Abstract
Introduction
This study aimed to assess the impact of the coronavirus disease 2019 (COVID-19) pandemic on the orthodontic patient. It also assessed the knowledge and attitude of patients to the COVID-19 infection and the willingness to carry out specific precautionary measures in the orthodontic clinics to mitigate the spread of the virus.
Methods
It was a cross-sectional descriptive study. Questionnaires were distributed to orthodontic patients via Google forms. The questionnaire assessed participants’ knowledge, attitude, the impact of the COVID-19 pandemic on orthodontic treatment, and willingness to carry out infection control precautionary measures in the orthodontic clinic.
Results
A total of 304 responses were obtained; 83 males (27.3%), 221 females (72.7%) with a mean age of 35.6 years. Subjects demonstrated good knowledge of COVID-19 infection (94.7%). Most respondents (95%) considered the infection as dangerous and believed the orthodontic patient was at risk of contracting the disease but were willing regardless to carry on with their orthodontic treatment during the pandemic. Fear of contracting the COVID-19 virus during orthodontic appointments and missed orthodontic appointments (74%), and increased treatment time (50%) were the immediate and long-term concerns, respectively. A high acceptance rate of compliance to precautionary measures to mitigate virus spread in the clinic was observed.
Conclusions
The COVID-19 pandemic has had a negative impact on the orthodontic treatment and the financial and emotional wellbeing of orthodontic patients. Patients were willing to continue with orthodontic management during the pandemic while complying with precautionary measures to prevent disease spread in the orthodontic practice setting.
Coronavirus disease 2019 (COVID-19) is caused by a new strain of the coronavirus, severe acute respiratory syndrome coronavirus 2, first reported in Wuhan, China, in December 2019.1 The COVID-19 infection has been reported to cause a wide spectrum of symptoms in humans ranging from mild to severe disease manifestations and may sometimes be fatal.2 It was declared a pandemic by the World Health Organization on January 30, 2020, and since then has spread very rapidly, affecting almost all the countries in the world, with over 10.98 million reported patients, multiple hospitalizations, and 524,036 mortalities as of July 3, 2020.3
The first official patient with COVID-19 in the country was reported on February 27, 2020. Since then, the infection has spread rapidly to all 36 states in the country, including the Federal Capital territory, with palpable strain on the health sector. The National Centre for Disease Control has reported approximately 27,110 COVID-19 cases and 616 COVID-19 related deaths.4
The mode of transmission of COVID-19 is primarily via droplet and aerosol spread by coughing, sneezing, talking, and direct contact with droplet/aerosol contaminated surfaces, with an incubation period lasting 2-14 days.5 , 6
Dental care involves the treatment and prevention of oral diseases/conditions, often using rotary dental and surgical instruments. These instruments produce sprays that contain large particle droplets of water, saliva, blood, microorganisms, and other debris. These sprays move a short distance and settle on dental surfaces, dental office staff and or patients.7
Dental treatments require proximity between the patient and dental health care workers.8 Orthodontic procedures such as bonding, debonding, interproximal reduction, replacement of broken brackets are capable of generating aerosols. This issue poses a consequent risk of cross-infection (patient to patient, patient to dental health care provider, and dental health care provider to dental health care provider transmission), especially if meticulous infection control measures are not employed.8 , 9
In view of the aforementioned risks in the dental practice setting, many national dental associations all over the world have recommended that dental clinics close down during this period or significantly scale down the level of dental care provided to strictly emergency and urgent dental care, while all elective dental procedures are suspended.10, 11, 12 Many countries also recommended a total or partial lockdown of the system to curtail the virus spread.
Orthodontics is a specialty of dentistry that deals with the management of malocclusion, with comprehensive fixed orthodontic treatment lasting approximately 2-3 years and regular review appointments about 6-8 weeks. Deferring treatment until the end of the pandemic will inadvertently prolong the treatment time with possible associated consequences on the patients and their orthodontic treatment.
With this consideration in mind, many orthodontists may have to resume clinical practice in the nearest future, bearing in mind the risk of infection and putting measures in place to prevent this.13
However, it is important to bear in mind that compliance with meticulous infection control measures and protocols by all dental health care workers is important to prevent COVID-19 spread in the dental clinic.
A good understanding of the pathogenesis of the disease is also required by the patients, as well as a willingness to comply with recommended measures to prevent the spread. Some of these precautions include frequent hand hygiene using soap and water or alcohol-based hand rub, proper respiratory hygiene, use of facemask, and physical distancing. These must be strictly adhered to ensure the safety of the dental health care workers and the patients alike if orthodontic practices are reopened.
Some possible effects of the COVID-19 pandemic on the orthodontic patients may not only be limited to missed orthodontic appointments and fear of contracting the virus but may span through psychological, emotional, and financial consequences.
This study aimed to assess the perceived impact of the COVID-19 pandemic on the orthodontic patient. It also assessed the knowledge and attitudes of patients to the COVID-19 infection, as well as a willingness to carry out specific precautions to help prevent the spread of the virus, especially in the orthodontic clinics.
Material and methods
The study was a cross-sectional descriptive study. Ethical approval for this study was obtained from the Institutional Review Board of the Lagos University Teaching Hospital, Idi-araba, Lagos, Nigeria. Self-administered structured multiple-choice questionnaires were distributed to consenting participants through an online data collection platform (Google forms). A purposive sampling technique was used. The study population comprised orthodontic patients receiving treatment in public and private dental facilities in the state.
The respondents were reached using the WhatsApp (Facebook, Inc, Menlo Park, Calif) platform, and via e-mails. The questionnaire (Supplementary Text), modified from a study carried out by Khader et al6 and Isiekwe et al14 was used as the instrument for data collection in this study. The questionnaire contained 4 sections: Section 1: participants' sociodemographics; Section 2: participants' perceived impact of the COVID-19 pandemic on orthodontic treatment; Section 3: participants’ knowledge about the COVID-19 infection; and Section 4: risk perception and attitude toward the COVID-19 infection.
A pilot study was done. The questionnaire was distributed to 10 orthodontic patients to assess the validity of the instrument. These were not included in the overall samples used for the study. The questionnaire distribution was carried out for over 6 weeks. The study instrument was sent out to 400 patients.
Statistical analysis was carried out using SPSS (version 23.0; IBM, Armonk, NY). Data were subjected to simple descriptive statistical analysis (means and standard deviation or median and interquartile range), and results were presented in frequency tables and charts. Comparisons between groups were carried out using the chi-square for categorical variables, and the level of significance was set at 0.05.
Results
A total of 400 questionnaires were sent out, with a response rate of 67% (304 responses). The demographic characteristics of the study subjects showed 304 respondents aged 9-56 years, with a mean age of 35.6 years. The predominant age group of respondents was 11-20 years. A higher female predominance was observed, accounting for 72.7% of the surveyed population. Approximately 62% of the subjects had attained a tertiary level of education (Table I ). A majority of the respondents were undergoing fixed appliance orthodontic treatment (91.1%), accessing treatment in a government hospital (64.5%), and were paying out of pocket for orthodontic care (88.8%) (Table I).
Table I.
Sociodemographic characteristics
| Variable | Frequency (%), n = 304 |
|---|---|
| Age, y | |
| <10 | 10 (3.3) |
| 11-20 | 132 (43.4) |
| 21-30 | 83 (27.3) |
| 31-40 | 49 (16.1) |
| 41-50 | 26 (8.6) |
| 51-60 | 4 (1.3) |
| Sex | |
| Female | 221 (72.7) |
| Male | 83 (27.3) |
| Religion | |
| Christianity | 274 (90.1) |
| Islam | 29 (9.5) |
| Others | 1 (0.3) |
| Marital status | |
| Married | 56 (18.4) |
| Single | 243 (79.9) |
| Others | 5 (1.6) |
| Level of education | |
| Postgraduate | 92 (30.3) |
| Primary | 11 (3.6) |
| Secondary | 105 (34.5) |
| Tertiary | 96 (31.6) |
| Number of months in orthodontic treatment | |
| 1-12 | 122 (40.1) |
| 13-24 | 85 (28.0) |
| 25-36 | 48 (15.8) |
| 37-48 | 11 (3.6) |
| >48 | 38 (12.5) |
| Facility where you are receiving treatment | |
| Government hospital | 196 (64.5) |
| Private hospital | 108 (35.5) |
| Modality of payment of orthodontic treatment | |
| Out of pocket (self) | 270 (88.8) |
| Health insurance | 3 (1.0) |
| A combination of both | 10 (3.3) |
| Others | 21 (6.9) |
| Type of orthodontic treatment | |
| Removable appliance | 25 (8.2) |
| Fixed | 277 (91.1) |
| Others | 2 (0.7) |
Almost all the participants considered their level of knowledge of COVID-19 to be moderate to high (98%). They demonstrated a good knowledge of disease etiology, symptoms, modes of transmission, and prevention of the COVID-19 infection. Hand hygiene with soap and water (99.3%), routine disinfection of contaminated surfaces (97.7%), hand sanitization using alcohol-based hand rub (96.4%) were popular preventive measures among respondents (Table II ).
Table II.
Knowledge of COVID-19 among participants
| Responses to questions asked on COVID-19 | Correct | Incorrect |
|---|---|---|
| What kind of infection is COVID-19 | ||
| Virus | 288 (94.7) | 16 (5.3) |
| Average incubation period of COVID-19 | ||
| 2-14 d | 276 (90.8) | 28 (9.2) |
| Symptoms of COVID-19 | ||
| May be asymptomatic | 167 (54.9) | 137 (45.1) |
| Fever | 279 (91.7) | 25 (8.3) |
| Cough | 288 (94.7) | 16 (5.3) |
| Sore throat | 249 (81.9) | 55 (18.1) |
| Shortness of breath | 286 (94.1) | 18 (5.9) |
| Diarrhea | 78 (25.7) | 226 (74.3) |
| Vomiting | 44 (14.5) | 260 (85.5) |
| Running nose | 103 (33.9) | 201 (66.1) |
| Red eyes | 26 (8.6) | 278 (91.4) |
| Skin rash | 24 (7.9) | 280 (92.1) |
| Joint/muscle pain | 79 (26) | 225 (74) |
| Loss of taste | 145 (47.7) | 159 (52.3) |
| Loss of smell | 138 (45.4) | 166 (54.6) |
| How COVID-19 can be prevented | ||
| Coughing and sneezing | 284 (93.4) | 20 (6.6) |
| Handshaking | 272 (89.5) | 32 (10.5) |
| Touching contaminated surfaces | 286 (94.1) | 18 (5.9) |
| Talking | 128 (42.1) | 176 (57.9) |
| How COVID-19 transmission can be transmitted | ||
| Regular handwashing with soap and water | 302 (99.3) | 2 (0.7) |
| Use of alcohol-based hand rub | 293 (96.4) | 11 (3.6) |
| Routine disinfection of contaminated surfaces | 297 (97.7) | 7 (2.3) |
| Use of personal protective clothing by all dental staffs | 277 (91.1) | 27 (8.9) |
| Use of facemasks by all patients | 270 (88.8) | 34 (11.2) |
| Keeping patients in well-ventilated rooms | 191 (62.8) | 113 (37.2) |
Note. Values are n (%).
A set of questions addressed the perceived risk assessment and attitude of orthodontic patients to the COVID-19 infection. More than 95% of them considered infection as dangerous. They believed the orthodontic patient was severely (40.8%) or moderately vulnerable (30.6%) to contracting the disease, but were willing regardless to carry on with their orthodontic treatment during the pandemic (72.4%) (Table III ).
Table III.
Responses to questions on the perceived risk assessment and attitude of orthodontic patients to COVID-19 infections
| Questions asked and responses | Frequency (%) |
|---|---|
| Perception concerning COVID-19 infection | |
| Moderately dangerous | 124 (40.8) |
| Not dangerous at all | 11 (3.6) |
| Very dangerous | 169 (55.6) |
| Perception concerning the vulnerability of orthodontic patients | |
| Moderately vulnerable | 93 (30.6) |
| Not vulnerable | 15 (4.9) |
| Severely vulnerable | 116 (38.2) |
| Slightly vulnerable | 42 (13.8) |
| I don't know | 38 (12.5) |
| Willing to continue orthodontic treatment during the pandemic | |
| No | 84 (27.6) |
| Yes | 220 (72.4) |
| Willing to continue orthodontic treatment after the pandemic | |
| No | 18 (5.9) |
| Yes | 286 (94.1) |
| How do you consider patients role in spreading information as regard COVID-19 | |
| Insignificant | 5 (1.6) |
| Moderately significant | 57 (18.8) |
| Very significant | 242 (79.6) |
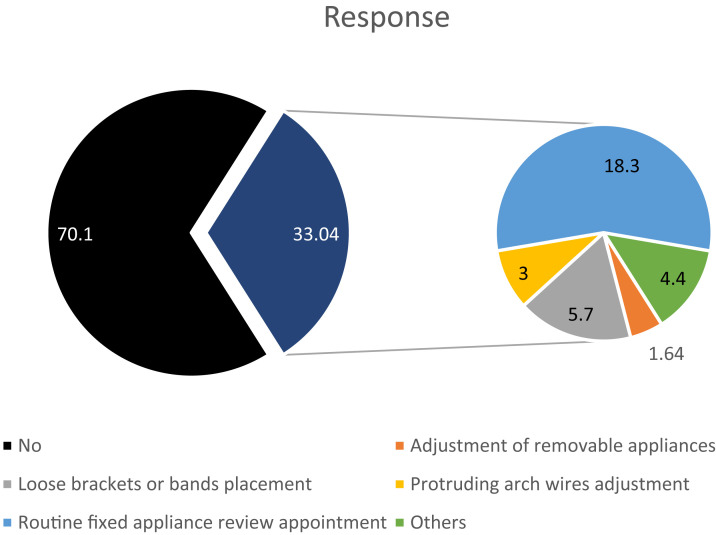
Responses showed that most of them (70.1%) had not been to the orthodontic clinics for appointments since the COVID-19 outbreak. The minority who had visited the clinics had routine fixed appliance review appointments, whereas the others were managed for orthodontic emergencies such as protruding archwire and loose bands or brackets (Fig ). Although the fear of contracting the COVID-19 virus during orthodontic appointments was the immediate concern of most of the respondents (39.8), they expressed worry over missed orthodontic appointments (74%) and increased treatment time (50%) in the near future (Table IV ). The assessment of the effect of the COVID-19 pandemic on the economic, emotional, and social wellbeing of the respondents revealed a negative impact on the financial and emotional domains. Responses from the social domain showed the highest percentage of respondents (48%) saying the pandemic had a positive effect, giving them adequate time to spend with their families (Table V ).
Fig.
Visit and reason for an orthodontic visit during the outbreak.
Table IV.
Effect of the COVID-19 pandemic on patients’ orthodontic appointments
| Questions and responses | Frequency (%) |
|---|---|
| Effect the pandemic had on your orthodontic treatment | |
| Fear of contracting the virus during a routine appointment | 121 (39.8) |
| Missed routine appointment | 83 (27.3) |
| Increase in treatment time | 108 (35.5) |
| Increase in cost of treatment | 26 (8.6) |
| No effect | 19 (6.3) |
| Other | 6 (2.0) |
| The perceived effect the pandemic will have on your orthodontic treatment | |
| Increased cost of treatment | 67 (22.0) |
| Missed routine appointments | 226 (74.3) |
| Increase in treatment time | 153 (50.3) |
| No effect | 11 (3.6) |
| Other | 3 (1.0) |
Table V.
Impact of COVID-19 on the economic, emotional, and social wellbeing of orthodontic patients
| Questions and responses | Frequency (%) |
|---|---|
| Economic impact | |
| Mildly negative | 49 (16.1) |
| Mildly positive | 10 (3.3) |
| Moderately negative | 76 (25) |
| Moderately positive | 10 (3.3) |
| No impact | 30 (9.9) |
| Severely negative | 62 (20.4) |
| Very positive | 8 (2.6) |
| I cannot tell | 59 (19.4) |
| Emotional impact | |
| No effect | 37 (12.2) |
| I feel depressed | 27 (8.9) |
| Happy, I can rest | 36 (11.8) |
| Unhappy, I can't work | 76 (25.0) |
| I can't tell immediately | 66 (21.7) |
| Unhappy, I can't go to school | 70 (23.0) |
| Social impact | |
| No effect | 13 (4.3) |
| Affected relationship with friends negatively | 19 (6.3) |
| Enriched relationship with friends | 30 (9.9) |
| Affected relationship with family negatively | 121 (39.8) |
| Enriched relationship with family | 146 (48.0) |
| Other | 9 (3.0) |
Over 50% of the respondents were unperturbed (31.6%) or neutral (22.7%) toward assessing orthodontic care during the pandemic and willing to undergo further orthodontic treatment in the near future (66.1%) (Table III).
A majority of the respondents believed the patients have a significant role in infection control in the orthodontic practice setting. An assessment of the willingness to carry out precautionary measures to mitigate the spread of the virus in the clinic showed a high acceptance rate among respondents, with hand hygiene, social distancing facemask, and temperature check having the highest acceptance rates (Table VI ). They also exhibited adequate knowledge on the precautionary measures to take if the exposure occurred within the dental clinic setting (Table VI).
Table VI.
Precautionary measures of COVID-19
| Questions asked | Not agreeable (%) | Slightly agreeable (%) | Agreeable (%) | Very agreeable (%) | Total agreement (%) |
|---|---|---|---|---|---|
| Consultation over the phone | 81 (26.6) | 46 (15.1) | 62 (20.4) | 32 (10.5) | 83 (27.3) |
| Wait in car to decongest clinic | 32 (10.5) | 21 (6.9) | 45 (14.8) | 50 (16.4) | 156 (51.3) |
| Social distancing in clinic | 4 (1.3) | 3 (1.0) | 19 (6.3) | 30 (9.9) | 248 (81.6) |
| Temperature screening before entering clinic | 2 (0.7) | 2 (0.7) | 15 (4.9) | 33 (10.9) | 252 (82.9) |
| Asked relevant screening questions | 8 (2.6) | 8 (2.6) | 30 (9.9) | 46 (15.1) | 212 (69.7) |
| Limiting number of child's company | 0 (0.0) | 6 (2.0) | 19 (6.3) | 39 (12.8) | 240 (78.9) |
| Wearing facemasks in clinic | 2 (0.7) | 0 (0.0) | 19 (6.3) | 37 (12.2) | 246 (80.9) |
| Handwashing in the dental clinic | 4 (1.3) | 4 (1.3) | 6 (2.0) | 21 (6.9) | 269 (88.5) |
The majority (79.6 %) of the participants believed that patients play a significant role in spreading information and increasing awareness concerning COVID-19. A high percentage of the respondents (83.9%) reported that they would move far away from a patient who coughs or sneezes beside them in the clinic. Above half of the participants claimed to know what to do if they have unprotected exposure, and the majority said they would go into self-isolation immediately.
Significant associations were observed between educational level and perceived knowledge of COVID-19 pandemic and between age, sex, and duration of treatment with a willingness to continue treatment (Table VII ).
Table VII.
Association between sociodemographic characteristics and willingness to continue orthodontic treatment during the COVID-19 pandemic
| Sociodemographics | Willingness |
P value | |
|---|---|---|---|
| Yes, n (%) | No, n (%) | ||
| Level of education | |||
| Primary | 11 (100) | 0 (0.0) | 0.010 |
| Secondary | 69 (65.7) | 36 (34.3) | |
| Tertiary | 65 (67.7) | 31 (32.3) | |
| Postgraduate | 57 (81.5) | 17 (18.5) | |
| Age, y | |||
| <10 | 6 (60.0) | 4 (40.0) | 0.015 |
| 11-20 | 88 (66.7) | 44 (33.3) | |
| 21-30 | 72 (86.7) | 11 (13.3) | |
| 31-40 | 36 (73.5) | 13 (26.5) | |
| 41-50 | 16 (61.5) | 10 (38.5) | |
| 51-60 | 2 (50.0) | 2 (50.0) | |
| Sex | |||
| Female | 172 (77.8) | 49 (22.2) | 0.001 |
| Male | 48 (57.8) | 35 (42.2) | |
| No. of months in orthodontic treatment | |||
| 1-12 | 103 (84.4) | 19 (15.6) | 0.003 |
| 13-24 | 56 (65.9) | 29 (34.1) | |
| 25-36 | 28 (58.3) | 20 (41.7) | |
| 37-48 | 8 (72.7) | 3 (27.3) | |
| >48 | 25 (65.8) | 13 (34.2) | |
Discussion
The transmission of COVID-19 poses a risk to patients who come in close contact with other infected persons.13 The risk is great among those who work in close contact with patients and vice versa. The approximate distance between the working field and the dentist is 35-40 cm; some orthodontic procedures can be time-consuming, which puts both the patients and the orthodontist at great risk of contracting COVID-19.13
Since declared as a pandemic in March 2020, the COVID-19 infection has had a devastating global effect, leading many countries to declare either a partial or total lockdown in an attempt to curb the virus spread. They encouraged their citizens to stay home, avoid public gatherings, and go out only when necessary while maintaining physical distancing.
Many dental associations9, 10, 11 advised their members to restrict dental care to only emergency and urgent procedures. Although no COVID-19 infection within the dental setting has been reported,15 dentistry, including orthodontics, requires proximity of the patient and dental health care workers,16 increasing risk of COVID-19 transmission within the dental setting.
No universal guidelines or recommendations to orthodontic practice during the pandemic exist. Therefore, this leaves the decision of whether or not to practice at the discretion of individual orthodontists. Orthodontic care spans a duration of approximately 2-3 years with patients making frequent orthodontic appointments every 4-6 weeks,17 thus making this category of dental patients peculiar. Therefore, this necessitated the need to review the COVID-19 situation from the orthodontic patients’ standpoint.
The objectives of this study were to assess orthodontic patients’ knowledge, attitude, and perception of COVID-19 as well as the financial, economic, and social impact of the pandemic.
An overview of the study showed that the majority (92%) of the participants claimed to have a moderate to high knowledge level of COVID-19, which is supported by their high knowledge level of etiology, incubation period, common symptoms, and route of transmission of COVID-19. This finding can be attributed to various means of dissemination of information regarding COVID-19. The subjects attributed sources of information about COVID-19 to predominantly the traditional media-93%, social media-81.7%. Knowledge deficiencies observed, especially in less common symptoms and mode of transmission among respondents, showed the need for further patient education.
A large percentage of the respondents perceived COVID-19 as dangerous (55.6%). This perception may be adduced to the lack of evidence-based definitive treatment for the COVID-19 infection18 as well as the global death rate of over 350,000 because of the COVID-19 pandemic since first reported in December 2019 in Wuhan, China.1 Orthodontists share a similar perception; as a study on the impact of COVID-19 among Nigerian orthodontists showed that the majority of them considered the infection dangerous.14
Most of the participants had not visited the orthodontic clinic since the onset of the pandemic. This result is contrary to the findings of Peloso et al,19 who reported that more than 50% of Brazilian patients attended the dental clinic, predominantly for orthodontic procedures since the pandemic began. Interestingly, most respondents in the current study were willing to continue their treatment during this period. The obvious fear of contracting the virus during orthodontic appointments as evidenced by responses in this study is consistent with findings in previous studies.19 , 20
There was a statistically significant association between age, sex, and willingness to continue treatment during the pandemic, with the females and younger patients more willing to undergo treatment. The reported higher COVID-19 related fatalities among the male sex and older patients1 might have influenced their reluctance in accessing dental care at this time. Similarly, other researchers observed increased willingness to access care by the younger population; however, contrary to our findings, they reported an increased willingness to access care among the males.19 , 20
Routine fixed appliance review, which involves archwire change in most cases, was the most common procedure done during the orthodontic appointment. The relative nonaerosol generating nature of this procedure might have contributed to the willingness of managing orthodontists to go ahead with the procedure at this time.
Evaluating the effect of the pandemic on the respondents, fear of contracting the virus in the dental practice setting was the most common immediate concern, while believing the pandemic will lead to missed appointments in the future. This finding is in tandem with previous studies.19 , 20 This valid concern possibly stems from the fact that many of the patients had missed at least 1 appointment as routine orthodontic appointment interval spans 4-6 months.17 Previous research has associated missed appointments with increased treatment time and cost.21 This is evidenced by the study participants’ inclusion of increased cost as a possible future effect of the pandemic on orthodontic treatment, especially as orthodontic care in the country is not covered by the National Health Insurance Scheme, and most of these orthodontic patients have to pay out of pocket. The increased treatment time may also increase patient burnout with unsatisfactory treatment outcome.21 This may therefore be the reason why subjects with longer treatment duration were more willing to continue treatment despite the pandemic in this study (P = 0.003).
As the COVID-19 pandemic continues without an end in sight, many countries are embracing the “new normal,” putting measures in place to function despite the rising numbers. This finding applies to dental care as some clinics have opened, whereas others are putting measures in place to do so. This is particularly important for the orthodontic patient whose treatment course is about 2 years, and indefinitely postponing treatment may be detrimental. Furthermore, prolonged orthodontic treatment is associated with complications such as tooth decalcification and root resorption, etc.22
Most orthodontic practices see many patients in a single day15 and are known for patient filled waiting areas. This creates a conducive environment for COVID-19 transmission. Furthermore, a good percentage of orthodontic patients are young and usually would be asymptomatic if infected.1 Although transmissibility during the asymptomatic phase remains questionable; caution should be exercised in managing this age group.
The patients' compliance with infection control measures is important to curtail the spread of the infection in the dental clinic setting.20 An evaluation of the patients’ willingness to adopt precautionary measures to prevent COVID-19 spread showed a very high acceptance rate in this study. Hand hygiene, use of facemasks, and social distancing showed the highest acceptance rates. These have been documented as effective measures in preventing COVID-19 infection transmission.1 , 2 , 18 The high acceptance level of these COVID-19 precautionary measures may be attributed to the high level of knowledge on the mode of transmission and prevention of the infection exhibited by the respondents. However, it was observed that over the phone consultation and waiting in the car to decongest the clinic if the need arises had the least acceptance. Telemedicine is important in resolving certain health challenges and prevents unnecessary hospital visits.23 The remote possibility of effectively managing the orthodontic patient via telemedicine may be responsible for its poor acceptance among orthodontic patients. Ensuring efficient appointment scheduling to reduce patient waiting time and avoid congesting the waiting area is recommended at this time, as patients may be unwilling to wait outside the clinic area, as evidenced from responses (Table VI).
Most study participants (79.6%) believed they play a significant role in spreading information and increasing awareness of COVID-19. This result corroborates the findings of a previous study.20 Therefore, it may be necessary to make use of audiovisual or posters in the clinics to improve patient knowledge. The use of fliers may not be used as it may encourage disease spread.
When asked what to do in the event of exposure to a COVID-19 patient, the uncertainty on the required action by respondents showed the need for further education, as exposure in the orthodontic clinic can occur.
The perceived impact of the COVID-19 pandemic on other aspects of the orthodontic patients’ well-being (emotional, economic, and social) was also evaluated. Although negative impacts on the economic and emotional wellbeing were reported among the patients, the highest percentage of respondents said it enriched the family relationship. A previous study reported a negative impact of COVID-19 in about 50% of surveyed orthodontic patients exhibited by either anxiety or fear.20 The obvious lack of income generation because of the lockdown during the study period may have accounted for the negative impact of the pandemic on the income of the orthodontic patients. This lockdown and restricted movement at the time of the survey may have created more time to spend with the family, hence the positive impact in the social domain.
As orthodontic practices consider reopening to meet the needs of the patients, meticulous infection control must be observed. Appointments schedules should be strictly adhered to. All COVID-19 precautionary measures must be made available in the clinic to mitigate virus spread. Continuous training of dental health care workers and patients is recommended.
A limitation of this study is the study design (a cross-sectional study with nonprobability sampling). However, the findings of this study filled a research gap in evaluating the impact of the COVID-19 pandemic on orthodontic patients. Until now, only 1 study has tried to answer the research question, with emphasis on emotional impact. Further studies are therefore recommended for validation of findings and to compare the COVID-19 impact among different orthodontic populations.
Footnotes
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and none were reported.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ajodo.2020.11.030.
Supplementary Text: Study questionnaire impact of coronavirus disease 2019 (COVID-19) pandemic on orthodontic patients
Informed consent:
Do you consent to take part in this study?∗
-
○
Yes
-
○
No
Section 1
Demographic characteristics
-
1.
Age (As of last birthday)∗
□
-
2.Sex∗
-
○Male
-
○Female
-
○
-
3.
Religion: Christianity ( ) Islam ( ) Others ( )
-
4.
Marital status: Single ( ) Married ( ) Divorced ( ) Separated ( ) Widow(er) ( ) Others ( )
-
5.
Level of education: Primary ( ) Secondary ( ) Tertiary ( ) Postgraduate
-
6.Number of months in treatment∗
-
○1-12 months
-
○13-24 months
-
○25-36 months
-
○37-48 months
-
○More than 48 months
-
○
-
7.Facility where you are receiving treatment∗
-
○Private hospital
-
○Government hospital
-
○
-
8.Modality of payment of orthodontic treatment∗
-
○Out of pocket (self)
-
○Health insurance
-
○A combination of both
-
○Others
-
○
-
9.Type of orthodontic treatment you are undergoing∗
-
○Removable appliance
-
○Fixed appliance
-
○Others
-
○
Section 2
Impact of the COVID-19 pandemic on Orthodontic practice
-
10.Have you been to the orthodontist since the outbreak of the COVID-19 pandemic outbreak?∗
-
○Yes
-
○No
-
○
-
11.If yes, what treatment did you receive?∗
-
○Adjustment of a removable appliance
-
○Routine fixed appliance review appointment
-
○Protruding arch-wires adjustment
-
○Loose brackets or bands replacement
-
○Other:
-
○
-
12.What effect has the COVID-19 pandemic HAD on your orthodontic treatment? (You can have multiple entries)∗
-
○Fear that I may contract the virus if I go for my routine Orthodontic appointment
-
○Missed routine appointments
-
○Increase in treatment time
-
○Increase in cost of treatment
-
○No effect
-
○Other:
-
○
-
13.What effect do you think the COVID-19 pandemic will have on your orthodontic treatment? (You can have multiple entries) ∗
-
○Increased cost of treatment
-
○Missed routine appointments
-
○Increase in treatment time
-
○No effect
-
○Other:
-
○
-
14.How would you describe the economic impact of the COVID-19 pandemic on your income/guardian or parent's income? ∗
-
○No impact
-
○Mildly negative
-
○Moderately negative
-
○Severely negative
-
○Mildly positive
-
○Moderately positive
-
○Very positive
-
○
-
15.What effect has the COVID-19 pandemic had on your psychosocial wellbeing? (You can have more than 1 entry) ∗
-
○It has had no effect
-
○I feel depressed
-
○I am happy; it has given me time to rest
-
○I feel unhappy, not being able to work or earn an income
-
○I cannot immediately tell
-
○
-
16.How would you describe the impact of the COVID-19 pandemic on your social life? (You can have more than 1 entry)∗
-
○It has had no effect on my social life.
-
○Has affected my relationship with my friends negatively
-
○Has enriched my relationship with my friends
-
○Has affected my relationship with my family negatively
-
○Has enriched my relationship with my family
-
○Other:
-
○
-
○
□
-
17.Do you think the pandemic is likely to affect your willingness to undergo further Orthodontic treatment in the near future?∗
-
○Yes
-
○No
-
○
-
18.Are you worried about receiving Orthodontic treatment during this period as a result of the COVID-19 pandemic?
-
○Yes …………….
-
○No……………….
-
○Indifferent……….
-
○
-
19.
If yes, to 16 above, what is your major worry?………………………………………….
Section 3
Knowledge of COVID-19
-
20.How would you rate your knowledge level on COVID-19?∗
-
○Low
-
○Moderate
-
○High
-
○
-
21.What kind of infection is COVID-19?∗
-
○Viral
-
○Bacteria
-
○Fungal
-
○Other:
-
○
-
○
□
-
22.What is the average incubation period of COVID-19?∗
-
○1-3 days
-
○1-7 days
-
○1-10 days
-
○1-14 days
-
○
-
23.What are the symptoms of COVID-19? (Tick all that apply)∗
-
○May be asymptomatic
-
○Fever
-
○Cough
-
○Sore throat
-
○Shortness of breath
-
○Diarrhea
-
○Vomiting
-
○Running nose
-
○Red eyes
-
○Skin rash
-
○Joint/muscle pain
-
○Loss of taste
-
○Loss of smell
-
○
-
24.How can COVID-19 be transmitted? (Tick all that apply)∗
-
○Coughing and sneezing
-
○Handshaking
-
○Touching contaminated surfaces
-
○Talking
-
○I don't know
-
○
-
25.How can COVID-19 transmission be prevented in the orthodontic clinic? (Tick all that apply)∗
-
○Regular handwashing with soap and water
-
○Use of alcohol-based hand rub
-
○Routine disinfection of contaminated surfaces
-
○Use of personal protective clothing by all dental staff members
-
○Use of facemasks by known or suspected patients
-
○Keeping known or suspected patients in well-ventilated rooms
-
○
-
26.What were your sources of information about the COVID-19? (Select all that apply)
-
○Media (newspaper, television, radio, etc.)
-
○Social network (Facebook, Twitter, blog, etc.)
-
○Friends or family members
-
○Orthodontist, medical doctors, or routinely visited physicians
-
○Academic training courses
-
○
Section 4
Risk perception and attitude toward COVID-19 as an orthodontic patient.
-
27.What is your perception concerning COVID-19 infection?∗
-
○Very dangerous
-
○Moderately dangerous
-
○Not dangerous at all
-
○
-
28.What is your perception concerning the vulnerability of orthodontic patients to COVID-19 infection?∗
-
○Orthodontic patients are not vulnerable
-
○Orthodontic patients are slightly vulnerable
-
○Orthodontic patients are moderately vulnerable
-
○Orthodontic patients are severely vulnerable
-
○I don't know
-
○
-
29.Will you be willing to continue your orthodontic treatment DURING the period of the COVID-19 pandemic?∗
-
○Yes
-
○No
-
○
-
30.Will you be willing to continue orthodontic treatment AFTER the COVID-19 pandemic?∗
-
○Yes
-
○No
-
○
Some of the precautionary measures to prevent the spread of the coronavirus in the dental clinic will require your cooperation and involvement. Kindly state how agreeable you are to performing these: (Answer all that apply)∗ (1, not agreeable; 2, slightly agreeable; 3, agreeable; 4, very agreeable; 5, total agreement)
-
31.
Carrying out some of your consult/treatment over the phone ( )
-
32.
Waiting in your car to decongest the clinic waiting room ( )
-
33.
Social distancing in the clinic waiting room ( )
-
34.
Having temperature screening in the clinic waiting room ( )
-
35.
Being asked relevant questions to screen all patients for COVID-19 ( )
-
36.
Limiting the number of people that accompany a child/adult to the clinic ( )
-
37.
Wearing facemasks while in clinic the waiting room ( )
-
38.
Washing your hands/use of hand sanitizers once in the dental clinic ( )
-
39.How do you consider the patients' role in spreading information and increasing awareness concerning COVID-19?∗
-
○Very significant
-
○Moderately significant
-
○Insignificant
-
○
-
40.If a patient sneezes or coughs persistently beside you in the clinic, how will you react? ∗
-
○I will move far away from the patient
-
○I will advise the patient to go to the hospital
-
○I will advise the dental staff to send the patient home
-
○I will leave the clinic without receiving treatment that day
-
○I'm not sure of what to do
-
○
-
41.Do you know what to do if you have unprotected exposure to a patient or dental staff with known or suspected COVID-19? ∗
-
○Yes
-
○No
-
○I have an idea, but I'm not sure.
-
○
-
42.What will you do if you have unprotected exposure to a patient with known or suspected COVID-19? (Tick all that apply) ∗
-
○Go to the hospital immediately for testing
-
○Self-isolate immediately
-
○Contact the concerned authorities if you have symptoms after days of self-isolation
-
○I do not know what to do
-
○Other:
-
○
References
- 1.World Health Organization Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at:
- 2.Worldometers Coronavirus update (live) https://www.worldometers.info/coronavirus/ Available at:
- 3.Nigeria Centre for Disease Control Index of/themes/common/files/sitreps. https://ncdc.gov.ng/themes/common/files/sitreps/ Available at:
- 4.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khader Y., Al Nsour M., Al-Batayneh O.B., Saadeh R., Bashier H., Alfaqih M. Dentists’ awareness, perception, and attitude regarding COVID-19 and infection control: cross-sectional study among Jordanian dentists. JMIR Public Health Surveill. 2020;6:e18798. doi: 10.2196/18798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gamio L. The workers who face the greatest coronavirus risk. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html?action=click&module=Top+Stories&pgtype=Homepage Available at:
- 9.Nigerian Dental Association About us. https://nigdentalasso.org/about-us/ Available at:
- 10.American Dental Association ADA statement on COVID-19. https://www.ada.org/en/publications/ada-news/2020-archive/march/ada-recommending-dentists-postpone-elective-procedures Available at:
- 11.British Dental Association Live updates: Coronavirus and dentistry. https://bda.org/advice/Coronavirus/Pages/latest-updates.aspx Available at:
- 12.Caprioglio A., Pizzetti G.B., Zecca P.A., Fastuca R., Maino G., Nanda R. Management of orthodontic emergencies during 2019-NCOV. Prog Orthod. 2020;21:10. doi: 10.1186/s40510-020-00310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pîrvu C., Pătraşcu I., Pîrvu D., Ionescu C. The dentist’s operating posture - ergonomic aspects. J Med Life. 2014;7:177–182. [PMC free article] [PubMed] [Google Scholar]
- 14.Isiekwe I.G., Adeyemi T.E., Aikins E.A., Umeh O.D. Perceived impact of the COVID-19 pandemic on orthodontic practice by orthodontists and orthodontic residents in Nigeria. J World Fed Orthod. 2020;9:123–128. doi: 10.1016/j.ejwf.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turkistani K.A. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: a review. Am J Orthod Dentofacial Orthop. 2020;158:175–181. doi: 10.1016/j.ajodo.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leggat P.A., Kedjarune U., Smith D.R. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45:611–621. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]
- 17.Long H., Pyakurel U., Wang Y., Liao L., Zhou Y., Lai W. Interventions for accelerating orthodontic tooth movement: a systematic review. Angle Orthod. 2013;83:164–171. doi: 10.2319/031512-224.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. World Health Organization. https://apps.who.int/iris/handle/10665/331446 Available at: License: CC BY-NC-SA 3.0 IGO.
- 19.Peloso R.M., Pini N.I.P., Sundfeld Neto D., Mori A.A., Oliveira R.C.G., Valarelli F.P. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Braz Oral Res. 2020;34:e84. doi: 10.1590/1807-3107bor-2020.vol34.0084. [DOI] [PubMed] [Google Scholar]
- 20.Cotrin P., Peloso R.M., Oliveira R.C., de Oliveira R.C.G., Pini N.I.P., Valarelli F.P. Impact of coronavirus pandemic in appointments and anxiety/concerns of patients regarding orthodontic treatment. Orthod Craniofac Res. 2020;23:455–461. doi: 10.1111/ocr.12395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beckwith F.R., Ackerman R.J., Jr., Cobb C.M., Tira D.E. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;115:439–447. doi: 10.1016/s0889-5406(99)70265-9. [DOI] [PubMed] [Google Scholar]
- 22.Uribe F., Soumya P., Allareddy V., Nanda R. Patients’, parents’, and orthodontists’ perceptions of the need for and costs of additional procedures to reduce treatment time. Am J Orthod Dentofacial Orthop. 2014;145(4 Suppl):S65–73. doi: 10.1016/j.ajodo.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 23.Kravitz N.D., Burris B., Butler D., Dabney C.W. Teledentistry, do-it-yourself orthodontics, and remote treatment monitoring. J Clin Orthod. 2016;50:718–726. [PubMed] [Google Scholar]