We have read with great interests the article by Jin and colleagues entitled “Laparoscopic pancreaticoduodenectomy for pancreatic cancer: a hope or hype?” recently published in HepatoBiliary Surgery and Nutrition (1). They came out with a conclusion that Laparoscopic pancreaticoduodenectomy (LPD) could be a safe and feasible approach for the patients with pancreatic cancers even at their advanced stage, and may also obtain comparable long-term oncologic outcomes. We really agree with this conclusion. We would here also like to report one of our experiences of an emergency LPD case of the treatment of pancreatic head cancer induced acute gastrointestinal hemorrhage, which could be the first case to the best of our knowledge based on literature research.
A 75-year-old man presented with hematochezia for 15 hours, with total blood loss of approximately 1,500 mL. He was admitted to the emergency department for gastrointestinal hemorrhage and hemorrhagic shock. He had mild jaundice and scleral icterus, and a hemoglobin level of 60 g/L. Enhanced computed tomography (CT) and CT angiogram (Figure 1A) showed contrast extravasation and a 1.8 cm × 2.8 cm irregular heterogeneously enhancing space-occupying lesion at the descending segment of the duodenum, close to the pancreatic head. Celiac trunk + superior mesenteric artery digital subtraction angiography failed to demonstrate contrast extravasation. Emergency gastroscopy showed duodenal bulbar deformity with stenosis distally, preventing the endoscope’s passage.
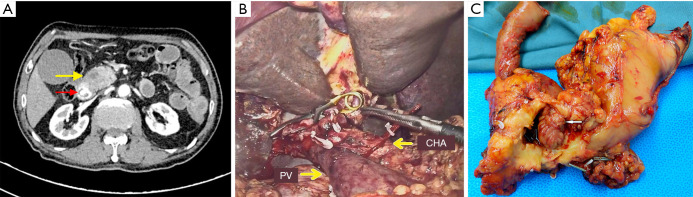
Figure 1.
Preoperative imaging, intraoperative photo, and surgical specimen. (A) Preoperative enhanced computed tomography and computed tomography angiogram. Red arrow: Contrast media extravasation is seen in the duodenum. Yellow arrow: A space-occupying lesion is present at the descending segment of the duodenum that is close to the pancreatic head. (B) Surgical field after specimen resection. (C) Surgical specimen. After surgery, the surgical specimen was incised. It was found that the pancreatic head tumor had invaded the wall of the descending segment of the duodenum (white arrow). PV, portal vein; CHA, common hepatic artery.
Based on these findings, acute hemorrhage due to periampullary carcinoma was highly suspected. The emergency LPD was conducted (Figure 1B,C). During the 260-minute surgery, intraoperative bleeding was 600 mL. Eight units of erythrocytes and 600 mL of plasma were transfused. The patient’s hemoglobin improved to 102 g/L postoperatively, and no blood transfusions were needed. The postoperative pancreatic fistula grade was B-level. The patient was discharged on Day 21 after surgery. Histopathology showed pancreatic ductal adenocarcinoma (T2N1M0).
The postoperative mortality of emergency pancreaticoduodenectomy (EPD) for non-traumatic disease, which is a high-risk surgery, is higher than that of elective pancreaticoduodenectomy (PD), with a morbidity of 80% or more (2). In patients with acute gastrointestinal hemorrhage secondary to pancreatic head cancer (PHC), EPD is the only available life-saving method when vascular intervention and gastroscopy cannot effectively stop hemorrhage. Since 2000, a total of 56 cases of non-traumatic EPD have been reported in English, over half of which (29, 51.8%) were due to hemorrhage. Thus, this case was consistent with the indications for EPD.
In recent years, laparoscopic and robotic pancreatic surgery, including LPD, has increasingly become a more common surgical approach in major medical centers with experienced surgeons. It has been found that in terms of perioperative complications, LPD in experienced hands was not significantly different from traditional open pancreaticoduodenectomy (OPD) (3,4), but its suitability for PHC has been in dispute. In particular, it is still controversial regarding whether LPD and OPD are similar in terms of tumor-related prognosis. In our center, over 400 cases of pancreatic surgery were performed annually, of which more than 100 were LPD. Moreover, our experience indicated that in large centers with a high volume of surgery similar to ours, LPD could be safe and feasible for PHC that has not invaded major blood vessels and might achieve an oncological outcome equal to or even better than that of OPD. Recently, a large-scale meta-analysis study drew similar conclusions (5).
The safety and feasibility of LPD in treating periampullary tumors have been gradually appreciated in the field (6), but those of emergency LPD have not been reported yet. When treating this emergency case, we explored the possibility of emergency LPD after careful consideration and succeeded. To date, the patient, who is undergoing postoperative adjuvant chemotherapy, has been followed up for three months and has shown no signs of tumor recurrence or metastasis.
Emergency LPD could be feasible and safe in emergency cases with surgical indications in a high-volume hospital that employs surgeons with considerable experience in laparoscopic techniques, and we believe that an increasing number of patients will benefit from this technique.
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Provenance and Peer Review: This article was commissioned by the editorial office, HepatoBiliary Surgery and Nutrition. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/hbsn-20-613). The authors have no conflicts of interest to declare.
References
- 1.Jin W, Cheung TTT, Mou Y. Laparoscopic pancreaticoduodenectomy for pancreatic cancer: a hope or hype? Hepatobiliary Surg Nutr 2020;9:388-90. 10.21037/hbsn-20-356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsai CY, Lai BR, Wang SY, et al. The impact of preoperative etiology on emergent pancreaticoduodenectomy for non-traumatic patients. World J Emerg Surg 2017;12:21. 10.1186/s13017-017-0133-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nickel F, Haney CM, Kowalewski KF, et al. Laparoscopic Versus Open Pancreaticoduodenectomy: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg 2020;271:54-66. 10.1097/SLA.0000000000003309 [DOI] [PubMed] [Google Scholar]
- 4.van Hilst J, de Rooij T, van den Boezem PB, et al. Laparoscopic pancreatoduodenectomy with open or laparoscopic reconstruction during the learning curve: a multicenter propensity score matched study. HPB (Oxford) 2019;21:857-64. 10.1016/j.hpb.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 5.Sun R, Yu J, Zhang Y, et al. Perioperative and oncological outcomes following minimally invasive versus open pancreaticoduodenectomy for pancreatic duct adenocarcinoma. Surg Endosc 2020. [Epub ahead of print]. 10.1007/s00464-020-07641-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asbun HJ, Moekotte AL, Vissers FL, et al. The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg 2020;271:1-14. 10.1097/SLA.0000000000003590 [DOI] [PubMed] [Google Scholar]