Abstract
Objective: The aim of this study was to evaluate the safety and efficacy of fractional CO2 laser for treatment of vulvovaginal atrophy.
Materials and methods: In this clinical trial study, we evaluated the laser effect on vulvovaginal atrophy in 47 women aged 43-80 years. Each woman was treated with fractional CO2 laser, SmartXide2V2LR, DEKA, Monalisa Touch, vaginal 360o probe and cosmetic probe. The severity of vulvovaginal atrophy symptoms was evaluated before first session of laser and every 4 weeks after laser treatment until 12 weeks. Adverse effects including pain and itching were assessed at all visits. The statistical analysis was performed using SPSS version 23.
Results: The response to laser therapy for vaginal dryness was significantly (p <0.001) improved. Also, the response to laser therapy for each symptom include dyspareunia, vaginal discharge, itching and urge urinary incontinence was statistically significant (p <0.001) based on visual analogue scale (VAS).
Conclusion: It seems vaginal fractional CO2 laser can be applied as an effective and safe treatment method in genitourinary syndrome of menopause (GSM). It is necessary to conduct studies with long-term follow-up.
Key Words: Fractional CO2 Laser, Menopausal Women, Genitourinary Syndrome, Vulvovaginal Atrophy
Introduction
Vulvovaginal atrophy (VVA) or genitourinary syndrome of menopause (GSM) is one of the most frequent complaint in menopausal women due to estrogen deficiency. Vaginal atrophy can also occur as results of iatrogenic events include surgery and chemotherapy or radiotherapy for oncological disorders (1). VVA is often described as a 'silent symptom' of menopause. While an estimated 10–40% of postmenopausal women are affected, only 25% of symptomatic women seek medical attention. This condition, which can have a large impact on quality of life and sexual function, is often underdiagnosed and undertreated (2).
Symptoms of VVA include vaginal dryness, burning, pruritus, dyspareunia and vaginal discharge, bleeding, or spotting. Urinary tract symptoms are dysuria, urinary frequency, urethral discomfort and haematuria (3). Symptoms of vaginal atrophy are usually progressive and worsen as time and hypoestrogenism continues (4).
In a large cohort surveys in western populations, 45-63% of postmenopausal women experienced vulvovaginal symptoms, most commonly vaginal dryness (5). In a survey on 1578 women with vaginal discomfort, 83% had vaginal dryness (6). Similarly, the frequency of vaginal dryness in Iranian menopause women has reported 41.1% and it is one of the most three frequent symptoms (7). In the postmenopausal survivors of breast cancer, 70% are affected by vaginal atrophic symptoms (6).
Given the fact that average age of menopause is 51 years old and the population aging, a large population with GSM is seeking treatment. Several therapeutic options are available for treatment of VVA symptoms including hormonal and non-hormonal methods. Most recently the interest in using Laser therapy as a non-hormonal treatment for GSM has been highlighted (6).
From the past, lasers have been used as a safe and effective method to treat diseases in various parts of the body, including skin of the face, neck and chest, as well as the mouth (6). Fractional CO2 laser has shown safety and remodelling tissue properties in many body regions including ex vivo vaginal specimens without damage or side effects (6, 8). The first microscopic and ultrastructure evidence of mucosal biopsy of vaginal wall after CO2 laser therapy demonstrate the recovery of the whole structures supporting a full functionality in the epithelial and connective tissue compartments (9).
This study applied fractional CO2 laser for treatment of GSM. The aim of this study is to evaluate the safety and efficacy of this method for treatment of VVA.
Materials and methods
Study design: This clinical trial study was conducted at the department of Obstetrics and Gynecology, Pelvic Floor ward of Imam Khomeini Hospital affiliated to Tehran University of Medical Sciences, Iran, after approval of both Research Committee and Ethics Committee of Imam Khomeini Hospital (IR.TUMS.IKHC.REC.1397.5008). The study was registered in the Iranian Registry of Clinical Trials (Registration number: IRCT20171004036562N2). It included postmenopausal women referred to our pelvic floor clinic with VVA symptoms. All the patients signed an informed consent.
Study population: Out of 60 women participated in this study, 47 women completed the 12-week follow-up and included in the final analyses. Inclusion criteria were: one or more symptoms of VVA (e.g., vaginal discharge, itching, dyspareunia, dryness and urge urinary incontinence); no menstruation for ≥ 12 months; not using local or systemic estrogen therapy; wishing to be sexual active. Exclusion criterias were: use of hormone replacement therapy (systemic or local) in last 6 months before entry to the study; pelvic organ prolapse stage > 2 (according to pelvic organ prolapse quantification (POP-Q) system); active genital infections; acute or recurrent urinary tract infection; use of any vaginal lubricants, moisturizers or local preparations within 30 days before entry to the study; psychiatric disorders which could interfere with informed consent, any chronic disease that could interfere with study compliance; abnormal uterine bleeding with no exact diagnosis, malignancies of urogenital.
Study protocol: Each woman was treated with fractional CO2 laser, SmartXide2V2LR, DEKA, Monalisa Touch, made in Italy, vaginal 360o probe and cosmetic probe. Setting of the device for vaginal laser was dot power 40 watt, dwell time 1000 µs, dot spacing 1000 µm and the smart stack parameter 1, DEKA pulse. The setting for vestibule and fourchette was dot power 24 watt, dwell time 400 µs, dot spacing 900 µm and the smart stack parameter 1, DEKA pulse.
Treatment was performed at pelvic floor clinic and without any analgesia or anaesthesia. Patients were received laser treatment at three sessions every four weeks. Coital sexual activity was recommended to avoid for 7 days after each session.
All three laser therapy treatments were completely free of charge for patients. The patient could be excluded from the study at any stage of the study. All laser sessions were done by the same gynaecologist. The outcome of the study was to investigate the changes in the VVA symptoms.
Data collection: At the begging, demographic data of patients were collected. Vaginal exam were done at first and before each treatment with laser. After verified inclusion and exclusion criteria, all the women signed the consent forms. The severity of VVA symptoms was measured using a 10-cm visual analogue scale (VAS). The left extreme of the scale represented ‘absence of symptom’ with 0 and the right ‘symptom as bad as it could be’ with 10 (10). The severity of VVA symptoms was evaluated before first session of laser and every 4 weeks after laser treatment until 12 weeks. Adverse effects were assessed at all visits.
Statistical analysis: The statistical analysis was performed using SPSS version 23. A Kendall's Concordance (W) Coefficient test used to compare outcome of laser therapy sessions for each VVA symptom. P value < 0.05 was considered statistically significant.
Results
In this clinical trial study, 47 women aged 43-80 years with median age of 56 years were recruited. The mean±SD age of subjects was 57.2 ± 6.8 years. For Parity, 1 case (2.1%) was nulligravid, 40 (85.1%) women had parity 1 to 5, and 6 (12.8%) had parity of more than 5. The patient was menopause from 1 to 30 years ago with a median of 5 years and IQR equal to 7. The mean±SD menopause time was 7.3 ± 7.7 years. A total of 46 individuals had a history of delivery. 40 cases (86.9%) had normal vaginal delivery, 5 (10.8%) had caesarean section and 1 (2.2%) had both. Assessment of outcome of treatment with laser by separating the symptoms and the laser sessions (before laser treatment, the first, second, and third follow-up) is presented in Table 1.
Table 1.
Follow-up assessment the symptoms of vulvovaginal atrophy with Laser treatment
| Symptom 1 | Follow-up (week) | Mean | P value 2 , 3 |
|---|---|---|---|
| Dryness | 0 | 3.99 | < 0.001 |
| 1 | 3.01 | ||
| 2 | 1.99 | ||
| 3 | 1.01 | ||
| Dyspareunia | 0 | 4.00 | < 0.001 |
| 1 | 2.97 | ||
| 2 | 2.03 | ||
| 3 | 1.00 | ||
| Itching | 0 | 3.20 | < 0.001 |
| 1 | 2.73 | ||
| 2 | 2.27 | ||
| 3 | 1.80 | ||
| Vaginal Discharge |
0 | 3.22 | < 0.001 |
| 1 | 2.72 | ||
| 2 | 2.23 | ||
| 3 | 1.82 | ||
| Urge Urinary Incontinence |
0 | 3.51 | < 0.001 |
| 1 | 2.84 | ||
| 2 | 2.11 | ||
| 3 | 1.54 |
- change in symptoms was measured with Visual Analogue
- Scales were analysed with Kendall's w test
- Statistical significance was P value<0.05.
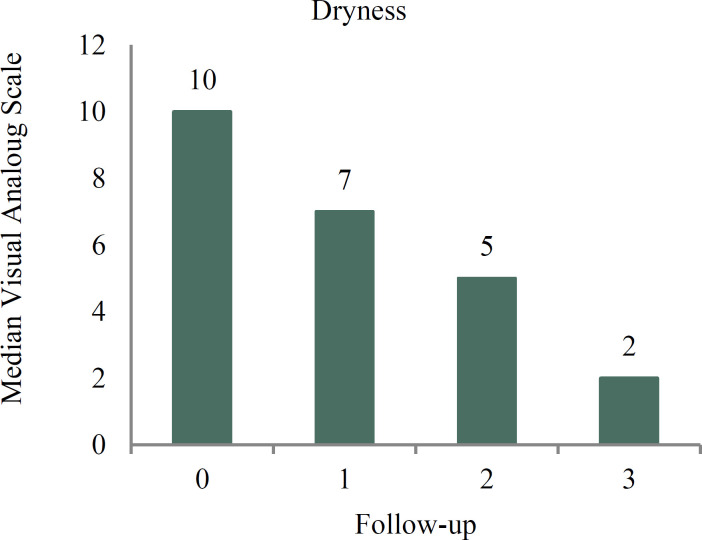
The response to laser therapy for vaginal dryness was significantly improved (p-value < 0.001). The process of recovery in treatment by increasing the number of laser sessions relative to each other based on the VAS is shown in figure 1.
Figure 1.
Trend of Median Visual Analogue Scale for Dryness at follow-up sessions.
Statistical analysis was performed using the Kendall's w test (P value < 0.001)
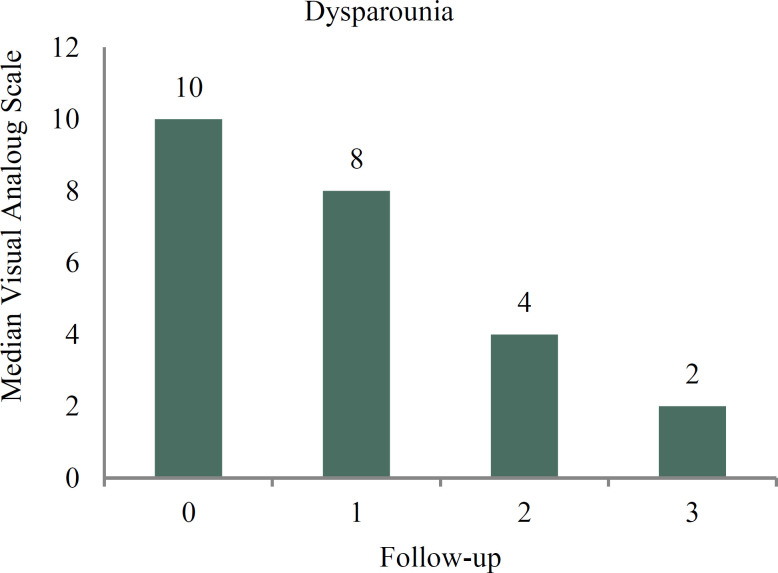
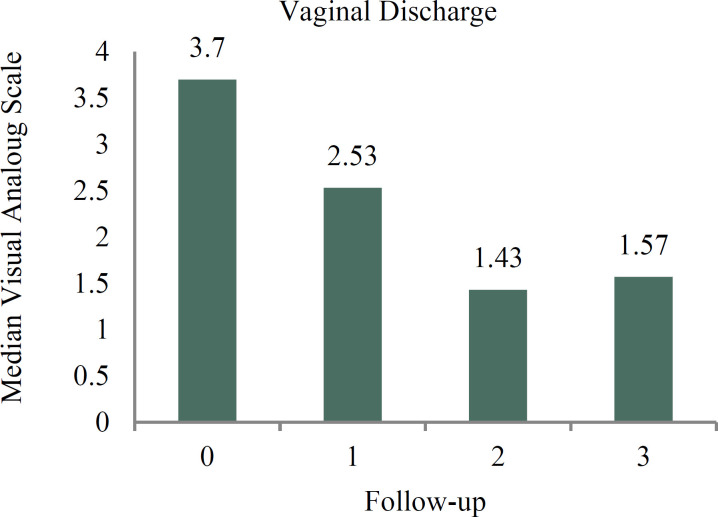
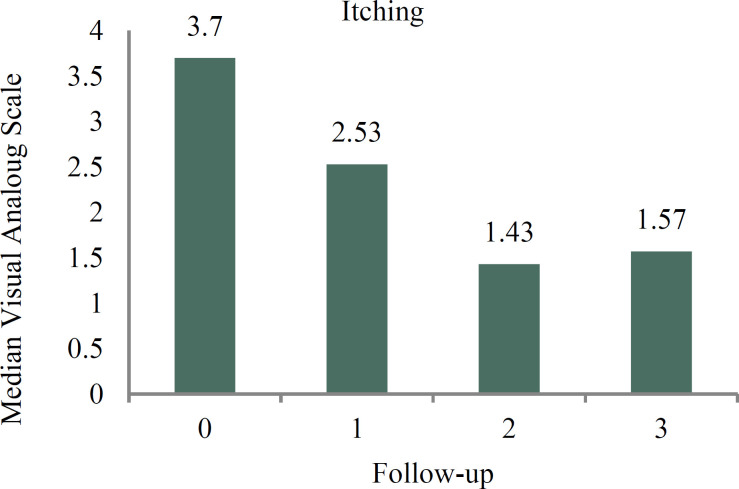
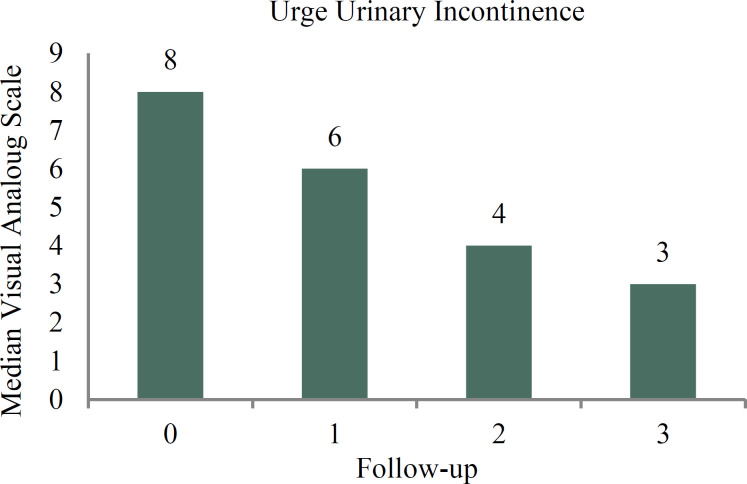
Also, the response to laser therapy for each symptom include dyspareunia, vaginal discharge, itching and urge urinary incontinence is statistically significant (p-value <0.001) based on VAS. For each of the above symptoms, the recovery process is shown by dividing the number of laser sessions in each other in figures 2, 3, 4 and 5.
Figure 2.
Trend of Median Visual Analogue Scale for Dyspareunia at follow-up sessions.
Statistical analysis was performed using the Kendall's w test (P value < 0.001).
Figure 3.
Trend of Mean Visual Analogue Scale for Vaginal Discharge at follow-up sessions
Statistical analysis was performed using the Kendall's w test (P value < 0.001).
Figure 4.
Trend of Mean Visual Analogue Scale for Itching at follow-up sessions.
Statistical analysis was performed using the Kendall's w test (P value < 0.001).
Figure 5.
Trend of Median Visual Analogue Scale for Urge Urinary Incontinence at follow-up sessions.
Statistical analysis was performed using the Kendall's w test (P value < 0.001).
In this study, there was no significant relationship between the response to laser therapy for dryness, dyspareunia, vaginal discharge, itching and urge urinary incontinence, with age (p-value = 0.500) and increased duration of menopausal (p-value = 0.100) and parity (p-value = 0.200). None of the patients reported a complication after laser therapy.
Discussion
During the past decade, CO2 laser has been widely used in medicine, especially in dermatology and plastic surgery (11). Indications considered by FDA for CO2 laser system which used in this study (DEKA SmartXide) are incision, excision, ablation, vaporization and coagulation of body soft tissues in medical specialties such as aesthetic, gynaecology and genitourinary surgery (12).
But the safety and effectiveness of these device have not been evaluated or confirmed by the FDA for "vaginal rejuvenation (13).
Within the recent years, a number of studied have been conducted on using the CO2 laser in treating the GSM as a non-hormonal technique. We concluded vaginal fractional CO2 laser in three treatment sessions for each symptom related to VVA including dryness, dyspareunia, itching, vaginal discharge and urge urinary incontinence in 3-month follow-up was significantly effective. Impact of laser on VVA symptoms was observed even on the first follow-up after the first treatment session. During the follow-up, no complication was seen.
In other studies, most of which have short-term follow-up, improvement of GSM symptoms with vaginal fractional CO2 laser were shown. For example, in the study by Baggish et al. (14), dryness, dyspareunia, urinary frequency and urgency as well as the symptoms related to lichen sclerosis were also improved.
In the study by Arroyo (15), as the VVA symptoms were examined by using Visual Health Index (VHI) system in 12th week after the 3rd treatment, 82% of patients had statistically significant improvement in VHI by laser therapy.
The study by Salvatore et al. (8) showed that after the laser treatment, a significant improvement occurred in each VVA symptoms leading to the considerable improvement of quality of life both in physical and mental scores. In another study, Salvatore et al. (10) reconfirmed the previous findings. No complication was observed in these studies.
Pieralli et al. (16) study was conducted on the survivors of breast cancer, significant improvement occurred in dyspareunia after three laser treatment sessions and 52% of patients were satisfied of this treatment after one year from the end of treatment.
In the study by Siliquini et al (17), significant improvement was seen in VAS score up to 15 months after the treatment and such long-term improvement was stable. Study of Perino et al. (11) has shown a considerable improvement in VVA symptoms among the patients who have attended three laser treatment sessions. Significant improvement of quality of life among these patients occurred after the treatment.
Study of Sokol et al. (18) also indicated the average improvement in VAS score in 3-month follow-up. Lang et al. (19) study has also approved that vaginal dryness after laser treatment was improved significantly and as a result, intercourse frequency among the patients is increased. Report of Gorbunova et al. has come to this conclusion that fractional CO2 laser treatment is suitable for improving the symptoms of sexual dysfunction, vaginal laxity, minor and major labia laxity, stress urinary incontinence, pelvic organs prolapse, and GSM and lichen sclerosis. In the other study, scores of quality of life in physical and mental areas and also quality of sexual life were significantly enhances compared to the baseline (20).
In the study by Behnia-Willison et al. (21), significant improvement was achieved in each GSM symptoms in long-term follow-up (12-24 months) among the patients after treatment with fractional CO2 laser.
Results of this study along with other studies’ conducted so far on GSM treatment by vaginal fractional CO2 laser are promising. The efficacy of fractional CO2 laser as a non-steroidal, non-estrogenic therapeutic method regarding the numerous cases of contraindication or interference with hormone therapy is important. By using this method, it is possible to avoid the disadvantages of these drugs, and suggest effective and useful treatment in patients who cannot use other methods. This advantage is particularly more specific and more striking among the patients with breast cancer who face limitations in hormonal therapy.
Lack of report on special side effects in numerous studies is an important point on this issue. In most patients, no discomfort was reported by them on performing such procedure or they have reported slight discomforts. Study of Salvatore et al. (22) mentioned the least discomfort on the first laser session resulting from embedding and movement of laser probe. Study of Arroyo et al. (15) has also found that itching is seen among 20% of patients.
The mechanism of action of vaginal fractional CO2 laser is fast and easy. Treatment sessions are not complicated which can be performed in clinic. In accordance with the report by Gorbunovaet al, the effects are also appeared in tissue and clinical status of patients within one week and one can feel improvement (20).
Limitation of present study includes the small size of sample, lack of control group and short-term follow-up. If the patients keep aware of the results of recent studies on improvement of GSM by vaginal fractional CO2 laser in short term, tendency to wider treatment is generated by this technique. In this case, studies with large size of sample can be conducted. Long-term follow-up will be made on patients of this study. Conducting the randomized clinical trial is also necessary in this regard.
Conclusion
With regards to the findings of this study, concluded that vaginal fractional CO2 laser can be applied as an effective and safe treatment method in GSM. It is necessary to conduct studies with long-term follow-up.
Acknowledgments
We would like to acknowledge the supports provided by the staff of vali asr hospital for their kind help.
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Nappi RE, Kokot-Kierepa M. Women's voices in the menopause: results from an international survey on vaginal atrophy. Maturitas. 2010;67:233–8. doi: 10.1016/j.maturitas.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Krapf JM, Belkin ZR, Goldstein AT. Advances in the treatment of vulvovaginal atrophy. Expert Review of Obstetrics & Gynecology. 2013;8:457–65. [Google Scholar]
- 3.Portman DJ1, Gass ML Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and the North American Menopause Society. Maturitas. 2014;21:1063–8. doi: 10.1097/GME.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 4.Weber MA, Limpens J, Roovers JP. Assessment of vaginal atrophy: a review. Int Urogynecol J. 2015;26:15–28. doi: 10.1007/s00192-014-2464-0. [DOI] [PubMed] [Google Scholar]
- 5.Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The Recent Review of the Genitourinary Syndrome of Menopause. J Menopausal Med. 2015;21:65–71. doi: 10.6118/jmm.2015.21.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hutchinson-Colas J, Segal S. Genitourinary syndrome of menopause and the use of laser therapy. Maturitas. 2015;82:342–5. doi: 10.1016/j.maturitas.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Asadi M, Jouyandeh Z, Nayebzadeh F. Prevalence of menopause symptoms among Iranian women. Journal of Family and Reproductive Health. 2012;6:1–3. [Google Scholar]
- 8.Salvatore S, Nappi R, Zerbinati N, Calligaro A, Ferrero S, Origoni M, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17:363–9. doi: 10.3109/13697137.2014.899347. [DOI] [PubMed] [Google Scholar]
- 9.Zerbinati N, Serati M, Origoni M, Candiani M, Iannitti T, Salvatore S, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30:429–36. doi: 10.1007/s10103-014-1677-2. [DOI] [PubMed] [Google Scholar]
- 10.Salvatore S, Roberti Maggiore UL, Athanasiou S, Origoni M, Candiani M, Calligaro A, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845–9. doi: 10.1097/GME.0000000000000401. [DOI] [PubMed] [Google Scholar]
- 11.Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80:296–301. doi: 10.1016/j.maturitas.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health and Human Services, Public Health Service, Food and Drug Administration. Electronic Engineering SpA Mr Paolo Peruzzi. 2014 [Google Scholar]
- 13.Ahluwalia J, Avram MM, Ortiz AE. Lasers and energy‐based devices marketed for vaginal rejuvenation: A cross‐sectional analysis of the MAUDE database. Lasers Surg Med. 2019;51:671–7. doi: 10.1002/lsm.23084. [DOI] [PubMed] [Google Scholar]
- 14.Baggish MS. Fractional CO2 laser treatment for vaginal atrophy and vulvar lichen sclerosus. Journal of Gynecologic Surgery. 2016;32:309–17. [Google Scholar]
- 15.Arroyo C. Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Womens Health. 2017;9:591–5. doi: 10.2147/IJWH.S136857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841–6. doi: 10.1007/s00404-016-4118-6. [DOI] [PubMed] [Google Scholar]
- 17.Siliquini GP, Tuninetti V, Bounous VE, Bert F, Biglia N. Fractional CO2 laser therapy: a new challenge for vulvovaginal atrophy in postmenopausal women. Climacteric. 2017;20:379–84. doi: 10.1080/13697137.2017.1319815. [DOI] [PubMed] [Google Scholar]
- 18.Sokol ER, Karram MM. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016;23:1102–7. doi: 10.1097/GME.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 19.Lang P, Dell JR, Rosen L, Weiss P, Karram M. Fractional CO2 laser of the vagina for genitourinary syndrome of menopause: Is the out-of-pocket cost worth the outcome of treatment? Lasers Surg Med. 2017;49:882–5. doi: 10.1002/lsm.22713. [DOI] [PubMed] [Google Scholar]
- 20.Gorbunova E, Apolikhin I, Sukhikh G. Monaco: AMWC; 2017. Laser in Gynecology: The First Russian Experience. Federal State Budget Institution Study presented at advanced course in genital rejuvenation & cosmetic gynecology - pre-congress courses - [Google Scholar]
- 21.Behnia-Willison F, Sarraf S, Miller J, Mohamadi B, Care AS, Lam A, et al. Safety and long-term efficacy of fractional CO2 laser treatment in women suffering from genitourinary syndrome of menopause. Eur J Obstet Gynecol Reprod Biol. 2017;213:39–44. doi: 10.1016/j.ejogrb.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 22.Salvatore S, Nappi R, Parma M, Chionna R, Lagona F, Zerbinati N, et al. Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climacteric. 2015;18:219–25. doi: 10.3109/13697137.2014.975197. [DOI] [PubMed] [Google Scholar]