Abstract
Background
The onset of the COVID-19 pandemic led to the postponement of low-acuity surgical procedures in an effort to conserve resources and ensure patient safety. This study aimed to characterize patient-reported concerns about undergoing surgical procedures during the pandemic.
Methods
We administered a cross-sectional survey to patients who had their general and plastic surgical procedures postponed at the onset of the pandemic, asking about barriers to accessing surgical care. Questions addressed dependent care, transportation, employment and insurance status, as well as perceptions of and concerns about COVID-19. Mixed methods and inductive thematic analyses were conducted.
Results
One hundred thirty-five patients were interviewed. We identified the following patient concerns: contracting COVID-19 in the hospital (46%), being alone during hospitalization (40%), facing financial stressors (29%), organizing transportation (28%), experiencing changes to health insurance coverage (25%), and arranging care for dependents (18%). Nonwhite participants were 5 and 2.5 times more likely to have concerns about childcare and transportation, respectively. Perceptions of decreased hospital safety and the consequences of possible COVID-19 infection led to delay in rescheduling. Education about safety measures and communication about scheduling partially mitigated concerns about COVID-19. However, uncertainty about timeline for rescheduling and resolution of the pandemic contributed to ongoing concerns.
Conclusions
Providing effective surgical care during this unprecedented time requires both awareness of societal shifts impacting surgical patients and system-level change to address new barriers to care. Eliciting patients’ perspectives, adapting processes to address potential barriers, and effectively educating patients about institutional measures to minimize in-hospital transmission of COVID-19 should be integrated into surgical care.
Keywords: Surgery, COVID-19, Patient experience, Patient perceptions, Delayed procedures
Introduction
In response to the COVID-19 pandemic, the surgical community rapidly mobilized resources and altered surgical workflows to accommodate a potential surge in patients in need of hospitalization.1, 2, 3, 4 On March 18, 2020, the U.S. Centers for Medicare and Medicaid Services published recommendations to pause all nonessential surgeries and procedures to conserve critical resources, such as ventilators and personal protective equipment.5 Subsequently, a large number of medically necessary but ‘nonessential’ surgeries were delayed. To facilitate this process, the University of California, San Francisco (UCSF) Health System developed a surge algorithm to classify surgical cases based on urgency in accordance with the American College of Surgeon Triage Guidelines, with tier 1 being truly elective cases.1 , 6 , 7
The COVID-19 pandemic has impacted every aspect of society. Patients' lives have been upended by the closure of childcare facilities and shifts to virtual schooling. Whole sectors of the economy have been ravaged with unemployment rates at levels not seen for decades.8 The latter has led to changes in health insurance coverage, financial stressors, and housing status.9 These social stressors may impact patients’ ability and desire to pursue surgical treatment, particularly for nonurgent diagnoses. In addition, many patients are concerned that hospitals are a high-risk setting for contracting COVID-19, which may further increase their reticence to seek medical care.9 , 10 Since the onset of the pandemic, reports in the literature have indicated that fear of contracting COVID-19 has contributed to delays in seeking care.9 This has been associated with a decrease in emergency department visits as well as overall reduction in procedural volumes since March 2020.8 , 10, 11, 12 Our region returned to normalization in scheduling tier 1 cases as of late May 2020.
In May 2020, UCSF looked to safely resume surgical care, with an initial focus on patients whose procedures were previously postponed. We sought to understand patients’ concerns, barriers, and facilitators to obtaining tier 1 surgical care and evaluate how demographics and social characteristics influence these concerns. Although studies have examined the effects of previous pandemics, like the 2003 SARS pandemic, on access to surgical care, little is known about patient perceptions of the challenges.13 To our knowledge, this is the first study to evaluate patient perspectives related to obtaining surgical care in the setting of a pandemic.
Methods
Setting
Faculty from the UCSF Department of Surgery attend at two San Francisco hospitals: UCSF Health and Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG). This study focused on tier 1 patients at the UCSF Health (700-bed academic medical center) and Zuckerberg San Francisco General Hospital (200-bed public, safety-net hospital).
Study design and analyses
Using a mixed-methods approach, we surveyed patients whose tier 1 surgical procedures were postponed because of the pandemic on the perceived barriers and facilitators they faced in accessing surgical care, the impact of external factors, and attitudes toward perioperative safety during the COVID-19 pandemic. Patient demographic information including age, gender, race, ethnicity, and language spoken were collected via electronic health record review. This information is culled in the record directly by patient self-report. We designed a telephone script with five-point Likert-scale survey questions and open text comments that queried for patient concerns associated with the following six domains developed based on clinical practice: caregiver burden, employment consideration, health insurance, transportation issues, exposure to the COVID-19 virus while in the hospital or in the community at large, and restricted visitation policies around the time of surgery. After the survey questions, the script included information about hospital practices related to COVID-19 including masking, visitor policy, hand hygiene, and the risk of acquiring COVID-19 during hospitalization. The survey was piloted on five patients and then revised to more clearly convey the purpose of the interview and facilitate rapport building between the caller and patient. Examples included acknowledging the stress and uncertainty associated with postponed procedures, inviting patients to explain their concerns, empathizing with patient worries, and providing education materials that addressed specific patient concerns especially around the COVID-19 virus and safety.
The student doctors and plastic surgery resident physicians conducted the phone interviews between May 1 and June 18, 2020. Calls were placed between 9 AM and 8 PM on Monday-Saturday during this time period. If patients did not answer, they were called back for a total of four attempts on two different days. An interpreter service was used if the primary language in the electronic health record was listed as other than English. This study was deemed exempt by the UCSF Institutional Review Board.
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at UCSF.14 , 15 STATA v16.1 was used to analyze quantitative data.16
Qualitative data were analyzed by a team of researchers using inductive thematic analysis to determine common themes and insights. A resident researcher with training in human-centered design through the UCSF Better Lab trained the other coders in this method.17 , 18 Researchers underwent practice rounds during which coding strategy was evaluated. Each researcher developed themes independently, and these were shared with the group along with all raw comments to confirm dependability of thematic analysis. This method has been described in by Wong et al. 10 The coded material was then grouped into major themes and organized into barriers and facilitating factors. This process was iterative in nature, and each researcher returned to the raw data to verify the trustworthiness of themes. Data were managed within Mural.co, a digital workspace that enables data and theme visualization.
Results
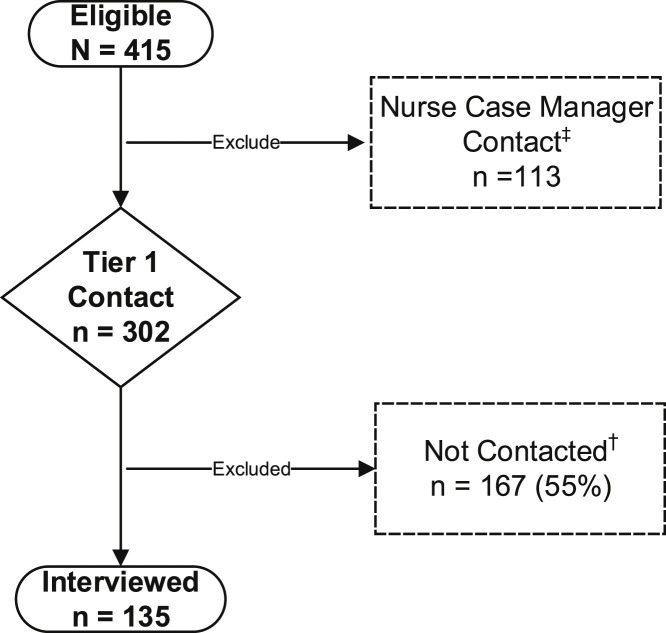
We identified 415 patients who had a delayed tier 1 general or plastic surgery procedure in March or April 2020 at UCSF (n = 365) or ZSFG (n = 50). We excluded (27%) from UCSF Health who were already receiving outreach by another group as part of the COVID-19 recovery program. The remaining 302 patients underwent medical record review by five student doctors and two plastic surgery resident physicians to confirm that they had been scheduled for surgery before the COVID-19 pandemic. Forty-seven patient charts were screened but excluded for the following reasons: the patient already had surgery, the patient was incarcerated, or there was a confidentiality prohibition in the medical record. One hundred twenty patients were called but not interviewed because they were not able to be reached or declined to participate (Fig. 1 ). We compared demographic and clinical characteristics for those who were contacted and agreed to be interviewed by phone versus those who declined participation or were unable to be contacted. No significant differences were observed between these two groups for mean age, gender, race, language preference, the need for a language interpreter, institution (UC Health versus ZSFG), or surgical priority status (low or normal status). However, those who were contacted were slightly older (48.9 y old (±14.3) versus 46.2 y old (±15.0) (P = 0.06)).
Fig. 1.
The consort diagram of study patients: Tier 1 surgery approved but on hold and quality of care phone follow-up.
In total, 135 patients were surveyed by telephone, a response rate of 45%. Patient demographic characteristics were compared between the two institutions using Student's t-test and Pearson's chi-square analysis. No significant difference was observed for age (p. 0.64). However, ZSFG patients were nearly equally distributed by sex, whereas UCSF Health patients were predominately female (76% versus 52%, P = 0.05). UCSF Health had more white patients than ZSFG (62% versus 16%, P < 0.05). Nearly half (48%) of patients interviewed at ZSFG required language interpretation versus <1% at UCSF Health (P < 0.01) (Table 1 ).
Table 1.
Demographic characteristics of tier 1 phone survey participants (n = 135).
| Characteristic | ZSFG§ |
UCSF‖ |
P-value |
|---|---|---|---|
|
n = 25 |
n = 110 |
||
| Mean (SD∗) | Mean (SD) | ||
| Age† (in years) | 50.6 (±14) | 48.5 (±14.4) | 0.64 |
| Sex‡ | n (%) | n (%) | 0.05 |
| Male | 12 (48) | 26 (23.6) | |
| Female | 13 (52) | 83 (75.5) | |
| Other | -- | 1 (0.9) | |
| Race/ethnicity‡ | n (%) | n (%) | 0.00 |
| Asian | 2 (8) | 5 (4.5) | |
| Black or African American | 5 (20) | 5 (4.5) | |
| Latinx | 13 (52) | 11 (10) | |
| White or Caucasian | 4 (16) | 68 (61.8) | |
| Other | -- | 6 (5.5) | |
| Unknown/declined | 2 (8) | 18 (16.4) | |
| Interpreter‡ | n (%) | n (%) | 0.00 |
| Required a language interpreter | 12 (48) | 1 (0.9) | |
| Language preference‡ | n (%) | n (%) | 0.00 |
| English | 13 (52) | 109 (99.1) | |
| Spanish | 11 (44) | 1 (0.9) | |
| Cantonese | 1 (4) | -- |
Bolded P-values denote statistical significance.
SD is standard deviation.
Student's t-test significance at ≤ 0.05.
Pearson's χ2 test significance at ≤ 0.05.
ZSFG is Zuckerberg San Francisco General Hospital.
UCSF is University of California San Francisco Health.
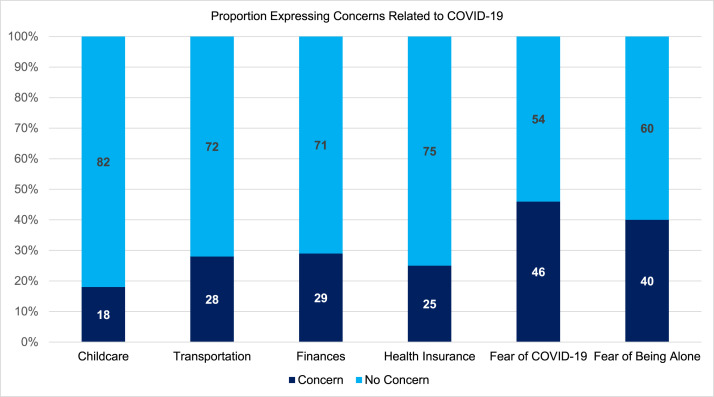
Patient concerns in the six question domains were recoded to a dichotomous outcome of no concern versus concerned because data were largely bimodal and to account for limited selection of some response options. Overall, 88% of patients reported concern in one or more of the six domains. Acquiring COVID-19 infection while hospitalized and the restrictive visitor policies generated the highest level of concern (54% and 40%, respectively) (Fig. 2 ). Despite concerns about contracting COVID-19, very few patients reported a personal history of COVID-19 infection (1.5%) or exposure to COVID-19 (4.5%), consistent with the low prevalence of COVID-19 in San Francisco as of June 18, 2020.19 Sixteen percent reported that their symptoms related to their surgical condition worsened while waiting to have surgery.
Fig. 2.
Areas of concern versus no concern (n = 1346). The fear of COVID question worded as “How worried are you about getting COVID-19 in the hospital?”. The fear of being alone question worded as “How concerned are you about being alone in the hospital if visitors are not allowed?”. (Color version of the figure is available online.)
We used univariate logistic regression to examine patient level of concern by the six domains (Table 2 ). When compared with older adults, younger adults (age 48 or younger) had 3.5 times the odds of having concerns about childcare or dependent care (P = 0.01), had 2.3 times the odds of having a transportation concern (P = 0.04), and had nearly 2.5 times the odds of having concerns regarding their financial well-being (P = 0.03). No significant differences were observed by sex for any of the six areas of concern. Compared with white participants, nonwhite participants had nearly 5 times the odds of having concerns about childcare or other dependent care (P = 0.01) and 2.5 times the odds of having concerns about transportation (P = 0.04); there was no significant difference in concern about finances (P = 0.09). Comparing the six areas of concern by hospital site revealed no statistically significant differences in childcare, transportation, health insurance, fear of COVID, or fear of being alone during hospitalization. Although not statistically significant (P = 0.07), financial concerns were expressed by 44% of patients at ZSFG compared with 26% of patients at UCSF Health.
Table 2.
| Characteristic | Odds ratio (95% CI) | P-value |
|---|---|---|
| Child/dependent care | ||
| Age (<49 y) | 3.47 (1.28-9.40) | 0.01 |
| Female | 1.23 (0.44-3.38) | 0.69 |
| Race (compared with white) | ||
| Nonwhite | 4.89 (1.71-13.94) | 0.01 |
| Unknown | 3.09 (0.77-12.44) | 0.11 |
| Transportation | ||
| Age (<49 y) | 2.27 (1.04-4.96) | 0.04 |
| Female | 0.96 (0.41-2.20) | 0.92 |
| Race (compared with white) | ||
| Nonwhite | 2.46 (1.04-5.97) | 0.04 |
| Unknown | 4.46 (1.48-13.43) | 0.01 |
| Economic | ||
| Age (<49 y) | 2.42 (1.11-5.27) | 0.03 |
| Female | 1.78 (0.73-4.35) | 0.20 |
| Race (compared with white) | ||
| Nonwhite | 2.05 (0.89-4.74) | 0.09 |
| Unknown | 2.98 (1.00-8.88) | 0.05 |
| Health insurance | ||
| Age (<49 y) | 1.27 (0.58-2.77) | 0.55 |
| Female | 1.39 (0.56-3.42) | 0.47 |
| Race (compared with white) | ||
| Nonwhite | 1.15 (0.49-13.94) | 0.74 |
| Unknown | 1.22 (0.38-3.92) | 0.73 |
| Fear of COVID | ||
| Age (<49 y) | 0.99 (0.50-1.96) | 0.98 |
| Female | 0.67 (0.31-1.45) | 0.32 |
| Race (compared with white) | ||
| Nonwhite | 0.96 (0.45-2.02) | 0.91 |
| Unknown | 1.83 (0.62-5.43) | 0.27 |
| Fear of being alone | ||
| Age (<49 y) | 0.90 (0.45-1.80) | 0.78 |
| Female | 1.23 (0.44-3.38) | 0.68 |
| Race (compared with white) | ||
| Nonwhite | 1.26 (0.59-2.71) | 0.54 |
| Unknown | 1.73 (0.61-4.90) | 0.30 |
CI = confidence interval.
6 One person contacted but not formally interviewed because of ‘other’ patient concerns about surgery. Therefore, reporting on 134 respondent concerns.
Bolded P-values denote statistical significance.
Age categorized ≥49 y old (0) or ≤ 48 y old (1); older age group used as reference; (range 18-82; median 48).
Gender dichotomous male (0) or female (1); male category used as a reference group.
Race categorial variable of white, Nonwhite, or unknown; white race used a reference group.
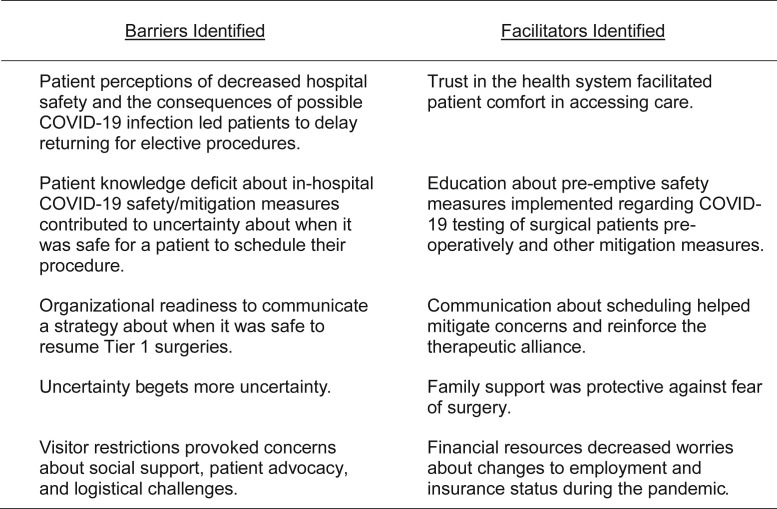
We then performed inductive thematic analysis of patient comments (Fig. 3 ). Concerns about hospital transmission were linked to impressions that the hospital was not taking adequate safety measures. Effective institution-patient communication and education improved patient perception of institutional safety measures and encouraged them to proceed with surgery. One interviewee commented that she “had slight concerns about getting COVID in the hospital…but that people on her care team were forthcoming about answering questions…and she felt reassured.” Patients reported uncertainty and frustration regarding the delay of their care and future scheduling. This uncertainty made arranging childcare, travel, and planning for the financial impacts of elective surgery difficult. Possible unemployment was tied to fears of losing insurance coverage, and travel concerns were often related to concerns about dependent care. One patient shared that they were “not sure how the delay will influence authorization and approval for surgery. Additionally, [I] may not have a job soon,” making the patient “nervous that this will affect insurance status.” Patients with reliable sources of income from retirement, established disability coverage, or pre-existing unemployment expressed less concern and were more amenable to rescheduling surgery once dates were offered.
Fig. 3.
Qualitative themes of barriers and facilitators to obtaining surgical care.
Discussion
This study demonstrates that patients who are in need of low-acuity elective surgery are experiencing many concerns as they consider surgical care during the COVID-19 pandemic. Concerns about the consequence of contracting COVID-19 in the hospital were rooted in fears that the hospital was not a safe environment and exacerbated by the presence of pre-existing conditions. Uncertainty surrounding the timing of surgery led patients to fear that their conditions may worsen or that impending loss of insurance coverage might lead to the future denial of a preapproved procedure. Visitor restrictions were a concern because visitors served as patient advocates and assisted in communicating patient needs to the health team. Racial and ethnic disparities were present in our patient population, with nonwhite patients reporting a higher burden of concern than white patients, specifically with respect to transportation and childcare as it related to surgery planning.
The COVID-19 pandemic has illuminated existing inequities in access to medical care in the United States.20, 21, 22 Studies have demonstrated that nonwhite populations have higher rates of infection and mortality than white populations.23, 24, 25 In our study, nonwhite patients had a higher level of concern regarding fundamental needs such as transportation and childcare, likely amplified by the closure of schools and reduction of public transit capacity during shelter in place.25, 26, 24 In addition, nearly a third of patients interviewed expressed financial concerns and more than a quarter reported concerns about changes to health insurance. Although many of these barriers likely preceded the pandemic, patients did note concerns specific to pandemic-related shifts including changes in insurance coverage, limited visitor policies, and concerns about public transportation.24 This highlights a key opportunity to support patients who will be imperative throughout the pandemic and beyond, as the insurance and employment landscape is ever-changing. Identifying and streamlining departmental and system-level processes (e.g., within teams such as social work and patient financial services) to ensure there is sufficient capacity to assist patients in navigating these changes should be adequately prioritized.27 , 28
Based on the findings of our study, since early May, as part of the UCSF Health COVID-19 recovery, we have continued to evolve our care to support our patients. These changes include modifying the visitor policy to allow all patients to have one visitor each day; the patient relations team has developed a task force and materials to support messaging around hospital safety in the setting of the COVID-19 pandemic, and in a subset of clinics, a patient navigator/social work pilot has been developed to support patients who are struggling to find childcare and transportation resources. Importantly, we developed collaborative work groups between the surgeons, clinics, and operational leaders to try to dynamically identify and address patient concerns that are surfaced during this constantly evolving and uncertain time.
Our study has several limitations. The patient population was limited to four surgical subspecialties at two specific UCSF-affiliated settings, a large academic medical center and a safety-net hospital. The perspectives of patients undergoing other types of procedures and in other settings such as Veterans Affairs Medical Centers or community hospitals may be different and could be addressed in futures studies. In addition, our effort was focused during a singular unique time when elective cases were initially postponed. However, it is likely that surgical care will continue to ebb and flow as the pandemic evolves, and patient concerns will persist. Finally, about a third of patients called were unable to be reached. We hypothesize that patients did not answer phone calls because of screening calls of unknown numbers or being unavailable during the workday, which we attempted to mitigate by expanding call times to evening hours and Saturdays. Future directions include surveying the same group of patients postoperatively, interviewing patients to develop a baseline understanding of the barriers and facilitators they faced to obtaining surgical care before the pandemic, as well as understanding the provider perspective to inform the development of more transparent systems of communication.
Conclusions
Our findings suggest that as the COVID-19 pandemic continues, it is imperative that we continue to understand, empathize with, and address the barriers and concerns of our patients. It is critical to develop systems that help us to understand and adapt to our patients’ perspectives and deliver safe, patient-centered surgical care during this unprecedented time.
Acknowledgment
We thank Julie Ann Sosa MD, MA, Chair of the Department of Surgery at UCSF, for her support in this study.
Authors' contributions
S.A.R., E.C.W., and T.B. contributed to study concept. S.A.R., J.M.B., S.B.K., and C.L.J. contributed to survey creation. C.L.J., H.S., A.G., S.H., O.N.N.S., L.E.W., D.B.M., S.B.K., and T.B. contributed to data acquisition and analysis. J.M.B. contributed to quantitative analysis. C.L.J., H.S., J.M.B., L.E.W., S.A.R., E.C.W., and T.B contributed to thematic analysis. C.L.J., H.S., A.G., S.H., O.N.N.S., L.E.W., D.B.M., S.B.K., and J.M.B. contributed to manuscript preparation. S.A.R., T.B., E.C.W., and J.M.B. contributed to manuscript editing. S.A.R. and E.C.W.contributed to study supervision.
Support: Drs. E.C.W. and J.M.B were supported by the Agency for Healthcare Research and Quality (AHRQ) [RO1#: 5R01HS024532, 09/30/2016-09/29/2020].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jss.2021.01.028.
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article. None of the authors have any COI/financial disclosure.
Appendix A. Supplementary data
References
- 1.Lancaster E.M., Sosa J.A., Sammann A., et al. Rapid response of an academic surgical department to the COVID-19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064–1073. doi: 10.1016/j.jamcollsurg.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flemming S., Hankir M., Ernestus R.-I., et al. Surgery in times of COVID-19—recommendations for hospital and patient management. Langenbecks Arch Surg. 2020;1–6 doi: 10.1007/s00423-020-01888-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Jabir A., Kerwan A., Nicola M., et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg Lond Engl. 2020;79:168–179. doi: 10.1016/j.ijsu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brindle E.M., Gawande A. Managing COVID-19 in surgical systems. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anon CMS Releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response | CMS. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental Available at:
- 6.Prachand V.N., Milner R., Angelos P., et al. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020;231:281–288. doi: 10.1016/j.jamcollsurg.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirk A., Siddiqui S. COVID-19: guidance for triage of non-emergent surgical procedures. Am Coll Surg. 2020 https://www.facs.org/covid-19/clinical-guidance/triage Available at: [Google Scholar]
- 8.Galea S., Abdalla S.M. COVID-19 pandemic, unemployment, and civil unrest: underlying deep racial and socioeconomic divides. JAMA Am Med Assoc. 2020;324:227–228. doi: 10.1001/jama.2020.11132. [DOI] [PubMed] [Google Scholar]
- 9.Claxton G., Damico A. Eligibility for ACA health coverage following job loss. Kaiser family foundation (KFF) 2020. 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/eligibility-for-aca-health-coverage-following-job-loss/ Available at:
- 10.Wong L.E., Hawkins J.E., Langness S., et al. Where are all the patients? Addressing covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal Innov Care Deliv. 2020;1:1–12. [Google Scholar]
- 11.Gao Y., Sun F., Jiang W., et al. Beliefs towards the COVID-19 pandemic among patients with emotional disorders in China. Gen Psychiatry. 2020:33. doi: 10.1136/gpsych-2020-100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lazzerini M., Barbi E., Apicella A., et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schull M.J., Stukel T.A., Vermeulen M.J., et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007;176:1827–1832. doi: 10.1503/cmaj.061174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris P.A., Taylor R., Thielke R., et al. Research Electronic Data Capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anon . StataCorp LLC; College Station, TX: 2019. StataCorp. Stata: release 16 statistical software. [Google Scholar]
- 17.Patel D., Berger C.A., Kityamuwesi A., et al. Iterative adaptation of a tuberculosis digital medication adherence technology to meet user needs: qualitative study of patients and health care providers using human-centered Design methods. JMIR Form Res. 2020;4:e19270. doi: 10.2196/19270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel D., Sarlati S., Martin-Tuite P., et al. Designing an information and communications technology tool with and for victims of violence and their case managers in san Francisco: human-centered Design study. JMIR Mhealth Uhealth. 2020;8:e15866. doi: 10.2196/15866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anon COVID-19 cases and deaths. https://data.sfgov.org/stories/s/COVID-19-Cases-and-Deaths/dak2-gvuj/ Available at:
- 20.Baum A., Schwartz M.D. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA Am Med Assoc. 2020;324:96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ku L., Brantley E. Widening social and health inequalities during the COVID-19 pandemic. JAMA Health Forum Am Med Assoc. 2020;1:e200721. doi: 10.1001/jamahealthforum.2020.0721. [DOI] [PubMed] [Google Scholar]
- 22.Tai D.B.G., Shah A., Doubeni C.A., et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA Am Med Assoc. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cyrus E., Clarke R., Hadley D., et al. medRxiv [Preprint]; 2020. The impact of COVID-19 on African American communities in the United States. Update in: Health Equity. 2020;4:476-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yancy C.W. COVID-19 and African Americans. JAMA Am Med Assoc. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 26.Anon COVID-19 health orders -- san Francisco department of public health. https://www.sfdph.org/dph/alerts/coronavirus-healthorders.asp Available at:
- 27.Anon Schools will close to students for 3 Weeks | SFUSD. https://www.sfusd.edu/about/news/current-news/schools-will-close-students-3-weeks Available at:
- 28.Fowler A. Starting March 30: new muni service changes. SFMTA 2020. https://www.sfmta.com/blog/starting-march-30-new-muni-service-changes Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.