Abstract.
In industrialized countries, Mycobacterium avium complex and other nontuberculous mycobacteria (NTM) are major causes of opportunistic infection–related deaths in HIV patients. However, in resource-limited regions, data on NTM are scarce, and tuberculosis (TB) was often assumed to be the cause of death in HIV patients with a positive acid-fast smear. We searched MEDLINE and Embase databases for studies on autopsied HIV patients in sub-Saharan Africa published between January 1997 and April 2020. We included studies that reported histopathological or microbiological evidences for diagnosis of TB and NTM infection. We excluded articles without mycobacterial evidence from culture or molecular testing, such as those that used verbal autopsy, death certificates, or national registry data (systematic review registration number: CRD42019129836 at PROSPERO). We included six eligible studies that reported 391 autopsies in sub-Saharan African HIV patients. The prevalence of NTM and TB at autopsy ranged from 1.3% to 27.3% and 11.8% to 48.7%, respectively. The weighted prevalence ratio of NTM versus TB was 0.16 indicating that for every seven HIV patients died with mycobacterial infections, there was one died with NTM infection. Of the 13 NTM infections, six were caused by M. avium complex. Mycobacterium avium complex and other NTM infections are important differential diagnoses of TB at the time of death among HIV patients in sub-Saharan Africa. Our findings highlight the need to systematically survey the prevalence of NTM infections among HIV patients seeking medical care in resource-limited regions.
INTRODUCTION
Mycobacterium avium complex (MAC) and other nontuberculous mycobacteria (NTM) were important causes of opportunistic infection–related deaths among people living with HIV in industrialized countries before the development of highly active antiretroviral therapy (ART).1–3 In modern ART era, disseminated MAC infections still occur in lately diagnosed HIV patients, and the associated mortality remains high.4 However, in resource-limited countries, the role of MAC and other NTM infections in HIV-associated deaths remains unclear because of limited data mainly because of the lack of diagnostic capacity to identify NTM to species level.
In regions with a high burden of tuberculosis (TB), diagnosis of NTM infections is challenging because NTM infections share similar clinical features and laboratory findings with TB.5 Both NTM and Mycobacterium tuberculosis (MTB) can appear positive under sputum acid-fast stain and present with fever and weight loss.5,6 Xpert MTB/RIF would register a negative result for an NTM specimen but does not identify organisms outside of MTB complex. Nontuberculous mycobacteria infections can only be definitely distinguished from TB using mycobacterial culture or specific molecular methods, such as GenoType mycobacteria direct line probe assay (Direct LPA) (Hain Lifesciences GmbH, Nehren, Germany).7,8 When these tools were not available, patients with an acid-fast positive sputum smear were often presumably treated as TB.9 Nevertheless, the differential diagnosis is important because standard first-line anti-TB therapy is not effective against NTM infections.
Adding to this diagnostic challenge, NTM are ubiquitous in the environment and can cause colonization without disease. To overcome this issue, the American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) recommended a set of stringent criteria to distinguish between NTM colonization and NTM disease.10 Nevertheless, a systematic review on the prevalence of NTM infections among living patients in sub-Saharan Africa11 showed that only a minority of the included studies (seven of 37) adhered to the criteria as recommended by the ATS/IDSA.10 Furthermore, this review did not separate HIV from non-HIV patients. The ratios of NTM versus TB were also not reported. Therefore, the relative importance of NTM versus TB in HIV-associated deaths remains unknown.
Compared with samples obtained from living patients, culture samples taken from deceased patients at autopsy are more likely to represent true infection, rather than colonization,12 and could yield better information on the NTM burden among HIV patients in resource-limited regions.13 We now conduct the first systematic review and meta-analysis on the relative proportion of NTM infections versus TB at death among HIV patients in sub-Saharan Africa.
METHODS
Search strategy.
The protocol of this systematic review and meta-analysis had been registered at PROSPERO (https://www.crd.york.ac.uk/prospero/) as CRD42019129836. In brief, we searched MEDLINE® and Embase®, looking for English articles published between January 1997 and April 2020 on autopsy studies performed on HIV-infected adults or children living in sub-Saharan Africa. (Details of our search strategy can be found in Supplemental Table 1.) Four search sets that address key terms such as autopsy, HIV/AIDS, TB/NTM/MAC, and Africa were created and combined using “and.” Next, articles were compiled into a database, and duplicate records were removed. We initially screened by title and abstract to assess for potential eligibility. The complete texts of those regarded eligible were then acquired and assessed. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist was used. An ethical review was waived because this study was a secondary analysis of published articles.
Study selection.
Two authors (C.-H. C. and P.-U. T.) independently identified relevant studies using a predefined search strategy (Supplemental Table 1). Disagreement over the eligibility of the assessed studies was resolved through discussion with a third reviewer (C.-T. F.). Autopsy (either complete or minimally invasive) studies in Africa carried out in either adult or children positive for HIV were included. Articles were included if they were published in English, reported at least 10 autopsies, and conducted between January 1997 and April 2020. To be included in this review, studies have to report histopathological and microbiological evidence of mycobacterial infection that could discriminate between NTM and TB. Studies that used verbal autopsy, death certificates, or national registry data, as well as those that focused only on either one of TB or NTM were excluded. Conference papers were excluded from this analysis because of uncertainty over the relevance and validity of the presented data.
Data extraction.
Data extracted were compiled into a predesigned spreadsheet and included the following: author, date of study, study setting and location, characteristics of study population (inclusion criteria, adult versus pediatric, and inpatient versus outpatient), autopsy methods (tissues autopsied and whether the samples were sent for mycobacterial culture confirmation), the total number of deaths that are potentially available for autopsy, the number and rate of autopsy conducted, the number of NTM or TB identified from the autopsy, and the type of NTM species identified. Additional information such as the CD4 cell count were also retrieved if available. Two authors (C.-H. C. and P.-U. T.) extracted data independently, and a third author (G. H. L.) checked for consistency. The main outcome of the study was the prevalence ratio of NTM and TB at autopsy. Study quality was assessed using a prespecified, graded checklist (Supplemental Table 2) as reported in a previous systematic review.13 Studies were considered to be of “high quality” if they scored at least 70% of points, “medium quality” if they scored 40–69%, and “low quality” if they scored below 40%.13
Statistical analysis.
The prevalence ratio of NTM and TB at autopsy was pooled across the studies using a random-effects model, and the corresponding forest plots were constructed. Heterogeneity between the studies was assessed through calculation of I2 statistics, where an I2 value greater than 50% indicated significant heterogeneity. All statistical analyses were performed using SPSS version 23 (IBM, Armonk, NY) and Review Manager (Rev-Man version 5.3. The Nordic Cochrane Centre, the Cochrane Collaboration, 2014 software, Copenhagen, Denmark).
RESULTS
Study selection.
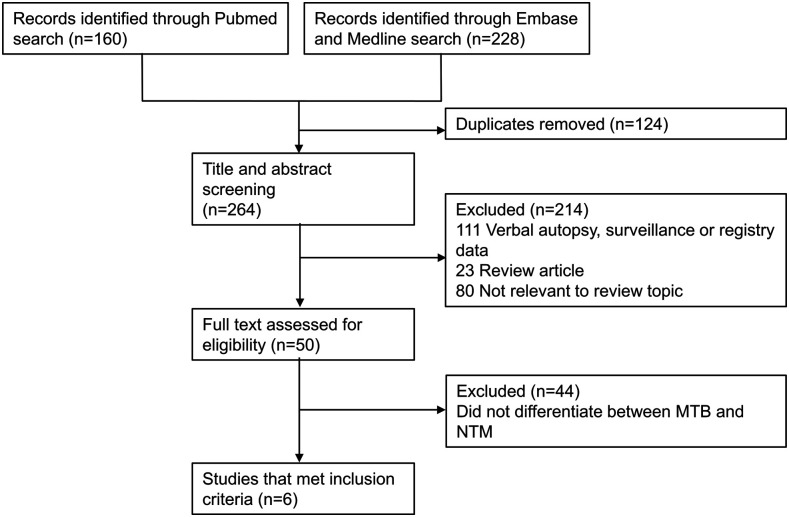
The PubMed and Embase search found 160 and 228 records, respectively. Following removal of 124 duplicates, the remaining articles were screened for relevance by title, abstract content, and full text as depicted in Figure 1. Forty-four publications were excluded because they did not explicitly differentiate between NTM and TB. The remaining six articles comprising 391 autopsies were included for further analysis.
Figure 1.
Flowchart showing the process of study selection. MTB = Mycobacterium tuberculosis; NTM = nontuberculous mycobacteria.
Study characteristics.
Of the six included studies, five were conducted on adult patients and one was conducted on children (Table 1).14–21 Five studies were conducted in South Africa and one in Zambia. In the five studies, the autopsies were conducted on patients who died during hospitalization, and one was conducted on patients who died at home. Two of the studies only included patients who were suspected or diagnosed as TB premortem,17,20 and one only included patients who were not on anti-TB treatment. The remaining studies analyzed all consecutive inpatient cases of mortality.
Table 1.
Basic demographics of the included studies investigating nontuberculous mycobacteria infection in African HIV patients in the ART era
| Author, published year | Country | Study dates | Study population* | Setting | Median/mean age (range) | Autopsy type | Tissues sampled | Postmortem diagnostic methods† | Study quality |
|---|---|---|---|---|---|---|---|---|---|
| Bates et al.16 | Zambia | 2011–2014 | All consecutive pediatric inpatient deaths | Hospital inpatient; National University Teaching Hospital | 19 months (12–45 months) | Minimally invasive autopsy | Lungs | ZN stain, histopathology, and PCR | High |
| Martinson et al.17 | South Africa | 2003–2005 | Consecutive adult inpatient deaths with premortem diagnosis of TB | Hospital inpatient; public, tertiary hospital | 34.5 years | Complete autopsy | Brain, lungs, heart, kidneys, liver, adrenals, spleen, and pancreas | ZN stain, histopathology, and culture | High |
| Cohen et al.18 | South Africa | 2008–2009 | All consecutive adult inpatient deaths | Hospital inpatient; regional hospital | 33 years (20–45 years) | Minimally invasive autopsy | Lungs, liver, and spleen | microscopy examination, liquid culture | High |
| Wong et al.19 | South Africa | 2009 | Consecutive adult inpatients receiving ART or eligible for ART | Hospital inpatient; public, tertiary hospital | 36 years (32–40 years) | Minimally invasive autopsy | CSF, liver, spleen, kidneys, bone marrow, heart, skin, lymph nodes, and any accessible masses | ZN stain, histopathology, and culture | High |
| Karat et al.20 | South Africa | 2012–2014 | Consecutive adults outpatient deaths with suspected or diagnosed TB | Hospital outpatient; TB Fast Track Program | 39 years | Minimally invasive autopsy | Liver, spleen, lungs. CSF, oro- and nasopharyngeal cavities, enlarged lymph nodes and skin lesions, urine, and blood | ZN stain, histopathology, culture, and PCR | High |
| Omar et al.21 | South Africa | 2012 | Sampled/selected home deaths who had no apparent cause of death and were not on anti-TB treatment | Home/households | 57 years (44–66 years) | Minimally invasive autopsy | Lungs | ZN stain, histopathology, culture, and PCR | High |
ART = antiretroviral therapy; CSF = cerebrospinal fluid; TB = tuberculosis; ZN = Ziehl–Neelsen.
“All consecutive” refers to the inclusion of all patients regardless of the cause of death or premortem diagnosis.
PCR/culture results discordant patients were considered to have mycobacterial infection if either PCR or mycobacterial culture was positive for mycobacteria.
All included studies detected mycobacterial infections in the autopsied samples based on results from the acid-fast stain, histopathological examination, and mycobacterial culture or PCR. Five studies performed minimally invasive autopsies, and one study performed complete autopsy. All of the included studies were assessed as being of high quality (Table 1 and Supplemental Table 3). Detailed descriptions of the autopsied tissues and samples that underwent mycobacterial culture or PCR testing were outlined in Table 1.
Isolation of TB and NTM from postmortem HIV patients.
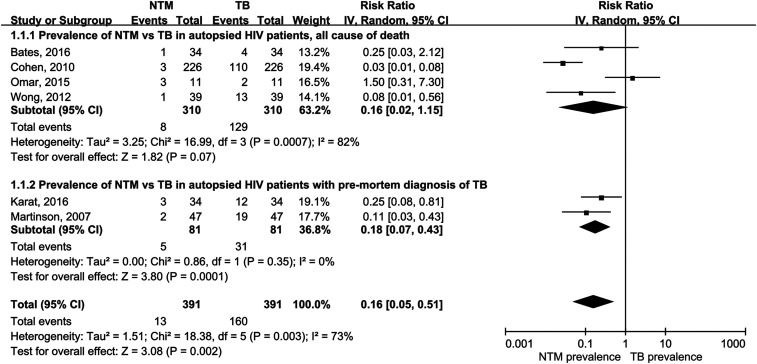
A total of 13 NTM and 160 TB cases were detected in 391 autopsies. The prevalence of NTM and TB at autopsy ranged from 1.3% to 27.3% and 11.8% to 48.7%, respectively (Table 2). The weighted prevalence ratio of NTM versus TB at autopsy was 0.16 (I2 = 73%) (Figure 2). Thus, one in seven autopsied mycobacterial infections were caused by NTM species. Of the 13 NTM cases isolated, six were further identified as disseminated MAC and one as pulmonary MAC. The species of NTM isolates in the remaining seven cases were not reported.
Table 2.
Isolation of TB or NTM from autopsy samples of African HIV patients in the antiretroviral therapy era
| First author, published year | Number of autopsies | Number of NTM culture or PCR | Number of TB culture or PCR | Prevalence of NTM (%) | Prevalence of TB (%) | Percentage of NTM as total mycobacterial infection (%) | Number of MAC |
|---|---|---|---|---|---|---|---|
| Bates et al.16 | 34 | 1 | 4 | 2.9 | 11.8 | 20.0 | Not specified |
| Martinson et al.17 | 47 | 2 | 19 | 4.3 | 40.4 | 9.5 | Two DMAC* |
| Cohen et al.18 | 226 | 3 | 110 | 1.3 | 48.7 | 2.7 | Not specified |
| Wong et al.19 | 39 | 1 | 13 | 2.6 | 33.3 | 7.1 | One DMAC† |
| Karat et al.20 | 34 | 3 | 12 | 8.8 | 35.3 | 20.0 | Three DMAC‡ |
| Omar et al.21 | 11 | 3 | 2 | 27.3 | 18.2 | 60.0 | One pulmonary MAC |
DMAC = disseminated MAC; MAC = Mycobacterium avium complex; NTM = nontuberculous mycobacteria; TB = tuberculosis.
Two DMAC isolates were recovered from the spleen.
One DMAC isolate was recovered from the spleen.
Organs from which the three DMAC isolates were recovered were not specified.
Figure 2.
Forest plot showing the prevalence of NTM vs. TB in autopsied HIV patients; prevalence of NTM vs. TB in autopsied HIV patients with premortem diagnosis of TB. NTM = nontuberculous mycobacteria; TB = tuberculosis.
Isolation of NTM from premortem HIV–TB suspects.
In the two studies (Martinson and Karat) that analyzed patients with premortem diagnosis of TB,17,20 five of 81 patients were found to have NTM infections after postmortem examinations (Figure 2); only 31 of these patients had culture- or PCR-confirmed TB. The weighted prevalence ratio of NTM versus TB in premortem TB suspects at autopsy was 0.18 (I2 = 0%).
Low CD4 count in NTM infection.
Two studies (Wong et al.19 and Karat et al.20) provided data on CD4 count of patients with NTM infection before death. Wong et al.19 reported a case of disseminated MAC infection with immune reconstitution inflammatory syndrome, whose premortem CD4 count was 17 cells/μL. In the autopsy study conducted by Karat et al.,20 all the three identified cases of MAC had low CD4 count with a range of 2–7 cells/μL (median = 2 cells/μL). In the same study, the premortem CD4 count for patients with positive TB was significantly higher, with 21–60 cells/μL (median = 44 cells/μL).
DISCUSSION
In this systematic review and meta-analysis, we found that the prevalence of NTM and TB in autopsied HIV patients in sub-Saharan Africa ranged from 1.3% to 27.3% and 11.8% to 48.7%, respectively. The weighted prevalence ratio of NTM versus TB was 0.16, which implied that for every seven HIV patients died with mycobacterial infections in sub-Saharan Africa, there will be one patient died with NTM infections which could be mistakenly treated as TB.
It is noteworthy that the two studies (Martinson and Karat) included patients with premortem diagnosis of TB, which were only based on clinical, and not microbiological, evidence. The five patients who were found to have NTM infections on postmortem culture did not have microbiological evidence of TB. Therefore, these studies did not suggest mixed infections of TB and NTM, but rather that some HIV patients who received premortem clinical diagnosis of TB may actually have NTM infections.
Increasing numbers of clinical studies from Africa have reported recovery of NTM from the sputum and blood samples of HIV–TB suspects.22–24 This is perhaps unsurprising because NTM and TB share similar clinical features. In some parts of Africa without adequate laboratory facilities, patients who present with TB-like symptoms are often treated as TB without confirmation by mycobacterial culture.9 Taking the NTM-to-TB ratio as 1:6 in autopsied patients, a significant proportion of presumed HIV–TB deaths may be attributed to NTM infections. Consistent with this finding, recent studies indicated that NTM, in particular disseminated MAC disease, has high associated mortality.25,26 The lack of efficacy of first-line antituberculous regimens against disseminated MAC disease further highlights the importance of differentiating between NTM and TB diagnosis among patients living with HIV.
Despite the development of ART and antimycobacterial therapy, we found that a significant number of HIV-positive patients still die from opportunistic infections such as TB and NTM in Africa. All four cases of NTM with known CD4 levels had low CD4 counts (2–17 cells/μL) before death. This is consistent with the literature that NTM infections usually occur in patients with a CD4 count lower than 50 cells/μL.10 More importantly, this finding reinforces the need to make ART available to more HIV patients in Africa, whereby a good control of the viral load and CD4 count would help prevent opportunistic infections.27
The weighted NTM:TB prevalence in our study might be underestimated. Many of the included studies performed mycobacterial culture only when the sampled tissues were found to have abnormal histopathological findings. However, reviews of mycobacteria pathology have reported that not all NTM cases exhibit the characteristic granulomatous pattern in mycobacterial infections.28 Thus, NTM cases with negative histopathological findings might not have been detected. Furthermore, some studies only performed autopsies on a limited number of organs, particularly the lungs. Such study designs could result in missed cases of disseminated NTM/MAC infections in the liver, spleen, and lymph nodes.
Before our study, a systematic review that reported on autopsied HIV patients found that TB was the cause of death in approximately 40% of the patients.13 However, in this previous review, most of the included studies did not distinguish between NTM and TB; TB was diagnosed primarily on the basis of positive acid-fast stain and relevant histopathological findings. No isolates of NTM were reported. It is possible that this earlier review overestimated the prevalence of HIV-associated TB deaths as some of the supposed TB deaths may, in fact, be caused by NTM infections.
Our study has important clinical implications. Given the significant presence of NTM infections among autopsied samples of HIV patients in high–TB burden regions, NTM infections need to be included in differential diagnoses. If facilities are available, mycobacterial culture should be performed for HIV patients present with TB-like syndrome, particularly in those with a CD4 count lower than 50 cells/μL. For a rapid molecular diagnosis of life-threatening disseminated NTM infections, negative Xpert MTB/RIF results would be inconclusive. It is worthwhile to consider introducing LPAs, such as GenoType mycobacteria direct LPA (Hain Lifesciences GmbH, Nehren, Germany). In resource-constrained scenarios, physicians can first apply a clinical algorithm to identify HIV patients with a high likelihood of disseminated NTM infections for a targeted molecular testing. We previously developed such an algorithm, based on a combination of low CD4, low body mass index, and absence of abnormal chest radiographic findings, which had a 98% specificity in differentiating disseminated MAC infection from TB.4 Applying aforementioned diagnostic procedure may facilitate an early decision to start life-saving anti-MAC therapy.
Our study is subjected to several limitations. First, autopsy findings might not reflect actual prevalence because it could not be performed in all patients, hence representing a potential selection bias. Furthermore, prevalence derived from autopsy studies is influenced by mortality rates. Given that disseminated MAC has higher mortality than TB, there may be an overestimation of the prevalence of NTM. On the other hand, because our estimates were derived from autopsy studies, they are more likely to be true disease as opposed to colonization. Moreover, there were considerable heterogeneities in the included studies likely because of differences in sample size, patient selection, and method of autopsy. Discrepancies in mycobacterial detection (culture versus PCR) probably also contributed to the heterogeneity across studies. Although NTM isolated postmortem from HIV patients may be consistent with NTM disease, this is also dependent on the species of NTM isolated. For example, NTM such as Mycobacterium gordonae, among others, are rarely associated with disease. It is important to note that some studies did not report NTM to the species level, and therefore, we could not ascertain the exact proportion of NTM that were truly pathogenic. Finally, most of the studies were conducted in South Africa, and therefore, our synthesis may not be generalizable across the entire sub-Saharan Africa region.
CONCLUSION
Mycobacterium avium complex and other NTM infections are important differential diagnoses of TB at the time of death among HIV patients in sub-Saharan Africa. Our findings highlight the need to further survey the prevalence of NTM infections among HIV patients seeking medical care in resource-limited regions.
Supplemental tables
Note: Supplemental tables appear at www.ajtmh.org.
REFERENCES
- 1.Wolinsky E, 1979. Nontuberculous mycobacteria and associated diseases. Am Rev Respir Dis 119: 107–159. [DOI] [PubMed] [Google Scholar]
- 2.Zakowski P, Fligiel S, Berlin GW, Johnson L, Jr., 1982. Disseminated Mycobacterium avium-intracellulare infection in homosexual men dying of acquired immunodeficiency. JAMA 248: 2980–2982. [DOI] [PubMed] [Google Scholar]
- 3.Moore RD, Chaisson RE, 1996. Natural history of opportunistic disease in an HIV-infected urban clinical cohort. Ann Intern Med 124: 633–642. [DOI] [PubMed] [Google Scholar]
- 4.Chiang CH, Lee GH, Chiang TH, Tang PU, Fang CT, 2020, Disseminated Mycobacterium avium complex infection as a differential diagnosis of tuberculosis in HIV patients. Int J Tuberc Lung Dis 24: 922–927. [DOI] [PubMed] [Google Scholar]
- 5.McCarthy KD, et al. 2012. Nontuberculous mycobacterial disease in patients with HIV in southeast Asia. Am J Respir Crit Care Med 185: 981–988. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh SM, Hung CC, Chen MY, Hsueh PR, Chang SC, Luh KT, 1998. Clinical features and outcome in disseminated mycobacterial diseases in AIDS patients in Taiwan. AIDS 12: 1301–1307. [DOI] [PubMed] [Google Scholar]
- 7.Luetkemeyer AF, et al. 2016. Evaluation of Xpert MTB/RIF versus AFB smear and culture to identify pulmonary tuberculosis in patients with suspected tuberculosis from low and higher prevalence settings. Clin Infect Dis 62: 1081–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luetkemeyer AF, et al. Adult AIDS Clinical Trials Group A5255 Study Team , 2014. Evaluation of two line probe assays for rapid detection of Mycobacterium tuberculosis, tuberculosis (TB) drug resistance, and non-TB Mycobacteria in HIV-infected individuals with suspected TB. J Clin Microbiol 52: 1052–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gopinath K, Singh S, 2010. Non-tuberculous mycobacteria in TB-endemic countries: are we neglecting the danger? PLoS Negl Trop Dis 4: e615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griffith DE, et al. ATS Mycobacterial Diseases Subcommittee , American Thoracic Society , Infectious Disease Society of America , 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 175: 367–416. Erratum in: Am J Respir Crit Care Med 175: 744–745. [DOI] [PubMed] [Google Scholar]
- 11.Okoi C, Anderson STB, Antonio M, Mulwa SN, Gehre F, Adetifa IMO, 2017. Non-tuberculous mycobacteria isolated from pulmonary samples in sub-Saharan Africa–a systematic review and meta analyses. Sci Rep 7: 12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lucas S, 2018. Investigating infectious diseases at autopsy. Diagn Histopathol 24: 357–364. [Google Scholar]
- 13.Gupta RK, Lucas SB, Fielding KL, Lawn SD, 2015. Prevalence of tuberculosis in post-mortem studies of HIV-infected adults and children in resource-limited settings: a systematic review and meta-analysis. AIDS 29: 1987–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rennert WP, Kilner D, Hale M, Stevens G, Stevens W, Crewe-Brown H, 2002. Tuberculosis in children dying with HIV-related lung disease: clinical-pathological correlations. Int J Tuberc Lung Dis 6: 806–813. [PubMed] [Google Scholar]
- 15.Rana FS, Hawken MP, Mwachari C, Bhatt SM, Abdullah F, Ng’ang’a LW, Power C, Githui WA, Porter JD, Lucas SB, 2000. Autopsy study of HIV-1-positive and HIV-1-negative adult medical patients in Nairobi, Kenya. J Acquir Immune Defic Syndr 24: 23–29. [DOI] [PubMed] [Google Scholar]
- 16.Bates M, et al. 2016. Burden of respiratory tract infections at post mortem in Zambian children. BMC Med 14: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinson NA, Karstaedt A, Venter WD, Omar T, King P, Mbengo T, Marais E, McIntyre J, Chaisson RE, Hale M, 2007. Causes of death in hospitalized adults with a premortem diagnosis of tuberculosis: an autopsy study. AIDS 21: 2043–2050. [DOI] [PubMed] [Google Scholar]
- 18.Cohen T, Murray M, Wallengren K, Alvarez GG, Samuel EY, Wilson D, 2010. The prevalence and drug sensitivity of tuberculosis among patients dying in hospital in KwaZulu-Natal, South Africa: a postmortem study. PLoS Med 7: e1000296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong EB, Omar T, Setlhako GJ, Osih R, Feldman C, Murdoch DM, Martinson NA, Bangsberg DR, Venter WD, 2012. Causes of death on antiretroviral therapy: a post-mortem study from South Africa. PLoS One 7: e47542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karat AS, et al. 2016. Autopsy prevalence of tuberculosis and other potentially treatable infections among adults with advanced HIV enrolled in out-patient care in South Africa. PLoS One 11: e0166158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Omar T, Variava E, Moroe E, Billioux A, Chaisson RE, Lebina L, Martinson N, 2015. Undiagnosed TB in adults dying at home from natural causes in a high TB burden setting: a post-mortem study. Int J Tuberc Lung Dis 19: 1320–1325. [DOI] [PubMed] [Google Scholar]
- 22.Agizew T, et al. 2017. Higher-than-expected prevalence of non-tuberculous mycobacteria in HIV setting in Botswana: implications for diagnostic algorithms using Xpert MTB/RIF assay. PLoS One 12: e0189981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bjerrum S, Oliver-Commey J, Kenu E, Lartey M, Newman MJ, Addo KK, Hilleman D, Andersen AB, Johansen IS, 2016. Tuberculosis and non-tuberculous mycobacteria among HIV-infected individuals in Ghana. Trop Med Int Health 21: 1181–1190. [DOI] [PubMed] [Google Scholar]
- 24.Aliyu G, El-Kamary SS, Abimiku A, Brown C, Tracy K, Hungerford L, Blattner W, 2013. Prevalence of non-tuberculous mycobacterial infections among tuberculosis suspects in Nigeria. PLoS One 8: e63170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kobayashi T, Nishijima T, Teruya K, Aoki T, Kikuchi Y, Oka S, Gatanaga H, 2016. High mortality of disseminated non-tuberculous mycobacterial infection in HIV-infected patients in the antiretroviral therapy era. PLoS One 11: e0151682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Varley CD, Ku JH, Henkle E, Schafer SD, Winthrop KL, 2017. Disseminated nontuberculous mycobacteria in HIV-infected patients, Oregon, USA, 2007–2012. Emerg Infect Dis 23: 533–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kharsany ABM, Karim QA, 2016. HIV infection and AIDS in sub-Saharan Africa: current status, challenges and opportunities . Open AIDS J 10: 34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marchevsky A, Damsker B, Gribetz A, Tepper S, Geller SA, 1982. The spectrum of pathology of nontuberculous mycobacterial infections in open-lung biopsy specimens. Am J Clin Pathol 78: 695–700. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.