Abstract
Objective
The objective of this study was to assess the number of dental procedures performed in the Brazilian Public Health System (SUS) during the first wave of COVID-19 in Brazil (1st semester of 2020) and compare it with the same period of 2019.
Methods
A retrospective study was conducted based on the SUS Dataset (DATASUS). Descriptive analysis of the number of dental procedures and socio-demographic regions was presented and the number of dental procedures during the first semester of 2020 was compared to 2019, using Wilcoxon Signed Rank Test (α = 0.05). The number of COVID-19 confirmed cases and deaths were also retrieved from DATASUS.
Results
Dental procedures decreased from 47 million in the first semester of 2019 to 15 million in 2020, representing an overall decrease of about 66%. Statistically significant differences were observed for the numbers of procedures regarding preventive actions related to oral health (-84.53%; p < 0.001), primary care (-60.69%; p < 0.001), endodontic specialized care (-52.50%; p < 0.001), and periodontal and oral surgery specialized care (-54.57%; p < 0.001).
Conclusion
The COVID-19 pandemic also reduced by half the number of oral health procedures provided by the SUS in almost all Brazilian states regardless of whether these states had a large number of confirmed cases or deaths. Future policies are recommended in order to reduce the negative impact of the suspension of dental services on the oral health of the population.
Keywords: Coronavirus, Health policies, Oral health, Pandemic, Public system, SUS
Public Interest Summary
During the early months of the COVID-19 pandemic, elective dental treatments were suspended with the aim of reducing the spread of the virus, but it may also have impacted oral health conditions. For this reason, this study investigated the number of dental procedures during the first semester of 2020 compared to 2019 in the SUS. Dental procedures decreased from 47 million in the first semester of 2019 to 15 million in 2020, and all types of dental procedures (root canal therapy, tooth extraction, and others) declined over the same time period. This study contributes to future policies to demonstrate and to reduce the negative impact of COVID-19 on oral health.
Introduction
The year 2020 started with the global outbreak of a novel coronavirus (severe acute respiratory syndrome coronavirus 2 - SARSCoV-2), which resulted in a rapid increase in the number of infected patients and fatalities [1]. SARSCoV-2 is the causative pathogen of the Coronavirus Disease 2019 (COVID-19). A relative delay in the official announcement of the epidemic by the Chinese Center for Disease Control and Prevention, [2] its high transmission rate, [3] and its low fatality rate compared to other recent epidemics (e.g. SARS – severe acute respiratory syndrome, and MERS – Middle East respiratory syndrome) may have facilitated its spread in the world. As a result, COVID-19 was declared a pandemic by the World Health Organization (WHO) on March 11, 2020 [4].
The literature emphasized the seriousness and pandemic potential of COVID-19, indicating that the identification and isolation of positive cases were needed to fully control the spread of the disease [5], [6], [7]. As the disease spread quickly, governments of the affected countries adopted social distancing and movement restriction policies. For instance, the Wuhan region in China and Italy were “locked down” in an effort to contain the spread of the coronavirus, since asymptomatic patients and patients in the incubation period were also carriers of the disease [8]. The COVID-19 pandemic also had a harmful effect on the global economy as a result of movement restrictions policies (lockdowns, travel bans, borders, and business closures), event cancellations, and limitations of a variety of different services, including non-urgent health care [9].
According to the Center for Disease Control (CDC), dental services were to be limited to only critical services only to reduce potential exposure to SARS-CoV-2 infections and limiting harm to patients [10]. Some studies recommended that non-urgent elective procedures of any kind be halted during the COVID-19 pandemic ([11,12]). This recommendation aimed to concentrate efforts and health care staff to care for COVID-19 patients, increasing the number of available medical rooms, including intensive care units for the cases related to the pandemic. It would also help to avoid nosocomial infections due to admission for elective procedures. Although such recommendations have been made by several studies [13], [14], [15], [16] and from governmental agencies in different countries, [4,17] the Brazilian government delayed adopting the WHO determinations for self-isolation, border closures, limitations on non-essential elective services in the public health system, and extensive testing for all suspected cases. As of DATE, the spread of COVID-19 in Brazil has killed more than 215,000 and infected more than 8 million Brazilians.
Although the available evidence has not demonstrated a clear and direct relationship between dental treatment and transmission of COVID-19, there is clearly the potential for transmission since some dental procedures generate aerosols containing salivary droplets, which is how SARS-CoV-2 is transmitted [13,16]. However, the suspension of non-urgent elective procedures may be seen as a relevant side effect of the measures adopted to reduce COVID-19 contamination, since the reduction of such treatments might result in significant oral health deterioration [18]. Therefore, it is important to assess the impact of COVID-19 on the number and type of dental procedures provided by the Brazilian public health system (Sistema Unico de Saude–SUS). Thus, the objective of this study was to assess the number of dental procedures performed in the SUS during the first wave of COVID-19 in Brazil (1st semester of 2020) and compare it with the same period of 2019 using the SUS dataset (DATASUS).
Material and methods
This retrospective study was based on secondary data from DATASUS, and in accordance to the Brazilian National Resolution (CNS, n° 510), Ethics Committee Approval was not mandatory [19]. This report follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [20].
Source
Data was acquired from DATASUS using the TABNET tool, which provides information to support objective analysis of the health care system, evidence-based decision making, and the development of health action programs [21]. The data extraction was performed independently and carried out for 2 investigators previously calibrated (ALCP, MAK). The method was based on a previous study [22].
Data acquisition
A search comprising provided treatments and the SUS codes related to any dental procedures provided by SUS at outpatient settings (for instance, patients who are not hospitalized overnight but who visits a hospital, clinic, or associated facility for diagnosis or treatment) in the first semester of 2020. Using the same criteria, data of the same time period of 2019 was obtained for comparison. Data was collected on October 9th, 2020.
All treatments were analysed and categorized into: a) preventive actions regarding oral health; b) primary oral care; c) endodontic specialized oral care, and d) periodontal and oral surgery specialized care. The definition of the procedures included in each classification and its SUS codes are presented in Table 1 . Descriptive analysis with the number of procedures per state with relative percentages among the Brazil's socio-demographic regions (south, southeast, northeast, north, and central-west) was performed. Statistical analysis was performed using Stata Software 14 (Stata Corporation, College Station, TX, USA). The impact of COVID-19 on the number of dental procedures provided by the SUS in 2020 was compared with the number of procedures in 2019 using Wilcoxon Signed Rank Test. The number of procedures was considered as the analysis unit and an alpha level of 0.05 was adopted.
Table 1.
Procedures and SUS codes included in the search strategy.
| Procedure | SUS Code | |
| Preventive actions | Collective action of topical application of fluoride gel | 101020015 |
| Fluoric mouthwash collective action | 101020023 | |
| Collective action of supervised tooth brushing | 101020031 | |
| Collective action of oral examination with epidemiological purposes | 101020040 | |
| Primary oral care | Cariostatic application (per tooth) | 101020058 |
| Sealant application (per tooth) | 101020066 | |
| Topical fluoride application (individual per session) | 101020074 | |
| Disclosure of plaque | 101020082 | |
| Temporary sealing of dental cavity | 101020090 | |
| Pulp capping | 307010015 | |
| Primary tooth restoration | 307010023 | |
| Anterior permanent tooth restoration | 307010031 | |
| Posterior permanent tooth restoration | 307010040 | |
| Primary tooth extraction | 414020120 | |
| Permanent tooth extraction | 414020138 | |
| Access to dental pulp and medication (per tooth) | 307020010 | |
| Dental pulpotomy | 307020070 | |
| Prophylaxis / plaque removal | 307030040 | |
| Subgingival scaling and root planing (per sextant) | 307030024 | |
| Supragingival scaling and root planing (per sextant) | 307030059 | |
| Endodontics specialized care | Temporary dressing with or without biomechanical preparation | 307020029 |
| Primary tooth filling | 307020037 | |
| Permanent bi-radicular tooth filling | 307020045 | |
| Permanent tooth filling with three or more roots | 307020053 | |
| Uniradicular permanent tooth filling | 307020061 | |
| Endodontic retreatment in bi-radicular permanent tooth | 307020088 | |
| Endodontic retreatment in permanent tooth with 3 or more roots | 307020096 | |
| Endodontic retreatment in uni-radicular permanent tooth | 307020100 | |
| Root perforation sealing | 307020118 | |
| Periodontics & Oral surgery specialized care | Corono-root scaling (by sextant) | 307030032 |
| Gingival graft | 414020081 | |
| Gingivectomy (by sextant) | 414020154 | |
| Gingivoplasty (per sextant) | 414020162 | |
| Periodontal surgical treatment (by sextant) | 414020375 | |
| Apicectomy with or without retrograde filling | 414020022 | |
| Deepening of the oral vestibule (per sextant) | 414020030 | |
| Correction of muscle bridles | 414020049 | |
| Correction of alveolar ridge irregularities | 414020057 | |
| Jaw tuberosity correction | 414020065 | |
| Periapical curettage | 414020073 | |
| Bone graft from intraoral donor area | 414020090 | |
| Multiple extraction with alveoloplasty by sextant | 414020146 | |
| Glossorraphy | 414020170 | |
| Marsupialization of cysts and pseudocysts | 414020200 | |
| Odontosection / radilectomy / tunneling | 414020219 | |
| Dental replantation and transplantation (per element) | 414020243 | |
| Retained tooth removal (included / impacted) | 414020278 | |
| Torus and exostosis removal | 414020294 | |
| Surgical treatment of oral-dental hemorrhage | 414020359 | |
| Surgical treatment for dental traction | 414020367 | |
| Treatment of alveolitis | 414020383 | |
| Ulotomy / ulectomy | 414020405 | |
| Osteointegrated dental implant | 414020421 | |
| Treatment of facial neuralgia | 307010058 | |
Also, the numbers of total confirmed cases and deaths in the first semester of 2020 were retrieved from the official health ministry website (https://covid.saude.gov.br, accessed on October 9th, 2020.).
Results
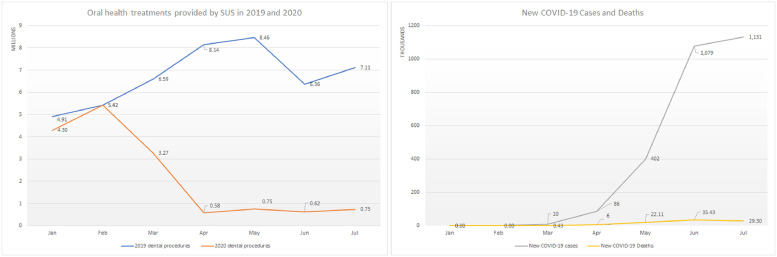
In the first semester (January to July) of 2019, the SUS provided about 47 million dental procedures, but in 2020 (January to July), the number of those same procedures declined to 15.67 million (Fig. 1 ). This decrease represents a reduction of more than 66% of the total number of dental procedures during those seven months of the pandemic. Fig. 1 also shows that before the COVID-19 pandemic (February 2020) the number of dental procedures for both years were similar, and they decreased rapidly after the COVID-19 outbreak in Brazil.
Fig. 1.
Line graphic comparing dental procedures in 2019 (blue), 2020 (orange), and the number of new confirmed COVID-19 cases (grey) and deaths (yellow) each month. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
When comparing the type of dental procedures, statistically significant differences were observed for the numbers of procedures regarding preventive actions related to oral health (-84.53%; p < 0.001; Table 2 ), primary care (-60.69%; p < 0.001; Table 3 ), endodontic specialized care (-52.50%; p < 0.001; Table 4 ), and periodontal and oral surgery specialized care (-54.57%; p < 0.001; Table 5 ). Despite the pandemic, two Brazilian states (Para: +1.39% and Tocantins +10.11%) had a greater number of overall dental procedures in 2020 than in 2019.
Table 2.
Distribution of preventive actions regarding oral health in the Brazilian public health system in 2019 and 2020 and its variation (%).
| 2019 |
2020 |
2019-2020 Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % in the region | % in the country | n | % in the region | % in the country | |||
| North | Acre | 19,600 | 7.71 | 0.15 | 82 | 0.12 | 0.00 | -99.58 |
| Amapa | 0 | 0.00 | 0.00 | 114 | 0.17 | 0.01 | - | |
| Amazonas | 138,330 | 54.38 | 1.08 | 44,367 | 64.59 | 2.24 | -67.93 | |
| Para | 24,951 | 9.81 | 0.19 | 4,720 | 6.87 | 0.24 | -81.08 | |
| Rondonia | 6,464 | 2.54 | 0.05 | 462 | 0.67 | 0.02 | -92.85 | |
| Roraima | 5,503 | 2.16 | 0.04 | 1,470 | 2.14 | 0.07 | -73.29 | |
| Tocantins | 59,531 | 23.40 | 0.47 | 17,474 | 25.44 | 0.88 | -70.65 | |
| Northeast | Alagoas | 59,612 | 2.68 | 0.47 | 10,643 | 5.37 | 0.54 | -82.15 |
| Bahia | 86,384 | 3.88 | 0.67 | 17,179 | 8.66 | 0.87 | -80.11 | |
| Ceara | 116,079 | 5.21 | 0.91 | 7,322 | 3.69 | 0.37 | -93.69 | |
| Maranhao | 1,553,746 | 69.76 | 12.14 | 126,879 | 63.97 | 6.41 | -91.83 | |
| Paraiba | 2,330 | 0.10 | 0.02 | 167 | 0.08 | 0.01 | -92.83 | |
| Pernambuco | 67,853 | 3.05 | 0.53 | 25,313 | 12.76 | 1.28 | -62.69 | |
| Piaui | 287,854 | 12.92 | 2.25 | 583 | 0.29 | 0.03 | -99.80 | |
| Rio Grande do Norte | 26,750 | 1.20 | 0.21 | 2,603 | 1.31 | 0.13 | -90.27 | |
| Sergipe | 26,808 | 1.20 | 0.21 | 7,653 | 3.86 | 0.39 | -71.45 | |
| Central-west | Goias | 148,084 | 15.65 | 1.16 | 59,248 | 34.69 | 2.99 | -59.99 |
| Federal district | 67,545 | 7.14 | 0.53 | 3,002 | 1.76 | 0.15 | -95.56 | |
| Mato Grosso | 268,410 | 28.37 | 2.10 | 50,338 | 29.47 | 2.54 | -81.25 | |
| Mato Grosso do Sul | 462,001 | 48.84 | 3.61 | 58,202 | 34.08 | 2.94 | -87.40 | |
| Southeast | Espirito Santo | 252,617 | 4.50 | 1.97 | 47,119 | 4.33 | 2.38 | -81.35 |
| Minas Gerais | 1,306,642 | 23.29 | 10.21 | 249,907 | 22.96 | 12.62 | -80.87 | |
| Rio de Janeiro | 441,287 | 7.87 | 3.45 | 73,697 | 6.77 | 3.72 | -83.30 | |
| Sao Paulo | 3,608,570 | 64.33 | 28.20 | 717,751 | 65.94 | 36.26 | -80.11 | |
| South | Parana | 2,518,036 | 66.94 | 19.67 | 255,682 | 56.42 | 12.92 | -89.85 |
| Rio Grande do Sul | 718,903 | 19.11 | 5.62 | 120,777 | 26.65 | 6.10 | -83.20 | |
| Santa Catarina | 524,418 | 13.94 | 4.10 | 76,713 | 16.93 | 3.88 | -85.37 | |
| Total | 12,798,308 | 1,979,467 | -84.53 | |||||
| p-value | <0.001 | |||||||
Table 3.
Distribution of primary oral care treatments in the Brazilian public health system in 2019 and 2020 and its variation (%).
| 2019 |
2020 |
2019-2020 Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % in the region | % in the country | n | % in the region | % in the country | |||
| North | Acre | 54.908 | 4.54 | 0.18 | 16.877 | 1.65 | 0.14 | -69.26 |
| Amapa | 28.559 | 2.36 | 0.09 | 10.087 | 0.99 | 0.08 | -64.68 | |
| Amazonas | 292.754 | 24.20 | 0.96 | 69.545 | 6.81 | 0.58 | -76.24 | |
| Para | 527.149 | 43.57 | 1.73 | 642.580 | 62.90 | 5.37 | 21.90 | |
| Rondonia | 115.687 | 9.56 | 0.38 | 14.935 | 1.46 | 0.12 | -87.09 | |
| Roraima | 8.863 | 0.73 | 0.03 | 3.645 | 0.36 | 0.03 | -58.87 | |
| Tocantins | 182.047 | 15.05 | 0.60 | 263.871 | 25.83 | 2.21 | 44.95 | |
| Northeast | Alagoas | 31.748 | 0.53 | 0.10 | 10.475 | 0.83 | 0.09 | -67.01 |
| Bahia | 1.593.051 | 26.73 | 5.23 | 276.354 | 21.80 | 2.31 | -82.65 | |
| Ceara | 732.040 | 12.28 | 2.41 | 177.175 | 13.98 | 1.48 | -75.80 | |
| Maranhao | 1.457.712 | 24.46 | 4.79 | 175.557 | 13.85 | 1.47 | -87.96 | |
| Paraiba | 231.463 | 3.88 | 0.76 | 56.681 | 4.47 | 0.47 | -75.51 | |
| Pernambuco | 657.104 | 11.03 | 2.16 | 206.909 | 16.33 | 1.73 | -68.51 | |
| Piaui | 120.993 | 2.03 | 0.40 | 39.160 | 3.09 | 0.33 | -67.63 | |
| Rio Grande do Norte | 799.275 | 13.41 | 2.63 | 242.384 | 19.12 | 2.03 | -69.67 | |
| Sergipe | 335.476 | 5.63 | 1.10 | 82.738 | 6.53 | 0.69 | -75.34 | |
| Central-west | Goias | 1.015.008 | 41.26 | 3.34 | 345.294 | 39.56 | 2.89 | -65.98 |
| Federal district | 55.676 | 2.26 | 0.18 | 33.271 | 3.81 | 0.28 | -40.24 | |
| Mato Grosso | 634.147 | 25.78 | 2.08 | 241.596 | 27.68 | 2.02 | -61.90 | |
| Mato Grosso do Sul | 755.202 | 30.70 | 2.48 | 252.621 | 28.94 | 2.11 | -66.55 | |
| Southeast | Espirito Santo | 800.104 | 5.07 | 2.63 | 638.244 | 9.08 | 5.33 | -20.23 |
| Minas Gerais | 4.945.644 | 31.33 | 16.25 | 1449.924 | 20.64 | 12.12 | -70.68 | |
| Rio de Janeiro | 1.219.239 | 7.72 | 4.01 | 429.978 | 6.12 | 3.59 | -64.73 | |
| Sao Paulo | 8.821.085 | 55.88 | 28.98 | 4507.230 | 64.16 | 37.67 | -48.90 | |
| South | Parana | 2.657.887 | 52.96 | 8.73 | 922.534 | 51.91 | 7.71 | -65.29 |
| Rio Grande do Sul | 927.222 | 18.48 | 3.05 | 355.008 | 19.98 | 2.97 | -61.71 | |
| Santa Catarina | 1.433.326 | 28.56 | 4.71 | 499.611 | 28.11 | 4.18 | -65.14 | |
| Total | 30,433,369 | 11.964.284 | -60.69 | |||||
| p-value | <0.001 | |||||||
Table 4.
Distribution of endodontic specialized care in the Brazilian public health system in 2019 and 2020 and its variation (%).
| 2019 |
2020 |
2019-2020 Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % in the region | % in the country | n | % in the region | % in the country | |||
| North | Acre | 3,282 | 3.76 | 0.25 | 1,049 | 1.79 | 0.17 | -68.04 |
| Amapa | 746 | 0.85 | 0.06 | 377 | 0.64 | 0.06 | -49.46 | |
| Amazonas | 12,661 | 14.50 | 0.98 | 4,121 | 7.03 | 0.67 | -67.45 | |
| Para | 55,886 | 63.99 | 4.32 | 37,101 | 63.26 | 6.03 | -33.61 | |
| Rondonia | 6,265 | 7.17 | 0.48 | 1,712 | 2.92 | 0.28 | -72.67 | |
| Roraima | 1,638 | 1.88 | 0.13 | 10,841 | 18.48 | 1.76 | 561.84 | |
| Tocantins | 6,856 | 7.85 | 0.53 | 3,447 | 5.88 | 0.56 | -49.72 | |
| Northeast | Alagoas | 7,534 | 2.80 | 0.58 | 2,902 | 2.55 | 0.47 | -61.48 |
| Bahia | 40,718 | 15.16 | 3.14 | 22,205 | 19.48 | 3.61 | -45.47 | |
| Ceara | 46,261 | 17.22 | 3.57 | 18,052 | 15.83 | 2.94 | -60.98 | |
| Maranhao | 37,287 | 13.88 | 2.88 | 13,122 | 11.51 | 2.13 | -64.81 | |
| Paraiba | 34,310 | 12.77 | 2.65 | 14,869 | 13.04 | 2.42 | -56.66 | |
| Pernambuco | 48,238 | 17.96 | 3.73 | 21,244 | 18.63 | 3.45 | -55.96 | |
| Piaui | 16,959 | 6.31 | 1.31 | 8,113 | 7.12 | 1.32 | -52.16 | |
| Rio Grande do Norte | 34,175 | 12.72 | 2.64 | 12,728 | 11.16 | 2.07 | -62.76 | |
| Sergipe | 3,143 | 1.17 | 0.24 | 767 | 0.67 | 0.12 | -75.60 | |
| Central-west | Goias | 40,685 | 34.75 | 3.14 | 25,489 | 41.50 | 4.14 | -37.35 |
| Federal district | 3,921 | 3.35 | 0.30 | 2,372 | 3.86 | 0.39 | -39.51 | |
| Mato Grosso | 20,659 | 17.65 | 1.60 | 11,143 | 18.14 | 1.81 | -46.06 | |
| Mato Grosso do Sul | 51,815 | 44.26 | 4.00 | 22,414 | 36.49 | 3.64 | -56.74 | |
| Southeast | Espirito Santo | 28,204 | 4.39 | 2.18 | 14,661 | 5.19 | 2.38 | -48.02 |
| Minas Gerais | 219,231 | 34.15 | 16.93 | 54,179 | 19.20 | 8.81 | -75.29 | |
| Rio de Janeiro | 82,662 | 12.88 | 6.38 | 41,902 | 14.85 | 6.81 | -49.31 | |
| Sao Paulo | 311,866 | 48.58 | 24.09 | 171,505 | 60.76 | 27.88 | -45.01 | |
| South | Parana | 93,461 | 51.97 | 7.22 | 46,814 | 47.41 | 7.61 | -49.91 |
| Rio Grande do Sul | 34,435 | 19.15 | 2.66 | 22,440 | 22.73 | 3.65 | -34.83 | |
| Santa Catarina | 51,946 | 28.88 | 4.01 | 29,482 | 29.86 | 4.79 | -43.24 | |
| Total | 1,294,844 | 615,051 | -52.50 | |||||
| p-value | <0.001 | |||||||
Table 5.
Distribution of periodontal and oral surgery specialized care in the Brazilian public health system in 2019 and 2020 and its variation (%).
| 2019 |
2020 |
2019-2020 Variation (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % in the region | % in the country | n | % in the region | % in the country | |||
| North | Acre | 3,273 | 1.33 | 0.13 | 1,625 | 1.35 | 0.14 | -50.35 |
| Amapa | 4,298 | 1.75 | 0.17 | 2,133 | 1.77 | 0.19 | -50.37 | |
| Amazonas | 47,603 | 19.33 | 1.93 | 20,781 | 17.27 | 1.85 | -56.35 | |
| Para | 149,880 | 60.87 | 6.06 | 83,993 | 69.82 | 7.48 | -43.96 | |
| Rondonia | 21,889 | 8.89 | 0.89 | 2,555 | 2.12 | 0.23 | -88.33 | |
| Roraima | 2,512 | 1.02 | 0.10 | 1,999 | 1.66 | 0.18 | -20.42 | |
| Tocantins | 16,775 | 6.81 | 0.68 | 7,217 | 6.00 | 0.64 | -56.98 | |
| Northeast | Alagoas | 25,370 | 3.57 | 1.03 | 9,841 | 3.02 | 0.88 | -61.21 |
| Bahia | 143,410 | 20.15 | 5.80 | 73,184 | 22.44 | 6.51 | -48.97 | |
| Ceara | 172,355 | 24.22 | 6.97 | 65,522 | 20.09 | 5.83 | -61.98 | |
| Maranhao | 32,626 | 4.58 | 1.32 | 51,577 | 15.82 | 4.59 | 58.09 | |
| Paraiba | 108,055 | 15.18 | 4.37 | 47,202 | 14.48 | 4.20 | -56.32 | |
| Pernambuco | 112,699 | 15.84 | 4.56 | 39,665 | 12.16 | 3.53 | -64.80 | |
| Piaui | 56,301 | 7.91 | 2.28 | 22,249 | 6.82 | 1.98 | -60.48 | |
| Rio Grande do Norte | 42,700 | 6.00 | 1.73 | 11,972 | 3.67 | 1.07 | -71.96 | |
| Sergipe | 18,095 | 2.54 | 0.73 | 4,857 | 1.49 | 0.43 | -73.16 | |
| Central-west | Goias | 88,841 | 48.55 | 3.59 | 41,139 | 51.80 | 3.66 | -53.69 |
| Federal district | 16,636 | 9.09 | 0.67 | 11,387 | 14.34 | 1.01 | -31.55 | |
| Mato Grosso | 35,623 | 19.47 | 1.44 | 12,008 | 15.12 | 1.07 | -66.29 | |
| Mato Grosso do Sul | 41,907 | 22.90 | 1.69 | 14,892 | 18.75 | 1.33 | -64.46 | |
| Southeast | Espirito Santo | 24,180 | 2.30 | 0.98 | 9,839 | 2.07 | 0.88 | -59.31 |
| Minas Gerais | 231,601 | 21.99 | 9.37 | 87,752 | 18.44 | 7.81 | -62.11 | |
| Rio de Janeiro | 261,636 | 24.84 | 10.58 | 162,062 | 34.06 | 14.43 | -38.06 | |
| Sao Paulo | 535,732 | 50.87 | 21.66 | 216,118 | 45.42 | 19.24 | -59.66 | |
| South | Parana | 115,068 | 41.27 | 4.65 | 50,897 | 41.75 | 4.53 | -55.77 |
| Rio Grande do Sul | 75,295 | 27.00 | 3.04 | 38,336 | 31.45 | 3.41 | -49.09 | |
| Santa Catarina | 88,478 | 31.73 | 3.58 | 32,669 | 26.80 | 2.91 | -63.08 | |
| Total | 2,472,838 | 1,123,471 | -54.57 | |||||
| p-value | <0.001 | |||||||
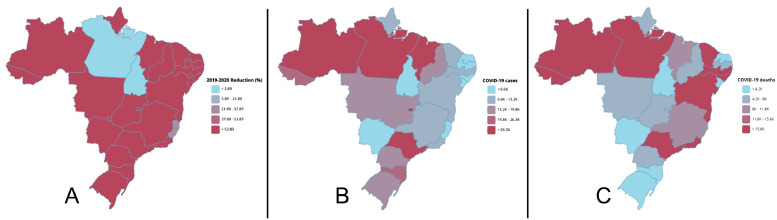
In Fig. 2 , different heat maps display the reduction of dental procedures provided by the SUS in 2020 compared to the same period of 2019. Fig. 2 also shows that the number of procedures decreased by more than 50% in almost the entire country regardless whether the states or regions were heavily affected by the disease or not.
Fig. 2.
Graphical comparison considering (A) the reduction of dental procedures provided by the Brazilian public health system in 2020 compared to the same period of 2019, the number of (B) confirmed COVID-19 cases and (C) deaths of the different Brazilian states.
Discussion
Brazil is one of the few countries that has achieved nearly universal access to health-care services for the population by means of its public health system (SUS). In this perspective, our study evaluated the impact of the COVID-19 pandemic in one of the largest health-care services globally. We identified a reduction of more than 66% of dental procedures from the same period of time in 2019 to 2020. This reduction was significant and occurred in many different procedures, including preventive care, endodontic treatment, periodontal, and surgical procedures. Understanding the number and pattern of this reduction might contribute to better understand the problems the world will face after the pandemic.
The COVID-19 has raised a number of concerns and brought many undesirable consequences to the whole world. The absence of proper treatment resulted in the need for social distancing as one of the most important methods to reduce the spread of the disease, which in turn, resulted in the emergence of an economic crisis amid an international health crisis, causing different countries to adopt different approaches to these problems [23]. While most of European and Asian countries have battled the COVID-19 with lockdowns and restrictive policies, countries like the United States of America and Brazil have adopted less restrictive protocols, which were officially justified by the need to keep their economic activity [24,25]. Not surprisingly, the latter are among the top 3 countries with the greatest number of COVID-19 confirmed cases and deaths, presenting high numbers of cases and death per million of population (USA: 64,323 cases/ 1M population and 1,091 deaths/1M population; Brazil: 36,350 cases/ 1M population and 922 deaths/1M population) according to the online interactive dashboard of the Johns Hopkins University [26].
Dental procedures are thought to involve high risk of COVID-19 transmission [10] because of the proximity to the mucosal of the oral cavity (high-risk route of COVID infection) and the generation of aerosols during a consultation [27,28]. In this perspective, the suspension of elective dental procedures during the COVID-19 pandemic outbreak might result in the reduction of the transmission rate and consequently reduce the pressure on the health care system [11,29]. Conversely, the suspension of elective dental procedures might facilitate the deterioration of the oral health of the population, leading to irreparable damages and consequently reducing the quality of life of these subjects [18]. Oral health and inequalities are a recognized major problem in the world, and such conditions is generally linked with lower-income segments of the population [30]. Thus, the reduction of elective procedures provided by the national public health system observed in our study could reflect the impact that is occurring throughout the globe.
The SUS is based on the principle that a citizen's health is a constitutional right and the government's duty [31], and it was designed to be decentralized, where services are financed and provided at federal, state, or municipal levels [32]. Understanding how the different regions and states of Brazil faced the COVID-19 pandemic, we identified an important reduction of all types of dental procedures provided by SUS in all regions of the country, except for two states that have shown an increase of overall dental procedures in the first semester from 2020 to 2019. This increase might reflect the freedom of this decentralized system, which allows managers to adopt different protocols for halting or keeping elective procedures during the pandemic, according to the characteristics and needs of each community.
Throughout 2020, a number of guidelines and recommendations for the management of dental procedures were proposed in an attempt to stabilize patient's oral health condition, protect the dental staff and patient's general health, and to reduce the burden of dental or hospital clinics [33,34]. Given that one can be infected by COVID-19 without presenting symptoms and that most dental procedures generate aerosols that can carry the virus, the risk of contamination is high. Therefore, teledentistry, with its subunits (teleconsultation, telediagnosis, teletriage, and telemonitoring), conducted by telephone or video-calls was suggested as one method to reduce the risk of contamination [35]. This is especially important for patients who are considered at high risk of severe illness or mortality due to a COVID-19 infection, e.g., in people who are older than 60 years or who have health conditions, like lung or heart disease, diabetes, or conditions that affect their immune system [36]. Although teledentistry was helpful for avoiding contamination in the dental practice, the use of such tool in a wide population service is difficult and needs thorough planning before its implementation.
Teledentistry was not officially recommended by SUS and this fact could explain the great impact on the reduction of all oral health procedures during the pandemics [37]. The reduction of all oral health procedures might have impacted the quality of life of patients during the pandemic and can also have impact on the oral health of an entire population due to the absence of preventive and therapeutic procedures. It is important to state that urgent procedures should have been carried out to reduce one's pain and to avoid irreversible problems on the oral health. Considering that the extent of contamination during oral procedures has not been completely elucidated, the use of personal protective equipment and initial screening is mandatory [38] and the implementation of another important infection-control practice could be the use of saliva tests to diagnose early or asymptomatic cases of COVID-19 prior to consultation [39].
Although this study has assessed a specific country and its public health system, the findings can provide initial guidance for other countries, depending on the characteristics of each country and its health care systems. In this context, we suggest that teledentistry programs and saliva testing could be implemented as standard policies in public health systems, not only to avoid the contamination related to oral health procedures during the pandemic but also to assist in the assessment of patients’ needs and thus help in the establishment of criteria so that oral care can be resumed in order to minimize the impact of this interruption on patients' oral health.
An important limitation of the present study is the data acquisition source, as there is a lack of sociodemographic data, since it does not provide access to patients' gender, age, etc. In addition, no information was available on the official governmental websites regarding the two states that surprisingly reported an increase in the number of oral health procedures during the pandemic. Another limitation of the present study is that there is no information about whether professionals or patients were infected that could be drawn from this database. Despite the financial cuts and restrictions that SUS has been suffering over the last years, the size of the Brazilian population and the additional pressure from COVID-19, SUS did not collapse during the first semester of 2020. However, as there is not yet a treatment or vaccine cleared by the regulatory agencies against COVID-19, caution is recommended to reduce the infection risk during dental treatment. Also, further research should be conducted in order to keep track of the number of procedures after the pandemic to determine whether a reduction in prevention was associated with subsequent increase in extractions.
Conclusion
The COVID-19 pandemic significantly reduced the number of preventive actions related to oral health, primary care, endodontic specialized care, and periodontal and oral surgery specialized care procedures provided by the SUS from 2019 to 2020. Future policies aimed at matching future increases in demand are recommended in order to reduce the effects of the suspension of dental service on the oral health of the population.
STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies
| Item No | Recommendation | |
| Title and abstract | 1 | (a) Indicate the study's design with a commonly used term in the title or the abstract (1) |
| (b) Provide in the abstract an informative and balanced summary of what was done and what was found (1) | ||
| Introduction | ||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported (2-3) |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses (3) |
| Methods | ||
| Study design | 4 | Present key elements of study design early in the paper (4) |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection (4) |
| Participants | 6 | (a) Give the eligibility criteria, and the sources and methods of selection of participants (4) |
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable (4/5) |
| Data sources/ measurement | 8* | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group (4) |
| Bias | 9 | Describe any efforts to address potential sources of bias (n/a) |
| Study size | 10 | Explain how the study size was arrived at (n/a) |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why (5) |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding (5) |
| (b) Describe any methods used to examine subgroups and interactions (5) | ||
| (c) Explain how missing data were addressed (5) | ||
| (d) If applicable, describe analytical methods taking account of sampling strategy (5) | ||
| (e) Describe any sensitivity analyses (5) | ||
| Results | ||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed (5) |
| (b) Give reasons for non-participation at each stage (5) | ||
| (c) Consider use of a flow diagram (N/A) | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders (5) |
| (b) Indicate number of participants with missing data for each variable of interest (5) | ||
| Outcome data | 15* | Report numbers of outcome events or summary measures (5) |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included (5/6) |
| (b) Report category boundaries when continuous variables were categorized | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses |
| Discussion | ||
| Key results | 18 | Summarise key results with reference to study objectives (6-8) |
| Limitations | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias(6-8) |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence (6-8) |
| Generalisability | 21 | Discuss the generalisability (external validity) of the study results (6-8) |
| Other information | ||
| Funding | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based (9) |
Give information separately for exposed and unexposed groups.
Note: An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement.org.
Conflict of Interest
The authors declare that there are no conflicts of interest related to this study.
Ethical Approval
Not required
Acknowledgements
This study was financed in part by Coordination for the Improvement of Higher Education Personnel (CAPES) Finance Code 001.
Footnotes
This study was financed in part by Coordination for the Improvement of Higher Education Personnel
(CAPES) Finance Code 001.
References
- 1.Phelan A.L., Katz R., Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020 doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wiersinga W.J., Prescott HC. What Is COVID-19? JAMA. 2020;324(8):816-. doi: 10.1001/jama.2020.12984. [DOI] [PubMed] [Google Scholar]
- 4.WHO . WHO Director general opening speech at the media briefing on COVID-19. World Health Organization; 2020. 11-March-2020 2020 [cited 2020 17-March] [Google Scholar]
- 5.Li R., Pei S., Chen B., Song Y., Zhang T., Yang W. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraemer M.U.G., Yang C.-.H., Gutierrez B., Wu C.-.H., Klein B., Pigott D.M. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020:eabb4218. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5(5):e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guidance for Dental Settings [Internet]. 2020.
- 11.Jamal M., Shah M., Almarzooqi S.H., Aber H., Khawaja S., El Abed R. Overview of transnational recommendations for COVID-19 transmission control in dental care settings. Oral Dis. 2020 doi: 10.1111/odi.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rösing C.K., Cavagni J., Langa G.P.J., Mazzetti T., Muniz F. Dental care and the COVID-19 pandemic: the precautionary principle and the best available evidence. Pesqui Bras Odontopediatria Clín Integr. 2020;20 [Google Scholar]
- 13.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T.T., Moon H.S., Le A., Carrasco L.R., Panchal N. Proceedings from the OMS resurgence conference for resuming clinical practice after COVID-19 in the USA. Int. J. Oral Maxillo-Fac Surg. 2020 doi: 10.1016/j.ijom.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brazilian Health Ministry . 1st edition. 2020. National contingency plan for human infection with the new coronavirus COVID-19.https://www.portalarquivos2saudegovbr/images/pdf/2020/fevereiro/13/plano-contingencia-coronavirus-COVID19pdf [Google Scholar]
- 16.Banakar M., Bagheri Lankarani K., Jafarpour D., Moayedi S., Banakar M.H., MohammadSadeghi A. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Health. 2020;20(1):275. doi: 10.1186/s12903-020-01270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Souza W.M., Buss L.F., Candido D.D.S., Carrera J.P. Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. 2020;4(8):856-65. [DOI] [PubMed]
- 18.Oliveira L.M., Zanatta FB. Self-reported dental treatment needs during the COVID-19 outbreak in Brazil: an infodemiological study. 2020;34:e114. [DOI] [PubMed]
- 19.MS . Resolution N° 510, from Apr-07-2016. Brazilian Health Ministry; 2016. [Google Scholar]
- 20.von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 21.SUS SUDS. Tabnet DATASUS. tabnet.datasus.gov.br Access: Mar-19-2020. 2020 [cited 2020 Mar-19]. tabnet.datasus.gov.br ].
- 22.Mda K., Pires A.L.C., Saporiti J.M. Dental implant therapy in the Brazilian public system: an overview of the last decade. Braz. J. Oral Sci. 2020;19(0) [Google Scholar]
- 23.Organization W.H. Impact of COVID-19 on people's livelihoods, their health and our food systems 2020. 2010. https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems Available from. [Google Scholar]
- 24.Bergquist S., Otten T., Sarich N. COVID-19 pandemic in the United States. Health Policy Technol. 2020;9(4):623–638. doi: 10.1016/j.hlpt.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monteiro de Oliveira M., Fuller T.L., Brasil P., Gabaglia C.R., Nielsen-Saines K. Controlling the COVID-19 pandemic in Brazil: a challenge of continental proportions. Nat Med. 2020;26(10):1505–1506. doi: 10.1038/s41591-020-1071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Izzetti R., Nisi M., Gabriele M., Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J. Dental Res. 2020;99(9):1030–1038. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 28.Xu H., Zhong L., Deng J., Peng J., Dan H., Zeng X. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li Y., Ren B., Peng X., Hu T. Saliva is a non-negligible factor in the spread of COVID-19. 2020;35(4):141-5. [DOI] [PMC free article] [PubMed]
- 30.Bastos T.F., Lima M.G., Malta D.C. Income inequalities in oral health and access to dental services in the Brazilian population: National Health Survey. Rev Brasi Epidemiol. 2013:22. doi: 10.1590/1980-549720190015.supl.2. LdPB M., NFdS S. [DOI] [PubMed] [Google Scholar]
- 31.Paim J., Travassos C., Almeida C., Bahia L., Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377(9779):1778–1797. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- 32.Pucca G.A., Jr., Gabriel M., de Araujo M.E., de Almeida F.C. Ten years of a national oral health policy in Brazil: innovation, boldness, and numerous challenges. J Dent Res. 2015;94(10):1333–1337. doi: 10.1177/0022034515599979. [DOI] [PubMed] [Google Scholar]
- 33.Azim A.A., Shabbir J., Khurshid Z., Zafar M.S., Ghabbani H.M., Dummer P.M.H. Clinical endodontic management during the COVID-19 pandemic: a literature review and clinical recommendations. Int Endod J. 2020;53(11):1461–1471. doi: 10.1111/iej.13406. [DOI] [PubMed] [Google Scholar]
- 34.Ather A., Patel B., Ruparel N.B., Diogenes A., Hargreaves KM. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46(5):584–595. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghai S. Teledentistry during COVID-19 pandemic. Diab Metab Syndr. 2020;14(5):933–935. doi: 10.1016/j.dsx.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ettinger R., Marchini L., Hartshorn J. Consideration in planning dental treatment of older adults. Dent Clin North Am. 2020 doi: 10.1016/j.cden.2020.12.001. [DOI] [PubMed] [Google Scholar]
- 37.Martins F.C., Pucca Junior G.A., Galante M.L. Teledentistry and the unified health system: an important tool for the resumption of primary health care in the context of the COVID-19 pandemic. Pesqu Bras Odontopediatria Clín Integr. 2020;20 FCdA C., BF M., EHGd L. [Google Scholar]
- 38.Gallagher J.E., Johnson I.G., Al-Yaseen W., Jones R., McGregor S. A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open. 2020;6:25. doi: 10.1038/s41405-020-00053-2. CS K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamid H., Khurshid Z., Adanir N., Zafar M.S., Zohaib S. COVID-19 Pandemic and role of human saliva as a testing biofluid in point-of-care technology. Eur J Dent. 2020;14(S 01):S123–S1s9. doi: 10.1055/s-0040-1713020. [DOI] [PMC free article] [PubMed] [Google Scholar]