | Recurrent or metastatic head and neck squamous cell carcinoma (HNSCC) | Disease progression on or after platinum-containing chemotherapy | August 5, 2016 | ||
| O KEYTRUDA, Merck & Co. Inc | Unresectable or metastatic melanoma | . | December 18, 2015 | ||
| O KEYTRUDA, Merck & Co. Inc | Metastatic non-small cell lung cancer (NSCLC) | Tumours express PD-L1 as determined by an FDA-approved test, with disease progression on or after platinum-containing chemotherapy | October 2, 2015 | ||
| O KEYTRUDA, Merck & Co. Inc | Unresectable or metastatic melanoma | Disease progression following ipilimumab BRAF V600 mutation positive |
September 4, 2014 | ||
| anti-CTLA4 | Ipilimumab | O YERVOY, Bristol-Myers Squibb Company | Cutaneous melanoma | Additional indication of adjuvant treatment of patients Pathologic involvement of regional lymph nodes of more than 1 mm who have undergone complete resection, including total lymphadenectomy |
October 28, 2015 |
| O YERVOY, Bristol-Myers Squibb Company | Unresectable or metastatic melanoma | March 25, 2011 | |||
| Nivolumab + ipilimumab |
O nivolumab (OPDIVO, Bristol-Myers Squibb Co.) + ipilimumab (YERVOY, Bristol-Myers Squibb Co.) + 2 cycles of platinum-doublet chemotherapy |
Metastatic or recurrent non-small cell lung cancer (NSCLC), with no epidermal | As first-line treatment With growth factor receptor (EGFR) or anaplastic lymphoma kinase(ALK) genomic tumour aberrations. |
May 26, 2020 | |
| Combination therapy | O nivolumab (OPDIVO, Bristol-Myers Squibb Co.) + ipilimumab (YERVOY, Bristol-Myers Squibb Co.) |
Metastatic non-small cell lung cancer | As first-line treatment Tumours express PD-L1(≥1%), as determined by an FDA-approved test With no epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genomic tumour aberrations |
May 15, 2020 | |
| O nivolumab (OPDIVO, Bristol-Myers Squibb Co.) + ipilimumab (YERVOY, Bristol-Myers Squibb Co.) |
Hepatocellular carcinoma (HCC) | Previously treated with sorafenib.. | March 10, 2020 | ||
|
O nivolumab (OPDIVO, Bristol-Myers Squibb Co.) + ipilimumab (YERVOY, Bristol-Myers Squibb Co.) |
Advanced renal cell carcinoma | Intermediate or poor risk previously untreated |
April 16, 2018 | ||
|
O nivolumab (OPDIVO, Bristol-Myers Squibb Co.) + ipilimumab (YERVOY, Bristol-Myers Squibb Co.) |
Unresectable or metastatic melanoma | With BRAF V600 wild-type | September 30, 2015 |
O approved
O accelerated approva
O updated prescribing information
ALK: anaplastic lymphoma kinase; EGFR: epidermal growth factor receptor; HER2: human epidermal growth factor receptor 2
The quantum leap of immune-related biomarkers
Programmed death ligand 1 (PD-L1)
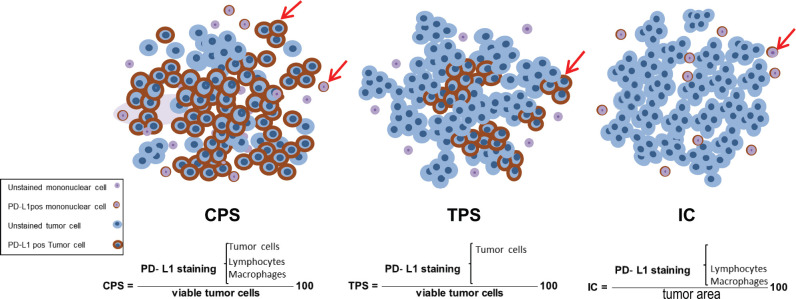
In 2015, FDA approved pembrolizumab as the first PD-1 inhibitor in NSCLC [35]. Since then, different clones of the antibody against PD-1 ligand, such as SP142 (Ventana Medical Systems), SP263 (Ventana Medical Systems) and 22C3 (Dako North America, Inc.) were validated as specific biomarkers for patient selection [36]. Immunohistochemistry (IHC) assessment of PD-L1 is employed for patient selection in several cancers [37]. PD-L1 evaluation differs in each tumour type, thus a conclusive protocol may not fit all malignancies. For instance, tumour proportion score (TPS) which is functional in lung cancer cannot be tailored for head and neck cancer, and vice versa for the combined positive score (CPS) [38]. TPS considers PD-L1-positivity merely in neoplastic cells, whereas CPS considers the positivity of tumour cells, lymphocytes and macrophages. CPS equals the number of PD-L1 positive tumour cells and lymphocytes, divided by the total number of viable tumour cells, multiplied by 100. Another example is represented by triple-negative breast cancers (TNBC), where the CDx test for this indication was PD-L1 (SP142) IHC Assay by using the immune cell (IC) scoring system [39]. IC scoring was considered as positive, for those with the presence of PD-L1POS ICs that covered more than 1% of the tumour area (tumour cells, associated intratumoural and contiguous peritumoural stroma) [2]. The PD-L1 scoring systems are shown in Figure 2. Pre-analytical and informative phases of PD-L1 testing have been coordinated in NSCLC where the propagative application of PD-L1 testing in clinical practices indicated coinciding results, mostly by using the 22C3 antibody clone [40]. PD-L1 plays a significant role in the NSCLC treatment profile. In this malignancy, PD-L1 expression is assessed by TPS of membrane expression [41]. Based on KEYNOTE‑042 (NCT02220894), pembrolizumab is approved as the first-line treatment of stage III NSCLC patients with no epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genomic aberrations, while also the tumour must express PD-L1 (TPS ≥1%) [42].
Figure 2. Schematic representation of the available scoring criteria for PD-L1 assessment. CPS counts for both tumour and mononuclear cells which are PD-L1pos among total viable tumour cells, multiplied by 100. While TPS and IC are contributed to PD-L1pos, tumour cells and mononuclear cells, respectively, divided by total number of viable tumour cells. PD-L1 stained and unstained tumour and mononuclear cells are depicted on the left bottom legend. PD-L1, programmed cell death ligand 1, CPS, combined positive score; TPS, tumour proportion score; IC, immune cell.
PD-L1 assessment is debated among scientists. In head and neck squamous cell carcinoma (HNSCC), irrespective of PD-L1 expression status, immunotherapy with nivolumab and pembrolizumab is consented by FDA for the second-line treatment of recurrent and/or metastatic HNSCC [43]. These agents show a greater overall survival (OS) in comparison with the standard, single-agent treatment in those with platinum-refractory, recurrent or metastatic HNSCC [44]. According to Ferris et al individuals treated with nivolumab, regardless of tumour PD-L1 expression, appeared to have greater OS than those treated with standard therapy. However, they noted that patients with a tumour PD-L1 expression level of more than 1% may benefit more from nivolumab therapy than those whose PD-L1 level was less than 1% [45].
In HNSCC, CPS is recommended for PD-L1 evaluation, where CPS > 20 represents a significantly longer OS [46]. In melanoma, tumours with PD-L1-overexpression are related to a fairly high response rate (>50%) and longer progression-free survival (PFS) and OS [47]. In PD-L1 positive, advanced and refractory gastric cancer (GC), those treated with pembrolizumab presented a greater objective response rate (ORR). Added to this, PD-L1 negative cases had also shown responses [48]. Regarding RCC, a meta-analysis comprising 4,063 patients suggested a greater OS and PFS in PD-L1 positive tumours [49]. In urothelial carcinoma, patients with high PD-L1 expression had a greater ORR and OS rate [50]. In TNBC, studies indicate that PD-L1 is highly expressed which suggests a potential role for immunotherapy [51]. Pembrolizumab implies durable anti-cancer effects in a small subset of PD-L1 positive metastatic TNBC [52].
Tumour-infiltrating lymphocytes (TILs)
Leukocytes are thought to be involved in both protumour and antitumour activities [53–55]. Molecular factors formed by ICs may lead to cancer cells’ fate of death or survival [4]. Lymphocytes migrated within tumour stroma or the tumour itself are termed as TILs [56]. In 2014, the International TILs Working Group (ITWG) suggested a standardised methodology for evaluating TILs with detailed information and instruction with step to step tutorial in breast cancer setting [57]. Later on, in 2017, other solid tumours were also included in the ITWG study framework [58] along with other studies confirmations or updates [59, 60]. Accordingly, TILs assessment is performed on haematoxylin and eosin slides by considering both the stromal and the intra-tumour cell compartments [61]. Stromal TILs (sTILs) refer to the area occupied by mononuclear inflammatory cells over the total stromal area, while intra-tumoural TILs (iTILs) are related to the tumour cell area [62]. sTILs and iTILs ought to be reported separately to avoid the effect of tumour cell density and growth pattern on the TIL count. Another reason for reporting individually is that in many tumours the density of TIL is different in both compartments [57]. After defining stromal and intra-tumoural areas with low magnification, the type of inflammatory infiltrates is supposed to be determined [61]. Based on the tumour type, either TILs subtypes or one of them needs to be evaluated. For example, in breast cancer, only sTILs provide valuable information [57]. Apart from TILs, other complementary biomarkers such as the CD4, CD8 and forkhead box P3 are of great relevance in the assessment of TILs function [63, 64].
The lymphocytic infiltration in primary cutaneous melanoma was originally noted by Clark et al in almost half a decade ago [65]. Later on, Day et al [65] provided data that highlighted the prognostic significance of infiltrated lymphocytes within tumours . The College of American Pathologist has divided TILs in melanoma into three groups, namely Brisk (i.e. diffuse permeation of the invasive tumour), non-Brisk (i.e. focally infiltrating lymphocytes) and not identified subsets [66]. A recent meta-analysis demonstrated non-brisk TILs as a favourable prognostic biomarker in melanoma [64].
In breast cancer, the presence of TILs has been thoroughly investigated, leading to interesting insights. Specifically, increased levels of TILs in TNBC have been associated with better OS and disease-free survival [67]. Another interesting study suggested that sTILs can identify a subset of stage I TNBC patients with exceptional prognosis without adjuvant chemotherapy [68]. Moreover, early-stage HER2POS breast cancer patients with the presence of TILs have been found to benefit when treated with trastuzumab and chemotherapy [69, 70]. However, according to De Angelis et al [71] HER2POS breast cancers with the presence of TILs above the threshold of 60%, established by the authors, were marginally associated with higher pathologic complete response rate when treated with lapatinib plus trastuzumab.
In GC, sTILs positivity has been associated with favourable prognosis [72, 73]. According to a systematic review and quantitative meta-analysis, including 43 studies, it has been suggested that high-density TILs also present a favourable prognosis in colorectal cancer [74]. In patients with high-grade serous carcinoma of the ovary, TILs levels may be associated with chemotherapeutic sensitivity [75]. Interestingly, TILs have also been reported as a predictive biomarker of response to anti-PD1 therapy in patients with metastatic NSCLC or metastatic melanoma [76]. However, in RCC, high TILs expression has been suggested to be correlated with poor prognosis [77]. All these studies make evident the extremely important role of TILs across different cancer types while they highlight the need for the discovery of essential information hidden behind TILs evaluation.
Finally, in malignant pleural mesotheliomas (MPMs), low CD4POS and high CD8POS sTILs are associated with poor patients’ survival [78]. In MPMs PD-L1 CPS > 1, stromal CD8HIGH seems to be a poor prognostic factor, while stromal CD4POS peritumoural TILs correlate with a worse prognosis [78]. In these tumours, a high CD4POS/CD8POS ratio in the immune microenvironment is an independent prognostic factor for survival. All these recent observations provide novel insights into the clinical scenario of immune-related biomarkers in MPM.
MMR deficiency and MSI
During the DNA recombination process, strands may detach and reanneal incorrectly, leading to mismatches [79]. However, during evolution, cells have developed strategies to identify and repair these errors. Within this DNA repair network, the mismatch repair (MMR) system is capable of solving insertion/deletion or base-base disparities on DNA [79, 80]. Six MMR proteins—mutL homologue 1 (MLH1), mutL homologue 3 (MLH3), mutS homologue 2 (MSH2), mutS homologue 3 (MSH3), mutS homologue 6 (MSH6) and postmeiotic segregation increased 2 (PMS2)—work coordinately within five complexes to repair mismatches [81]. Deficiency in the compartments of this system may result in modifications in repeated-sequence motifs, termed as microsatellites [79, 80].
Replication errors are more probable in microsatellites due to their repeated structure [82]. Hence, they are considered a potential biomarker for identifying MMR malfunction. The presence of multiple alterations in the length of microsatellites is defined as MSI [83]. MMR/MSI testing is utilised mainly to identify potential Lynch syndrome families. MLH1, MSH2, MSH6 and PMS2 proteins are assessed by IHC antibodies. This evaluation is preferred as one of the most cost-effective and available means of measurement [84]. MSI detection is generally performed through polymerase chain reaction (PCR) approaches by amplifying microsatellite markers with PCR-based methods and detecting MSI by measuring the length of the fragments [85]. Next-generation sequencing (NGS) with higher sensitivity is also being used to detect MSI in various malignancies [86]. In colorectal [87], ovarian [88], endometrial [89] and GC [90], MMR malfunction/MSI is reported as a prognostic biomarker. Contrary, it has been shown that in breast cancer, IHC and MSI testing are not interchangeable tests meaning that each type of cancer requires different and optimised management [8, 91].
The role of gene signature evaluation has become more blatant when FDA related novel immunotherapies to MMR and MSI status regardless of primary tumour site [92]. For the first time in 2017, the FDA approved the use of immunotherapy based on patients’ MMR/MSI status. Accordingly, MMR-deficient and MSI-high metastatic colorectal cancer with progression following treatment with fluoropyrimidine, oxaliplatin and irinotecan were permitted for anti-PD-1 treatment. This accelerated approval was related to nivolumab (OPDIVO, Bristol-Myers Squibb Company) [93]. Later on, in 2018, another accelerated approval was granted, adding ipilimumab (YERVOY, Bristol-Myers Squibb Company Inc.) as a combination therapy to nivolumab of those patients previously noted in 2017 [94] (Table 1).
Tumour mutational burden (TMB)
The concept of TMB refers to the number of somatic coding DNA mutations in the tumour exome [95]. TMB is noted as a beneficial biomarker in tumour immunotherapy [96]. Genetically unstable characteristics of cancer cells raise the possibility of somatic mutations resulting in neoantigens [97]. Diverse types of tumours display a different load of somatic mutations [97]. To date, melanoma and NSCLC show the highest frequencies of mutations [98]. As PD-L1 expression is reported to be highly heterogeneous, predicting the efficacy of immune checkpoint inhibitors (ICPis) in NSCLC is not yet feasible by this biomarker. Hence TMB has shown a new perspective in identifying the most fitting candidates for immunotherapy [99]. According to Hellmann et al [100], combination therapy of nivolumab and ipilimumab results in a greater PFS in high TMB cases. Remarkably, this study considered patients regardless of PD-L1 expression . Another study indicated a positive relation between atezolizumab efficacy and high level of TMB, resulting in improved ORR and duration of response in other tumours [101]. These findings suggested the importance of TMB assessment regardless of PD-L1 expression.
Generally, TMB is performed on the DNA extracted from tumour tissue, however, the analysis of circulating tumour DNA (ctDNA) is being investigated in the clinical practice, particularly in follow-up settings [102, 103]. The gold standard method for assessing TMB is whole-exome sequencing (WES) by using NGS technology [104]. This technology estimates the neoantigen load based on somatic nonsynonymous coding mutations [95]. WES highlights the presence of mutations in around 22,000 genes which makes it an expensive and time-consuming application to run [95, 97]. Targeted NGS panels are being used routinely in the clinic for oncogenic mutation detection [97]. A standardised guideline that clearly states methods and analytical validation are of importance as there are several platforms with similar targeted panels and technologies [105].
CGP assays
CGP is a targeted assay with great value in personalised cancer care transformation [106]. This assay identifies genomic alterations including mutations, copy number variants (amplification) and fusions (rearrangements), associated with targeted therapy opportunities in clinically relevant cancer genes [107]. TMB reports the number of mutations per megabase. However, there is no agreed threshold in existing assays with similar intended use [108]. Friends of Cancer Research and Quality Assurance Initiative Pathology joined to come up with harmonise and standardise TMB testing results [109]. FoundationOne® CDx is an approved CDx test by FDA [110]. This CDx identifies genetic alterations in 324 genes, MSI and TMB by extracting DNA from formalin-fixed paraffin-embedded tumour tissue specimens. The sequenced DNA is then evaluated for the presence or absence of mutations [108]. Another FDA-approved testing panel is IMPACT which utilises NGS to identify the presence of mutations in 468 unique genes, as well as other molecular changes [111]. This assay has more than 99% accuracy with the ability to detect mutations at a frequency of 2 to 5 percent [111]. Rizvi et al [112] showed that TMB quantified by targeted NGS closely correlates with TMB as quantified by WES. However, not all NGS panels may be well suited to estimate TMB.
Biomarkers and precision immunotherapy future prospectives (hope)
ICPis therapies have significantly improved precise treatment in several types of solid tumours [113]. Immunotherapy based on immune checkpoints is being widely expanded in clinical practice by gaining FDA approval in different antibody settings [114]. As listed in Table 1, PD-L1 was approved by the FDA as a biomarker in the line of predicting response to ICPis in several solid tumours [115]. FDA has also approved the application of other biomarkers such as MMR and MSI for colorectal cancer in both monotherapy and combination therapy [116]. Added to these, several other biomarkers and therapies are under the process of accelerated approval which is expected to add more value to ICPis therapy in the near future (Table 1).
Mechanisms associated with ICPIs resistance and predictive biomarkers for ICPis therapy are being actively studied [117]. Immunotherapy efficacy is strictly related to the tumour microenvironment (TME) [118]. Hence, studying components within TME is of interest in forthcoming studies. For instance, myeloid-derived suppressor cells (MDSCs), as a component of TME, are associated with ICPIs inhibition [119]. Reportedly, immunotherapy response can be improved by blocking MDSC activity [120]. Also, a correlation between MDSCs expression and poor OS and PFS is noted [121]. Another perspective issue focuses on stimulating T cell responses in which elevated co-stimulatory molecules result in favourable anti-tumour alterations [121]. For example, inducible T-cell co-stimulator, an indicator of T cell-mediated immune response, that enables early prediction of therapeutic response over multiple treatment regimens [122]. The combination of epigenetic modulator inhibitors with ICPis represents another promising approach in cancer management; as epigenetic alterations may downregulate tumour antigens by disturbing immune recognition [123]. Hong et al [124] used nivolumab in order to target epigenetic modulators which significantly increased apoptosis. The application of neoantigen vaccines as modulators of the immune microenvironment is another upcoming topic. Neoantigens resulted in mutations, may give rise to immune responses [125]. As a result, synthesised peptides may induce CD4POS and CD8POS T cell responses [126]. Reportedly, low mutation load and low T cell infiltrating TME are suitable candidates for vaccination [127]. Genetically engineered oncolytic viruses are also of interest. OVs destroy tumour cells by selectively replicating in these cells and inducing systematic anti-tumour immune responses [128]. Several clinical trials are under investigation in combining OV with cancer immunotherapies [129]. Last but not least, gut microbial alterations may lead to the additional possibility of cancer treatment. The gut microbiome is considered as a potential biomarker for ICPis response [121]. Modulation of the gut microbiome to enhance therapeutic response is being tested in multiple ongoing clinical studies [130]. Accordingly, antibiotic consumption before ICPIs had worse OS than unexposed patients [131].
Several studies suggest potential improvement of ICPis efficacy in combination with treatments such as chemotherapy, radiation and targeted therapy. These treatments can modulate the TME resulting in increased immunogenicity [132, 133]. Thus, upcoming findings in novel combinations of therapeutic agents may hopefully unravel the current gap of partial effectiveness of single-agent ICPis therapy [134]. Chemotherapy and radiotherapy are not only able to kill cancer cells directly but also present immunomodulatory properties [135]. Destruction of cancer cells with chemotherapy agents can be followed by the release of tumour-associated antigens that activate immune response as well as reduction of immunosuppressive cells such as MDSCs and Tregs [136, 137]. Radiation not only causes the release of tumour antigens but also improves antigen presentation and TIL infiltration stimulating an immune response [138]. Interestingly, studies have tested the efficacy of either chemotherapy plus ICPis or administration of ICPis after radiotherapy reporting encouraging results [139–141], while high-expectation clinical trials are ongoing (e.g. NCT04262687, NCT03453892). Targeted therapy presents similar immunomodulatory effects [132]. A phase 2 ongoing trial (NCT02954536) evaluated the safety profile and activity of pembrolizumab in combination with trastuzumab and chemotherapy in first-line HER2-positive metastatic gastric, oesophageal and gastroesophageal junction cancer. The response rate of 91% and median OS (27·3 months) were improved compared to the response rate (47%) and median OS (16 months) previously reported for chemotherapy plus trastuzumab. According to this trial, pembrolizumab can be safely combined with trastuzumab and chemotherapy and has promising activity in HER2-positive metastatic esophagogastric cancer [142]. Trastuzumab in combination with pembrolizumab may enhance HER2-specific T-cell responses and improve T cell and dendritic cell trafficking [142]. Other benefits of targeted therapy along with immunotherapy cross-talk could be seen in anti-PD-1 antibody treatment in combination with lenvatinib. This combinatory treatment mainly targets vascular endothelial growth factor and fibroblast growth factor receptors in patients with advanced endometrial cancers. In this study, lenvatinib reduced tumour-associated macrophages and increased the percentage of activated CD8POS T cells secreting interferon [143].
A promising application of ICPis can also be found in neoadjuvant therapy as recent publications note neoadjuvant immunotherapy may result in better clinical efficacy over an adjuvant application ICPis may also be used in the neoadjuvant setting since recent studies support that neoadjuvant immunotherapy can result in better clinical efficacy compared to the corresponding adjuvant therapy [144]. Added to all dated advancements, common means of time-consuming and painful tissue biopsies may be replaced by ctDNA in the peripheral blood [145, 146]. Most tumours are highly heterogeneous and may change during the progression of the disease. To define optimal therapeutic strategies, temporal sampling is mandatory. However, tissue biopsies are not always easy to perform since the tumour site may not be accessible and may not be representative of the whole tumour. Thus, the innovative approach of ‘liquid biopsy’ is gaining more and more attention. The fast turnover of tumour cells leads to a constant release in the peripheral blood of circulating tumour cells (CTCs) and cell-free ctDNA [147]. CTCs are believed to be passively spread from the primary and/or metastatic tumour sites into the bloodstream and may be responsible for the establishment of distant metastases. The liquid biopsy approach allows a repetitive and less invasive interrogation of tumours’ evolution, making sample collection much easier and efficient both for patients and clinicians [148]. All these improvements which are usually based on well-validated principles of certain biomarkers give hope for better results in precision immunotherapy.
Pitfalls in biomarker-based patients’ selection (reality)
ICPis have drastically transformed cancer treatment profiles by giving hope to physicians in cancer management [149]. However, a significant proportion of patients do not benefit from immunotherapy (with an ORR of only 20% to 23%) [150]. Biomarkers are therefore applied for the finest patient selection. Yet, assortment based on a single biomarker does not appear to be highly efficient [3]. Thus far, numerous gaps should be considered carefully to achieve optimal therapeutic benefit [151]. As stated by Pagni et al [4] ‘we do need biomarkers’ to target immune-related pathways in precise therapy. PD-L1 plays a great role as a biomarker [151]. Despite the availability and low cost of PD-L1 assessment by IHC, several technical issues are related to this method. Firstly, the IHC assessment of PD-L1 has limited accuracy due to tumour heterogeneity [151]. Moreover, several antibody clones produced by different companies are used in clinical trials; this variety of antibody clones is mystifying [153]. Added to this, different scoring methodologies—iTILs, sTILs, pTILs—which vary in different tumour types, potentially lead to confusion [154]. Besides, the PD-L1 assessment by itself does not grant to come up with an optimal therapeutic strategy [155].
Resistance to pharmacotherapy is a major issue that prevents a significant subset of patients from responding to PD-1/PD-L1 blockade. Thus, tumour immune microenvironment classification may lighten up the reasons behind [156]. When PD-L1 expression is accompanied by the presence of TILs, it characterises an adaptive resistance of tumours related to the PD-1 pathway (type-I). When both PD-L1 and TILs are not sufficient, termed as immunologically ignorant, ICs do not migrate toward cancer cells (type II). Positive PD-L1 and negative TILs lead to the induction of PD-L1 expression in tumour cells (type III). Contrary, low PD-L1 expression with optimal TILs is referred to as tolerance since the present TILs do not induce PD-L1 expression (type IV) [157]. Ultimately, the goal is to harmonise the patient’s TME with sufficient PD-L1 and TILs [158]. Added to these, not only ICPis response may remain temporarily, with the median duration of response of 1 to 2 years in NSCLC, but it can also result in resistance after the initial response [159]. The mechanisms behind therapeutic resistance are essential to address details of current misfunctions. Yet, introducing proper immunotherapeutic agents and related biomarkers to highlight malfunction is of necessity [160].
Several studies have reported TILs as a potential prognostic and predictive marker in various types of cancer [66]. Even though the TILs working group recommended standardised methodologies for the assessment of immuno-oncology biomarkers/TILs in different malignancies, the efficacy of this evaluation is suggested to be assessed by a large cohort of studies on all solid tumours [161]. MMR-wise, different methods of evaluation such as IHC, MSI and TMB are introduced to evaluate MMR status, hence a single method of assessment could provide more uniform and reliable results [81]. Several institutions perform TMB measurements mostly based on targeted NGS [97]. Despite WES is the gold standard method, usually, it is time-consuming and not affordable to run routinely [104]. Moreover, dedicated platforms are not available in all pathology laboratories [162]. As an alternative, panel-based NGS assays are of use to measure TMB. However, TMB levels are variable among each tumour type and cut-off values need to be established to reliably assess this emerging biomarker. [163]. Regarding adverse events, likewise other medications, ICPis administration brings along unwanted effects [164]. Auto-immune reactions are among the most common side effects and they can be presented as simple skin rashes but also as severe neurologic, hematologic, cardiac and respiratory implications [165]. These can be initiated by nonspecific activations of the immune system through different mechanisms. It is of note that about 2% of irAEs lead to treatment-related deaths, varying by ICPis [33]. Above all, further irAE may have not been documented yet as ICPis have only recently been introduced in therapeutic schemes. Consequently, a more detailed investigation is needed to fully approve ICPis safety profile [149].
The excessive cost of immunotherapy can be considered another important limiting factor [162]. Despite great importance, the economical aspect of this therapy has not been shielded to date [166]. ICPis therapies ought to be bearable so that not only patients can benefit from the latest therapies but also scientists could implement expanded databases for additional validations of their investigations.
Conclusion
Cancer is a complicated malignancy that involves several mechanisms and immune-related pathways. Therefore, a combination of innovative therapeutic strategies that rely on precise biomarkers has to be developed to profoundly address this issue [167]. Precision immunotherapy has already started to light up a new era in cancer management. It is fair to conclude that several struggles are yet to be addressed in patients’ selection for immunotherapy. We highlight the importance of implementing tumour-specific tests and precise guidelines in routine clinical practice for optimal therapeutic outcomes.
List of abbreviations
PD-L1, Programmed death-ligand 1; TILs, Tumour-infiltrating lymphocytes; MSI, Microsatellite instability; MMR, Mismatch repair; TMB, Tumour mutational burden; CGP, Comprehensive genomic profiling; MHC, Major histocompatibility complex; CTLA4, Cytotoxic T-lymphocyte antigen 4; PD-1, Checkpoint axis programmed cell death protein 1; NSCLC, Non-small cell lung cancer; RCC, Renal cell carcinoma; FDA, Food and Drugs Administration; irAEs, Immune-related adverse events; ICPis, Immune checkpoint inhibitors; IHC, Immunohistochemistry; TPS, Tumour proportion score; CPS, Combined positive score; TNBC, Triple-negative breast cancers; ICs, Immune cells; HNSCC, Head and neck squamous cell carcinoma; OS, Overall survival; ORR, Objective response rate; ITWG, International TILs Working Group; sTILs, Stromal TILs; iTILs, intra-tumoural TILs; GC, Gastric cancer; MLH1, mutL homologue 1; MLH3, mutL homologue 3; MSH2, mutS homologue 2; MSH3, mutS homologue 3; MSH6, mutS homologue 6; PMS2, postmeiotic segregation increased 2; NGS, Next-generation sequencing; ctDNA, circulating tumour DNA; WES, Whole exome sequencing; CDx, companion diagnostic; TME, Tumour microenvironment; MDSCs, Myeloid-derived suppressor cells; PFS, Progression-free survival; CTCs, Circulating tumour cells
Conflicts of interest
Nicola Fusco has received honoraria for consulting/advisory role from Merck Sharp & Dohme (MSD), Boehringer Ingelheim and Novartis. These companies had no role in the design of the study, in the collection, analyses or interpretation of data, in the writing of the manuscript and/or in the decision to publish the results. All the other authors declare no conflicts of interest.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Napolitano M, Schipilliti FM, Trudu L, et al. Immunotherapy in head and neck cancer: The great challenge of patient selection. Crit Rev Oncol Hematol. 2019;144:102829. doi: 10.1016/j.critrevonc.2019.102829. [DOI] [PubMed] [Google Scholar]
- 2.Reisenbichler ES, Han G, Bellizzi A, et al. Prospective multi-institutional evaluation of pathologist assessment of PD-L1 assays for patient selection in triple negative breast cancer. Mod Pathol. 2020;33(9):1746–1752. doi: 10.1038/s41379-020-0544-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iivanainen S, Koivunen JP. Possibilities of improving the clinical value of immune checkpoint inhibitor therapies in cancer care by optimizing patient selection. Int J Mol Sci. 2020;21(2) doi: 10.3390/ijms21020556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pagni F, Guerini-Rocco E, Schultheis AM, et al. Targeting immune-related biological processes in solid tumors: we do need biomarkers. Int J Mol Sci. 2019;20(21) doi: 10.3390/ijms20215452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of Immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2018;36(17):1714–1768. doi: 10.1200/JCO.2017.77.6385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi J, Lee SY. Clinical characteristics and treatment of immune-related adverse events of immune checkpoint inhibitors. Immune Netw. 2020;20(1):e9. doi: 10.4110/in.2020.20.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gambardella V, Tarazona N, Cejalvo JM, et al. Personalized medicine: recent progress in cancer therapy. Cancers (Basel) 2020;12(4) doi: 10.3390/cancers12041009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venetis K, Sajjadi E, Haricharan S, et al. Mismatch repair testing in breast cancer: the path to tumor-specific immuno-oncology biomarkers. Transl Cancer Res. 2020;9(7) doi: 10.21037/tcr-20-1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Signorelli D, Giannatempo P, Grazia G, et al. Patients selection for immunotherapy in solid tumors: overcome the naïve vision of a single biomarker. Biomed Res Int. 2019;2019 doi: 10.1155/2019/9056417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samstein RM, Lee CH, Shoushtari AN, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet. 2019;51(2):202–206. doi: 10.1038/s41588-018-0312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salmaninejad A, Valilou SF, Shabgah AG, et al. PD-1/PD-L1 pathway: basic biology and role in cancer immunotherapy. J Cell Physiol. 2019;234(10):16824–16837. doi: 10.1002/jcp.28358. [DOI] [PubMed] [Google Scholar]
- 12.Lopez G, Noale M, Corti C, et al. PTEN expression as a complementary biomarker for mismatch repair testing in breast cancer. Int J Mol Sci. 2020;21(4) doi: 10.3390/ijms21041461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fusco N, Sajjadi E, Venetis K, et al. PTEN alterations and their role in cancer management: are we making headway on precision medicine? Genes. 2020;11(7):719. doi: 10.3390/genes11070719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costa C, Wang Y, Ly A, et al. PTEN loss mediates clinical cross-resistance to CDK4/6 and PI3Kα inhibitors in breast cancer. Cancer Discov. 2020;10(1):72–85. doi: 10.1158/2159-8290.CD-18-0830. [DOI] [PubMed] [Google Scholar]
- 15.Razavi P, Dickler MN, Shah PD, et al. Alterations in PTEN and ESR1 promote clinical resistance to alpelisib plus aromatase inhibitors. Nat Cancer. 2020;1(4):382–393. doi: 10.1038/s43018-020-0047-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vidotto T, Melo CM, Castelli E, et al. Emerging role of PTEN loss in evasion of the immune response to tumours. Br J Cancer. 2020;122(12):1732–1743. doi: 10.1038/s41416-020-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malone ER, Oliva M, Sabatini PJB, et al. Molecular profiling for precision cancer therapies. Genome Med. 2020;12(1):8. doi: 10.1186/s13073-019-0703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee EY, Kulkarni RP. Circulating biomarkers predictive of tumor response to cancer immunotherapy. Expert Rev Mol Diagn. 2019;19(10):895–904. doi: 10.1080/14737159.2019.1659728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Labani-Motlagh A, Ashja-Mahdavi M, Loskog A. The tumor microenvironment: a milieu hindering and obstructing antitumor immune responses. Front Immunol. 2020;11:940. doi: 10.3389/fimmu.2020.00940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gil Del Alcazar CR, Alečković M, Polyak K. Immune escape during breast tumor progression. Cancer Immunol Res. 2020;8(4):422–427. doi: 10.1158/2326-6066.CIR-19-0786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He Q, Jiang X, Zhou X, et al. Targeting cancers through TCR-peptide/MHC interactions. J Hematol Oncol. 2019;12(1):139. doi: 10.1186/s13045-019-0812-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Coillie S, Wiernicki B, Xu J. Molecular and cellular functions of CTLA-4. Adv Exp Med Biol. 2020;1248:7–32. doi: 10.1007/978-981-15-3266-5_2. [DOI] [PubMed] [Google Scholar]
- 23.Hosseini A, Gharibi T, Marofi F, et al. CTLA-4: From mechanism to autoimmune therapy. Int Immunopharmacol. 2020;80:106221. doi: 10.1016/j.intimp.2020.106221. [DOI] [PubMed] [Google Scholar]
- 24.Han Y, Liu D, Li L. PD-1/PD-L1 pathway: current researches in cancer. Am J Cancer Res. 2020;10(3):727–742. [PMC free article] [PubMed] [Google Scholar]
- 25.He X, Xu C. Immune checkpoint signaling and cancer immunotherapy. Cell Res. 2020;30(8):660–669. doi: 10.1038/s41422-020-0343-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang JY, Yan YY, Li JJ, et al. PD-1/PD-L1 based combinational cancer therapy: icing on the cake. Front Pharmacol. 2020;11:722. doi: 10.3389/fphar.2020.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weiss SA, Wolchok JD, Sznol M. Immunotherapy of melanoma: facts and hopes. Clin Cancer Res. 2019;25(17):5191–5201. doi: 10.1158/1078-0432.CCR-18-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang Y, Chen M, Nie H, et al. PD-1 and PD-L1 in cancer immunotherapy: clinical implications and future considerations. Hum Vaccin Immunother. 2019;15(5):1111–1122. doi: 10.1080/21645515.2019.1571892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Das S, Johnson DB. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J Immunother Cancer. 2019;7(1):306. doi: 10.1186/s40425-019-0805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palmieri DJ, Carlino MS. Immune checkpoint inhibitor toxicity. Curr Oncol Rep. 2018;20(9):72. doi: 10.1007/s11912-018-0718-6. [DOI] [PubMed] [Google Scholar]
- 31.Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med. 2018;378(2):158–168. doi: 10.1056/NEJMra1703481. [DOI] [PubMed] [Google Scholar]
- 32.O’Kane GM, Labbé C, Doherty MK, et al. Monitoring and management of immune‐related adverse events associated with programmed cell death protein‐1 axis inhibitors in lung cancer. Oncologist. 2017;22(1):70–80. doi: 10.1634/theoncologist.2016-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5(1):95. doi: 10.1186/s40425-017-0300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doroshow DB, Sanmamed MF, Hastings K, et al. Immunotherapy in non-small cell lung cancer: facts and hopes. Clin Cancer Res. 2019;25(15):4592–4602. doi: 10.1158/1078-0432.CCR-18-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peters S, Kerr KM, Stahel R. PD-1 blockade in advanced NSCLC: A focus on pembrolizumab. Cancer Treat Rev. 2018;62:39–49. doi: 10.1016/j.ctrv.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Davis AA, Patel VG. The role of PD-L1 expression as a predictive biomarker: an analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors. J Immunother Cancer. 2019;7(1):278. doi: 10.1186/s40425-019-0768-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooks T, Theodorou SD, Paparouna E, et al. Immunohisto(cyto)chemistry: an old time classic tool driving modern oncological therapies. Histol Histopathol. 2019;34(4):335–352. doi: 10.14670/HH-18-069. [DOI] [PubMed] [Google Scholar]
- 38.Burtness B, Harrington KJ, Greil R, et al. KEYNOTE-048: Phase III study of first-line pembrolizumab (P) for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC) Ann Oncol. 2018;29 doi: 10.1093/annonc/mdy424.045. [DOI] [Google Scholar]
- 39.Atezolizumab Combo Approved for PD-L1-positive TNBC Cancer Discov. 9. United States: ©. Philadelphia: American Association for Cancer Research; 2019. p Of2. [DOI] [PubMed] [Google Scholar]
- 40.Vigliar E, Malapelle U, Bono F, et al. The reproducibility of the immunohistochemical PD-L1 testing in non-small-cell lung cancer: a multicentric italian experience. Biomed Res Int. 2019;2019:6832909. doi: 10.1155/2019/6832909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Udall M, Rizzo M, Kenny J, et al. PD-L1 diagnostic tests: a systematic literature review of scoring algorithms and test-validation metrics. Diagn Pathol. 2018;13(1):12. doi: 10.1186/s13000-018-0689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mok TSK, Wu YL, Kudaba I, et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393(10183):1819–1830. doi: 10.1016/S0140-6736(18)32409-7. [DOI] [PubMed] [Google Scholar]
- 43.Cohen EEW, Bell RB, Bifulco CB, et al. The Society for Immunotherapy of Cancer consensus statement on immunotherapy for the treatment of squamous cell carcinoma of the head and neck (HNSCC) J Immunother Cancer. 2019;7 doi: 10.1186/s40425-019-0662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mehra R, Seiwert TY, Gupta S, et al. Efficacy and safety of pembrolizumab in recurrent/metastatic head and neck squamous cell carcinoma: pooled analyses after long-term follow-up in KEYNOTE-012. Br J Cancer. 2018;119(2):153–159. doi: 10.1038/s41416-018-0131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferris RL, Licitra L, Fayette J, et al. Nivolumab in patients with recurrent or metastatic squamous cell carcinoma of the head and neck: efficacy and safety in CheckMate 141 by prior cetuximab use. Clin Cancer Res. 2019;25(17):5221–5230. doi: 10.1158/1078-0432.CCR-18-3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kulangara K, Hanks DA, Waldroup S, et al. Development of the combined positive score (CPS) for the evaluation of PD-L1 in solid tumors with the immunohistochemistry assay PD-L1 IHC 22C3 pharmDx. J Clin Oncol. 2017;35(15_suppl):e14589. doi: 10.1200/JCO.2017.35.15_suppl.e14589. [DOI] [Google Scholar]
- 47.Kythreotou A, Siddique A, Mauri FA, et al. PD-L1. J Clin Pathol. 2018;71(3):189–194. doi: 10.1136/jclinpath-2017-204853. [DOI] [PubMed] [Google Scholar]
- 48.Fuchs CS, Doi T, Jang RW, et al. Safety and efficacy of pembrolizumab monotherapy in patients with previously treated advanced gastric and gastroesophageal junction cancer: phase 2 clinical KEYNOTE-059 trial. JAMA Oncol. 2018;4(5):e180013. doi: 10.1001/jamaoncol.2018.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roviello G, Corona SP, Nesi G, et al. Results from a meta-analysis of immune checkpoint inhibitors in first-line renal cancer patients: does PD-L1 matter? Ther Adv Med Oncol. 2019;11:1758835919861905. doi: 10.1177/1758835919861905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu X, Gu Z, Chen Y, et al. Application of PD-1 blockade in cancer immunotherapy. Comput Struct Biotechnol J. 2019;17:661–674. doi: 10.1016/j.csbj.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tomioka N, Azuma M, Ikarashi M, et al. The therapeutic candidate for immune checkpoint inhibitors elucidated by the status of tumor-infiltrating lymphocytes (TILs) and programmed death ligand 1 (PD-L1) expression in triple negative breast cancer (TNBC) Breast Cancer. 2018;25(1):34–42. doi: 10.1007/s12282-017-0781-0. [DOI] [PubMed] [Google Scholar]
- 52.Planes-Laine G, Rochigneux P, Bertucci F, et al. PD-1/PD-L1 targeting in breast cancer: the first clinical evidences are emerging—a literature review. Cancers (Basel) 2019;11 doi: 10.3390/cancers11071033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simon SCS, Utikal J, Umansky V. Opposing roles of eosinophils in cancer. Cancer Immunol Immunother. 2019;68(5):823–833. doi: 10.1007/s00262-018-2255-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol. 2019;106(2):309–322. doi: 10.1002/JLB.4RI0818-311R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Giese MA, Hind LE, Huttenlocher A. Neutrophil plasticity in the tumor microenvironment. Blood. 2019;133(20):2159–2167. doi: 10.1182/blood-2018-11-844548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roncati L, Gasparri P, Gallo G, et al. Appendix tumor microenvironment. Adv Exp Med Biol. 2020;1226:87–95. doi: 10.1007/978-3-030-36214-0_7. [DOI] [PubMed] [Google Scholar]
- 57.Hendry S, Salgado R, Gevaert T, et al. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immunooncology biomarkers working group: part 1: assessing the host immune response, tils in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv Anat Pathol. 2017;24(5):235–251. doi: 10.1097/PAP.0000000000000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hendry S, Salgado R, Gevaert T, et al. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immuno-oncology biomarkers working group: part 2: TILs in melanoma, gastrointestinal tract carcinomas, non-small cell lung carcinoma and mesothelioma, endometrial and ovarian carcinomas, squamous cell carcinoma of the head and neck, genitourinary carcinomas, and primary brain tumors. Adv Anat Pathol. 2017;24(6):311–335. doi: 10.1097/PAP.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kojima YA, Wang X, Sun H, et al. Reproducible evaluation of tumor-infiltrating lymphocytes (TILs) using the recommendations of International TILs Working Group 2014. Ann Diagn Pathol. 2018;35:77–79. doi: 10.1016/j.anndiagpath.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 60.Dieci MV, Radosevic-Robin N, Fineberg S, et al. Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: a report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin Cancer Biol. 2018;52(Pt 2):16–25. doi: 10.1016/j.semcancer.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 61.Iseki Y, Shibutani M, Maeda K, et al. A new method for evaluating tumor-infiltrating lymphocytes (TILs) in colorectal cancer using hematoxylin and eosin (H-E)-stained tumor sections. PLoS One. 2018;13(4):e0192744. doi: 10.1371/journal.pone.0192744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu J, Xu Y, Yu M, et al. Increased stromal infiltrating lymphocytes are associated with circulating tumor cells and metastatic relapse in breast cancer patients after neoadjuvant chemotherapy. Cancer Manag Res. 2019;11:10791–1800. doi: 10.2147/CMAR.S220327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Orhan A, Vogelsang RP, Andersen MB, et al. The prognostic value of tumour-infiltrating lymphocytes in pancreatic cancer: a systematic review and meta-analysis. Eur J Cancer. 2020;132:71–84. doi: 10.1016/j.ejca.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 64.Fu Q, Chen N, Ge C, et al. Prognostic value of tumor-infiltrating lymphocytes in melanoma: a systematic review and meta-analysis. Oncoimmunology. 2019;8(7):1593806. doi: 10.1080/2162402X.2019.1593806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Antohe M, Nedelcu RI, Nichita L, et al. Tumor infiltrating lymphocytes: the regulator of melanoma evolution. Oncol Lett. 2019;17(5):4155–4161. doi: 10.3892/ol.2019.9940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Badalamenti G, Fanale D, Incorvaia L, et al. Role of tumor-infiltrating lymphocytes in patients with solid tumors: can a drop dig a stone? Cell Immunol. 2019;343:103753. doi: 10.1016/j.cellimm.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 67.Gao G, Wang Z, Qu X, et al. Prognostic value of tumor-infiltrating lymphocytes in patients with triple-negative breast cancer: a systematic review and meta-analysis. BMC Cancer. 2020;20(1):179. doi: 10.1186/s12885-020-6668-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Park JH, Jonas SF, Bataillon G, et al. Prognostic value of tumor-infiltrating lymphocytes in patients with early-stage triple-negative breast cancers (TNBC) who did not receive adjuvant chemotherapy. Ann Oncol. 2019;30(12):1941–1949. doi: 10.1093/annonc/mdz395. [DOI] [PubMed] [Google Scholar]
- 69.Dieci MV, Conte P, Bisagni G, et al. Association of tumor-infiltrating lymphocytes with distant disease-free survival in the ShortHER randomized adjuvant trial for patients with early HER2+ breast cancer. Ann Oncol. 2019;30(3):418–423. doi: 10.1093/annonc/mdz007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ignatiadis M, Van den Eynden G, Roberto S, et al. Tumor-infiltrating lymphocytes in patients receiving trastuzumab/pertuzumab-based chemotherapy: a TRYPHAENA substudy. J Natl Cancer Inst. 2019;111(1):69–77. doi: 10.1093/jnci/djy076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.De Angelis C, Nagi C, Hoyt CC, et al. Evaluation of the predictive role of tumor immune infiltrate in patients with HER2-positive breast cancer treated with neoadjuvant anti-HER2 therapy without chemotherapy. Clin Cancer Res. 2020;26(3):738–745. doi: 10.1158/1078-0432.CCR-19-1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liu JY, Yang GF, Chen FF, et al. Evaluating the prognostic significance of tumor-infiltrating lymphocytes in solid tumor: practice of a standardized method from the International Immuno-Oncology Biomarkers Working Group. Cancer Manag Res. 2019;11:6815–6827. doi: 10.2147/CMAR.S201538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zheng X, Song X, Shao Y, et al. Prognostic role of tumor-infiltrating lymphocytes in gastric cancer: a meta-analysis. Oncotarget. 2017;8(34):57386–57398. doi: 10.18632/oncotarget.18065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Idos GE, Kwok J, Bonthala N, et al. The prognostic implications of tumor infiltrating lymphocytes in colorectal cancer: a systematic review and meta-analysis. Sci Rep. 2020;10(1):3360. doi: 10.1038/s41598-020-60255-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Choi KU, Kim A, Kim JY, et al. Differences in immune-related gene expressions and tumor-infiltrating lymphocytes according to chemotherapeutic response in ovarian high-grade serous carcinoma. J Ovarian Res. 2020;13(1):65. doi: 10.1186/s13048-020-00667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uryvaev A, Passhak M, Hershkovits D, et al. The role of tumor-infiltrating lymphocytes (TILs) as a predictive biomarker of response to anti-PD1 therapy in patients with metastatic non-small cell lung cancer or metastatic melanoma. Med Oncol. 2018;35(3):25. doi: 10.1007/s12032-018-1080-0. [DOI] [PubMed] [Google Scholar]
- 77.Kawashima A, Kanazawa T, Kidani Y, et al. Tumour grade significantly correlates with total dysfunction of tumour tissue-infiltrating lymphocytes in renal cell carcinoma. Sci Rep. 2020;10(1):6220. doi: 10.1038/s41598-020-63060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fusco N, Vaira V, Righi I, et al. Characterization of the immune microenvironment in malignant pleural mesothelioma reveals prognostic subgroups of patients. Lung Cancer. 2020;150:53–61. doi: 10.1016/j.lungcan.2020.09.026. [DOI] [PubMed] [Google Scholar]
- 79.Motegi A, Masutani M, Yoshioka KI, et al. Aberrations in DNA repair pathways in cancer and therapeutic significances. Semin Cancer Biol. 2019;58:29–46. doi: 10.1016/j.semcancer.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 80.Trenner A, Sartori AA. Harnessing DNA double-strand break repair for cancer treatment. Front Oncol. 2019;9:1388. doi: 10.3389/fonc.2019.01388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Corti C, Sajjadi E, Fusco N. Determination of mismatch repair status in human cancer and its clinical significance: does one size fit all? Adv Anat Pathol. 2019;26(4):270–279. doi: 10.1097/PAP.0000000000000234. [DOI] [PubMed] [Google Scholar]
- 82.Yamamoto H, Imai K. An updated review of microsatellite instability in the era of next-generation sequencing and precision medicine. Semin Oncol. 2019;46(3):261–270. doi: 10.1053/j.seminoncol.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 83.Viale G, Trapani D, Curigliano G. Mismatch repair deficiency as a predictive biomarker for immunotherapy efficacy. Biomed Res Int. 2017;2017 doi: 10.1155/2017/4719194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yurgelun MB, Hampel H. Recent advances in lynch syndrome: diagnosis, treatment, and cancer prevention. Am Soc Clin Oncol Educ Book. 2018;38:101–109. doi: 10.1200/EDBK_208341. [DOI] [PubMed] [Google Scholar]
- 85.Baudrin LG, Deleuze JF, How-Kit A. Molecular and computational methods for the detection of microsatellite instability in cance. Front Oncol. 2018;8:621. doi: 10.3389/fonc.2018.00621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kok M, Chalabi M, Haanen J. How I treat MSI cancers with advanced disease. ESMO Open. 2019;4(Suppl 2):e000511. doi: 10.1136/esmoopen-2019-000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gong Q, Zhang HH, Sun SB, et al. Mismatch repair-deficient status associates with favorable prognosis of Eastern Chinese population with sporadic colorectal cancer. Oncol Lett. 2018;15(5):7007–7013. doi: 10.3892/ol.2018.8192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhao C, Li S, Zhao M, et al. Prognostic values of DNA mismatch repair genes in ovarian cancer patients treated with platinum-based chemotherapy. Arch Gynecol Obstet. 2018;297(1):153–159. doi: 10.1007/s00404-017-4563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tangjitgamol S, Kittisiam T, Tanvanich S. Prevalence and prognostic role of mismatch repair gene defect in endometrial cancer patients. Tumour Biol. 2017;39(9):1010428317725834. doi: 10.1177/1010428317725834. [DOI] [PubMed] [Google Scholar]
- 90.Wang L, Zhang Q, Ni S, et al. Programmed death-ligand 1 expression in gastric cancer: correlation with mismatch repair deficiency and HER2-negative status. Cancer Med. 2018;7(6):2612–2620. doi: 10.1002/cam4.1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fusco N, Lopez G, Corti C, et al. Mismatch Repair protein loss as a prognostic and predictive biomarker in breast cancers regardless of microsatellite instability. JNCI Cancer Spectr. 2018;2(4):pky056. doi: 10.1093/jncics/pky056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhang L, Peng Y, Peng G. Mismatch repair-based stratification for immune checkpoint blockade therapy. Am J Cancer Res. 2018;8(10):1977–1988. [PMC free article] [PubMed] [Google Scholar]
- 93.Ganesh K, Stadler ZK, Cercek A, et al. Immunotherapy in colorectal cancer: rationale, challenges and potential. Nat Rev Gastroenterol Hepatol. 2019;16(6):361–375. doi: 10.1038/s41575-019-0126-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lichtenstern CR, Ngu RK, Shalapour S, et al. Immunotherapy, inflammation and colorectal cancer. Cells. 2020;9(3) doi: 10.3390/cells9030618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fancello L, Gandini S, Pelicci PG, et al. Tumor mutational burden quantification from targeted gene panels: major advancements and challenges. J Immunother Cancer. 2019;7(1):183. doi: 10.1186/s40425-019-0647-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Nagahashi M, Shimada Y, Ichikawa H, et al. Next generation sequencing-based gene panel tests for the management of solid tumors. Cancer Sci. 2019;110(1):6–15. doi: 10.1111/cas.13837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chan TA, Yarchoan M, Jaffee E, et al. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol. 2019;30(1):44–56. doi: 10.1093/annonc/mdy495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stenzinger A, Allen JD, Maas J, et al. Tumor mutational burden standardization initiatives: Recommendations for consistent tumor mutational burden assessment in clinical samples to guide immunotherapy treatment decisions. Genes Chromosomes Cancer. 2019;58(8):578–588. doi: 10.1002/gcc.22733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Greillier L, Tomasini P, Barlesi F. The clinical utility of tumor mutational burden in non-small cell lung cancer. Transl Lung Cancer Res. 2018;7(6):639–646. doi: 10.21037/tlcr.2018.10.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378(22):2093–2104. doi: 10.1056/NEJMoa1801946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Legrand F, Gandara DR, Mariathasan S, et al. Association of high tissue TMB and atezolizumab efficacy across multiple tumor types. J Clin Oncol. 2018;36:12000. doi: 10.1200/JCO.2018.36.15_suppl.12000. [DOI] [Google Scholar]
- 102.Hofman P. Liquid biopsy and therapeutic targets: present and future issues in thoracic oncology. Cancers (Basel) 2017;9(11) doi: 10.3390/cancers9110154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fumagalli C, Bianchi F, Raviele PR, et al. Circulating and tissue biomarkers in early-stage non-small cell lung cancer. Ecancermedicalscience. 2017;11:717. doi: 10.3332/ecancer.2017.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bartha Á, Győrffy B. Comprehensive outline of whole exome sequencing data analysis tools available in clinical oncology. Cancers (Basel) 2019;11(11) doi: 10.3390/cancers11111725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Truesdell J, Miller VA, Fabrizio D. Approach to evaluating tumor mutational burden in routine clinical practice. Transl Lung Cancer Res. 2018;7(6):678–681. doi: 10.21037/tlcr.2018.10.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Signorovitch J, Zhou Z, Ryan J, et al. Budget impact analysis of comprehensive genomic profiling in patients with advanced non-small cell lung cancer. J Med Econ. 2019;22(2):140–150. doi: 10.1080/13696998.2018.1549056. [DOI] [PubMed] [Google Scholar]
- 107.Nesline MK, DePietro P, Dy GK, et al. Oncologist uptake of comprehensive genomic profile guided targeted therapy. Oncotarget. 2019;10(45):4616–4629. doi: 10.18632/oncotarget.27047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Büttner R, Longshore JW, López-Ríos F, et al. Implementing TMB measurement in clinical practice: considerations on assay requirements. ESMO Open. 2019;4(1):e000442. doi: 10.1136/esmoopen-2018-000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stenzinger A, Endris V, Budczies J, et al. Harmonization and standardization of panel-based tumor mutational burden measurement: real-world results and recommendations of the quality in pathology study. J Thorac Oncol. 15(7):1177–1189. doi: 10.1016/j.jtho.2020.01.023. [DOI] [PubMed] [Google Scholar]
- 110.Wu HX, Wang ZX, Zhao Q, et al. Designing gene panels for tumor mutational burden estimation: the need to shift from ‘correlation’ to ‘accuracy’. J Immunother Cancer. 2019;7(1):206. doi: 10.1186/s40425-019-0681-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.@US_FDA. FDA Unveils a Streamlined Path for the Authorization of Tumor Profiling Tests Alongside Its Latest Product Action. Maryland: FDA; 2017. [Google Scholar]
- 112.Rizvi H, Sanchez-Vega F, La K, et al. Molecular determinants of response to anti–programmed cell death (PD)-1 and anti–programmed death-ligand 1 (PD-L1) blockade in patients with non–small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol. 2018;36:633–641. doi: 10.1200/JCO.2017.75.3384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Havel JJ, Chowell D, Chan TA. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat Rev Cancer. 2019;19(3):133–150. doi: 10.1038/s41568-019-0116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Vaddepally RK, Kharel P, Pandey R, et al. Review of indications of fda-approved immune checkpoint inhibitors per NCCN guidelines with the level of evidence. Cancers (Basel) 2020;12(3) doi: 10.3390/cancers12030738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Christofi T, Baritaki S, Falzone L, et al. Current perspectives in cancer immunotherapy. Cancers (Basel) 2019;11(10) doi: 10.3390/cancers11101472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rawla P, Barsouk A, Hadjinicolaou AV. Immunotherapies and targeted therapies in the treatment of metastatic colorectal cancer. Med Sci (Basel) 2019;7(8) doi: 10.3390/medsci7080083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Seto T, Sam D, Pan M. Mechanisms of primary and secondary resistance to immune checkpoint inhibitors in cancer. Med Sci (Basel) 2019;7(2) doi: 10.3390/medsci7020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Alissafi T, Hatzioannou A, Legaki AI, et al. Balancing cancer immunotherapy and immune-related adverse events: The emerging role of regulatory T cells. J Autoimmun. 2019;104:102310. doi: 10.1016/j.jaut.2019.102310. [DOI] [PubMed] [Google Scholar]
- 119.Osipov A, Saung MT, Zheng L, et al. Small molecule immunomodulation: the tumor microenvironment and overcoming immune escape. J Immunother Cancer. 2019;7(1):224. doi: 10.1186/s40425-019-0667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Park SM, Youn JI. Role of myeloid-derived suppressor cells in immune checkpoint inhibitor therapy in cancer. Arch Pharm Res. 2019;42(7):560–566. doi: 10.1007/s12272-019-01165-6. [DOI] [PubMed] [Google Scholar]
- 121.Murciano-Goroff YR, Warner AB, Wolchok JD. The future of cancer immunotherapy: microenvironment-targeting combinations. Cell Res. 2020;30(6):507–519. doi: 10.1038/s41422-020-0337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Xiao Z, Mayer AT, Nobashi TW, et al. ICOS is an indicator of T-cell-mediated response to cancer immunotherapy. Cancer Res. 2020;80(14):3023–3032. doi: 10.1158/0008-5472.CAN-19-3265. [DOI] [PubMed] [Google Scholar]
- 123.Olino K, Park T, Ahuja N. Exposing Hidden Targets: Combining epigenetic and immunotherapy to overcome cancer resistance. Semin Cancer Biol. 2020;65:114–122. doi: 10.1016/j.semcancer.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 124.Hong YK, Li Y, Pandit H, Li S, Pulliam Z, Zheng Q, et al. Epigenetic modulation enhances immunotherapy for hepatocellular carcinoma. Cell Immunol. 2019;336:66–74. doi: 10.1016/j.cellimm.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 125.Keenan TE, Burke KP, Van Allen EM. Genomic correlates of response to immune checkpoint blockade. Nat Med. 2019;25(3):389–402. doi: 10.1038/s41591-019-0382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen X, Yang J, Wang L, et al. Personalized neoantigen vaccination with synthetic long peptides: recent advances and future perspectives. Theranostics. 2020;10(13):6011–6023. doi: 10.7150/thno.38742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Keskin DB, Anandappa AJ, Sun J, et al. Neoantigen vaccine generates intratumoral T cell responses in phase Ib glioblastoma trial. Nature. 2019;565(7738):234–239. doi: 10.1038/s41586-018-0792-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gujar S, Bell J, Diallo JS. SnapShot: cancer immunotherapy with oncolytic viruses. Cell. 2019;176(5):1240–1240.e1. doi: 10.1016/j.cell.2019.01.051. [DOI] [PubMed] [Google Scholar]
- 129.Shi T, Song X, Wang Y, et al. Combining oncolytic viruses with cancer immunotherapy: establishing a new generation of cancer treatment. Front Immunol. 2020;11:683. doi: 10.3389/fimmu.2020.00683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Warner AB, McQuade JL. Modifiable host factors in melanoma: emerging evidence for obesity, diet, exercise, and the microbiome. Curr Oncol Rep. 2019;21(8):72. doi: 10.1007/s11912-019-0814-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mohiuddin JJ, Chu B, Facciabene A, et al. Association of antibiotic exposure with survival and toxicity in patients with melanoma receiving immunotherapy. J Natl Cancer Inst. 2020. [DOI] [PMC free article] [PubMed]
- 132.Murciano-Goroff YR, Warner AB, Wolchok JD. The future of cancer immunotherapy: microenvironment-targeting combinations. Cell Res. 2020;30(6):507–519. doi: 10.1038/s41422-020-0337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Serrano-Del Valle A, Naval J, Anel A, et al. Novel forms of immunomodulation for cancer therapy. Trends Cancer. 2020;6(6):518–532. doi: 10.1016/j.trecan.2020.02.015. [DOI] [PubMed] [Google Scholar]
- 134.Doroshow DB, Herbst RS. Treatment of advanced non-small cell lung cancer in 2018. JAMA Oncol. 2018;4(4):569–570. doi: 10.1001/jamaoncol.2017.5190. [DOI] [PubMed] [Google Scholar]
- 135.Hennequin C, Guillerm S, Quero L. Combination of chemotherapy and radiotherapy: a thirty years evolution. Cancer Radiother. 2019;23(6–7):662–665. doi: 10.1016/j.canrad.2019.07.157. [DOI] [PubMed] [Google Scholar]
- 136.Opzoomer JW, Sosnowska D, Anstee JE, et al. Cytotoxic chemotherapy as an immune stimulus: a molecular perspective on turning up the immunological heat on cancer. Front Immunol. 2019;10:1654. doi: 10.3389/fimmu.2019.01654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Luo Q, Zhang L, Luo C, et al. Emerging strategies in cancer therapy combining chemotherapy with immunotherapy. Cancer Lett. 2019;454:191–203. doi: 10.1016/j.canlet.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 138.Mondini M, Levy A, Meziani L, et al. Radiotherapy-immunotherapy combinations - perspectives and challenges. Mol Oncol. 2020;14(7):1529–1537. doi: 10.1002/1878-0261.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379(22):2108–2121. doi: 10.1056/NEJMoa1809615. [DOI] [PubMed] [Google Scholar]
- 140.Kim HJ, Chang JS, Roh MR, et al. Effect of radiotherapy combined with pembrolizumab on local tumor control in mucosal melanoma patients. Front Oncol. 2019;9:835. doi: 10.3389/fonc.2019.00835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mohamad O, Diaz de Leon A, Schroeder S, et al. Safety and efficacy of concurrent immune checkpoint inhibitors and hypofractionated body radiotherapy. Oncoimmunology. 2018;7(7):e1440168. doi: 10.1080/2162402X.2018.1440168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Janjigian YY, Maron SB, Chatila WK, et al. First-line pembrolizumab and trastuzumab in HER2-positive oesophageal, gastric, or gastro-oesophageal junction cancer: an open-label, single-arm, phase 2 trial. Lancet Oncol. 2020;21(6):821–831. doi: 10.1016/S1470-2045(20)30169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kato Y, Tabata K, Kimura T, et al. Lenvatinib plus anti-PD-1 antibody combination treatment activates CD8+ T cells through reduction of tumor-associated macrophage and activation of the interferon pathway. PLoS One. 2019;14(2):e0212513. doi: 10.1371/journal.pone.0212513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.O’Donnell JS, Hoefsmit EP, Smyth MJ, et al. The promise of neoadjuvant immunotherapy and surgery for cancer treatment. Clin Cancer Res. 2019;25(19):5743–5751. doi: 10.1158/1078-0432.CCR-18-2641. [DOI] [PubMed] [Google Scholar]
- 145.Said R, Guibert N, Oxnard GR, et al. Circulating tumor DNA analysis in the era of precision oncology. Oncotarget. 2020;11(2):188–211. doi: 10.18632/oncotarget.27418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Snyder A, Morrissey MP, Hellmann MD. Use of circulating tumor dna for cancer immunotherapy. Clin Cancer Res. 2019;25(23):6909–6915. doi: 10.1158/1078-0432.CCR-18-2688. [DOI] [PubMed] [Google Scholar]
- 147.Bidard FC, Weigelt B, Reis-Filho JS. Going with the flow: from circulating tumor cells to DNA. Science translational medicine. 2013;5(207):207ps14. doi: 10.1126/scitranslmed.3006305. [DOI] [PubMed] [Google Scholar]
- 148.Fanelli GN, Naccarato AG, Scatena C. Recent advances in cancer plasticity: cellular mechanisms, surveillance strategies, and therapeutic optimization. Front Oncol. 2020;10:569. doi: 10.3389/fonc.2020.00569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Martins F, Sofiya L, Sykiotis GP, et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat Rev Clin Oncol. 2019;16(9):563–580. doi: 10.1038/s41571-019-0218-0. [DOI] [PubMed] [Google Scholar]
- 150.Rodriguez-Vida A, Perez-Gracia JL, Bellmunt J. Immunotherapy combinations and sequences in urothelial cancer: facts and hopes. Clin Cancer Res. 2018;24(24):6115–6124. doi: 10.1158/1078-0432.CCR-17-3108. [DOI] [PubMed] [Google Scholar]
- 151.Otoshi T, Nagano T, Tachihara M, et al. Possible biomarkers for cancer immunotherapy. Cancers (Basel) 2019;11(7) doi: 10.3390/cancers11070935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Yan YF, Zheng YF, Ming PP, et al. Immune checkpoint inhibitors in non-small-cell lung cancer: current status and future directions. Brief Funct Genomics. 2019;18(2):147–156. doi: 10.1093/bfgp/ely029. [DOI] [PubMed] [Google Scholar]
- 153.Tsao MS, Kerr KM, Kockx M, et al. PD-L1 immunohistochemistry comparability study in real-life clinical samples: results of blueprint phase 2 project. J Thorac Oncol. 2018;13(9):1302–1311. doi: 10.1016/j.jtho.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.De Meulenaere A, Vermassen T, Aspeslagh S, et al. TILs in head and neck cancer: ready for clinical implementation and why (not)? Head Neck Pathol. 2017;11(3):354–363. doi: 10.1007/s12105-016-0776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Li JX, Huang JM, Jiang ZB, et al. Current clinical progress of PD-1/PD-L1 immunotherapy and potential combination treatment in non-small cell lung cancer. Integr Cancer Ther. 2019;18:1534735419890020. doi: 10.1177/1534735419890020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Shergold AL, Millar R, Nibbs RJB. Understanding and overcoming the resistance of cancer to PD-1/PD-L1 blockade. Pharmacol Res. 2019;145:104258. doi: 10.1016/j.phrs.2019.104258. [DOI] [PubMed] [Google Scholar]
- 157.Chen L, Cao MF, Zhang X, et al. The landscape of immune microenvironment in lung adenocarcinoma and squamous cell carcinoma based on PD-L1 expression and tumor-infiltrating lymphocytes. Cancer Med. 2019;8(17):7207–7218. doi: 10.1002/cam4.2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hamada T, Soong TR, Masugi Y, et al. TIME (Tumor Immunity in the MicroEnvironment) classification based on tumor CD274 (PD-L1) expression status and tumor-infiltrating lymphocytes in colorectal carcinomas. Oncoimmunology. 2018;7(7):e1442999. doi: 10.1080/2162402X.2018.1442999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gettinger S, Choi J, Hastings K, et al. Impaired HLA class i antigen processing and presentation as a mechanism of acquired resistance to immune checkpoint inhibitors in lung cancer. Cancer Discov. 2017;7(12):1420–1435. doi: 10.1158/2159-8290.CD-17-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Tran L, Theodorescu D. Determinants of resistance to checkpoint inhibitors. Int J Mol Sci. 2020;21(5) doi: 10.3390/ijms21051594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Fuchs TL, Sioson L, Sheen A, et al. Assessment of tumor-infiltrating lymphocytes using International TILs Working Group (ITWG) system is a strong predictor of overall survival in colorectal carcinoma: a study of 1034 patients. Am J Surg Pathol. 2020;44(4):536–544. doi: 10.1097/PAS.0000000000001409. [DOI] [PubMed] [Google Scholar]
- 162.Lantuejoul S, Damotte D, Hofman V, et al. Programmed death ligand 1 immunohistochemistry in non-small cell lung carcinoma. J Thorac Dis. 2019;11(Suppl 1):S89–S101. doi: 10.21037/jtd.2018.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Galuppini F, Dal Pozzo CA, Deckert J, et al. Tumor mutation burden: from comprehensive mutational screening to the clinic. Cancer Cell Int. 2019;19:209. doi: 10.1186/s12935-019-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Darnell EP, Mooradian MJ, Baruch EN, et al. Immune-related adverse events (irAEs): diagnosis, management, and clinical pearls. Curr Oncol Rep. 2020;22(4):39. doi: 10.1007/s11912-020-0897-9. [DOI] [PubMed] [Google Scholar]
- 165.Myers G. Immune-related adverse events of immune checkpoint inhibitors: a brief review. Curr Oncol. 2018;25(5):342–347. doi: 10.3747/co.25.4235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Verma V, Sprave T, Haque W, et al. A systematic review of the cost and cost-effectiveness studies of immune checkpoint inhibitors. J Immunother Cancer. 2018;6(1):128. doi: 10.1186/s40425-018-0442-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Venetis K, Invernizzi M, Sajjadi E, et al. Cellular immunotherapy in breast cancer: the quest for consistent biomarkers. Cancer Treat Rev. 2020;90 doi: 10.1016/j.ctrv.2020.102089. [DOI] [PubMed] [Google Scholar]