Abstract
In migraine pain, cannabis has a promising analgesic action, which, however, is associated with side psychotropic effects. To overcome these adverse effects of exogenous cannabinoids, we propose migraine pain relief via activation of the endogenous cannabinoid system (ECS) by inhibiting enzymes degrading endocannabinoids. To provide a functional platform for such purpose in the peripheral and central parts of the rat nociceptive system relevant to migraine, we measured by activity-based protein profiling (ABPP) the activity of the main endocannabinoid-hydrolases, monoacylglycerol lipase (MAGL) and fatty acid amide hydrolase (FAAH). We found that in trigeminal ganglia, the MAGL activity was nine-fold higher than that of FAAH. MAGL activity exceeded FAAH activity also in DRG, spinal cord and brainstem. However, activities of MAGL and FAAH were comparably high in the cerebellum and cerebral cortex implicated in migraine aura. MAGL and FAAH activities were identified and blocked by the selective and potent inhibitors JJKK-048/KML29 and JZP327A, respectively. The high MAGL activity in trigeminal ganglia implicated in the generation of nociceptive signals suggests this part of ECS as a priority target for blocking peripheral mechanisms of migraine pain. In the CNS, both MAGL and FAAH represent potential targets for attenuation of migraine-related enhanced cortical excitability and pain transmission.
Keywords: migraine, pain, endocannabinoid, serine hydrolases, analgesia
1. Introduction
Migraine is a widespread neurovascular disabling disorder affecting up to 15% of the worldwide population and is typically characterized by one-sided throbbing long-lasting moderate or severe pain [1,2]. Migraine is associated with multiple psychiatric comorbidities such as anxiety, depression and panic disorders [3,4,5,6]. Despite this clear association, the CNS neuronal centers underlying the link between migraine and the comorbid psychiatric conditions remains to be determined. Migraine has a clear trend to chronicization, namely, a progression from episodic to chronic migraine [7]. This trend might be due to excessive use of analgesic including opioids drugs leading to condition known as a ’medication overuse headache’ [8]. Although cannabis can help in opioid detoxification [9], its abuse can trigger psychiatric risk factors for migraine such as anxiety and depression, which are common among cannabis users [10] and associated with the chronicization of migraine [4,11]. Also, the post-traumatic stress disorder has been shown to be associated with migraine and drug abuse [12]. The main complaint of migraine patients is long-lasting pulsating pain, which is intractable in many cases thus leading to chronic stress and depression [3,13,14]. Known from ancient times [15], cannabinoids emerged recently as a promising analgesic approach to treat migraine pain [16,17,18]. In particular, cannabis, now legalized in many countries, has shown a therapeutic effect in migraine [16,19]. Indeed, marijuana had been used in the past for medicinal purposes to relieve headaches [20]. However, the exocannabinoids, exogenous compounds from cannabis and marijuana, which bind and activate cannabinoid receptors, have many adverse psychotropic and other unwanted effects [21]. Psychotropicity may be as detrimental as the migraine condition itself for conducting everyday life. Therefore, an alternative approach for migraine pain therapy might be based on the selective enhancement of endogenous cannabinoids (endoCB), which are naturally generated in the nociceptive system in the body [22]. The Endocannabinoid System (ECS) is composed of endoCBs, a class of unique lipidic mediators including 2-arachidonoyl glycerol (2-AG) and anandamide (N-arachidonoyl ethanolamine, AEA), the metabolic enzymes for their synthesis and degradation along with the two G protein-coupled cannabinoid receptors (CB1 and CB2) [23]. The enhancement of endoCBs-activities is primarily important for conditions such as Clinical Endocannabinoid Deficiency (CECD), which was already proposed as a complication for several treatment-resistant types of pain, including migraine [16,24].
There are two major types of migraine, migraine with and without aura [25]. Whether the mechanisms initiating migraine attack are located in the CNS or in the periphery remains debated. The peripheral ‘trigeminovascular system’ (TGVS) is composed by meningeal nerves, vessels and immune cells. In migraine with aura, a plausible early event is the cortical spreading depolarization (CSD), which leads to global depolarization of neurons and glial cells [26,27]. The depolarization slowly propagates along the cortical areas and, leading to activation of the TGVS [26,27]. In the absence of CSD, for instance, in episodic migraine without aura, the mechanisms triggering migraine are not still clearly established. However, it has been shown that the potential trigger for migraine attack is psychogenic stress, which can precipitate or worsen migraine [28,29]. Such stress can promote the release of corticotropin-releasing hormone [29], directly activating meningeal mast cells that are closely interacting with the dural nerves in the TGVS [30,31,32]. Alternatively, stress can provoke sleep disturbances, also known to trigger migraine episodes [33,34]. Among other key mechanisms initiating migraine attack is the release of the neuropeptides such as calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating peptide (PACAP) [35,36,37]. In most migraine cases, there is an involvement of CNS centers, including the brainstem nuclei and hypothalamus [38].
Taken together, these data suggest that migraine pain may be regulated at multiple levels, suggesting that pro-nociceptive signaling before or during an attack may be inhibited by endogenous analgesic molecules in the peripheral nervous system (PNS) or within the CNS.
The analgesic anti-nociceptive potential of cannabinoid CB1 receptors is well established [39,40]. Moreover, it has been shown that AEA, one of the key endoCBs, inhibited trigeminal neurons in animal models of migraine [41,42]. However, the activity profile of endoCB-degrading enzymes, monoacylglycerol lipase (MAGL) and fatty acid amide hydrolase (FAAH), targeting 2-AG and AEA respectively, is poorly studied within the nociceptive system. Normally, MAGL and FAAH activity maintains low physiological levels of endoCBs. High local MAGL and FAAH activity in the PNS and CNS can keep the endogenous analgesic action of endoCBs at low levels, giving rise to CECD [16,24]. Given that migraine pain is different in the pathogenesis from somatic pain, it needs analgesic agents specifically targeting TGVS. In this regard, one intriguing issue is whether the profile of MAGL/FAAH activity is different in the trigeminal ganglia (TG) implicated in migraine and dorsal root ganglion (DRG) involved in the transmission of somatic and visceral pain.
Given the contributing to migraine severity role of psychogenic stress, an additional promising line of anti-migraine therapy could be the activation of the ECS by selected plant cannabinoids combined with partner terpenes reducing the level of stress or severity of comorbid mood disorders [43,44].
Therefore, by proposing MAGL and FAAH as main targets for an innovative multitarget (analgesic and antidepressant) treatment for migraine, we studied their activity in the rat PNS and CNS, in areas important for the generation and propagation of migraine-specific pain signals. The activity of these enzymes was evaluated by a versatile chemoproteomic method, activity-based protein profiling (ABPP), utilizing for validation of specificity the recently developed potent and specific MAGL and FAAH inhibitors [45,46].
2. Results
2.1. Peripheral and Central Activity of the Endocannabinoid-Hydrolyzing Enzymes MAGL and FAAH
2.1.1. MAGL Activity Prevails at Peripheral Level: Trigeminal Ganglia and Dorsal Root Ganglia
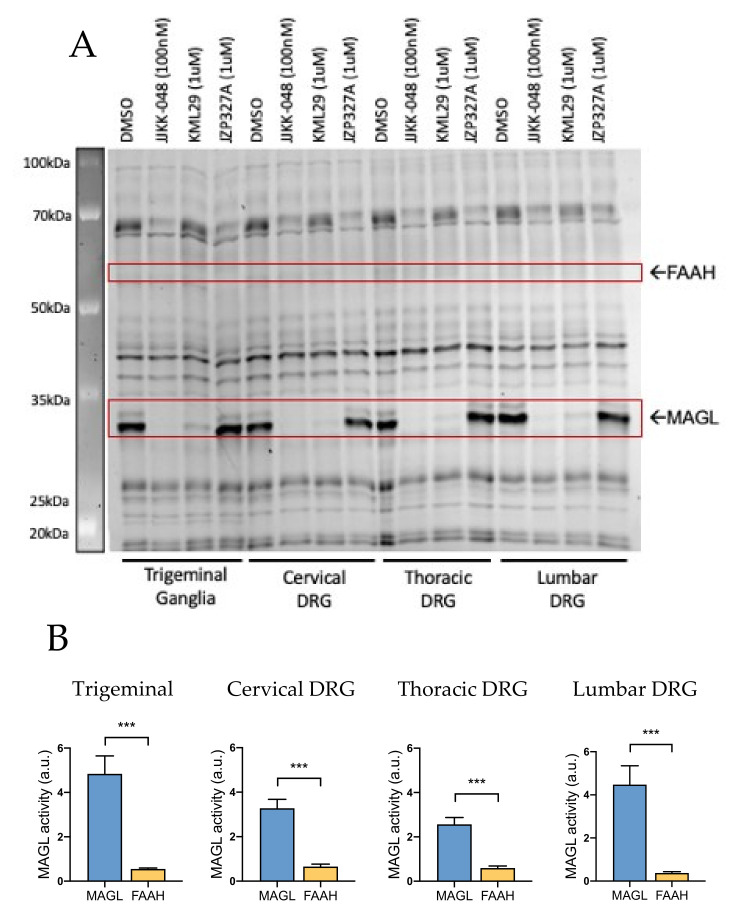
We found that both in TG and DRG, the basal MAGL activity (treatment with DMSO) was very high (Figure 1A). In both of these tissues, MAGL activity appeared as two MAGL-isoforms resulting a double-band. This activity was fully inhibited by the ultrapotent MAGL inhibitor JJKK-048 (100 nM) and almost totally blocked by the specific MAGL inhibitor KML29 (1 μM). A closer analysis of MAGL isoforms revealed that the short MAGL isoform appeared to be more active than the long isoform in peripheral tissues. However, both isoforms were equally active in the CNS (Supplementary Figure S1). Notice that, in contrast to MAGL, the basal FAAH activity (selectively inhibited by JZP327A) in rat TG and DRG was relatively low at these peripheral parts of the nociceptive system (Figure 1A).
Figure 1.
Competitive gel-based activity-based protein profiling (ABPP) reveals higher monoacylglycerol lipase (MAGL) activity over fatty acid amide hydrolase (FAAH) in trigeminal ganglia (TG) and cervical, thoracic and lumbar dorsal root ganglion (DRG). (A) Rat TG and DRG proteomes were preincubated for 1 h with vehicle (DMSO), the MAGL-inhibitors JJKK-048 (100 nM) and KML29 (1 μM) and FAAH-inhibitor JZP327A (1 μM). Then they were labeled with the fluorescent probe TAMRA-FP, as indicated in Materials and Methods. TAMRA-FP labeled bands (active serine hydrolases) appear dark after in-gel imaging. FAAH and MAGL were identified based on selective inhibition and their expected molecular weights. Notice that MAGL activity after DMSO treatment is high whereas the FAAH activity was almost absent. (B) Histograms comparing the basal activity of MAGL and FAAH in TG and DRG. Basal MAGL activity was approximately 9-fold higher compared that of FAAH in TG (in a.u., arbitrary units). Similarly, MAGL activity compared to that of FAAH was ~5-fold higher in cervical DRG, ~4-fold higher in thoracic DRG and ~11-fold higher in lumbar DRG. Unpaired t-test, *** p < 0.001, n = 8.
Figure 1B shows that both rat TG and DRG have significantly higher MAGL activity compared to FAAH. This observation was particularly clear in TG, where the basal MAGL activity was approximately 9-fold higher compared to that of FAAH. Similarly, MAGL activity compared to FAAH was ~5-fold higher in cervical DRG, ~4-fold higher in thoracic DRG and ~11-fold higher in lumbar DRG.
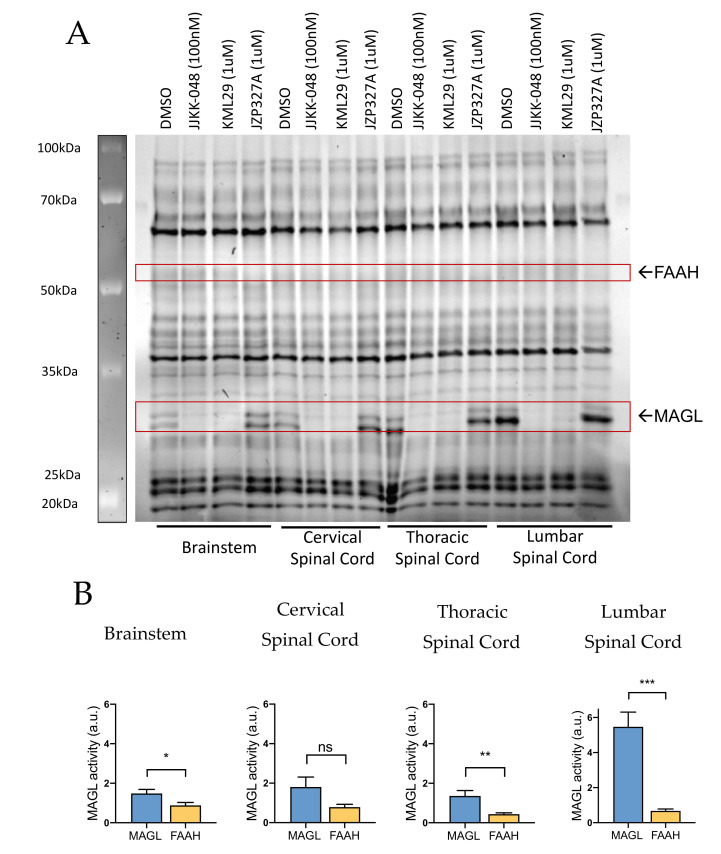
2.1.2. MAGL and FAAH Activity in Brainstem and Spinal Cord
Next, to identify additional molecular targets for analgesia by affecting the most active ECS enzymes, we investigated the activity of MAGL and FAAH in central areas involved in the generation and transmission of migraine pain. ABPP testing of rat brainstem and cervical, thoracic and lumbar spinal cord samples revealed the presence of both MAGL and FAAH activity (Figure 2A). MAGL activity appeared high in the lumbar spinal cord, where it was ~8-fold higher compared to FAAH activity (Figure 2B). A lower relative basal MAGL activity against FAAH was observed also in the brainstem (~2-fold higher) and thoracic spinal cord (~4-fold higher). In contrast, no significant difference between basal MAGL and FAAH activities in the cervical spinal cord was found (Figure 2B).
Figure 2.
Competitive gel-based ABPP reveals variable MAGL and FAAH activities in rat brainstem and cervical, thoracic and lumbar spinal cord. (A) Brainstem and spinal cord proteomes were incubated for 1 h with vehicle (DMSO), MAGL inhibitors JJKK-048 (100 nM) and KML29 (1 μM) and FAAH inhibitor JZP327A (1 μM), and then labeled with the fluorescent probe TAMRA-FP, as indicated in Materials and Methods. FAAH and MAGL were identified based on selective inhibition and their expected molecular weights. Note that basal MAGL activity was high in the lumbar spinal cord but less intense in samples of the brainstem, cervical and thoracic spinal cord. Based on this analysis, FAAH activity was not found in samples of the brainstem and spinal cord. (B) Histograms comparing the basal activity of MAGL and FAAH in the brainstem and different spinal cord parts. Basal MAGL activity was approximately 2-fold higher compared to that of FAAH in brainstem, and ~4-fold higher in thoracic spinal cord. In the lumbar spinal cord, MAGL activity was ~8-fold higher than of FAAH. Unpaired t-test, * p < 0.05, ** p < 0.01, *** p < 0.001, ns = nonsignificant, n = 11 (BS, cSC) and n = 8 (tSC, lSC).
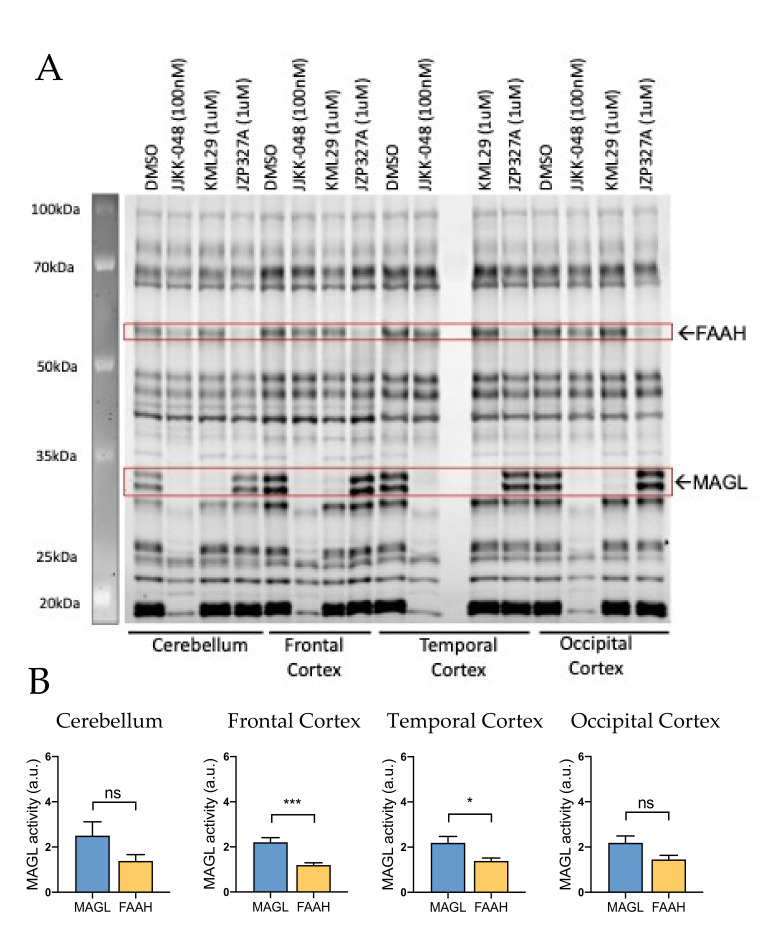
2.1.3. MAGL and FAAH Share the Spotlight at Central Cortical Level
Next, we explored whether MAGL and FAAH were active also at the level of CNS. Using cerebellum and cortex samples (Figure 3A), we observed high MAGL and, for the first time, relatively high basal FAAH activity in cerebellum, frontal, temporal and occipital cortexes (Figure 3A). Indeed, in the cerebellum, frontal and temporal cortexes, the basal MAGL activity was only approximately 2-fold higher compared to that of FAAH (Figure 3B). No significant difference was observed between basal MAGL vs. FAAH activities in the occipital cortex, suggesting a comparable contribution of both of these hydrolases in control of endoCBs in this important for migraine area of the brain (Figure 3B).
Figure 3.
Competitive gel-based ABPP reveals MAGL and FAAH activity in rat cerebellum and cortex. (A) Cerebellar and frontal, temporal and occipital cortexes proteomes were incubated for 1 h with vehicle (DMSO), MAGL inhibitors JJKK-048 (100 nM) and KML29 (1 μM) and FAAH inhibitor JZP327A (1 μM), and then labeled with the fluorescent probe TAMRA-FP, as indicated in Materials and Methods. FAAH and MAGL were identified based on selective inhibition and their expected molecular weights. Both MAGL and FAAH activities were high in the cerebellum and cortex. (B) Histograms showing the basal activity of MAGL and FAAH in the cerebellum and frontal, temporal and occipital cortexes. Basal MAGL activity was ~2-fold higher compared to that of FAAH in frontal and temporal cortexes. In contrast, MAGL and FAAH activities were not found statistically different in samples of the cerebellum and occipital cortex. Unpaired t-test, * p < 0.05, *** p < 0.001, ns = nonsignificant, n = 10.
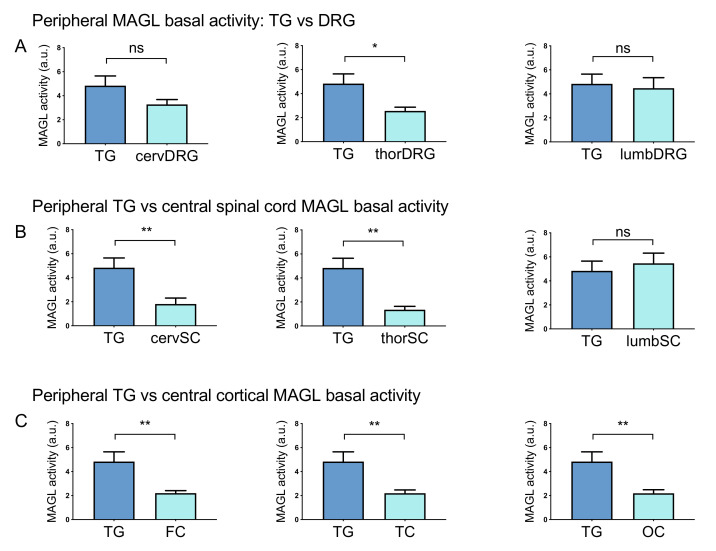
2.2. MAGL has a Key Activity at Peripheral Level
Given the overall prevalence of MAGL over FAAH in basal activity in most of the peripheral and central areas, we also investigated whether MAGL has a similar prevailing activity in certain areas of the PNS and CNS in comparison with a key migraine-related tissue such as TG. We found that MAGL activity was higher in peripheral TG than in most of the other areas (Figure 1A, Figure 2A, Figure 3A and Supplementary Figures S2–S4). In particular, Figure 4A shows that MAGL activity in TG was ~2-fold higher than in thoracic DRG. However, we could not find a significant difference among activities in TG and cervical and lumbar DRG (Figure 4A, Figure 1A). Basal MAGL activity in TG prevails on most of the other tissues: ~3-fold higher than in cervical and thoracic spinal cord and ~2-fold higher than in cortexes (Figure 4B,C, Figure 1A, Figure 2A, Figure 3A).
Figure 4.
Comparing the basal MAGL activity in peripheral and central rat tissues. (A) Comparison of basal MAGL activity between TG and DRG. Basal MAGL activity was ~2-fold higher in TG than in thoracic DRG but no significant difference was found in TG vs cervical and lumbar DRG. (B) Comparison of basal MAGL activities between peripheral TG and CNS spinal cord tracts. Basal MAGL activity in the cervical (cervSC) and thoracic (thorSC) spinal cord was ~3-fold lower than in TG. The level of MAGL activity was similar between samples of TG and the lumbar spinal cord (lumbSC). (C) Comparison of basal MAGL activities between peripheral TG and cortical samples. Basal MAGL activity in frontal (FC), temporal (TC) and occipital cortexes (OC) was approximately half of that in the TG sample. Unpaired t-test, * p < 0.05, ** p < 0.01, ns = nonsignificant, n = 8 (TGs, DRGs), n = 11 (BS, cSC), n = 8 (tSC, lSC) and n = 10 (Cbl, cortex).
2.3. Inhibition of MAGL and FAAH in Peripheral and Central Nervous Tissues
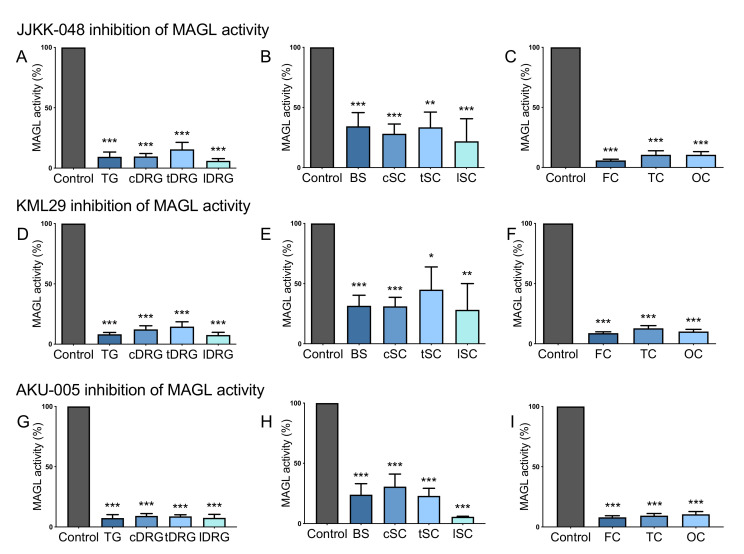
2.3.1. JJKK-048, KML29 and AKU-005 Block Basal MAGL Activity in Both Peripheral and Central Samples
In order to find the most efficient ways to block MAGL and FAAH activities on TG, DRG, brainstem, spinal cord and cortex, we numerically evaluated the inhibitory action on these tissues of the recently proposed MAGL inhibitors JJKK-048 and KML29, FAAH inhibitor JZP327A and the dual MAGL-FAAH inhibitor AKU-005 (Figure 5, Supplementary Figures S2–S4). In this testing, we used the fully effective concentrations of the inhibitors based on our previous studies, determining the dose-responses of these compounds [24,25,26].
Figure 5.
The blocking capacity of the MAGL inhibitors JJKK-048, KML29 and the dual MAGL-FAAH inhibitor AKU-005 in the CNS and the PNS. (A) JJKK-048 (100 nM) almost completely inhibited MAGL activity at peripheral level: by 90% in TG and cervical DRG (cDRG), 85% in thoracic DRG (tDRG) and 95% in lumbar DRG (lDRG). (B) JJKK-048 (100 nM) inhibited MAGL activity by 66% in brainstem (BS), 72% in cervical spinal cord (cSC), 68% in thoracic spinal cord (tSC), 79% in lumbar spinal cord (lSC). (C) JJKK-048 (100 nM) inhibited MAGL activity by 95% in frontal cortex (FC) and 90% in temporal and occipital cortexes (TC and OC). (D) KML29 (1 μM) strongly reduced MAGL activity at peripheral level: 92% TG, 88% cDRG, 86% tDRG, 93% lDRG. (E) KML29 (1 μM) inhibitory effect on brainstem and cSC was 69%, in tSC 55% and 72% in lSC. (F) KML29 (1 μM) strongly reduced MAGL activity at cortical level: by 92% in FC, 88% in TC, 90% in OC. (G) AKU-005 (1 μM) reduced MAGL basal activity at peripheral level: 93% in TG, 91% in cDRG, 92% in tDRG and 93% in lDRG. (H) AKU-005 (1 μM) inhibited basal MAGL activity also in brainstem (77%) and spinal cord (70% cSC, 78% tSC, 95% lSC). (I) AKU-005 (1 μM) inhibitory effect on cortical MAGL activity was of 92% in FC, 91% in TC and 90% in OC. One-way ANOVA with Tukey’s multiple comparison post-hoc test was used for statistical analysis between the MAGL activities after control (DMSO) and inhibitor treatments, (* p < 0.05, ** p < 0.01, *** p < 0.001). For JJKK-048: n = 8 (TGs, DRGs), n = 11 (BS, cSC), n = 8 (tSC, lSC) and n = 9 (cortex); For KML29: n = 8 (TGs, DRGs), n = 11 (BS, cSC), n = 8 (tSC, lSC) and n = 9 (cortex); For AKU-005: n = 4 (TGs, DRGs, BS, tSC, lSC), n = 5 (cSC, cortex).
We found that the specific MAGL inhibitor JJKK-048 (100 nM) almost completely inhibited the activity of this ECS enzyme in peripheral parts of the nociceptive system (represented by TG and DRG). In particular, MAGL activity was reduced by 90% in TG and cervical DRG, by 85% in thoracic DRG and by 95% in lumbar DRG (Figure 5A). Moreover, this treatment also inhibited MAGL activity in the CNS. Figure 5B illustrates a reduction of MAGL activity by 66% in the brainstem (BS), 72% in the cervical spinal cord (cSC), by 68% in the thoracic spinal cord (tSC) and by 79% in the lumbar spinal cord (lSC). JJKK-048-mediated inhibition at the cortical level was even stronger, with a 95% reduction of MAGL activity in the frontal cortex (FC) and 90% in temporal and occipital cortexes (TC and OC, Figure 5C).
Another selective MAGL inhibitor KML29 (1 μM) also strongly reduced MAGL activity in the PNS, including TG and DRG (by 92% in TG, 88% in cDRG, 86% in tDRG and 93% in lDRG, Figure 5D). Likewise, it also strongly reduced MAGL activity in the cerebral cortex (by 92% in FC, 88% in TC and 90% in OC; Figure 5F). Moreover, we observed a noticeable KML29-dependent inhibitory effect on basal MAGL activity on the brainstem (69%), cervical (69%), thoracic (55%) and lumbar spinal cord (72%) (Figure 5E).
The dual MAGL-FAAH inhibitor AKU-005 (1 μM) exhibited the same inhibitory effect as JJKK-048 and KML29; a strong reduction of MAGL activity was observed at peripheral (by 93% in TG, 91% in cDRG, 92% in tDRG and 93% in lDRG, Figure 5G) and cortical level (by 92% in FC, 91% in TC and 90% in OC, Figure 5I). Although, AKU-005 had a moderate inhibitory effect on MAGL activity in the brainstem (77%) and spinal cord (70% cSC, 78% tSC, we observed a 95% reduction in lSC, Figure 5H).
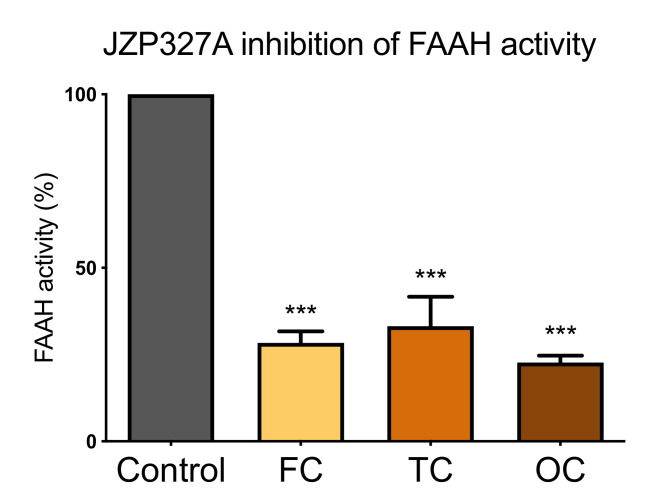
2.3.2. JZP327A Blocks FAAH Activity in the Cerebral Cortex
Unlike the peripheral tissues, as well as the brainstem and spinal cord, we observed a significantly high basal FAAH activity only in cortical samples (Figure 3). This high activity, therefore, represented a reliable model to evaluate specific FAAH inhibitors. Indeed, the endoCB -hydrolyzing activity of FAAH in the cortex was readily blocked by the specific FAAH inhibitor JZP327A (1 μM) (Figure 6). Thus, JZP327A reduced basal FAAH activity by 72% in the frontal cortex (FC), 67% in the temporal cortex (TC) and 78% in occipital cortex (OC) samples.
Figure 6.
FAAH inhibitor JZP327A reduces basal FAAH activity in vitro at the cortical level. Data is from ABPP testing of the frontal cortex (FC), temporal cortex (TC) and occipital cortex (OC) proteomes incubated for 1 h with vehicle (DMSO) and the specific FAAH inhibitor JZP327A (1 μM). Notice that JZP327A reduced FAAH activity by 72% in FC, 67% in TC and 78% in OC. One-way ANOVA with Tukey’s multiple comparison post-hoc test was used for comparison, *** p < 0.001, n = 9.
3. Discussion
In this study, we evaluated, for the first time, the activity of the ECS metabolic enzymes in the PNS, including the peripheral trigeminovascular nociceptive system, and in the CNS areas such as the spinal cord, brainstem, cerebellum and cerebral cortex. These areas are involved in the generation and transmission of migraine pain as well as in other migraine-related events such as migraine aura. By utilizing a sensitive chemoproteomic ABPP assay, we profiled the activity of MAGL and FAAH, two major endocannabinoid-hydrolyzing enzymes in these tissues. Our data suggest MAGL as a potential peripheral neuronal target for the treatment of migraine pain. At the cortical level, where the activity of FAAH was similar to MAGL, the dual-inhibition of these enzymatic pathways can attenuate, via raising the levels of two main endoCBs 2-AG and AEA, the phenomenon of CSD, underlying aura and reduce the central pain transmission. We propose recently developed potent and selective MAGL and FAAH inhibitors for the activation of ECS in peripheral and central nervous structures involved in the anti-nociceptive signaling.
3.1. MAGL and FAAH Activity in Peripheral Nervous Systems
By utilizing the ABPP assay, we demonstrated the prevailing active state of the main endocannabinoid-degrading enzyme MAGL over FAAH in TG, which are the main constituent of the TGVS, the place where migraine pain originates from [36,47,48,49]. The activity of MAGL was higher than the respective activity of FAAH not only in TG, but also in DRG and brainstem, which are also implicated in the transmission of migraine pain [50,51]. Interestingly, we observed that the activity of MAGL was higher in TG than in some DRG suggesting the specific role of this pathway in trigeminal pain, including migraine headache.
One previous study reported high FAAH expression in rat DRG and spinal cord, suggesting a key role of AEA in modulating peripheral nociceptive signaling [52]. Notably, our data do not contradict this conclusion as the ABPP assay allowed us to estimate not only the expression level but also to detect the activity of serine hydrolases in the peripheral tissues that are implicated in the generation and transmission of migraine pain. The demonstration of the relatively high peripheral activity of MAGL over FAAH in neuronal tissues, suggests that any increase of 2-AG levels occurring at the periphery during a migraine attack would be largely damped down by high MAGL activity. This was a specific reason to suggest the treatment of migraine pain by the MAGL inhibitor to elevate the level of the anti-nociceptive 2-AG. However, within the TGVS, the generation of pain involves not only neurons but also vessels and immune cells, in particular, mast cells [32,53]. Thus, AEA could interfere with these immuno-vascular mechanisms in the meninges, ultimately leading to reduced nociception [54]. This can happen at the level of meningeal afferents or via the suppressed transmission of peripheral signals to the second-order brainstem neurons [16]. Moreover, the role of AEA could be enhanced during migraine states [55], which are known to be associated with intensive neuro-inflammatory processes [48]. Therefore, our data do not exclude the role of FAAH/AEA-signalling as a target for peripheral analgesia but suggests the MAGL/2-AG as the most straightforward target for anti-nociceptive treatments operating via neuronal mechanisms.
2-AG is the primary endoCB operating via inhibitory Gi/o-protein-coupled CB1 and CB2 receptors [16]. Indeed, the MAGL-substrate 2-AG was previously found to fully activate these receptors whereas the FAAH-substrate AEA behaves as a partial agonist at both receptors [23,56,57]. This view is consistent with our findings on the prevailing activity of MAGL over FAAH in neuronal tissues at the periphery.
Notably, apart from the accumulation of the analgesic endoCBs 2-AG and AEA, the inhibition of MAGL and FAAH has additional benefits for anti-nociception, by diminishing the level of endoCB degradation product arachidonic acid which is a precursor for the pro-inflammatory and pro-nociceptive prostaglandins [16]. Therefore, peripheral MAGL and FAAH inhibition may have a multicomponent effect on migraine and other types of inflammatory pain, mediated by mechanical hypersensitivity, and probably, neuropathic pain, which, like migraine, is characterized by allodynia.
3.2. MAGL and FAAH Activity in the Central Nervous Systems
In contrast to peripheral nociceptive pathways, the activity of FAAH was much higher in the CNS. However, the activity of MAGL remained high in the brain. The high activity of these two endoCB-degrading enzymes might indicate a relatively low tonic inhibitory role of both 2-AG and AEA in modulating central pain processes in healthy states. In the CNS, the level of 2-AG has some prevalence over AEA [57], suggesting 2-AG as the primary modulator of synaptic processes in the brain. Nevertheless, both 2-AG and AEA can serve as the common retrograde messengers released from post-synaptic membranes to target the inhibitory CB1 presynaptic receptors in glutamatergic and GABAergic synapses [23].
Together, these data indicate a high potential for pharmacological interventions in the ECS in order to activate, via endoCBs, the inhibitory CB1/2 receptors for the treatment of migraine pain.
The role of central neuronal networks and brain centers in migraine is region-specific. Thus, both the brainstem and cervical spinal cord (C1-C3) are implicated in the transmission of pain signals from the primary afferents to the second-order neurons [17,50,51]. Consistent with this, our study showed that in the cervical spinal cord, unlike other spinal cord areas, the activity of FAAH was not significantly different from MAGL, reflecting their specific role in migraine mechanisms.
The occipital cerebral cortex tested in our study, is the common area for the development of CSD, a phenomenon underlying aura in the specific form of migraine with aura [58]. Accordingly, CSD is likely giving rise to multiple visual abnormalities at the initiation of migraine attacks [59,60,61,62]. Temporal, frontal cortical lobes and the cerebellum were also reported to be altered in chronic migraine patients during pain signaling events [63,64,65,66]. In migraine-related cortex and cerebellum, we found the high activity of both MAGL and FAAH, suggesting a potential reserve for therapeutic interventions against the MAGL and FAAH activity by their specific inhibitors. Indeed, both MAGL and FAAH signaling have been shown to modulate pain transmission at central and peripheral levels [67]. It is generally accepted that CSD is an attractive target for anti-migraine agents [68]. Moreover, the suppression of CSD by activating CB1 receptors has already been shown [69], implying that similar effects may be achieved via activation of ECS.
Thus, the enhancement and anti-nociceptive signaling of endoCBs, 2-AG and AEA, via MAGL and FAAH inhibition, can provide a beneficial reduction of the excessive cortical excitability and attenuate the central pain transmission in migraine and in inflammatory or neuropathic pain.
3.3. Novel Endocannabinoid Hydrolase Inhibitors for the Treatment of Migraine
The identification of the ECS in several CNS areas presents an avenue to pharmacologically enhance the beneficial role of endoCBs in several pathological conditions, including pain, cancer, addictive behavior, epilepsy and psychiatric diseases [22,41]. In this study, we showed for the first time, the comprehensive profile of activity and specific inhibition of endoCB-hydrolyzing enzymes MAGL and FAAH in tissues of origin and transmission of migraine pain.
The majority of previously tested MAGL inhibitors lack high selectivity among different hydrolases [70]. In contrast, the recently found KML29 [46] compound has high MAGL-specificity and has been validated for its analgesic and anti-allodynic effects in vivo [71,72,73,74]. We propose the newly-synthesized highly potent MAGL inhibitor JJKK-048 (IC50 < 0.4 nM) [46,75] as strong prototype drug candidate for migraine analgesia.
Previous studies on FAAH inhibition using OL-135, URB597 [76,77] and PF3845 showed analgesic effects [72,76]. These results raised further interest in the application of FAAH inhibitors to different pain states and the identification of more efficient and selective compounds. In our study, we used the recently developed selective FAAH inhibitor JZP327A [45], which completely blocked FAAH activity in cerebral cortex samples.
An alternative and powerful tool for targeting both MAGL and FAAH in either TGVS and CNS is the recently developed dual MAGL-FAAH inhibitor AKU-005 that showed a strong inhibitory effect, even at nanomolar concentrations (IC50 value 0.2–1.1 nM) [46]. Moreover, another dual inhibitor JZL195 has been reported to elicit stronger pain relief than the other selective MAGL or FAAH inhibitors [78].
3.4. Summary
In summary, we observed distinct profiles of MAGL and FAAH activity in healthy PNS and CNS. We show that novel selective MAGL and FAAH inhibitors can fully block the peripheral and cortical activity of these endCB-degrading enzymes in vitro. Our findings highlight MAGL and FAAH as promising targets for novel anti-migraine strategies via selective enhancement of the anti-nociceptive endoCB drive in this common neurological disorder. Future research efforts may focus on testing novel MAGL and FAAH inhibitors in in vivo models of migraine.
4. Materials and Methods
4.1. Animals
Animal House of the University of Eastern Finland provided male Wistar rats for this study. For testing MAGL and FAAH activity, experiments were conducted on organ samples from 10–12 rats, on occipital cortex slices from 8 rats and trigeminal ganglia fragments from 7 rats. Animals were housed under the following conditions: 12h dark/light cycle, grouped housing, ad libitum access to food and water, at an ambient temperature of 22 °C. All experimental procedures performed in this study follow the rules of the European Community Council Directive of 22 September 2010 (2010/63/EEC). The Animal Care and Committee of the University of Eastern Finland approved all experimental protocols (licence EKS-008-2019, protocol from 25 November 2019).
4.2. Animals Dissection
4-6 weeks male Wistar rats were dissected according to published protocols to isolate the trigeminal ganglia [79], cortical areas, brainstem, cerebellum [80] dorsal root ganglia and spinal cord [81]. The spinal cord was divided into cervical (C2-C8), thoracic (T1–T13) and lumbar (L1–S4) tracts. We dissected cervical, thoracic and lumbar DRGs following the same vertebral segmentation.
4.3. Activity-Based Protein Profiling of Serine Hydrolases
Organ samples were mechanically homogenized (glass-glass homogenizer) in ice-cold PBS, and protein concentrations were determined with BCA protein assay (Pierce, Rockford, IL, USA), as previously described [82]. Competitive ABPP using tissue homogenates was conducted to visualize the selectivity of inhibitors toward endocannabinoid hydrolases FAAH and MAGL and against other serine hydrolases in tissue proteomes. We used the active site serine-targeting fluorescent fluorophosphonate probe TAMRA-FP (ActivX Fluorophosphonate Probes, Thermo Fisher Scientific Inc., Rockford, IL, USA) as previously described [83]. Briefly, tissue homogenates (100 μg protein) were pre-treated for 1 h with DMSO or the selected MAGL inhibitors JJKK-048 (School of Pharmacy, UEF) and KML29 (Cayman Chemicals (Ann Arbor, MI, USA), FAAH inhibitor JZP-327A (School of Pharmacy, UEF) or the dual MAGL/FAAH inhibitor AKU-005 (School of Pharmacy, UEF) with indicated concentrations, after which TAMRA-FP incubation was conducted for 1 h at room temperature (final probe concentration 2 μM) to label active serine hydrolases. The reaction was quenched by adding 2× gel loading buffer, after which 10 μg protein was loaded per lane and the proteins were resolved in 10 % SDS-PAGE together with molecular weight standards. TAMRA-FP labelled proteins were visualized by ChemiDoc™ MP imaging system (BIO-RAD, Hercules, CA, USA) with Cy3 blot application (602/50, Green Epi, Manual Exposure 10s–120s). Quantification of bands was performed by the software ImageLab (2020 Bio-Rad Laboratories) on the basis of band intensity (MAGL/FAAH activity, a.u.).
4.4. Statistical Analysis
Data were analyzed using GraphPad Prism 8 (GraphPad Prism Software, La Jolla, USA). The data are presented as mean ± SEM (standard error of the mean). Student’s unpaired t-test and One-way ANOVA with Tukey’s multiple comparison post-hoc test were used to detect statistical significances.
Acknowledgments
We would like to thank Jayendra Z. Patel for providing JZP327A, Taina Vihavainen for the help with increasing ABPP assays replicates, Raisa Giniatullina for contributing to rat samples collection and Sweelin Chew for language editing of the manuscript.
Abbreviations
| 2-AG | 2-arachidonoyl glycerol |
| ABPP | Activity-based protein profiling |
| AEA | N-arachidonoyl ethanol amine, anandamide |
| BS | Brainstem |
| CB1, CB2 | Cannabinoid receptors 1, 2 |
| Cbl | Cerebellum |
| cDRG | Cervical dorsal root ganglia |
| CECD | Clinical endocannabinoid deficiency |
| cerv | Cervical |
| CGRP | Calcitonin generelated peptide |
| CNS | Central nervous system |
| cSC | Cervical dorsal root ganglia |
| CSD | Cortical spreading depression |
| DMSO | Dimethyl sulfoxide |
| DRG | Dorsal root ganglia |
| ECS | Endocannabinoid system |
| endoCB | Endocannabinoids |
| FAAH | Fatty acid amide hydrolase |
| FC | Frontal cortex |
| lDRG | Lumbar dorsal root ganglia |
| lSC | Lumbar spinal cord |
| lumb | Lumbar |
| MAGL | Monoacylglycerol lipase |
| NMDA | N-methyl-D-aspartate |
| NMDAR | N-methyl-D-aspartate receptors |
| OC | Occipital cortex |
| PACAP | Pituitary adenylate cyclase-activating enzyme |
| PNS | Peripheral nervous system |
| TC | Temporal cortex |
| TG | Trigeminal ganglia |
| TGVS | Trigeminovascular system |
| tDRG | Thoracic dorsal root ganglia |
| thor | Thoracic |
| tSC | Thoracic spinal cord |
Supplementary Materials
Supplementary materials are available online at https://www.mdpi.com/1422-0067/22/3/1204/s1, can be found in the file “Supplementary materials—Molecular keys for migraine treatment via selective inhibition of endocannabinoid-hydrolyzing enzymes”.
Author Contributions
Conceptualization, A.D.P., R.G. and J.R.S.; methodology, A.D.P.; formal analysis, A.D.P.; investigation, A.D.P.; resources, R.G. and J.R.S.; data curation, A.D.P.; writing—original draft preparation, A.D.P., R.G. and J.R.S.; writing—review and editing, A.D.P., R.G. and J.R.S.; visualization, A.D.P., R.G. and J.R.S.; supervision, R.G. and J.R.S.; project administration, R.G. and J.R.S.; funding acquisition, R.G. and J.R.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the 2019 Migraine Research Foundation Impact Award. RG and A.D.P were partially supported by the Finnish Academy grant (No 325392) to R.G.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Animal Care and Committee of the University of Eastern Finland (licence EKS-008-2019 protocol from 25 November 2019).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
None of the authors has any conflict of interest to disclose. This paper is in line with ethical guidelines requested by the journal.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Migraine Research Foundation. [(accessed on 20 December 2020)]; Available online: https://migraineresearchfoundation.org.
- 2.World Health Organization. [(accessed on 20 January 2021)]; Available online: https://www.who.int/news-room/fact-sheets/detail/headache-disorders.
- 3.Buse D.C., Silberstein S.D., Manack A.N., Papapetropoulos S., Lipton R.B. Psychiatric comorbidities of episodic and chronic migraine. J. Neurol. 2013;260:1960–1969. doi: 10.1007/s00415-012-6725-x. [DOI] [PubMed] [Google Scholar]
- 4.Minen M.T., De Dhaem O.B., van Diest A.K., Powers S., Schwedt T.J., Lipton R., Silbersweig D. Migraine and its psychiatric comorbidities. J. Neurol. Neurosurg. Psychiatry. 2016;87:741–749. doi: 10.1136/jnnp-2015-312233. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Q., Shao A., Jiang Z., Tsai H., Liu W. The exploration of mechanisms of comorbidity between migraine and depression. J. Cell. Mol. Med. 2019;23:4505–4513. doi: 10.1111/jcmm.14390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dresler T., Caratozzolo S., Guldolf K., Huhn J.-I., Loiacono C., Niiberg-Pikksööt T., Puma M., Sforza G., Tobia A., Ornello R., et al. Understanding the nature of psychiatric comorbidity in migraine: A systematic review focused on interactions and treatment implications. J. Headache Pain. 2019;20:51. doi: 10.1186/s10194-019-0988-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buse D.C., Greisman J.D., Baigi K., Lipton R.B. Migraine Progression: A Systematic Review. Headache. 2019;59:306–338. doi: 10.1111/head.13459. [DOI] [PubMed] [Google Scholar]
- 8.Diener H.-C., Dodick D., Evers S., Holle D., Jensen R.H., Lipton R.B., Porreca F., Silberstein S., Schwedt T. Pathophysiology, prevention, and treatment of medication overuse headache. Lancet Neurol. 2019;18:891–902. doi: 10.1016/S1474-4422(19)30146-2. [DOI] [PubMed] [Google Scholar]
- 9.Baron E.P. Medicinal Properties of Cannabinoids, Terpenes, and Flavonoids in Cannabis, and Benefits in Migraine, Headache, and Pain: An Update on Current Evidence and Cannabis Science. Headache. 2018;58:1139–1186. doi: 10.1111/head.13345. [DOI] [PubMed] [Google Scholar]
- 10.Ma L., Hettema J.M., Cousijn J., Bjork J.M., Steinberg J.L., Keyser-Marcus L., Woisard K., Lu Q., Roberson-Nay R., Abbate A., et al. Resting-State Directional Connectivity and Anxiety and Depression Symptoms in Adult Cannabis Users. Biol. Psychiatry Cogn. Neurosci. Neuroimaging. 2020 doi: 10.1016/j.bpsc.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smitherman T.A., Rains J.C., Penzien D.B. Psychiatric comorbidities and migraine chronification. Curr. Pain Headache Rep. 2009;13:326–331. doi: 10.1007/s11916-009-0052-7. [DOI] [PubMed] [Google Scholar]
- 12.Peterlin B.L., Rosso A.L., Sheftell F.D., Libon D.J., Mossey J.M., Merikangas K.R. Post-traumatic stress disorder, drug abuse and migraine: New findings from the National Comorbidity Survey Replication (NCS-R) Cephalalgia. 2011;31:235–244. doi: 10.1177/0333102410378051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merikangas K.R. Migraine and Psychopathology. Arch. Gen. Psychiatry. 1990;47:849. doi: 10.1001/archpsyc.1990.01810210057008. [DOI] [PubMed] [Google Scholar]
- 14.Breslau N., Davis G.C., Andreski P. Migraine, psychiatric disorders, and suicide attempts: An epidemiologic study of young adults. Psychiatry Res. 1991;37:11–23. doi: 10.1016/0165-1781(91)90102-U. [DOI] [PubMed] [Google Scholar]
- 15.Bifulco M., Marasco G., Colucci-D’Amato L., Pisanti S. Headaches in the medieval Medical School of Salerno. Cephalalgia. 2020;40:871–877. doi: 10.1177/0333102420905317. [DOI] [PubMed] [Google Scholar]
- 16.Leimuranta P., Khiroug L., Giniatullin R. Emerging role of (endo)cannabinoids in migraine. Front. Pharmacol. 2018;9:1–7. doi: 10.3389/fphar.2018.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greco R., Demartini C., Zanaboni A.M., Piomelli D., Tassorelli C. Endocannabinoid System and Migraine Pain: An Update. Front. Neurosci. 2018;12 doi: 10.3389/fnins.2018.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kinsey S.G., Long J.Z., O’Neal S.T., Abdullah R.A., Poklis J.L., Boger D.L., Cravatt B.F., Lichtman A.H. Blockade of Endocannabinoid-Degrading Enzymes Attenuates Neuropathic Pain. J. Pharmacol. Exp. Ther. 2009;330:902–910. doi: 10.1124/jpet.109.155465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhyne D.N., Anderson S.L., Gedde M., Borgelt L.M. Effects of medical marijuana on migraine headache frequency in an adult population. Pharmacotherapy. 2016;36:505–510. doi: 10.1002/phar.1673. [DOI] [PubMed] [Google Scholar]
- 20.Baron E.P. Comprehensive Review of Medicinal Marijuana, Cannabinoids, and Therapeutic Implications in Medicine and Headache: What a Long Strange Trip It’s Been …. Headache J. Head Face Pain. 2015;55:885–916. doi: 10.1111/head.12570. [DOI] [PubMed] [Google Scholar]
- 21.Khademi H., Kamangar F., Brennan P., Malekzadeh R. Opioid Therapy and its Side Effects: A Review. Arch. Iran. Med. 2016;19:870–876. doi: 10.1002/sim.4107. [DOI] [PubMed] [Google Scholar]
- 22.Guindon J., Hohmann A.G. The endocannabinoid system and pain. CNS Neurol. Disord. Drug Targets. 2009;8:403–421. doi: 10.2174/187152709789824660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Savinainen J.R., Saario S.M., Laitinen J.T. The serine hydrolases MAGL, ABHD6 and ABHD12 as guardians of 2-arachidonoylglycerol signalling through cannabinoid receptors. Acta Physiol. 2012;204:267–276. doi: 10.1111/j.1748-1716.2011.02280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russo E.B. Clinical endocannabinoid deficiency (CECD): Can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions? Neuro Endocrinol. Lett. 2008;29:192–200. [PubMed] [Google Scholar]
- 25.IHS classification ICHD-3. [(accessed on 20 December 2020)]; Available online: https://ichd-3.org.
- 26.Zhang X., Levy D., Noseda R., Kainz V., Jakubowski M., Burstein R. Activation of Meningeal Nociceptors by Cortical Spreading Depression: Implications for Migraine with Aura. J. Neurosci. 2010;30:8807–8814. doi: 10.1523/JNEUROSCI.0511-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao H., Eising E., de Vries B., Vijfhuizen L.S., Anttila V., Winsvold B.S., Kurth T., Stefansson H., Kallela M., Malik R., et al. Gene-based pleiotropy across migraine with aura and migraine without aura patient groups. Cephalalgia. 2016;36:648–657. doi: 10.1177/0333102415591497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swanson S.A., Zeng Y., Weeks M., Colman I. The contribution of stress to the comorbidity of migraine and major depression: Results from a prospective cohort study. BMJ Open. 2013;3:e002057. doi: 10.1136/bmjopen-2012-002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Theoharides T.C., Spanos C., Pang X., Alferes L., Ligris K., Letourneau R., Rozniecki J.J., Webster E., Chrousos G.P. Stress-induced intracranial mast cell degranulation: A corticotropin-releasing hormone-mediated effect. Endocrinology. 1995;136:5745–5750. doi: 10.1210/endo.136.12.7588332. [DOI] [PubMed] [Google Scholar]
- 30.Della Pietra A., Mikhailov N., Giniatullin R. The emerging role of mechanosensitive piezo channels in migraine pain. Int. J. Mol. Sci. 2020;21:696. doi: 10.3390/ijms21030696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koroleva K., Gafurov O., Guselnikova V., Nurkhametova D., Giniatullina R., Sitdikova G., Mattila O.S., Lindsberg P.J., Malm T.M., Giniatullin R. Meningeal Mast Cells Contribute to ATP-Induced Nociceptive Firing in Trigeminal Nerve Terminals: Direct and Indirect Purinergic Mechanisms Triggering Migraine Pain. Front. Cell. Neurosci. 2019;13 doi: 10.3389/fncel.2019.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levy D. Migraine pain, meningeal inflammation, and mast cells. Curr. Pain Headache Rep. 2009;13:237–240. doi: 10.1007/s11916-009-0040-y. [DOI] [PubMed] [Google Scholar]
- 33.Negro A., Seidel J.L., Houben T., Yu E.S., Rosen I., Arreguin A.J., Yalcin N., Shorser-Gentile L., Pearlman L., Sadhegian H., et al. Acute sleep deprivation enhances susceptibility to the migraine substrate cortical spreading depolarization. J. Headache Pain. 2020;21:86. doi: 10.1186/s10194-020-01155-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burch R.C., Buse D.C., Lipton R.B. Migraine. Neurol. Clin. 2019;37:631–649. doi: 10.1016/j.ncl.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Edvinsson L., Haanes K.A., Warfvinge K., Krause D.N. CGRP as the target of new migraine therapies—Successful translation from bench to clinic. Nat. Rev. Neurol. 2018;14:338–350. doi: 10.1038/s41582-018-0003-1. [DOI] [PubMed] [Google Scholar]
- 36.Haanes K.A., Edvinsson L. Pathophysiological Mechanisms in Migraine and the Identification of New Therapeutic Targets. CNS Drugs. 2019;33:525–537. doi: 10.1007/s40263-019-00630-6. [DOI] [PubMed] [Google Scholar]
- 37.Iyengar S., Johnson K.W., Ossipov M.H., Aurora S.K. CGRP and the Trigeminal System in Migraine. Headache J. Head Face Pain. 2019;59:659–681. doi: 10.1111/head.13529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chan C., Wei D.Y., Goadsby P.J. Biochemical Modulation and Pathophysiology of Migraine. J. Neuro-Ophthalmology. 2019;39:470–479. doi: 10.1097/WNO.0000000000000875. [DOI] [PubMed] [Google Scholar]
- 39.Iversen L. Cannabinoids: A real prospect for pain relief. Curr. Opin. Pharmacol. 2002;2:50–55. doi: 10.1016/S1471-4892(01)00120-5. [DOI] [PubMed] [Google Scholar]
- 40.Pertwee R.G. The pharmacology of cannabinoid receptors and their ligands: An overview. Int. J. Obes. 2006;30:S13–S18. doi: 10.1038/sj.ijo.0803272. [DOI] [PubMed] [Google Scholar]
- 41.Akerman S., Holland P.R., Lasalandra M.P., Goadsby P.J. Endocannabinoids in the Brainstem Modulate Dural Trigeminovascular Nociceptive Traffic via CB1 and “Triptan” Receptors: Implications in Migraine. J. Neurosci. 2013;33:14869–14877. doi: 10.1523/JNEUROSCI.0943-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akerman S., Kaube H., Goadsby P.J. Anandamide Is Able to Inhibit Trigeminal Neurons Using an In Vivo Model of Trigeminovascular-Mediated Nociception. J. Pharmacol. Exp. Ther. 2004;309:56–63. doi: 10.1124/jpet.103.059808. [DOI] [PubMed] [Google Scholar]
- 43.Ferber S.G., Hazani R., Shoval G., Weller A. Targeting the Endocannabinoid System in Borderline Personality Disorder. Curr. Neuropharmacol. 2020;18 doi: 10.2174/1570159X18666200429234430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferber S.G., Namdar D., Hen-Shoval D., Eger G., Koltai H., Shoval G., Shbiro L., Weller A. The “Entourage Effect”: Terpenes Coupled with Cannabinoids for the Treatment of Mood Disorders and Anxiety Disorders. Curr. Neuropharmacol. 2020;18:87–96. doi: 10.2174/1570159X17666190903103923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel J.Z., Parkkari T., Laitinen T., Kaczor A.A., Saario S.M., Savinainen J.R., Navia-Paldanius D., Cipriano M., Leppänen J., Koshevoy I.O., et al. Chiral 1,3,4-Oxadiazol-2-ones as Highly Selective FAAH Inhibitors. J. Med. Chem. 2013;56:8484–8496. doi: 10.1021/jm400923s. [DOI] [PubMed] [Google Scholar]
- 46.Aaltonen N., Savinainen J.R., Ribas C.R., Rönkkö J., Kuusisto A., Korhonen J., Navia-Paldanius D., Häyrinen J., Takabe P., Käsnänen H., et al. Piperazine and Piperidine Triazole Ureas as Ultrapotent and Highly Selective Inhibitors of Monoacylglycerol Lipase. Chem. Biol. 2013;20:379–390. doi: 10.1016/j.chembiol.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 47.Messlinger K. Migraine: Where and how does the pain originate? Exp. Brain Res. 2009;196:179–193. doi: 10.1007/s00221-009-1756-y. [DOI] [PubMed] [Google Scholar]
- 48.Moskowitz M.A. Defining a Pathway to Discovery from Bench to Bedside: The Trigeminovascular System and Sensitization. Headache J. Head Face Pain. 2008;48:688–690. doi: 10.1111/j.1526-4610.2008.01110.x. [DOI] [PubMed] [Google Scholar]
- 49.Olesen J., Burstein R., Ashina M., Tfelt-Hansen P. Origin of pain in migraine: Evidence for peripheral sensitisation. Lancet Neurol. 2009;8:679–690. doi: 10.1016/S1474-4422(09)70090-0. [DOI] [PubMed] [Google Scholar]
- 50.Kilinc E., Guerrero-toro C., Zakharov A., Vitale C., Gubert-olive M., Koroleva K., Timonina A., Luz L.L., Shelukhina I., Giniatullina R., et al. Neuropharmacology serotonergic mechanisms of trigeminal meningeal nociception: Implications for migraine pain. Neuropharmacology. 2017;116:160–173. doi: 10.1016/j.neuropharm.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 51.Andreou A.P., Holland P.R., Lasalandra M.P., Goadsby P.J. Modulation of nociceptive dural input to the trigeminocervical complex through GluK1 kainate receptors. Pain. 2015;156:439–450. doi: 10.1097/01.j.pain.0000460325.25762.c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lever I.J., Robinson M., Cibelli M., Paule C., Santha P., Yee L., Hunt S.P., Cravatt B.F., Elphick M.R., Nagy I., et al. Localization of the Endocannabinoid-Degrading Enzyme Fatty Acid Amide Hydrolase in Rat Dorsal Root Ganglion Cells and Its Regulation after Peripheral Nerve Injury. J. Neurosci. 2009;29:3766–3780. doi: 10.1523/JNEUROSCI.4071-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levy D. Endogenous Mechanisms Underlying the Activation and Sensitization of Meningeal Nociceptors: The Role of Immuno-Vascular Interactions and Cortical Spreading Depression. Curr. Pain Headache Rep. 2012;16:270–277. doi: 10.1007/s11916-012-0255-1. [DOI] [PubMed] [Google Scholar]
- 54.Cruz S.L., Sánchez-Miranda E., Castillo-Arellano J.I., Cervantes-Villagrana R.D., Ibarra-Sánchez A., González-Espinosa C. Anandamide inhibits FcεRI-dependent degranulation and cytokine synthesis in mast cells through CB2 and GPR55 receptor activation. Possible involvement of CB2-GPR55 heteromers. Int. Immunopharmacol. 2018;64:298–307. doi: 10.1016/j.intimp.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 55.Greco R., Demartini C., Zanaboni A.M., Tumelero E., Reggiani A., Misto A., Piomelli D., Tassorelli C. FAAH inhibition as a preventive treatment for migraine: A pre-clinical study. Neurobiol. Dis. 2020;134:104624. doi: 10.1016/j.nbd.2019.104624. [DOI] [PubMed] [Google Scholar]
- 56.Stella N., Schweitzer P., Piomelli D. A second endogenous cannabinoid that modulates long-term potentiation. Nature. 1997;388:773–778. doi: 10.1038/42015. [DOI] [PubMed] [Google Scholar]
- 57.Sugiura T., Waku K. Cannabinoid Receptors and Their Endogenous Ligands. J. Biochem. 2002;132:7–12. doi: 10.1093/oxfordjournals.jbchem.a003200. [DOI] [PubMed] [Google Scholar]
- 58.Van den Maagdenberg A.M.J., Pietrobon D., Pizzorusso T., Kaja S., Broos L.A., Cesetti T., van de Ven R.C., Tottene A., van der Kaa J., Plomp J.J., et al. A Cacna1a Knockin Migraine Mouse Model with Increased Susceptibility to Cortical Spreading Depression. Neuron. 2004;41:701–710. doi: 10.1016/S0896-6273(04)00085-6. [DOI] [PubMed] [Google Scholar]
- 59.Perenboom M.J.L., Schenke M., Ferrari M.D., Terwindt G.M., den Maagdenberg A.M.J.M., Tolner E.A. Responsivity to light in familial hemiplegic migraine type 1 mutant mice reveals frequency-dependent enhancement of visual network excitability. Eur. J. Neurosci. 2020 doi: 10.1111/ejn.15041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hadjikhani N., Albrecht D.S., Mainero C., Ichijo E., Ward N., Granziera C., Zürcher N.R., Akeju O., Bonnier G., Price J., et al. Extra-Axial Inflammatory Signal in Parameninges in Migraine with Visual Aura. Ann. Neurol. 2020;87:939–949. doi: 10.1002/ana.25731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Godukhin O.V., Obrenovitch T.P. Asymmetric Propagation of Spreading Depression Along the Anteroposterior Axis of the Cerebral Cortex in Mice. J. Neurophysiol. 2001;86:2109–2111. doi: 10.1152/jn.2001.86.4.2109. [DOI] [PubMed] [Google Scholar]
- 62.Hadjikhani N., del Rio M.S., Wu O., Schwartz D., Bakker D., Fischl B., Kwong K.K., Cutrer F.M., Rosen B.R., Tootell R.B.H., et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl. Acad. Sci. USA. 2001;98:4687–4692. doi: 10.1073/pnas.071582498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moulton E.A., Becerra L., Maleki N., Pendse G., Tully S., Hargreaves R., Burstein R., Borsook D. Painful Heat Reveals Hyperexcitability of the Temporal Pole in Interictal and Ictal Migraine States. Cereb. Cortex. 2011;21:435–448. doi: 10.1093/cercor/bhq109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sprenger T., Borsook D. Migraine changes the brain. Curr. Opin. Neurol. 2012;25:252–262. doi: 10.1097/WCO.0b013e3283532ca3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Valfrè W., Rainero I., Bergui M., Pinessi L. Voxel-Based Morphometry Reveals Gray Matter Abnormalities in Migraine. Headache J. Head Face Pain. 2007;48:109–117. doi: 10.1111/j.1526-4610.2007.00723.x. [DOI] [PubMed] [Google Scholar]
- 66.Dichgans M., Herzog J., Freilinger T., Wilke M., Auer D.P. 1H-MRS alterations in the cerebellum of patients with familial hemiplegic migraine type 1. Neurology. 2005;64:608–613. doi: 10.1212/01.WNL.0000151855.98318.50. [DOI] [PubMed] [Google Scholar]
- 67.Manzanares J., Julian M., Carrascosa A. Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Curr. Neuropharmacol. 2006;4:239–257. doi: 10.2174/157015906778019527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Costa C., Tozzi A., Rainero I., Cupini L.M., Calabresi P., Ayata C., Sarchielli P. Cortical spreading depression as a target for anti-migraine agents. J. Headache Pain. 2013;14:62. doi: 10.1186/1129-2377-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kazemi H., Rahgozar M., Speckmann E.-J., Gorji A. Effect of cannabinoid receptor activation on spreading depression. Iran. J. Basic Med. Sci. 2012;15:926–936. [PMC free article] [PubMed] [Google Scholar]
- 70.Ahn K., McKinney M.K., Cravatt B.F. Enzymatic pathways that regulate endocannabinoid signaling in the nervous system. Chem. Rev. 2008;108:1687–1707. doi: 10.1021/cr0782067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Busquets-Garcia A., Puighermanal E., Pastor A., De La Torre R., Maldonado R., Ozaita A. Differential role of anandamide and 2-arachidonoylglycerol in memory and anxiety-like responses. Biol. Psychiatry. 2011;70:479–486. doi: 10.1016/j.biopsych.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 72.Ghosh S. Ph.D. Thesis. Virginia Commonwealth University; Richmond, VA, USA: 2014. Targeting the Endocannabinoid Metabolic Enzymes to Reduce Inflammatory Pain. [Google Scholar]
- 73.Ignatowska-Jankowska B.M., Ghosh S., Crowe M.S., Kinsey S.G., Niphakis M.J., Abdullah R.A., Tao Q., O’Neal S.T., Walentiny D.M., Wiley J.L., et al. In vivo characterization of the highly selective monoacylglycerol lipase inhibitor KML29: Antinociceptive activity without cannabimimetic side effects. Br. J. Pharmacol. 2014;171:1392–1407. doi: 10.1111/bph.12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Spradley J.M., Guindon J., Hohmann A.G. Inhibitors of monoacylglycerol lipase, fatty-acid amide hydrolase and endocannabinoid transport differentially suppress capsaicin-induced behavioral sensitization through peripheral endocannabinoid mechanisms. Pharmacol. Res. 2010;62:249–258. doi: 10.1016/j.phrs.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Korhonen J., Kuusisto A., van Bruchem J., Patel J.Z., Laitinen T., Navia-Paldanius D., Laitinen J.T., Savinainen J.R., Parkkari T., Nevalainen T.J. Piperazine and piperidine carboxamides and carbamates as inhibitors of fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL) Bioorgan. Med. Chem. 2014;22:6694–6705. doi: 10.1016/j.bmc.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 76.Chang L., Luo L., Palmer J.A., Sutton S., Wilson S.J., Barbier A.J., Breitenbucher J.G., Chaplan S.R., Webb M. Inhibition of fatty acid amide hydrolase produces analgesia by multiple mechanisms. Br. J. Pharmacol. 2006;148:102–113. doi: 10.1038/sj.bjp.0706699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Otrubova K., Ezzili C., Boger D.L. The discovery and development of inhibitors of fatty acid amide hydrolase (FAAH) Bioorgan. Med. Chem. Lett. 2011;21:4674–4685. doi: 10.1016/j.bmcl.2011.06.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barnes N.S.A., Mitchell V.A., Kazantzis N.P., Vaughan C.W. Actions of the dual FAAH/MAGL inhibitor JZL195 in a murine neuropathic pain model. Br. J. Pharmacol. 2016;173:77–87. doi: 10.1111/bph.13337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Malin S.A., Davis B.M., Molliver D.C. Production of dissociated sensory neuron cultures and considerations for their use in studying neuronal function and plasticity. Nat. Protoc. 2007;2:152–160. doi: 10.1038/nprot.2006.461. [DOI] [PubMed] [Google Scholar]
- 80.Spijker S. Neuroproteomics. Humana Press; Totowa, NJ, USA: 2011. Dissection of Rodent Brain Regions; pp. 13–26. [Google Scholar]
- 81.Richner M., Jager S.B., Siupka P., Vaegter C.B. Hydraulic extrusion of the spinal cord and isolation of dorsal root ganglia in rodents. J. Vis. Exp. 2017;2017:1–6. doi: 10.3791/55226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Navia-Paldanius D., Patel J.Z., Navarro M.L., Jakupović H., Goffart S., Pasonen-Seppänen S., Nevalainen T.J., Jääskeläinen T., Laitinen T., Laitinen J.T., et al. Chemoproteomic, biochemical and pharmacological approaches in the discovery of inhibitors targeting human α/β-hydrolase domain containing 11 (ABHD11) Eur. J. Pharm. Sci. 2016;93:253–263. doi: 10.1016/j.ejps.2016.08.031. [DOI] [PubMed] [Google Scholar]
- 83.Navia-Paldanius D., Savinainen J.R., Laitinen J.T. Biochemical and pharmacological characterization of human α/β-hydrolase domain containing 6 (ABHD6) and 12 (ABHD12) J. Lipid Res. 2012;53:2413–2424. doi: 10.1194/jlr.M030411. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.