Abstract
The aryl hydrocarbon receptor (AhR) plays a crucial role in environmental responses and xenobiotic metabolism, as it controls the transcription profiles of several genes in a ligand-specific and cell-type-specific manner. Various barrier tissues, including skin, display the expression of AhR. Recent studies revealed multiple roles of AhR in skin physiology and disease, including melanogenesis, inflammation and cancer. Tryptophan metabolites are distinguished among the groups of natural and synthetic AhR ligands, and these include kynurenine, kynurenic acid and 6-formylindolo[3,2-b]carbazole (FICZ). Tryptophan derivatives can affect and regulate a variety of signaling pathways. Thus, the interest in how these substances influence physiological and pathological processes in the skin is expanding rapidly. The widespread presence of these substances and potential continuous exposure of the skin to their biological effects indicate the important role of AhR and its ligands in the prevention, pathogenesis and progression of skin diseases. In this review, we summarize the current knowledge of AhR in skin physiology. Moreover, we discuss the role of AhR in skin pathological processes, including inflammatory skin diseases, pigmentation disorders and cancer. Finally, the impact of FICZ, kynurenic acid, and kynurenine on physiological and pathological processes in the skin is considered. However, the mechanisms of how AhR regulates skin function require further investigation.
Keywords: aryl hydrocarbon receptor, tryptophan, kynurenine, FICZ, skin, kynurenic acid, atopic dermatitis, psoriasis, melanoma
1. Introduction
The aryl hydrocarbon receptor (AhR) is expressed in various tissues characterized by a rapid growth rate, including skin [1]. Gene expression analysis revealed that AhR activation enhances or suppresses the expression of several genes, thus influencing the gene expression profile [2]. Previous studies revealed the crucial role of AhR in several physiological and pathological processes in the skin. Among the groups of natural and synthetic AhR ligands is the group of tryptophan derivatives [1,3]. Some of them, including kynurenine, kynurenic acid, and 6-formylindolo[3,2-b]carbazole (FICZ), have been previously recognized as ligands of this receptor. However, recently discovered biological properties of these substances, their widespread presence, and potential continuous exposure may suggest the important role of tryptophan-derived AhR ligands in many physiological and pathological processes in the skin [4]. Unfortunately, the role of AhR itself and the biological effect of the tryptophan-derived ligands in the prevention, pathogenesis, and progression of skin diseases are not fully understood to date.
2. Aryl Hydrocarbon Receptor (AhR)
AhR is a transcription factor from the evolutionarily old family of a basic helix-loop-helix/Per-ARNT-Sim (bHLH-PAS) transcription regulators, acting in a DNA sequence-specific manner. The bHLH motif contains two domains that are responsible for DNA sequence binding and protein dimerization [1]. Several low-molecular-weight chemical compounds activate the cytosolic AhR after entering cells via diffusion [3,5]. Air pollution compounds [3], endogenous amino acid derivatives [6,7,8], some food components (e.g., indoles, polyphenols, glucosinolates) [9,10,11], and some yeast and bacterial metabolites [12] are considered AhR ligands. AhR has only one binding pocket, whose amino acid composition determines ligand binding strength [1]; however, AhR may also be activated by a number of stress factors and some substances that might not fit into the binding pocket (e.g., hypoxia and oxidized low-density lipoproteins) [13].
The type of AhR ligand determines the level of activation and the spectrum of genes transcribed [14,15,16]. An increased AHR expression is observed in the placenta, liver, lungs, intestines, and skin, which are barrier tissues or play an important role in metabolism. The lowest AHR expression is reported in the brain, kidneys, and skeletal muscles [2]. Recent studies revealed additional functions of AhR in the body, including control of liver and vascular development, intestinal immunity, hematopoiesis, and perinatal growth [17,18,19,20,21,22]. Moreover, AhR signaling may be associated with stem cell proliferation and carcinogenesis [2].
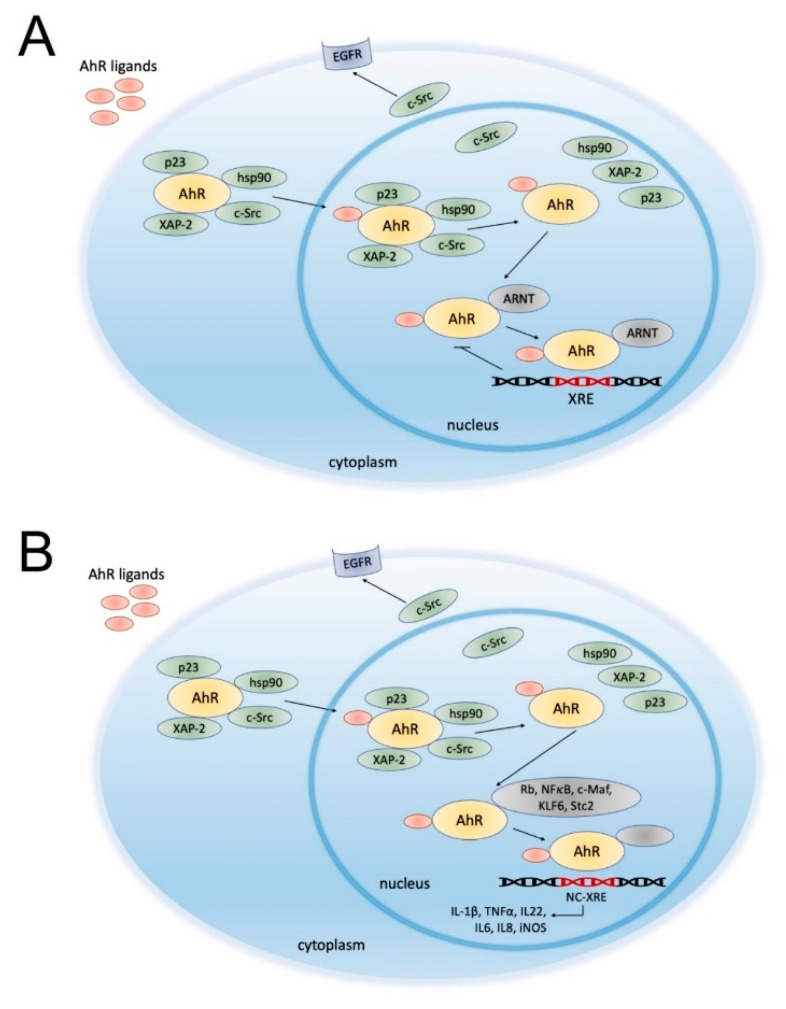
After ligand binding, AhR dissociates from its chaperones (e.g., proto-oncogene tyrosine-protein kinase c-Src, heat shock protein 90 (HSP90), p23, and the hepatitis B virus X-associated protein 2 (XAP2)) and undergoes conformational changes, resulting in the exposition of the nuclear translocation signal and induction of AhR transport into the nucleus (Figure 1A) [23].
Figure 1.
Schematic overview of aryl hydrocarbon receptor (AhR) signaling pathways: canonical (A) and noncanonical (B). In physiological conditions, AhR is localized in the cytosol and complexed with specific proteins, such as the hepatitis B virus X-associated protein 2 (XAP-2), heat shock protein 90 (HSP90), c-Src and p23. Upon ligand binding, AhR changes its conformation and is translocated to the nucleus, where it dimerizes with AhR nuclear transporter (ARNT) (A) or other partners, such as transcription factors (e.g., Kruppel-like factor 6 (KLF6)). (B). Dissociated c-Src interacts with the epidermal growth factor receptor (EGFR). To date, several different types of crosstalk between AhR and other proteins have been described. For instance, AhR interaction with the hyperphosphorylated form of the retinoblastoma protein (Rb) results in growth arrest at the G1/S phase of the cell cycle [24]. AhR signaling may also promote nuclear factor kappa-light-chain-enhancer of activated B cell (NF-κB) activation via RelA and RelB interaction [25,26,27]. Moreover, AhR signaling is associated with the activity and function of the estrogen receptor [28]. The AhR/ARNT complex binds to the xenobiotic-responsive element (XRE) and induces the transcription of AhR-responsive genes (e.g., CYP1A1). On the other hand, AhR ligation promotes the transcription of its inhibitor—the AhR repressor (AhRR). AhRR forms a heterodimer with ARNT and competes with AhR/ARNT to bind to the XRE sequence, inhibiting AhR-induced transcription. However, previous studies suggest that AhR repression may not occur solely by inhibition of the DNA binding site and AhR/ARNT complex formation [29,30]. Moreover, Wilson et al. indicated that AhR–KLF6 complex formation may be involved in cell cycle regulation [31]. AhR and KLF6 proteins form a heterodimer that recognizes novel nonconsensus XRE (NC-XRE), highlighting a distinction from the XRE-dependent AhR signaling mechanism. This noncanonical signaling pathway may influence cell cycle regulation, as it controls the expression of the cyclin-dependent kinase inhibitor p21Waf1/Cip1 [31]. Jackson et al. revealed that 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)-mediated p21Waf1/Cip1 activation is associated with disrupted liver regeneration [32]. Therefore, while the KLF6-mediated noncanonical AhR signaling pathway might suppress tumor growth by regulating p21Waf1/Cip1 expression, carcinogenic AhR agonists might activate the canonical AhR signaling pathway and promote tumorigenesis. As outlined above, AhR might influence cell survival by various mechanisms. However, AhR might also interact with different genes that have a similar binding pattern, such as STC2 gene, encoding a glycoprotein responsible for the regulation of endoplasmic reticulum stress [33]. Vogel et al. revealed that AhR forms a complex with NF-κB subunit RelB. The NF-κB-RelB-binding site is targeted by AhR and promotes the expression of chemokine genes, such as BAFF, BLC, and IRF3 [34]. Furthermore, Ge et al. identified Rb as an AhR dimerization partner, suggesting its role in cell cycle arrest [35]. Recently, Huang et al. described a novel NC-XRE in the promoter of the gene encoding plasminogen activator inhibitor-1 (PAI-1) that might be targeted by a distinct protein complex [36]. However, further investigations are needed to determine the contribution of canonical and noncanonical AhR signaling pathways to cell homeostasis. The scheme is based on previously reported data [2,3,14].
Chaperone c-Src disconnected from AhR initiates internalization and nuclear translocation of the epidermal growth factor receptor (EGFR) and activation of mitogen-activated protein kinases (MAPK) signaling cascades, which are involved in cell proliferation, migration, and angiogenesis [37]. In the nucleus, AhR dimerizes with the AhR nuclear transporter (ARNT), another member of the bHLH-PAS family [38]. Genes possessing AhR binding sites (xenobiotic response elements, XRE) in their promoters are transcribed when bound to an AhR/ARNT dimer. After the interaction with XRE, AhR is transported back into the cytosol and degraded. The crosstalk between AhR and other signaling pathways may modify the effects of AhR and its ligands’ interaction (Figure 1B) [1].
The wide spectrum of genes interacting with AhR within XRE indicates that AhR signaling is specific to the type of cell, tissue, or prevailing conditions (Table 1) [15,16].
Table 1.
The effect of AhR on selected cellular processes.
| Alterations in Cellular Functions | Biological Effect | Type of Cell/ Mouse Model |
Reference | |
|---|---|---|---|---|
| Cell metabolism |
|
AHR-deficient mice | [39] | |
| Cell proliferation | Inhibition |
|
5L cells | [40] |
| HUVEC | [41] | |||
|
LNCaP cells | [42] | ||
| BP8 5L HEK293 |
[43] | |||
|
Hepa-1c1c7 MCF-7 |
[44] | ||
|
HepG2 | [45] | ||
| Stimulation |
|
MCF-7 | [45] | |
|
A549 | [46] | ||
|
HepG2 | [47] | ||
| Cell migration * |
|
T-FGM-AHR−/− myofibroblasts | [48] | |
|
MCF-7 HepG2 |
[49] | ||
|
MDA-MB-231 T47D |
[50] | ||
|
MDA-MB-231 | [51] | ||
|
MCF-7 | [52] | ||
|
HSC-3 CAL27 |
[53] | ||
| Regulation of Signaling Pathways and Nuclear Receptors | ||||
| NF-κB signaling pathway |
|
U937 macrophages | [54] | |
|
B6 mice | [25] | ||
| Nuclear factor-erythroid 2-related factor-2 (Nrf2) signaling pathway |
|
NHEK | [55,56] | |
| Calcium-dependent signaling pathways |
|
Hepa-1 | [57] | |
|
3T3-L1 | [58,59] | ||
| Hypoxia-induced factor (HIF) |
|
HepG2 HaCaT |
[60] | |
|
HEK Krt14-Cre+ mice |
[61] | ||
|
Zebrafish caudal fin regeneration model | [62] | ||
| Estrogen and retinoid receptors |
|
BG1 | [63] | |
|
MCF-7 | Reviewed in [28,64] | ||
* Although AhR activity may influence cell migration and invasion, the ability of the AhR to drive tumor growth is mostly tissue specific. AhR—aryl hydrocarbon receptor; CDK—cyclin-dependent kinase; Rb—retinoblastoma protein; E2F—a group of transcription factors, which are downstream effectors of Rb; SOS1—son of sevenless 1; TCDD—2,3,7,8-tetrachlorodibenzo-p-dioxin; IL17A—interleukin 17A; CCL20—chemokine (C-C motif) ligand 20; NQO1—NAD(P)H quinone dehydrogenase 1; PAH—polycyclic aromatic hydrocarbons; cAMP—3′5′-cyclic adenosine monophosphate; PKC—protein kinase C; PKA—protein kinase A; ARNT—aryl hydrocarbon receptor nuclear translocator; LPR6—LDL receptor-related protein 6; ERα—estrogen receptor α; NF-κB—nuclear factor kappa-light-chain-enhancer of activated B cells; HIF—hypoxia-induced factor; Nrf2—nuclear factor-erythroid 2-related factor-2.
The transcription of genes encoding xenobiotic-metabolizing enzymes (CYP1A1, CYP1A2, and CYP1B1), genes responsible for cell differentiation and regulation of the cell cycle, and genes coordinating the immune response is dependent, even partially, on AhR activity [65,66]. Moreover, induction of CYP1A1 expression allows for the degradation of some AhR ligands, including FICZ. During this process, a large amount of reactive oxygen species (ROS) is produced. ROS activity affects cell metabolism, leading to DNA damage and expression of various cytokines [65,67].
Interestingly, microarray studies indicated a ligand-specific differences in AhR-induced gene expression profile [68]. To date, many cellular metabolites and xenobiotic compounds were defined as AhR agonists [2,67].
The mechanism of downregulation of AhR signaling is still unclear. It is based on the activity of the negative AhR regulator, the AhR repressor (AhRR). Upon AhR activation, AHRR expression is induced. The AhRR forms a heterodimer with ARNT and competes with the AhR/ARNT complex for the XRE binding site. This feedback loop consequently inhibits AhR transcriptional activity [69]. On the other hand, Evans et al. reported that AhRR-mediated AhR inhibition is not the cause of ARNT sequestration [29]. A distinct mechanism of AhRR action was proposed, indicating that AhR inhibition occurs through protein–protein interaction [29]. Therefore, AhR repression does not occur solely by inhibition of the DNA binding site and AhR/ARNT complex formation.
3. The Role of AhR in Skin Physiology
Skin, the largest organ of the human body, is a protective barrier against harmful environmental factors. The maintenance of body fluid balance and a constant temperature depends on the proper condition and function of the skin. A battery of receptors and nerve endings present in the skin enable a reaction to various stimuli and communication with the surrounding environment [70].
The skin has a layered structure, consisting of (from the outside): epidermis, formed mainly by keratinocytes; dermis, created mainly by fibroblasts; and subcutaneous tissue. Among skin cells, there are also Langerhans cells (LCs), melanocytes, sebocytes, and immune cells (mast cells, CD8+ T cells, and dendritic cells (DCs)) [70]. AhR is observed in all skin cells, but particular cell types differ in its expression level [2].
The skin is exposed to biological, physical, mechanical, and chemical factors. Interestingly, AhR signaling appears to play an important role in maintaining skin homeostasis as it participates in many processes such as metabolism of environmental toxins, maintaining redox balance in the cell, response to ultraviolet (UV) radiation, melanogenesis, regulation of immunological processes, and functioning of the epidermal barrier [2].
AhR/ARNT signaling initiates the activation of the OVO-like 1 (OVOL1) transcription factor, which subsequently enhances the expression of filaggrin (FLG) and loricrin (LOR), proteins specific to fully differentiated keratinocytes and corneocytes [71]. Thus, the activation of this pathway contributes to accelerating the final differentiation of the epidermis and formation of epidermal barrier.
The role of the skin in immune processes is based on protecting the host from pathogens while suppressing excessive inflammation. High levels of AhR in the skin cells may be associated with an AhR-mediated immune response. AhR signaling is essential for the maturation of LCs and its capacity to present antigens, as demonstrated in studies on AHR-null mice [72]. Interestingly, inflammatory skin lesions were observed in mice with permanently active AhR in keratinocytes [73]. High AHR expression was previously reported in Th17 cells. Moreover, IL-22 secretion by these lymphocytes depends on AhR activation [74]. In summary, AhR deficiency or alterations within AhR activity may disrupt the immune response or impair the development and function of the epidermal barrier [75].
4. AhR and Skin Pathological Processes
In addition to the prominent and well-documented role of AhR in skin homeostasis, this receptor is also involved in many pathological processes within the skin through alterations in AhR-controlled signaling pathways. Moreover, it may be associated with exposure to toxic AhR ligands present in air pollution. Disorders whose pathomechanism is associated with AhR function in the skin include, among others, chloracne, hyperpigmentation, and vitiligo, as well as inflammatory diseases such as psoriasis or atopic dermatitis [66].
Skin diseases may be related to air pollution. The most common air pollutants with high affinity for AhR include the following: 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD), benzo[a]pyrene (BaP), polychlorinated dibenzofurans (PCDFs), polychlorinated dibenzo-p-dioxins (PCDDs), and polychlorinated biphenyls (PCBs) [2,66]. Although exposure to high doses of toxic AhR ligands is relatively rare and accidental, even low doses of these compounds have previously caused skin irritation or worsened the symptoms of diseases [76]. Chloracne and hyperpigmentation are the most frequently mentioned among skin diseases in people exposed to high doses of air pollution components [77,78,79,80]. AhR may also be activated due to chronic exposure to PM2.5, which is made up of dioxin derivatives [76].
Activation of the AhR signaling pathway in epidermal keratinocytes is sufficient to initiate inflammatory skin lesions [73]. Tauchi et al. suggest that the activation of the AhR signaling pathway and the expression of AhR target genes are the main mechanisms of inflammatory skin disorders induced by PAH [73]. Thus, blocking of AhR signals that induce transcription of selected genes may be a potential therapeutic target in the treatment of some skin diseases.
A Double Agent: The Role of AhR in Oxidative Stress
Oxygen molecules do not always undergo full four-electron reduction, which leads to the formation of unstable ROS. In physiological conditions, ROS are formed during biochemical reactions and are characterized by high reactivity. Moreover, ROS are produced as a result of exposure to environmental stress, such as UV radiation or ionizing radiation. Xenobiotics and air pollutants may also increase ROS formation. The balance between the rate of ROS formation and the activity of antioxidants produced by the cells determines the biological response to ROS. The consequences of increased cell exposure to ROS include the following: a decrease in adenosine triphosphate (ATP) levels, lipid peroxidation, cell membrane depolarization, morphological changes in cell surfaces, and DNA damage. However, the biological activity of ROS is not limited to adverse effects, as at a physiological concentration, they play an important role in cell homeostasis by regulation of proliferation, apoptosis, and migration [81].
The interaction of TCDD with AhR enhances the expression of cytochrome P450 family members such as CYP1A1, CYP1A2, and CYP1B1. Due to the stable structure of TCDD, these enzymes are not able to metabolize TCDD dioxin effectively. Furthermore, excessive CYP1A1 activity, resulting from the constant interaction between TCDD and AhR, induces the generation of ROS. Increasing oxidative stress may cause oxidation of fatty acids in skin cell membranes, structural proteins (mainly collagen), and enzymatic proteins [14]. CYP1A1-induced excessive production of ROS may indirectly affect cell metabolism due to direct activation of multiple signaling pathways. Moreover, an interaction of ROS with various molecules such as NF-κB, c-Jun oncoprotein, or Rb may affect the cell cycle [82,83].
Activation of the AhR/CYP1A1 signaling pathway also contributes to increased production of inflammatory mediators, including interleukin 1 (IL-1), IL-6, and IL-8. Furthermore, BaP exposure is associated with an increased expression of CYP1A1, and IL-8, ROS production. This phenomenon may underlie the inflammatory skin diseases in tobacco smokers, as BaP is a component of tobacco smoke [84,85].
On the other hand, AhR activity induces the expression of nuclear factor erythroid 2-related factor 2 (Nrf2), a transcription factor with antioxidant properties. Upon AhR-mediated activation, Nrf2 increases the expression of antioxidant enzymes such as glutathione S-transferases and NAD(P)H quinone dehydrogenase 1 (NQO1) [56]. Some AhR ligands are more active in promoting the antioxidant response (Table 2).
Table 2.
The AhR signaling pathway mediates antioxidative signals in response to different substances, e.g., herbal medicines and flavonoids.
| Substance | Outcome | Cell Type | References |
|---|---|---|---|
| Ketoconazole |
|
NHEK | [55] |
| Bidens pilosa |
|
Human dermal endothelial cells | [86] |
| Epigallocatechin gallate |
|
Primary vascular endothelial cells | [87] |
| Quercitrin |
|
JB6 cells | [88] |
| Quercetin, kaempferol |
|
Caco2 | [89] |
| Cinnamaldehyde |
|
HaCaT | [11] |
| Cynaropicrin (Cynara scolymus) |
|
NHEK | [10] |
| Opuntia ficus indica |
|
HNEK | [9] |
| Hesperetin |
|
MCF-7 | [90] |
| Quercetin, resveratrol, curcumin |
|
HaCaT | [91] |
AhR—aryl hydrocarbon receptor; Nrf2—nuclear factor-erythroid 2-related factor-2; NQO1—NAD(P)H quinone dehydrogenase 1; TNF-α—tumor necrosis factor alpha; BaP—benzo[a]pyrene; ROS—reactive oxygen species; AhRR—aryl hydrocarbon receptor repressor; FLG—filaggrin; FICZ—6-formylindolo[3,2-b]carbazole.
Modulation of the activity of various proteins, including downstream AhR targets, such as CYP1A1 or Nrf2 via the AhR/ARNT pathway, determines the redox balance of the cells [56].
In contrast to TCDD, coal tar induces Nrf2 nuclear translocation and follows the induction of NQO1 expression, thereby triggering an antioxidant signal pathway that neutralizes the negative effect of ROS in keratinocytes [92]. Activation of this pathway may be a clue suggesting the lack of toxicity and carcinogenicity of coal tar used in the treatment of psoriasis [93]. On the other hand, chronic exposure to TCDD results in growing immunotoxicity, thereby increasing the risk of cancer [65]. Although the mechanism of coal tar activity is not fully understood, a comprehensive study in a large group of patients with psoriasis and eczema has not indicated a relationship between the use of coal tar and an increased risk of skin cancers [93]. In summary, both ROS production and antioxidative response resulting from AhR activation depend on the AhR ligand type.
5. Role of AhR in Inflammatory Skin Diseases
5.1. Atopic Dermatitis
Atopic dermatitis (AD) is a heterogeneous skin disease accompanied by eczema, Th2-deviated inflammation, and chronic itching. Due to the reduced expression of FLG and other proteins involved in the differentiation and maturation of skin cells, the skin barrier integrity in AD is impaired [94]. Moreover, skin barrier dysfunction causes an increased colonization of microorganisms, such as Staphylococcus aureus, which further promotes skin inflammation [95].
Previous studies suggested that Th2-mediated immune response is associated with reduced production of the tryptophan-derived AhR ligand indole-3-aldehyde (IAId) by the skin microbiome. Yu et al. reported that IAId-induced AhR activation attenuated AD-like dermatitis [96]. Decreased inflammation was associated with the inhibition of thymic stromal lymphopoietin (TSLP) production in keratinocytes. TSLP is an inflammatory cytokine overexpressed in keratinocytes of AD patients. Upon IAId stimulation, AhR may interact with the TSLP promoter region and promote immune homeostasis in the skin of healthy subjects. TSLP expression is also observed in MC903-induced AD-like dermatitis mouse model, as it plays a crucial role in Th2-mediated inflammation. Although the inhibitory effect of IAId on TSLP expression reduces the inflammatory response in MC903-induced AD-like dermatitis in mice, this effect has not been observed in different models of AD-like skin inflammation, such as imiquimod (IMQ)-induced psoriatic dermatitis and oxazolone (OXA)-induced contact hypersensitivity. Due to aberrant skin microbiota, a reduced level of IAId may indicate alterations in TSLP expression, leading to skin inflammation in patients diagnosed with AD. Therefore, a deficiency of physiological AhR ligands in the Th2-deviated environment may underlie the skin lesions in AD [96].
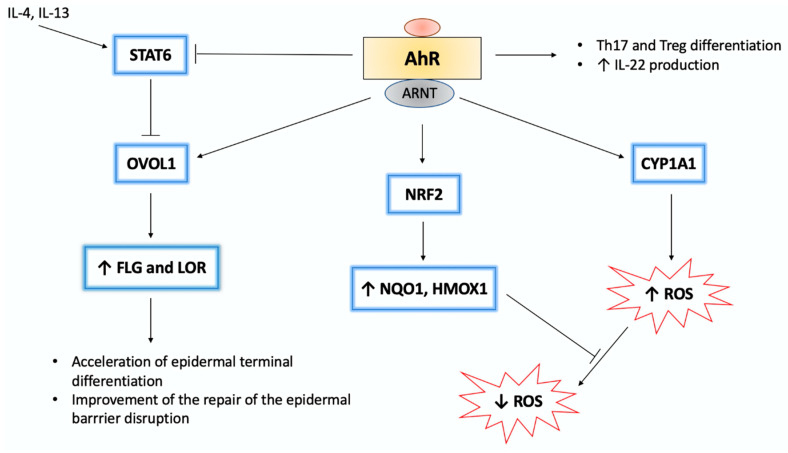
Expression of FLG in keratinocytes is dependent on AhR activity as AhR ligation leads to OVOL1 nuclear translocation and subsequent FLG transcription [62]. The AhR/ARNT/FLG signaling pathway may be activated by both rapidly metabolized AhR ligands, such as IAId or FICZ, and by dioxins (Figure 2) [97,98].
Figure 2.
Molecular interactions within the AhR signaling pathway [99]. In the nucleus, AhR/ARNT complex binds to the XRE sequence, thus initiating the transcription of AhR-responsive genes, such as CYP1A1. CYP1A1 activity is associated with ROS production. Furthermore, AhR ligands are degraded by CYP1A1. Regarding chemically stable ligands, such as dioxins, sustained CYP1A1 activation leads to enhanced ROS generation. On the other hand, several AhR ligands activate nuclear factor-erythroid 2-related factor-2 (Nrf2), a transcription factor, which induces expression of antioxidative enzymes (e.g., heme oxygenase 1 (HMOX1) and NQO1). Moreover, AhR signaling is associated with the differentiation of immune cells, such as Th17 and Treg. Regarding inflammatory skin diseases, such as psoriasis and atopic dermatitis, AhR-mediated IL-22 production plays a crucial role in alleviating skin lesions. AhR/ARNT interaction upregulates filaggrin (FLG) and loricrin (LOR) expression via activation of the OVO-like 1 (OVOL1) transcription factor. Both FLG and LOR play a key role in epidermal differentiation. However, IL-4/IL-13-mediated signal transducer and activator of transcription 6 (STAT6) activation inhibits the OVOL1/FLG/LOR pathway. AhR stimulation may inhibit STAT6 and upregulate FLG and LOR expression. The pathogenic implication of AhR signaling in inflammatory skin diseases is not fully understood as the activation of the AhR/OVOL1/FLG/LOR pathway may become harmful. As the use of rapid metabolizing AhR ligands, such as FICZ, may alleviate skin inflammation, sustainable activation of this pathway by dioxins exacerbates epidermal barrier dysfunction. The scheme is based on previously reported data [9,10,84,99]. ↑-activation, upregulation, ↓-downregulation, T-arrow-inhibition.
Therefore, dioxin-mediated or persistent AhR activation may promote skin barrier dysfunction and exacerbate the course of AD [97]. However, topically applied FICZ reduced inflammation in skin lesions in a murine dermatitis model by AhR activation [98]. Moreover, a decrease in Il 22 expression and an increase in FLG transcription were observed [98].
However, the role of AhR in AD pathogenesis is not fully understood. Kim et al. showed an increase in ARNT and CYP1A1 messenger RNA (mRNA) expression in AD skin [100]. On the other hand, Hong et al. revealed an increased protein level of AhR and ARNT but not CYP1A1 in skin lesions of AD patients [97]. Hu et al. demonstrated higher expression of AHR in serum and increased protein level of AhR in skin lesions of AD patients compared to healthy controls. Moreover, mRNA levels of AHR, AHRR, and CYP1A1 in peripheral blood mononuclear cells (PBMCs) of AD patients were higher in comparison to healthy controls. Thus, AHR expression level in PBMCs may be associated with eczema area and severity index score in AD patients [101].
The antioxidative transcription factor Nrf2 may be activated by some AhR ligands, and recent studies indicated a therapeutic effect of this group of AhR agonists. For instance, coal tar attenuates inflammatory response in AD and psoriasis patients by NRF2 activation upon AhR interaction [92,102]. However, excessive activation of AhR leads to abnormally accelerated keratinization of cells and the formation of pruritic artemin [103,104].
One of genes encoding nerve elongation factors that may be related to epidermal hyperinnervation is ARNT. ARNT, encoding artemin, acts as pruritus-related AhR target gene. Edamitsu et al. suggest that besides ARNT overexpression, constitutive AhR activation may exacerbate alterations in the epidermis in patients with AD [103]. Moreover, artemin expression and alloknesis may be enhanced by air pollutants via AhR activation [104]. Artemin expression is higher in patients with AD compared to healthy controls [104]. Topical application of 7,12-dimethylbenz[a]anthracene (DMBA), an exogenous AhR agonist, induced an AD-like phenotype, but this effect was not achieved when using endogenous AhR ligand FICZ. As FICZ is rapidly metabolized by CYP1A1, it cannot efficiently activate AD-related target genes. Therefore, prolonged AhR activation is crucial for pruritic AD symptoms induction [104].
A few reports indicate that some AhR agonists, such as FICZ, 2-(1H-Indol-3-ylcarbonyl)-4-thiazolecarboxylic acid methyl ester (ITE), and soybean tar Glyteer, may activate both canonical and noncanonical AhR signaling pathways. For instance, in human keratinocytes, FICZ promotes wound healing via extracellular signal-regulated kinase (ERK) signaling in an AhR-independent manner [105]. AhR endogenous ligand ITE also reduces transforming growth factor-beta (TGF-β) signaling without AhR activation. However, the recruitment of Th2 cells in AD skin lesions is regulated by chemokine (CC motif) ligand 17 (CCL17) and CCL22 expression. Both chemokines are produced via signal transducer and activator of transcription 6 (STAT6) activation in DCs. Takemura et al. demonstrated that soybean tar Glytter inhibits STAT6 expression; thus, CCL17 and CCL22 production in DCs is reduced [106]. Moreover, STAT6 expression is blocked by coal tar via AhR-mediated activation of the Nrf2 signaling pathway [92]. Interestingly, coal tar induces a shift in skin microbiome composition due to the microbiome-modulating properties of some AhR agonists. As the skin microbiome plays an important role in the development of inflammatory skin diseases, this biological mechanism of coal tar may have an essential therapeutic value [107].
Clinical studies confirm the efficacy of the AhR agonist tapinarof in the treatment of AD [108]. The action of tapinarof is based on the activation of the Nrf2-antioxidative pathway. Improvement in skin condition after tapinarof application is also associated with reduced IL-17A production and increased FLG expression [108].
5.2. Psoriasis
Psoriasis is a chronic inflammatory skin disease characterized by the thickened epidermis and skin infiltration of polymorphonuclear cells. The tumor necrosis factor-alpha (TNF-α)/IL-23/IL-17A axis plays a key role in induction and progression of psoriasis; thus, biological drugs against TNFα/IL-23/IL-17A have good therapeutic efficacy [109].
The interaction between AhR and endogenous ligands changes the inflammatory profile of skin lesions in psoriasis [110]. AhR-mediated Th17 activity controls the expression of IL-22 [111,112]. Monitoring of IL-22 plasma concentration allows the assessment of the severity of the disease [113]. Furthermore, the activity of IL-22 in keratinocytes is associated with increased expression of the transcription factor STAT3, which contributes to increased proliferation of epidermal cells [114]. IL-22 also affects the final stage of epidermal cell differentiation, leading to psoriasis-like skin lesions [115,116].
Interestingly, AhR activity is required for IL-22 production specifically by Th17 cells. AhR induction is not necessary for other types of IL-22-producing cells, including γδ T cells, CD4(−)CD8(−)TCRβ(+) T cells, and innate lymphoid cells. It is still unclear why Th17 specifically requires AhR stimulation to produce IL-22. Nevertheless, the reason for it may indicate the diversity of interactions of AhR downstream effectors with other transcription factors. For instance, TGF-β, which induces c-Maf activity, is involved in the differentiation of Th17 cells. C-Maf inhibits IL-22 expression by binding to its promoter. Hence, AhR activity appears to be necessary to overcome the suppressive activity of TGF-β [115].
On the other hand, the interaction of AhR with endogenous ligand FICZ reduces the inflammatory response in the IMQ-induced model of skin lesions [117]. Moreover, AHR-null mice presented significant exacerbation of the disease when compared to the AHR-sufficient control. In addition, an increase in mRNA expression of several proinflammatory cytokines involved in psoriasis, such as Il 17a, Il 17c, Il 23, Il 22, and Il 1b, was observed in the skin lesions of AHR-deficient mice [117].
Nevertheless, the role of AhR in psoriasis is controversial [99]. Kim et al. reported an increase in AhR and ARNT protein level in skin lesions in psoriasis, whereas CYP1A1 level was decreased when compared to healthy skin [100]. However, the fact that AhR may induce the expression of other genes not involved in the metabolism of xenobiotics cannot be ignored. It should be underlined that AhR controls activation of several signaling pathways, including phosphoinositide 3-kinase/protein kinase B (PI3K/Akt) and ERK signaling pathways, and the expression of various genes contributing to proliferation, adhesion, migration, or immune response [118,119]. On the other hand, serum levels of AhR and CYP1A1 in psoriasis patients were significantly higher when compared to the control group in the study conducted by Beranek et al. [120].
One of the genes that is found to be consistently upregulated in psoriatic skin lesions is KYNU, encoding an enzyme of the tryptophan metabolism. Kynureninase (KYNU) degrades kynurenine, an endogenous AhR ligand [121]. Gudjonsson et al. revealed other genes (e.g., IDO1, CYP2E1, CYP4B1, SMOX, and ALDH3A2) of the tryptophan catabolism pathway to be differentially regulated in psoriasis [122]. Deregulation of tryptophan metabolism in the skin may lead to a reduction of AhR ligands, such as kynurenine, kynurenic acid, and FICZ [123,124,125].
In both human psoriasis samples and an IMQ-induced model of skin inflammation, FICZ-induced AhR activation ameliorates inflammatory response. Moreover, Di Meglio et al. revealed that the expression of 29 out of 41 genes upregulated in psoriasis, including inflammatory-related genes such as IFIT, IFIT3, RSAD2 and MX2, was reduced after FICZ-induced AhR activation. Thus, decreased AhR activity in psoriatic skin lesions may be associated with increased expression of proinflammatory cytokines in this tissue leading to hyperinflammation [117]. Moreover, AhR activity seems to be crucial modulator of the severity of psoriasis [117]. In summary, the limited availability of endogenous AhR ligands could affect skin homeostasis regulated by this receptor.
It is not explicitly confirmed that a specific cytokine profile is responsible for the severity of skin lesions. This crosstalk between immune cells and nonhematopoietic cells involved in the inflammatory response is crucial for determining the pathogenesis of diseases such as psoriasis. However, the treatment of autoimmune inflammation is based on the modulation of the immune response [126]. An absence of AhR or blockade of its activity is associated with dysregulation of skin cell responses, mainly keratinocytes, to inflammatory stimuli. A number of inflammatory pathways are involved in the pathogenesis of psoriasis; thus, it is difficult to indicate the leading role of individual inflammatory mediators in the development of skin lesions. Recent studies indicate that the use of IL-17 blockers in an IMQ-induced psoriasis-like skin model is not sufficient to decrease the formation of skin lesions in AHR-deficient mice [127]. Moreover, AhR activity in the epidermal capillaries limits the recruitment of neutrophils, thus limiting the formation of skin lesions [128].
6. Skin Pigmentation Disorders
6.1. Hyperpigmentation
Hyperpigmentation of the skin is characteristic of tobacco smokers, and it may result from BaP-mediated AhR activation and enhanced melanogenesis [129]. The microphthalmia-associated transcription factor (MITF) is a major regulator of melanogenesis, which activates tyrosinase (TYR) and tyrosinase-related proteins (TYRPs). The expression of these melanogenic enzymes leads to melanin granules production [130]. The interaction of AhR with BaP or TCDD induces MITF activation, which in turn enhances TYR expression, resulting in increased melanogenesis [131]. Benzanthrone is another AhR ligand contributing to hyperpigmentation. Increased melanogenesis was observed in murine melanocytes treated with benzanthrone in vitro [132]. Skin pigmentation was also diagnosed in patients from Japan (Yusho) and Taiwan (Yucheng) after mass poisoning caused by cooking oil contaminated with PCBs and PCDFs [77,79]. Additionally, long-time exposure to high concentrations of PM2.5 may also be associated with hyperpigmentation [76].
6.2. Vitiligo
Vitiligo is an acquired pigmentary disorder, characterized by the loss of functioning melanocytes in skin, hair, or both. The pathogenesis of vitiligo is based on melanocyte defects, an innate immune response, and T-cell-mediated melanocyte destruction [133]. Vitiligo patients reveal a reduced expression of AHR in skin lesions compared to healthy controls [134]. However, furanochromones psoralen and khellin, in combination with UVA phototherapy, activate AhR, thus increasing melanogenesis [135].
AhR-mediated Treg cell differentiation and IL-10 expression may be associated with vitiligo pathogenesis, as IL-10 plays a crucial role in the development of self-tolerance [136,137]. Importantly, vitiligo is an autoimmune disease in which macrophages, T cells, cytokines, and other proinflammatory mediators play a prominent role [138]. Recent studies demonstrated increased TNF-α concentration and decreased IL-10 production in the serum of vitiligo patients [136,139]. Moreover, Tregs from AHR-null mice produced decreased level of IL-10 [27]. On the other hand, Taher et al. revealed that tacrolimus-induced increase in IL-10 level inhibited the degradation of melanocytes and might reduce disease symptoms [138].
The pathogenesis of this disease may be related to AHR − 129C > T polymorphism [139]. The T allele of this polymorphism increases the binding affinity of the SP1 transcription factor to AHR, thereby increasing the activity of the AHR promoter. Multiple TATA-less genes responsible for cell growth and immune response are controlled by SP1. AHR lacks TATA boxes, although its core promoter region possesses GC-rich fragments with several putative SP1 binding sites [140]. The abnormal binding affinity of the AHR promoter to SP1 (due to AHR hypermethylation or under the influence of an SP1 inhibitor) may decrease AHR expression. Interestingly, increased AHR expression was observed in carriers of the −129 T allele; thus, it could potentially be a genetic marker for vitiligo. On the other hand, −129 T allele possession is associated with higher expression of IL-10. Therefore, AHR − 129C > T polymorphism may be related to vitiligo by altering IL-10 production [139].
IL-22-producing cells, whose activity is dependent on AhR ligation, may also contribute to abnormal immune response underlying vitiligo [141]. Furthermore, IL-17 expression is correlated with vitiligo and may play a role in its pathogenesis [142]. However, the relationship between AhR-mediated IL-17 expression and vitiligo has not yet been stated. Similarly, the involvement of ROS in vitiligo pathogenesis remains controversial [143].
7. Skin Appendage Disorder: Chloracne
Chloracne is characterized by acne-like eruptions, blackheads, cysts, and pimples on the skin and may appear in response to permanent exposure to AhR ligands from polluted air, such as TCDD and PCDFs [77,78,79]. Chloracne skin lesions are located mainly on retroauricular and malar areas of the face as well as on the ear lobes and groin [80,144]. Increased AHR expression is observed in skin lesions of people exposed to dioxins present in polluted air [101]. Moreover, constitutive activation of AhR and excessive production of ROS may be crucial for the development of this disease [145]. Pathogenesis of chloracne is based on the accelerated process of final differentiation of keratinocytes induced by AhR agonists, although the molecular aspect of this mechanism is not fully understood [146,147].
Caputo et al. reported that exposure to high doses of TCDD contained in polluted air caused chloracne in children after the explosion in Seveso [78]. Similarly, massive poisoning of PCDFs and their derivatives induced chloracne in Japan (Yusho) [80] and Taiwan (Yucheng) [81]. Skin lesions covering over 30% of body surface area and sebaceous gland involution are observed in people exposed to very high doses of TCDD [146].
In physiological conditions, AhR activation also leads to accelerated keratinocyte differentiation [148]. However, structural stability of dioxins may be crucial for chloracne development, as endogenous AhR ligands are rapidly degraded. The key role of AhR in keratinization was confirmed in studies in on AHR-deficient and AHR-transgenic mice [73,149].
Furthermore, lipophilic dioxins can accumulate in the sebaceous glands with high AHR expression and might be secreted with sebum [144,150,151]. Moreover, chloracne indicates hyperkeratinization of interfollicular epidermis hair follicle cells [152]. In addition, a change in the physiology of sebocytes is observed in the form of a gradual loss of sebaceous cells and involution of sebaceous glands, which leads to cyst formation [150,153]. AhR-dioxins interaction results in hyperkeratinization of keratinocytes and transformation of sebocytes into keratinocytes [151,152,154].
Pathogenesis of chloracne is related to upregulation of the expression of particular genes and proteins. The reduced number of sebaceous glands and sebocytes may be associated with the altered metabolism of the mature sterol-binding protein (mSREBP-1), resulting from AMP-activated protein kinase (AMPK) activation [155]. On the other hand, the MAPK signaling pathway is also crucial for skin lesion formation in chloracne patients, as AhR activation in chloracne induces the activation of EGFR and MAPK [156]. EGFR and AhR compete for common coactivator p300 for their transcriptional activity. Thus, the activation of the EGFR pathway results in inhibition of AhR-mediated CYP1A1 expression [157].
A number of compounds coordinate the course of each stage of keratinization, which includes transglutaminase-1 and -3 of ceramides and various epidermal differentiation complex (EDC) proteins [158]. TCDD indirectly accelerates keratinization by interacting with EDC molecules such as LOR and FLG [159]. The expression of LOR and FLG increases due to the interaction with TCDD and induces earlier maturation of the epidermal barrier in the skin of mouse fetuses [160]. Application of TCDD directly on hairless mouse skin resulted in hyperkeratosis, epidermal hyperplasia, and sebaceous gland metaplasia [161].
Moreover, TCDD-induced activation of AhR increases the expression of genes involved in the keratinization process. This applies especially to EDC genes and genes responsible for ceramide synthesis [162]. Inflammation in chloracne results from increased expression of cytokines (IL-6, IL-8, and IL-1a) produced by keratinocytes and sebocytes [8,84,153].
The previous studies suggested that the severity of chloracne depends on the level of dioxins in the blood [80]. AhR stimulation is associated with impaired sebocyte proliferation and impaired lipid synthesis in these cells. As a result of dioxin-induced AhR activity, sebocytes lose their characteristic phenotype; thus, inhibition of lipogenesis and a decrease in the expression of keratin 7 and the epithelial antigen membrane occur. Moreover, the transformation of sebocytes into keratinocytes is associated with increased expression of the keratinocyte-specific molecules: keratin 10 and peroxisome proliferator-activated receptor-δ (PPAR-δ) [151,152,153]. Dedifferentiation of sebocytes may depend on the activity of the AhR/Blimp1 signaling pathway. Inhibition of lipogenesis and sebaceous gland atrophy is associated with inhibition of sebocyte proliferation and reduction of c-Myc expression mediated by Blimp1 activity. Furthermore, AhR–TCDD interaction induces the AhR/Blimp1 signaling activity [152].
8. Skin Cancer
AhR is also associated with carcinogenesis and tissue homeostasis [163,164]. However, its role in carcinogenesis is not clearly defined, and opposite effects of AhR on tumor progression have been reported. It is hypothesized that this seemingly contradictory function of AhR in tumor progression may be partially dependent on its cell-type-specific roles in cell migration [reviewed in [165]].
There is no clear confirmation that AhR activation leads to the development of skin cancers. However, the observed procarcinogenic effects of some AhR ligands and the biological role of down-effector genes activated by this receptor suggest its involvement in carcinogenesis. Long-term observations revealed that overexposure to some synthetic AhR ligands (e.g., polycyclic aromatic hydrocarbons) or UVB may lead to premalignant lesions or skin cancer [166,167,168].
Carcinogenicity might be associated with the activity of cytochrome P-450 enzymes, as it leads to either detoxification or potential carcinogens formation. Importantly, UVB is also involved in the induction of cytochrome P-450 subfamilies, including CYP1A1 and CYP1B1, and metabolic activation and transformation of organic procarcinogens to carcinogens. Moreover, several UV-induced mechanisms may be associated with skin carcinogenesis, such as direct UVB damage to skin cell DNA, reduced apoptosis, intensified keratinocyte proliferation, and chronic skin inflammation [169]. Finally, the stimulation of AhR leads to activation of MAPK signaling which may be involved in cancer cell proliferation.
8.1. Squamous Cell Carcinoma
Squamous cell carcinoma (SCC) is the most frequent skin malignancy in humans [170]. Importantly, AhR was identified as one of the genetic determinants of susceptibility to SCC in humans [171]. Several procarcinogenic and proinflammatory AhR-related genes potentially involved in carcinogenesis and cancer progression are upregulated in keratinocytes exposed to UVB, including CYP1A1, CYP1B1, COX-2, CXCL5, and matrix metalloproteinases (MMPs) (reviewed in [172]). It was suggested that the AhR signaling pathway is involved in the initiation of keratinocyte-derived skin cancers induced by UVB radiation [23]. Moreover, AhR signaling may contribute to the degradation of the cyclin-dependent kinase inhibitor p27Kip1 involved in cell cycle regulation, proliferation, and apoptosis in keratinocytes [172,173,174].
8.2. Melanoma
Surprisingly, there have been very few studies reported on the role of AhR in melanoma promotion and progression, although AHR is highly expressed in melanoma cell lines [175]. Furthermore, the interactions between tumor and stroma are mediated by AhR. It was reported that although AHR expression in the tumor inhibits melanoma growth and metastasis, the expression of this receptor in the stroma promotes melanomagenesis. AhR might act as tumor suppressor regarding melanoma cells, as its activity was associated with decreased migration and invasion, a reduced numbers of cancer stem-like cells, and aberrant β1-integrin and caveolin 1 concentrations. Human melanoma cell lines with the highest protein level of AhR have also inhibited migration and invasion activity. Moreover, AhR protein level is reduced in human melanomas with respect to nevi lesions. It is supposed that tumor progression and metastasis depend on stromal AhR in the case of AHR knockdown in melanoma cells [165]. Activation of AhR signaling in the tumor microenvironment may stimulate cancer cell proliferation, and migration by enhanced expression of proangiogenic mediators and factors increased cancer cell motility, including the vascular endothelial growth factor (VEGF) and TGF-β [48,176].
On the other hand, it was reported that environmental chemicals considered as AhR agonists contribute to melanoma progression and invasion through the stimulation and activity of MMPs [177]. Another study revealed that exposure to TCDD leads to upregulation of the melanogenic pathway not only in melanocytes but also in melanoma cells. However, no stimulation of melanoma cell proliferation was observed [131].
9. The Role of Tryptophan-Derived AhR Ligands in Skin Homeostasis
Previous studies revealed several ligands of AhR that can be grouped as follows:
Exogenous/synthetic ligands (i.e., TCDD, biphenyls, DMBA, methylcholanthrene, and BaP);
Exogenous/natural compounds, found in or metabolized from dietary plants (i.e., resveratrol and other glucosinolates, flavonoids, indolcarbinols, and kynurenic acid);
Endogenous ligands formed in the body (i.e., kynurenine, kynurenic acid, ITE, a tryptophan–cysteine dimer, and FICZ).
Several AhR agonists are derived from tryptophan, which is an essential amino acid that is considered as the strongest near-UV absorbing chromophore [65]. Thus, the role of these AhR ligands may be crucial for various processes in the skin. UV absorption by tryptophan leads to the production of several stable photoproducts that may have various biological activities. Some of these are considered as AhR ligands since conformational changes of tryptophan under exposure to UV radiation in the skin result in FICZ production [75,178]. Importantly, some other non-UV-induced tryptophan metabolites produced enzymatically in cells are also considered as AhR ligands (i.e., kynurenine and kynurenic acid) [123,179,180].
Three main ways by which tryptophan-derived AhR ligands reach the skin can be distinguished: topical application on the skin, as these ligands may be the compounds of skin care products; endogenous synthesis in cells of the skin [4]; and intragastric administration [181,182]. Furthermore, tryptophan-derived ligand activity affects various physiological and pathological processes.
9.1. FICZ
FICZ, a tryptophan oxidation product formed by exposure to UV or visible irradiation, binds with high affinity to AhR in mammalian cells, inducing expression of CYP1A1 [183]. UVB is the most efficient in FICZ formation from aqueous tryptophan, whereas visible light and UVA induce FICZ production with lower yields [184]. FICZ has a very high affinity for AhR but is quickly and efficiently degraded in cells by AhR-induced CYP1A1, CYP1A2, and CYP1B1, giving it low intracellular levels [185,186]. Importantly, FICZ has been found to be physiologically relevant in human skin [187]. However, the biological role of this tryptophan metabolite in physiological and pathological processes in the skin has not been fully studied. It was revealed that direct FICZ-mediated AhR activation alleviates inflammation in both human psoriasis samples and a mouse model of psoriasis-like skin lesions [117]. The FICZ–AhR interaction activates the AhR/ROS signaling pathway and increases the expression of inflammatory mediators (IL-1A, IL-1B, and IL-6) and, thus, may be associated with the dangerous effects of exposure to UVB radiation [8].
FICZ reveals a photosensitizing effect on keratinocytes. The simultaneous exposure to FICZ and UVA radiation induces apoptosis of keratinocytes due to caspase 3 activation and heat shock protein 70 (HSP70) production [183,184]. Moreover, FICZ reduces TGF-β-mediated collagen formation in human dermal fibroblasts [187,188]. These data indicate that FICZ may be responsible for the effect of photoaging after UVB exposure.
On the other hand, FICZ limits the production of IL-17 and IL-22 in skin lesions and reduces inflammation in dermatitis model [98,117]. Moreover, FICZ-mediated AhR activation is associated with increased expression of EDC, such as FLG and LOR [71]. FICZ promotes wound healing by increasing keratinocyte migration due to the activation of the MEK/ERK pathway in an AhR-independent manner [105]. Cell migration is supported by FICZ even in the conditions of AHR knockdown by small interfering RNAs (siRNAs) or an AhR inhibitor [105]. Therefore, inflammatory cell migration may result directly from interactions between FICZ and the TGF-β/ERK signaling pathway. However, the effect of FICZ may be associated with other molecular mechanisms stimulated by injury. These results shed a new light on the role of FICZ in skin homeostasis. Nevertheless, the mechanism of FICZ-mediated keratinocyte migration may be relevant to managing the treatment of skin wounds.
Mengoni et al. reported that AHR expression strictly correlates with the degree of dedifferentiation in both human melanoma samples and human and mouse melanoma cell lines [189]. Moreover, in the inflammatory environment, FICZ-mediated AhR activation induces the phenotypic switch of melanoma cells into the dedifferentiated state [189]. In addition, AhR-induced suppression of E-cadherin expression and induction of MMP activity resulted in reduced cell adhesion and increased cell motility [177,190]. Taken together, these data indicate that AhR activity may promote invasive features of tumor cells.
9.2. Kynurenine
Kynurenine, a key metabolite of the main route of tryptophan catabolism, is an endogenous agonist of AhR [191]. Although kynurenine activates the AhR using classical response genes such as CYP1A [191], it was previously revealed that kynurenine plays a more important role in AhR-dependent immunological responses rather than in the metabolism of xenobiotics. In a dose-dependent manner, kynurenine upregulates the expression of immunosuppressive genes, such as TGFB1 and IDO1 [192,193]. Kynurenine regulates T-cell differentiation and induces immunosuppressive strategies in cancer cells [124,191]. Moreover, kynurenine may display an immunosuppressive activity; thus, it takes part in disease tolerance pathways and represents a link between tryptophan catabolism and the AhR signaling pathway [192].
Although the impact of kynurenine on cancer cell proliferation is not fully understood, recent studies indicate that kynurenine activity is related to anticancer immune response. Kynurenine is produced by the tryptophan catabolizing enzymes, indoleamine 2,3-dioxygenase (IDO) and tryptophan 2,3-dioxygenase (TDO), in several types of cancer, including melanoma, to promote immune evasion [124,194]. Moreover, TCDD, one of the synthetic AhR ligand, determines tumor immunity as it promotes IDO activation, leading to kynurenine formation. IDO is constitutively expressed by many tumors and promotes immunosuppressive mechanisms due to depletion of tryptophan. Moreover, IDO promotes the formation of several tryptophan metabolites such as kynurenine with immunosuppressive activity. It was reported that IDO expression is associated with unfavorable prognosis in patients with various malignancies (reviewed in [195]). Importantly, expression and activity of IDO 1 and 2 are controlled by inflammatory mediators [196].
Similarly to tryptophan derivatives, AhR activity is associated with immune response regulation, as it was previously demonstrated in fibroblasts, endothelial cells, and macrophages [197,198,199]. Bessede et al. reported that tryptophan metabolites—AhR interaction contributes to the activation of Scr kinase, thus promoting IDO1 phosphorylation [192]. Furthermore, TGF-β expression is blocked, as kynurenic acid cannot induce its activation without IDO1. TGF-β is a major immune tolerance indicator; thus, AhR-mediated IDO1 phosphorylation affects immune response [192].
9.3. Kynurenic Acid
Kynurenic acid, a product of tryptophan metabolism enzymatically formed from kynurenine, is a natural ligand for AhR. Kynurenic acid is produced by kynurenine aminotransferases (KATs), which promotes L-kynurenine transamination. Moreover, the presence of ROS allows the direct transformation of tryptophan or kynurenine into kynurenic acid (reviewed in [179,196]). Kynurenic acid in nanomolar concentrations is an efficient agonist for the human AhR inducing IL-6 production and xenobiotic metabolism in cells [123]. Nevertheless, the role of kynurenine pathway metabolites in AhR-mediated skin homeostasis remains unclear. Recent studies indicate that AhR-kynurenic acid interaction may be relevant for maintaining the immunosuppressive microenvironment in several cancer types [179,200].
It has been revealed that kynurenic acid has various biological activities, including neuroprotective, anticonvulsant, anti-inflammatory, antioxidant, and antiulcer activity (reviewed in [179,196]). Importantly, kynurenic acid also has antiproliferative and antimigratory properties against various types of cancer cells (reviewed in [179]) by inhibition of signaling pathways (MAPK, PI3K/Akt) and overexpression of cell cycle regulatory proteins (p21Waf1/Cip1) [119,201]. Moreover, a recent study confirmed the biological activity of kynurenic acid towards melanoma A375 and RPMI-7951 cells [202].
Kynurenic acid is formed endogenously and is present in almost all human body fluids and tissues (reviewed in [179]) Importantly, kynurenic acid is also present in several products of human diet [181,182]. The intragastrically administered KYNA is absorbed and transported to peripheral organs via the bloodstream [203]. The role of kynurenic acid in the skin is not fully studied. It was reported that kynurenic acid is phototoxic for erythrocytes and glia cells, but no specific studies regarding skin cells have been performed [204,205].
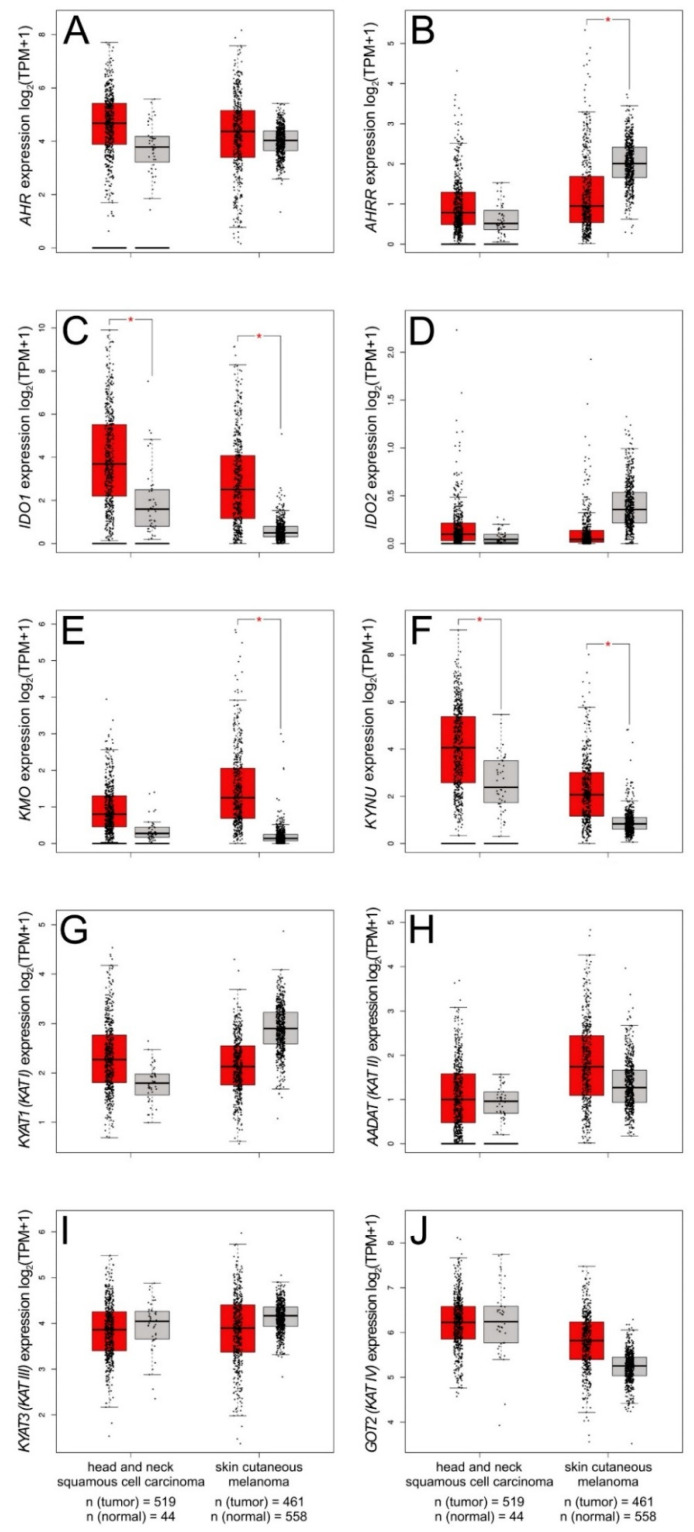
Although AHR expression levels do not differ significantly in various types of skin cancer (Figure 3A), we observed a significant downregulation of AHRR expression in skin cutaneous melanoma (SKCN) (Figure 3B). Vogel et al. report that the upregulated AhRR expression inhibits the AhR-mediated antiapoptotic response in mouse embryonic fibroblasts [206]. As AhRR tends to play a significant role in suppressing inflammation, the downregulated AHRR expression may promote tumor growth.
Figure 3.
Expression pattern of genes encoding AHR (A), AHRR (B), tryptophan catabolizing enzymes (IDO1 (C), IDO2 (D), KMO (E), KYNU(F)) and kynurenine aminotransferases (KAT I–IV (G–J)) in human head and neck squamous cell carcinoma and skin cutaneous melanoma. Expression of KYAT1 (KAT I), AADAT (KAT II), KYAT3 (KAT III), GOT2 (KAT IV) was analyzed. Significant downregulation of AHRR expression was observed in skin cutaneous melanoma (B). Both head and neck squamous cell carcinoma and skin cutaneous melanoma showed significantly higher expression of IDO1 (C). Moreover, significantly upregulated expression of KMO was found in skin cutaneous melanoma (SKCM) (E). Significantly upregulated KYNU expression was observed in both HNSC and SKCM (F). GEPIA2 was queried for skin cancers: human head and neck squamous cell carcinoma and skin cutaneous melanoma [207]. Differences in gene expression levels were studied using ANOVA. * p < 0.01 and fold-change threshold (|Log2FC| cutoff) of 1.
Interestingly, the expression of genes encoding tryptophan catabolizing enzymes (e.g., IDO1 and KYNU) is significantly upregulated in two types of skin cancer: head and neck squamous cell carcinoma (HNSC) and SKCN (Figure 3).
Although the reason for this phenomenon has not yet been revealed, a few hypotheses seems to be reliable and feasible. The kynurenine pathway is a major metabolic pathway involved in the formation of key a coenzyme, nicotinamide adenine dinucleotide (NAD+). As cancer cells display increased energy requirements, overexpression of IDO1 and KYNU may arise from the need of an additional source of energy NAD+. On the other hand, it cannot be ignored that the increased activation of KYNU may be caused by the need to reduce the amount of kynurenine or kynurenic acid, which may have a negative effect on cancer cells.
Theate et al. indicate that the expression of IDO1 may act like a negative prognostic marker in various cancer types, including melanoma and carcinomas of the cervix, bladder, kidney, and lung [208]. Moreover, AhR regulates the expression of IDO1 and TDO. Regarding the tumor microenvironment, a decreased level of tryptophan caused by IDO1 and TDO activity may result in loss of immune function through the suppression of antigen-specific T-cell response and stimulation of DC-mediated immune tolerance [124]. Thus, declined effectiveness of the anticancer immune response, resulting from deregulation of the kynurenine pathway, may be associated with cancer progression. Moreover, as the activation of the IDO/kynurenine/AhR pathway is associated with the resistance to immune checkpoint blockade, AhR may be involved in therapy resistance [209].
9.4. Skin Microbiome Metabolites
The epidermis may be colonized by various species of commensal microbes. For instance, lipophilic yeasts Malassezia are capable of converting tryptophan into indole compounds, some of which are AhR agonists. Malassezia furfur and Malassezia globosa colonize the skin of approximately 80% of the healthy population. However, their impact on skin physiology is controversial [12,210].
The activity of tryptophan-derived AhR agonists produced by Malassezia is associated with the hyperproliferation in seborrheic dermatitis and altered inflammatory in pityriasis versicolor [210]. Moreover, Malassezia metabolites affect cell cycle regulation and DNA repair, thus increasing the risk of skin cancer. Gaitanis et al. also reported that AhR ligands produced by Malassezia change ROS production and suppress the inflammatory response [211].
10. Conclusions
Previous studies confirmed at least a partial role of AhR in the pathogenesis of various skin diseases, including inflammatory diseases, skin pigmentation disorders, and cancer [84,89,154]. However, the function of AhR is complex as the outcome of AhR activation depends on the type of cell and ligand [13,15]. Furthermore, many different biological responses to AhR stimulation or inhibition in the skin are observed [56]. Most of the reported data are focused on the immunological and oncological effect of AhR stimulation. However, AhR ligation may induce excessive expression of proinflammatory cytokines and ROS production, leading to inflammatory disease development or carcinogenesis [55]. On the other hand, AhR-agonist-mediated activity may affect the differentiation of Treg cells, thus promoting immune tolerance [126,127]. Therefore, to determine the physiological mechanism of AhR and its role in skin disease development, more data are needed from both basic and clinical studies.
Importantly, tryptophan derivatives are a large group of AhR ligands that may potentially play a role in the pathogenesis or treatment of many skin diseases [7,169]. They are produced by enzymatic reactions or due to UV radiation in various skin cells; thus, skin is constantly exposed to tryptophan-derived AhR ligands. Additionally, some of them are present in herbs and plant extracts commonly used in skincare and treatment. However, their biological role requires further examination. In future studies, the involvement of tryptophan-derived AhR ligands in the initiation and progression of skin diseases should be clarified. The question of whether tryptophan-derived AhR ligands should be used in the prevention of skin diseases or whether we should avoid contact with them due to their negative impact on disease progression remains without a clear answer.
Acknowledgments
The results shown in this review are in part based upon data generated by the TCGA Research Network: https://www.cancer.gov/tcga.
Abbreviations
| AD | atopic dermatitis |
| AhR | aryl hydrocarbon receptor |
| AhRR | aryl hydrocarbon receptor repressor |
| Akt | protein kinase B |
| AMPK | AMP-activated protein kinase |
| ARNT | aryl hydrocarbon receptor nuclear translocator |
| ATP | adenosine triphosphate |
| BaP | benzo[a]pyrene |
| cAMP | 3′5′-cyclic adenosine monophosphate |
| CCL17 | chemokine (C-C motif) ligand 17 |
| CCL22 | chemokine (C-C motif) ligand 22 |
| CDK | cyclin-dependent kinase |
| DC | dendritic cell |
| DMBA | 7,12-dimethylbenz[a]anthracene |
| EDC | epidermal differentiation complex |
| EGFR | epidermal growth factor receptor |
| ER | estrogen receptor |
| ERK | extracellular signal-regulated kinase |
| FICZ | 6-formylindolo[3,2-b]carbazole |
| FLG | Filaggrin |
| HIF | hypoxia-induced factor |
| HNSC | head and neck squamous cell carcinoma |
| HMOX1 | heme oxygenase 1 |
| HSP | heat shock protein |
| IaId | indole-3-aldehyde |
| IDO | indoleamine 2,3-dioxygenase |
| IFN-γ | interferon gamma |
| ITE | 2-(1H-Indol-3-ylcarbonyl)-4-thiazolecarboxylic acid methyl ester |
| KAT | kynurenine aminotransferases |
| KLF6 | Kruppel-like factor 6 |
| KYNA | kynurenic acid |
| KYNU | kynureninase |
| LC | Langerhans cell |
| LOR | Loricrin |
| LPR6 | LDL receptor related protein 6 |
| MAPK | mitogen-activated protein kinase |
| MITF | microphtalmia-associated transcription factor |
| Msrebp-1 | mature sterol-binding protein |
| NAD | nicotinamide adenine dinucleotide |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NQO1 | NAD(P)H quinone dehydrogenase 1 |
| Nrf2 | nuclear factor-erythroid 2-related factor-2 |
| PAH | polycyclic aromatic hydrocarbons |
| PBMC | peripheral blood mononuclear cell |
| PCB | polychlorinated biphenyls |
| PCDD | polychlorinated dibenzo-p-dioxins |
| PCDF | polychlorinated dibenzofurans |
| PI3K | phosphoinositide 3-kinase |
| PKA | protein kinase A |
| PKC | protein kinase C |
| PPAR-δ | peroxisome proliferator-activated receptor-δ |
| PTD | photodynamic therapy |
| Rb | retinoblastoma protein |
| ROS | reactive oxygen species |
| SCC | squamous cell carcinoma |
| siRNA | small interfering RNA |
| SKCN | skin cutaneous melanoma |
| SOS1 | son of sevenless 1 |
| STAT | signal transducer and activator of transcription |
| TCDD | 2,3,7,8-tetrachlorodibenzo-p-dioxin |
| TDO | tryptophan 2,3-dioxygenase |
| TGF-β | transforming growth factor beta |
| TNF-α | tumor necrosis factor alpha |
| Treg | T regulatory cell |
| TRP | tryptophan |
| TSLP | thymic stromal lymphopoietin |
| TYR | tyrosinase |
| TYRP | tyrosinase-related protein |
| VEGF | vascular endothelial growth factor |
| XAP2 | the hepatitis B virus X-associated protein 2 |
| XRE | xenobiotic-responsive element |
Author Contributions
Conceptualization, K.W.; writing—original draft preparation, M.S., K.W.; writing—review and editing, K.W., T.P.; visualization, M.S.; supervision, K.W., T.P.; project administration, K.W.; funding acquisition, K.W., T.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by National Science Centre, Poland 2015/17/D/NZ7/02170 (DEC-2015/17/D/NZ7/02170) and Medical University of Lublin, Poland DS 544.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abel J., Haarmann-Stemmann T. An introduction to the molecular basics of aryl hydrocarbon receptor biology. Biol. Chem. 2010;391:1235–1248. doi: 10.1515/bc.2010.128. [DOI] [PubMed] [Google Scholar]
- 2.Esser C., Rannug A. The aryl hydrocarbon receptor in barrier organ physiology, immunology, and toxicology. Pharmacol. Rev. 2015;67:259–279. doi: 10.1124/pr.114.009001. [DOI] [PubMed] [Google Scholar]
- 3.Denison M.S., Nagy S.R. Activation of the aryl hydrocarbon receptor by structurally diverse exogenous and endogenous chemicals. Annu. Rev. Pharmacol. Toxicol. 2003;43:309–334. doi: 10.1146/annurev.pharmtox.43.100901.135828. [DOI] [PubMed] [Google Scholar]
- 4.Sheipouri D., Braidy N., Guillemin G.J. Kynurenine pathway in skin cells: Implications for UV-induced skin damage. Int. J. Tryptophan. Res. 2012;5:15–25. doi: 10.4137/IJTR.S9835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mimura J., Fujii-Kuriyama Y. Functional role of AhR in the expression of toxic effects by TCDD. Biochim. et Biophys. Acta Gen. Subj. 2003 doi: 10.1016/S0304-4165(02)00485-3. [DOI] [PubMed] [Google Scholar]
- 6.Kawasaki H., Chang H.W., Tseng H.C., Hsu S.C., Yang S.J., Hung C.H., Zhou Y., Huang S.K. A tryptophan metabolite, kynurenine, promotes mast cell activation through aryl hydrocarbon receptor. Allergy. 2014;69:445–452. doi: 10.1111/all.12346. [DOI] [PubMed] [Google Scholar]
- 7.Wirthgen E., Hoeflich A., Rebl A., Günther J. Kynurenic Acid: The janus-faced role of an immunomodulatory tryptophan metabolite and its link to pathological conditions. Front. Immunol. 2018;8:1957. doi: 10.3389/fimmu.2017.01957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tanaka Y., Uchi H., Hashimoto-Hachiya A., Furue M. Tryptophan Photoproduct FICZ Upregulates IL1A, IL1B, and IL6 Expression via Oxidative Stress in Keratinocytes. Oxid. Med. Cell Longev. 2018;2018:9298052. doi: 10.1155/2018/9298052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakahara T., Mitoma C., Hashimoto-Hachiya A., Takahara M., Tsuji G., Uchi H., Yan X., Hachisuka J., Chiba T., Esaki H., et al. Antioxidant opuntia ficus-indica extract activates AHR-NRF2 signaling and upregulates filaggrin and loricrin expression in human keratinocytes. J. Med. Food. 2015;18:1143–1149. doi: 10.1089/jmf.2014.3396. [DOI] [PubMed] [Google Scholar]
- 10.Takei K., Hashimoto-Hachiya A., Takahara M., Tsuji G., Nakahara T., Furue M. Cynaropicrin attenuates UVB-induced oxidative stress via the AhR-Nrf2-Nqo1 pathway. Toxicol. Lett. 2015;234:74–80. doi: 10.1016/j.toxlet.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Uchi H., Yasumatsu M., Morino-Koga S., Mitoma C., Furue M. Inhibition of aryl hydrocarbon receptor signaling and induction of NRF2-mediated antioxidant activity by cinnamaldehyde in human keratinocytes. J. Dermatol. Sci. 2017;85:36–43. doi: 10.1016/j.jdermsci.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Krämer H.J., Podobinska M., Bartsch A., Battmann A., Thoma W., Bernd A., Kummer W., Irlinger B., Steglich W., Mayser P. Malassezin, a novel agonist of the aryl hydrocarbon receptor from the yeast Malassezia furfur, induces apoptosis in primary human melanocytes. Chembiochem. 2005;6:860–865. doi: 10.1002/cbic.200400247. [DOI] [PubMed] [Google Scholar]
- 13.Wincent E., Bengtsson J., Bardbori A.M., Alsberg T., Luecke S., Rannug U., Rannug A. Inhibition of cytochrome P4501-dependent clearance of the endogenous agonist FICZ as a mechanism for activation of the aryl hydrocarbon receptor. Proc. Natl. Acad. Sci. USA. 2012;109:4479–4484. doi: 10.1073/pnas.1118467109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitchell K.A., Elferink C.J. Timing is everything: Consequences of transient and sustained AhR activity. Biochem. Pharmacol. 2009;77:947–956. doi: 10.1016/j.bcp.2008.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun Y.V., Boverhof D.R., Burgoon L.D., Fielden M.R., Zacharewski T.R. Comparative analysis of dioxin response elements in human, mouse and rat genomic sequences. Nucleic Acids Res. 2004;32:4512–4523. doi: 10.1093/nar/gkh782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frericks M., Meissner M., Esser C. Microarray analysis of the AHR system: Tissue-specific flexibility in signal and target genes. Toxicol. Appl. Pharmacol. 2007;220:320–332. doi: 10.1016/j.taap.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Wakx A., Nedder M., Tomkiewicz-Raulet C., Dalmasso J., Chissey A., Boland S., Vibert F., Degrelle S.A., Fournier T., Coumoul X., et al. Expression, localization, and activity of the aryl hydrocarbon receptor in the human placenta. Int. J. Mol. Sci. 2018;19:3762. doi: 10.3390/ijms19123762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreno-Marín N., Barrasa E., Morales-Hernández A., Paniagua B., Blanco-Fernández G., Merino J.M., Fernández-Salguero P.M. Dioxin receptor adjusts liver regeneration after acute toxic injury and protects against liver carcinogenesis. Sci. Rep. 2017;7:10420. doi: 10.1038/s41598-017-10984-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmidt J.V., Su G.H., Reddy J.K., Simon M.C., Bradfield C.A. Characterization of a murine Ahr null allele: Involvement of the Ah receptor in hepatic growth and development. Proc. Natl. Acad. Sci. USA. 1996;93:6731–6736. doi: 10.1073/pnas.93.13.6731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carreira V.S., Fan Y., Wang Q., Zhang X., Kurita H., Ko C.I., Naticchioni M., Jiang M., Koch S., Medvedovic M., et al. Ah receptor signaling controls the expression of cardiac development and homeostasis genes. Toxicol. Sci. 2015;147:425–435. doi: 10.1093/toxsci/kfv138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krock B.L., Eisinger-Mathason T.S., Giannoukos D.N., Shay J.E., Gohil M., Lee D.S., Nakazawa M.S., Sesen J., Skuli N., Simon M.C. The aryl hydrocarbon receptor nuclear translocator is an essential regulator of murine hematopoietic stem cell viability. Blood. 2015;125:3263–3272. doi: 10.1182/blood-2014-10-607267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yu M., Wang Q., Ma Y., Li L., Yu K., Zhang Z., Chen G., Li X., Xiao W., Xu P., et al. Aryl hydrocarbon receptor activation modulates intestinal epithelial barrier function by maintaining tight junction integrity. Int. J. Biol. Sci. 2018;14:69–77. doi: 10.7150/ijbs.22259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agostinis P., Garmyn M., van Laethem A. The Aryl hydrocarbon receptor: An illuminating effector of the UVB response. Sci. STKE. 2007;2007:pe49. doi: 10.1126/stke.4032007pe49. [DOI] [PubMed] [Google Scholar]
- 24.Levine-Fridman A., Chen L., Elferink C.J. Cytochrome P4501A1 promotes G1 phase cell cycle progression by controlling aryl hydrocarbon receptor activity. Mol. Pharmacol. 2004;65:461–469. doi: 10.1124/mol.65.2.461. [DOI] [PubMed] [Google Scholar]
- 25.Ishihara Y., Kado S.Y., Hoeper C., Harel S., Vogel C.F.A. Role of NF-kB RelB in Aryl hydrocarbon receptor-mediated ligand specific effects. Int. J. Mol. Sci. 2019;20:2652. doi: 10.3390/ijms20112652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim D.W., Gazourian L., Quadri S.A., Romieu-Mourez R., Sherr D.H., Sonenshein G.E. The RelA NF-kappaB subunit and the aryl hydrocarbon receptor (AhR) cooperate to transactivate the c-myc promoter in mammary cells. Oncogene. 2000;19:5498–5506. doi: 10.1038/sj.onc.1203945. [DOI] [PubMed] [Google Scholar]
- 27.Kimura A., Naka T., Nohara K., Fujii-Kuriyama Y., Kishimoto T. Aryl hydrocarbon receptor regulates Stat1 activation and participates in the development of Th17 cells. Proc. Natl. Acad. Sci. USA. 2008;105:9721–9726. doi: 10.1073/pnas.0804231105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swedenborg E., Pongratz I. AhR and ARNT modulate ER signaling. Toxicology. 2010;268:132–138. doi: 10.1016/j.tox.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 29.Evans B.R., Karchner S.I., Allan L.L., Pollenz R.S., Tanguay R.L., Jenny M.J., Sherr D.H., Hahn M.E. Repression of aryl hydrocarbon receptor (AHR) signaling by AHR repressor: Role of DNA binding and competition for AHR nuclear translocator. Mol. Pharmacol. 2008;73:387–398. doi: 10.1124/mol.107.040204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hahn M.E., Karchner S.I., Evans B.R., Franks D.G., Merson R.R., Lapseritis J.M. Unexpected diversity of aryl hydrocarbon receptors in non-mammalian vertebrates: Insights from comparative genomics. J. Exp. Zool. A Comp. Exp. Biol. 2006;305:693–706. doi: 10.1002/jez.a.323. [DOI] [PubMed] [Google Scholar]
- 31.Wilson S.R., Joshi A.D., Elferink C.J. The tumor suppressor Kruppel-like factor 6 is a novel aryl hydrocarbon receptor DNA binding partner. J. Pharmacol. Exp. Ther. 2013;345:419–429. doi: 10.1124/jpet.113.203786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson D.P., Li H., Mitchell K.A., Joshi A.D., Elferink C.J. Ah receptor-mediated suppression of liver regeneration through NC-XRE-driven p21Cip1 expression. Mol. Pharmacol. 2014;85:533–541. doi: 10.1124/mol.113.089730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joshi A.D., Carter D.E., Harper T.A., Jr., Elferink C.J. Aryl hydrocarbon receptor-dependent stanniocalcin 2 induction by cinnabarinic acid provides cytoprotection against endoplasmic reticulum and oxidative stress. J. Pharmacol. Exp. Ther. 2015;353:201–212. doi: 10.1124/jpet.114.222265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vogel C.F., Sciullo E., Matsumura F. Involvement of RelB in aryl hydrocarbon receptor-mediated induction of chemokines. Biochem. Biophys. Res. Commun. 2007;363:722–726. doi: 10.1016/j.bbrc.2007.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ge N.L., Elferink C.J. A direct interaction between the aryl hydrocarbon receptor and retinoblastoma protein. Linking dioxin signaling to the cell cycle. J. Biol. Chem. 1998;273:22708–22713. doi: 10.1074/jbc.273.35.22708. [DOI] [PubMed] [Google Scholar]
- 36.Huang G., Elferink C.J. A novel nonconsensus xenobiotic response element capable of mediating aryl hydrocarbon receptor-dependent gene expression. Mol. Pharmacol. 2012;81:338–347. doi: 10.1124/mol.111.075952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fritsche E., Schäfer C., Calles C., Bernsmann T., Bernshausen T., Wurm M., Hübenthal U., Cline J.E., Hajimiragha H., Schroeder P., et al. Lightening up the UV response by identification of the arylhydrocarbon receptor as a cytoplasmatic target for ultraviolet B radiation. Proc. Natl. Acad. Sci. USA. 2007;104:8851–8856. doi: 10.1073/pnas.0701764104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soshilov A., Denison M.S. Role of the Per/Arnt/Sim domains in ligand-dependent transformation of the aryl hydrocarbon receptor. J. Biol. Chem. 2008;283:32995–33005. doi: 10.1074/jbc.M802414200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fernandez-Salguero P.M., Hilbert D.M., Rudikoff S., Ward J.M., Gonzalez F.J. Aryl-hydrocarbon receptor-deficient mice are resistant to 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced toxicity. Toxicol. Appl. Pharmacol. 1996;140:173–179. doi: 10.1006/taap.1996.0210. [DOI] [PubMed] [Google Scholar]
- 40.Kolluri S.K., Weiss C., Koff A., Göttlicher M. p27(Kip1) induction and inhibition of proliferation by the intracellular Ah receptor in developing thymus and hepatoma cells. Genes. Dev. 1999;13:1742–1753. doi: 10.1101/gad.13.13.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pang P.H., Lin Y.H., Lee Y.H., Hou H.H., Hsu S.P., Juan S.H. Molecular mechanisms of p21 and p27 induction by 3-methylcholanthrene, an aryl-hydrocarbon receptor agonist, involved in antiproliferation of human umbilical vascular endothelial cells. J. Cell Physiol. 2008;215:161–171. doi: 10.1002/jcp.21299. [DOI] [PubMed] [Google Scholar]
- 42.Barnes-Ellerbe S., Knudsen K.E., Puga A. 2,3,7,8-Tetrachlorodibenzo-p-dioxin blocks androgen-dependent cell proliferation of LNCaP cells through modulation of pRB phosphorylation. Mol. Pharmacol. 2004;66:502–511. doi: 10.1124/mol.104.000356. [DOI] [PubMed] [Google Scholar]
- 43.Huang G., Elferink C.J. Multiple mechanisms are involved in Ah receptor-mediated cell cycle arrest. Mol. Pharmacol. 2005;67:88–96. doi: 10.1124/mol.104.002410. [DOI] [PubMed] [Google Scholar]
- 44.Marlowe J.L., Knudsen E.S., Schwemberger S., Puga A. The aryl hydrocarbon receptor displaces p300 from E2F-dependent promoters and represses S phase-specific gene expression. J. Biol. Chem. 2004;279:29013–29022. doi: 10.1074/jbc.M404315200. [DOI] [PubMed] [Google Scholar]
- 45.Abdelrahim M., Smith R., 3rd, Safe S. Aryl hydrocarbon receptor gene silencing with small inhibitory RNA differentially modulates Ah-responsiveness in MCF-7 and HepG2 cancer cells. Mol. Pharmacol. 2003;63:1373–1381. doi: 10.1124/mol.63.6.1373. [DOI] [PubMed] [Google Scholar]
- 46.Watabe Y., Nazuka N., Tezuka M., Shimba S. Aryl hydrocarbon receptor functions as a potent coactivator of E2F1-dependent trascription activity. Biol. Pharm. Bull. 2010;33:389–397. doi: 10.1248/bpb.33.389. [DOI] [PubMed] [Google Scholar]
- 47.Pierre S., Bats A.S., Chevallier A., Bui L.C., Ambolet-Camoit A., Garlatti M., Aggerbeck M., Barouki R., Coumoul X. Induction of the Ras activator Son of Sevenless 1 by environmental pollutants mediates their effects on cellular proliferation. Biochem. Pharmacol. 2011;81:304–313. doi: 10.1016/j.bcp.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 48.Mulero-Navarro S., Pozo-Guisado E., Pérez-Mancera P.A., Alvarez-Barrientos A., Catalina-Fernández I., Hernández-Nieto E., Sáenz-Santamaria J., Martínez N., Rojas J.M., Sánchez-García I., et al. Immortalized mouse mammary fibroblasts lacking dioxin receptor have impaired tumorigenicity in a subcutaneous mouse xenograft model. J. Biol. Chem. 2005;280:28731–28741. doi: 10.1074/jbc.M504538200. [DOI] [PubMed] [Google Scholar]
- 49.Diry M., Tomkiewicz C., Koehle C., Coumoul X., Bock K.W., Barouki R., Transy C. Activation of the dioxin/aryl hydrocarbon receptor (AhR) modulates cell plasticity through a JNK-dependent mechanism. Oncogene. 2006;25:5570–5574. doi: 10.1038/sj.onc.1209553. [DOI] [PubMed] [Google Scholar]
- 50.Hanieh H., Mohafez O., Hairul-Islam V.I., Alzahrani A., Ismail M.B., Thirugnanasambantham K. Novel aryl hydrocarbon receptor agonist suppresses migration and invasion of breast cancer cells. PLoS ONE. 2016;11:e0167650. doi: 10.1371/journal.pone.0167650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jin U.H., Lee S.O., Pfent C., Safe S. The aryl hydrocarbon receptor ligand omeprazole inhibits breast cancer cell invasion and metastasis. BMC Cancer. 2014;14:498. doi: 10.1186/1471-2407-14-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yamashita N., Saito N., Zhao S., Hiruta N., Park Y., Bujo H., Nemoto K., Kanno Y. Heregulin-induced cell migration is promoted by aryl hydrocarbon receptor in HER2-overexpressing breast cancer cells. Exp. Cell Res. 2018;366:34–40. doi: 10.1016/j.yexcr.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 53.Stanford E.A., Ramirez-Cardenas A., Wang Z., Novikov O., Alamoud K., Koutrakis P., Mizgerd J.P., Genco C.A., Kukuruzinska M., Monti S., et al. Role for the aryl hydrocarbon receptor and diverse ligands in oral squamous cell carcinoma migration and tumorigenesis. Mol. Cancer Res. 2016;14:696–706. doi: 10.1158/1541-7786.MCR-16-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vogel C.F., Sciullo E., Li W., Wong P., Lazennec G., Matsumura F. RelB, a new partner of aryl hydrocarbon receptor-mediated transcription. Mol. Endocrinol. 2007;21:2941–2955. doi: 10.1210/me.2007-0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsuji G., Takahara M., Uchi H., Matsuda T., Chiba T., Takeuchi S., Yasukawa F., Moroi Y., Furue M. Identification of ketoconazole as an AhR-Nrf2 activator in cultured human keratinocytes: The basis of its anti-inflammatory effect. J. Investig. Dermatol. 2012;132:59–68. doi: 10.1038/jid.2011.194. [DOI] [PubMed] [Google Scholar]
- 56.Haarmann-Stemmann T., Abel J., Fritsche E., Krutmann J. The AhR-Nrf2 pathway in keratinocytes: On the road to chemoprevention? J. Investig. Dermatol. 2012;132:7–9. doi: 10.1038/jid.2011.359. [DOI] [PubMed] [Google Scholar]
- 57.Puga A., Hoffer A., Zhou S., Bohm J.M., Leikauf G.D., Shertzer H.G. Sustained increase in intracellular free calcium and activation of cyclooxygenase-2 expression in mouse hepatoma cells treated with dioxin. Biochem. Pharmacol. 1997;54:1287–1296. doi: 10.1016/S0006-2952(97)00417-6. [DOI] [PubMed] [Google Scholar]
- 58.Li W., Matsumura F. Significance of the nongenomic, inflammatory pathway in mediating the toxic action of TCDD to induce rapid and long-term cellular responses in 3T3-L1 adipocytes. Biochemistry. 2008;47:13997–14008. doi: 10.1021/bi801913w. [DOI] [PubMed] [Google Scholar]
- 59.Matsumura F. The significance of the nongenomic pathway in mediating inflammatory signaling of the dioxin-activated Ah receptor to cause toxic effects. Biochem. Pharmacol. 2009;77:608–626. doi: 10.1016/j.bcp.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 60.Vorrink S.U., Severson P.L., Kulak M.V., Futscher B.W., Domann F.E. Hypoxia perturbs aryl hydrocarbon receptor signaling and CYP1A1 expression induced by PCB 126 in human skin and liver-derived cell lines. Toxicol. Appl. Pharmacol. 2014;274:408–416. doi: 10.1016/j.taap.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wong W.J., Richardson T., Seykora J.T., Cotsarelis G., Simon M.C. Hypoxia-inducible factors regulate filaggrin expression and epidermal barrier function. J. Investig. Dermatol. 2015;135:454–461. doi: 10.1038/jid.2014.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mathew L.K., Sengupta S.S., Ladu J., Andreasen E.A., Tanguay R.L. Crosstalk between AHR and Wnt signaling through R-Spondin1 impairs tissue regeneration in zebrafish. FASEB J. 2008;22:3087–3096. doi: 10.1096/fj.08-109009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rogers J.M., Denison M.S. Analysis of the antiestrogenic activity of 2,3,7,8-tetrachlorodibenzo-p-dioxin in human ovarian carcinoma BG-1 cells. Mol. Pharmacol. 2002;61:1393–1403. doi: 10.1124/mol.61.6.1393. [DOI] [PubMed] [Google Scholar]
- 64.Safe S., Wang F., Porter W., Duan R., McDougal A. Ah receptor agonists as endocrine disruptors: Antiestrogenic activity and mechanisms. Toxicol. Lett. 1998;102–103:343–347. doi: 10.1016/S0378-4274(98)00331-2. [DOI] [PubMed] [Google Scholar]
- 65.Denison M.S., Soshilov A.A., He G., DeGroot D.E., Zhao B. Exactly the same but different: Promiscuity and diversity in the molecular mechanisms of action of the aryl hydrocarbon (dioxin) receptor. Toxicol. Sci. 2011;124:1–22. doi: 10.1093/toxsci/kfr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Esser C., Bargen I., Weighardt H., Haarmann-Stemmann T., Krutmann J. Functions of the aryl hydrocarbon receptor in the skin. Semin. Immunopathol. 2013;35:677–691. doi: 10.1007/s00281-013-0394-4. [DOI] [PubMed] [Google Scholar]
- 67.Schmidt J.V., Bradfield C.A. Ah receptor signaling pathways. Annu. Rev. Cell Dev. Biol. 1996;12:55–89. doi: 10.1146/annurev.cellbio.12.1.55. [DOI] [PubMed] [Google Scholar]
- 68.Dere E., Forgacs A.L., Zacharewski T.R., Burgoon L.D. Genome-wide computational analysis of dioxin response element location and distribution in the human, mouse, and rat genomes. Chem. Res. Toxicol. 2011;24:494–504. doi: 10.1021/tx100328r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mimura J., Ema M., Sogawa K., Fujii-Kuriyama Y. Identification of a novel mechanism of regulation of Ah (dioxin) receptor function. Genes. Dev. 1999;13:20–25. doi: 10.1101/gad.13.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wong R., Geyer S., Weninger W., Guimberteau J.C., Wong J.K. The dynamic anatomy and patterning of skin. Exp. Dermatol. 2016;25:92–98. doi: 10.1111/exd.12832. [DOI] [PubMed] [Google Scholar]
- 71.Tsuji G., Hashimoto-Hachiya A., Kiyomatsu-Oda M., Takemura M., Ohno F., Ito T., Morino-Koga S., Mitoma C., Nakahara T., Uchi H., et al. Aryl hydrocarbon receptor activation restores filaggrin expression via OVOL1 in atopic dermatitis. Cell Death Dis. 2017;8:e2931. doi: 10.1038/cddis.2017.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jux B., Kadow S., Esser C. Langerhans cell maturation and contact hypersensitivity are impaired in aryl hydrocarbon receptor-null mice. J. Immunol. 2009;182:6709–6717. doi: 10.4049/jimmunol.0713344. [DOI] [PubMed] [Google Scholar]
- 73.Tauchi M., Hida A., Negishi T., Katsuoka F., Noda S., Mimura J., Hosoya T., Yanaka A., Aburatani H., Fujii-Kuriyama Y., et al. Constitutive expression of aryl hydrocarbon receptor in keratinocytes causes inflammatory skin lesions. Mol. Cell Biol. 2005;25:9360–9368. doi: 10.1128/MCB.25.21.9360-9368.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Veldhoen M., Hirota K., Westendorf A.M., Buer J., Dumoutier L., Renauld J.C., Stockinger B. The aryl hydrocarbon receptor links TH17-cell-mediated autoimmunity to environmental toxins. Nature. 2008;453:106–109. doi: 10.1038/nature06881. [DOI] [PubMed] [Google Scholar]
- 75.Ma Q. Influence of light on aryl hydrocarbon receptor signaling and consequences in drug metabolism, physiology and disease. Expert Opin. Drug Metab. Toxicol. 2011;7:1267–1293. doi: 10.1517/17425255.2011.614947. [DOI] [PubMed] [Google Scholar]
- 76.Peng F., Xue C.H., Hwang S.K., Li W.H., Chen Z., Zhang J.Z. Exposure to fine particulate matter associated with senile lentigo in Chinese women: A cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2017;31:355–360. doi: 10.1111/jdv.13834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guo Y.L., Yu M.L., Hsu C.C., Rogan W.J. Chloracne, goiter, arthritis, and anemia after polychlorinated biphenyl poisoning: 14-year follow-Up of the Taiwan Yucheng cohort. Environ. Health Perspect. 1999;107:715–719. doi: 10.1289/ehp.99107715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Caputo R., Monti M., Ermacora E., Carminati G., Gelmetti C., Gianotti R., Gianni E., Puccinelli V. Cutaneous manifestations of tetrachlorodibenzo-p-dioxin in children and adolescents. Follow-up 10 years after the Seveso, Italy, accident. J. Am. Acad. Dermatol. 1988;19:812–819. doi: 10.1016/S0190-9622(88)70238-8. [DOI] [PubMed] [Google Scholar]
- 79.Furue M., Uenotsuchi T., Urabe K., Ishikawa T., Kuwabara M. Overview of Yusho. J. Dermatol. Sci. Suppl. 2005;1:3–10. doi: 10.1016/j.descs.2005.03.002. [DOI] [Google Scholar]
- 80.Mitoma C., Mine Y., Utani A., Imafuku S., Muto M., Akimoto T., Kanekura T., Furue M., Uchi H. Current skin symptoms of Yusho patients exposed to high levels of 2,3,4,7,8-pentachlorinated dibenzofuran and polychlorinated biphenyls in 1968. Chemosphere. 2015;137:45–51. doi: 10.1016/j.chemosphere.2015.03.070. [DOI] [PubMed] [Google Scholar]
- 81.Dandekar A., Mendez R., Zhang K. Cross talk between ER stress, oxidative stress, and inflammation in health and disease. Methods Mol. Biol. 2015;1292:205–214. doi: 10.1007/978-1-4939-2522-3_15. [DOI] [PubMed] [Google Scholar]
- 82.Haarmann-Stemmann T., Bothe H., Abel J. Growth factors, cytokines and their receptors as downstream targets of arylhydrocarbon receptor (AhR) signaling pathways. Biochem. Pharmacol. 2009;77:508–520. doi: 10.1016/j.bcp.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 83.Puga A., Ma C., Marlowe J.L. The aryl hydrocarbon receptor cross-talks with multiple signal transduction pathways. Biochem. Pharmacol. 2009;77:713–722. doi: 10.1016/j.bcp.2008.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tsuji G., Takahara M., Uchi H., Takeuchi S., Mitoma C., Moroi Y., Furue M. An environmental contaminant, benzo(a)pyrene, induces oxidative stress-mediated interleukin-8 production in human keratinocytes via the aryl hydrocarbon receptor signaling pathway. J. Dermatol. Sci. 2011;62:42–49. doi: 10.1016/j.jdermsci.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 85.Fortes C., Mastroeni S., Leffondré K., Sampogna F., Melchi F., Mazzotti E., Pasquini P., Abeni D. Relationship between smoking and the clinical severity of psoriasis. Arch. Dermatol. 2005;141:1580–1584. doi: 10.1001/archderm.141.12.1580. [DOI] [PubMed] [Google Scholar]
- 86.Kohda F., Takahara M., Hachiya A., Takei K., Tsuji G., Yamamura K., Furue M. Decrease of reactive oxygen species and reciprocal increase of nitric oxide in human dermal endothelial cells by Bidens pilosa extract: A possible explanation of its beneficial effect on livedo vasculopathy. J. Derm. Sci. 2013;72:75–77. doi: 10.1016/j.jdermsci.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 87.Han S.G., Han S.S., Toborek M., Hennig B. EGCG protects endothelial cells against PCB 126-induced inflammation through inhibition of AhR and induction of Nrf2-regulated genes. Toxicol. Appl. Pharmacol. 2012;261:181–188. doi: 10.1016/j.taap.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yin Y., Li W., Son Y.O., Sun L., Lu J., Kim D., Wang X., Yao H., Wang L., Pratheeshkumar P., et al. Quercitrin protects skin from UVB-induced oxidative damage. Toxicol. Appl. Pharmacol. 2013;269:89–99. doi: 10.1016/j.taap.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Niestroy J., Barbara A., Herbst K., Rode S., van Liempt M., Roos P.H. Single and concerted effects of benzo[a]pyrene and flavonoids on the AhR and Nrf2-pathway in the human colon carcinoma cell line Caco-2. Toxicol. In Vitro. 2011;25:671–683. doi: 10.1016/j.tiv.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 90.Tan Y.Q., Chiu-Leung L.C., Lin S.M., Leung L.K. The citrus flavonone hesperetin attenuates the nuclear translocation of aryl hydrocarbon receptor. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2018;210:57–64. doi: 10.1016/j.cbpc.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 91.Mohammadi-Bardbori A., Bengtsson J., Rannug U., Rannug A., Wincent E. Quercetin, resveratrol, and curcumin are indirect activators of the aryl hydrocarbon receptor (AHR) Chem. Res. Toxicol. 2012;25:1878–1884. doi: 10.1021/tx300169e. [DOI] [PubMed] [Google Scholar]
- 92.Van den Bogaard E.H., Bergboer J.G., Vonk-Bergers M., van Vlijmen-Willems I.M., Hato S.V., van der Valk P.G., Schröder J.M., Joosten I., Zeeuwen P.L., Schalkwijk J. Coal tar induces AHR-dependent skin barrier repair in atopic dermatitis. J. Clin. Investig. 2013;123:917–927. doi: 10.1172/JCI65642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roelofzen J.H., Aben K.K., Oldenhof U.T., Coenraads P.J., Alkemade H.A., van de Kerkhof P.C., van der Valk P.G., Kiemeney L.A. No increased risk of cancer after coal tar treatment in patients with psoriasis or eczema. J. Investig. Dermatol. 2010;130:953–961. doi: 10.1038/jid.2009.389. [DOI] [PubMed] [Google Scholar]
- 94.Furue M., Ulzii D., Vu Y.H., Tsuji G., Kido-Nakahara M., Nakahara T. Pathogenesis of atopic dermatitis: Current paradigm. Iran. J. Immunol. 2019;16:97–107. doi: 10.22034/IJI.2019.80253. [DOI] [PubMed] [Google Scholar]
- 95.Iwamoto K., Moriwaki M., Miyake R., Hide M. Staphylococcus aureus in atopic dermatitis: Strain-specific cell wall proteins and skin immunity. Allergol. Int. 2019;68:309–315. doi: 10.1016/j.alit.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 96.Yu J., Luo Y., Zhu Z., Zhou Y., Sun L., Gao J., Sun J., Wang G., Yao X., Li W. A tryptophan metabolite of the skin microbiota attenuates inflammation in patients with atopic dermatitis through the aryl hydrocarbon receptor. J. Allergy Clin. Immunol. 2019;143:2108–2119.e12. doi: 10.1016/j.jaci.2018.11.036. [DOI] [PubMed] [Google Scholar]
- 97.Hong C.H., Lee C.H., Yu H.S., Huang S.K. Benzopyrene, a major polyaromatic hydrocarbon in smoke fume, mobilizes Langerhans cells and polarizes Th2/17 responses in epicutaneous protein sensitization through the aryl hydrocarbon receptor. Int. Immunopharmacol. 2016;36:111–117. doi: 10.1016/j.intimp.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 98.Kiyomatsu-Oda M., Uchi H., Morino-Koga S., Furue M. Protective role of 6-formylindolo[3,2-b]carbazole (FICZ), an endogenous ligand for arylhydrocarbon receptor, in chronic mite-induced dermatitis. J. Dermatol. Sci. 2018;90:284–294. doi: 10.1016/j.jdermsci.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 99.Furue M., Hashimoto-Hachiya A., Tsuji G. Aryl hydrocarbon receptor in atopic dermatitis and psoriasis. Int. J. Mol. Sci. 2019;20:5424. doi: 10.3390/ijms20215424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kim H.O., Kim J.H., Chung B.Y., Choi M.G., Park C.W. Increased expression of the aryl hydrocarbon receptor in patients with chronic inflammatory skin diseases. Exp. Dermatol. 2014;23:278–281. doi: 10.1111/exd.12350. [DOI] [PubMed] [Google Scholar]
- 101.Hu Y.Q., Liu P., Mu Z.L., Zhang J.Z. Aryl hydrocarbon receptor expression in serum, peripheral blood mononuclear cells, and skin lesions of patients with atopic dermatitis and its correlation with disease severity. Chin. Med. J. (Engl.) 2020;133:148–153. doi: 10.1097/CM9.0000000000000591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Takei K., Mitoma C., Hashimoto-Hachiya A., Uchi H., Takahara M., Tsuji G., Kido-Nakahara M., Nakahara T., Furue M. Antioxidant soybean tar Glyteer rescues T-helper-mediated downregulation of filaggrin expression via aryl hydrocarbon receptor. J. Dermatol. 2015;42:171–180. doi: 10.1111/1346-8138.12717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Edamitsu T., Taguchi K., Kobayashi E.H., Okuyama R., Yamamoto M. Aryl Hydrocarbon receptor directly regulates artemin gene expression. Mol. Cell Biol. 2019;39:e00190-19. doi: 10.1128/MCB.00190-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hidaka T., Ogawa E., Kobayashi E.H., Suzuki T., Funayama R., Nagashima T., Fujimura T., Aiba S., Nakayama K., Okuyama R., et al. The aryl hydrocarbon receptor AhR links atopic dermatitis and air pollution via induction of the neurotrophic factor artemin. Nat. Immunol. 2017;18:64–73. doi: 10.1038/ni.3614. [DOI] [PubMed] [Google Scholar]
- 105.Morino-Koga S., Uchi H., Mitoma C., Wu Z., Kiyomatsu M., Fuyuno Y., Nagae K., Yasumatsu M., Suico M.A., Kai H., et al. 6-Formylindolo[3,2-b]Carbazole accelerates skin wound healing via activation of ERK, but not aryl hydrocarbon receptor. J. Investig. Dermatol. 2017;137:2217–2226. doi: 10.1016/j.jid.2016.10.050. [DOI] [PubMed] [Google Scholar]
- 106.Takemura M., Nakahara T., Hashimoto-Hachiya A., Furue M., Tsuji G. Glyteer, soybean tar, impairs IL-4/Stat6 signaling in murine bone marrow-derived dendritic cells: The basis of its therapeutic effect on atopic dermatitis. Int. J. Mol. Sci. 2018;19:1169. doi: 10.3390/ijms19041169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Smits J.P.H., Ederveen T.H.A., Rikken G., van den Brink N.J.M., van Vlijmen-Willems I.M.J.J., Boekhorst J., Kamsteeg M., Schalkwijk J., van Hijum S.A.F.T., Zeeuwen P.L.J.M., et al. Targeting the cutaneous microbiota in atopic dermatitis by coal tar via AHR-dependent induction of antimicrobial peptides. J. Investig. Dermatol. 2020;140:415–424.e10. doi: 10.1016/j.jid.2019.06.142. [DOI] [PubMed] [Google Scholar]
- 108.Smith S.H., Jayawickreme C., Rickard D.J., Nicodeme E., Bui T., Simmons C., Coquery C.M., Neil J., Pryor W.M., Mayhew D., et al. Tapinarof is a natural AhR agonist that resolves skin inflammation in mice and humans. J. Investig. Dermatol. 2017;137:2110–2119. doi: 10.1016/j.jid.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 109.Kamata M., Tada Y. Safety of biologics in psoriasis. J. Dermatol. 2018;45:279–286. doi: 10.1111/1346-8138.14096. [DOI] [PubMed] [Google Scholar]
- 110.Cibrian D., Saiz M.L., de la Fuente H., Sánchez-Díaz R., Moreno-Gonzalo O., Jorge I., Ferrarini A., Vázquez J., Punzón C., Fresno M., et al. CD69 controls the uptake of L-tryptophan through LAT1-CD98 and AhR-dependent secretion of IL-22 in psoriasis. Nat. Immunol. 2016;17:985–996. doi: 10.1038/ni.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Qiu J., Heller J.J., Guo X., Chen Z.M., Fish K., Fu Y.X., Zhou L. The aryl hydrocarbon receptor regulates gut immunity through modulation of innate lymphoid cells. Immunity. 2012;36:92–104. doi: 10.1016/j.immuni.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Martin B., Hirota K., Cua D.J., Stockinger B., Veldhoen M. Interleukin-17-producing gammadelta T cells selectively expand in response to pathogen products and environmental signals. Immunity. 2009;31:321–330. doi: 10.1016/j.immuni.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 113.Shimauchi T., Hirakawa S., Suzuki T., Yasuma A., Majima Y., Tatsuno K., Yagi H., Ito T., Tokura Y. Serum interleukin-22 and vascular endothelial growth factor serve as sensitive biomarkers but not as predictors of therapeutic response to biologics in patients with psoriasis. J. Dermatol. 2013;40:805–812. doi: 10.1111/1346-8138.12248. [DOI] [PubMed] [Google Scholar]
- 114.Wolk K., Witte E., Wallace E., Döcke W.D., Kunz S., Asadullah K., Volk H.D., Sterry W., Sabat R. IL-22 regulates the expression of genes responsible for antimicrobial defense, cellular differentiation, and mobility in keratinocytes: A potential role in psoriasis. Eur. J. Immunol. 2006;36:1309–1323. doi: 10.1002/eji.200535503. [DOI] [PubMed] [Google Scholar]
- 115.Cochez P.M., Michiels C., Hendrickx E., Van Belle A.B., Lemaire M.M., Dauguet N., Warnier G., de Heusch M., Togbe D., Ryffel B., et al. AhR modulates the IL-22-producing cell proliferation/recruitment in imiquimod-induced psoriasis mouse model. Eur. J. Immunol. 2016;46:1449–1459. doi: 10.1002/eji.201546070. [DOI] [PubMed] [Google Scholar]
- 116.Wolk K., Haugen H.S., Xu W., Witte E., Waggie K., Anderson M., Vom Baur E., Witte K., Warszawska K., Philipp S., et al. IL-22 and IL-20 are key mediators of the epidermal alterations in psoriasis while IL-17 and IFN-gamma are not. J. Mol. Med. (Berl.) 2009;87:523–536. doi: 10.1007/s00109-009-0457-0. [DOI] [PubMed] [Google Scholar]
- 117.di Meglio P., Duarte J.H., Ahlfors H., Owens N.D.L., Li Y., Villanova F., Tosi I., Hirota K., Nestle F.O., Mrowietz U., et al. Activation of the aryl hydrocarbon receptor dampens the severity of inflammatory skin conditions. Immunity. 2014;40:989–1001. doi: 10.1016/j.immuni.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Goldsmith Z.G., Dhanasekaran D.N. G protein regulation of MAPK networks. Oncogene. 2007;26:3122–3142. doi: 10.1038/sj.onc.1210407. [DOI] [PubMed] [Google Scholar]
- 119.Walczak K., Turski W.A., Rajtar G. Kynurenic acid inhibits colon cancer proliferation in vitro: Effects on signaling pathways. Amino Acids. 2014;46:2393–2401. doi: 10.1007/s00726-014-1790-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Beránek M., Fiala Z., Kremláček J., Andrýs C., Krejsek J., Hamáková K., Palička V., Borská L. Serum levels of aryl hydrocarbon receptor, cytochromes P450 1A1 and 1B1 in patients with exacerbated psoriasis vulgaris. Folia. Biol. (Praha.) 2018;64:97–102. doi: 10.14712/fb2018064030097. [DOI] [PubMed] [Google Scholar]
- 121.Tian S., Krueger J.G., Li K., Jabbari A., Brodmerkel C., Lowes M.A., Suárez-Fariñas M. Meta-analysis derived (MAD) transcriptome of psoriasis defines the “core” pathogenesis of disease. PLoS ONE. 2012;7:e44274. doi: 10.1371/journal.pone.0044274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gudjonsson J.E., Ding J., Johnston A., Tejasvi T., Guzman A.M., Nair R.P., Voorhees J.J., Abecasis G.R., Elder J.T. Assessment of the psoriatic transcriptome in a large sample: Additional regulated genes and comparisons with in vitro models. J. Investig. Dermatol. 2010;130:1829–1840. doi: 10.1038/jid.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.DiNatale B.C., Murray I.A., Schroeder J.C., Flaveny C.A., Lahoti T.S., Laurenzana E.M., Omiecinski C.J., Perdew G.H. Kynurenic acid is a potent endogenous aryl hydrocarbon receptor ligand that synergistically induces interleukin-6 in the presence of inflammatory signaling. Toxicol. Sci. 2010;115:89–97. doi: 10.1093/toxsci/kfq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Opitz C.A., Litzenburger U.M., Sahm F., Ott M., Tritschler I., Trump S., Schumacher T., Jestaedt L., Schrenk D., Weller M., et al. An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature. 2011;478:197–203. doi: 10.1038/nature10491. [DOI] [PubMed] [Google Scholar]
- 125.Wei Y.D., Bergander L., Rannug U., Rannug A. Regulation of CYP1A1 transcription via the metabolism of the tryptophan-derived 6-formylindolo[3,2-b]carbazole. Arch. Biochem. Biophys. 2000;383:99–107. doi: 10.1006/abbi.2000.2037. [DOI] [PubMed] [Google Scholar]
- 126.di Meglio P., Perera G.K., Nestle F.O. The multitasking organ: Recent insights into skin immune function. Immunity. 2011;35:857–869. doi: 10.1016/j.immuni.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 127.van der Fits L., Mourits S., Voerman J.S., Kant M., Boon L., Laman J.D., Cornelissen F., Mus A.M., Florencia E., Prens E.P., et al. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J. Immunol. 2009;182:5836–5845. doi: 10.4049/jimmunol.0802999. [DOI] [PubMed] [Google Scholar]
- 128.Zhu Z., Chen J., Lin Y., Zhang C., Li W., Qiao H., Fu M., Dang E., Wang G. Aryl hydrocarbon receptor in cutaneous vascular endothelial cells restricts psoriasis development by negatively regulating neutrophil recruitment. J. Investig. Dermatol. 2020;140:1233–1243.e9. doi: 10.1016/j.jid.2019.11.022. [DOI] [PubMed] [Google Scholar]
- 129.Nakamura M., Ueda Y., Hayashi M., Kato H., Furuhashi T., Morita A. Tobacco smoke-induced skin pigmentation is mediated by the aryl hydrocarbon receptor. Exp. Dermatol. 2013;22:556–558. doi: 10.1111/exd.12170. [DOI] [PubMed] [Google Scholar]
- 130.Nguyen N.T., Fisher D.E. MITF and UV responses in skin: From pigmentation to addiction. Pigment Cell Melanoma Res. 2019;32:224–236. doi: 10.1111/pcmr.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Luecke S., Backlund M., Jux B., Esser C., Krutmann J., Rannug A. The aryl hydrocarbon receptor (AHR), a novel regulator of human melanogenesis. Pigment Cell Melanoma Res. 2010;23:828–833. doi: 10.1111/j.1755-148X.2010.00762.x. [DOI] [PubMed] [Google Scholar]
- 132.Abbas S., Alam S., Singh K.P., Kumar M., Gupta S.K., Ansari K.M. Aryl hydrocarbon receptor activation contributes to benzanthrone-induced hyperpigmentation via modulation of melanogenic signaling pathways. Chem. Res. Toxicol. 2017;30:625–634. doi: 10.1021/acs.chemrestox.6b00364. [DOI] [PubMed] [Google Scholar]
- 133.Rashighi M., Harris J.E. Vitiligo pathogenesis and emerging treatments. Dermatol. Clin. 2017;35:257–265. doi: 10.1016/j.det.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rekik R., Ben Hmid A., Lajnef C., Zamali I., Zaraa I., Ben Ahmed M. Aryl hydrocarbon receptor (AhR) transcription is decreased in skin of vitiligo patients. Int. J. Dermatol. 2017;56:1509–1512. doi: 10.1111/ijd.13761. [DOI] [PubMed] [Google Scholar]
- 135.Haarmann-Stemmann T., Esser C., Krutmann J. The janus-faced role of aryl hydrocarbon receptor signaling in the skin: Consequences for prevention and treatment of skin disorders. J. Investig. Dermatol. 2015;135:2572–2576. doi: 10.1038/jid.2015.285. [DOI] [PubMed] [Google Scholar]
- 136.Dwivedi M., Kemp E.H., Laddha N.C., Mansuri M.S., Weetman A.P., Begum R. Regulatory T cells in vitiligo: Implications for pathogenesis and therapeutics. Autoimmun. Rev. 2015;14:49–56. doi: 10.1016/j.autrev.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 137.Ahmed M.B., Zaraa I., Rekik R., Elbeldi-Ferchiou A., Kourda N., Belhadj Hmida N., Abdeladhim M., Karoui O., Ben Osman A., Mokni M., et al. Functional defects of peripheral regulatory T lymphocytes in patients with progressive vitiligo. Pigment Cell Melanoma Res. 2012;25:99–109. doi: 10.1111/j.1755-148X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- 138.Taher Z.A., Lauzon G., Maguiness S., Dytoc M.T. Analysis of interleukin-10 levels in lesions of vitiligo following treatment with topical tacrolimus. Br. J. Dermatol. 2009;161:654–659. doi: 10.1111/j.1365-2133.2009.09217.x. [DOI] [PubMed] [Google Scholar]
- 139.Wang X., Li K., Liu L., Shi Q., Song P., Jian Z., Guo S., Wang G., Li C., Gao T. AHR promoter variant modulates its transcription and downstream effectors by allele-specific AHR-SP1 interaction functioning as a genetic marker for vitiligo. Sci. Rep. 2015;5:13542. doi: 10.1038/srep13542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Eguchi H., Hayashi S.I., Watanabe J., Gotoh O., Kawajiri K. Molecular cloning of the human ah receptor gene promoter. Biochem. Biophys. Res. Commun. 1994;203:615–622. doi: 10.1006/bbrc.1994.2227. [DOI] [PubMed] [Google Scholar]
- 141.Behfarjam F., Jadali Z. Vitiligo patients show significant up-regulation of aryl hydrocarbon receptor transcription factor. An. Bras. Dermatol. 2018;93:302–303. doi: 10.1590/abd1806-4841.20187183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Singh R.K., Lee K.M., Vujkovic-Cvijin I., Ucmak D., Farahnik B., Abrouk M., Nakamura M., Zhu T.H., Bhutani T., Wei M., et al. The role of IL-17 in vitiligo: A review. Autoimmun. Rev. 2016;15:397–404. doi: 10.1016/j.autrev.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schallreuter K.U., Salem M.A., Gibbons N.C., Martinez A., Slominski R., Lüdemann J., Rokos H. Blunted epidermal L-tryptophan metabolism in vitiligo affects immune response and ROS scavenging by Fenton chemistry, part 1: Epidermal H2O2/ONOO(-)-mediated stress abrogates tryptophan hydroxylase and dopa decarboxylase activities, leading to low serotonin and melatonin levels. FASEB J. 2012;26:2457–2470. doi: 10.1096/fj.11-197137. [DOI] [PubMed] [Google Scholar]
- 144.Saurat J.H., Kaya G., Saxer-Sekulic N., Pardo B., Becker M., Fontao L., Mottu F., Carraux P., Pham X.C., Barde C., et al. The cutaneous lesions of dioxin exposure: Lessons from the poisoning of Victor Yushchenko. Toxicol. Sci. 2012;125:310–317. doi: 10.1093/toxsci/kfr223. [DOI] [PubMed] [Google Scholar]
- 145.Furue M., Tsuji G. Chloracne and hyperpigmentation caused by exposure to hazardous aryl hydrocarbon receptor ligands. Int. J. Environ. Res. Public Health. 2019;16:4864. doi: 10.3390/ijerph16234864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Panteleyev A.A., Bickers D.R. Dioxin-induced chloracne--reconstructing the cellular and molecular mechanisms of a classic environmental disease. Exp. Dermatol. 2006;15:705–730. doi: 10.1111/j.1600-0625.2006.00476.x. [DOI] [PubMed] [Google Scholar]
- 147.Suskind R.R. Chloracne, “the hallmark of dioxin intoxication”. Scand. J. Work Environ. Health. 1985;11:165–171. doi: 10.5271/sjweh.2240. [DOI] [PubMed] [Google Scholar]
- 148.Van den Bogaard E.H., Podolsky M.A., Smits J.P., Cui X., John C., Gowda K., Desai D., Amin S.G., Schalkwijk J., Perdew G.H., et al. Genetic and pharmacological analysis identifies a physiological role for the AHR in epidermal differentiation. J. Investig. Dermatol. 2015;135:1320–1328. doi: 10.1038/jid.2015.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Fernandez-Salguero P.M., Ward J.M., Sundberg J.P., Gonzalez F.J. Lesions of aryl-hydrocarbon receptor-deficient mice. Vet. Pathol. 1997;34:605–614. doi: 10.1177/030098589703400609. [DOI] [PubMed] [Google Scholar]
- 150.Morokuma S., Tsukimori K., Hori T., Kato K., Furue M. The vernix caseosa is the main site of dioxin excretion in the human foetus. Sci. Rep. 2017;7:739. doi: 10.1038/s41598-017-00863-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Hu T., Wang D., Yu Q., Li L., Mo X., Pan Z., Zouboulis C.C., Peng L., Xia L., Ju Q. Aryl hydrocarbon receptor negatively regulates lipid synthesis and involves in cell differentiation of SZ95 sebocytes in vitro. Chem. Biol. Interact. 2016;258:52–58. doi: 10.1016/j.cbi.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 152.Ju Q., Fimmel S., Hinz N., Stahlmann R., Xia L., Zouboulis C.C. 2,3,7,8-Tetrachlorodibenzo-p-dioxin alters sebaceous gland cell differentiation in vitro. Exp. Dermatol. 2011;20:320–325. doi: 10.1111/j.1600-0625.2010.01204.x. [DOI] [PubMed] [Google Scholar]
- 153.Liu Q., Wu J., Song J., Liang P., Zheng K., Xiao G., Liu L., Zouboulis C.C., Lei T. Particulate matter 2.5 regulates lipid synthesis and inflammatory cytokine production in human SZ95 sebocytes. Int. J. Mol. Med. 2017;40:1029–1036. doi: 10.3892/ijmm.2017.3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hu T., Pan Z., Yu Q., Mo X., Song N., Yan M., Zouboulis C.C., Xia L., Ju Q. Benzo(a)pyrene induces interleukin (IL)-6 production and reduces lipid synthesis in human SZ95 sebocytes via the aryl hydrocarbon receptor signaling pathway. Environ. Toxicol. Pharmacol. 2016;43:54–60. doi: 10.1016/j.etap.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 155.Muku G.E., Blazanin N., Dong F., Smith P.B., Thiboutot D., Gowda K., Amin S., Murray I.A., Perdew G.H. Selective Ah receptor ligands mediate enhanced SREBP1 proteolysis to restrict lipogenesis in sebocytes. Toxicol. Sci. 2019;171:146–158. doi: 10.1093/toxsci/kfz140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Liu J., Zhang C.M., Coenraads P.J., Ji Z.Y., Chen X., Dong L., Ma X.M., Han W., Tang N.J. Abnormal expression of MAPK, EGFR, CK17 and TGk in the skin lesions of chloracne patients exposed to dioxins. Toxicol. Lett. 2011;201:230–234. doi: 10.1016/j.toxlet.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 157.Sutter C.H., Yin H., Li Y., Mammen J.S., Bodreddigari S., Stevens G., Cole J.A., Sutter T.R. EGF receptor signaling blocks aryl hydrocarbon receptor-mediated transcription and cell differentiation in human epidermal keratinocytes. Proc. Natl. Acad. Sci. USA. 2009;106:4266–4271. doi: 10.1073/pnas.0900874106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kypriotou M., Huber M., Hohl D. The human epidermal differentiation complex: Cornified envelope precursors, S100 proteins and the ‘fused genes’ family. Exp. Dermatol. 2012;21:643–649. doi: 10.1111/j.1600-0625.2012.01472.x. [DOI] [PubMed] [Google Scholar]
- 159.Loertscher J.A., Sattler C.A., Allen-Hoffmann B.L. 2,3,7,8-Tetrachlorodibenzo-p-dioxin alters the differentiation pattern of human keratinocytes in organotypic culture. Toxicol. Appl. Pharmacol. 2001;175:121–129. doi: 10.1006/taap.2001.9202. [DOI] [PubMed] [Google Scholar]
- 160.Muenyi C.S., Carrion S.L., Jones L.A., Kennedy L.H., Slominski A.T., Sutter C.H., Sutter T.R. Effects of in utero exposure of C57BL/6J mice to 2,3,7,8-tetrachlorodibenzo-p-dioxin on epidermal permeability barrier development and function. Environ. Health Perspect. 2014;122:1052–1058. doi: 10.1289/ehp.1308045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Panteleyev A.A., Thiel R., Wanner R., Zhang J., Roumak V.S., Paus R., Neubert D., Henz B.M., Rosenbach T. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCCD) affects keratin 1 and keratin 17 gene expression and differentially induces keratinization in hairless mouse skin. J. Investig. Dermatol. 1997;108:330–335. doi: 10.1111/1523-1747.ep12286478. [DOI] [PubMed] [Google Scholar]
- 162.Kennedy L.H., Sutter C.H., Carrion S.L., Tran Q.T., Bodreddigari S., Kensicki E., Mohney R.P., Sutter T.R. 2,3,7,8-Tetrachlorodibenzo-p-dioxin-mediated production of reactive oxygen species is an essential step in the mechanism of action to accelerate human keratinocyte differentiation. Toxicol. Sci. 2013;132:235–249. doi: 10.1093/toxsci/kfs325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Pohjanvirta R. The AH Receptor in Biology and Toxicology. John Wiley & Sons; New York, NY, USA: 2012. pp. 485–497. [DOI] [Google Scholar]
- 164.Furness S.G., Lees M.J., Whitelaw M.L. The dioxin (aryl hydrocarbon) receptor as a model for adaptive responses of bHLH/PAS transcription factors. FEBS Lett. 2007;581:3616–3625. doi: 10.1016/j.febslet.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 165.Contador-Troca M., Alvarez-Barrientos A., Barrasa E., Rico-Leo E.M., Catalina-Fernández I., Menacho-Márquez M., Bustelo X.R., García-Borrón J.C., Gómez-Durán A., Sáenz-Santamaría J., et al. The dioxin receptor has tumor suppressor activity in melanoma growth and metastasis. Carcinogenesis. 2013;34:2683–2693. doi: 10.1093/carcin/bgt248. [DOI] [PubMed] [Google Scholar]
- 166.Aziz M.H., Reagan-Shaw S., Wu J., Longley B.J., Ahmad N. Chemoprevention of skin cancer by grape constituent resveratrol: Relevance to human disease? FASEB J. 2005;19:1193–1195. doi: 10.1096/fj.04-3582fje. [DOI] [PubMed] [Google Scholar]
- 167.Gawkrodger D.J. Occupational skin cancers. Occup. Med. (Lond.) 2004;54:458–463. doi: 10.1093/occmed/kqh098. [DOI] [PubMed] [Google Scholar]
- 168.Richard G., Puisieux A., Caramel J. Antagonistic functions of EMT-inducers in melanoma development: Implications for cancer cell plasticity. Cancer Cell Microenviron. 2014:e61. doi: 10.14800/ccm.61. [DOI] [Google Scholar]
- 169.Kostyuk V.A., Potapovich A.I., Lulli D., Stancato A., De Luca C., Pastore S., Korkina L. Modulation of human keratinocyte responses to solar UV by plant polyphenols as a basis for chemoprevention of non-melanoma skin cancers. Curr. Med. Chem. 2013;20:869–879. [PubMed] [Google Scholar]
- 170.Rogers H.W., Weinstock M.A., Feldman S.R., Coldiron B.M. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015;151:1081–1086. doi: 10.1001/jamadermatol.2015.1187. [DOI] [PubMed] [Google Scholar]
- 171.Chahal H.S., Lin Y., Ransohoff K.J., Hinds D.A., Wu W., Dai H.J., Qureshi A.A., Li W.Q., Kraft P., Tang J.Y., et al. Genome-wide association study identifies novel susceptibility loci for cutaneous squamous cell carcinoma. Nat. Commun. 2016;7:12048. doi: 10.1038/ncomms12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Vogeley C., Esser C., Tüting T., Krutmann J., Haarmann-Stemmann T. Role of the aryl hydrocarbon receptor in environmentally induced skin aging and skin carcinogenesis. Int. J. Mol. Sci. 2019;20:6005. doi: 10.3390/ijms20236005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kalmes M., Hennen J., Clemens J., Blömeke B. Impact of aryl hydrocarbon receptor (AhR) knockdown on cell cycle progression in human HaCaT keratinocytes. Biol. Chem. 2011;392:643–651. doi: 10.1515/bc.2011.067. [DOI] [PubMed] [Google Scholar]
- 174.Pollet M., Shaik S., Mescher M., Krutmann J., Haarmann-Stemmann T. The AHR represses nucleotide excision repair and apoptosis and contributes to UV-induced skin carcinogenesis. Cell Death Differ. 2018;25:1823–1836. doi: 10.1038/s41418-018-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.O’Donnell E.F., Kopparapu P.R., Koch D.C., Jang H.S., Phillips J.L., Tanguay R.L., Kerkvliet N.I., Kolluri S.K. The aryl hydrocarbon receptor mediates leflunomide-induced growth inhibition of melanoma cells. PLoS ONE. 2012;7:e40926. doi: 10.1371/journal.pone.0040926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Roman A.C., Carvajal-Gonzalez J.M., Rico-Leo E.M., Fernandez-Salguero P.M. Dioxin receptor deficiency impairs angiogenesis by a mechanism involving VEGF-A depletion in the endothelium and transforming growth factor-beta overexpression in the stroma. J. Biol. Chem. 2009;284:25135–25148. doi: 10.1074/jbc.M109.013292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Villano C.M., Murphy K.A., Akintobi A., White L.A. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) induces matrix metalloproteinase (MMP) expression and invasion in A2058 melanoma cells. Toxicol. Appl. Pharmacol. 2006;210:212–224. doi: 10.1016/j.taap.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 178.Helferich W.G., Denison M.S. Ultraviolet photoproducts of tryptophan can act as dioxin agonists. Mol. Pharmacol. 1991;40:674–678. [PubMed] [Google Scholar]
- 179.Walczak K., Wnorowski A., Turski W.A., Plech T. Kynurenic acid and cancer: Facts and controversies. Cell Mol. Life Sci. 2020;77:1531–1550. doi: 10.1007/s00018-019-03332-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Cella M., Colonna M. Aryl hydrocarbon receptor: Linking environment to immunity. Semin. Immunol. 2015;27:310–314. doi: 10.1016/j.smim.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Turski M.P., Turska M., Zgrajka W., Bartnik M., Kocki T., Turski W.A. Distribution, synthesis, and absorption of kynurenic acid in plants. Planta Med. 2011;77:858–864. doi: 10.1055/s-0030-1250604. [DOI] [PubMed] [Google Scholar]
- 182.Turski M.P., Turska M., Zgrajka W., Kuc D., Turski W.A. Presence of kynurenic acid in food and honeybee products. Amino Acids. 2009;36:75–80. doi: 10.1007/s00726-008-0031-z. [DOI] [PubMed] [Google Scholar]
- 183.Jönsson M.E., Franks D.G., Woodin B.R., Jenny M.J., Garrick R.A., Behrendt L., Hahn M.E., Stegeman J.J. The tryptophan photoproduct 6-formylindolo[3,2-b]carbazole (FICZ) binds multiple AHRs and induces multiple CYP1 genes via AHR2 in zebrafish. Chem. Biol. Interact. 2009;181:447–454. doi: 10.1016/j.cbi.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Park S.L., Justiniano R., Williams J.D., Cabello C.M., Qiao S., Wondrak G.T. The tryptophan-derived endogenous aryl hydrocarbon receptor ligand 6-Formylindolo[3,2-b]Carbazole is a nanomolar UVA photosensitizer in epidermal keratinocytes. J. Investig. Dermatol. 2015;135:1649–1658. doi: 10.1038/jid.2014.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Mukhtar H., DelTito B.J., Jr., Matgouranis P.M., Das M., Asokan P., Bickers D.R. Additive effects of ultraviolet B and crude coal tar on cutaneous carcinogen metabolism: Possible relevance to the tumorigenicity of the Goeckerman regimen. J. Investig. Dermatol. 1986;87:348–353. doi: 10.1111/1523-1747.ep12524446. [DOI] [PubMed] [Google Scholar]
- 186.Katiyar S.K., Matsui M.S., Mukhtar H. Ultraviolet-B exposure of human skin induces cytochromes P450 1A1 and 1B1. J. Investig. Dermatol. 2000;114:328–333. doi: 10.1046/j.1523-1747.2000.00876.x. [DOI] [PubMed] [Google Scholar]
- 187.Rannug A., Fritsche E. The aryl hydrocarbon receptor and light. Biol. Chem. 2006;387:1149–1157. doi: 10.1515/BC.2006.143. [DOI] [PubMed] [Google Scholar]
- 188.Murai M., Tsuji G., Hashimoto-Hachiya A., Kawakami Y., Furue M., Mitoma C. An endogenous tryptophan photo-product, FICZ, is potentially involved in photo-aging by reducing TGF-β-regulated collagen homeostasis. J. Dermatol. Sci. 2018;89:19–26. doi: 10.1016/j.jdermsci.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 189.Mengoni M., Braun A.D., Gaffal E., Tüting T. The aryl hydrocarbon receptor promotes inflammation-induced dedifferentiation and systemic metastatic spread of melanoma cells. Int. J. Cancer. 2020;147:2902–2913. doi: 10.1002/ijc.33252. [DOI] [PubMed] [Google Scholar]
- 190.Ikuta T., Kawajiri K. Zinc finger transcription factor Slug is a novel target gene of aryl hydrocarbon receptor. Exp. Cell Res. 2006;312:3585–3594. doi: 10.1016/j.yexcr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 191.Mezrich J.D., Fechner J.H., Zhang X., Johnson B.P., Burlingham W.J., Bradfield C.A. An interaction between kynurenine and the aryl hydrocarbon receptor can generate regulatory T cells. J. Immunol. 2010;185:3190–3198. doi: 10.4049/jimmunol.0903670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Bessede A., Gargaro M., Pallotta M.T., Matino D., Servillo G., Brunacci C., Bicciato S., Mazza E.M., Macchiarulo A., Vacca C., et al. Aryl hydrocarbon receptor control of a disease tolerance defence pathway. Nature. 2014;511:184–190. doi: 10.1038/nature13323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Nuti R., Gargaro M., Matino D., Dolciami D., Grohmann U., Puccetti P., Fallarino F., Macchiarulo A. Ligand binding and functional selectivity of L-tryptophan metabolites at the mouse aryl hydrocarbon receptor (mAhR) J. Chem. Inf. Model. 2014;54:3373–3383. doi: 10.1021/ci5005459. [DOI] [PubMed] [Google Scholar]
- 194.Pilotte L., Larrieu P., Stroobant V., Colau D., Dolusic E., Frédérick R., De Plaen E., Uyttenhove C., Wouters J., Masereel B., et al. Reversal of tumoral immune resistance by inhibition of tryptophan 2,3-dioxygenase. Proc. Natl. Acad. Sci. USA. 2012;109:2497–2502. doi: 10.1073/pnas.1113873109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Litzenburger U.M., Opitz C.A., Sahm F., Rauschenbach K.J., Trump S., Winter M., Ott M., Ochs K., Lutz C., Liu X., et al. Constitutive IDO expression in human cancer is sustained by an autocrine signaling loop involving IL-6, STAT3 and the AHR. Oncotarget. 2014;5:1038–1051. doi: 10.18632/oncotarget.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wirthgen E., Hoeflich A. Endotoxin-induced tryptophan degradation along the kynurenine pathway: The role of indolamine 2,3-Dioxygenase and aryl hydrocarbon receptor-mediated immunosuppressive effects in endotoxin tolerance and cancer and its implications for immunoparalysis. J. Amino Acids. 2015;2015:973548. doi: 10.1155/2015/973548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Zhang S., Patel A., Chu C., Jiang W., Wang L., Welty S.E., Moorthy B., Shivanna B. Aryl hydrocarbon receptor is necessary to protect fetal human pulmonary microvascular endothelial cells against hyperoxic injury: Mechanistic roles of antioxidant enzymes and RelB. Toxicol. Appl. Pharmacol. 2015;286:92–101. doi: 10.1016/j.taap.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Baglole C.J., Maggirwar S.B., Gasiewicz T.A., Thatcher T.H., Phipps R.P., Sime P.J. The aryl hydrocarbon receptor attenuates tobacco smoke-induced cyclooxygenase-2 and prostaglandin production in lung fibroblasts through regulation of the NF-kappaB family member RelB. J. Biol. Chem. 2008;283:28944–28957. doi: 10.1074/jbc.M800685200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Sekine H., Mimura J., Oshima M., Okawa H., Kanno J., Igarashi K., Gonzalez F.J., Ikuta T., Kawajiri K., Fujii-Kuriyama Y. Hypersensitivity of aryl hydrocarbon receptor-deficient mice to lipopolysaccharide-induced septic shock. Mol. Cell. Biol. 2009;29:6391–6400. doi: 10.1128/MCB.00337-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Murray I.A., Patterson A.D., Perdew G.H. Aryl hydrocarbon receptor ligands in cancer: Friend and foe. Nat. Rev. Cancer. 2014;14:801–814. doi: 10.1038/nrc3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Walczak K., Turski W.A., Rzeski W. Kynurenic acid enhances expression of p21 Waf1/Cip1 in colon cancer HT-29 cells. Pharmacol. Rep. 2012;64:745–750. doi: 10.1016/S1734-1140(12)70870-8. [DOI] [PubMed] [Google Scholar]
- 202.Walczak K., Langner E., Makuch-Kocka A., Szelest M., Szalast K., Marciniak S., Plech T. Effect of tryptophan-derived Ahr ligands, kynurenine, kynurenic acid and FICZ, on proliferation, cell cycle regulation and cell death of melanoma cells-in vitro studies. Int. J. Mol. Sci. 2020;21:7946. doi: 10.3390/ijms21217946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Turski M.P., Turska M., Paluszkiewicz P., Parada-Turska J., Oxenkrug G.F. Kynurenic Acid in the digestive system-new facts, new challenges. Int. J. Tryptophan. Res. 2013;6:47–55. doi: 10.4137/IJTR.S12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Swanbeck G., Wennersten G., Nilsson R. Participation of singlet state excited oxygen in photohemolysis induced by kynurenic acid. Acta Derm. Venereol. 1974;54:433–436. [PubMed] [Google Scholar]
- 205.Wennersten G., Brunk U. Cellular aspects of phototoxic reactions induced by kynurenic acid. I. Establishment of an experimental model utilizing in vitro cultivated cells. Acta Derm. Venereol. 1977;57:201–209. [PubMed] [Google Scholar]
- 206.Vogel C.F.A., Ishihara Y., Campbell C.E., Kado S.Y., Nguyen-Chi A., Sweeney C., Pollet M., Haarmann-Stemmann T., Tuscano J.M. A protective role of aryl hydrocarbon receptor repressor in inflammation and tumor growth. Cancers (Basel) 2019;11:589. doi: 10.3390/cancers11050589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Tang Z., Kang B., Li C., Chen T., Zhang Z. GEPIA2: An enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019;47(W1):W556–W560. doi: 10.1093/nar/gkz430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Théate I., van Baren N., Pilotte L., Moulin P., Larrieu P., Renauld J.C., Hervé C., Gutierrez-Roelens I., Marbaix E., Sempoux C., et al. Extensive profiling of the expression of the indoleamine 2,3-dioxygenase 1 protein in normal and tumoral human tissues. Cancer Immunol. Res. 2015;3:161–172. doi: 10.1158/2326-6066.CIR-14-0137. [DOI] [PubMed] [Google Scholar]
- 209.Labadie B.W., Bao R., Luke J.J. Reimagining IDO Pathway inhibition in cancer immunotherapy via downstream focus on the tryptophan-kynurenine-aryl hydrocarbon axis. Clin. Cancer Res. 2019;25:1462–1471. doi: 10.1158/1078-0432.CCR-18-2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Vlachos C., Schulte B.M., Magiatis P., Adema G.J., Gaitanis G. Malassezia-derived indoles activate the aryl hydrocarbon receptor and inhibit Toll-like receptor-induced maturation in monocyte-derived dendritic cells. Br. J. Dermatol. 2012;167:496–505. doi: 10.1111/j.1365-2133.2012.11014.x. [DOI] [PubMed] [Google Scholar]
- 211.Gaitanis G., Velegraki A., Magiatis P., Pappas P., Bassukas I.D. Could Malassezia yeasts be implicated in skin carcinogenesis through the production of aryl-hydrocarbon receptor ligands? Med. Hypotheses. 2011;77:47–51. doi: 10.1016/j.mehy.2011.03.020. [DOI] [PubMed] [Google Scholar]