Abstract
Background
Healthcare workers are at high risk of occupational exposure to needle stick injury worldwide. Occupational exposure to needle stick injury represents the most common sources of infection such as hepatitis B virus, hepatitis C virus, and human immunodeficiency virus. Thus, this review aimed to determine the career time and previous one-year global pooled prevalence of occupational exposure to needle stick injury among healthcare workers.
Methods
The review considered articles written in English language and published from 2012 to 2020. The articles were searched using nine electronic databases (PubMed, Google Scholar, CINAHL, MEDLINE, Cochrane library, Web of Science, SCOPUS, MedNar, and ScienceDirect) using a combination of Boolean logic operators (AND, OR, and NOT), Medical Subject Headings, and keywords. Quality assessment was performed to determine the relevance of the articles using Joanna Briggs Institute critical appraisal tools. Several steps of assessment and evaluation were taken to select and analyze the relevant articles.
Results
The worldwide pooled prevalence of needle stick injuries among healthcare workers during career time and previous one year was 56.2% (95% CI: 47.1, 64.9) and 32.4% (95% CI: 22.0, 44.8), respectively. The career time pooled prevalence of needle stick injuries based on the socioeconomic development and study area was 54.8% and 55.1%, respectively, and one-year pooled prevalence of needle stick injury was 26.0% and 20.9%.
Conclusion
The review found a high prevalence of occupational exposure to needle stick injury among healthcare workers and suggests the need to improve occupational health and safety services in the healthcare systems.
1. Introduction
Needle stick injuries (NSIs) are among the most common occupational hazards among healthcare workers (HCWs) worldwide that need to be addressed and represent the most common sources of infection [1]. Infectious complications related to occupational exposure to NSI can result in serious health problems ranging from mild to extreme anxiety [2].
Today, at least 20 different pathogens are transmitted by NSIs such as hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) [3, 4]. Annually, hundreds of thousands of HCWs are at high risk of work-related infections such as HBV, HCV, and HIV as a result of exposure to contaminated needle sticks and sharp injuries [5, 6]. Furthermore, the risk of infections from NSIs ranges from 0.2 to 0.5% for HIV, 3–10% for HCV, and 40% for HBV [7].
According to Centers for Disease Control and Prevention (CDC) and European Agency for Safety and Health at Work, more than 385,000 and one million NSIs cases are reported annually among HCWs working in hospitals in the United States and Europe, respectively [8, 9]. Worldwide, about three million of HCWs were exposed to blood pathogens through percutaneous, of which two million were exposed to HBV, 0.9 million exposed to HCV, and 170,000 exposed to HIV of which more than 90% occurred in developing countries [10–12].
World Health Organization (WHO) estimated that NSIs cause HCV that account 16,000, HBV that account 66,000, and HIV that account 1,000 annually among HCWs [13]. Furthermore, percutaneous exposure accounts for approximately 37.0% of HBV, 39.0% of HCV, and 4.4% of HIV cases among HCWs [14].
Determining the worldwide prevalence of needle stick injury among HCWs is necessary, particularly in reducing NSI, creating safer working conditions and cultures, reducing costs, and provision of higher quality services [15–17].
Prior to this study, many studies have reported the prevalence of NSI among healthcare workers at the country, regional, or institutional level [18–22]. Also, there are a few studies that provide worldwide evidence of the prevalence of occupational exposure to NSIs among HCWs and reported one-year prevalence alone [1]. Thus, this study aimed to determine and provide the worldwide pooled prevalence of needle stick injury (both one year and career time prevalence) among healthcare workers that are very important for understanding the problems and designing prevention program including occupational health and safety practices and standard precautions.
2. Methods
2.1. Eligibility Criteria
The articles that met the following inclusion criteria were included in the systematic review and meta-analysis:
(i). Study Design. Cross-sectional studies
(ii). Outcome. Studies that provide quantitated outcomes (magnitude, frequency, or prevalence of NSI)
(iii). Study Area. Studies conducted in developed and/or developing countries
(iv). Language. Full-text articles published in the English language
(v). Population. Healthcare workers and medical students regardless of their occupation
(vi). Publication Issue. Articles published in peer-reviewed journals from 2012 to 2020
On the contrary, the studies reported period prevalence (such as 3 or/and 6 months) of NSIs, case reports, case series, qualitative studies, review articles, surveillance data/reports, conference abstracts, personal opinions, non-healthcare workers study participants, studies that utilized less than 120 participants, articles written in non-English language, high risk of bias articles, study not available in full texts, and studies published before 2012 were excluded from the study.
2.2. Information Sources and Search Strategy
The articles were searched using nine electronic databases (PubMed, Google Scholar, CINAHL, MEDLINE, Cochrane library, Web of Science, SCOPUS, MedNar, and ScienceDirect) using a combination of Boolean logic operators (AND, OR, and NOT), Medical Subject Headings, and keywords such as health professionals, healthcare workers, healthcare system, developing country, developed country, needle stick injury, and occupational exposure.
The articles were searched using a combination of Boolean logic operators (AND, OR, and NOT), Medical Subject Headings (MeSH), and keywords. The following is a search term used in the initial searching (((“prevalence”[MeSH Terms] OR “prevalence”[All Fields]) AND ((“occupational”[MeSH Terms] OR “occupational”[All Fields], OR “work place”[All Fields] OR “workplace”[MeSH])) AND ((“needle stick injury”[MeSH Terms] OR (“needle stick”[All Fields] AND “injury”[All Fields]) OR “needle stick injury” [All Fields])) AND ((“healthcare workers” [MeSH Terms] OR “healthcare”[All Fields] AND “workers”[All Fields]) OR “healthcare workers”[All Fields])) OR ((“health professional”[MeSH Terms] OR (“health”[All Fields] AND “professional”[All Fields]) OR “health professional”[All Fields])) OR ((“health provider”[MeSH Terms] OR (“health”[All Fields] AND “provider”[All Fields]) OR “health provider”[All Fields])) AND ((“developing country”[MeSH Terms] OR (“developing”[All Fields] AND “countries”[All Fields]) OR “developing countries”[All Fields])) OR ((“developed countries”[MeSH Terms] OR (“developed”[All Fields] AND “countries”[All Fields]) OR “developed countries”[All Fields])).
Then, all identified keywords and an index term were checked across the included nine electronic databases. Finally, searching the reference list of all identified articles for further articles was conducted.
2.3. Study Selection
Duplicated articles were removed using the ENDNOTE software version X5 (Thomson Reuters, USA). The authors (DA. Mengistu, ST. Tolera, and YM. Demmu) screened the titles and abstracts of the identified articles by applying the inclusion and exclusion criteria. Finally, the review included only articles conducted to determine the prevalence of NSIs among healthcare workers in healthcare systems of developing or developed countries.
2.4. Quality Assessment
Full-text articles, available in English language, with clear objectives and methodology, and studies including needle stick injury as a dependent variable and providing quantitative outcomes were selected. These articles were then evaluated to confirm their relevance to the study and to confirm the quality of the work.
Furthermore, selected articles were subjected to a rigorous, independent appraisal using standardized critical appraisal tools (JBI Critical Appraisal tools) [23] to determine the quality and relevance of the articles. Then, the score was taken across all studies and graded as high (85% and above score), moderate (60–85% score), and low (<60% score) quality. Disagreement made on what is to be extracted was solved by discussion. The PRISMA guidelines protocol [24] was used to conduct the review.
2.5. Data Extraction
The authors (DA. Mengistu, ST. Tolera, and YM. Demmu) independently extracted data from the included articles. A predefined Microsoft Excel 2016 format was used to extract information from selected studies under the following headings: author, publication year, country of study, study design, and primary outcomes such as prevalence or magnitude of exposure to NSI and possible confounding factors considered. In general, all required data were extracted from the eligible articles.
2.6. Data Analysis and Statistical Procedures
The prevalence of NSI was categorized into career time and 12-month prevalence. For those studies reporting the frequency of NSI without calculating the prevalence, the prevalence was calculated by dividing the frequency of exposed to the total sample size or multiplying the ratio of exposed to sample size.
The pooled prevalence of both NSIS was done using Comprehensive Meta-Analysis (CMA) version 3.0 statistical software. The random-effect model and forest plot were used to estimate the pooled prevalence of needle stick injury among healthcare workers with 95% confidence intervals (95% CI). The possibility of publication bias was assessed by visual funnel plots, and a p value <0.05 was considered as the evidence for publication bias. Furthermore, subgroup analysis was conducted based on the countries where the articles were conducted, and socioeconomic development, to minimize the random variations (heterogeneity) between the point estimates of the included articles.
2.7. Heterogeneity
In this study, Cochran's Q test (Q) and (I Squared test) I2 statistics were used to evaluate the heterogeneity of the included articles. Furthermore, the differences among included articles were evaluated using graphical and statistical tests. Then, the characteristics of the articles were described using texts, tables, and forest plots. Forest plot was used to evaluate the pooled prevalence of both NSIs. Subgroup analysis was done based on study area and socioeconomic development.
3. Results
3.1. Study Selection
A total of 3,018 studies published from 2012 to 2020 were identified. Then, 976 duplicate articles were excluded, while 1,781 articles were excluded based on the exclusion criteria. Furthermore, 161 full-text studies were further assessed to determine their eligibility, of which 143 studies were excluded as they failed to report the prevalence of needle stick injuries, due to their unclear objectives, unclear methods, small sample size, and non-healthcare worker participants.
Finally, 18 articles that met the inclusion criteria were included in the review (Figure 1).
Figure 1.
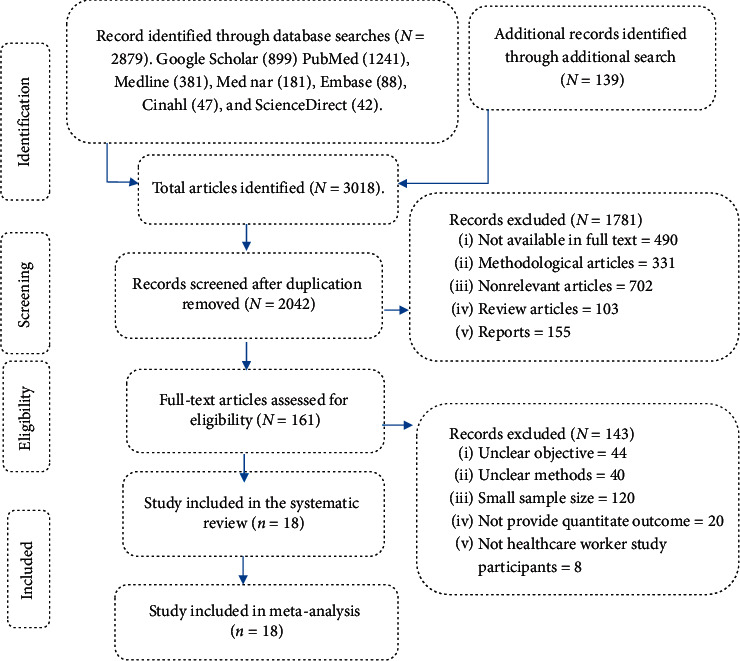
PRISMA flow diagram shows the selection process of included articles for a systematic review and meta-analysis.
3.2. Study Characteristics
A total of 10,233 healthcare workers were included in 18 studies, of which were conducted in 14 countries [16, 25–41]: three articles [29, 33, 41] in Iran, two in Ethiopia [27, 36], two in India [28, 39], and one (5.55%) in other countries such as Nigeria [30], USA [25], China [31], Serbia [26], Saudi Arabia [32], Bangalore [34], Thailand [16], Australia [35], Bosnia and Herzegovina [37], Tanzania [38], and Switzerland [40].
The included studies had a sample size ranging from 120 [30] to 2691 [40] HCWs. Based on JBI Critical Appraisal tool, 15 (83.3%) of the included articles had a low risk of bias, while the remaining three had a medium risk of bias. The career time and previous one-year prevalence of NSIs among HCWs was in the range from 29.8% [32] to 100% [33] and from 9.7% [40] to 81.7% [33], respectively.
Among the included articles, 6 articles [26–30, 33] reported both prevalence of NSIs in career time and previous one year, while 6 [25, 31, 32, 36, 37, 41] and 6 [16, 34, 35, 38–40] of articles reported career time alone and previous one-year prevalence of NSIs alone, respectively. Most ( 5 (83.3%)) of the included articles [16, 26–34, 36–39, 41] were conducted in the developing countries, while the rest of the studies [25, 35, 40] were in a developed country (Table 1).
Table 1.
Overall characteristics of included articles in the systematic review and meta-analysis.
| Authors (publication year) | N | NSI prevalence | Study design | Location | Socioeconomic development | Risk of bias | Reference | |
|---|---|---|---|---|---|---|---|---|
| Life time | One year | |||||||
| Alhazmi and Surber, 2018 | 926 | 54.64 | NA | Cross-sectional | USA | Developed | Low | [25] |
| Marković et al., 2013 | 216 | 60.6 | 15.7 | Cross-sectional | Serbia | Developing | Low | [26] |
| Yasin et al., 2019 | 282 | 42.2 | 20.6 | Cross-sectional | Ethiopia | Developing | Low | [27] |
| Archana et al., 2018 | 950 | 68.3 | 35.3 | Cross-sectional | India | Developing | Low | [28] |
| Jahangiri et al., 2015 | 168 | 76.0 | 54.0 | Cross-sectional | Iran | Developing | Low | [29] |
| Amira and Awobusuyi, 2014 | 120 | 40.2 | 24.5 | Cross-sectional | Nigeria | Developing | Low | [30] |
| Tabatabaei et al., 2016 | 393 | 60.3 | NA | Cross-sectional | China | Developing | Low | [31] |
| AlDakhil et al., 2019 | 450 | 29.8 | NA | Cross-sectional | Saudi Arabia | Developing | Low | [32] |
| Akhuleh et al., 2019 | 306 | 100 | 81.7 | Cross-sectional | Iran | Developing | Low | [33] |
| Selladurai, and Shireen, 2019 | 240 | NA | 47.5 | Cross-sectional | Bangalore | Developing | Low | [34] |
| Kasatpibal et al., 2016 | 2031 | NA | 23.7 | Cross-sectional | Thailand | Developing | Low | [16] |
| Marjadi et al., 2017 | 169 | NA | 16.6 | Cross-sectional | Australia | Developed | Low | [35] |
| Abere et al., 2020 | 241 | 73.3 | NA | Cross-sectional | Ethiopia | Developing | Low | [36] |
| Musa et al., 2014 | 203 | 40.4 | NA | Cross-sectional | Bosnia and Herzegovina | Developing | Medium | [37] |
| Chalya et al., 2015 | 436 | NA | 35.32 | Cross-sectional | Tanzania | Developing | Low | [38] |
| Jaybhaye et al., 2014 | 220 | NA | 49.1 | Cross-sectional | India | Developing | Medium | [39] |
| Voide et al., 2012 | 2.691 | NA | 9.7 | Cross-sectional | Switzerland | Developed | Low | [40] |
| Shaghaghian et al., 2015 | 191 | 43.5 | NA | Cross-sectional | Iran | Developing | Medium | [41] |
NSI = needle stick injury; NA = not applicable; N = sample size.
3.3. Prevalence of Needle Stick Injury
3.3.1. Career Time Prevalence of Needle Stick Injury
The career time prevalence of occupational exposure to needle stick injury among healthcare workers was 56.2% (95% CI of 47.1 to 64.9), with I2 = 96.474% and a p value < 0.001 (Figure 2).
Figure 2.
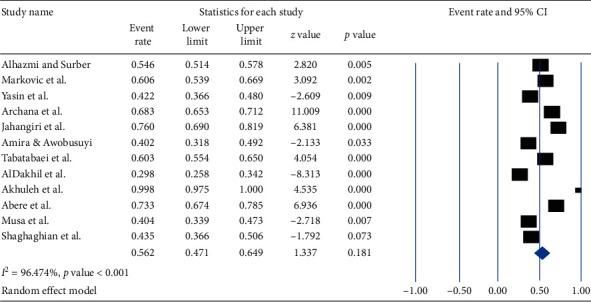
Forest plot shows the pooled prevalence of career time occupational exposure to needle stick injury among healthcare workers.
Based on a subgroup analysis by country where the studies are conducted, the lowest prevalence (29.8% (95% CI: 25.8, 34.2%) with a value of <0.001) of career time exposure to NSI among HCWs was observed in Saudi Arabia, whereas the highest prevalence (81.5%, (95% CI: 49.3–95.3%) with a p value of 0.05) was in Iran. The overall pooled prevalence of career time occupational exposure to NSI was 55.1% (95% CI: 53.3–56.8%) with a value of p < 0.001 (Figure 3).
Figure 3.
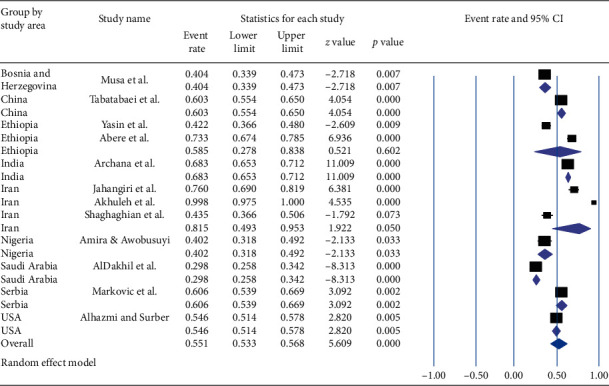
Forest plot shows the subgroup analysis of pooled prevalence of career time occupational exposure to needle stick injury based on the study area.
Based on socioeconomic development, the lowest pooled prevalence (54.6% (95% CI: 51.4, 57.8%) with a p value of 0.005) of career time occupational exposure to NSI was in developed countries while the highest pooled prevalence (57.0%, (95% CI: 46.1–67.3%) with a p value of 0.02) was in developing countries. The overall pooled prevalence of career time occupational exposure to NSI among HCWs was 54.8% (95% CI: 51.7–57.9%) with a p value of 0.002 (Figure 4).
Figure 4.
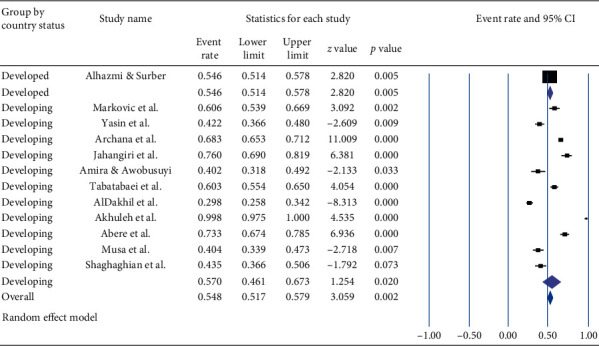
Forest plot shows the subgroup analysis of pooled prevalence of career time occupational exposure to needle stick injury based on socioeconomic development.
3.3.2. Previous One-Year Prevalence of Needle Stick Injury
The pooled prevalence of occupational exposure to needle stick injury among HCWs in the previous 12 months was 32.4% (95% CI: 22.0, 44.8 and a p value = 0.006) with I2 = 98.76% and a p value of <0.001 (Figure 5).
Figure 5.
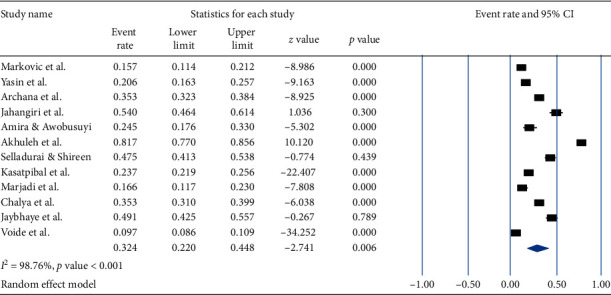
Forest plot shows the pooled prevalence of occupational exposure to needle stick injury in the previous one year.
Based on a subgroup analysis by countries where the studies are conducted, the lowest prevalence [9.7% (95% CI: 8.6%–10.9%)] of NSI in the previous one year was observed in Switzerland, whereas the highest prevalence [69.6%, (95% CI: 38.2–89.5%)] of NSI was observed among the studies conducted in Iran. The overall pooled prevalence during the previous one year was 20.9% (95% CI: 19.8–22.0%) with a value of p < 0.001 (Figure 6).
Figure 6.
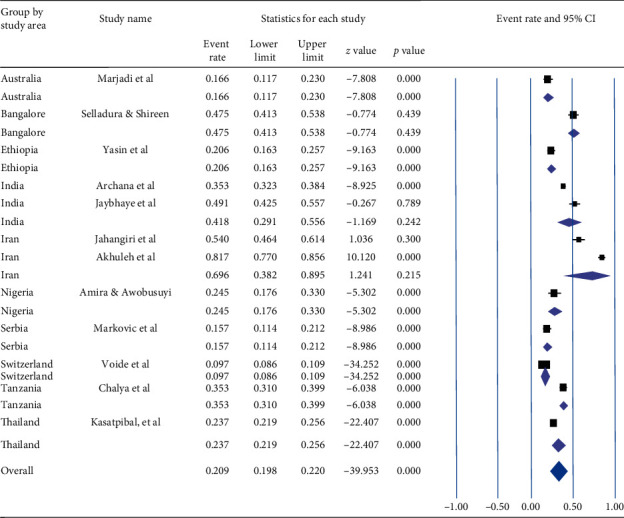
Forest plot shows the subgroup analysis of pooled prevalence of needle stick injury during the previous one year based on the study area.
Based on socioeconomic development, the pooled prevalence of NSI among HCWs in the previous one year was 12.4% (95% CI: 7.2%–20.5%, a p value <0.0001) and 37.8% (95% CI: 27.6–49.2%, a p value of 0.036) in developed and developing countries, respectively. The overall pooled prevalence of NSI was 26.0% (95% CI: 19.6–33.7%) with a p value of <0.001 (Figure 7).
Figure 7.
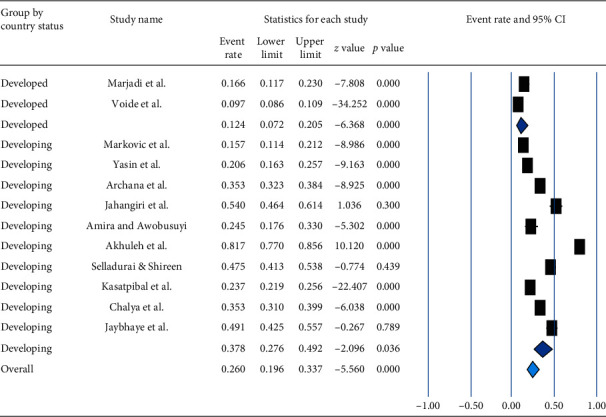
Forest plot shows the subgroup analysis of pooled prevalence of needle stick injury in the previous one year based on socioeconomic development.
4. Discussion
Occupational exposure to NSIs is a major source for the transmission of blood-borne pathogens such as HBV, HCV, and HIV. However, the current review found the pooled prevalence of needle stick injury among HCWs during career time and previous one year accounted 56.2% and 32.4%, respectively. Also, we found a lower pooled prevalence of the previous one-year needle stick injury than the prevalence of NSI injury reported by Bouya et al., 2020 (44.5%; 95% CI 33.7, 53.2) [1]. Auta et al., 2018 [42], also reported the one-year global pooled prevalence of percutaneous injuries that accounted 36.4% (95% CI: 32.9, 40.0) that was higher than our estimates.
The pooled prevalence of needle stick injury among HCWs during their career time and in the previous one year varied based on publication year, socioeconomic development, and study area (country). This finding may be related to the variation in the application of standard procedures, occupational health and safety systems, availability and implementation of policies, poor NSI management, and unsafe working environments. The health problems related to occupational exposure to NSI such as HBV, HCV, and HIV infections were higher in developing countries [10, 13, 42, 43]. Our review also found the pooled prevalence of NSIs during career time and previous one year among HCWs in developing countries was higher than in developed countries.
Overall, the review reported a high prevalence of NSIs among HCWs; thus occupational health and safety are crucial to reduce the risk of occupational exposure to NSI and the transmission of infectious diseases. Applying at least the following principles such as (1) establishing and implementing policies on NSIs management, (2) creating an appropriate safety and organizational culture, (3) applying standard precautions, (4) regular training on infection prevention and standard precautions, (5) regularly monitoring the proper implementation of guidelines, and (6) developing long-term NSIs reporting systems that play a great role in reducing NSIs and preventing infectious disease [1, 10, 42–45].
Our review included studies from only fourteen countries. Most of these studies were conducted in developing countries, which limits the interpretation of results. Furthermore, the included articles were cross-sectional studies and the methodological limitations of such studies need to be considered when interpreting their results. Also, data from most studies were collected based on a self-reported manner and this can affect the prevalence of needle stick injury due to reporting of exposure.
5. Conclusion
The review found a high prevalence of occupational exposure to needle stick injury among HCWs and suggests the need to improve occupational health and safety services in healthcare system globally. Thus, applying standard precautions, regularly training on infection prevention, and regularly monitoring the proper implementation of guidelines play a great role in reducing NSIs and preventing infectious diseases.
Abbreviations
- CDC:
Centers for Disease Control and Prevention
- CMA:
Comprehensive meta-analysis
- HBV:
Hepatitis B virus
- HCV:
Hepatitis C virus
- HCWs:
Healthcare workers
- HIV:
Human immunodeficiency virus
- JBI:
Joanna Briggs Institute
- NSI:
Needle stick injury
- PRISMA:
Preferred Reporting Items for Systematic Review and Meta-Analysis
- WHO:
World Health Organization.
Data Availability
All the data are included in the systematic review and meta-analysis. In addition, PRISMA Protocols 2015 checklist is the recommended item to address in a systematic review and meta-analysis.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
DA. Mengistu conceived the idea and had major roles in the data review, extraction, and analysis. ST. Tolera and YM. Demmu also had a role in data extraction. All authors (DA. Mengistu, ST. Tolera, and YM. Demmu) contributed to analysis, writing, drafting, and editing, read and approved the final version to be published, and agreed on all aspects of this work.
Supplementary Materials
PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis) 2015 checklist is one of the recommended items to address in a systematic review.
References
- 1.Bouya S., Balouchi A., Rafiemanesh H., Amirshahi M., Dastres M., Moghadam M. P. Behnamfar et al, “Global Prevalence and Device Related Causes of Needle Stick Injuries among Health Care Workers. A Systematic Review and Meta-Analysis, Annals of Global Health. 2020;86(1):1–8. doi: 10.5334/aogh.2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yimechew Z., Tiruneh G., Ejigu T., et al. Occupational exposures to blood and body fluids among health care workers and medical students in University of Gondar Hospital, northwest of Ethiopia. Global Journal of Medical Research Microbiology and Pathology. 2013;13:17–23. [Google Scholar]
- 3.Collins C. H., Kennedy D. A. Microbiological hazards of occupational needlestick and “sharps” injuries. Journal of Applied Microbiology. 1987;62(5):385–402. [PubMed] [Google Scholar]
- 4.Whitby R. M., McLaws M. L. Hollow‐bore needlestick injuries in a tertiary teaching hospital: epidemiology, education and engineering. Medical Journal of Australia. 2002;177(8):418–422. doi: 10.5694/j.1326-5377.2002.tb04881.x. [DOI] [PubMed] [Google Scholar]
- 5.Stein A. D., Makarawo T. P., Ahmad M. F. R. A survey of doctors’ and nurses’ knowledge, attitudes and compliance with infection control guidelines in Birmingham teaching hospitals. Journal of Hospital Infection. 2003;54(1):68–73. doi: 10.1016/s0195-6701(03)00074-4. [DOI] [PubMed] [Google Scholar]
- 6.Nagao Y., Baba H., Torii K., et al. A long-term study of sharps injuries among health care workers in Japan. American Journal of Infection Control. 2007;35(6):407–411. doi: 10.1016/j.ajic.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Cheng HC., Su CY., Yen AM., Huang CF. Factors affecting occupational exposure to needlestick and sharps injuries among dentists in Taiwan” A nationwide survey. PLoS One. 2012;7 doi: 10.1371/journal.pone.0034911.e34911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Stop Sticks Campaign–Sharps Injuries. 2019, https://www.cdc.gov/niosh/%20stopsticks/sharpsinjuries.html. [Google Scholar]
- 9.Himmelreich H., Rabenau HF., Rindermann M., et al. The management of needlestick injuries. Deutsches Ärzteblatt International. 2013;110:p. 61. doi: 10.3238/arztebl.2013.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization (WHO) The World Health Report: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 11.Sagoe-Moses C., Pearson R. D., Perry J., Jagger J. Risks to health care workers in developing countries. New England Journal of Medicine. 2001;345(7):538–541. doi: 10.1056/nejm200108163450711. [DOI] [PubMed] [Google Scholar]
- 12.ILO and WHO. Joint ILO/WHO Guidelines on Health Services Organization and HIV/AIDS. Geneva, Switzerland: Anonymous; 2005. pp. 15–17. ISBN 92-2-117554-5. [Google Scholar]
- 13.Prüss-Üstün A., Rapiti E., Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. American Journal of Industrial Medicine. 2005;48(6):482–490. doi: 10.1002/ajim.20230. [DOI] [PubMed] [Google Scholar]
- 14.Rapiti E., Prüss-Üstün A., Hutin Y. Sharps Injuries: Assessing the Burden of Disease from Sharps Injuries to Health-Care Workers at National and Local Levels. Geneva, Switzerland: World Health Organization; 2005. http://www.who.int/quantifying_ehimpacts/%20publications%20/ebd11.pdf?ua=1. [Google Scholar]
- 15.Cooke C. E., Stephens J. M. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Medical Devices: Evidence and Research. 2017;10:p. 225. doi: 10.2147/mder.s140846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kasatpibal N., Whitney J. D., Katechanok S., et al. Prevalence and risk factors of needlestick injuries, sharps injuries, and blood and body fluid exposures among operating room nurses in Thailand. American Journal of Infection Control. 2016;44(1):85–90. doi: 10.1016/j.ajic.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Santos L. T. D., Rocha F. L. R., Marziale M. H. P. Needlesticks with safety devices and accident prevention: an integrative review. Revista Brasileira De Enfermagem. 2018;71(6):3084–3092. doi: 10.1590/0034-7167-2017-0719. [DOI] [PubMed] [Google Scholar]
- 18.Senthil A., Anandh B., Jayachandran P., et al. Perception and prevalence of work-related health hazards among health care workers in public health facilities in southern India. International Journal of Occupational and Environmental Health. 2015;21(1):74–81. doi: 10.1179/2049396714y.0000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Desalegn Z., Gebreselassie S., Asemamaw Y. Epidemiology of needle stick-sharp injuries (NSSIs) and potential high risk exposures among health professionals in Ethiopia: neglected public health concern. American Journal of Health Research. 2015;3(5):298–304. doi: 10.11648/j.ajhr.20150305.16. [DOI] [Google Scholar]
- 20.Jahnavi R., Manjunath M., Mahendra B. J., et al. Needle stick injury among health care workers in a government teaching hospital, mandya. International Journal of Scientific Study. 2014;2(7):103–106. [Google Scholar]
- 21.Dilie A., Amare D., Gualu T. Occupational exposure to needle stick and sharp injuries and associated factors among health care workers in awi zone, amhara regional state, northwest Ethiopia. Journal of Environmental and Public Health. 2017;2017:p. 6. doi: 10.1155/2017/2438713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Auta A., Adewuyi E. O., Tor-Anyiin A., et al. Health-care workers’ occupational exposures to body fluids in 21 countries in Africa: systematic review and meta-analysis. Bulletin of the World Health Organization. 2017;95(12):831–841F. doi: 10.2471/blt.17.195735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Joanna Briggs Institute. Critical Appraisal Tools for Use in the JBI Systematic Reviews Checklist for Prevalence Studies. Adelaide SA 5005, Australia: The University of Adelaide; 2014. https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_Appraisal%20Checklist_for_%20Prevalence_Studies2017_0.pdf. [Google Scholar]
- 24.Moher D., Shamseer L., Clarke M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1) doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alhazmi R. A., Surber Occupationa S. J. Exposure to blood and bodily fluids among health care workers in a medical teaching hospital. Journal of Public Health Hygiene and Safety. 2018;1(1):p. 101. [Google Scholar]
- 26.Marković-Denić L., Branković M., Maksimović1 N., et al. Occupational exposures to blood and body fluids among health care workers at university hospitals. Srpski arhiv za celokupno lekarstvo. 2013;141(11-12):789–793. doi: 10.2298/sarh1312789m. [DOI] [PubMed] [Google Scholar]
- 27.Yasin J., Fisseha R., Mekonnen F., Yirdaw K. Occupational exposure to blood and body fluids and associated factors among health care workers at the University of Gondar Hospital, Northwest Ethiopia. Environmental Health and Preventive Medicine. 2019;24(18) doi: 10.1186/s12199-019-0769-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Archana L. P. A., Ashraf R., Meriton S. A., Christina M. P., Haggadist G. J. A cross sectional study on needle stick and sharp injuries among health care providers in tertiary centers, Tamil Nadu. International Journal Of Community Medicine And Public Health. 2018;5(3):982–986. doi: 10.18203/2394-6040.ijcmph20180524. [DOI] [Google Scholar]
- 29.Jahangiri M., Rostamabadi A., Hoboubi N., Tadayon N., Soleimani A. Needle stick injuries and their related safety measures among nurses in a university hospital, shiraz, Iran. Safety and Health at Work. 2016;7:72–77. doi: 10.1016/j.shaw.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amira C. O., Awobusuyi J. O. Needle-stick injury among health care workers in hemodialysis units in Nigeria: a multi-center study. International Journal of Occupational and Environmental Medicine. 2014;5:1–8. [PMC free article] [PubMed] [Google Scholar]
- 31.Tabatabaei S. M., Behmanesh Pour F., Ordoni Avval J., Osmani S., Mokhtari S., Aghebat Bekheyr M. Occupational exposure to blood and other body fluids among healthcare workers in three teaching hospitals, southeast Iran. International Journal of Infection. 2016;3(3) doi: 10.17795/iji-32879.e32879 [DOI] [Google Scholar]
- 32.AlDakhil L., Yenugadhati N., Al Seraihi O., Al Zoughoo M. Prevalence and associated factors for needlestick and sharp injuries (NSIs) among dental assistants in Jeddah, Saudi Arabia. Environmental Health and Preventive Medicine. 2019;24:p. 6. doi: 10.1186/s12199-019-0815-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Akhuleh O. Z., Nasiri E., Heidari M., Bazari Z. Frequency of sharp injuries and its related factors among high-risk wards staff. Journal of Nursing and Midwifery Sciences. 2019;6:204–209. doi: 10.4103/JNMS.JNMS_25_19. [DOI] [Google Scholar]
- 34.Selladurai S., Shireen N. A study to estimate the prevalence of occupational exposure to blood and body fluids among the health care workers in a teaching hospital attached to Bangalore medical college and research Institute (BMCRI), Bangalore. National Journal of Community Medicine. 2019;10(5):252–255. [Google Scholar]
- 35.Marjadi B., Nguyen J. D., Hoppett P., Mary-Louise M. Needlestick injury among medical students in an Australian university. Journal of Infectious Diseases and Epidemiology. 2017;3(2) doi: 10.23937/2474-3658/1510034. [DOI] [Google Scholar]
- 36.Abere G., Yenealem D. G., Wami S. D. “Occupational exposure to blood and body fluids among health care workers in gondar town, northwest Ethiopia”, A result from cross-sectional study. Journal of Environmental and Public Health. 2020;2020:p. 9. doi: 10.1155/2020/3640247.3640247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Musa S., Peek-Asa C., Young T., Jovanovic N. Needle stick injuries, sharp injuries and other occupational exposures to blood and body fluids among health care workers in a general hospital in sarajevo, Bosnia and Herzegovina. International Journal of Occupational Safety and Health. 2014;4(1):31–371. doi: 10.3126/ijosh.v4i1.9847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chalya L., Seni J., Mushi F., et al. Needle-stick injuries and splash exposures among health-care workers at a tertiary care hospital in north-western Tanzania. Tanzania Journal of Health Research”. 2015;17(2):1–15. doi: 10.4314/thrb.v17i2.3. [DOI] [Google Scholar]
- 39.Jaybhaye D. R., Dahire P. L., Nagaonkar A. S., Vedpathak V. L., Deo D. S., Kawalkar U. G. Needle stick injuries among health care workers in tertiary care hospital of rural India. International Journal of Medical Science and Public Health. 2014;3:48–51. doi: 10.5455/ijmsph.2013.230920133. [DOI] [Google Scholar]
- 40.Voide C., Darling K., Kenfak-Foguena A., Erard V., Cavassini M., Lazor-Blanchet C. Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital. Swiss Medical Weekly. 2012;142 doi: 10.4414/smw.2012.13523. [DOI] [PubMed] [Google Scholar]
- 41.Shaghaghian S., Golkari A., Pardis S., Rezayi A. Occupational exposure of shiraz dental students to patients’ blood and body fluid. Journal of Dentistry Shiraz University Medical Sciences. 2015;16(3):206–213. [PMC free article] [PubMed] [Google Scholar]
- 42.Auta A., Adewuyi E. O., Tor-Anyiin A., et al. Global prevalence of percutaneous injuries among healthcare workers: a systematic review and meta-analysis. International Journal of Epidemiology. 2018;47(6):1980–1972. doi: 10.1093/ije/dyy208. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC) How to Prevent Needlestick and Sharps Injuries. Atlanta, GA, USA: Centers for Disease Control and Prevention; 2012. https://www.cdc.gov/niosh/docs/2012-123/default.html. [Google Scholar]
- 44.Centers for Disease Control and Prevention (CDC) Atlanta, GA, USA: Centers for Disease Control and Prevention; 2020. National occupational research agenda (NORA). Stop sticks–Sharps Injuries. https://www.cdc.gov/nora/councils/hcsa/stopsticks/sharpsinjuries.html. [Google Scholar]
- 45.Yazie T. D., Chufa K. A., Tebeje M. G. Prevalence of needlestick injury among healthcare workers in Ethiopia: a systematic review and meta-analysis. Environmental Health and Preventive Medicine. 2019;24:p. 52. doi: 10.1186/s12199-019-0807-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis) 2015 checklist is one of the recommended items to address in a systematic review.
Data Availability Statement
All the data are included in the systematic review and meta-analysis. In addition, PRISMA Protocols 2015 checklist is the recommended item to address in a systematic review and meta-analysis.


