Abstract
Purpose
The COVID-19 pandemic brought several challenges to cancer practice, especially in ensuring continuity of treatment during this period while minimizing the risks of transmission to a vulnerable population. For radiation oncology departments in Brazil, this contingency has become even more complex owing to the significant effect observed in different sectors of society and the large number of COVID-19 cases and deaths. This study estimated the effect of the COVID-19 pandemic on Brazilian radiation oncology departments and the coping measures used in the country.
Methods and Materials
The Brazilian Radiotherapy Society developed a questionnaire, with 14 questions, that were sent to all heads of radiation oncology departments in the country between May and June 2020. These data were evaluated regarding cases confirmed and deaths by COVID-19 in epidemiologic week 28, on July 11, 2020.
Results
One hundred twenty-six questionnaires from different regions were answered, representing 44% of the country’s services. A drop in the number of patients was observed in 61% of services. This drop was observed both in patients from the public and supplementary private health insurance systems. Regarding patients and employees with COVID-19, we observed that services that primarily treat Unified Health System patients reported significantly fewer cases of the disease. About half of the services had collaborators and patients during radiation therapy with a positive diagnosis of COVID-19. Among the coping measures, the services used intensified hygiene and cleanliness practices, interpersonal distancing, restrictions on access to companions, and other changes in daily practice.
Conclusions
Thus, there was an important drop in the number of radiation therapy patients in the country during the pandemic, and this effect was similar among the services, regardless of the characteristics of the patients and the departments’ coping measures adopted during the pandemic.
Introduction
COVID-19 was declared a pandemic by the World Health Organization, given the growing incidence and the complex repercussions observed in different social environments worldwide, requiring comprehensive care for the population, especially those with associated comorbidities.1 In this context, patients with cancer have a higher risk of severe infections and mortality, especially during cancer treatment when they are vulnerable. The COVID-19 and Cancer Consortium2 and Thoracic Cancers International COVID-19 Collaboration3 ran studies on patients with COVID-19. They identified that patients with advanced age, male gender, impaired functional status, and associated comorbidities, such as hypertension, chronic lung disease, diabetes, and those with active cancer who are under treatment have a higher risk of morbidity and mortality.2, 3, 4, 5
To minimize the effect of the intense demand caused by the increase in the number of contaminants in the country, above its installed capacities, several contingency measures for health services have been proposed to guarantee access to patients with severe acute respiratory syndrome (SARS) caused by the new coronavirus (severe acute respiratory syndrome corona virus-2 [SARS-CoV-2]). Thus, medical care considered elective and those procedures of less complexity and low risk of aggravation were suspended in almost all health services in Brazil. However, even patients with a high suspicion of cancer had delayed diagnosis and treatment.
Universal and comprehensive health care is guaranteed by the Unified Health System (SUS). Still, the country is facing a restriction of access to public health due to insufficient resources and structure to meet the needs of the Brazilian population. This structural deficiency made it challenging to face the COVID-19 pandemic and hampered the maintenance of essential health programs, such as cancer care. Also, about 22% of the country’s population has additional assistance through supplementary private health insurance, managed by the private health sector.6 It is observed that the pandemic has affected supplementary private health insurance services, which have suffered from the burden of patients diagnosed with SARS and are often forced to suspend or delay the diagnosis and treatment of other diseases.
Radiation oncology departments are sensitive and dependent on diagnostic confirmation and therapeutic indication in cancer care. It is necessary to assess the changes caused by social isolation measures and the suspension of elective services. The Brazilian Radiotherapy Society (SBRT) developed guidelines for tackling the pandemic to guide the conduct of the country’s services. These guidelines recommended interpersonal distancing, restricted access, hygiene protocols, cleaning common facilities, reorganization of the flow of care for suspected and confirmed patients without the possibility of temporary leave.
Considering the deficiency of cancer care that existed before the COVID-19 pandemic, aggravated by the restriction of access to specialized cancer services and by the restriction on diagnostic and therapeutic tests, we intended to estimate the effect of the COVID-19 pandemic on Brazilian radiation oncology departments, also analyzing the actions taken to fight the pandemic.
Methods and Materials
The SBRT established the COVID-19 Coping Committee (CERT) in April 2020 to elaborate on coping actions and guidelines for the country’s radiation oncology departments during the pandemic period. Among the actions of CERT, a questionnaire was prepared, addressed to the heads of radiation therapy departments, and sent digitally in May to the 284 services in the country. CERT prepared the questionnaire with 14 multiple choice questions about the service profile and actions to deal with the COVID-19 pandemic. The service profile was addressed, asking about the average number of monthly visits and the origin of patients, whether they had public or supplementary private health insurance, the percentage range of effect on the number of patients undergoing treatment due to the pandemic, and the causes of the reduction in treatments. The frequency and actions concerning patients and collaborators contaminated by SARS-CoV-2 and the prevention policies adopted by the services were also addressed.
Data analysis was performed using MedCalc Statistical Software version 16.4.3 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2016). Numerical data were reported as a percentage or median with quartile intervals. Categorical variables were compared using the χ2 test with Yates correction. The data analyses were performed on July 11, 2020, which was epidemiologic week 28. Statistical significance was considered as a 2-tailed P < .05.
Results
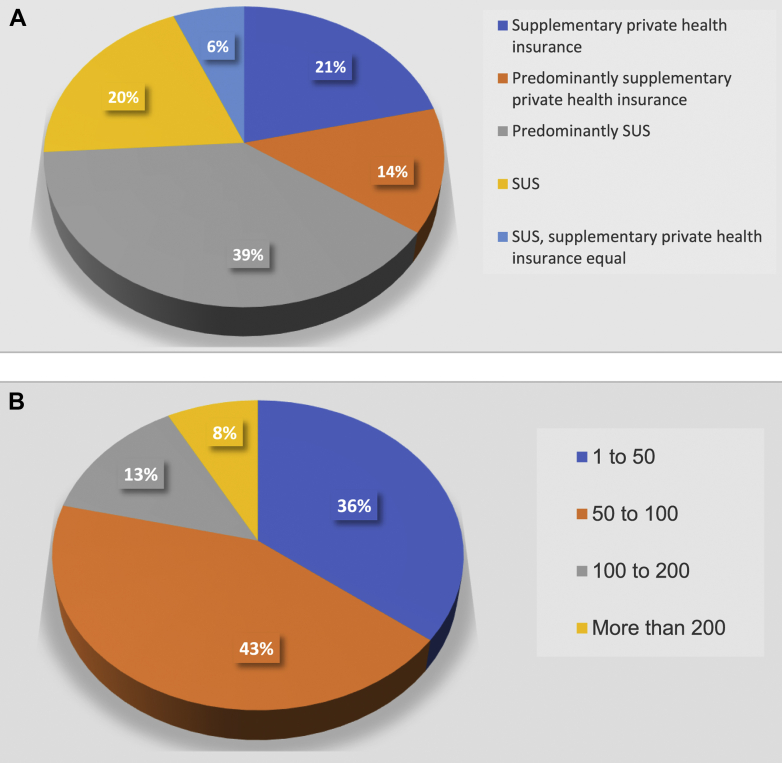
In total, 126 responses came from 24 Federative Units in the 5 regions of Brazil. These represent 44.4% of the 284 radiation oncology departments in the country. Most responses came from the state of São Paulo (37; 29.4%), Rio Grande do Sul (21; 16.6%), Minas Gerais (17; 13.4%), Rio de Janeiro (11; 8.7%), Bahia (5; 4%), Goiás, Ceará, and Paraná (4; 3.2%). The rest of the responses came from 13 Federative Units and the Federal District. There were no responses from services in the state of Rondônia. The states of Amapá and Roraima do not have radiation oncology departments. Considering the Brazilian regions, the answers were from services in the southeast (66; 52.4%), south (26; 20.6%), northeast (20; 15.9%), midwest and Federal District (9; 7.1%), and north (5; 4.1%). The answers concerning the origin of patients and the volume of patients treated are shown in Figure 1.
Figure 1.
Characteristics of the answering services. (A) Origin of patients (Unified Health System [SUS] or supplementary private health insurance). (B) Capacity of radiation oncology departments and the number of patients treated per day at the service.
The percentage drop in patient care during the pandemic period was asked about. Considering the drop, about 59% of the services reported a reduction greater than 20%. Of these, about 14% reported a reduction greater than 50% of patients undergoing radiation therapy (Table 1). The reduction was proportionally similar in the origin of the patients, with a decrease both in patients coming from supplementary private health insurance and SUS patients (Table 2).
Table 1.
Percentage drop in patient care during the COVID-19 pandemic in radiation oncology departments in Brazil
| Drop percentage | No. | % |
|---|---|---|
| Less than 20% | 34 | 27.0 |
| Between 20%-50% | 59 | 46.8 |
| More than 50% | 18 | 14.3 |
| No drop | 15 | 11.9 |
| Total | 126 | 100.0 |
Table 2.
Patient systems responsible for the drop in care during the COVID-19 pandemic in radiation oncology departments in Brazil
| Origin | No. | % |
|---|---|---|
| Supplementary private health insurance | 27 | 28.4 |
| Predominantly supplementary private health insurance | 15 | 15.8 |
| Predominantly SUS | 18 | 18.9 |
| SUS | 27 | 28.4 |
| SUS, supplementary private health insurance (equal proportions) | 8 | 8.4 |
| Total | 95 | 100.0 |
Abbreviation: SUS = Unified Health System.
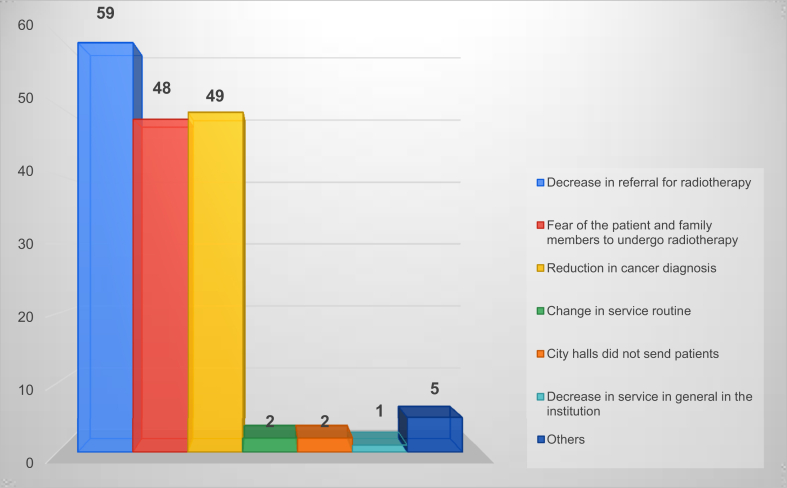
The causes for the decrease in the number of patients undergoing treatment were a decrease in referrals (36%), patient or family fear (30%), and a reduction in cancer diagnosis (30%) (Fig 2).
Figure 2.
Causes of the drop in patient care during the pandemic.
Regarding the diagnosis of COVID-19, it was asked whether radiation therapy was attended by any patient diagnosed with the disease. Sixty-six services, corresponding to 52% of respondents, claimed to have patients with the disease. In the same vein, it was asked whether the service detected any collaborator with the pathology. Sixty-eight respondents (54%) stated that their employees tested positive.
Of the patients with COVID-19, 39 (34.5%) discontinued treatment, and 30 (26%) maintained therapy after the closing time of the service to isolate those infected. The main measures to prevent the transmission of SARS-COV-2 were the intensification of hygiene and cleaning measures in 126 services, distancing measures used by 123 services, use of personal protective equipment by employees was instituted in 122 services, and restricted companion access for healthy patients was employed in 117 services. Among the least used, we have the temporary suspension of weekly reviews by 67 services, postponing the start of radiation therapy in 65 services, and testing in employees and patients was adopted in 33 services. The conduct related to contaminated patients and measures for the prevention of contagion are presented in Table 3.
Table 3.
Conduct toward patients with COVID-19 and contagion containment measures during the COVID-19 pandemic in radiation oncology departments in Brazil
| Conduct related to the patient with COVID-19 | No. | % |
|---|---|---|
| Interruption of radiation therapy and isolation | 39 | 34.5 |
| There was no positive patient | 37 | 32.7 |
| Radiation therapy performed at the end of the day | 30 | 26.5 |
| Another conduct other than those described above | 7 | 6.2 |
| Total | 113 | 100.0 |
| Prevention measures for the transmission of SARS-COV-2 | n | % |
|---|---|---|
| Intensification of hygiene and cleaning service measures | 126 | 15.2 |
| Distancing measures | 123 | 14.9 |
| Use of PPE by employees | 122 | 14.7 |
| Restriction of companion access for healthy patients | 117 | 14.1 |
| Change in practices and routines (eg, hypofractionation) | 90 | 10.9 |
| Access monitoring (eg, use of thermometer at service entrances) | 85 | 10.3 |
| Temporary suspension of weekly reviews | 67 | 8.1 |
| Postponing the start of radiation therapy | 65 | 7.9 |
| Testing on employees and patients | 33 | 4.0 |
| Total | 828 | 100.0 |
Abbreviations: PPE = personal protective equipment; SARS-COV-2 = severe acute respiratory syndrome corona virus-2.
There was a practice of rotation of assistance teams during the pandemic period. Questioned about the practice, 44 services (34.9%) claimed to perform such rotation. Table 4 shows the χ2 association tests for the different responses obtained in the questionnaire. The services that presented patients or collaborators with COVID-19 had a similar distribution among the regions of the country and service characteristics. However, we observed that primarily public healthcare services (SUS) reported significantly fewer cases among patients and staff COVID-19 infection than private supplemental healthcare services. Size of the department, patient origin, and the number of COVID-19 infected patients and employees correlated with a drop in the volume of treatment by more significant than 50% and staff turnover.
Table 4.
Chi-square analysis with Yates correction for categorized variables
| Categorization | Frequency (%) | χ2 | P value | Contingency | |
|---|---|---|---|---|---|
| Patients diagnosed COVID-19 | No patients diagnosed COVID-19 | ||||
| Less than 100 new cases/mo | 50 (50.5) | 49 (49.5) | |||
| 100 new cases or more/mo | 16 (59.3) | 11 (40.7) | |||
| Total | 66 (52.4) | 60 (47.6) | 0.348 | .555 | 0.052 |
| Patients diagnosed COVID-19 | No patients diagnosed COVID-19 | ||||
| Not predominantly SUS | 34 (65.4) | 18 (34.6) | |||
| Predominantly SUS | 32 (43.2) | 42 (56.8) | |||
| Total | 66 (52.4) | 60 (47.6) | 5.147 | .023 | 0.198 |
| Employee diagnosed with COVID-19 | No employee diagnosed with COVID-19 | ||||
| Less than 100 new cases/mo | 51 (51.5) | 48 (48.5) | |||
| 100 new cases or more/mo | 16 (59.3) | 11 (40.7) | |||
| Total | 67 (53.2) | 59 (46.8) | 0.247 | .619 | 0.044 |
| Employee diagnosed with COVID-19 | No employee diagnosed with COVID-19 | ||||
| Not predominantly SUS | 34 (65.4) | 18 (34.6) | |||
| Predominantly SUS | 33 (44.6) | 41 (55.4) | |||
| Total | 67 (53.2) | 59 (46.8) | 4.499 | .033 | 0.186 |
| Drop in care above 20% | No drop in care above 20% | ||||
| Less than 100 new cases/mo | 63 (63.6) | 36 (36.4) | |||
| 100 new cases or more/mo | 14 (51.9) | 13 (48.1) | |||
| Total | 77 (61.1) | 49 (38.9) | 0.793 | .373 | 0.079 |
| Drop in care above 20% | No drop in care above 20% | ||||
| Not predominantly SUS | 32 (61.5) | 20 (38.5) | |||
| Predominantly SUS | 45 (60.8) | 29 (39.2) | |||
| Total | 77 (61.1) | 49 (38.9) | 0.010 | .917 | 0.009 |
| Indication of hypofractionation | No indication of hypofractionation | ||||
| Less than 100 new cases/mo | 78 (78.8) | 21 (21.2) | |||
| 100 new cases or more/mo | 20 (74.1) | 7 (25.9) | |||
| Total | 98 (77.8) | 28 (22.2) | 0.068 | .794 | 0.023 |
| Indication of hypofractionation | No indication of hypofractionation | ||||
| Not predominantly SUS | 43 (82.7) | 9 (17.3) | |||
| Predominantly SUS | 55 (74.3) | 19 (25,7) | |||
| Total | 98 (77.8) | 28 (22.2) | 0.800 | .370 | 0.079 |
| Team rotation | No team rotation | ||||
| Less than 100 new cases/mo | 36 (36.4) | 63 (63.6) | |||
| 100 new cases or more/mo | 8 (29.6) | 19 (70.4) | |||
| Total | 44 (34.9) | 82 (65.1) | 0.179 | .672 | 0.037 |
| Team rotation | No team rotation | ||||
| Not predominantly SUS | 20 (38.5) | 32 (61.5) | |||
| Predominantly SUS | 24 (32.4) | 50 (67.6) | |||
| Total | 44 (34.9) | 82 (65.1) | 0.259 | .610 | 0.045 |
Abbreviation: SUS = Unified Health System.
The binomial variables of the χ2 analysis are presented in a 2 × 2 table, with number of patients and percentage (compared with overall number of patients) in each of the 4 squares, the row and column total count and percentage (compared with overall number of patients), and the P value for each analysis.
Discussion
The first case of COVID-19 in Brazil was registered on February 25, 2020. Since then, the country has recorded 1,839,850 cases and 71,469 deaths, with the second-highest number of confirmed cases and deaths.7 Worldwide, 12,476,028 COVID-19 cases have been confirmed so far. The United States is the country with the highest number of cases (3,184,633), followed by Brazil, India (820,916), Russia (713,936), and Peru (319,646). Regarding deaths, 559,998 have been confirmed worldwide, with the United States being the country with the highest absolute number of deaths (134,097), followed by Brazil (71,469), the United Kingdom (44,650), Italy (34,938), and Mexico (34,191). So far, Brazil has a mortality rate of 340 deaths/1 million inhabitants (12th place in the world). The demographic characteristics of the country, large territory, and actions to reduce the contagion caused stability in about a thousand deaths daily, with epidemiologic change to cities in the interior of the country and central-west and south regions.8
Since the beginning of the pandemic, the SBRT has organized several actions and recommendations for the country’s radiation oncology departments as a subsidy for the adequate confrontation of the pandemic and minimization of the risk of contagion between patients and collaborators. These measures ensured the maintenance of treatments, the temporary relaxation of the regulations of the National Nuclear Energy Commission, and the safety of the environments and people involved in the care of patients with cancer. Thus, our study aimed to identify which measures were taken by the services and their effect on patient care routines. These data are representative of the situation perceived by radiation oncology departments in Brazil during the COVID-19 pandemic, in a cutoff in June 2020, given the dynamics and variability observed in the patterns of disease transmission.
About 72% of the answers came from services in the south and southeast regions, maintaining the proportion of the distribution of services by regions of the country. The characteristics such as patient profile and the number of patients undergoing treatment per month were also proportional to the public databases.
Estimates by the Brazilian Society of Pathology and Surgical Oncology point out that almost 50,000 Brazilians have not been diagnosed. Thousands of patients already diagnosed with cancer had their treatments suspended or delayed. During April alone, it is estimated that 5940 pathologic examinations were performed in the public network of the city of São Paulo, with 22,680 biopsies in the same period in 2019, showing a reduction of 70% in comparison with the previous year.9
In the survey carried out by SBRT, about 61% of services reported a reduction above 20%. Of these, about 14% reported a reduction above 50% of patients undergoing radiation therapy. In questionnaires for the European radiation oncology departments, the European SocieTy for Radiotherapy and Oncology10 observed a 60% reduction in the number of patients. Of these, about 14% reported a reduction above 50% of patients undergoing radiation therapy. The leading causes were reduced referrals, postponements for cases of low-risk disease, and lack of personnel.
The services that presented patients or collaborators with COVID-19 had a similar distribution among the regions. There was a statistical difference in the number of services with infected employees and patients and the patients' origin. Services that treat patients from SUS presented lower rates of infection by COVID-19 among patients and employees. It is not possible to state precisely why this difference was found. One explanation is that at the time of application of the questionnaire, access to the COVID test was still challenging. Most of those services that treat predominantly SUS patients integrate bigger health care facilities with broader access to those tests. There was no statistically significant association in the number of services with infected employees and the size of the service. In the European SocieTy for Radiotherapy and Oncology questionnaire, about 57% of the services had employees on leave to care for family members or transferred to other sectors of the hospital, and there was a diagnosis of COVID-19 in 26% of these, reaching 75% in Spain and the United Kingdom.
The primary data from the questionnaire to radiation oncology departments during the current COVID-19 pandemic show a reduction in the number of patients by 61% in radiation oncology departments in Brazil. This reduction occurred without distinction between SUS and supplementary private health insurance services and wasn’t related to the size of the service. About half of the services had infected patients or employees, which reduced the workforce. About a third of services interrupted treatment for patients with COVID-19, and a quarter maintained treatment at alternative times. Prevention actions were adopted, such as the intensification of hygiene and cleaning measures in the service, distancing measures, the use of personal protective equipment by employees, the restriction of companion access for healthy patients, and changes in practices and routines (eg, hypofractionation).
This study presents a global view of radiation oncology departments in Brazil during June 2020. The recommendations and procedures vary according to incidence, mortality, regional health structure, and the updating of preliminary studies on COVID-19 treatment. It is essential to understand the regional differences in the country, with the heterogeneous distribution of radiation oncology departments and the dissemination of COVID-19 at the time of the analysis.
Conclusions
COVID-19 caused a drop in demand and the installed capacity of the radiation oncology departments. Regarding patients and employees with COVID-19, we observe that services that primarily treat SUS patients reported significantly fewer disease cases. Despite the epidemiologic dynamics being different among the regions (starting in the north/northeast and moving to the center-south), the effect and the coping strategies adopted were similar among services.
Acknowledgments
The Brazilian Radiotherapy Society (SBRT) thanks the Brazilian radiation oncology departments for keeping radiation therapy open to patients during the COVID-19 pandemic.
Footnotes
Sources of support: This work has specific funding of the Brazilian Radiotherapy Society (SBRT).
Disclosures: none.
Research data are available at: www.sbradioterapia.com.br.
References
- 1.Jordan R.E., Adab P., Cheng K.K. Covid-19: Risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 2.Kuderer N.M., Choueiri T.K., Shah D.P., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whisenant J.G., Trama A., Torri V., et al. TERAVOLT: Thoracic Cancers International COVID-19 collaboration. Cancer Cell. 2020;37:742–745. doi: 10.1016/j.ccell.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garassino M.C., Whisenant J.G., Huang L.C., et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): First results of an international, registry-based, cohort study. Lancet Oncol. 2020;21:914–922. doi: 10.1016/S1470-2045(20)30314-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubinstein S.M., Steinharter J.A., Warner J., Rini B.I., Peters S., Choueiri T.K. The COVID-19 and Cancer Consortium: A collaborative effort to understand the effects of COVID-19 on patients with cancer. Cancer Cell. 2020;37:738–741. doi: 10.1016/j.ccell.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fontenelle L.F., Camargo MBJ de, Bertoldi A.D., Gonçalves H., Maciel E.L.N., Barros A.J.D. Cobertura por plano de saúde ou cartão de desconto: inquérito domiciliar na área de abrangência da Estratégia Saúde da Família. Cad Saude Publica. 2017;33 doi: 10.1590/0102-311X00141515. [DOI] [PubMed] [Google Scholar]
- 7.Ministério da Saúde - Secretaria de Vigilância em Saúde Boletim Epidemiológico Especial - Situação Epidemiológica Da COVID-19. https://ourworldindata.org/coronavirus Available at:
- 8.World Health Organization Coronavirus Disease (COVID-19) Situation Report-173. https://apps.who.int/iris/handle/10665/333298 Available at:
- 9.Sociedades médicas apontam redução de 70% das cirurgias e que 50 mil brasileiros não receberam diagnóstico de câncer - SBCO. https://sbco.org.br/2020/05/14/sociedades-medicas-apontam-reducao-de-70-das-cirurgias-e-que-50-mil-brasileiros-nao-receberam-diagnostico-de-cancer/ Available at:
- 10.Slotman B.J., Lievens Y., Poortmans P., et al. Effect of COVID-19 pandemic on practice in European radiation oncology centers. Radiother Oncol. 2020;150:40–42. doi: 10.1016/j.radonc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]