Highlights
What do we already know about this topic?
Traumatic appendicitis is often mis or underdiagnosed due to its extreme rarity.
How does your research contribute to the field?
My research highlights the causal link between trauma and acute appendicitis especially in pediatric population and demonstrates that displacement of appendicolith remains the frequent mechanism.
What are your research’s implications toward theory, practice, or policy?
Although rare, traumatic appendicitis requires a high index of clinical suspicion and should be considered in the setting of right lower quadrant pain following blunt abdominal trauma.
Introduction
Acute bappendicitis (AP) is one of the most common surgical emergencies encountered in clinical practice. It results typically from obstruction of the appendiceal lumen. While children are more vulnerable to direct trauma,
Traumatic appendicitis has been reported as a very rare condition especially seen in pediatric population. Herein; we report a case of acute appendicitis following blunt abdominal trauma (BAT) in an 8-year-old boy, we discussed the link between trauma and appendicitis and we reviewed the literature on this matter.
Case Report
An 8-year-old boy caucasian presented to our pediatric emergency department with a progressive abdominal pain which began 24 hours after direct trauma to the right lower quadrant of his abdomen. While playing soccer with his friends, the boy fell over a boulder and sustained injury in the lower abdomen. At the following day, the pain increased in severity becoming worsened by movement. He was accompanied by nausea, vomiting and anorexia.
The boy had negative past medical and surgical history.
On examination, the patient was conscious and hemodynamically stable with a pulse of 120/min, a blood pressure of 110/80 mm Hg, a respiratory rate of 17, a temperature of 38.5°C, and a weight of 24 Kg. On palpation, abdomen was not distended, moderately tender with considerable tenderness on the lower quadrant without peritoneal signs. The rest of clinical examination was unremarkable. Blood examination revealed 12.0 g/dl hemoglobin, 1100 white blood cells/mm3. Renal function tests and chest radiography demonstrated normal findings.
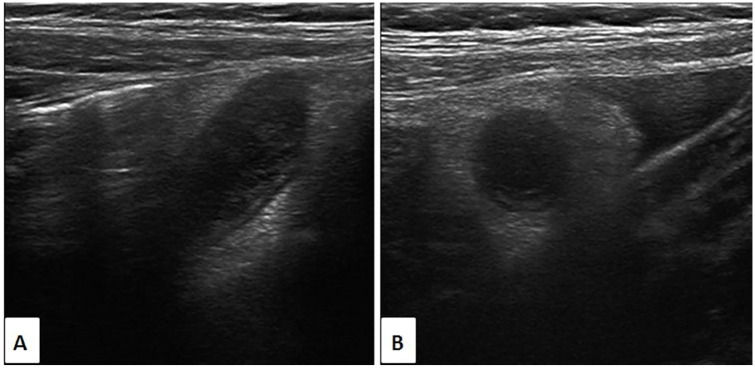
Abdominopelvic ultrasonography (US) showed aperistaltic and non-compressible tubular structure in the right lower quadrant of the abdomen with an ill-defined wall and a dilated lumen measuring 10 mm, surrounded by fat infiltration and accompanied with a small amount of free fluid suggesting an appendicitis (Figure 1). Solid organs were intact.
Figure 1.
Ultrasonographic images in longitudinal (A) and orthogonal (B) views show a tubular structure in the right lower quadrant with an ill-defined wall and a dilated lumen, surrounded by fat infiltration and accompanied with a small amount of free fluid.
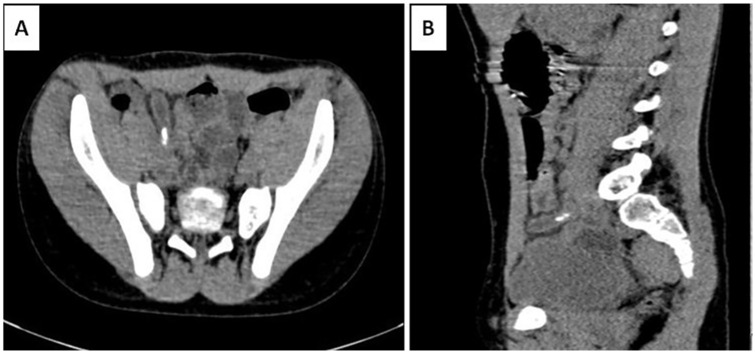
For further investigation, an intravenous contrast-enhanced computed tomography (CT) scan was performed demonstrating appendicitis with impacted appendicolith into the lumen (Figure 2). No abnormal abdominal solid organ or abdominal wall injury were observed.
Figure 2.
Axial (A) and coronal (B) contrast enhanced CT image of the abdomen through the lower quadrants demonstrate appendicitis with impacted appendicolith into the appendiceal lumen.
Through a Mc Burney’s incision, an appendectomy was performed. The appendix was grossly hyperemic and edematous (Figure 3). Histopathology confirmed diagnosis of acute appendicitis. Our patient made an excellent recovery, and he was discharged from the hospital in stable condition 3 days later.
Figure 3.

Intra operative image showing the inflamed appendicitis.
Discussion
Traumatic appendicitis is a very rare condition firstly described by J. Murphy in 1892.1 Therefore, The most famous case relating acute appendicitis to direct abdominal trauma is that of the Hungarian escapologist and stunt performer, Harry Houdini, who died in 1926 following a ruptured appendix after being punched several times (with permission) in the abdomen by a trainee.2 The incidence of AP following BTA remains low. It is higher in children than in adults with a predilection of male.2
Four diagnostic criteria should be fulfilled to incriminate the trauma in this condition: No abdominal complaints prior to the trauma, direct trauma should be severe involving the abdominal wall in the right half especially; Symptoms must begin between 6 and 48 hours after the traumatic event, and persist till surgical confirmation.2,3
The patient presented in this case report fulfills all the 4 criteria for the diagnosis of traumatic appendicitis.
The relationship between appendicitis and trauma is not yet clearly identified.
Some authors have claimed that appendix is very rarely affected by direct trauma due to its significant mobility and small size, and that is often associated with other intra-abdominal organ injuries.4
Several mechanisms had been proposed to explain the genesis of AP after BAT. Compressive forces generate an increase intracecal pressure leading to distension of the appendix with a consequent injury of appendiceal mucosa and decreased blood flow which leads to acute inflammation.2,3 It was also suggested that trauma may cause an obstruction of the appendiceal lumen because of edema formation, appendiceal intramural hematomas and/or intrinsic lymphoid tissue hyperplasia with enlarged mesenteric lymph node.5 Another mechanism has been described is that violent trauma with increased cecal pressure can result in displacement of an asymptomatic appendicolith deeply into the appendix leading to obstruction of the appendiceal lumen or its perforation.1,2,5 Moreover, deceleration forces expose to microvascular tears causing ischemia with subsequent perforation.6
In the present case, acute appendicitis was caused by an impacted appendicolith into the appendiceal lumen which is the most common mechanism reported in the literature especially in pediatric population.
It has been noticed that appendicoliths are more common among traumatic appendicitis (60%–65%) than nontraumatic appendicitis (35%) and up to 15% of cases may have an obliteration of the appendix lumen by a fecalith without signs of appendiceal inflammation.2
Mechanisms of trauma in the reported cases are variable but include seatbelt injuries, falls, handlebar injuries, assault, blunt trauma sustained during a motor vehicle collision.7
Due to their vulnerability to direct trauma, their small abdominal cavity and the less muscular abdominal wall, children are more affected than adults and particularly older children who participate in more outdoor activities and can rarely protect themselves against trauma compared with adults.3,5
The clinical presentation of traumatic appendicitis is similar to that of non traumatic appendicitis, beginning from the inception of trauma and persists till the surgical confirmation. Leucocytosis is not consistent.
Perforation with signs of peritonitis may occur immediately or within the 48 hours following trauma.
As in non-traumatic appendicitis, urgent imaging tools such as US and CT scan are highly recommended for stable patients.
They confirm diagnosis of AP, reveal which mechanisms resulting from and help to exclude other clinical entities.
Whatever the context of occurrence, radiological criteria to make an accurate diagnosis of AP remain the same, and imaging findings of the appendix typically mirror those of non-traumatic appendicitis.
In cases when US and CT are non-conclusive, serial physical and radiological examination (especially US) were the major key factor for the diagnosis of TA.8
Diagnostic laparoscopy can be also used in patients who are haemodynamically stable when there is a high index of clinical suspicion and equivocal imaging findings.5
Delay in diagnosis leads to appendiceal perforation with peritonitis requiring a laparotomy with a high rate of morbidity.
Treatment of traumatic appendicitis includes parenteral antibiotics and appendectomy.7
In this case, diagnosis of AP following BAT was made preoperatively by US and CT and the patient underwent appendectomy through a Mc Burney’s incision.
Conclusion
Traumatic appendicitis is an uncommon condition that may occasionally encounter in emergency department especially in pediatric population. Due to its rarity, the diagnosis is often delayed or mistaken. The causal link between trauma and appendicitis remains discussed and several mechanisms had been suggested either in isolation or combination. In stable patients, urgent imaging tools (US, CT) can make an accurate preoperative diagnosis and may reveal the causal mechanism whenever is objective. Although rare, traumatic appendicitis requires a high index of clinical suspicion and should be considered in the setting of right lower quadrant pain following blunt abdominal trauma.
Footnotes
Author Contributions: OC: contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
SC: contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
SEH: contributed to conception; contributed to acquisition and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
NA: contributed to conception; contributed to analysis and interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
LC: contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval is not required for de-identified single case reports based on institutional policies.
Informed Consent: Informed consent was obtained for publication.
ORCID iD: Olaia Chalh  https://orcid.org/0000-0003-1857-4574
https://orcid.org/0000-0003-1857-4574
References
- 1. Ramsook C. Traumatic appendicitis: fact or fiction? Pediatr Emerg Care. 2001;17:264-266. [DOI] [PubMed] [Google Scholar]
- 2. Toumi Z, Chan A, Hadfield MB, Hulton NR. Systematic review of blunt abdominal trauma as a cause of acute appendicitis. Ann R Coll Surg Engl. 2010;92:477-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zvizdic Z, Pasic-Sefic I, Vranic S. Acute perforated appendicitis after blunt abdominal trauma: a report from a 7-year-old boy and literature review. Am J Emerg Med. 2020;38:408.e1-408.e2. [DOI] [PubMed] [Google Scholar]
- 4. Serour F, Efrati Y, Klin B, Shikar S, Weinberg M, Vinograd I. Acute appendicitis following abdominal trauma. Arch Surg. 1996;131:785-786. [DOI] [PubMed] [Google Scholar]
- 5. Gupta R, Mathur V, Bansal J, et al. Acute appendicitis following blunt abdominal trauma in children: by chance or a cause? Formos J Surg. 2016;49:217-222. doi: 10.1016/j.fjs.2016.05.005 [DOI] [Google Scholar]
- 6. Ahmed ST, Ranjan R, Saha SB, Singh B. Lumbar hernia: a diagnostic dilemma. BMJ Case Rep. 2014;2014: bcr2013202085. doi: 10.1136/bcr-2013-202082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cobb T. Appendicitis following blunt abdominal trauma. Am J Emerg Med. 2017;35:1386.e5-1386.e6. doi: 10.1016/j.ajem.2017.06.051 [DOI] [PubMed] [Google Scholar]
- 8. Paschos KA, Boulas K, Liapis A, Georgiou E, Vrakas X. Traumatic appendicitis in minor blunt abdominal injury. Emerg Med Australas. 2012;24:343-346. doi: 10.1111/j.1742-6723.2012.01557.x [DOI] [PubMed] [Google Scholar]