Abstract
Comorbidities affecting physical function increase with advanced-age and rural living. This study investigated the degree of benefit from resistance training (RT) in older adults based on age (50–89 years), location (urban vs. rural), and program duration (10 vs. 8-weeks). 260 participants completed pre- and post-program dynamic and static tasks and flexibility testing. Paired and independent t-tests and one-way and repeated measures ANOVAs were used to test group improvements. All ages improved performance (all p ≤ .002) but those in their 50’s improved flexibility the most and those in their 60’s improved 30STS more and tandem balance less than those in their 80’s. Both rural and urban participants improved in all areas (all p ≤ .002), but rural participants reported greater improvements in tandem balance. Both 10- and 8-week classes improved performance (all p ≤ .001), but 8-week participants improved dynamic tasks and tandem balance more. RT can reduce functional discrepancies in older adults and rural residents.
Keywords: physical activity, aging, falls, quality of life
Older adults who remain physically active can combat age-related declines in musculoskeletal health and physical function (Fragala et al., 2019). Unfortunately, according to the Administration of Community Living’s (ACL, 2019) Profile of Older Americans only 21% of adults aged 55 to 64 years are meeting weekly national guidelines (Riebe et al., 2018) for aerobic and resistance training (RT) exercises. This percentage continues to decline with increasing age as only 11% of those who are 75+ years are meeting national weekly guidelines (ACL, 2019). Furthermore, older adults have many unique barriers to engaging in regular exercise, such as transportation, financial cost, and physical limitations. Current data suggests these barriers are greater as adults age into their 70’s and 80’s and may be exercise-type specific as a greater proportion of older adults engage in aerobic exercises than RT (ACL, 2019). Age-related discrepancies in RT frequency is in-part due to most RT programs being created for and tested on older adults under the age of 70 years (Ball et al., 2013). This discrepancy is significant because deficits in muscle strength, gait, and balance are the most prominent predisposing risk factors for falls and loss of independence and increase in severity as older adults age into their 70’s and 80’s (Ganz & Latham, 2020) but RT improves these parameters to a greater extent than aerobic training (Baker et al., 2020; Villareal et al., 2017).
Most muscle-strengthening and RT programs that are developed specifically for older adults’ have been shown to improve muscle capacity and bone integrity (Ball et al., 2013; Foster & Armstrong, 2018; Giangregorio et al., 2014; Guizelini et al., 2018), cardiometabolic risk factors (Beavers et al., 2018), self-confidence (Dionigi, 2007), and sleep quality (Baker et al., 2020; Yang et al., 2012). As healthy independent aging relies heavily on these factors, the most successful RT interventions must target as many of these factors as possible, simultaneously. Unfortunately, most of these programs have not been tested in rural areas which are defined as populations <50,000 (Ratcliffe et al., 2016), and are not offered outside metropolitan areas. This is of particular concern as rural older adults report more falls (Zhang et al., 2019), greater rates of physical inactivity and obesity (Cohen et al., 2018), and elevated risk for the top five leading causes of death (Centers for Disease Control and Prevention [CDC], 2017) compared to their urban neighbors. RT programs must address this geography-related discrepancy by increasing access and testing for program efficacy in rural areas.
Ideal RT program duration is debated, but in general, longer durations often result in greater magnitudes of musculoskeletal improvements (Fragala et al., 2019); however, program progression is a key factor to consider. Modeled after RT programs such as Growing Stronger (Seguin et al., 2017), Fit and Strong (Hughes et al., 2004), Geri-Fit (Goble et al., 2017), and the StrongWomen program (Seguin et al., 2008) the Stay Strong Stay Healthy (SSSH) RT program has historically been offered as a 10-week or 8-week program in urban areas. The 10-week SSSH program did not utilize a standard progression of RT volume but still was shown to improve older adults’ muscle strength, flexibility, and static balance (Ball et al., 2013). The newer 8-week progressive program has also shown to improve older adults’ muscle strength, flexibility, and dynamic balance (Baker et al., 2020), but to-date the vast majority of RT research, SSSH included, has neglected older adults who reside outside of urban areas further widening the access-gap for rural older adults.
This study aimed to assess if age, geographical location, or program duration influenced the degree of improvement in dynamic postural change, static balance with and without additional challenges, and lower-body flexibility after SSSH participation. We hypothesized that younger older adults and urban residents would perform better and report greater magnitudes of improvement than participants 70+ years or who lived in rural areas. Additionally, we hypothesized that both 10- and 8-week programs would equally improve functional performance in older adults.
Materials and Methods
Participants
Retrospective access to deidentified SSSH program data was approved by the University of Missouri Institutional Review Board (IRB # 2031903). Data extraction for the 10- and 8-week SSSH programs included 159 and 258 participants, respectively. 10-week participants were included in the analysis if they completed both pre and post functional assessments and had less than 10% missing data, resulting in 130 participants being included. The dataset for the 8-week program was larger allowing for matching of 130 participants based on geographical location (urban and rural counties). Due to insufficient sample sizes, adults aged 40 to 49 years and from 90 to 99 years were not included in the age analysis (total n = 25). In total, 232 individuals (50–59 years n = 26, 60–69 years n = 82, 70–79 years n = 84, 80–89 years n = 40) were included in the age analysis, 255 individuals were included in the population analysis (urban n = 133, rural n = 122), and 260 individuals (10-week n = 130; 8-week n = 130) were included in the duration analysis. The total sample was aged from 47 to 96 years old, was nearly 85% female, and 51% reported living in urban areas with a population of greater than 50,000 residents (Ratcliffe et al., 2016).
SSSH Programming
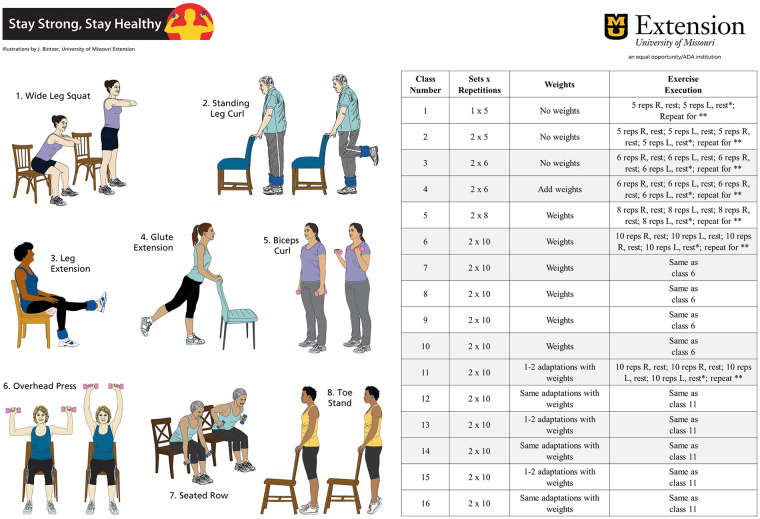
Before 2016, all SSSH programs were 10 weeks in duration and did not incorporate structured progression of RT exercise volume. The program then transitioned to 8 weeks of structured progressive resistance training. 10-week (Ball et al., 2013) and 8-week (Baker et al., 2020) SSSH programming have been described elsewhere, but in summary the program meets in-person two times per week for 60 minutes, with each session beginning with a warm-up and ending with a cool down. The warm-up period lasts nine minutes and includes marching, walking, side-steps, squats, and dynamic and static stretching of the major muscle groups. Next, four standing exercises and four seated exercises are performed using a 2:4 second tempo. Standing exercises include: wide leg squat, leg curls, toe stand and side leg raise for the 10-week classes or the glute extension for the 8-week classes. Seated exercises include: biceps curl, overhead press, bent-over seated row, and knee extension (Figure 1). All classes ended with a 5-minute cool down period including light stretching and breathing exercises. All instructors have completed formal training from the SSSH program and follow the progression chart (Figure 1) and either have or are working toward a Master’s of Science degree in Exercise Science or a related field.
Figure 1.
All eight exercises used throughout the 8-week SSSH classes are on the left. The progression chart used during the 8-week SSSH classes is on the right.
Functional Assessments
All participants completed pre and post intervention functional assessments that fall into three categories, dynamic postural change, static balance with and without additional challenges, and lower body flexibility. The dynamic postural change tasks included a 30-second sit-to-stand task (30STS) and an 8 foot timed-up-and-go task (TUG) (Baker et al., 2020). The 30STS is reported as the number of full chair stands a participant completes in 30 seconds, is attempted once, and is a test of lower body strength and endurance, dynamic balance, and coordination. The TUG is reported as the time in seconds it takes for a participant to rise from a chair, walk around a marker 8 feet away and return to the seated position, is attempted once, and is used as an overall dynamic assessment of balance, gait speed, and coordination. Both of these dynamic tasks have been validated and have strong predictive capabilities for fall risk in older adults (Kahraman et al., 2020; Rose et al., 2002). The five static balance tasks included tandem and single leg stances with and without additional challenge: (1) tandem without challenge; (2) tandem with eyes closed (EC); (3) tandem with eyes closed and with a head turn (EC + HT); (4) single leg stance without challenge; (5) single leg stance with EC. Each stance was scored according to the number of seconds the participant could maintain the stance without using a support for up to 10 seconds. Static balance tests have long been used as a proxy for fall risk (CDC, 2018; Dominguez, 2020) but dual task tasks have been shown to be stronger predictors of fall risk (Commandeur et al., 2018). The current study incorporated both single- and dual-task static balance tests. The seated sit and reach (SnR) test was used for lower body flexibility testing (Baker et al., 2020). SnR was measured once for each leg and averaged for a mean lower body flexibility score in inches. Each SSSH instructor has been trained on the correct methodology for collecting these measures and collected both the pre and post intervention measures for their respective classes. Past research from this research group shows the interclass coefficient ranges from 0.948 to 0.967 over separate days of testing for these measures (Baker et al., 2020).
Statistical Analysis
All statistical procedures were performed using IBM SPSS (v26, Armonk, New York) and significance was set at alpha = 0.05. All data are reported as unadjusted means ± standard deviations (SD) in tables or unadjusted means and standard errors (SE) in figures. Repeated measures ANOVA (RMANOVA) were used to analyze potential group × time interactions and when significant interaction models were found they were further decomposed using paired t-tests for within group or independent t-tests for between groups. Absolute magnitudes of change were calculated for each measure and compared between the age groups using a one-way analysis of variance (ANOVA) with a Bonferroni post hoc and between the duration and population groups using independent t-tests. A summary of improvements using the whole group were assessed using paired t-tests with a Bonferroni correction. Fewer than five of those in their 80’s attempted the tandem with eyes closed and head turn or the single leg with eyes closed tasks. Because of this low sample size, they were not included in the age analysis and are marked as N/A in the tables.
Results
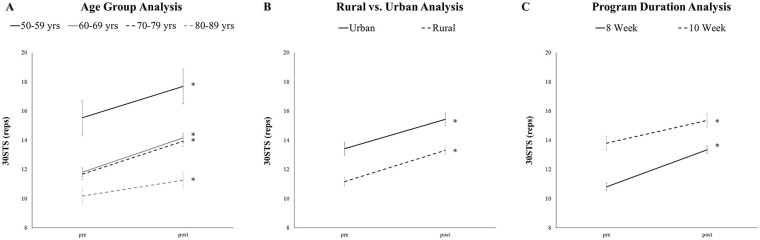
When assessing if the pre and post intervention functional scores and magnitude of improvements would be different between age groups we found significant (group × time) interactions for the 30STS, tandem stance without challenge, and SnR (all p ≤ .030; Table 1). Those in their 50’s had greater 30STS performance than all other groups and those in their 60’s and 70’s performed better than those in their 80’s (all post hoc p ≤ .015, Table 1, Figure 2—panel A). After post hoc analysis the only group difference for tandem balance without challenge and SnR was greater performance for those in their 60’s compared to those in their 80’s (both post hoc p ≤ .014). After post hoc analysis, those in their 60’s reported a greater absolute improvement in the 30STS but less of an improvement in their tandem balance without challenge compared to those in their 80’s (both post hoc p ≤ .027). Additionally, those in their 50’s improved their SnR distance more than those in the 70’s and 80’s (both post hoc p ≤ .018).
Table 1.
Comparison of Age Groups for the Interaction Effects and Absolute Changes—Mean (SD).
| Measures | 50–59 years | 60–69 years | 70–79 years | 80–89 years | Interaction sig. (p) | Time sig. (p) | Group sig. (p) |
|---|---|---|---|---|---|---|---|
| Pre 30STS (reps) | 15.5 (6.1) | 11.8 (2.7) | 11.7 (3.4) | 10.2 (3.5) | .030* | <.001* | <.001* |
| Post 30STS (reps) | 17.7 (5.6) | 14.2 (3.1)† ‡ | 13.9 (3.8)† ‡ | 11.3 (3.6)† | |||
| Abs ∆ 30STS (reps) | 2.2 (2.9) | 2.3 (2.4) | 2.2 (2.2) | 1.1 (1.5)• | |||
| Pre TUG (seconds) | 6.2 (3.5) | 6.8 (2.4) | 7.1 (2.1) | 9.1 (3.4) | .651 | <.001* | <.001* |
| Post TUG (seconds) | 5.3 (2.9) | 5.6 (1.6) | 6.0 (1.4) | 8.2 (3.1) | |||
| Abs ∆ TUG (seconds) | −0.9 (1.2) | −1.2 (1.3) | −1.1 (1.1) | −0.9 (1.7) | |||
| Pre tandem (seconds) | 9.6 (2.0) | 9.8 (0.8) | 9.0 (2.6) | 8.0 (3.7) | .016* | .002* | .003* |
| Post tandem (seconds) | 9.6 (2.0) | 9.9 (0.7)‡ | 9.6 (1.4) | 9.4 (1.8) | |||
| Abs ∆ tandem (seconds) | 0.0 (0.0) | 0.0 (1.6) | 0.6 (2.3) | 1.4 (3.8)• | |||
| Pre tandem + EC (seconds) | 8.3 (2.9) | 5.8 (4.2) | 5.4 (4.1) | 4.2 (4.3) | .851 | .001* | .002* |
| Post tandem + EC (seconds) | 9.2 (1.8) | 7.6 (3.4) | 6.7 (3.8) | 6.0 (4.0) | |||
| Abs ∆ tandem + EC (seconds) | 0.1 (2.8) | 1.8 (4.4) | 1.3 (5.0) | 1.8 (3.1) | |||
| Pre tandem + EC + HT (seconds) | 5.1 (4.0) | 3.5 (3.8) | 4.6 (4.4) | N/A | .212 | .001* | .044* |
| Post tandem + EC + HT (seconds) | 8.8 (1.7) | 6.1 (4.0) | 5.2 (4.1) | N/A | |||
| Abs ∆ tandem + EC + HT (seconds) | 3.7 (4.1) | 2.6 (5.2) | 0.7 (6.1) | N/A | |||
| Pre single leg (seconds) | 9.4 (2.2) | 7.8 (3.6) | 7.3 (3.6) | 4.5 (4.1) | .076 | <.001* | <.001* |
| Post single leg (seconds) | 9.5 (2.1) | 9.0 (2.2) | 8.2 (2.9) | 6.6 (3.7) | |||
| Abs ∆ single leg (seconds) | 0.0 (0.2) | 1.3 (3.0) | 1.0 (3.2) | 2.0 (0.8) | |||
| Pre single leg + EC (seconds) | 2.5 (3.1) | 2.6 (2.7) | 2.9 (2.7) | N/A | .705 | <.001* | .907 |
| Post single leg + EC (seconds) | 6.1 (4.1) | 5.4 (3.7) | 4.8 (2.8) | N/A | |||
| Abs ∆ single leg + EC (seconds) | 4.2 (6.4) | 3.4 (4.0) | 2.1 (3.8) | 1.0 (0.0) | |||
| Pre sit-and-reach (inches) | −0.5 (3.4) | 0.7 (2.8) | 0.4 (3.4) | −0.8 (3.2) | .010* | <.001* | .024* |
| Post sit-and-reach (inches) | 1.3 (3.1) | 1.4 (3.1)‡ | 0.8 (3.4) | −0.7 (3.1) | |||
| Abs ∆ sit-and-reach (inches) | 1.7 (2.8) | 0.7 (1.8) | 0.3 (1.9) • | 0.1 (2.7) • |
Note. 30STS = 30 second sit-to-stand; TUG = timed up-and-go; EC = eyes closed; HT = head turn; Abs. ∆ = absolute change.
Sig.: Significance set at p ≤ .05. †Significantly different from 50 to 59 years age group after post hoc. ‡Significantly different from 80 to 89 years age group after post hoc. •Significantly different absolute magnitude of change.
Figure 2.
Significant 30STS improvements over time for the age groups (panel A), rural versus urban (panel B), and duration groups (panel C).
*Indicates a significant time effect, p ≤ .05.
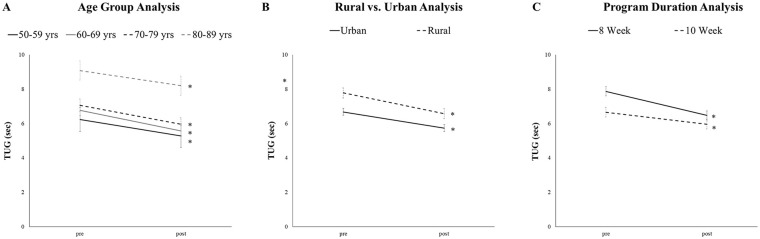
When assessing if the pre and post intervention functional scores and magnitude of improvements would be different between those who resided in rural areas compared to their urban neighbors we found significant (group × time) interaction for the tandem stance without challenge (p = .009, Table 2). Post hoc analysis shows that only rural participants significantly improved tandem scores (post hoc p < .001). Significant group effects were found for rural participants who reported reduced pre and post 30STS, TUG, tandem with eyes closed, and single legged stance values than their rural neighbors (all p ≤ .047, Figures 2 and 3—panel B). When comparing the absolute change in functional performance scores between geography groups tandem balance without challenge improved to a significantly greater extent in rural participants compared to urban participants (p = .028). Both groups improved all other measures to a similar extent (all p ≥ .059).
Table 2.
Comparison of Rural and Urban SSSH Classes for the Interaction Effects and Absolute Changes—mean (SD).
| Measures | Urban SSSH | Rural SSSH | Interaction sig. (p) | Time sig. (p) | Group sig. (p) |
|---|---|---|---|---|---|
| Pre 30STS (reps) | 134. (5.0) | 11.2 (3.2) | .434 | <.001* | <.001* |
| Post 30STS (reps) | 15.4 (5.1) | 13.3 (3.7) | |||
| Abs ∆ 30STS (reps) | 1.9 (2.3) | 2.1 (2.3) | |||
| Pre TUG (seconds) | 6.7 (2.2) | 7.8 (3.2) | .059 | <.001* | .003* |
| Post TUG (seconds) | 5.7 (1.8) | 6.6 (2.7) | |||
| Abs ∆ TUG (seconds) | −0.9 (1.1) | −1.2 (1.5) | |||
| Pre tandem (seconds) | 9.5 (1.8) | 8.8 (2.9) | .009* | .001* | .060 |
| Post tandem (seconds) | 9.7 (1.5) | 9.6 (1.5)† | |||
| Abs ∆ tandem (seconds) | 0.1 (1.8) | 0.8 (2.9)• | |||
| Pre tandem + EC (seconds) | 6.5 (4.0) | 5.5 (4.3) | .902 | <.001* | .047* |
| Post tandem + EC (seconds) | 8.0 (3.2) | 7.0 (3.7) | |||
| Abs ∆ tandem + EC (seconds) | 1.5 (4.3) | 1.5 (4.5) | |||
| Pre tandem + EC + HT (seconds) | 4.9 (4.3) | 4.7 (4.4) | .667 | <.001* | .984 |
| Post tandem + EC + HT (seconds) | 6.8 (3.6) | 7.0 (4.2) | |||
| Abs ∆ tandem + EC + HT (seconds) | 1.9 (4.4) | 2.4 (6.1) | |||
| Pre single leg (seconds) | 8.0 (3.4) | 6.9 (4.0) | .175 | <.001* | .008* |
| Post single leg (seconds) | 8.8 (2.5) | 8.0 (3.2) | |||
| Abs ∆ single leg (seconds) | 0.7 (2.7) | 1.3 (3.2) | |||
| Pre single leg + EC (seconds) | 2.5 (2.4) | 3.5 (3.4) | .234 | .002* | .891 |
| Post single leg + EC (seconds) | 6.0 (3.5) | 5.1 (3.7) | |||
| Abs ∆ single leg + EC (seconds) | 3.5 (4.6) | 1.6 (5.0) | |||
| Pre sit-and-reach (inches) | 0.5 (3.3) | −0.1 (3.2) | .275 | <.001* | .056 |
| Post sit-and-reach (inches) | 1.2 (3.2) | 0.3 (3.4) | |||
| Abs ∆ sit-and-reach (inches) | 0.7 (2.1) | 0.4 (2.2) |
Note. 30STS = 30-second sit-to-stand; TUG = timed up-and-go; EC = eyes closed; HT = head turn; Abs. ∆ = absolute change.
Sig.: Significance set at p ≤ .05. †Significantly different from pre within group. ‡Significantly different from urban pre or post. •Significantly different absolute magnitude of change from urban.
Figure 3.
Significant TUG improvements over time for the age groups (panel A), rural versus urban (panel B), and duration groups (panel C).
*Indicates a significant time effect, p ≤ .05.
When assessing if the pre and post intervention functional scores and magnitude of improvements would be different between the 10-week SSSH program and the progressive 8-week SSSH program we found significant (group × time) interactions for 30STS, TUG, and tandem stance without challenge (all p ≤ .02, Table 3, Figures 2 and 3—panel C). Both groups significantly improved 30STS over time but pre and post measures were lower in the 8-week group compared to the 10-week group (all post hoc p < .001). Both groups significantly improved TUG over time but only pre TUG measures were higher in the 8-week group compared to the 10-week group (all post hoc p ≤ .002). Only the 8-week group improved pre tandem without challenge times after post hoc analysis (p < .001). 30STS, TUG, and tandem balance improved to a greater extent in the progressive 8-week SSSH program (all p ≤ .011) but all other measures improved to a similar extent (all p ≥ .222).
Table 3.
Comparison of 8- and 10-Week Programs for the Interaction Effects and Absolute Changes—Mean (SD).
| Measures | 8 week SSSH | 10 week SSSH | Interaction sig. (p) | Time sig. (p) | Group sig. (p) |
|---|---|---|---|---|---|
| Pre 30STS (reps) | 10.8 (2.9)‡ | 13.8 (5.1) | .001* | <.001* | <.001* |
| Post 30STS (reps) | 13.4 (3.6)† ‡ | 15.4 (5.3)† | |||
| Abs ∆ 30STS (reps) | 2.5 (2.2) | 1.6 (2.3)• | |||
| Pre TUG (seconds) | 7.9 (3.0)‡ | 6.7 (2.8) | <.001* | <.001* | <.001* |
| Post TUG (seconds) | 6.5 (2.3)† | 6.0 (2.6)† | |||
| Abs ∆ TUG (seconds) | −1.4 (1.5) | −0.7 (1.1)• | |||
| Pre tandem (seconds) | 8.9 (2.7) | 9.5 (2.1) | .020* | .001* | .320 |
| Post tandem (seconds) | 9.7 (1.4)† | 9.6 (1.6) | |||
| Abs ∆ tandem (seconds) | 0.8 (2.5) | 0.1 (2.2)• | |||
| Pre tandem + EC (seconds) | 5.4 (4.1) | 6.7 (4.2) | .323 | <.001* | .001* |
| Post tandem + EC (seconds) | 6.6 (3.7) | 8.6 (3.0) | |||
| Abs ∆ tandem + EC (seconds) | 1.2 (4.6) | 1.9 (4.2) | |||
| Pre tandem + EC + HT (seconds) | 4.2 (3.7) | 5.3 (4.7) | .220 | <.001* | .007* |
| Post tandem + EC + HT (seconds) | 5.5 (3.9) | 8.0 (3.3) | |||
| Abs ∆ tandem + EC + HT (seconds) | 1.4 (5.6) | 2.7 (4.5) | |||
| Pre single leg (seconds) | 6.9 (3.9) | 8.0 (3.4) | .254 | <.001* | .025* |
| Post single leg (seconds) | 8.1 (2.8) | 8.7 (2.8) | |||
| Abs ∆ single leg (seconds) | 1.2 (2.7) | 0.7 (3.3) | |||
| Pre single leg + EC (seconds) | 1.6 (2.6) | 2.6 (3.4) | .501 | .001 | .030* |
| Post single leg + EC (seconds) | 4.0 (3.1) | 6.2 (3.6) | |||
| Abs ∆ single leg + EC (seconds) | 2.4 (4.0) | 3.6 (5.5) | |||
| Pre sit-and-reach (inches) | −0.1 (3.3) | 0.6 (3.2) | .238 | <.001* | .045* |
| Post sit-and-reach (inches) | 0.3 (3.3) | 0.8 (3.3) | |||
| Abs ∆ sit-and-reach (inches) | 0.4 (1.8) | 0.7 (2.4) |
Note. 30STS = 30 second sit-to-stand; TUG = timed up-and-go; EC = eyes closed; HT = head turn; Abs. ∆ = absolute change.
Sig.: Significance set at p ≤ .05. †Significantly different from pre within group. ‡Significantly different from 10 week. •Significantly different absolute magnitude of change from 8 week.
When all 260 participants are combined in a summary analysis, functional performance improved for all measures (Table 4). Participants averaged a nearly two repetition increase in their 30STS performance and over a 1 second reduction in their TUG time (both p < .001). All three tandem and both single legged stance performance significantly improved by an average of 1.7 seconds (all p ≤ .001), and SnR distance significantly improved as participants could reach an additional 0.6″ (p < .001).
Table 4.
Evaluation of the Whole Group’s Improvements After SSSH Participation—mean (SD).
| Measures | Sample size | Pre SSSH | Post SSSH | Sig. (p) |
|---|---|---|---|---|
| Dynamic postural change tasks | ||||
| 30STS (reps) | 251 | 12.3 (4.4) | 14.4 (4.6) | <.001* |
| TUG (seconds) | 228 | 7.3 (3.0) | 6.2 (2.5) | <.001* |
| Static balance tasks | ||||
| Tandem (seconds) | 238 | 9.2 (24) | 9.7 (1.5) | <.001* |
| Tandem + EC (seconds) | 159 | 6.1 (4.2) | 7.6 (3.5) | <.001* |
| Tandem + EC + HT (seconds) | 87 | 4.8 (4.3) | 6.9 (3.8) | <.001* |
| Single leg (seconds) | 221 | 7.4 (3.8) | 8.4 (2.9) | <.001* |
| Single leg + EC (seconds) | 42 | 2.3 (3.2) | 5.6 (3.5) | <.001* |
| Flexibility tests | ||||
| Sit and reach (inches) | 258 | 0.2 (3.3) | 0.8 (3.3) | <.001* |
Note. 30STS = 30 second sit-to-stand; TUG = timed up-and-go; EC = eyes closed; HT = head turn.
Sig.: Significance after Bonferroni correction p ≤ .00625.
Discussion
This study demonstrates that participation in the SSSH RT program can improve dynamic postural change and static balance tasks that are critical for maintaining independence and mitigating fall risk. Most importantly, RT improved physical outcomes for high-risk rural older adults and those of advanced age suggesting the SSSH RT program may be well-suited for large-scale implementation.
Participation in the SSSH RT program improved key physical attributes that are necessary for reducing fall risk. For instance, the CDC’s (2018) STEADI initiative (Stopping Elderly Accidences, Deaths and Injuries) publishes normative values for the 30STS task based on age. According to these data, those in this study who were in their 60’s, 70’s, and 80’s had pre-SSSH 30STS scores indicative of increased fall risk. However, after SSSH engagement participants in those age groups had 30STS scores greater than the national average suggesting a shift from “at risk for falls” to “normal” classification. Furthermore, according to Rose et al. (2002) 8 feet TUG scores of greater than 8.5 seconds are highly predictive of falls in community-living older adults suggesting participants from the current study in their 80’s were at increased risk for falls or classified as “fallers”. After SSSH participation those in their 80’s improved their TUG times by nearly a second moving them to the “nonfallers” group. These data suggest SSSH participation effectively combats advanced age-related declines resulting in reduced fall risk by improving lower body dynamic task performance.
The degree of instability during standing balance tasks have been strongly associated with fall risk and mortality in older adults (Crenshaw et al., 2018; Dominguez, 2020). The tandem task with eyes open is a commonly used measure of postural sway and is often easy for many older adults to complete. In the current study, over 90% of participants were able to maintain the stance for the full 10 seconds. However, recently many static balance tasks have been combined with additional challenges such as closing participant’s eyes, incorporating a head turn (Singh et al., 2017), or adding a cognitive challenge during the motor task (Van Bloemendaal et al., 2019). These dual-task challenges provide greater discriminatory power between fallers and non-fallers (Commandeur et al., 2018) and in the current study all dual-task balance test scores significantly improved for all groups. Springer et al. (2007) suggest normative values for single legged stance with eyes closed should be between 8.3 and 1.9 seconds for those in their 50’s, 60’s, 70’s, and 80’s. According to these recommendations, participants in the current study were below average prior to SSSH participation but those in their 60’s, 70’s, and 80’s improved to above average levels after SSSH participation. These findings demonstrate SSSH participation can improve static balance further reducing fall risk specifically for those at greatest risk, the 70 and 80+ years age group.
Many significant health discrepancies exist between urban and rural older adults. For instance, rural older adults report reduced physical activity and increased obesity rates (Cohen et al., 2018) compared to their urban neighbors. Many of these discrepancies are in part caused by a lack of safe spaces to exercise and fewer consistent exercise program offerings in rural communities. In this study, rural participants who were able to participate in locally offered SSSH programs reported significantly reduced pre- and post-SSSH dynamic and static balance task performance compared to their urban counterparts, supporting documented increased fall risk associated with rural living (Zhang et al., 2019). However, it is important to note that despite beginning and ending the study with reduced performance values, those in the rural setting improved their tandem task performance to a greater extent and all other measures to the same extent as urban participants. These findings partially support our first hypothesis and fully support those of Smith et al. (2012) who noted rural Texans also reported significantly reduced pre- and post-intervention measures but increased performance to the same or a greater extent than their city-dwelling neighbors. Future RT programs targeting older adults must ensure their programs can benefit both urban and rural participants and may need to consider unique access barriers that exist for successful program implementation in rural communities. For instance, geography related barriers for rural participants may be circumnavigated using virtual delivery, however, these modes of delivery will need to be further tested for efficacy and safe implementation.
Exercise progression is a key principle for positive musculoskeletal adaptations for both young and older adults (Fragala et al., 2019). Despite a 20% reduction in program duration, the introduction of standardized progression and exercise modification by formerly trained SSSH instructors in the 8-week SSSH program has yielded equal and/or superior results compared to the longer 10-week program, refuting our second hypothesis. The most important difference between the two duration groups was the magnitude of improvement in the dynamic tasks, 30STS and TUG. As noted previously these tasks are strongly associated with fall risk and 8-week SSSH participation allowed individuals to move from an at-risk for falls classification to a low risk for falls classification. These data suggest the progression scheme utilized for the 8-week SSSH program is sufficient to improve older adults’ static and dynamic balance, resulting positive fall risk reductions. Additionally, the 8-week program can improve these key aspects of independence in both rural older adults and those of advanced age. It is key that future programs implemented in both urban and rural areas targeting older adults utilize similar exercise progression schemes to maximize benefit to the participant in the shortest amount of time.
Limitations for the current study include small sample sizes for some groups, dual-task balance test sample attrition, and lack of longitudinal follow-up. The number of individuals within the 90+ age group were too small to consider, reducing our ability to make inferences regarding the efficacy of SSSH in the potentially most frail age group. Additionally, the more difficult dual-task balance tests such as tandem with eyes closed and a head turn or single legged stance with eyes closed were rarely attempted by those in their 80’s and 90’s suggesting these test batteries are not appropriate for these age groups and other more suitable tasks are needed. Lastly, results from this study demonstrate significant improvements in measures strongly associated with falls; however, no direct measure of falls were recorded and no long-term follow-up was conducted. Our current endeavors now include 3-, 6-, and 12-month follow-ups to address this limitation.
Conclusion
In conclusion, the SSSH program improves both dynamic and static balance performance that are important aspects of fall risk reduction. These improvements were similar across age groups and geographical location suggesting the program is well designed for mass implementation.
Acknowledgments
Authors would like to thank the 10,000+ participants of the SSSH program, regional specialists/instructors, and all program coordinators for making past, current, and future SSSH programs a key resource for healthy and independent aging.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: University of Missouri Extension and Engagement Office.
IRB Protocol Institution and Number: The University of Missouri Institutional Review Board has approved this work and assigned the IRB # 2031903.
ORCID iDs: Breanne S. Baker  https://orcid.org/0000-0002-0098-149X
https://orcid.org/0000-0002-0098-149X
Kelsey J. Weitzel  https://orcid.org/0000-0003-3608-6996
https://orcid.org/0000-0003-3608-6996
Data Accessibility Statement: If interested in the data used in this publication please contact the corresponding author for details.
References
- Adminstration for Community Living. (2019). Profile of older Americans. https://acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans
- Baker B. S., Weitzel K. J., Royse L. A., Miller K., Guess T. M., Ball S. D., Duren D. L. (2020). Efficacy of an 8-week resistance training program in Older adults: A randomized controlled trial. Journal of Aging and Physical Activity. Advance online publication. 10.1123/japa.2020-0078 [DOI] [PubMed] [Google Scholar]
- Ball S. D., Gammon R., Kelly P. J., Cheng A., Chertoff K., Kaume L., Abreu E. L., Brotto M. (2013). Outcomes of stay strong, stay healthy in community settings. Journal of Aging and Health, 25(8), 1388–1397. 10.1177/0898264313507318 [DOI] [PubMed] [Google Scholar]
- Beavers K. M., Walkup M. P., Weaver A. A., Lenchik L., Kritchevsky S. B., Nicklas B. J, Ambrosius W. T., Stitzel J. D., Register T. C., Shapses S. A., Marsh A. P., Rejeski W. J. (2018). Effect of exercise modality during weight loss on bone health in older adults with obesity and cardiovascular disease or metabolic syndrome: A randomized controlled trial. Journal of Bone and Mineral Research, 33(12), 2140–2149. 10.1002/jbmr.3555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Rural Americans at higher risk of death from five leading causes. https://www.cdc.gov/media/releases/2017/p0112-rural-death-risk.html
- Centers for Disease Control and Prevention. (2018). Stopping elderly accidents, deaths, and injuries (STEADI). 2017. https://www.cdc.gov/steadi/materials.html#
- Cohen S. A., Greaney M. L., Sabik N. J. (2018). Assessment of dietary patterns, physical activity and obesity from a national survey: Rural-urban health disparities in older adults. PLoS One, 13(12), e0208268. 10.1371/journal.pone.0208268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commandeur D., Klimstra M., MacDonald S., Inouye K., Cox M., Chan D., Hundza S. (2018). Difference scores between single-task and dual-task gait measures are better than clinical measures for detection of fall-risk in community-dwelling older adults. Gait and Posture, 66, 155–159. 10.1016/j.gaitpost.2018.08.020 [DOI] [PubMed] [Google Scholar]
- Crenshaw J. R., Bernhardt K. A., Atkinson E. J., Khosla S., Kaufman K. R., Amin S. (2018). The relationships between compensatory stepping thresholds and measures of gait, standing postural control, strength, and balance confidence in older women. Gait and Posture, 65, 74–80. 10.1016/j.gaitpost.2018.06.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionigi R. (2007). Resistance training and older adults’ beliefs about psychological benefits: The importance of self-efficacy and social interaction. Journal of Sport and Exercise Psychology, 29(6), 723–746. 10.1123/jsep.29.6.723 [DOI] [PubMed] [Google Scholar]
- Dominguez L., Jr. (2020). Postural control and perturbation response in aging populations: Fall risk implications. Journal of Neurophysiology, 124, 1309–1311. 10.1152/jn.00767.2019 [DOI] [PubMed] [Google Scholar]
- Foster C., Armstrong M. (2018). What types of physical activities are effective in developing muscle and bone strength and balance. Journal of Frailty, Sarcopenia and Falls, 3(2), 58–65. 10.22540/JFSF-03-058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fragala M. S., Cadore E. L., Dorgo S., Izquierdo M., Kraemer W. J., Peterson M. D., Ryan E. D. (2019). Resistance training for older adults: Position statement from the national strength and conditioning association. The Journal of Strength and Conditioning Research, 33(8), 2019–2052. 10.1519/JSC.0000000000003230 [DOI] [PubMed] [Google Scholar]
- Ganz D. A., Latham N. K. (2020). Prevention of falls in community-dwelling older adults. New England Journal of Medicine, 382(8), 734–743. 10.1056/NEJMcp1903252 [DOI] [PubMed] [Google Scholar]
- Giangregorio L., Papaioannou A., Macintyre N., Ashe M., Heinonen A., Shipp K., Wark J. S., Keller H., Jain R. J., Laprade J., Cheung A. M. (2014). Too fit to fracture: Exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporosis International, 25(3), 821–835. 10.1007/s00198-013-2523-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goble D. J., Hearn M. C., Baweja H. S. (2017). Combination of BTrackS and Geri-Fit as a targeted approach for assessing and reducing the postural sway of older adults with high fall risk. Clinical Interventions in Aging, 12, 351–357. https://doi.org/10.2147%2FCIA.S131047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guizelini P. C., de Aguiar R. A., Denadai B. S., Caputo F., Greco C. C. (2018). Effect of resistance training on muscle strength and rate of force development in healthy older adults: A systematic review and meta-analysis. Experimental Gerontology, 102, 51–58. 10.1016/j.exger.2017.11.020 [DOI] [PubMed] [Google Scholar]
- Hughes S. L., Seymour R. B., Campbell R., Pollak N., Huber G., Sharma L. (2004). Impact of the fit and strong intervention on older adults with osteoarthritis. The Gerontologist, 44(2), 217–228. 10.1093/geront/44.2.217 [DOI] [PubMed] [Google Scholar]
- Kahraman B. O., Ozsoy I., Akdeniz B., Ozpelit E., Sevinc C., Acar S., Savci S. (2020). Test-retest reliability and validity of the timed up and go test and 30-second sit to stand test in patients with pulmonary hypertension. International Journal of Cardiology, 304, 159–163. 10.1016/j.ijcard.2020.01.028 [DOI] [PubMed] [Google Scholar]
- Ratcliffe M., Burd C., Holder K., Fields A. (2016). Defining rural at the US Census Bureau. American Community Survey and Geography Brief, 1(8). [Google Scholar]
- Riebe D., Ehrman J. K., Liguori G., Magal M.(2018). American College of Sports Medicine’s guidelines for exercise testing and prescription. Wolters Kluwer. [Google Scholar]
- Rose D. J., Jones C. J., Lucchese N. (2002). Predicting the probability of falls in community-residing older adults using the 8-foot up-and-go: A new measure of functional mobility. Journal of Aging and Physical Activity, 10(4), 466–475. 10.1123/japa.10.4.466 [DOI] [Google Scholar]
- Seguin R. A., Economos C. D., Nelson M. E., Hyatt R., Palombo R., Reed P. N. (2008). Peer reviewed: Design and national dissemination of the Strongwomen Community Strength Training Program. Preventing Chronic Disease, 5(1), A25. [PMC free article] [PubMed] [Google Scholar]
- Seguin R. A., Folta S. C., Nelson M. E., Hanson K. L., LaCroix A. Z. (2017). Long-term body weight maintenance among StrongWomen–Healthy Hearts program participants. Journal of Environmental and Public Health, 2017, 1–6. 10.1155/2017/4372048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H., Sanders O., Waller S. M., Bair W.-N., Beamer B., Creath R. A., Rogers M. W. (2017). Relationship between head-turn gait speed and lateral balance function in community-dwelling older adults. Archives of Physical Medicine and Rehabilitation, 98(10), 1955–1961. 10.1016/j.apmr.2017.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M. L., Ahn S. N., Sharkey J. R., Horel S., Mier N., Ory M. G. (2012). Successful falls prevention programming for older adults in Texas: Rural–urban variations. Journal of Applied Gerontology, 31(1), 3–27. https://doi.org/10.1177%2F0733464810378407 [Google Scholar]
- Springer B. A., Marin R., Cyhan T., Roberts H., Gill N. W. (2007). Normative values for the unipedal stance test with eyes open and closed. Journal of Geriatric Physical Therapy, 30(1), 8–15. [DOI] [PubMed] [Google Scholar]
- Van Bloemendaal M., Bout W., Bus S. A., Nollet F., Geurts A. C., Beelen A. (2019). Validity and reproducibility of the Functional Gait Assessment in persons after stroke. Clinical Rehabilitation, 33(1), 94–103. https://doi.org/10.1177%2F0269215518791000 [DOI] [PubMed] [Google Scholar]
- Villareal D. T., Aguirre L., Gurney A. B., Waters D. L., Sinacore D. R., Colombo E., Armamentro-Villarea R., Qualls C. (2017). Aerobic or resistance exercise, or both, in dieting obese older adults. New England Journal of Medicine, 376(20), 1943–1955. 10.1056/NEJMoa1616338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang P. Y., Ho K. H., Chen H. C., Chien M. Y. (2012). Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. Journal of Physiotherapy, 58(3), 157–163. 10.1016/S1836-9553(12)70106-6 [DOI] [PubMed] [Google Scholar]
- Zhang L., Ding Z., Qiu L., Li A. (2019). Falls and risk factors of falls for urban and rural community-dwelling older adults in China. BMC Geriatrics, 19(1), 1–17. 10.1186/s12877-019-1391-9 [DOI] [PMC free article] [PubMed] [Google Scholar]