Abstract
A 44-year-old woman with known trichorhinophalangeal syndrome presented with an unheralded out of hospital cardiac arrest. Transthoracic echocardiography showed severe left ventricular systolic dysfunction with an ejection fraction <25% and cardiac MRI confirmed a diagnosis of congenital non-ischaemic dilated cardiomyopathy. The case highlights a very rare syndrome, it is previously unknown association with dilated cardiomyopathy and the possible benefit of cardiac screening for patients with known trichorhinophalangeal syndrome.
Keywords: cardiovascular medicine, arrhythmias, heart failure, resuscitation, genetic screening / counselling
Background
This case details the first ever reported case of dilated cardiomyopathy (DCM) associated with the rare syndrome trichorhinophalangeal syndrome (TRPS). Cases of this type are incredibly rare, and therefore, this case plays a important role in developing the evidence base further. It also touches on screening for such cases and how it might prevent mortality by sudden cardiac death.
Case presentation
A 44-year-old Caucasian woman with a background of TRPS type I and mild asthma was brought to the emergency department with an out of hospital cardiac arrest (OOHCA). She had no family history of cardiac disease, was a non-smoker and was otherwise healthy. She did not take any regular medications. She was witnessed to collapse at a bus stop and a bystander confirmed cardiac arrest secondary to ventricular fibrillation (VF). Cardiopulmonary resuscitation (CPR) was commenced, and she was given a total of five shocks before return of spontaneous circulation. She received epinephrine, amiodarone and was intubated at the scene by the ambulance crew. On arrival to the emergency department, she was cold and clammy, with a heart rate of 90 beats per minute and a normal blood pressure. Clinical examination was normal.
Investigations
Blood tests including full blood count, renal function, liver function and troponin were all normal. An initial ECG showed sinus rhythm with ventricular ectopics and T-wave inversion of leads V3–V6 (figure 1). Bedside transthoracic echocardiogram (TTE) was performed immediately which showed mildly dilated left ventricular size (5.7 cm), severe left ventricular dysfunction with an ejection fraction (EF) of <25% and severely hypokinetic walls. She was urgently transferred to the catheter lab and underwent coronary angiography which revealed unobstructed coronary arteries. On the intensive care unit, she remained on vasopressor support for 1 day and cardiac monitoring showed episodes of non-sustained ventricular tachycardia (VT) (figure 2), which was treated with an amiodarone infusion. Following stabilisation and successful extubation, she was stepped down to the coronary care unit. A subsequent TTE, however, still demonstrated severely reduced EF and she was started on optimal heart failure medications. She proceeded to having a cardiac MRI, in order to ascertain any structural heart abnormality that could explain the cardiac arrest. Cardiac MRI showed moderate to severe impairment of left ventricular systolic function with a moderately dilated left ventricle (end-diastolic volume 236 mL) in keeping with a diagnosis of non-ischaemic DCM (figure 3), likely congenital in nature.
Figure 1.
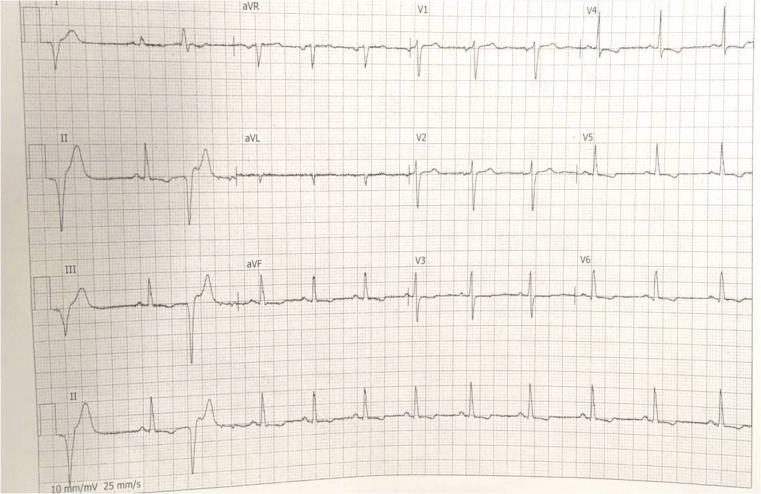
ECG showing normal sinus rhythm with ventricular ectopics, T-wave inversion noted in leads V3–V6 taken on arrival to the emergency department.
Figure 2.
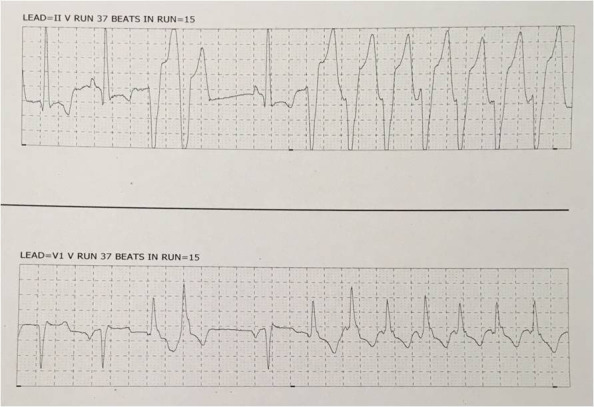
Cardiac monitoring showing runs of broad complex tachycardia while on the intensive care unit.
Figure 3.
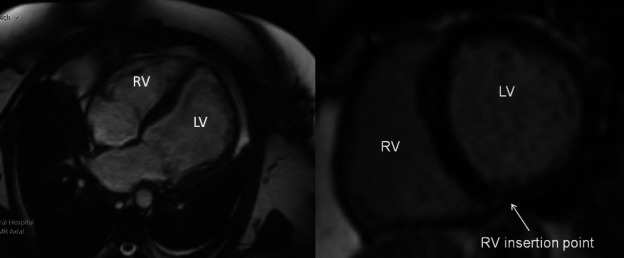
Cardiac MR parasternal and short axis images. Images show moderate to severe left ventricular systolic dysfunction (ejection fraction 35%) with moderate left ventricular dilatation with an EDV of 236 mL (normal range 90–171 mL). Right ventricular systolic function is normal with no right ventricular dilatation. There is mild left atrial enlargement (left atrial area 29 cm2, right atrial area 20 cm2). There is hyperenhancement at the inferior RV insertion point. Appearances are suggestive of a non-ischaemic dilated cardiomyopathy. EDV, end-diastolic volume; LV left ventricle; RV right ventricle.
Treatment
She was given optimal heart failure medications as per national guidelines including ramipril, bisoprolol and spironolactone. The doses of all of these were up titrated over the course of her admission in coronary care unit, monitoring for blood pressure and heart rate changes. She had a subcutaneous implantable cardiac defibrillator (ICD) implanted and was discharged home a few days later.
Outcome and follow-up
A follow-up was done in cardiology and heart failure clinic within 4 weeks of discharge. Her recovery had been remarkable; her only complaints were of short-term memory loss and chest discomfort secondary to CPR which had been treated with analgesia. She had a repeat TTE a few months later which showed that her cardiac function had improved, with her EF now reporting at 40%. Further pacing checks did not reveal further ventricular arrthymias.
Discussion
OOHCA has a very poor prognosis with 95% of victims dying before reaching hospital.1 VT or VF are thought to be the most common cause for OOHCA, accounting for approximately three-quarters of all cases.2 Among young adults cardiac arrests are most commonly due to an undiagnosed congenital or hereditary condition such as a coronary artery anomaly or an inherited cardiomyopathy.3 To the best of our knowledge, there are no case reports in the literature in relation to TRPS with a DCM, and our patient may be the first documented case.
TRPS is a rare autosomal dominant genetic syndrome that is characterised by skeletal, ectodermal and craniofacial abnormalities.4 There are three subtypes of TRPS which have all been associated with TRPS1 gene mutations on chromosome 8 and have a wide clinical spectrum.5 There are, however, clinical features that are highly characteristic and common to all three subtypes; a long flat philtrum, thin upper lips with laterally sparse eyebrows, slow-growing scalp hair, bulbous nose tip and protruding ears. Individuals are likely to have delayed bone age and slowed growth leading to short stature.
In those individuals with mild symptoms, a diagnosis may be easily missed or go unreported. Therefore, it is difficult to determine the true frequency of this disorder in the general population and at present there is no diagnostic criteria.4 5 Diagnosis primarily consists of a combination of extensive history taking, clinical examination and genetic testing.
TRPS has been found to be associated with various congenital cardiovascular defects. One article states that cardiac defects are present in 15% of affected individuals.6 These defects include patent ductus arteriosus, bicuspid aortic valve, mitral regurgitation, persistent foramen ovale and aortic stenosis. Individual case reports have shown an association of TRPS with mitral valve disease and mitral valve prolapse.7 8 All three subtypes of TRPS have been associated with cardiac manifestations, however, this is the first case showing an association of TRPS with a cardiomyopathy.
Screening of patients with all subtypes of TRPS and also their relatives, in particular first-degree relatives, using ECG, TTE and cardiac MRI may offer risk protection against serious tachyarrhythmias and cardiac arrest. An early diagnosis, at a less advanced disease stage and the use of effective evidence-based pharmacological treatment such as ACE inhibitors and beta-blockers and non-pharmacological therapies such as an ICDs and cardiac resynchronisation would contribute to the improved prognosis of patients with TRPS and DCM.9 10
Learning points.
Out of hospital cardiac arrests, often due to ventricular tachycardia or ventricular fibrillation, have a very poor prognosis.
Hereditary conditions such as cardiomyopathies are a common cause of unheralded cardiac arrests.
Trichorhinophalangeal syndrome is a rare genetic disorder, which has previously not been associated with a dilated cardiomyopathy.
Screening should be offered to patients with trichorhinophalangeal syndrome, irrespective of their subtype to aid an early diagnosis of cardiomyopathy.
Acknowledgments
We thank the patient for their permission in writing up this case.
Footnotes
Twitter: @manasinha
Contributors: All authors were directly involved in the patient’s care and contributed to the creation of this article. All authors meet the International Committee of Medical Journal Editors Recommendations for the Conduct, Reporting, Editing and Publication of Scholarly Work in Medical Journals (ICMJE) criteria for authorship and GS is the lead and corresponding author. GS conceived the idea for the report. GS drafted the article. All authors were involved in the final approval of the version published. All authors are accountable for the article. EB drafted the article. All authors were involved in the final approval of the version published. All authors are accountable for the article. MS conceived the idea for the report. MS drafted the article. All authors were involved in the final approval of the version published. All authors are accountable for the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Perkins GD, Lockey AS, de Belder MA. Community resuscitation group. National initiatives to improve outcomes from out-of-hospital cardiac arrest in England. Emerg Med J 2016;33:448–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katritsis DG, Gersh BJ, Camm AJ, et al. A clinical perspective on sudden cardiac death. Arrhythm Electrophysiol Rev 2016;5:177–82. 10.15420/aer.2016:11:2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyer L, Stubbs B, Fahrenbruch C, et al. Incidence, causes, and survival trends from Cardiovascular-Related sudden cardiac arrest in children and young adults 0 to 35 years of age. Circulation 2012;126:1363–72. 10.1161/CIRCULATIONAHA.111.076810 [DOI] [PubMed] [Google Scholar]
- 4.Lüdecke HJ, Schaper J, Meinecke P, et al. Genotypic and phenotypic spectrum in tricho-rhino-phalangeal syndrome types I and III. Am J Hum Genet 2001;68:81–91. 10.1086/316926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maas SM, Shaw AC, Bikker H, et al. Phenotype and genotype in 103 patients with tricho-rhino-phalangeal syndrome. Eur J Med Genet 2015;58:279–92. 10.1016/j.ejmg.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 6.Weaver DD, Cohen MM, Smith DW. The tricho-rhino-phalangeal syndrome. J Med Genet 1974;11:312–4. 10.1136/jmg.11.3.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robert SC, Cooper JP. A patient with tricho-rhino-phalangeal syndrome and mitral valve disease. Int J Cardiol 2007;114:E129–30. 10.1016/j.ijcard.2006.08.011 [DOI] [PubMed] [Google Scholar]
- 8.Tasic V, Gucev Z, Ristoska-Bojkovska N, et al. Tricho-Rhino-Phalangeal syndrome in a 13-year-old girl with chronic renal failure and severe growth retardation. Ren Fail 2014;36:619–22. 10.3109/0886022X.2014.882237 [DOI] [PubMed] [Google Scholar]
- 9.Moretti M, Merlo M, Barbati G, et al. Prognostic impact of familial screening in dilated cardiomyopathy. Eur J Heart Fail 2010;12:922–7. 10.1093/eurjhf/hfq093 [DOI] [PubMed] [Google Scholar]
- 10.Aleksova A, Sabbadini G, Merlo M, et al. Natural history of dilated cardiomyopathy: from asymptomatic left ventricular dysfunction to heart failure – a subgroup analysis from the Trieste cardiomyopathy registry. J Cardiovasc Med 2009;10:699–705. 10.2459/JCM.0b013e32832bba35 [DOI] [PubMed] [Google Scholar]


