Abstract
BACKGROUND
The current study aimed to update prior systematic review and meta-analyses (SRMA) in order to determine the effects of supervised exercise-based cardiac rehabilitation (EBCR) and introduce a suitable exercise protocol for management of lipid profile abnormalities in patients with cardiovascular disease (CVD).
METHODS
PubMed, Scopus, and Web of Science databases were searched from 1980 to December 2018. All published, randomized controlled trials (RCTs) reporting the efficacy of supervised EBCR in patients with CVD and measuring at least 1 component of lipid profile were included. The quality of articles was assessed based on the Physiotherapy Evidence Database (PEDro) scale. Random effect model was used to calculate the effect size of post-intervention data.
RESULTS
Initially 774 RCTs were reviewed, 14 of them were included in the study. In comparison with the control group, supervised EBCR was associated with higher serum levels of high-density lipoprotein (HDL) [weight mean difference (WMD): 1.297; 95% confidence interval (CI): -1.620, 4.214] and lower serum level of low-density lipoprotein (LDL) (WMD: -7.797; 95%CI: -14.005, -1.588), total cholesterol (TC) (WMD: -11.029; 95%CI: -20.716, -1.342), and triglyceride (TG) (WMD: -14.602; 95%CI: -28.992, -0.212).
CONCLUSION
It seems that EBCR is correlated with an insignificant increase in HDL serum level and a significant decrease in LDL, TC, and TG serum levels. Considering subgroup analysis results, it is suggested that long duration, moderate exercise volume (EV), and combination of aerobic exercise (AE) and resistance exercise (RE) be used to improve HDL and TG serum levels. Short duration, high EV, and AE+RE seem to significantly reduce LDL serum level. Moreover, moderate EV is associated with a significant reduction in TC level.
Keywords: Cardiac Rehabilitation, Cardiovascular Diseases, Exercise, Lipids, Meta-Analysis
Introduction
Cardiovascular diseases (CVDs) are important causes of increased mortality, morbidity, and physical disability.1-3 Based on the World Health Organization (WHO) reports, 17.7 million people die every year from CVDs 75% of whom are from low-income and middle-income countries.4 Moreover, many studies report that unhealthy diet, physical inactivity, and obesity are the major causes of CVDs.5 Additionally, economic burden and poor quality of life (QOL) are negative impacts on patients’ condition following CVD.6,7
Effective treatments for CVDs include appropriate pharmacotherapy, percutaneous coronary intervention (PCI), surgical procedures, and cardiac rehabilitation (CR). CR is a multi-disciplinary and comprehensive long-term program for secondary prevention, which comprises medical evaluation, aerobic exercise (AE), resistance exercise (RE), education, and nutritional and psychological counseling.8
It is important that patients with CVD participate in CR due to medical complications, prolonged bed rest, and disability that occur after CVD.9 It seems that the most important cardiovascular outcomes of CR are the reduction of morbidity, hospital readmissions, risk of future cardiac events, and cardiac risk factors such as lipid profile and blood pressure.10-12
Lipid profile includes serum total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and total triglycerides (TG) factors. It is suggested that HDL serum level, and TC/HDL and TG/HDL ratios are associated with all-cause mortality and risk of hospitalization in patients with CVD.13 In addition, some studies indicate that short-term CR can reduce TC, LDL, and TG serum levels in patients with CVD.14,15
The effect of the supervised exercise-based cardiac rehabilitation (EBCR) program has been reviewed in patients with coronary artery disease (CAD) in previous systematic review and meta-analyses (SRMA).16,17 Due to the importance of lipid profile as an essential risk factor for CVD and high risk of CVD occurrence in patients without controlled LP, we updated prior SRMAs. Although the CR program is a multi-professional program, the main objective of the current study was to only evaluate the exercises of the CR program. Therefore, the current SRMA aimed to determine and evaluate the effect of EBCR on lipid profile in patients with CVD. The second aim of the study was to determine and recommend the best exercise training characteristics for the improvement of lipid profile in patients with CVD.
Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were employed to perform the current SRMA.
Searching methods
The three online databases of PubMed, Scopus, and Web of Science were systematically searched from 1980 to December 2018 to identify the potentially relevant studies. Moreover, all references cited in the included studies and relevant review articles were checked to find other potential studies.
The inclusion criteria were as follows:
Type of study: All human studies with randomized controlled trial (RCT) design were included. If an article had more than 1 intervention group receiving different types of exercises, we split it into 2 (or more) studies and each intervention group was separately compared with the control group. Language was not a limitation in the current study.
Type of participants: All studies on patients with CVD were included. All patients must have a stable medical condition to participate in the CR program. Both studies with and without surgical procedure were eligible for the current SRMA.
Type of intervention: Studies using the supervised EBCR with a focus on exercise training (ET) with or without dietary, psychological, or lifestyle counseling were included. Control group was defined as a group that received only medication, usual care, or education about risk factors. Studies with home exercise prescription in the intervention or control group were not included. Furthermore, all studies with a dietary prescription, and psychological or lifestyle counseling in the control group were excluded.
Type of outcome measures: Studies that investigated at least 1 of the lipid profile components were included. Data on general items, characteristics of the CR program, main outcome measures, and predefined criteria were extracted from articles. General items included the name of the first author, publication year, type and phase of CVD, as well as number, age, gender, and body mass index (BMI) of participants in the intervention and control groups. Characteristics of the CR program: included duration, number of sessions per week (frequency), and other received interventions in the experimental and control groups. The main outcome measurements comprised HDL, LDL, TC, and TG serum levels. The predefined criteria included the baseline BMI of participants (BMI < 18 kg/m2 as underweight, 18 ≤ BMI < 25 kg/m2 as normal weight, 25 ≤ BMI < 30 kg/m2 as overweight, and BMI ≥ 30 kg/m2 as obese),18 quality of included articles [Physiotherapy Evidence Database (PEDro) ≤ 3 as low-quality, 4 ≤ PEDro ≤ 6 as medium-quality, and 7 ≤ PEDro ≤ 9 as high-quality], duration of CR (0-8 weeks as short, 9-12 weeks as medium, and 13-24 weeks as long), frequency of CR program (1-2 or 3-4 times per week), and exercise volume (EV) (duration of CR session × frequency) (EV < 120 minute/week as low, 120 ≤ EV < 180 minute/week as moderate, and EV ≥ 180 minute/week as high).
Searching and data extraction procedure: Two independent authors systematically searched the databases and reviewed titles and abstracts. The full texts of all included studies were rechecked. If a full-text paper or its download or purchase link was not available on the website of the database or journal, 3 e-mails during 3 months were sent to the corresponding author and the full-text article was requested. Data of all included studies were extracted by 2 independent authors. Disagreements between the authors were resolved by a third party. In case of lack of data in the included studies, 2 e-mails requesting data were sent to the corresponding author within a 2-week interval.
Quality assessment: The full texts of all included studies were reviewed and critically appraised by 2 authors using the PEDro scale.19 Since patient and therapist blinding is not possible in CR interventions, the maximum score of studies was 9.
Data synthesis and statistical analysis: The post-intervention data were employed for analysis in the current meta-analysis. Post-intervention mean ± SD of lipid profile was extracted from articles. If the confidence interval (CI) was reported in a study, SD was calculated from upper limit, lower limit, and total number of participants in the group. Due to there being more than 1 effect size among studies, the random effect model (Der Simonian-Laird) was employed to calculate the overall effect size. Cochran Q test and I2 analysis, with the significance level of < 0.1, were applied to calculate the heterogeneity between studies.20 Moreover, subgroup analysis was performed based on the predefined criteria to find the potential source of heterogeneity and identify the effect of each criterion. Furthermore, Egger’s test was used to assess any potential publication bias and funnel plots were drawn to illustrate it, P-value < 0.050 was considered the level of significance. All of the statistical analyses were performed in Stata software (version 11.2; StataCorp., College Station, TX, USA).
Results
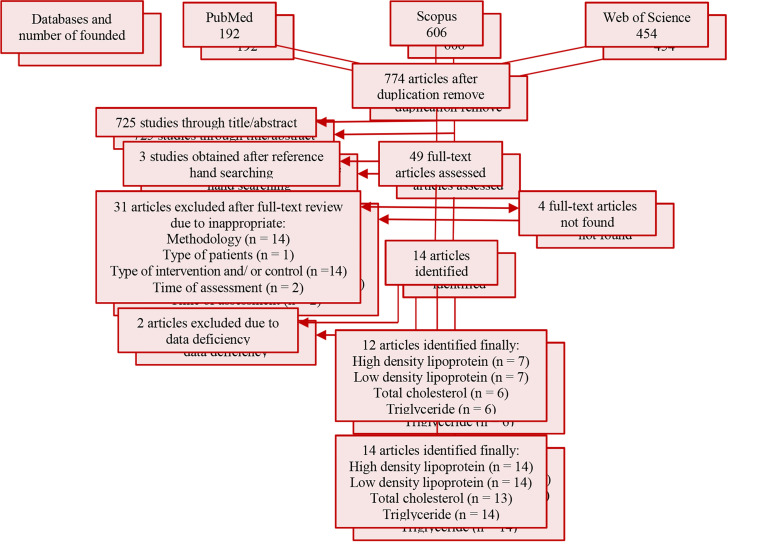
In total, 774 potentially relevant articles were identified through an online search, 725 of which were excluded after scrutiny of titles and abstracts. In addition, 3 articles were found through a manual search. The full text of 4 papers could not be found after searching the scientific databases and websites of related journals. Thus, 3 e-mails were sent to their corresponding authors, but no response was received; therefore, they were excluded from the study.21-24 Moreover, 3 articles were in languages other than English.25-27 These articles were translated into English by native or expert translators. Finally, 12 articles were selected for the current SRMA27-38 (Figure 1).
Figure 1.
The flow diagram for the identification of the eligible articles evaluating the effect of cardiac rehabilitation on lipid profile RCT: Randomized controlled trials
Characteristics of the included studies: A summary of the characteristics of the included studies is presented in table 1; 10 out of 12 articles had a two-arm parallel design (CR and control) and 2 articles had a three-arm parallel design. In one study with a control group, the AE+RE were applied to 2 groups.28 In another one, Seki et al. randomly assigned the participants to 3 groups including continuous aerobic exercise (CAE), intermittent aerobic exercise (IAE), and the control group.34 Each of these studies was divided into 2 independent studies. Therefore, 14 studies were analyzed in the current meta-analysis. The language of 11 articles was English, and 1 article was in French.27 In total, 775 participants were included in the current SRMA (412 in the intervention group and 334 in the control group). The mean age of participants in the intervention and control groups was 58.7 ± 5.47 and 58.9 ± 5.46 years, respectively. Table 2 shows details of the CR program of each included study. The CR program started from 6-9 days after acute myocardial infraction (AMI) with PCI to 24 weeks after MI. In the study by Hassan and Nahas, patients were included if they had PCI history of less than 48 weeks. Therefore, the exact duration of PCI to CR program was unclear.37 Moderate intensity was applied to all studies except 1 study that used high intensity exercise (80% of maximum heart rate) in the intervention group.35 All studies evaluated HDL, LDL, and TC serum levels. The outcome measures of 1 study did not contain serum TC level.27
Table 1.
Summary of characteristics of the included studies
| First Author | Type of disease | Sample size |
Mean age |
BMI |
Other intervention | Intervention of cont. | |||
|---|---|---|---|---|---|---|---|---|---|
| Cont. | Int. | Cont. | Int. | Cont. | Cont. | ||||
| Wosornu et al.28 | CABG | 27 | 26 | 56.5 | 56.6 | 26.9 | 27.5 | Medication | Medication |
| 25 | 59.2 | 25.8 | |||||||
| Belardinelli et al.29 | CAD with successful CA | 59 | 59 | 53 | 59 | 24.3 | 23.9 | Medication | Medication and Avoidance of physical training |
| Yu et al.30 | AMI or PCI | 72 | 40 | 62.3 | 61.2 | 27.6 | 27.4 | Domiciliary or vocational environment training by occupational therapist | Education about risk factors and disease and benefits of physical activity |
| Vona et al.31 | Uncomplicated AMI | 28 | 24 | 56 | 57 | 26.5 | 25.7 | Encourage to increase daily physical activity | Avoidance of regular physical activity |
| Volaklis et al.32 | CAD (MI, CABG, CA) | 11 | 10 | 58 | 51 | NM | NM | NM | Usual daily activities |
| Seki et al.34 | AMI, CABG, & PCI | 18 | 16 | 69 | 70 | 23.4 | 23.5 | Medication | Medication & usual outpatient care |
| Balen et al.33 | Post-AMI with PCI | 30 | 30 | 59 | 61 | 28.8 | 28 | Standard care, 30 min supervised walking | Standard care |
| Luk et al.35 | CAD treated by medication | 32 | 32 | 67.7 | 66.6 | 24.7 | 25.1 | Education, Counseling, risk factor modification | Education, Counseling, risk factor modification |
| Ghroubi et al.27 | MI with coronary stenting | 30 | 38 | 50 | 53 | 27.14 | 25.5 | Education | NM |
| Aksoy et al.36 | CHF (LVEF: 35-55%), CHF with dilated or ischemic cardiomyopathy, CHF with ventricular rhythm | 19 19 | 19 | 63.7 | 57.5 | 28.4 | 29.1 | NM | NM |
| 59.6 | 30.1 | ||||||||
| Hassan and Nahas37 | PCI | 30 | 30 | 52.6 | 53.8 | 30.3 | 30.2 | Medication & risk factors education | Medication & risk factors education |
| Tamburus et al.38 | CAD: MI, PCI, CABG | 12 | 10 | 56.2 | 60.4 | 28.7 | 28.3 | NM | Usual daily activity |
Int.: Intervention; Cont.: Control; CABG: Coronary artery bypass graft; CAD: Coronary artery disease; CA: Coronary angioplasty; AMI: Acute myocardial infraction; PCI: Percutaneous coronary intervention; MI: Myocardial infraction; NM: Not mentioned; min: Minute; CHF: Cardiac heart failure; LVEF: Left ventricular ejection fraction
Table 2.
Details of cardiac rehabilitation program characteristics of the included studies
| First Author | Start time of CR program | Type of Exercise(s) | Duration of exercise training | Intensity | Duration of CR (w) | Frequency (s/w) |
|---|---|---|---|---|---|---|
| Wosornu et al.28 | NM | AE: arm circling and raising, step-ups, trunk rotation, bridging, hip abduction, trunk side lying, running, and star jumps RE: bench press, military press, biceps curl, upright row, pull down, push down, pulley row, quadriceps curl, hamstring curl, and sit ups | 12-40 min | AE: start with 3*10 and increase over time RE: start with 3*10 and 2-5 kg with increase over time | 24 | 3 |
| Belardinelli et al.29 | NM | Cycle ergometry | Warm-up: 15 min Main program: 30 min Cool-down: 8 min | Moderate aerobic training: 60% of peak O2 uptake | 24 | 3 |
| Yu et al.30 | 6 w | NM | 60 min | Moderate aerobic training: 65 to 85% of maximum aerobic capacity | 8 | 2 |
| Vona et al.31 | 0-3 w | Cycle ergometry | Warm-up: 10 min Main program: 40 min Cool-down: 10 min | Moderate aerobic training: 75% of maximum HR | 12 | 3 |
| Volaklis et al.32 | NM | AE: walking, running, cycling, cycle ergometry RE: bench press, seated row, leg extension, pull down, peck-deck, hamstring curl, curl-ups, and back extension | AE (2 sessions): Warm-up: 10 min Main program: 30-40 min (15-20 min running on treadmill and 15-20 min on ergometer) Cool-down: 10 min RE (2 sessions): Warm-up: 10 min Main program: 30-40 min (8 stations) Cool-down: 10 min | Aerobic sessions: 60-80% of maximum HR Resistance sessions: 60% of 1-RM (2 to 3 sets of 12 to 15 repetitions) | 24 | 4 |
| Seki et al.34 | ≥ 24 w | Walking, bicycling, jogging, light isotonic exercises | Warm-up: 15 min Main program: 20-60 min Cool-down: 15 min | Moderate aerobic training Borg score: 12-13 | 24 | 1 |
| (Phase III) | ||||||
| Balen et al.33 | 6-9 d | Cycle ergometry | 45 min | Moderate aerobic intensity: 50%-60% of peak O2 uptake | 3 | 1 |
| Luk et al.35 | > 24 w | AE: treadmill, cycle ergometry, rowing, steps, arm ergometry RE: dumbbell, weight training | Warm-up: 5 min Main program: 50 min Cool-down: 5 min | AEs: 80% maximum HR (Progressive) RE: 80% maximum HR (Progressive) | 8 | 3 |
| Ghroubi et al.27 | 8-12 w | Cycle ergometry | Warm-up: 10 min Main program: 2*10 min (5 min rest) Cool-down: 10 min | 70% maximum HR | 8 | 3 |
| Aksoy et al.36 | NM | Ergometry | CAE: Warm-up: 5 min Main program: 25 min (with a certain intensity during the session) Cool-down: 5 min IAE: Warm-up: 5 min Main program: 25 min (60 s with determined intensity and 60 s with low intensity) Cool-down: 5 min | 75% of peak O2 uptake (Progressive) | 10 | 3 |
| Hassan and Nahas37 | > 48 w | Bicycle ergometry | Warm-up: 5-10 min Main program: 30 min Cool-down: 5-10 min | Mild to moderate intensity exercise: based on 11 to 14 of the Borg scale | 24 | 3 |
| Tamburus et al.38 | MI > 24 w PCI & CABG > 12 w | Cycle ergometry | Warm-up: 10 min Main program: 30-40 min Cool-down: 5-10 min | Moderate intensity exercise: 110% of VAT | 16 | 3 |
CR: Cardiac rehabilitation; w: Weeks; s/w: Session(s) per week; d: Days; NM: Not mentioned; AE: Aerobic exercise; RE: Resistance exercise; min: Minute; HR: Heart rate; CAE: Continuous aerobic exercise; IAE: Intermittent aerobic exercise; MI: Myocardial infraction; PCI: Percutaneous coronary intervention; CABG: Coronary artery bypass surgery; VAT: Ventilatory anaerobic threshold
Results of quality assessment: All the included articles mentioned proper random allocation and baseline similarity of the groups. Assessor blinding was performed in 4 studies; 6 articles had high quality scores, and 6 had medium quality scores. A summary of the PEDro assessment domains of the included articles is provided in table 3.
Table 3.
Quality assessment of included studies based on the PEDro scale
| Item | Wosornu et al.28 | Belardinelli et al.29 | Yu et al.30 | Vona et al.31 | Volaklis et al.32 | Seki et al.34 | Balen et al.33 | Luk et al.35 | Ghroubi et al.27 | Aksoy et al.36 | Hassan and Nahas37 | Tamburus et al.38 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eligibility criteria specification | No | No | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes |
| Randomization allocation | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Allocation concealment | No | No | No | No | No | No | No | No | No | No | No | Yes |
| Groups’ similarity at baseline | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Subject blinding | No | No | No | No | No | No | No | No | No | No | No | No |
| Therapist blinding | No | No | No | No | No | No | No | No | No | No | No | No |
| Assessor blinding | Yes | Yes | No | Yes | No | No | No | Yes | No | No | No | No |
| Outcome measure obtaining from 85% of subjects initially allocated to groups | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes |
| Use of intention to treat analysis | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | No | No |
| Reporting between-group statistical comparisons | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Reporting point measures and measures of variability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Total | 7 | 7 | 6 | 7 | 5 | 5 | 6 | 7 | 7 | 5 | 5 | 7 |
| Quality | High | High | Medium | High | Medium | Medium | Medium | High | High | Medium | Medium | High |
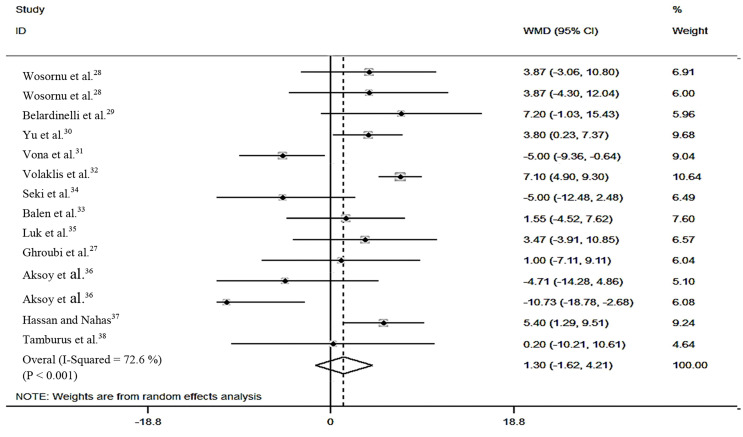
Data pooling and meta-analysis: Regarding the serum HDL level, 3 studies reported significant difference,32,36,37 and 2 studies reported marginal significant difference30,31 between the groups after the interventions (P < 0.050). The forest plot of HDL analysis showed that the HDL serum level of 4 studies was lower in the intervention group than the control group at the end of the study.31,34,36 Significant change was not observed in HDL serum level after the intervention in any of the studies (n = 14; weight mean difference (WMD): 1.297; 95% CI: -1.620, 4.214; P = 0.383; Figure 2). Subgroup analysis revealed that in studies performed over a long duration with AR+RE and moderate EV, the HDL serum level increased significantly in comparison with the control group (P < 0.010; Table 4).
Figure 2.
Forest plots of high-density lipoprotein serum level differences between the intervention and control groups after cardiac rehabilitation using random effect analysis WMD: Weighted mean difference; CI: Confidence interval
Table 4.
Subgroup analysis of high-density lipoprotein based on random effect analysis
| Subgroup | Effect size (n) | WMD (95%CIs) | P-within | I2 (%) | Q-test |
|---|---|---|---|---|---|
| Overall | 14 | 1.297 (-1.620, 4.214) | 0.383 | 72.6 | < 0.001 |
| BMI | |||||
| Not detected | 1 | - | - | - | - |
| Normal | 3 | 1.759 (-5.270, 8.789) | 0.624 | 60.1 | 0.081 |
| Overweight | 8 | 0.677 (-2.325, 3.680) | 0.658 | 42.4 | 0.096 |
| Obese | 2 | -2.279 (-18.068, 13.510) | 0.777 | 91.8 | < 0.001 |
| Study quality | |||||
| Medium | 7 | 0.856 (-3.253, 4.964) | 0.683 | 80.1 | < 0.001 |
| High | 7 | 1.507 (-2.210, 5.223) | 0.427 | 44.7 | 0.093 |
| Exercise duration | |||||
| Short | 4 | 3.011 (0.331, 5.692) | 0.028 | 0 | 0.882 |
| Medium | 3 | -6.080 (-9.640, -2.520) | 0.001 | 0 | 0.450 |
| Long | 7 | 4.259 (1.284, 7.235) | 0.005 | 46.6 | 0.085 |
| Exercise type | |||||
| AE | 11 | 0.127 (-3.107, 3.360) | 0.939 | 65.4 | 0.001 |
| RE | 1 | 3.870 (-4.301, 12.041) | 0.353 | - | - |
| AE+RE | 2 | 6.804 (4.696, 8.911) | < 0.001 | 0 | 0.355 |
| Exercise frequency | |||||
| 1-2 times per week | 3 | 0.990 (-3.730, 5.709) | 0.681 | 54.2 | 0.113 |
| 3-4 times per week | 11 | 1.411 (-2.262, 5.083) | 0.452 | 76.2 | < 0.001 |
| Exercise volume | |||||
| Low | 6 | -1.561 (-6.203, 3.080) | 0.510 | 55.4 | 0.047 |
| Moderate | 5 | 4.190 (1.811, 6.569) | 0.001 | 0 | 0.726 |
| High | 3 | 1.906 (-6.591, 10.403) | 0.660 | 91.5 | < 0.001 |
AE: Aerobic exercise; RE: Resistance exercise; WMD: Weighted mean difference (mg/dl); HDL: High-density lipoprotein cholesterol; BMI: Body mass index
I2: Percent variation in WMD attributable to heterogeneity/ Q-test: Test for heterogeneity with significance of < 0.10/ P-Within: Test of WMD of sub-groups by random-effect model with significance of < 0.05
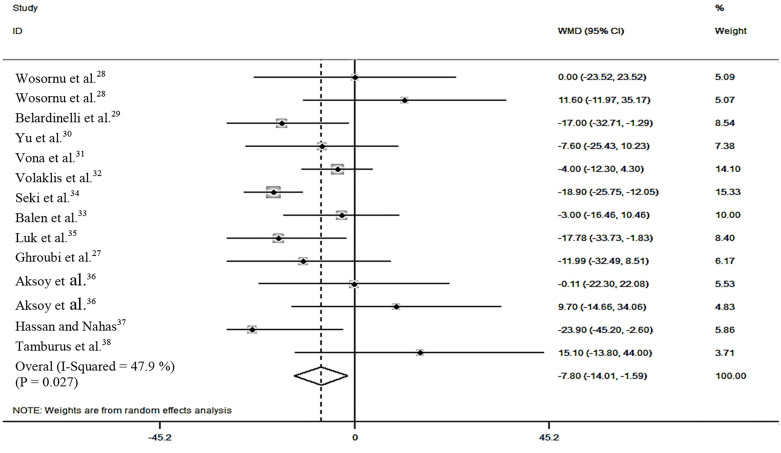
In terms of serum LDL level, 4 out of 14 studies reported a significant difference between groups after the interventions (P < 0.050).29,32,33,37 Furthermore, 3 studies showed higher LDL serum level in the intervention group than the control group, although the difference was not significant.28,36,38 Pooling data of all studies showed a significant difference in the LDL serum level after CR (n = 14; WMD = -7.797; 95%CI = -14.005, -1.588; P = 0.014; Figure 3). Subgroup analysis indicated that high-quality studies performed over a medium and long duration with AE+RE and low and moderate EV did not significantly change the serum level of LDL (P > 0.050; Table 5).
Figure 3.
Forest plots of low-density lipoprotein serum level differences between the intervention and control groups after cardiac rehabilitation using random effect analysis WMD: Weighted mean difference; CI: Confidence interval
Table 5.
Subgroup analysis of low-density lipoprotein cholesterol based on random effect analysis
| Subgroup | Effect size (n) | WMD (95%CIs) | P-within | I2 (%) | Q-test |
|---|---|---|---|---|---|
| Overall | 13 | -7.797 (-14.005, -1.588) | 0.014 | 47.9 | 0.027 |
| BMI | |||||
| Not detected | 1 | - | - | - | - |
| Normal | 3 | -9.536 (-18.682, -0.391) | 0.041 | 0 | 0.401 |
| Overweight | 7 | -3.810 (-10.428, 2.808) | 0.259 | 9.3 | 0.385 |
| Obese | 2 | -7.642 (-40.553, 25.268) | 0.649 | 75.9 | 0.042 |
| Study quality | |||||
| Medium | 7 | -10.846 (-18.946, -2.745) | 0.009 | 46.5 | 0.082 |
| High | 6 | -4.164 (-12.387, 4.059) | 0.321 | 24.9 | 0.247 |
| Exercise duration | |||||
| Short | 3 | -12.937 (-23.219, -2.655) | 0.014 | 0 | 0.702 |
| Medium | 3 | -2.300 (-9.707, 5.106) | 0.543 | 0 | 0.568 |
| Long | 7 | -8.160 (-18.206, 1.886) | 0.111 | 60.5 | 0.019 |
| Exercise type | |||||
| AE | 10 | -6.572 (-12.557, -0.587) | 0.031 | 20.2 | 0.257 |
| RE | 1 | 11.600 (-11.965, 35.165) | 0.335 | - | - |
| AE+RE | 2 | -18.205 (-24.704, -11.706) | < 0.001 | 0 | 0.531 |
| Exercise frequency | |||||
| 1-2 times per week | 3 | -8.761 (-17.669, 0.148) | 0.054 | 0 | 0.377 |
| 3-4 times per week | 10 | -6.802 (-14.786, 1.183) | 0.095 | 57.1 | 0.013 |
| Exercise volume | |||||
| Low | 6 | -2.485 (-11.091, 6.120) | 0.571 | 15.9 | 0.312 |
| Moderate | 4 | -10.949 (-24.170, 2.273) | 0.105 | 42.3 | 0.158 |
| High | 3 | -11.761 (-23.105, -0.416) | 0.042 | 72.9 | 0.025 |
AE: Aerobic exercise; RE: Resistance exercise; WMD: Weighted mean difference (mg/dl); LDL: Low-density lipoprotein cholesterol; BMI: Body mass index
I2: Percent variation in WMD attributable to heterogeneity/ Q-test: Test for heterogeneity with significance of < 0.10/ P-Within: Test of WMD of sub-groups by random-effect model with significance of < 0.05
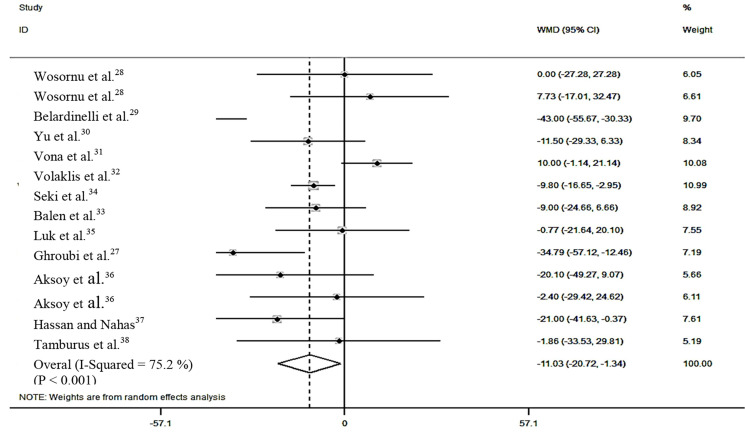
In terms of serum TC level, 3 of 14 studies29,32,34 reported a significant difference and 1 study37 reported a marginal significant difference between the intervention and control groups after the intervention. The forest plot showed that in 2 studies, LDL serum levels were significantly higher in the intervention group than the control group.28,31 Pooling data of all studies revealed significant differences in TC serum level after CR (n = 13; WMD = -11.029; 95% CI: -20.716, -1.342; P = 0.026; Figure 4). Subgroup analysis indicated insignificant differences in the TC serum level between the groups in the high-quality studies with low and high EV on subjects with overweight and obesity (P > 0.500; Table 6).
Figure 4.
Forest plots of total cholesterol serum level differences between the intervention and control groups after cardiac rehabilitation using random effect analysis WMD: Weighted mean difference; CI: Confidence interval
Table 6.
Subgroup analysis of total cholesterol based on random effect analysis
| Subgroup | Effect size (n) | WMD (95%CIs) | P-within | I2 (%) | Q-test |
|---|---|---|---|---|---|
| Overall | 13 | -11.029 (-20.716, -1.342) | 0.026 | 75.2 | < 0.001 |
| BMI | |||||
| Not detected | 1 | - | - | - | - |
| Normal | 3 | -28.929 (-51.346, -6.512) | 0.011 | 82.0 | 0.004 |
| Overweight | 7 | 0.768 (-7.330, 8.865) | 0.853 | 10.8 | 0.347 |
| Obese | 2 | -13.829 (-31.573, 3.915) | 0.127 | 13.0 | 0.284 |
| Study quality | |||||
| Medium | 7 | -10.069 (-15.361, -4.778) | < 0.001 | 0 | 0.851 |
| High | 6 | -10.920 (-34.218, 12.377) | 0.358 | 89.0 | < 0.001 |
| Exercise duration | |||||
| Short | 3 | -15.156 (-33.558, 3.246) | 0.106 | 59.5 | 0.084 |
| Medium | 3 | -0.053 (-17.385, 17.279) | 0.995 | 48.8 | 0.142 |
| Long | 7 | -13.050 (-26.423, 0.323) | 0.056 | 77.7 | < 0.001 |
| Exercise type | |||||
| AE | 10 | -10.438 (-23.481, 2.605) | 0.117 | 78.4 | < 0.001 |
| RE | 1 | 7.730 (-17.014, 32.474) | 0.540 | - | - |
| AE+RE | 2 | -34.790 (-57.121, -12.459) | 0.104 | 77.3 | 0.036 |
| Exercise frequency | |||||
| 1-2 times per week | 3 | -7.841 (18.089, 2.406) | 0.134 | 0 | 0.732 |
| 3-4 times per week | 10 | -12.133 (-24.723, 0.457) | 0.059 | 81.0 | < 0.001 |
| Exercise volume | |||||
| Low | 6 | -4.435 (-13.602, 4.733) | 0.343 | 0 | 0.761 |
| Moderate | 4 | -21.711 (-40.825, -2.598) | 0.026 | 74.4 | 0.008 |
| High | 3 | -9.296 (-28.526, 9.935) | 0.343 | 87.1 | < 0.001 |
AE: Aerobic exercise; RE: Resistance exercise; WMD: Weighted mean difference (mg/dl); LDL: Low-density lipoprotein cholesterol; BMI: Body mass index
I2: Percent variation in WMD attributable to heterogeneity/ Q-test: Test for heterogeneity with significance of < 0.10/ P-Within: Test of WMD of sub-groups by random-effect model with significance of < 0.05
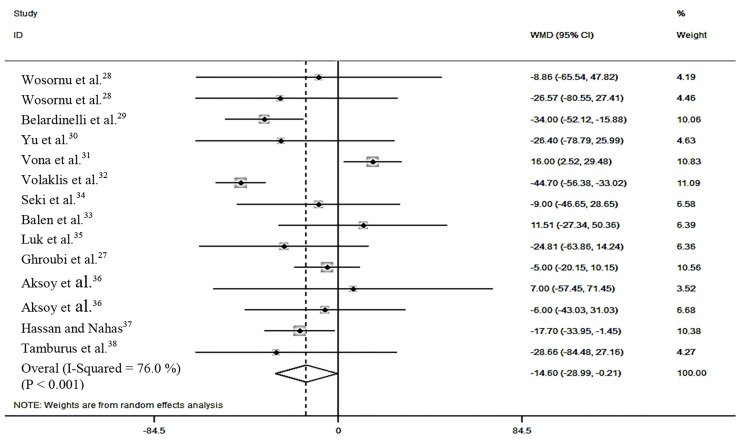
Regarding the TG serum level, 2 studies reported a significant difference,29,32 and 1 study reported a marginal significant difference37 after the interventions (P < 0.050). The current analysis showed that 3 studies revealed higher TG serum level in the intervention group than the control group at the end of the intervention.31,33,36 The combination of all studies showed marginal significant differences in serum TG level after CR (n = 14; WMD = -14.602; 95% CI: -28.992, -0.212; P = 0.470; Figure 5). Subgroup analysis showed that studies performed over a short and medium duration with AE+RE and low and high EV on subjects with overweight did not decrease the serum TG level significantly (P > 0.050, Table 7).
Figure 5.
Forest plots of triglyceride serum level differences between the intervention and control groups after cardiac rehabilitation using random effect analysis WMD: Weighted mean difference; CI: Confidence interval
Table 7.
Subgroup analysis of triglyceride based on random effect analysis
| Subgroup | Effect size (n) | WMD (95%CIs) | P-within | I2 (%) | Q-test |
|---|---|---|---|---|---|
| Overall | 14 | -14.602 (-28.992, -0.212) | 0.047 | 76.0 | < 0.001 |
| BMI | |||||
| Not detected | 1 | - | - | - | - |
| Normal | 3 | -28.628 (-43.694, -13.563) | < 0.001 | 0 | 0.492 |
| Overweight | 8 | 1.412 (-10.519, 13.344) | 0.817 | 18.5 | 0.284 |
| Obese | 2 | -15.81 (-30.689, -0.933) | 0.037 | 0 | 0.571 |
| Study quality | |||||
| Medium | 7 | -17.349 (-35.685, 0.988) | 0.064 | 64.2 | 0.010 |
| High | 7 | -12.642 (-31.775, 6.492) | 0.195 | 72.1 | 0.002 |
| Exercise duration | |||||
| Short | 4 | -6.632 (-19.500, 6.236) | 0.312 | 0 | 0.520 |
| Medium | 3 | 13.188 (0.760, 25.615) | 0.038 | 0 | 0.540 |
| Long | 7 | -29.622 (-41.756, -17.488) | < 0.001 | 37.6 | 0.142 |
| Exercise type | |||||
| AE | 11 | -8.590 (-21.499, 4.319) | 0.192 | 57.6 | 0.009 |
| RE | 1 | -26.570 (-80.548, 27.408) | 0.335 | - | - |
| AE+RE | 2 | -43.067 (-54.255, -31.879) | < 0.001 | 0 | < 0.001 |
| Exercise frequency | |||||
| 1-2 times per week | 3 | -4.817 (-28.843, 19.208) | 0.694 | 0 | 0.502 |
| 3-4 times per week | 11 | -16.391 (-32.838, 0.057) | 0.051 | 80.7 | < 0.001 |
| Exercise volume | |||||
| Low | 6 | -4.442 (-22.722, 13.838) | 0.634 | 0 | 0.913 |
| Moderate | 5 | -18.927 (-31.427, -6.427) | 0.003 | 34.0 | 0.195 |
| High | 3 | -17.461 (-63.812, 28.890) | 0.460 | 95.5 | < 0.001 |
AE: Aerobic exercise; RE: Resistance exercise; WMD: Weighted mean difference (mg/dl); LDL: Low-density lipoprotein cholesterol; BMI: Body mass index
I2: Percent variation in WMD attributable to heterogeneity/ Q-test: Test for heterogeneity with significance of < 0.10/ P-Within: Test of WMD of sub-groups by random-effect model with significance of < 0.05
In all analyses, pooled studies were heterogeneous (P < 0.010). Subgroup analysis suggested that exercise frequency and volume were potential sources of heterogeneity among all analyses. BMI was suggested as a potential source of heterogeneity in HDL, LDL, and TC serum level analyses. Furthermore, the study quality and type of exercise were potential sources of heterogeneity in HDL, LDL, and TG serum level analyses.
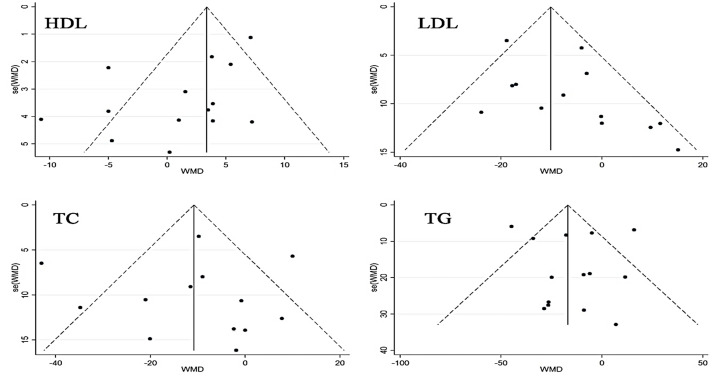
Publication bias: Based on the results of Egger’s test and visual inspection of funnel plots, the analysis of HDL (P = 0.030) showed publication bias (Figure 6). However, analysis of LDL (P = 0.081), TC (P = 0.955), and TG (P = 0.695) did not present any evidence of publication bias.
Figure 6.
Metafunnel plot of high-density lipoprotein, low-density lipoprotein, total cholesterol, and triglyceride serum level analyses based on Egger’s test *All plots represent pseudo 95% confidence intervals. WMD: Weighted mean difference; HLD: High-density lipoprotein; LDL: Low-density lipoprotein; TC: Total cholesterol; TG: Triglycerides
Discussion
The present SRMA was conducted to provide evidence about the influence of supervised EBCR on lipid profile changes in patients with CVD. Based on the current study results, supervised EBCR can significantly reduce serum LDL, TC, and TG levels. Moreover, the increase in HDL serum level was not significant.
The current study findings were not consistent with previous SRMAs. In a Cochrane SRMA by Jolliffe et al., none of the assessed LPs significantly improved after supervised EBCR.16 This may be explained by the inclusion of a limited number of studies in their study. Moreover, in a SRMA, Chen et al. evaluated the effect of endurance exercise training on patients with CAD and concluded that serum HDL and LDL levels were improved after AE, but TG and TC serum levels was not statistically reduced.17 They analyzed only 4 articles all of which were included in the current SRMA;29-31,34 however, 6 other eligible articles were also included in the current study.27,28,33,36-38 These differences between the results can be again due to the inclusion of different articles in the meta-analysis process. There were also 2 SRMAs with different analysis outputs (serum levels of HDL and LDL unchanged, TC and TG decreased significantly).39,40 These studies included both center-based and home-based CR programs.
CR is one of the most accepted interventions associated with decreased cardiac mortality, all-cause mortality, risk of re-admission, and infraction.41,42 Lowering LP decreases cardiac mortality, all-cause mortality, and vascular event rates.43,44
Based on the results of the subgroup analysis, it is suggested that the level of each component of LP be significantly improved in a specific CR characteristic.
It seems that supervised EBCR programs performed over a long duration using AE+RE with moderate EV can significantly improve HDL and TG serum levels. Furthermore, supervised EBCR programs performed over a short duration using AE+RE with high EV can significantly decrease LDL serum level. Moreover, moderate EV was the only EBCR property that was associated with significant TC serum level reduction. Although the results of subgroup analysis indicated that frequency of supervised EBCR sessions during a week was not an effective factor on the LP changes, total duration of CR in a week (EV) affected changes in each component of LP.
According to the current study results, AE+RE resulted in more beneficial effects than the implementation of each of them alone. Only 2 studies that used AR+RE were included in the current study; thus, the study findings should be generalized with caution. The current study results were similar to the findings of other studies that compared the effects of AE+RE and AE alone.45,46
The current study findings should be interpreted with the consideration of some limitations. First, only the studies with supervised EBCR were included in this meta-analysis. Many patients cannot participate in regular sessions outside their home due to different reasons. Further SRMAs should be conducted to compare the effect of center-based and home-based CRs on LP changes in patients with CVD. Second, the study was only aimed at evaluating the effects of supervised EBCR. As mentioned above, CR program is a comprehensive treatment and it seems that the result of comprehensive CR programs differ from EBCR. This should be studied in randomized controlled trials (RCTs) and SRMAs. Third, most RCTs in the current meta-analysis were conducted on middle-aged participants. Therefore, these results should be generalized to older patients with caution. Further RCTs are needed to evaluate the effect of supervised EBCR in elderly patients with CVD. Fourth, all of the studies included in the current review were performed on participants with widely different types of diseases; therefore, the type of disease could not be set as a predefined criterion for subgroup analysis. Moreover, the timespan between disease onset and CR initiation was not reported in 4 of the 12 studies. Accordingly, the CR initiation time criterion and the question about favorable time to start CR phase II remained unanswered. Fifth, 2 categories were defined for frequency in subgroup analysis, 1-2 and 3-4 session(s) per week. There was only 1 study with 1 session per week frequency. Therefore, articles with 2 sessions per week frequency were included more than those with 1 session per week frequency. Finally, all of the reviewed RCTs were performed on patients with a clinically stable condition. Patients with severe CVD or other serious complications were excluded. Consequently, the present findings should not be generalized to patients with severe CVD. No study reported any adverse effects of EBCR during interventions and at the end of the interventions.
Conclusion
The current SRMA analyzed the effect of supervised EBCR on changes in LP in patients with CVD. In total, the subgroup analysis indicated that a supervised EBCR significantly reduced serum LDL, TG, and TC levels. Moreover, it seems that CR programs performed over a long duration using AE+RE with moderate EV can significantly improve the serum level of HDL and TG. Furthermore, the characteristics of short duration, high EV, and AE+RE CR seem to significantly reduce serum LDL level. Finally, moderate EV seems to be associated with significant reduction in TC serum level. The current evidence may help physiotherapists and other disciplines responsible for exercise prescription to achieve better outcomes in CVD patients with dyslipidemia. Further RCTs are necessary to assess the obtained results.
Clinical messages
Exercise-based cardiac rehabilitation can improve all components of lipid profile.
The combination of aerobic and resistance exercises improves lipid profile.
Moderate exercise for a long duration is suggested for the improvement of HDL and TG levels.
High EV for a short duration is suggested for decreasing LDL serum level.
Acknowledgments
None.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Bennett SJ, Sauve MJ. Cognitive deficits in patients with heart failure: A review of the literature. J Cardiovasc Nurs. 2003;18(3):219–42. doi: 10.1097/00005082-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132(17):1667–78. doi: 10.1161/CIRCULATIONAHA.114.008720. [DOI] [PubMed] [Google Scholar]
- 3.Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345(12):892–902. doi: 10.1056/NEJMra001529. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Obesity: Preventing and managing the global epidemic. Geneva, Switzerland: WHO; 2000. [PubMed] [Google Scholar]
- 5.Thompson DR, Jenkinson C, Roebuck A, Lewin RJ, Boyle RM, Chandola T. Development and validation of a short measure of health status for individuals with acute myocardial infarction: The myocardial infarction dimensional assessment scale (MIDAS). Qual Life Res. 2002;11(6):535–43. doi: 10.1023/a:1016354516168. [DOI] [PubMed] [Google Scholar]
- 6.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: Heart disease and stroke statistics-2012 update: A report from the American Heart Association. Circulation. 2012;125(1):188–97. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 7.Yeates K, Lohfeld L, Sleeth J, Morales F, Rajkotia Y, Ogedegbe O. A global perspective on cardiovascular disease in vulnerable populations. Can J Cardiol. 2015;31(9):1081–93. doi: 10.1016/j.cjca.2015.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ades PA, Coello CE. Effects of exercise and cardiac rehabilitation on cardiovascular outcomes. Med Clin North Am. 2000;84(1):251–xi. doi: 10.1016/s0025-7125(05)70217-0. [DOI] [PubMed] [Google Scholar]
- 9.Leon AS, Franklin BA, Costa F, Balady GJ, Berra KA, Stewart KJ, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: An American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111(3):369–76. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 10.Chen JT, Lin TH, Voon WC, Lai WT, Huang MH, Sheu SH, et al. Beneficial effects of home-based cardiac rehabilitation on metabolic profiles in coronary heart-disease patients. Kaohsiung J Med Sci. 2016;32(5):267–75. doi: 10.1016/j.kjms.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, Rees K, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7):CD001800. doi: 10.1002/14651858.CD001800.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–72. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Orozco-Beltran D, Gil-Guillen VF, Redon J, Martin-Moreno JM, Pallares-Carratala V, Navarro-Perez J, et al. Lipid profile, cardiovascular disease and mortality in a Mediterranean high-risk population: The ESCARVAL-RISK study. PLoS One. 2017;12(10):e0186196. doi: 10.1371/journal.pone.0186196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redfern J, Briffa T, Ellis E, Freedman SB. Patient-centered modular secondary prevention following acute coronary syndrome: A randomized controlled trial. J Cardiopulm Rehabil Prev. 2008;28(2):107–15. doi: 10.1097/01.HCR.0000314204.86805.13. [DOI] [PubMed] [Google Scholar]
- 15.Yates BC, Rowland S, Mancuso K, Kupzyk KA, Norman JF, Shurmur S, et al. Reducing cardiovascular risk in spouses of cardiac patients: A randomized controlled trial. West J Nurs Res. 2015;37(1):85–102. doi: 10.1177/0193945914551390. [DOI] [PubMed] [Google Scholar]
- 16.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(1):CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 17.Chen YC, Tsai JC, Liou YM, Chan P. Effectiveness of endurance exercise training in patients with coronary artery disease: A meta-analysis of randomised controlled trials. Eur J Cardiovasc Nurs. 2017;16(5):397–408. doi: 10.1177/1474515116684407. [DOI] [PubMed] [Google Scholar]
- 18.Lysen LK, Israel DA. Nutrition in weight management. In: Mahan LK, Escott-Stump S, Raymond JL, Krause MV, editors. Krause's food & the nutrition care process. Philadelphia, PA: Elsevier Health Sciences; 2012. pp. 462–88. [Google Scholar]
- 19.Furuyama F, Koba S, Yokota Y, Tsunoda F, Shoji M, Kobayashi Y. Effects of Cardiac Rehabilitation on High-Density Lipoprotein-mediated Cholesterol Efflux Capacity and Paraoxonase-1 Activity in Patients with Acute Coronary Syndrome. J Atheroscler Thromb. 2018;25(2):153–69. doi: 10.5551/jat.41095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Hobiken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 21.Berg A. Influence of physical exercise therapy (heart groups) on cardiovascular and metabolic functions in patients after myocardial-infarction. Herz Kreislauf. 1985;17(10):522–8. [Google Scholar]
- 22.Bigi R, Corradetti C, Gemma S, Occhi G, Partesana N, Curti PN. Short-term effect of a cardiac rehabilitation program on high-density lipoprotein-cholesterol of male survivors of myocardial infarction. Minerva Cardioangiol. 1985;33(3):127–34. [PubMed] [Google Scholar]
- 23.Li S, Wu X, Sun Q, He ZS, Ru LS, Yang L, et al. Effects of a two-week, hospitalized cardiac rehabilitation program on serum lipid profiles, quality of life and psychological status in patients with acute myocardial infarction. Chinese Journal of Rehabilitation Medicine. 2006;21(8):696. [Google Scholar]
- 24.Aronov DM, Krasnitskii VB, Bubnova MG, Posdniakov I, Ioseliani DV, Shchegol'kov AN, et al. Exercise in outpatient complex rehabilitation and secondary prophylaxis in patients with ischemic heart disease after acute coronary events (a cooperative trial in Russia). Ter Arkh. 2006;78(9):33–8. [PubMed] [Google Scholar]
- 25.Aronov DM, Krasnitskii VB, Bubnova MG, Pozdniakov I, Ioseliani DG, Shchegol'kov AN, et al. Physical training at ambulatory-polyclinical stage in complex rehabilitation and secondary prevention of patients with ischemic heart disease after acute incidents. Effect on physical working capacity, hemodynamics, blood lipids, clinical course and prognosis (Russian cooperative study). Kardiologiia. 2009;49(3):49–56. [PubMed] [Google Scholar]
- 26.Korzeniowska-Kubacka I, Piotrowicz R. Influence of exercise training on physical capacity, lipid profile and return to work of women after myocardial infarction. Folia Cardiol. 2004;10:719–25. [Google Scholar]
- 27.Ghroubi S, Elleuch W, Abid L, Kammoun S, Elleuch MH. Cardiac rehabilitation, coronary stenting and myocardial infarction. J Readapt Med. 2014;34(4):173–81. [Google Scholar]
- 28.Wosornu D, Bedford D, Ballantyne D. A comparison of the effects of strength and aerobic exercise training on exercise capacity and lipids after coronary artery bypass surgery. Eur Heart J. 1996;17(6):854–63. doi: 10.1093/oxfordjournals.eurheartj.a014966. [DOI] [PubMed] [Google Scholar]
- 29.Belardinelli R, Paolini I, Cianci G, Piva R, Georgiou D, Purcaro A. Exercise training intervention after coronary angioplasty: the ETICA trial. J Am Coll Cardiol. 2001;37(7):1891–900. doi: 10.1016/s0735-1097(01)01236-0. [DOI] [PubMed] [Google Scholar]
- 30.Yu CM, Li LS, Ho HH, Lau CP. Long-term changes in exercise capacity, quality of life, body anthropometry, and lipid profiles after a cardiac rehabilitation program in obese patients with coronary heart disease. Am J Cardiol. 2003;91(3):321–5. doi: 10.1016/s0002-9149(02)03159-4. [DOI] [PubMed] [Google Scholar]
- 31.Vona M, Rossi A, Capodaglio P, Rizzo S, Servi P, De Marchi M, et al. Impact of physical training and detraining on endothelium-dependent vasodilation in patients with recent acute myocardial infarction. Am Heart J. 2004;147(6):1039–46. doi: 10.1016/j.ahj.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 32.Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise in patients with coronary artery disease: Eeffects on body composition, blood lipids, and physical fitness. Am Heart J. 2007;154(3):560–6. doi: 10.1016/j.ahj.2007.06.029. [DOI] [PubMed] [Google Scholar]
- 33.Balen S, Vukelic-Damijani N, Persic V, Ruzic A, Miletic B, Samardiija M, et al. Anti-inflammatory effects of exercise training in the early period after myocardial infarction. Coll Antropol. 2008;32(1):285–91. [PubMed] [Google Scholar]
- 34.Seki E, Watanabe Y, Shimada K, Sunayama S, Onishi T, Kawakami K, et al. Effects of a phase III cardiac rehabilitation program on physical status and lipid profiles in elderly patients with coronary artery disease: Juntendo Cardiac Rehabilitation Program (J-CARP). Circ J. 2008;72(8):1230–4. doi: 10.1253/circj.72.1230. [DOI] [PubMed] [Google Scholar]
- 35.Luk TH, Dai YL, Siu CW, Yiu KH, Chan HT, Lee SW, et al. Effect of exercise training on vascular endothelial function in patients with stable coronary artery disease: A randomized controlled trial. Eur J Prev Cardiol. 2012;19(4):830–9. doi: 10.1177/1741826711415679. [DOI] [PubMed] [Google Scholar]
- 36.Aksoy S, Findikoglu G, Ardic F, Rota S, Dursunoglu D. Effect of 10-week supervised moderate-intensity intermittent vs. continuous aerobic exercise programs on vascular adhesion molecules in patients with heart failure. Am J Phys Med Rehabil. 2015;94(10 Suppl 1):898–911. doi: 10.1097/PHM.0000000000000306. [DOI] [PubMed] [Google Scholar]
- 37.Hassan AM, El Nahas. Efficacy of cardiac rehabilitation after percutaneous coronary intervention. Int J PharmTech Res. 2016;9:134–41. [Google Scholar]
- 38.Tamburus NY, Kunz VC, Salviati MR, Castello S, Catai AM, Da SE. Interval training based on ventilatory anaerobic threshold improves aerobic functional capacity and metabolic profile: a randomized controlled trial in coronary artery disease patients. Eur J Phys Rehabil Med. 2016;52(1):1–11. [PubMed] [Google Scholar]
- 39.Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 40.Oldridge N. Exercise-based cardiac rehabilitation in patients with coronary heart disease: Meta-analysis outcomes revisited. Future Cardiol. 2012;8(5):729–51. doi: 10.2217/fca.12.34. [DOI] [PubMed] [Google Scholar]
- 41.Lawler PR, Filion KB, Eisenberg MJ. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Am Heart J. 2011;162(4):571–84. doi: 10.1016/j.ahj.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 42.Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 43.Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–53. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 44.Fox KM. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: Randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet. 2003;362(9386):782–8. doi: 10.1016/s0140-6736(03)14286-9. [DOI] [PubMed] [Google Scholar]
- 45.Dor-Haim H, Barak S, Horowitz M, Yaakobi E, Katzburg S, Swissa M, et al. Improvement in cardiac dysfunction with a novel circuit training method combining simultaneous aerobic-resistance exercises. A randomized trial. PLoS One. 2018;13(1):e0188551. doi: 10.1371/journal.pone.0188551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pierson LM, Herbert WG, Norton HJ, Kiebzak GM, Griffith P, Fedor JM, et al. Effects of combined aerobic and resistance training versus aerobic training alone in cardiac rehabilitation. J Cardiopulm Rehabil. 2001;21(2):101–10. doi: 10.1097/00008483-200103000-00007. [DOI] [PubMed] [Google Scholar]