Abstract
Background:
Little is known about the scope of problems driving referrals to child and adolescent psychiatry services. Identifying the full range of mental disorders affecting a particular child can help triage the child to a clinician with the appropriate level of expertise. The Child Behavior Checklist (CBCL) is an easy-to-use assessment tool that may provide invaluable information regarding the severity of the presenting complaints and also aid in the referral process.
Objective:
To assess the utility of the CBCL to gain insights into the type of clinical problems driving referrals of youth to an outpatient pediatric psychiatry clinic.
Method:
The sample consisted of 418 newly referred youth 4-18 years of age of both sexes. Parents completed the CBCL assessing psychopathology and competence. Rates of patients with elevated T-scores on each scale were calculated for the whole group and stratified by sex and age (≤12 versus >12).
Results:
The CBCL identified high rates of psychopathology affecting referred youth. It also provided information on the type of suspected disorders affecting a particular child as well as their severity, critical information to guide likely differing clinical needs and therapeutic approaches. It also helped identify a high number of youth affected with multiple psychopathological conditions, likely to require a high level of clinical attention. Overall, males were significantly more impaired than females but there were no major differences between children and adolescents.
Conclusions:
The CBCL can aid in the identification of individual and comorbid mental disorders affecting youth seeking mental health services by providing specific information about the presence and the severity of specific suspected disorder. These findings have implications for prioritizing scarce resources in child mental health and for improved consideration of the complexity of clinical presentations to pediatric psychiatry programs of any type.
Keywords: Psychopathology, referral, assessment, CBCL, youth, pediatric psychiatry
Introduction
There is a clear recognition of the limited resources available in child and adolescent psychiatry across the world. For example, in the United States, that is most likely one of the countries with the largest number of child psychiatrists in the world, there are only 9.75 trained child psychiatrists per 100,000 children (1). This is clearly an inadequate number of psychiatrists trained to attend to the large number of youth with mental health needs in general and the many affected with serious psychiatric disorders (1, 2). Yet, surprisingly little is known about the scope of problems driving referrals to child and adolescent psychiatry services to help triage youth with more and less serious forms of psychopathology to the clinician with the most appropriate level of expertise.
While some conditions, such as mild forms of pediatric depression and anxiety, can be addressed with psychosocial interventions (3) disorders like attention-deficit/hyperactivity disorder (ADHD) often require pharmacological interventions (4), and very severe mental disorders such as bipolar disorder need medications and high levels of expertise (5).These issues are further compounded when the child is affected with multiple mental disorders requiring prioritization of care (6). For example, a child referred for the management of depressive symptoms with bipolar features may respond poorly to treatment with antidepressants (7-10). Thus, failure to identify the full range of mental disorders affecting a particular child could have unfavorable consequences for the well-being of the child and affect treatment decisions (10).
While a better understanding of the specific clinical issues driving referrals to a child psychiatry program is essential to better serve the many youth requiring mental health services and provide high quality care, this is not always easy to accomplish. This is so because diagnostic acumen in child mental health programs can be heterogeneous and the level of expertise can be variable. Thus, easy-to-use tools designed to facilitate the assessment of children referred to mental health clinics prior to their clinical visit can be very useful aids for the assessment and management of children with mental health problems in clinical practice.
One such tool is the Child Behavior Checklist (CBCL) (11), an easy-to-use, empirically derived, low-cost dimensional assessment tool of psychopathology that is completed by the parent and provides useful information on broad and specific domains of psychopathology and functioning. It has outstanding psychometric properties and, because it has been translated into many languages, has been widely used across the world. With the responses provided, software generates T-scores for clinical and functioning scales that compare the findings in a referred child with other children of the same age and sex. These T-scores quantify the severity of clinical acuity in a specific domain afflicting the referred child. While the CBCL is well known for introducing the meta-structure of internalizing and externalizing features of psychopathology (12) it also provides detailed information on specific domains of psychopathology and functioning (11). This broad and specific information can help clinicians gain invaluable insights as to the nature and severity of the presenting complaint and associated conditions allowing for the appropriate development of priorities for care.
Research conducted by us and others has documented very good convergence between CBCL clinical scales and clinical diagnoses particularly for the Attention Problems scale with ADHD, the Aggressive Behavior scale with oppositional defiant disorder, the Rule Breaking Behavior scale with conduct disorder, and the Anxious/Depressed and Withdrawn/Depressed scales with anxiety and depressive disorders (13-15) (Table 1). Our group has expanded the clinical use of individual scales by documenting that certain profiles of scales correspond to more complicated clinical diagnoses, particularly the A-A-A profile consisting of the Anxiety/Depression, Aggression, and Attention scales corresponding to a diagnosis of bipolar disorder (16) and the CBCL-Autism Spectrum Disorder (ASD) profile consisting of the Withdrawn/Depressed, Thought Problems and Social Problems profile corresponding to a clinical diagnosis of ASD (17). These results suggest that information gleaned from the CBCL can infer the likely presence of specific disorders.
Table 1.
Documented relationships between the CBCL clinical scales and psychiatric diagnoses
| CBCL clinical scales | CBCL developer confirmed DSM-IV diagnoses | Structured interview derived diagnoses | CBCL clinical scale T-score cut-point | Supporting clinical research |
|---|---|---|---|---|
| Attention problems | Attention-Deficit/Hyperactivity Disorder | Attention-Deficit/Hyperactivity Disorder | >60 | Biederman et al, 1993 |
| Anxious/depressed | All Anxiety Disorders | Multiple (≥2) Anxiety Disorders; Major Depressive Disorder | >60; >55 | Biederman et al., 1993; Uchida et al., 2018 |
| Withdrawn/depressed | Depressive Disorders (Major Depressive Disorder and Dysthymia) | N/A | N/A | N/A |
| Rule-breaking behavior | Conduct Disorder | Conduct Disorder | >60 | Biederman et al., 1993; Yule et al., (in press) |
| Aggressive behavior | Oppositional Defiant Disorder | Oppositional Defiant Disorder | >60 for boys >65 for girls | Biederman et al., 2008 |
| CBCL aggregate scales | ||||
| CBCL-Autistic Traits Profile (Social problems + thought problems + withdrawn/depressed) | N/A | Autism Spectrum Disorder | >195 | Biederman et al., 2010 |
| CBCL-Bipolar Disorder Profile (Attention problems + Aggressive behavior + anxious/depressed) | N/A | Bipolar Disorder | >210 | Faraone et al., 2005 |
Note. N/A = not applicable
Several authors have relied on the CBCL to address different clinical questions. For example, Costello et al.(18) used the CBCL to examine why some disturbed children are brought for treatment while others are not, finding no differences between the groups in the proportions receiving a psychiatric diagnosis, or in the proportions with more than one mental disorder. These findings suggest that untreated children may be no less impaired than those who receive treatment and struggle with significant mental health issues. Katsuki et al. used the CBCL to help identify subgroups of ADHD children defined by specific patterns of emotional and behavioral symptoms. Cluster analysis yielded a solution with four distinct subgroups: 1) “high internalizing/externalizing”, 2) “inattention and internalizing”, 3) “aggression and externalizing” with a high rate of comorbid oppositional defiant disorder and conduct disorder, and 4) “less psychopathology” with low scores on all syndrome scales (19). While noteworthy, these findings provide little guidance for clinicians assessing children with ADHD on how to best approach the management of a particular child with ADHD referred to clinical care.
Mazefsky et al. (20) investigated patterns of CBCL scores in children with high-functioning ASD and IQ- and age-matched controls. Scores on the CBCL Thought and Social Problems scales significantly differentiated children with ASD from controls. Similarly, de Nijs et al. (21) used data from the CBCL to conduct latent class analysis on the Attention Problems, Aggressive Behavior, and Rule-Breaking Behavior scales of the CBCL in a large referred sample of adolescents. Two groups of adolescents with high levels of attention problems were identified: one with high and one with low levels of aggressive and rule-breaking behaviors, suggesting that problems with attention, impulsivity and hyperactivity could be considered as a diagnostic construct that should be distinguished from aggressive or rule-breaking behaviors.
Dimensional approaches to classification of psychopathology, such as the Hierarchical Taxonomy of Psychopathology (HiTOP) (22-24), have been proposed as an alternative taxonomic system for a wide range of psychiatric problems. Yet, its application to clinical practice has been lacking. While it is true that mental health problems lie on the continuum between pathology and normality, for treatment purposes we still need to provide a boundary, however artificial it may be, to help distinguish what is a healthy behavior versus mental illness, much like defining obesity and hypertension despite lying on the continuums of weight and blood pressure, respectively.
The continuum approach to the problem of comorbidity has provided important insights into the structure of psychopathology by modeling patterns of co-occurrence among signs and symptoms within a varied hierarchy of dimensional concepts (22). These findings have also been confirmed by genome-wide association studies which show that genetic liability is a continuous, polygenic trait that is partially shared among disorders (25). The pervasiveness of psychiatric comorbidity is particularly relevant in clinical practice since it is well recognized that it represents a major source of morbidity and dysfunction in pediatric psychiatry (4, 26-30). Clinicians, however, need a validated means of translating dimensional measures of comorbidity into decision thresholds that can be used to identify patients in need of additional treatments. For example, the presence of comorbidity may signal the need for different clinical and therapeutic approaches as well as prioritization of care (6).
Mattison el al. (31) discussed Cantwell’s (1996) (32) argument that specific ADHD comorbidity patterns may have both etiological and treatment implications. Research on CBCL scales (33, 34) found that comorbid clinical elevations on specific pairs of scales may have prognostic implications, indicating a worse prognosis, compared with only single elevations (31). Thus, despite its limitations, clinical diagnosis and attention to comorbidity are important in clinical practice because they have important prognostic and therapeutic implications, issues that are important for everyday psychiatric care. From this point of view, continuous and categorical taxonomic systems can be viewed as complimentary to each other rather than competing.
The main aim of this study was to evaluate the utility of the CBCL to aid in characterizing specific domains of psychopathology and dysfunction affecting youth referred to a child and adolescent clinic with the overarching goal of gaining better insights as to the specific problems driving clinical referrals. We believe that this knowledge can facilitate the triage of referred youth to the clinician with the most appropriate expertise to manage the particular set of problems and thereby improve care and outcomes of affected youth.
Methods
Sample
Our sample consisted of 418 newly referred children and adolescents 4-18 years of age of both sexes who presented to a child psychiatry outpatient clinic at Massachusetts General Hospital between September 2016 and August 2019. There was no selection bias based on social class or insurance restrictions. We received institutional review board approval to review, analyze, and report anonymously on these subjects.
Assessment procedures
The parent or guardian of each patient completed a battery of rating scales before their child’s initial evaluation. Medication history collected information on current and past treatments for ADHD and other disorders. The Child Behavior Checklist (CBCL) is a 113-item parent-rated assessment of a child’s behavior problems and social competence (11). Raw scores are calculated and used to generate T-scores for eight clinical subscales, two composite scales, one total scale, and four competence scales. The creators of the CBCL used 1,753 non-referred children to construct their norms (11). These non-referred children had not had any mental health, substance abuse, or special educational services in the 12 months preceding when the parent completed the assessment. Norms were developed separately for each sex (male or female) and age group (6-11 and 12-18). T-scores ≥70 are in the clinical range for the clinical subscales, T-scores ≥64 are in the clinical range for the composite scales and total scale, and T-scores ≤30 are in the clinical range for the competence scales. As described in a previous study (35), emotional dysregulation was defined as an aggregate T-score of ≥210 on the Attention Problems, Aggressive Behavior, and Anxious/Depressed scales. Autistic traits were defined as an aggregate score ≥195 on the Withdrawn/Depressed, Social Problems, and Thought Problems scales (17).
Statistical analysis
We examined the clinical profile of the entire group by calculating the percentage of subjects with scores in the clinical and subclinical range for each clinical scale of the CBCL. As previously reported, subthreshold scores are clinically meaningful (36, 37). We performed two stratified analyses by sex and age and compared the profile of males versus females and patients ≤12 years of age versus patients >12 years of age using logistic and ordered logistic regression models depending on the distribution of the data. All tests were two-tailed and performed at the 0.05 alpha level using Stata (Version 16.0) (38). Descriptive statistics are presented as means ± standard deviations or counts and percentages.
Results
Socio-Demographic and clinical characteristics Socio-demographic and clinical characteristics are presented in Table 2. Patients had an average age of 11.2 ± 3.6 years. Sixty percent were ≤12 years of age, 67% (N=282/418) were male, 75% (N=314/418) were Caucasian, 62% (N=252/407) had a lifetime history of psychiatric medications, and 54% (N=218/407) were currently taking psychiatric medications.
Table 2.
Demographic characteristics of 418 youths presenting to child psychiatry outpatient clinics
| Total sample N=418 (Mean ± SD) | |
| Age (years) | 11.2 ± 3.6 |
| N (%) | |
| Age ≤12 | 251 (60) |
| Male | 282 (67) |
| Race | |
| Asian; Native Hawaiian/Pacific Islander | 15 (3.5) |
| Black/African American | 12 (3) |
| Caucasian | 314 (75) |
| Hispanic/Latino | 16 (4) |
| More than one race | 46 (11) |
| Unknown or unreported | 15 (3.5) |
| Lifetime history of psychiatric medications | 252 (62) |
| N=407 | |
| Currently taking psychiatric medications N=407 | 218 (54) |
Child Behavior Checklist (CBCL) profiles
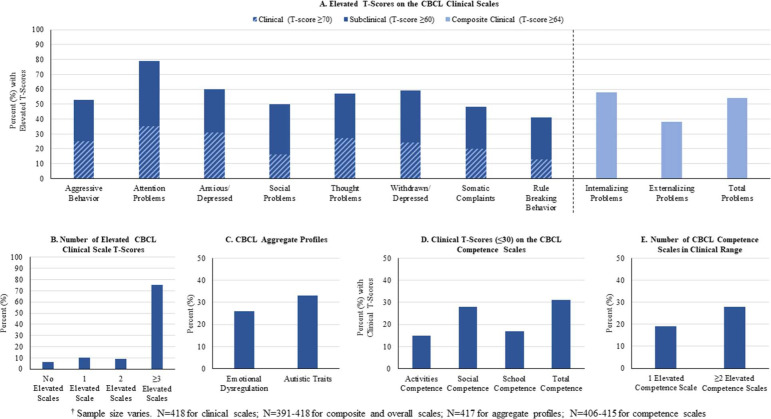
As shown in Figure 1A, the Attention Problems scale was the most commonly elevated scale with 79% (N=332/418) of patients having clinical (≥70) or subclinical (≥60) T-scores, followed by the Anxious/Depressed (60%; N=250/418) and Withdrawn/Depressed (59%; N=246/418) scales. Examining the composite scales, 38% (N=155/405) had Externalizing Problems T-scores in the clinical range (≥64) and 58% (N=226/391) had Internalizing Problems T-scores in the clinical range (≥64). Overall, 54% (N=225/418) had Total Problems T-scores in the clinical range (≥64). As shown in Figure 1B, using T-scores ≥60 to define elevated scales, 75% (N=316/418) had at least three elevated scales. Examining the aggregate CBCL profiles, 26% (N=109/417) of patients had emotional dysregulation (aggregate T-score ≥210) and 33% (N=137/417) had autistic traits (aggregate T-score ≥195) (Figure 1C).
FIGURE 1.
Child Behavior Checklist (CBCL) Profiles of 418’ Youths Presenting to Child Psychiatry Outpatient Clinics
Consistent with the clinical findings were the functional findings. As shown in Figure 1D, rates of patients with T-scores in the clinical range (≤30) on the Competence scales ranged from 15% (N=60/406) for Activities Competence to 28% (N=117/415) for Social Competence, with 31% of patients (N=124/406) having a Total Competence T-scores in the clinical range. Twenty-eight percent (N=115/411) of patients had at least two abnormal competence scales (Figure 1E).
Examination of covariates: Sex and age
The first stratified analysis compared males (N=282) and females (N=136). As shown in Figure 2A, a significantly greater percentage of males compared to females had clinical (≥70) or subclinical (≥60) T-scores on the Aggressive Behavior, Attention Problems, Social Problems, Thought Problems, and Rule Breaking Behavior scales (all p<0.05), as well as clinical (≥64) T-scores on the Externalizing Problems and Total Problems composite scales (both p<0.05). There was a significant difference in the number of elevated scales with a greater percentage of males compared to females having at least three elevated scales (p=0.02) (Figure 2B). Further, a significantly greater percentage of males compared to females had autistic traits (aggregate T-score ≥195) (p=0.04) (Figure 2C). Examining the competence scales, a greater percentage of males compared to females had clinical (≤30) T-scores on the Social Competence and Total Competence scales (both p<0.05) (Figure 2D) and had ≥2 elevated competence scales (p=0.01) (Figure 2E).
FIGURE 2.
Child Behavior Checklist (CBCL) Profiles of 418’ Youths Presenting to Child Psychiatry Outpatient Clinics Stratified by Sex
The second stratified analysis compared patients ≤12 year of age (N=251) and patients >12 years of age (N=167). As shown in Figure 3A, a significantly greater percentage of patients >12 compared to patients ≤12 had clinical (≥70) or subclinical (≥60) T-scores on the Withdrawn/Depressed and Somatic Complaints scales (all p<0.05). Conversely, a significantly greater percentage of patients ≤12 compared to patients >12 had clinical (≥70) or subclinical (≥60) T-scores on the Aggressive Behavior and Rule Breaking Behavior scales (all p<0.05). There were no significant differences between patients >12 and patients ≤12 in the number of elevated scales (Figure 3B) or in the percentage of those with elevated scores on the aggregate profiles (Figure 3C). There were also no differences between the two groups in rates of clinical scores on any of the competence scales or in the number of impaired competence scales (all p>0.05) (Figures 3D & 3E).
FIGURE 3.
Child Behavior Checklist (CBCL) Profiles of 418’ Youths Presenting to Child Psychiatry Outpatient Clinics Stratified by Age
Discussion
The main aim of this study was to assess the utility of the CBCL for characterizing the type of psychopathology and dysfunction affecting youth referred to a child psychiatry clinic in a manner that would be useful as a screening tool in clinical settings. Findings reveal that the CBCL clinical scales identify specific disorders with very different clinical needs, thereby providing clinicians with useful information to begin to address patients’ individual clinical needs.
Strengths of this study include its large sample size of youth referred to a pediatric psychiatric clinic with a large representation of children and adolescents of both sexes. Additional strengths include the fact that the CBCL was used in the assessment of all referrals and that it was completed at baseline before the patients were seen. Furthermore, our clinic operates in an institution that accepts public and private insurances, including patients and families on public assistance, as well as all social classes and ethnic groups, adding to the generalizability of findings. Also, a strength is the fact that close to half of the sample has never been previously medicated, which supports the idea that the sample is not biased towards tertiary care referrals.
Our search of the extant literature failed to identify previous studies evaluating systematic methods to help identify the type of diagnostic problems that drive referrals of pediatric patients seeking mental health services. Considering the scarcity of resources in child and adolescent psychiatry, more information on this topic can help provide better guidelines for matching youth with mental health disorders to the most appropriate clinical service to provide high quality of care.
The preponderance of males over females in our sample is consistent with the literature that suggests that boys are at higher risk for psychopathology and dysfunction, at least early in development. Although the reason for this apparent female protective effect against the development of impairments is not entirely clear, it is possible that they could be driven by neurobiological dimorphism between the sexes in the expression of psychopathology and dysfunction (39).
In contrast, there were fewer differences in comparisons examining age effects indicating that preadolescent children have as high a vulnerability to psychopathology and dysfunction as adolescents. This emphasizes the importance of assessing children presenting to clinical practice and intervening to minimize the risk of future complications and impairment
Although our psychopathological findings relied on the CBCL, previous research conducted by us and others documents very good convergence between the CBCL Attention Problems scale with ADHD, the CBCL Aggressive Behavior scale with oppositional defiant disorder, the Rule Breaking Behavior with conduct disorders, and the Anxiety/Depression and Withdrawal scales with anxiety and depressive disorders (13-15). Moreover, previous work also documented the correspondence between specific CBCL scale profiles with more complicated clinical diagnoses, such as the Anxiety/Depression-Aggression-Attention profile corresponding to a structured interview diagnosis of bipolar disorder (16) and the CBCL autism spectrum profile corresponding to a clinical diagnosis of autism spectrum disorder (17).
Our results showing that most of the referrals consisted of youth with multiple psychopathological conditions emphasize that psychiatric comorbidity is the rule rather than the exception in youth referred to specialty mental health services. These findings mapping the scope of potential mental disorders affecting the referred child with a simple-to-use instrument have important implications for clinical care, providing individualized treatment, and avoiding complications stemming from inadequate attention to the presence of co-occurring mental disorders. In many settings, time constraints and variable levels of expertise do not allow all clinicians to assess all forms of psychopathology. As a result, comorbid conditions may not be identified. Easy-to-use assessment instruments like the CBCL could greatly facilitate the identification of children who need additional diagnostic workup or require a more specialized clinician.
Our findings need to be viewed considering some methodological limitations. Our findings relied on the CBCL, therefore we do not know whether other instruments may have led to similar or different results. For example, Goodman et al. (40) used a computerized algorithm to predict child psychiatric diagnoses on the basis of the symptom and impact scores derived from Strengths and Difficulties Questionnaire (SDQs) applied to patients attending child mental health clinics in Britain (N = 101) and Bangladesh (N =89). The level of chance-corrected agreement between SDQ prediction and an independent clinical diagnosis was substantial and highly significant suggesting that it could be of practical value in planning the assessment of new referrals to a child mental health service. These findings stress impairment as a key determinant of the need for referral and an aid for prioritization. Clearly more work is needed to further evaluate these important issues.
Although we did not have a comparison group of non-referred individuals, our focus was on aiding diagnostic issues in clinical referrals. Moreover, the CBCL T-scores provide normative data from other children of the same age and sex in the population. Additionally, while a more comprehensive picture of the child could have been obtained if the companion youth and teacher report versions of the CBCL were to have been completed, the parent report is certainly highly informative (41) and teacher reports are not always available. Future studies should examine the contribution of teacher reports.
The CBCL was collected before the clinical evaluation and we do not have information on how this report was utilized by the clinical team. Future studies should examine how pediatric mental health administrators could use this information to match patients with the most appropriate clinician.
Although our findings are limited to a single clinic in a major metropolitan area, the reported data were derived from a large, unselected sample of consecutively referred outpatients from all ethnic and social class groups, with a sizeable representation of pre-adolescent and adolescent patients, males and females, and previously medicated and medication naïve subjects, providing generalizable findings to other child psychiatry services.
Despite these considerations, our results showed that the CBCL can be a useful instrument to identify the type and severity of psychopathological conditions affecting youth refereed to mental health services. Because the CBCL is easy to use in most clinical settings, its use would likely improve the identification and appropriate treatment of simple and complex cases.
Clinical significance
The present study evaluated the utility of the CBCL to help characterize specific domains of psychopathology and dysfunction affecting youth referred to a child and adolescent psychiatry clinic. Findings reveal that the CBCL clinical scales identify specific disorders with likely differing clinical needs and therapeutic approaches. The CBCL also identified a high number of youth affected with multiple psychopathological conditions, likely to require a high level of clinical attention. These findings have implications for prioritizing scarce resources in child mental health and for improved consideration of the complexity of clinical presentations to pediatric psychiatry programs of any type.
Footnotes
Conflicts of interest
Dr. Biederman reports research support from: MGH Pediatric Psychopharmacology Council Fund, American Academy of Child and Adolescent Psychiatry, Feinstein Institute for Medical Research, Food & Drug Administration, Genentech, Headspace Inc., National Institute on Drug Abuse, Pfizer Pharmaceuticals Inc., Tris, National Institutes of Health, Lundbeck AS, and Neurocentriaa Inc. during the conduct of the study. Departmental Royalties from copyrighted rating scale used for ADHD diagnoses from: Bracket Global, Ingenix, Prophase, Shire, Sunovion, and Theravance outside the submitted work. In addition, Dr. Biederman has a patent US Patent (#14/027,676) licensed to MGH Corporate Licensing, a patent US Patent (#10,245,271 B2) licensed to MGH Corporate Licensing, and a patent (#61/233,686) pending.
Dr. Vaudreuil reports that the study was supported in part from Louis V. Gerstner III Research Scholars Program, during the conduct of the study.
Dr. Wozniak reports research support from PCORI, Demarest Lloyd, Jr. Foundation, Eli Lilly, Janssen, McNeil, Merck/Schering-Plough, National Institutes of Mental Health, Pfizer, Shire, other from Bantam Books, outside the submitted work.
Dr. Faraone reports income, potential income, travel expenses, continuing education support and/or research support from Rhodes, OnDosis, Tris, Otsuka, Arbor, Ironshore, Takeda, and Genomind; research support from Shire, Enzymotec, Neurovance, Alcobra, CogCubed, KemPharm, Neurolifesciences Lundenback/Takeda, Otsuka, other from McNeil, Janssen, Novartis, Pfizer, and Eli Lilly; royalties from from Guiliford Press, Oxford University Press, and Elsevier. Dr. Faraone is Principal Investigator at www.adhdinadults.com outside the submitted work.
Drs. Maura DiSalvo, Mai Uchida, K. Yvonne Woodworth and Allison Green report no conflicts of interest.
References
- 1.McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, Yu H.. Growth and distribution of child psychiatrists in the United States: 2007-2016. Pediatrics 2019;144(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.University of Michigan Behavioral Health Workforce Research Center Estimating the Distribution of the U.S. Psychiatric Subspecialist Workforce. Ann Arbor, MI: UMSPH; 2018. [Google Scholar]
- 3.March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J,. et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 2004;292(7):807-20. [DOI] [PubMed] [Google Scholar]
- 4.Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA,. et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers 2015;1:15020. [DOI] [PubMed] [Google Scholar]
- 5.Liu B, Zhang Y, Fang H, Liu J, Liu T, Li L.. Efficacy and safety of long-term antidepressant treatment for bipolar disorders - A meta-analysis of randomized controlled trials. J Affect Disord 2017;223:41-8. [DOI] [PubMed] [Google Scholar]
- 6.Wilens T, Spencer T, Biederman J, Wozniak J, Connor D.. Combined pharmacotherapy: An emerging trend in pediatric psychopharmacology. J Am Acad Child Adolesc Psychiatry 1994;34(1):110-2. [DOI] [PubMed] [Google Scholar]
- 7.Faedda GL, Baldessarini RJ, Glovinsky IP, Austin NB.. Treatment-emergent mania in pediatric bipolar disorder: A retrospective case review. J Affect Disord 2004;82(1):149-58. [DOI] [PubMed] [Google Scholar]
- 8.Akiskal HS, Benazzi F.. Psychopathologic correlates of suicidal ideation in major depressive outpatients: is it all due to unrecognized (bipolar) depressive mixed states? Psychopathology 2005;38(5):273-80. [DOI] [PubMed] [Google Scholar]
- 9.Baldessarini RJ, Faedda GL, Hennen J.. Risk of mania with antidepressants. Arch Pediatr Adolesc Med 2005;159(3):298; author reply 298-9. [DOI] [PubMed] [Google Scholar]
- 10.Wilens T, Biederman J, Kwon A, Chase R, Greenberg L, Mick E,. et al. A systematic chart review of the nature of psychiatric adverse effects in children and adolescents treated with selective serotonin reuptake inhibitors. J Child Adolesc Psychopharmacol 2003;13:143-52. [DOI] [PubMed] [Google Scholar]
- 11.Achenbach TM.. Manual for the Child Behavior Checklist/4-18 and the 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 12.Achenbach TM, Ivanova MY, Rescorla LA.. Empirically based assessment and taxonomy of psychopathology for ages 1(1/2)-90+ years: Developmental, multi-informant, and multicultural findings. Compr Psychiatry 2017;79:4-18. [DOI] [PubMed] [Google Scholar]
- 13.Chen W, Faraone S, Biederman J, Tsuang M.. Diagnostic accuracy of the child behavior checklist scales for attention deficit hyperactivity disorder: A receiver operating characteristic analysis. J Consult Clin Psychol 1994;62(5):1017-25. [DOI] [PubMed] [Google Scholar]
- 14.Biederman J, Monuteaux M, Kendrick E, Klein K, Faraone S.. The CBCL as a screen for psychiatric comorbidity in pediatric patients with ADHD. Arch Dis Child 2005;90(10):1010-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biederman J, Ball SW, Monuteaux MC, Kaiser R, Faraone SV.. CBCL clinical scales discriminate ADHD youth with structured-interview derived diagnosis of oppositional defiant disorder (ODD). J Atten Disord 2008;12(1):76-82. [DOI] [PubMed] [Google Scholar]
- 16.Faraone SV, Althoff RR, Hudziak JJ, Monuteaux MC, Biederman J.. The CBCL predicts DSM bipolar disorder in children: A receiver operating characteristic curve analysis. Bipolar Disord 2005;7(6):518-24. [DOI] [PubMed] [Google Scholar]
- 17.Biederman J, Petty CR, Fried R, Wozniak J, Micco JA, Henin A,. et al. Child behavior checklist clinical scales discriminate referred youth with autism spectrum disorder: a preliminary study. J Dev Behav Pediatr 2010;31(6):485-90. [DOI] [PubMed] [Google Scholar]
- 18.Costello EJ, Janiszewski S.. Who gets treated? Factors associated with referral in children with psychiatric disorders. Acta Psychiatr Scand 1990;81(6):523-9. [DOI] [PubMed] [Google Scholar]
- 19.Katsuki D, Yamashita H, Yamane K, Kanba S, Yoshida K.. Clinical subtypes in children with attention deficit hyperactivity disorder according to their Child Behavior Checklist profile. Child Psychiatry Hum Dev 2020. https://doi:10.1007/s10578-020-00977-8. Epub ahead of print [DOI] [PubMed]
- 20.Mazefsky CA, Anderson R, Conner CM, Minshew N.. Child Behavior Checklist scores for school-aged children with autism: Preliminary evidence of patterns suggesting the need for referral. J Psychopathol Behav Assess 2011;33(1):31-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Nijs PF, van Lier PA, Verhulst FC, Ferdinand RF.. Classes of disruptive behavior problems in referred adolescents. Psychopathology 2007;40(6):440-5. [DOI] [PubMed] [Google Scholar]
- 22.Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ,. et al. Progress in achieving quantitative classification of psychopathology. World Psychiatry 2018;17(3):282-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruggero CJ, Kotov R, Hopwood CJ, First M, Clark LA, Skodol AE,. et al. Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. J Consult Clin Psychol 2019;87(12):1069-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R,. et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect Psychol Sci 2019;14(3):419-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smoller JW, Andreassen OA, Edenberg HJ, Faraone SV, Glatt SJ, Kendler KS.. Psychiatric genetics and the structure of psychopathology. Mol Psychiatry 2018. [DOI] [PMC free article] [PubMed]
- 26.Biederman J, Newcorn J, Sprich S.. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 1991;148(5):564-77. [DOI] [PubMed] [Google Scholar]
- 27.Biederman J, Petty CR, O’Connor KB, Hyder LL, Faraone SV.. Predictors of persistence in girls with attention deficit hyperactivity disorder: results from an 11-year controlled follow-up study. Acta Psychiatr Scand. 2012;125(2):147-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biederman J, Petty CR, Evans M, Small J, Faraone SV.. How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res 2010;177(3):299-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elia J, Ambrosini P, Berrettini W.. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health 2008;2(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention Mental health in the United States. Prevalence of diagnosis and medication treatment for attention-deficit/hyperactivity disorder--United States, 2003. MMWR Morb Mortal Wkly Rep 2005;54(34):842-7. [PubMed] [Google Scholar]
- 31.Mattison R, Spitznagel E.. Long-term stability of Child Behavior Checklist Profile types in a child psychiatric clinic population. J Am Acad Child Adolesc Psychiatry 1999;38(6):700-7. [DOI] [PubMed] [Google Scholar]
- 32.Cantwell DP.. Attention deficit disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1996;35(8):978-87. [DOI] [PubMed] [Google Scholar]
- 33.MacDonald VM, Achenbach TM.. Attention problems versus conduct problems as 6-year predictors of signs of disturbance in a national sample. J Am Acad Child Adolesc Psychiatry 1999;38(10):1254-61. [DOI] [PubMed] [Google Scholar]
- 34.Verhulst F, van der Ende J.. “Comorbidity” in an epidemiological sample: A longitudinal perspective. J Child Psychol Psychiatry 1993;34(5):767-83. [DOI] [PubMed] [Google Scholar]
- 35.Yule A, Fitzgerald M, Wilens T, Wozniak J, Woodworth KY, Pulli A,. et al. Further evidence of the Diagnostic Utility of the Child Behavior Checklist for identifying pediatric Bipolar I Disorder. Scan J Child Adolesc Psychiatry Psychol 2019;7:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kirova AM, Kelberman C, Storch B, DiSalvo M, Woodworth KY, Faraone SV,. et al. Are subsyndromal manifestations of attention deficit hyperactivity disorder morbid in children? A systematic qualitative review of the literature with meta-analysis. Psychiatry Res 2019;274:75-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaudreuil CAH, Faraone SV, Di Salvo M, Wozniak JR, Wolenski RA, Carrellas NW,. et al. The morbidity of subthreshold pediatric bipolar disorder: A systematic literature review and meta-analysis. Bipolar Disord 2019;21(1):16-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.StataCorp Stata Statistical Software: Release 16. College Station, TX: StatCorp LLC; 2019. [Google Scholar]
- 39.Mahone EM, Wodka EL.. The neurobiological profile of girls with ADHD. Dev Disabil Res Rev 2008;14(4):276-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goodman R, Renfrew D, Mullick M.. Predicting type of psychiatric disorder from Strengths and Difficulties Questionnaire (SDQ) scores in child mental health clinics in London and Dhaka. Eur Child Adolesc Psychiatry 2000;9(2):129-34. [DOI] [PubMed] [Google Scholar]
- 41.Biederman J, Faraone SV, Milberger S, Doyle AE.. Diagnoses of attention deficit hyperactivity disorder from parent reports predict diagnoses based on teacher reports. J Am Acad Child Adolesc Psychiatry 1993;32(2):315-7. [DOI] [PubMed] [Google Scholar]