Abstract
The SARS-CoV-2 pandemic has focused attention on prevention, restriction and treatment methods that are acceptable worldwide. This means that they should be simple and inexpensive. This review examines the possible role of glycosaminoglycan (GAG) antithrombotics in the treatment of COVID-19. The pathophysiology of this disease reveals a complex interplay between the hemostatic and immune systems that can be readily disrupted by SARS-CoV-2. Some of the GAG antithrombotics also possess immune-modulatory actions and since they are relatively inexpensive they could play an important role in the management of COVID-19 and its complications.
Keywords: COVID-19, pathophysiology, GAG-antithrombotics, danaparoid sodium, sulodexide
Background
Pandemics occur when an infectious agent is easily transmitted and outwits manoeuvres to prevent its spread. The likelihood of a pandemic increases in the absence of herd immunity, when the resultant infection is asymptomatic and no viable vaccine or treatment to prevent its spread is available. SARS-CoV-2 (COVID-19) is easily transmitted through aerosol droplets from sneezing, coughing and amplified speaking, with an asymptomatic incubation period of about 2-3 weeks. Patients may present with potentially fatal viral pneumonia that can progress to acute respiratory distress syndrome (ARDS). The COVID-19 pandemic is an example where early recognition and measures to limit its spread were either ineffective, too late or both.
In COVID-19 infection the virus enters cells via the ubiquitous surface angiotensin-converting enzyme 2 (ACE2) receptors facilitated by binding to local surface heparan sulphates.1 The majority of COVID-19 infected subjects recover with few or no sequelae, but some patients develop significantly abnormal coagulation parameters. Severe Covid-19 pneumonia is the commonest presentation but generalized thrombotic vasculitis that causes significant organ dysfunction may occur. Mortality is generally lower than with infection caused by other corona viruses, however certain patients appear to be at particular risk for poorer clinical outcomes. These risk groups include the elderly, diabetic, hypertensive, obese and immunocompromised patients. Because the patients at higher risk are to varying extents pre-conditioned with vascular disease, organ damage, increased plasmin levels and a weakened immune system, they are more likely to develop more severe outcomes.
Once admitted to hospital patients with COVID-19 infection often remain for a long time requiring both direct and supportive drug and non-drug management strategies that mainly treat the symptoms. It is estimated that approximately one fifth of admitted patients require intensive care unit (ICU) management.2 This makes treatment expensive and the limited availability of physical resources such as ICU beds and ventilators has led some countries to adopt a “lottery” system treatment based on clinical severity and, unfortunately, for uninsured low income patients treatment may be out of reach. Hospital resources may become overwhelmed and the necessity for reallocation of rooms, facilities and beds means delays in the diagnosis and treatment of patients with other often chronic and/or serious clinical problems. Any measures to limit viral spread within the community, as well as the number of severe COVID-19 cases would reduce the need for expensive and sometimes limited hospital resources, allowing for more patients to be treated, with less disruption for patients with other medical conditions that require urgent management.
An ideal drug therapy for a patient with COVID-19 infection would be one that quickly and completely inactivates and kills the virus without harming the patient. Such a treatment should prevent SAR-CoV-2 cellular invasion, mitigate the vascular attack, maintain normal organ function against aberrant immune and coagulation function, and facilitate the body’s natural systems for repair and restoration of organ dysfunction. An ideal treatment should also be relatively inexpensive and readily available. While there is no single drug currently available that meets these requirements, there is a group of antithrombotics that in-vivo and in-vitro appears to have the ability to ameliorate inflammatory and immune damage, protect and restore the injured endothelium and preserve and restore organ function.
Heparin and the heparinoids are widely used antithrombotics for well over half a century. There has been a burgeoning interest in heparin and related glycosaminoglycans (GAG) polysaccharides, as potential agents in various applications including COVID-19. This interest arises from the ability of GAGs to interact with, and alter the activity of, a wide range of proteins and intrinsic molecular mechanisms. This review will look at aspects of COVID-19 infection that might respond positively to heparin and related GAGs.
Pathophysiological Aspects of COVID-19 Infection
SARS-CoV-2 (COVID-19) is known to move from one animal vector to another. It has also acquired the ability to easily invade all organs and tissues, by high-jacking the ubiquitous membrane ACE2 receptors to enter cells. Like many other pathogenic viruses it uses various cell membrane annexins3 and heparan sulphate sites4 to increase invasiveness and virulence. By entering the body via the upper respiratory tract the virus takes advantage of the separation of the alveolar cells from the blood circulation by only the extracellular matrix (ECM) and a single layer of endothelial cells (ECs). In addition from the oral cavity, the virus may be swallowed either directly or by shedding into saliva. In patients on proton pump inhibitors and the elderly the protective effect of gastric acid is lost allowing the virus to pass more readily into subsequent portions of the gastro-intestinal tract, particularly the intestines.5
Once inside the alveolar and intestinal mucosa cells, SARS-CoV-2 can readily accesses the vascular endothelium of the adjacent rich capillary networks to exert direct cytotoxic effects. Damaged endothelial cells (ECs) lose their tight junctions allowing local plasma leakage. Damaged alveolar and intestinal mucosal cells and ECs release pro-inflammatory mediators that activate the innate and adaptive immune systems including the pro and anti-coagulant proteins and platelets. These responses are part of the body’s natural defense mechanisms that constantly monitor for invasion by foreign organisms and tissue damage. The systems involved initially respond in a co-operative fashion during common medical conditions (infection, trauma, surgery and cancer) by engaging in “cross-talk” aimed at eliminating the pathogenic invasion and effecting tissue repair and recovery.6 The response of the contact system and release of tissue factor (TF) from injured ECs leads to local microvascular thromboses that limit viral spread, but the occlusions also produce local patches of hypoxic cell death and damage causing further problems by way of damage associated molecular patterns (DAMPs) and pathogen associated molecular patterns (PAMPs) released from dead or dying cells.7
DAMPs and PAMPs bind to special receptors on innate immune cells, macrophages, mast cells, dendritic cells, epithelial cells and fibroblasts that stimulate further release of signalling and inflammatory responses with subsequent recruitment and activation of platelets and inflammatory cells. These initial host reactions to viral invasion and cellular damage are more likely to be successful when the viral load is not excessive and/or the host natural mechanisms are sufficient to contain the infection. However, when viral infection is able to overcome these interactions between coagulation and immune/inflammatory responses there will be increases in vascular permeability and oedema, cellular death, thromboses and localized hypoxia that amplify cell damage and hence the host responses.
In many patients the alveoli fill with exudate, dead cells and fibrin resulting in an interstitial pneumonia and, if unchecked, acute respiratory distress syndrome (ARDS).8,9 A significant contribution to this is probably the virus induced breakdown on the renin-angiotensin-aldosterone system (RAAS) producing proinflammatory, pro-oxidative, vasoconstrictive and fibrotic effects.9 A large viral load present in the gastro-intestinal tract is likely to produce symptom of diarrhea, vomiting and abdominal pain. Left unchecked signs and symptoms of hepatic invasion may subsequently develop.10,11
Once the virus has entered the circulation it “targets” pre-diseased regions such as damaged cardiovascular endothelium, myocardial tissue and blood vessels, nephritic kidneys, the mucosa of inflammatory bowel disease and weakened areas of the central nervous system including the brain (which it may access more directly via the nose).
Impaired Immune Response Due to COVID-19
Infected, damaged alveolar epithelial cells respond to COVID-19 infection by upregulating interferon production and the release of cytokines and chemokines that recruit a wide variety of cell types including phagocytes, natural killer cells, basophils, mast cells and eosinophils. As ECs become injured, killed or undergo voluntary apoptosis12 they also release a cocktail of interleukins, cytokines and clotting factors. Platelets are recruited to plug the intercellular gaps and in response to the exposed underlying extravascular matrix containing collagen, they are activated along with the clotting cascade with consequent increased risk of thromboses.
In addition the alveolar and endothelial damage activates the innate immune system, that in turn activates the adaptive immune system to mount an antibody response to eliminate the virus, but this takes time. In the meantime the innate immune system as the first line of defense usually produces a co-ordinated non-specific humoral response to the infection that involves upregulation and secretion of interferons, interleukins, tumor-necrosis factors, chemokines, complement and complement-derived peptides, kinins and opsonins from phagocytes, macrophages and neutrophils attracted to the sites of viral invasion and cell damage.
The complement system has evolved to kill pathogens, send danger signals, and expedite the elimination of apoptotic cells without damaging healthy host cells. It is principally activated via the lectin pathway reacting to contact with the virus. In addition, several of its components can also be activated by hemostasis components. Plasmin (generated by kallikrein), thrombin and Factors IXa, Xa, and XIa are able to activate complement components C3 and C5. Coagulation Factor XIIa can activate component C1 leading to the initiation of the classical complement pathway and of bradykinin formation. Complement component C5a is able to trigger release of endothelial surface proteoglycans which in turn release bound endogenous heparin (HP), heparan sulphates (HS), chondroitins and PF4 into the circulation. Physiologically, HS is the anticoagulant equivalent of therapeutic unfractionated heparin (UFH), since endogenous heparin (HP) only appears to play a local role in the defense against invading organisms and in protecting the mast cells from digestion by their own stored proteases.13 These interactions provide an illustration of the complexity of the systems involved and the importance of the correct cross-talk between them.
Ultimately the complexity of the interactions between the immune/inflammatory system and hemostasis with its many checks and balances is its undoing. If dysregulated the effector function of the complement system being relatively non-specific causes collateral damage to host cells and abnormal hemostatic responses may develop into a coagulopathy or increased fibrinolysis with bleeding.14
The chemokines of the pro-inflammatory response are small predominantly basic molecules intended to attack the virus, protect uninfected cells, process the damaged cells and limit viral spread to other areas of the body. They are particularly involved in attracting leukocytes and immune cells to areas of damage. To do this many need to interact with the glycosaminoglycans (GAGs) of the ECM and the glycocalyx (on the luminal surface of ECs) to achieve full functionality or for protection against proteolysis.15
Acidic HSs make up over 50% of these GAGs16 and are usually bound to specific proteins as proteoglycans. This essential interaction with GAGs, however, has a disadvantage if the cytokine presence is high enough to swamp the negative charges on the HS leading to interference with their ability to act as a sieve, by restricting the movement of positively charged proteins across the extracellular matrix and cell membranes.17 Thus membrane permeability increases allowing fluid to cross more easily and in the lungs flooding the alveoli making breathing difficult.
In patients with risk factors for serious clinical outcomes the inflammatory response becomes increasingly dysregulated and morphs into the so-called “cytokine storm” with even more damaging effects.18 As the infection progresses the increasing endothelial injury, activation and dysregulation of complement and coagulation control leads to a widespread thrombotic micro-angiopathy develops with intracellular complement deposition19 that further exacerbates the inflammatory injury and response causing serious morbidity and potentially fatal organ damage.
Endothelial Damage
Once inside the lungs COVID-19 targets the vascular endothelium via the alveolar cells. The endothelium normally presents a well-controlled 2-way barrier separating the blood from the tissues and controlling local hemostasis and vascular repair. Viral elements have been identified at autopsy within the ECs with an accumulation of inflammatory cells and evidence of endothelial and inflammatory cell death12 showsg that they are the next line of attack.
The virus induces the ECs to initiate coagulation, up-regulates EC bradykinin 1 receptors and, by occupying the ACE2 receptors for cell entry, it prevents ACE2 inactivation of bradykinin.20 The accumulation of bradykinin produces angioedema which reduces oxygen transfer from alveoli to lung capillaries producing local hypoxaemia and systemic hypoxia that results in further damage to the basement membranes and endothelium. The resultant increase in porosity and permeability of the basement membrane produces local tissue oedema and vessel narrowing. Damaged alveolar and ECs release not only procoagulant factors including tissue factor and kinins that trigger the extrinsic and intrinsic pathways of the clotting cascade respectively, but also pro-inflammatory mediators to attract leukocytes. Eventually some patients experience a breakdown of the normally co-operative cross-talk between the immune and hemostasis systems leading to an endotheliopathy21 characterized by direct viral cytotoxicity causing death of ECs and inflammatory cells, cytokine induced apoptosis, increased generation of Factor Xa and thrombin and release of von Willebrand Factor (vWF) that facilitates platelet adhesion to the injured cell surfaces. These platelets in turn become activated and release platelet agonists (adenosine di phosphate and thromboxane A2) that amplify platelet activation, procoagulant microparticles that increase thrombin production and cytokines including platelet factor 4 (PF4).
PF4 under normal repair situations is chemotactic for neutrophils, fibroblasts and monocytes, inhibits EC proliferation and possibly participates in wound repair and inflammation. However, it also promotes coagulation, by binding to and inactivating the endogenous HS anticoagulant, and HP, and prevents activation of heparin co-factor II (HCII) by dermatan sulphate (DS).22 This reduces the protective effect of the local HP and administered UFH on the vascular endothelium and increases the thickness of fibrin strands in clots. It is also an antithrombotic because it can stimulate thrombin-thrombomodulin (TM) dependent formation of activated Protein C (APC).23,24
To complicate matters further if local Protein C levels are reduced during COVID-19 infection then thrombin, via its complexing with TM, mainly acts to promote activation of TAFI (thrombin activated fibrinolysis inhibitor).23 Under certain circumstances PF4 blocks this action leading to increased expression of plasmin and fibrinolytic activity.24 Added to this are the effects of a bacterial superinfection that can augment the disruption of the host defense mechanisms. These intricate relationships between PF4, thrombin, TM, APC and TAFI and their connections with the immune system add further levels of complexity to COVID-19 disease expression and its possible treatment.
Amplification of the rate of viral replication and its increasingly disruptive effects producing both local and systemic cytokine storms lead to a combination of uncontrolled inflammation and a widespread endotheliitis.12,21,25
Another serious consideration is that increased PF4 concentrations may at least contribute to UFH and low molecular weight heparin (LMWH) resistance seen in the most severely affected COVID-19 patients26 or at worst trigger formation of anti-platelet antibodies to produce an immune mediated thrombocytopenia.
Endothelial Antibodies
Although COVID-19 infection is not a chronic disease it can take some months before it is brought under control, during which time it is not unlikely that the endotheliitis provokes formation of anti-endothelial antibodies (AEA). Alternatively AEA may already be present in patients with a history of autoimmune disease associated with vasculitis such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), Wegener’s granulomatosis and diabetes. AEA activate ECs to further increase the inflammatory response and are capable of suppressing EC thrombomodulin production required for activated protein C (APC) production. In addition the AEA may cross-react with heparin,27 especially in the presence of the increased local and systemic PF4 levels, to enhance endothelial binding and damage similar to the occurrence in patients with heparin-induced thrombocytopenia HIT.28
Hemostasis Disruption
The coagulation cascade normally acts as an intermediary when blood vessels are damaged to either limit bleeding by providing a fibrin framework that is able to attract and stimulate specific cells to repair any endothelial damage in otherwise intact vessels and to repair and remodel severed vessels. Local upregulation of plasminogen production and its activation should lyse any microthrombi restoring circulation to tissues and endothelium under repair. If the endothelium is disrupted the ECs release tissue factor (TF) that rapidly increases local thrombin generation. This effect with some related viruses initiates a hyperinflammatory response29 and probably underlies the early pathogenesis of COVID-19 infection.
In some subjects the EC invasion by the SARS-Cov-2 results in direct cell cytotoxicity that is augmented by the role of the C3a, C4b and C5a components of the complement cascade. Although cleavage of thrombin by C5a possibly provides a check on the increasing thrombin generation it also leads to platelet activation and release of TF and microparticles thus amplifying thrombin production and coagulation. Which one of these opposing actions predominates in an individual COVID-19 patient is unclear, but it may be related to the viral load, patient susceptibility and the extent of cell damage. The inflammatory damage also releases GAGs from ECs and HP from activated mast cells to provide negatively charged surfaces for the autoactivation of released Factor XII and kallikrein that not only initiate clotting cascade activity via the intrinsic pathway but also directly increase local fibrin fiber density to strengthen the tissue deposits.
Concomitant release of polyanions from the endothelium includes the local anticoagulant, a high molecular weight, highly sulphated, AT binding heparan sulphate (HS) that is the endogenous equivalent of unfractionated heparin (UFH).
Runaway thrombin generation may develop as a result of dysregulation of both the coagulation and complement cascades, increased platelet sensitivity and their activation by components of both cascades, complement activation and damage, formation and release of vWF multimers, formation of neutrophil extracellular traps (NETs), release of extracellular histones and the endotheliitis. All these factors contribute to the appearance of an at first localized thrombotic microangiopathy (TMA).30
Starting in the lungs the TMA appears to be an “if all else fails” attempt to limit viral spread. However the finding of its involvement in the pathology of many organs and tissues at autopsy suggests little success, since it only serves to produce more hypoxia-induced endothelial damage and necrosis that may finally result in organ dysfunction and failure. The TMA associated with COVID-19 appears to be similar to the TA-TMA (transplant associated thrombotic microangiopathy) and thrombocytopenia that develops in response to the chemotherapy conditioning in preparation for bone marrow transplantation in leukemic patients since both respond to treatment with anticomplement drugs e.g. eculizumab.31
Thrombin Generation
Thrombin is emerging as one of the most important mediators of morbidity in COVID-19, influencing both coagulation and immune reactions. Its generation is enhanced by tissue factor (TF) and kinin release from damaged ECs that activate the extrinsic and intrinsic coagulation pathways of the coagulation cascade. In addition several components of the innate immune system can also lead to thrombin generation,9 e.g. MASP-2, a component of the lectin pathway of complement activation is able to convert prothrombin to thrombin21 and complement components 4d and 3a deposited on the platelet surface in trauma patients promote platelet aggregation and release of pro-coagulant proteins.
The main regulators of the clotting cascade are the inhibitors APC, AT (antithrombin), HCII and TFPI (tissue factor pathway inhibitor) that ensure that thrombin generation is sufficient to maintain hemostasis and for its many other functions, e.g. pro-inflammatory, acting via its specific cell membrane protease activated receptors PAR-1, PAR-3 and PAR-4 to increase leukocyte recruitment into atherosclerotic plaques, enhance oxidative stress and migration and proliferation of vascular smooth muscle cells, and influence apoptosis and angiogenesis.
Low levels of thrombin are anticoagulant because with thrombomodulin it activates Protein C to form APC. APC inhibits activation of clotting Factors VIII and V that participate in the tenase and prothrombinase complexes that generate Factors Xa and thrombin respectively. However, plasma APC levels are low compared with other clotting factors and inhibitors and in some patients with COVID-19 infection the pace of thrombin generation, geared by increasing levels of coagulation cascade activators, and the ability of thrombin to upregulate its own generation via several positive feedback loops, one of which is via activation of Factor IX, outstrips the capacity of APC and the other antithrombotic regulators to control it. This is the so-called “thrombin paradox”32 in which low levels of thrombin are anticoagulant and high levels are pro-coagulant. The switchover between the 2 states is determined by the level at which the hemostat is set in relation to the strength of the stimulus to change and is, to a large extent, patient specific.
Plasmin Activator Inhibitor (PAI-1), Plasmin and Fibrinolysis
The fibrinolytic status of COVID-19 patients is determined by local and circulating plasmin levels. In most early infected patients the level is mainly suppressed by increasing production and release of PAI-1 in response to:
cytokine TNF-α (tissue necrosis factor- α) that stimulates PAI-1 release from ECs, and the adipocytes in obese subjects,
interference of the renin-angiotensin system (RAAS) with loss of effective ACE2 receptors
inflammatory responses that induce platelets and macrophages to release PAI-1
hypoxia that induces monocytes to release PAI-1,
reduced levels of APC.
The resultant high PAI-1 levels circulate as highly active vitronectin complexes that inhibit tissue plasminogen activator (t-PA) and urokinase activation of plasminogen to plasmin. In combination with increased activation of α2-antiplasmin and TAFI, plasmin generation is greatly reduced producing a “fibrinolysis shutdown.”33
The endothelium derived PAI-1 locally inhibits Factor XIa in vitro and also inactivates thrombin thus acting as a local anticoagulant. However, it has no effect on the inflammation-induced increased activation of Factor XII and the kallikrein-kinin system thus supporting complement activation. PAI-1-vibronectin complexes also efficiently inactivate APC, thus removing an inhibitor of TNF-α production by the ECs and further promoting PAI-1 synthesis and release. Depending on the local conditions high APC concentrations are able to deplete PAI-1 leading to increased fibrinolysis.34
The fibrinolysis shut-down appears to predict both thrombo-embolic events (TEs) and acute kidney injury (AKI) with the need for hemodialysis (HD). In a study of 44 COVID-19 patients,35 those with fibrinolytic shutdown had a 40% rate of TE (mainly pulmonary emboli, deep vein thrombosis and ischemic stroke) and an 80% rate of HD compared with 5% and 14% respectively in patients without shutdown. The authors concluded that “fibrinolysis shutdown, as evidenced by elevated D-dimer levels and complete failure of clot lysis at 30 minutes on thromboelastography predicts thromboembolic events and need for hemodialysis in critically ill patients with COVID-19.” This emphasizes the need for anticoagulant and/or fibrinolytic therapy.
Plasmin is released by macrophages and its generation increases in response to upregulation of t-PA by increasing levels of bradykinin released from ECs as part of the inflammatory response and cytokine storm. It is not only a thrombolytic for intravascular thrombi but is also essential for removing fibrin deposits in the lungs, thereby reducing the risk of hyaline membrane formation and alveolar fibrosis, digesting many of the misfolded and necrotic proteins36 remaining on the battlefield as the viral invasion moves on, and supressing the inflammatory and immune systems. However, on the downside plasmin exacerbates lung oedema via Factor XII /bradykinin activation and is able to cleave one of the COVID-2 viral spike proteins to facilitate its entry into the cells thus increasing its infectivity and virulence.37
Interestingly the patients with risk factors for poor outcomes of COVID-19 infection, i.e. hypertension, diabetes, old age and obesity, may already have increased plasmin(ogen) levels prior to infection. In addition, mast cells recruited by the inflammatory response to EC damage release trypsin as part of the initial innate immune system response and both trypsin and kallikrein can convert plasminogen to plasmin leading to increased fibrinolysis.
The disruption of the thrombotic, fibrinolytic and inflammatory systems coupled with diffuse endothelial damage causes many severely ill patients to develop a syndrome similar to disseminated intravascular thrombosis (DIC).14 It may be present on admission to hospital or develop later but is associated with a poor prognosis.38 It differs from classical DIC in that the fibrinogen level is raised not lowered, platelet count reductions are usually not so profound, thrombosis rather than bleeding occurs, the D-dimer level increases are more pronounced (due mainly to the infection severity than the coagulopathy39) and it is profibrinolytic (possibly resulting from inhibition of TAFI activation by high levels of PF423). The hemostatic situation resembles a combination of chronic DIC and TMA,40 and in some respects too the DIC with increased fibrinolysis found in promyelocytic leukemia, heat stroke and some malignancies. This latter variant also includes increased thrombin generation and thrombocytopenia but, unlike the coagulopathy of COVID-19 infection, fibrinogen levels are low and bleeding is frequent and often severe. Thus which predominates, the “hypercoagulation associated with the fibrinolysis shutdown” or the “coagulopathy associated with hyperfibrinolysis,” depends on the balance between local sub-endothelium concentrations and systemic levels of plasmin and thrombin and their many influencing factors.
APC and PAR Activation
APC protects the microcirculation from thrombosis. It is formed when EC thrombomodulin binds and blocks the coagulant sites of thrombin to form a complex that activates Protein C. During its formation APC is bound to specific endothelial receptors (EPCRs) situated on the luminal surface but dissociates from these receptors to bind to Protein S and become fully activated. When bound to the EPCR, APC activates PAR-1 a member of the PAR family of transmembrane proteins critical for the interplay between the coagulation and inflammation.41 The members of the PAR family between them regulate chemotactic cellular responses that provide cytoprotective effects on endothelial cells and leukocytes, but each member of the family has a different role as cofactor for regulation of hemostasis, endothelial permeability, cell adhesion, inflammatory responses, vascular tone and down-regulating vascular adhesion molecule production etc. The members of the PAR family are activated not only by APC, but also by Factor Xa that upregulates PAR-1 and PAR-2, and thrombin that upregulates PAR-1 and 3 directly and PAR-4 only at high thrombin concentrations. However the duration of activation, the location of PAR and presence of co-receptors also factor into which PAR family member is activated.42 Thus APC directly or indirectly negatively influences TNF-α production, EC E-selectin expression, neutrophil activation and mast cell degranulation.43 It also downregulates and inactivates PAI-1 to promote fibrinolysis and by activating PAR-3 it inhibits neutrophil extracellular traps (NETs) formation (NETosis).
In severe infections levels of APC are reduced by significant hepatic (ischemic) damage, consumption, extravascular leakage and renal loss, down-regulation of EPCRs by thrombin or inflammatory cytokines, by reduced availability of thrombomodulin and high levels of PAI-1: vitronectin complexes. In addition fibrin networks, by inducing platelet activation with microparticle and cytokine release, activate the clotting cascade to amplify the levels of Factors Xa and thrombin. The sustained release in COVID-19 infection of both proteases and low APC activity leads to dysregulation of the normally protective interactions between the different PAR proteins, producing increased end-organ damage from increased inflammation, endothelial permeability and thrombosis induced ischemia. Thus it is important to prevent or restore the disruption of PAR components by reducing the excessive activation of the clotting cascade, thrombin production and maintenance of at least normal levels of APC. In addition, reduction in PAI-1 activity may also be reduced if APC levels are maintained.
HMGB-1, Histones, NETs and Cellular microRNA
Damaged cells release nuclear contents including high-mobility group box 1 (HMGB1), an abundant small nuclear protein that normally binds chromatin. In addition, it is possible that the effective loss of ACE2 receptors taken over by the virus also stimulates its release.44 Once outside the cell free HMGB-1 acts as a cytokine, further contributing to the cytokine storm and inflammatory response. It also regulates autophagy—a process involved in COVID-19 infection and viral entry and replication in cells.
In COVID-19 viral toxicity is the most immediate cause of cell death and platelets activated in response to the pathogenic invasion, induce neutrophils to commit suicide and release DNA fibrils packed with histones (nucleosomes).45 This process of NETosis produces extracellular traps or NETs containing a mixture of antimicrobials, myeloperoxidase (MPO)-bound DNA, and histones. NETs serve as a physical barrier to prevent further spread of the pathogen by trapping and chemically disarming pathogens using a variety of weapons including neutrophil elastase, cathepsin G and histones. In addition, NETs may prevent potentially injurious proteins like proteases from diffusing away and inducing damage in adjacent healthy tissue and in providing a framework for platelet adhesion via vWF leading to local micro-thromboses they also appear to localize the invasion. However these beneficial actions can turn against the host since an overwhelming viral load can produce overactive NETs that promote coagulation via activation of Factor XII and then compromise the microcirculation by clogging blood vessels. They also circulate uncontrolled in the bloodstream to increase both locally and systemically the level of inflammation46 by inducing immune complex formation and cytokine and chemokine release and increase the risk of micro and macro-thromboses and morbidity. The balance between protective or potentially pathogenic effects NETs is very much related to their protein content which appears to be influenced by local concentrations of thrombin and plasmin,47 and to the tissues and circumstances of their formation.
Histones are highly cationic intra-nuclear proteins that normally support chromatin development and regulation of gene expression in the cell nucleus. Apart from their participation in NETs they can be released into the extracellular space as DAMPs from dead and dying cells in response to stress48 either free or as a DNA-bound nucleosome. In COVID-19 extracellular histones have been demonstrated in the tissues and circulating in the blood where they become thrombogenic by activating platelets to release microparticles and TF, thus stimulating local thrombin production, and reduce TM production required for APC formation. Furthermore, depending on the circulating DNA: histone ratio, formation of DNA: heparin complexes softens clots but histone: heparin complexes increase clot strength and also inhibit the antithrombotic activity of HS and administered UFH/LMWH.49 However the non-anticoagulant chains of the heparins, i.e. depleted of the binding sites for AT are able to “mop up” circulating histones and destabilize NETs50 by dissociating histones from their DNA binding sites.
Histones are also cytotoxic51 since they promote cleavage of C5 and terminal complement components, increase calcium entry into cells by binding to membrane phospholipids,52 amplify the inflammatory response,53 alter membrane permeability and when bound to UFH they interfere with NETosis. APC by degrading extracellular histones ameliorates the deleterious effects of both NETs and histones, provided that its generation has not been compromised by rising levels of thrombin and PAI-1.
Reduced local cellular levels of microRNA (miRNA) are associated with increased susceptibility to and mortality in infectious lung diseases. MiRNA regulate gene expression by controlling the activity of messenger RNAs in the cell, and some induce virus infected cells to self-destruct thereby limiting the potential amount of virus the infected cell can produce. Corona viruses are able to bind and inactivate these miRNA and it is hypothesised that SARS-CoV-2 particularly binds to apoptosis-inducing miRNAs. This effectively reduces the cellular concentration and activity of the miRNA and prevents/delays apoptosis. Thus the cell lives longer to produce more virus and the virulence of SARS-CoV-2 is increased.54
Thrombocytopenia and HIT
Platelets are important not only for primary hemostasis and thrombus formation but also because they co-ordinate inflammation and the immune response by releasing cytokines and inflammatory mediators and interact with different types of leukocyte and the endothelium. In severe COVID-19, viral RNA can be found in platelets that are activated by lower concentrations of thrombin. Despite a high level of platelet activation from the start of COVID-19, as part of the first line of defense against the virus, the count remains normal or only mildly reduced, unlike the early thrombocytopenia in that other state of high platelet activation, HIT. One suggestion for this is their release from lung megakaryocytes in response to an increase in hepatic thrombopoietin production.55,56 As the infection and its complications worsen the platelet count decreases as a result of increased clearance after viral uptake, platelet sequestration in (pulmonary) thrombi and NETs, response to the endotheliitis, as part of the development of TMA and the possibility that the virus could block release of platelets from lung megakaryocytes. In addition, the late appearance of the DIC-like disorder, or the presence of an active co-morbid disorder such as anti-phospholipid syndrome (APL) or immune thrombocytopenic purpura (ITP),57 or drug-induced platelet reductions (including various HIT syndromes), will exacerbate the problem. Ultimately the severity of the thrombocytopenia, that can occur in up to 60% of severely affected COVID-19 patients, and the earlier it occurs, become prognostic indicators of increased morbidity and fatal outcome.58
In one study in DIC patients59 PF4: heparin complexes were detected by polyspecific enzyme immune assays (EIAs) and IgG-specific enzyme-linked immunosorbent assay (ELISA) in 11 of 35 patients (31.4%) receiving heparin and in 3 of 45 patients not receiving heparin. In the 14 positive patients both platelet counts and coagulation parameters (D-dimer, and thrombin-antithrombin and plasmin: antiplasmin complexes) were significantly lower compared with the negative patients. Only 3 of the heparin treated patients (8.5%) were diagnosed with HIT on the basis of optical density (OD) levels by both polyspecific and IgG ELISAs that exceeded 1.0. Interestingly one of these 3 patient also had by far the highest OD (>3.0) for IgM antibodies and the 3 non heparin patients with heparin: PF4 antibodies were not discussed further.
HIT has also been described in COVID-19 patients60 and thrombocytopenia improved with a heparin replacement. Platelet activation during COVID-19 results in high levels of circulating PF4 and 2 types of HIT have been described. True HIT with positive platelet activating IgG and polyspecific EIAs for antibodies to heparin: PF4 complexes. “Spontaneous” HIT with no history of heparin exposure61 either during or prior to the COVID-19. This “Spontaneous” HIT may have been induced by endogenous heparin released from surface proteoglycans of injured endothelial cells augmented by mast cell activation during the innate immune response to the infection. However, if stoichiometric conditions allow then any polyanion can bind to PF4 (or perhaps other positively charged proteins such as interleukin-8 and neutrophil activating peptide-2) to form complexes that induce antiplatelet antibody formation, including the highly sulphated endogenous anticoagulant HS released from the injured endothelium. Furthermore, the similarity between specific domains within different GAGs and heparin may be sufficient to produce serological cross-reactivity and for the spontaneous HIT to be exacerbated by heparin administration.
True and spontaneous HIT are clinically virtually indistinguishable and without carefully designed serological testing many cases of thrombocytopenia due to spontaneous HIT will be missed especially if the test for HIT only detects heparin: PF4 antibodies. Early “preclinical” spontaneous HIT will not yet show a platelet count reduction of 50%, hence if heparin treatment is initiated it may induce a further platelet count reduction and if this occurs HIT should be suspected since its combination with DIC and/or renal dysfunction is associated with a high mortality.62 Its frequency prompted the authors to recommend heparin avoidance, but we must also keep in mind that but heparin use has also been reported to significantly reduce mortality63 in non-HIT patients. Thus, as in any situation where heparin is used, checking platelet counts prior to and during heparin therapy, especially if a new thrombosis occurs despite seemingly adequate dosing, is of vital importance. Any (further) reduction greater than 30% should trigger applying the 4Ts scoring system despite its lower value in the ICU for excluding HIT,64 the performance of at least a sensitive functional test and a polyspecific Ig test to detect platelet activating antibodies induced by heparin: PF4 complexes, and possibly tests for antibodies directed against other polyanion/polycation complexes.65 Although HIT can be over-diagnosed in the ICU setting the possibility of spontaneous HIT and the contribution of HIT in general to increased morbidity and mortality is a reason for extra vigilance and caution.
Thrombosis Risk
Patients with severe COVID-19 infection satisfy all the conditions of Virchow’s Triad for an increased risk of thrombosis: hypercoagulable state, endothelial damage and stasis (being bedridden) and their frequency is higher than in other conditions.66 Platelet activation, increased blood viscosity due to high fibrinogen levels,67 increased heparanase expression,68 altered blood flow caused by vasoconstriction secondary to down-regulation of endothelial nitric oxide production and fibrinolytic shut-down, further increase the risk of micro and macro-thrombotic occlusion and organ failures.69 Thus COVID-19 infection has been found to be associated with up to 42% symptomatic and asymptomatic venous thromboembolism (VTE) plus 3.7% arterial thrombi70–72 affecting the cerebral, cardiac and gastrointestinal circulations.
Although patients may receive thrombosis prophylaxis or treatment, or additional support to maintain extracorporeal circuit (ECC) patency, thrombosis often seems to occur despite seemingly adequate levels of prophylaxis.70,72 This may be related to the type of clots formed in response to circulating NETs or high levels of heparin binding proteins22 particularly PF4 which also binds to and changes the structure of fibrin making the clot stiffer73 and more resistant to fibrinolysis.74
Bleeding Risk
The risk of bleeding is generally low in COVID-19 but increases with the severity of the patient’s illness, particularly if the hyper-fibrinolytic DIC-like syndrome develops.75 It usually occurs in patients receiving anticoagulant treatment, nevertheless, it remains less than the usual frequency encountered in classical DIC patients possibly because of the extreme level of platelet activation in COVID-19, analogous to the situation in patients with HIT (who usually fail to bleed even with platelet counts <10 Giga/L). The site of bleeding is often determined by the extent of tissue damage and duration of hypoxaemia following microvascular thrombosis and cell necrosis, hence the upper respiratory tract is a frequent site. However severe events are usually associated with PE, gastrointestinal hemorrhage and intracranial bleeding (due to breakdown of the blood-brain barrier or hemorrhagic transformation of ischemic strokes) and are not uncommon contributions to COVID-19 infection fatalities.
Summary
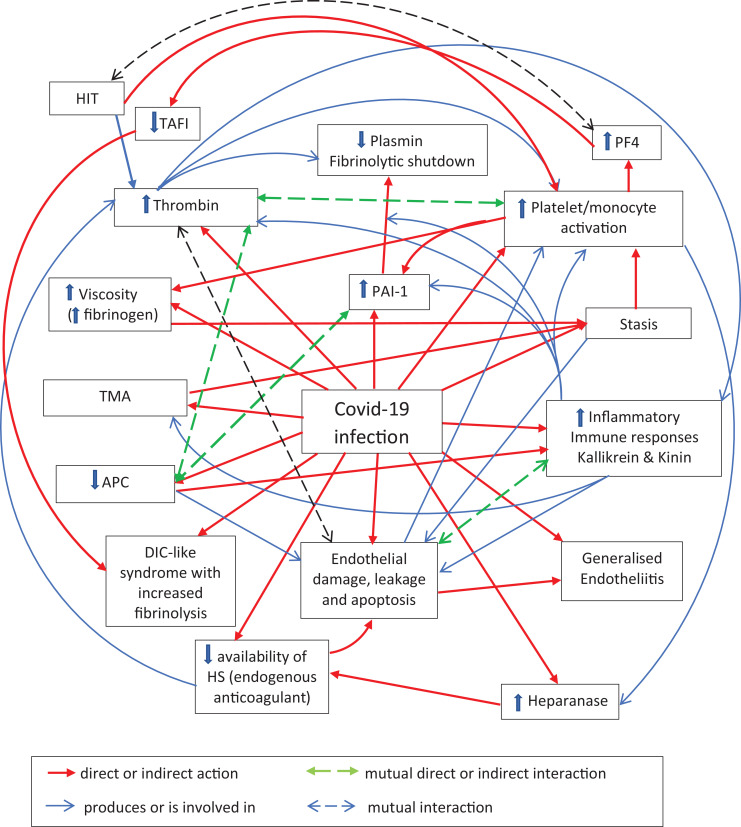
While each aspect of COVID-19 can be dissected out individually the complexity of their interactions on both the local and systemic scale is more difficult to predict but ultimately determines the fate of the patient. Every system involved starts out to protect the host but the often devious ways the virus takes to interfere and produce dysregulation can often lead to damaging effects, particularly in hosts with systems that are faulty or set at a homeostatic level that is more easily disturbed.
The complex pathophysiological reactions induced by COVID-19 affect the body’s organs to varying extents related to the viral load and individual patient susceptibility although certain patterns have become evident.76 The dilemma is compounded by the extent of interplay between local and systemic immune, inflammatory, coagulation and fibrinolytic responses to the virus that varies at different stages of the infection. Hence the therapeutic challenge is to identify the correct management strategy at the time of patient presentation. The goal would be to provide measures to prevent or ameliorate the harmful effects of the cytokine storm, hemostasis disruption, excessive complement activation, PARs dysregulation, extracellular histones and other deleterious changes in homeostatic mechanisms as early as possible.
Additional Effects of Risk Factors for Poor Outcomes in COVID-19 Patients
Diabetes
Diabetes is a significant predictor of morbidity and mortality in COVID-19 patients77 Diabetics have more ACE2 receptors thus intensifying the COVID-19 cell invasion and virulence, and uncontrolled hyperglycaemia itself is associated with:
Glycation with thickening of the vascular basement membrane,
Increased expression of heparanase78 resulting in cleavage and loss of HS from the glycocalyx and basement membrane,79–81
Reduction of synthesis and sulphation of the heparan sulphate proteoglycans,
Reduction in the luminal glycocalyx volume by shedding of negatively charges GAGs,
Increased expression of adhesion molecules,
Formation of cross-linked collagen with reduction in the elasticity of the vascular wall.
Insulin resistance is also associated with increased levels of complement due to its upregulation and activation. One consequence of this is increased cleavage of HS in both the vascular glycocalyx and basement membrane thus reducing their negative charge and increasing endothelial permeability to leukocytes, proteins and fluid. The result is loss of local tissue homeostasis and inappropriate responses to inflammation and immune stimuli.81 The albuminuria in diabetes therefore reflects not just the nephropathy but the general angiopathy that allows free access of positively charged proteins and fluid to the urine or sub-endothelial space. In the kidney this leads to deteriorating renal function and eventually failure, in the eye leakage from retinal blood vessels and capillaries produces a proliferative retinopathy that can lead to blindness and in larger vessels it results in accelerated atherosclerosis and its consequences. Even short-term, low dose treatment with heparins and heparinoids has been shown to alleviate the proteinuria and retinopathy, i.e. it generally improves the angiopathy probably by restoring negative charges in the vascular glycocalyx.
Diabetes is also responsible for increased PAI-1 production, reduced fibrinolysis, endothelial dysfunction, abnormal platelet function, increased levels of HMGB-182 and increased or dysfunctional cytokine release—changes which further promote the risk of thrombosis and inflammation in the presence of the angiopathy.
Obesity
Obesity unlike hypertension and diabetes is more prevalent in women than men. It is associated with increased glucose intolerance, hypertension and dyslipidaemia, all of which increase the likelihood of vascular disease and thrombosis. In addition, the sheer mass of adipose tissue reduces lung capacity and increases vulnerability to severe lung problems in COVID-19. Obesity is also associated with increased PAI-1 production particularly if insulin resistance is present. The source of the PAI-1 is probably ECs and adipocytes.83
Obesity is also associated with increased HMGB-1 levels and the adipose tissue is pro-inflammatory,84 hence it shares with most chronic diseases disturbances of inflammatory control as a result of the hypoxia that occurs in hypertrophied adipose tissue. This stimulates expression of inflammatory genes, activates immune cells and is reflected in increased circulating levels of pro-inflammatory proteins. Thus the inflammatory and immune system imbalance in obesity only serves to enhance the effects of SARS-CoV-2 infection.
Hypertension
Hypertension associated with dysregulation of RAAS (the renin–angiotensin–aldosterone system consisting of a cascade of vasoactive peptides), is so closely linked with age, diabetes and obesity that it is not easy to separate any specific association with outcomes of COVID-19.85 However, in hypertension ACE2 activity is reduced, hence conversion of angiotensin II to angiotensin 1-7 is reduced thus augmenting the inflammatory effects of angiotensin II and reducing the vasodilator and anti-inflammatory effects of angiotensin 1-7.
When SARS-CoV-2 binds to surface ACE2 receptors which are then internalized it effectively reduces ACE2 activity. Thus both pre-existing hypertension and the infection result in reduced angiotensin 1-7 level in the lungs and other organs that contribute to the inflammation and microangiopathy with the potential for increasing the risk of organ damage. Therefore reducing formation of angiotensin II, protecting ACE2 receptors or increasing ACE2 activity might mitigate the serious effects of COVID-19.86
Risks Associated With the Neurological System
The central nervous system is often the source of the first symptoms of COVID-19.since it can readily gain access to the brain via the nose. It appears to be able to cross the blood-brain barrier extension of the vascular system, especially if it is involved in the hyper-inflammatory state, cytokine storm and endotheliitis. It is also possible that the aged patient, in particular, already has a brain barrier/cerebral circulation that is compromised by a pre-COVID-19 infection or subclinical vascular disturbances as a result of hypertension, a systemic vasculitis, sports injuries or silent lacunar strokes.87 The virus again exploits ACE2 receptors to enter neurones and glial cells that respond by releasing interleukins and TNF-α to produce a local inflammatory state. Supporting this is the finding of the virus in the CSF of patients with neurological symptoms, the early loss of smell and taste and the increased occurrence, though uncommon, of encephalopathy, meningitis, altered mental status, and Guillain-Barré syndrome during the infection.88,89 It is possible that COVID-19 may produce chronic neurological damage leading to degenerative disorders and inhibition of neuronal replication to initiate the development of dementia.
Advanced Age
Aging has been identified as a risk factor for developing severe outcomes to infection with the SARS-CoV-2.90 This is possibly due to lower immunity, frailty, a higher prevalence of chronic illnesses and a reduced ability to clear viruses. Age-related changes in immunity begin in earnest in the 6th decade of life and progression from there is downhill. The aging immune system gradually loses the ability to protect against infections and cancer, fails to support appropriate wound healing, and vaccination responses become impaired. Conversely, inflammatory responses mediated by the innate immune system gain in intensity and duration, increasing the susceptibility of older individuals to tissue-damaging immune and inflammatory disorders. Ultimately these functional losses may be associated with age-related reduction in the accuracy of the DNA repair system. In addition, age related reduction of microRNA (miRNA) in the body has been recognized that could facilitate viral replication and increase the viral load and virulence in an already at-risk population.54
Age-associated remodeling of the vasculature occurs involving impaired vasorelaxation, an increase in vascular permeability, inflammation, and fibrosis as vessels become stiffer and thicker. Aging ECs become dysfunctional and more vulnerable to pathogenic attack and less responsive to normal stimuli.91 Thus age is also a risk factor for thrombosis with age-related increases in coagulation factors, particularly fibrinogen and vWF, venous stasis due to inactivity, the gradual life-long build-up of arterial atheroma and the effects of age-related hypertension.
After 60 years gastric acid secretion declines. Consequently the reduced acidity is unable to prevent swallowed virus from invading the intestinal tract. Thus the viral load in the elderly is greater than in younger subjects.92
Renal Dysfunction
COVID 19 produces a high frequency of renal failure and evidence of renal dysfunction—proteinuria and microscopic hematuria.93 General age-related reduction in renal function is more often seen and more pronounced in males94 hence it appears to be dependent upon the testosterone: estrogen ratio. Testosterone suppresses the RAAS system, a critical regulator of blood volume and systemic vascular resistance and highly important for structural and functional renal impairment.
In addition some patients will have pre-existing renal pathology particularly hyperglycaemic damage in diabetics. This and COVID-19 induced TMA and endotheliitis, down regulation of nitric oxide production, increased glomerular heparanase expression (upregulated by both AngII and hyperglycaemia79), hypoxia and, the hyper-inflammatory response leading to depletion of negatively charged HS from the basement membranes and the appearance of proteinuria) also contribute to the development of age related renal problems. COVID-19 infection is able to exacerbate all these effects and with further inflammatory changes in the nephrons including glomeruli filled with fibrin, acute tubular necrosis and ischemic changes resulting from its thrombotic microangiopathy the insults may rapidly lead to renal failure.95 Transient management with continuous or intermittent HD support is frequently required and may further exacerbate the inflammatory process. Because of the local and systemic hypercoagulable state citrate protection of the circuit may be insufficient and an antithrombotic will be required.
Male Sex
Current data suggest similar infection rates for men and women yet males are disadvantaged when it comes to survival. The higher fatality rate for men infected with the COVID-19 virus may derive from gender-based immunological differences,90,96 or be associated with pre-infection comorbidities, including hypertension, cardiovascular diseases, obesity and diabetes which affect more men than women. However, not to be discounted is the fact that female cells have 2 X chromosomes compared with the single X of male cells.
The X chromosome is fundamental in determining sex-specific immune responses, so for males this means only a 50% chance of having the best alleles of genes that regulate immunity, whereas females have a choice of 2 alleles instead of one for each gene and the action of the better of the 2 will predominate making them more immunoreactive than males and better survivors. A Dutch study97 found in young men with severe COVID-19 infection that the gene on the X chromosome for the Toll-like receptor 7 (TLR7) that allows immune cells to detect the virus, is not operating properly. This could allow SARS-CoV-2 to move unchecked by the immune system. Thus the authors speculate that the difference in TLR7 dosage between men and women could in part explain the predisposition of men to develop severe COVID-19.
Summary
SARS-CoV-2 invasion creates the potential for increasingly complex interactions between the body’s local and systemic defense mechanisms involving the immune system and hemostasis. The opportunity for dysregulation and consequent development of a generalized vasculitis leading to local and systemic hypoxia and increasing tissue and organ damage is especially high in patients with pre-existing clinical problems, particularly vascular disease, organ dysfunction, a hemostasis balance set at a level more vulnerable to minor perturbations and a weakened immune system. These factors focus, facilitate and exacerbate the effects of the virus.
Antithrombotics in the Management of COVID-19
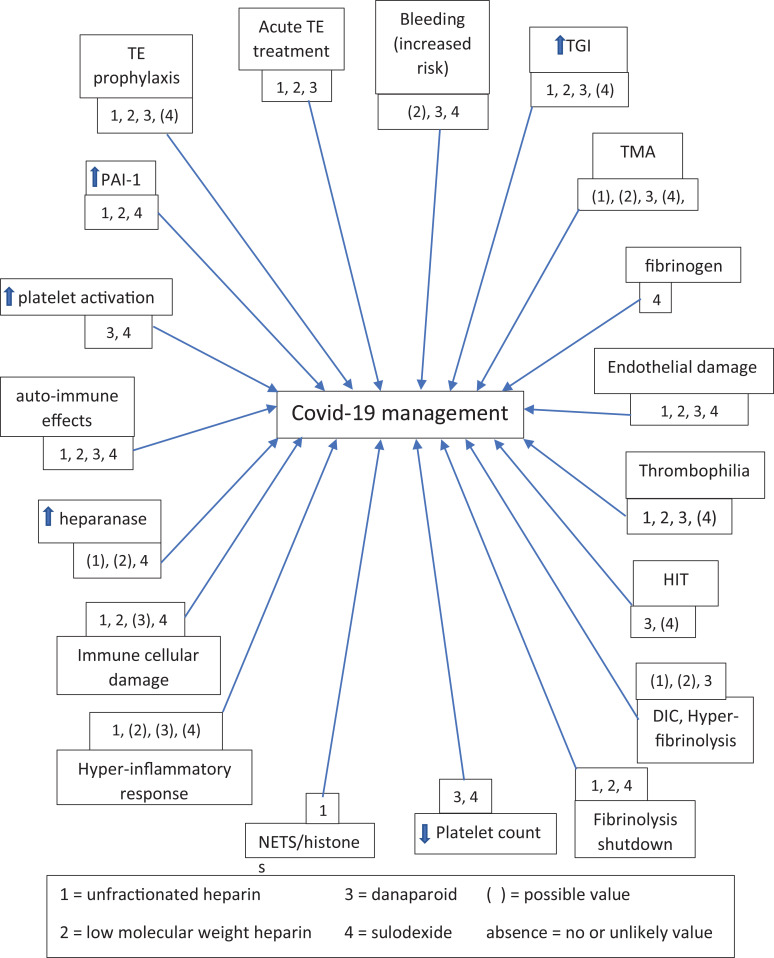
Once SARS-CoV-2 has gained entry via the lungs, the circulatory system appears to be the main target as the means of reaching the rest of the body. It does this by inducing endothelial injury, interference with the hemostasis-immune system cross-talk so that by cytokine and hypoxia induced damage it is able to invade the entire body. Antithrombotics have direct and/or indirect effects on some or all of these virally induced disruptions (see Table 1).
Table 1.
Antithrombotics With Anticoagulant and Immune Modulating Activity.
| Antithrombotic type | Anticoagulant | Immune modulation | ||
|---|---|---|---|---|
| Direct action | Indirect action1 | Direct action | Indirect action2 | |
| Direct thrombin inhibitors (DTIs) | x | x | ||
| Direct Xa inhibitors (DaXas) | x | x | ||
| Heparins (UFH & LMWHs) | (x) | x | x | x |
| Fondaparinux | x | x | ||
| Sulodexide | x | x | x | |
| Dermatan sulphate | x | (x) | x | |
| Danaparoid sulphate | x | x | x | x |
1 via a clotting cascade inhibitor, e.g. AT and/or HCII.
2 via an activated clotting factor, e.g. Factor Xa or Thrombin.
Currently the trend is toward use of LMWH, or UFH in preference to direct oral anticoagulants (DOACs) due to possible drug-drug interactions with concomitant antiviral (anti-HIV protease inhibitors such as ritonavir) and antibacterials (azithromycin).98 Such treatments interfering with drug metabolism (P450 isozymes) or drug resistance (P-gp) pathways may increase the bleeding risk or reduce the antithrombotic effect in case of DOAC use.
Glycosaminoglycans (GAGs)
Glycosaminoglycans (GAGs) consist of families of unbranched polyanions that include the heparin (HP)/heparan sulfate (HS) and chondroitin sulfate (CS)/dermatan sulfate (DS) groups. They can exist free or as carbohydrate moieties of proteoglycans attached to virtually all cell surfaces or in the extracellular matrix (ECM). They are also found in secretory vesicles in some types of cells. GAGs regulate the activity of a wide range of proteins (including chemokines, cytokines, chemotaxins, complement regulation, growth factors, enzymes, morphogens, and adhesion molecules etc.) and participate in cell dynamics, inflammation and signaling pathways. Thus they are intimately involved in routine physiology and surveillance for and responses to invasion by pathological organisms.
However, pathogens have evolved strategies that take advantage of GAGs at virtually every major portal of entry to the body to invade host cells, move from one cell to another, and protect themselves from immune attack. Thus several corona viruses are dependent on binding to cell surface HS to facilitate cell access to the ACE2 receptors.99
The different GAG families show polydispersity of chain length and chemical (micro)heterogeneity with respect to the types of hexoses, hexosamines, or hexuronic acids in each repeating disaccharide unit making up their polysaccharide chains. CS and DS are galactosaminoglycans in which the second hexose of each disaccharide is glucuronic acid in CS or its epimer iduronic acid in DS. HP and HS are glucosaminoglycans since the second hexose of each disaccharide is predominantly iduronic acid in HP or glucuronic acid in HS. In the body HP and HS represent a continuum of molecules with molecular weights ranging from 3 to 70 kDa, gradually reversing ratios of iduronic to glucuronic acid and highly sulphated to sparsely sulphated chains. The levels of sulphation and carboxylation provide an overall negative charge density of the chains, and the clustering of certain hexose units into charged and non-charged domains determines their conformation and ability to interact with specific ligands and hence their functions. Most ligands are polycationic proteins such as Antithrombin (AT), PF4, fibronectin, vitronectin, histidine-rich glycoprotein, lipoprotein lipase, complement factors C3 and C4b and apolipoproteins etc. Other ligands have small cationic domains that allow GAG binding that directs their function. For heparin, this binding to so-called heparin binding proteins limits its bioavailability both as an antithrombotic and for other functions. The GAGs in sulodexide and danaparoid have a high bioavailability because their low overall charge density and chemical structures are not conducive to binding to anything other than their main target proteins (AT and HCII).
The presence (or not), position and number of the hexose sulphation sites (2-O, 3-O or 6-O) and chain length (i.e. number of hexose units) determine the specificity and avidity of GAG binding to other molecules. Some HP and HS chains contain the highly negatively charged cluster of hexoses constituting the pentasaccharide binding site for AT. It is based around the 3-O tri-sulphated glucosamine residue essential for a ∼1000-fold increased affinity of AT for Xa and thrombin.100 However, to achieve this the chains have to be at least 15-16 hexose units long for thrombin inhibition but the pentasaccharide alone is sufficient for factor-Xa inactivation. Such differences in physico-chemical characteristics allow GAGs to maintain the integrity of interactions between cells and their intercellular matrix and influence the activities of not only the coagulation cascade but also the immune/inflammatory system in a way that can be unique to the animal, the type of GAG and its tissue location.
Endogenous HP is virtually only found in the mast cell, a highly specialized leukocyte that can adapt its phenotype and function to its local microenvironment. Mast cells store different types of mediators that carry out effector and regulatory tasks when they are released in response to external and internal stimuli and GAG mediators in turn are structurally adapted to functions specific for the tissue in which the mast cell finds itself. The gastro-intestinal tract mucosa contains the highest density of mast cells in the body. They are guardians of the intestinal barrier, regulating epithelial function and integrity, by modulating both innate and adaptive mucosal immunity, and maintaining the neuro-immune interactions essential for normal gut function and protection against invasion by the myriad of bacteria and viruses that normally make the intestine their home. Oddly, despite 30% of its chains possessing the pentasaccharide site essential for enhancing AT activity, endogenous HP does not appear to the physiological anticoagulant. Rather, it regulates the types and amount of cationic proteins stored in mast cells and by binding to endogenous AT appears to switch off its antiangiogenic activity.101
Heparan sulphates (HS) are ubiquitous, being found as proteoglycans in the extracellular matrix, basement membranes and on all cell surfaces, where they contribute to the glycocalyx. Their marked structural diversity allows interactions with many proteins and proteases to promote or inhibit their actions. Binding is closely related to the chain length, charge density and the pattern of charged and sulphated groups along the chains, and these structural characteristics and their interactions are often site-specific. They have multiple roles in inflammatory responses, participate at almost every step of leukocyte transmigration through the blood-vessel wall and in the establishment of both acute and chronic inflammatory reactions. HS appears to be the physiological counterpart of medicinal heparin102 but only 1% to 10% of its chains contain the pentasaccharide sequence required for AT binding, compared with up to 30% of HP and UFH chains. As an anticoagulant during endothelial injury HS acts principally at the EC surface and sub-endothelium where it appears to be important for control of local thrombin activity.
Dermatan sulphates (DS) are found mainly in the skin, but also in the intestinal mucosa, blood vessels, heart valves, tendons and lungs. They are attached to cell surfaces as proteoglycans and also participate in the extracellular matrix. They too are involved in wound repair103 hence the high levels in the skin, blood coagulation and the response to infection. The specific anticoagulant action of DS against thrombin is mediated via HCII.104 DS chains include a hexasaccharide, containing N-acetylgalactosamine-4-O-sulfate residues, that interacts with HCII which then binds with high affinity to thrombin at exosite I.105 This is analogous with the UFH pentasaccharide that activates AT. UFH also binds directly to both HCII and thrombin (at exosite II).106,107 Chain length is also important for maximal thrombin effect.108 DS is principally expressed on the surface of fibroblasts and vascular smooth muscle cells after injury to the adventitia. It has a higher affinity for HCII because of its specific binding site Its antithrombotic action occurs mainly at extravascular sites where it limits the extent of any local fibrin mesh required to stop bleeding when the arterial wall is breached. Although HCII is also present in the blood at a similar relatively high concentration as AT, its activation by DS does not appear to play a significant role in systemic blood coagulation but it may be important locally at extravascular sites of high thrombin generation. DS may also enhance the role of HCII in regulating local acute inflammation and wound healing, by binding a chemotactic peptide for neutrophils and monocytes that is released by leukocyte elastase and cathepsin G proteolysis,109 and in pregnancy the interaction with HCII may also have a role protecting the placenta from thrombosis.
Heparins and Heparinoids
It appears somewhat paradoxical that GAG antithrombotics, particularly HS, should be considered potentially useful in the management of patients with COVID-19 given the ways they are exploited in-vivo to the advantage of the virus. However the isolated products may differ in many ways from the GAGs that the virus exploits. Thus far the clinical experience appears to have been positive and the heparins are usually recommended.110 Many investigators seek to refine the use of GAGs based on the relationship between chemical structures and their influence on physiological function. However many of the structures used to illustrate GAGs are based on either generic formulae or cover a huge range of possibilities while it has been established that even small differences in hexose unit, charge and distribution of sulphate residues can alter the chain conformation and hence its interactions and functions.
The 4 different types of negatively charged GAG—HP, HS, DS and chondroitin sulphates, can all be found in the intestinal mucosa and extracted individually or as mixtures such as Heparin, Orgaran and Sulodexide. While the range of different chains within each product is potentially infinite, as a result of structural heterogeneity, it is considerably constrained by their isolation and purification processes aimed at providing different, reproducible products limited to well-defined mixtures of distinct ranges of GAG chains. In addition the isolation procedures themselves involving alkaline peroxide treatment, use of permanganate and hypochlorite etc. can produce their own modifications of the length and fine structure of the GAG chains.100 Thus the proportions of the different types of GAGs and their spectrum of chains in the isolated products does not reflect their relationship in the tissue of origin. A preparation of any one proteoglycan (defined by its core protein) represents a diverse population of molecules, each potentially representing a unique structural entity.111
Table 2 summarizes some physico-chemical characteristics of these therapeutic mixtures. As would be expected, apart from molecular weight the LMWHs are most similar to UFH, but sulodexide and danaparoid differ considerably in many respects from UFH and from each other.
Table 2.
Physico-Chemical Characteristics.
| Heparin | LMWHs | Sulodexide | Danaparoid | |
|---|---|---|---|---|
| MWave (Da) | 15,500 | 3,600-6,500 | 7,0001 | 4,5002,3 |
| HP | 97-100% | 97-100% | 80% | -- |
| HS | -- | -- | -- | 84% |
| DS | trace | trace | 20% | 12% |
| CS | trace | trace | -- | 4% |
| Iduronic/Glucuronic acid ratio | high | high | high | low |
| Sulphates/ hexosamine | 1.8-2.4 | 1.8 | <1.8->0.6 | <0.64 |
| SO3 - to COO- ratio3 | 2.1-2.8 | 2.1-2.8 | nd | 1.2-1.3 |
| N-sulphation | yes | yes | yes | no |
| 2-O, 3-O desulphated GAG chains | (yes) | (yes) | nd | yes |
| 6-O desulphated GAG chains | (yes) | (yes) | nd | low |
| Anti-Xa to Anti-IIa activity ratio | 1 | 3-10 | 0.5 | >22 |
| AT activating fraction (w/w%) | 30 | 20 | 20 | 4 |
| HCII activating fraction (w/w%) | v. low | v. low | 20 | 12 |
1 HP MWave = 7000 Da, DS MWave = 25,000 Da.
2 HS MWave = 3400 Da, DS MWave = 6600 Da.
3 ref 111.
4 due to its isolation procedure the HS in danaparoid is not typical of HS in general since its MWave is < 10 KD.
HP = heparin sulphate chains, HS = heparan sulphate chains, DS = dermatan sulphate chains, CS = chondroitin sulphate chains. Brackets refer to ≤5% for DS and CS or “low” for desulphated chains.
They would appear to represent reasonably distinct parts of the GAG spectrum of molecules. In addition 95% of the HS in danaparoid differs greatly from the endogenous HS that binds to viruses in that its chains are much shorter, and its overall charge density much lower (due to the low degree of sulphated and acid side chains).
Commercial HP (i.e. UFH) is isolated with a high overall charge density and contains a much higher sulphate content and iduronic acid to glucuronic acid ratio and a higher number and ratios of SO3 - to COO- and 3-O sulphates to 6-O and 2-O sulphates compared with HS. It is virtually devoid of DS and CS (total <3%). The LMWHs being post-extraction derivatives of HP are similar to HP but of shorter chain length.
Danaparoid is extracted as a low molecular weight mixture of HS (85%) with about 12% DS and traces of CS. Despite removal of HP chains a small HS subfraction (the high affinity HS (HA-HS)), 5% by weight of the total HS and 4% of the total mass of danaparoid) is more highly sulphated because it contains the pentasaccharide site for binding AT, whereas the remaining 80% HS (the no affinity HS (NA-HS)) does not.112 This specific sequence contains most of the small amount of iduronic acid of danaparoid sodium and gives the HA-HS a higher degree of sulphation and overall negative surface charge density than the rest of the heparan sulphate chains of danaparoid that do not bind AT. The remainder of the HS in danaparoid has a low sulphate and overall negative charge density, hence is totally unlike the body’s HS physiological anticoagulant. Danaparoid unlike sulodexide and the heparins is not an anticoagulant because it hardly affects the routine clotting tests (aPTT, PT and TT) at recommended therapeutic dosing levels (2500-4800 U/day).
The extraction method of Sulodexide isolates a mixture of 2 GAGs. An electrophoretically fast moving heparin constitutes 80% of the product. It has a lower degree of sulphation than native HP chains, a low MWave of 7000 Da, and more resembles a heparin than a heparan (which it is often called) due to its relatively high iduronic acid content. The other fraction is a DS (20%) with a high MWave of 25,000 Da. This DS appears to be more active than that of danaparoid perhaps because of its greater chain length, however, it is not clear if all DS chains possess the HCII binding site or like UFH binding to AT, only a portion of its chains is involved.
Tables 3 and 4 summarize the physiological activity of the 4 GAG antithrombotics. Note that while danaparoid elimination from the circulation is independent of the administration route the value is highly dependent on the activity under assay. Thus the mean t½ for a-Xa activity = 24.5 h, for anti-IIa activity = 4.3 h and TGI = 6.7 h. Only the last represents the total effect of danaparoid on the clotting cascade.
Table 3.
Comparison of Main Mechanisms of Action and Pharmacokinetics.
| UFH | LMWH | Sulodexide | Danaparoid | |
|---|---|---|---|---|
| Coagulation cascade inhibition: | ||||
| Co-factor dependent | IXa, Xa, XIa, IIa | Xa, IIa | Xa, IIa | Xa, (IIa) |
| Co-factor independent | IXa | IXa | -- | IXa |
| Potency in buffer: | ||||
| anti-Xa |
193 IU/mg |
80-120 IU/mg |
90-105 USP U/mg |
18 U/mg1
|
| anti-IIa | 193 IU/mg | 35-45 IU/mg | 180 IU/mg | <1.0 U/mg1 |
| Administration route | IV, SC, Nebulized | IV, SC, Nebulized | IV, SC, PO, IM | IV, SC, Nebulized |
| Inhibits thrombin activity | yes | yes | yes | very weak |
| Inhibits thrombin generation | yes | yes | weak | Yes |
| Activates platelets | yes | (yes) | no | No |
| Increases fibrinolysis | yes | yes | yes | No |
| AT concentration sensitive | yes | yes | nd | (no)2 |
| Bleeding risk | at high doses | low | low | low |
| Bioavailability | IV 20-30% | IV 85-95% | 90% (IM), 50% (PO) | IV ∼100% |
| Elimination half-life IV (hours) | 1.5 (a-Xa) | average 4.0 (a-Xa) | 12 (mg)3 | 6.7 (TGI) |
| Elimination route | RE system | Renal 10-40% | hepato-renal4 | Renal >50% |
AT = Antithrombin, IU = International unit, U = anti-Xa unit, IM = intramuscular, IV = intravenous, PO = per os, SC = subcutaneous.
1 for danaparoid assay in buffer U and IU are interchangeable.
2 in one study of PVT treatment113 found less efficacy of danaparoid if AT <50%.
3 mg = 10 Lipesic units, t½ i.v. = 11.7h, i.m. = 7,7h, p.o. 50 mg = 18.7h and 100 mg = 25.8h (no indication whether this is anti-Xa or anti-IIa activity).
4 metabolized in the liver, excreted by the kidneys.
Table 4.
Comparison of Additional Pharmacodynamic Actions.
| UFH | LMWH | Sulodexide | Danaparoid | |
|---|---|---|---|---|
| TFPI release | Yes | yes | yes | (low) |
| Clotting test prolongation1 | aPTT,PT,TT,HepT | aPTT,PT,TT,HepT | (aPTT,PT) TT,HepT | HepT |
| Inhibition of clot extension | yes | yes | nd | yes |
| Inhibition of clot bound IIa | at v high doses | no | yes via HCII | no |
| Increase clot permeability2 | yes | no | no | yes |
| Primary hemostasis inhibition | yes | yes | yes | no |
| Maintains APC levels | at low doses | at low doses | nd | yes |
| Rebound thrombosis may occur | yes | yes | nd | no |
| “Heparin” resistance | Common5 | nd | nd | very low6 |
| Reduces plasma viscosity | yes | yes | yes | nd |
| Lipoprotein lipase release | high | high | high | low3 |
| C-R4 with H:PF4 antibody | high | high | intermediate | low (if any) |
C-R = cross reactivity with the platelet activating heparin:PF4 antibody, IIa = thrombin.
1 aPTT, PT and TT thrombin times depend on thrombin inhibition, the HepT (Heptest) measures anti-Xa and anti-IIa activities.
2 increases plasmin access within the thrombus.
3 <25% of the lipolytic activity released by UFH.
4 serological cross-reactivity.
5 in patients with COVID-19 infection.
6 described rarely in patients with HIT.
All products have been shown to reduce endotoxin injury, pro-inflammatory cytokine release, endothelium/glycocalyx/tissue injury, reperfusion injury, PAF and burns/smoke inhalation injury, growth factor production/cell proliferation, immune-modulatory activities to varying extents. The differences in structure and chains length of these GAGs is reflected in their effects on plasma anti-Xa: anti-IIa activity ratios. However, these ratios are not directly reflected in their antithrombotic activity since all have about the same inhibitory action on thrombin generation and antithrombotic potency at therapeutic dosing levels, but some studies have shown superiority of sulodexide and danaparoid compared with some LMWHs.112-115 Part of this is due to the high level of antithrombin activity of the DS fraction of sulodexide and the direct inhibition of a major thrombin feed-back loop via factor-IXa by the NA-HS subfraction of danaparoid.
All 4 preparations have been shown in-vitro and, to a lesser extent, in vivo to have some direct or indirect anti-inflammatory/immune modulatory actions summarized in Table 5.
Table 5.
GAG Immuno-Modulator Effects at Therapeutic Dose Levels.
| GAG inhibits or attenuates: | Heparin | LMWHs | Sulodexide | Danaparoid |
|---|---|---|---|---|
| Endotoxin lung injury1 local coagulopathy | yes | yes | nd | yes |
| Inflammation | no | no | nd | no |
| Fibrinolysis | no | nd | nd | no |
| systemic coagulopathy | yes | nd | nd | yes |
| PAF induced injury | yes | yes | nd | yes |
| Reperfusion injury | Yes | yes | yes | yes |
| Anti-inflammatory | Yes | yes | yes | yes |
| Endothelial glycocalyx damage | (yes) | (yes) | yes | yes |
| Free histone inactivation | yes | yes | nd | yes |
| Growth factor production | yes | yes | yes | yes |
| Interferon | yes | yes | nd | yes |
| Tumor cell growth | yes | yes | nd | (yes)3 |
| Burn/smoke inhalation injury | yes | yes | nd | yes |
| Endothelium (barrier) injury | yes | yes | yes | yes |
| Intimal hyperplasia after arterial injury | yes | (yes) | yes | (yes) |
| Cell proliferation | yes | yes | yes | yes |
| Heparanase inhibition | yes | yes | yes | no |
| Angiogenesis | yes | yes | yes | yes |
| Annexin binding2 | yes | yes | nd | yes |
| Tissue protection and repair | yes | (yes) | yes | nd |
| Leukocyte activation and adhesion | yes | yes | yes | yes |
| NETosis | yes | yes | nd | nd |
| Heparin | LMWH | Sulodexide | Danaparoid | |
| Heat stroke | yes | yes | nd | yes |
| Organ damage | yes | yes | yes | yes |
| Effects of HMGB-1 | yes | yes | nd | yes |
| Immune complex binding to GBM | yes | yes | yes | (yes) |
| Virus transduction | yes | (yes) | nd | weak4 |
| Spontaneous “HIT” induction | yes | yes | nd | no |
| Inhibits HIT antibody interactions | no | no | nd | yes |
1 after nebulized inhalation.
2 however highly dependent on the specific annexin & degree of sulphation of the GAG involved.
3 effect appears to be tumor dependent.116
4 single report using recombinant adeno-associated virus- type 2.117
nd-no data, brackets indicate action occurs under certain circumstances or is weaker.
To some extent the results of these anti-inflammatory immune modulatory studies reflect the functional role of these GAGs at their site of origin, i.e. the intestinal mucosa which may not correspond with the test situation and may only be of relevance in patients with predominantly gastro-intestinal effects of COVID-19. However, nebulized danaparoid is able to attenuate the effects of acute lung injury similar to AT and APC. Danaparoid was the only one showing systemic anticoagulant effects118 due possibly to its lower MWave (4.5 kD compared with 56 and 58 kD for AT and APC respectively) allowing access to the bloodstream. Furthermore, the inter-GAG product differences relate to their specific ranges of physico-chemical structural characteristics as determined by their extraction processes.
Additional studies with synthetic or chemically modified GAGs have also shed light on structural requirements in terms of sulphation sites for some their actions:
6-0 sulphate group is required for angiogenesis, anti-inflammatory actions of heparin via its interaction with selectins, and anti-Xa activity of heparins, especially if the 2-O and 3-O sulphate groups are removed,119 and anti-proliferative potency,120
non-sulphated GAGs inhibit inflammation, cancer growth and spread, and heparanase activity,
removal of 2-O and 3-O sulphation from heparin reduces HMGB-1 secretion and prevents neutrophil elastase mediated airways inflammation,121
3-O and 6-O sulphation supports heparanase activity while the 2-O sulphate group on a uronic acid122 is required for its substrate recognition,123
3-O sulphation is required for hepatic binding and subsequent elimination of heparin.124 3-O sulphation of native high molecular weight HS is also important for entry of some viruses into cells125,126 and increases the affinity of heparin for AT,102
2-O sulphation is required for hepatic uptake of lipoproteins,127 and PF4 binding.128,129
N-sulphation is important for Respiratory Syncytial virus infection,130,131
a higher negative charge density level and MW >17 kDa are required for endometrial differentiation,132
the heparin binding site on AT is essential for its angiogenic activity and is blocked by (GAGs with) the specific pentasaccharide required for acceleration of its antithrombin activity,101 and for its inhibition of MASP-1 and 2133
various O sulphation patterns facilitate entry of different viruses into cells,126
non-AT binding heparin chains prevent the damaging effects of histones in- vivo,50
N-desulphated heparin and heparin and LMWH can reduce Ig and complement deposition in glomerular capillaries in susceptible mice.134
GAG-ligand binding is predominantly ionic, but hydrogen bonding is also important while hydrophobic forces play a minor role.135 However, the fine structure and pattern of distribution of sulphation sites along the chains essential for specific interactions of the heparins and heparinoids with the coagulation and immune systems have not been so precisely defined. Despite this, based on structural requirements, the relatively low content of 2-O, 3-O and 6-O-sulphated chains in danaparoid might promote heparanase inhibition,116 but a direct study v UFH in a mouse cancer model did not confirm this.136 However, the dose of heparin used in the latter study was 4 times that of danaparoid in terms of daily anti-Xa units administered, but it would have been more relevant to compare multiples of antithrombotic doses (for the mouse) since that is what dosing will be based on in COVID-19 patients. In addition, the GAG chains of danaparoid may be too short and/or mouse might be an inappropriate model.117
In another set of experiments137 anti-viral activity, studied as inhibition of rAAV binding to cell-membrane-associated HS, was 80% with therapeutic concentrations of UFH, but equipotent anti-Xa levels of LMWH and danaparoid only achieved <40% and <20% inhibition respectively, while lepirudin had no effect. The results suggest that a high negative charge and possibly longer chain length are essential for blocking or displacing viral interaction with the HS, but they might not necessarily extrapolate to COVID-19 despite the virus exploiting local HS to facilitate cell internalization by attachment to ACE2 receptors. This is because the high PF4 levels in COVID-19 could block this and other actions of heparin. Based on the overall information all 4 candidates appear to possess some characteristics that might favor their use in COVID-19.
Without direct comparison in the same test systems a realistic ranking of their suitability based on the results shown is not possible. In addition, extrapolation to desirable clinical outcomes of GAG treatment is confounded by the mix of in-vitro or in-vivo experiments and by: using different experimental conditions, e.g. tissues v whole animals that include species with different responses to the same stimulus (guinea-pig, mouse, rat, rabbit, monkey etc.),117 not distinguishing between results of male and female animals, using different triggers to elicit the supposedly “same” inflammatory response and using different administration routes, different dosing intensities and duration, different times of response evaluation, different methods of response evaluation and finally often basing the GAG dosing on human pharmacokinetics that may be totally inappropriate for the animal model used.
Many of these differences in animal studies also apply to the human experience, especially the use of healthy volunteers, effect of gender and age, type and stage of disease and influence of organ dysfunction, dosing intensity and duration. All the GAG antithrombotics under review have been shown in various animal models and ex-vivo studies with patients to ameliorate or prevent tissue damage and promote repair after exposure to specific damaging agents. With a human breast cell cancer model Fluhr and colleagues138 found an effect of heparin and various LMWHs on Interferon-γ-inducible cytokines that might be harmful to tumor-immune interactions but since this was not evident for danaparoid they concluded it might be a better antithrombotic without negative side-effects on chemokines in breast cancer patients. But are such observations of relevance to the almost chaotic consequences of the immunological problems that arise during COVID-19? Thus with the above caveats in mind Table 6 summarizes clinical outcome experience in patients.
Table 6.
Positive Treatment Experiences With GAG Antithrombotics.
| Safe use in: | Heparin | LMWHs | Sulodexide | Danaparoid |
|---|---|---|---|---|
| Pregnancy and lactation | pregnancy | pregnancy | limited data | both |
| Pediatrics | yes | yes | nd | yes |
| Routine VTE prophylaxis and treatment | yes | yes | little data | yes |
| Arterial TE prophylaxis and treatment | both | both | nd | both in HIT |
| Hemorrhagic states | moderate | moderate | good | good |
| AKI & CKI for HD or CRRT | yes | yes | yes | yes |
| Moderate/severe hepatic dysfunction | yes | yes | nd | yes |
| DIC treatment | (yes) | (yes) | nd | yes |
| Hyperfibrinolysis syndrome treatment | yes | yes | nd | yes |
| HIT antibody cross-reactivity (in & ex vivo) | high | intermediate | intermediate | very low1 |
| HIT treatment | no | (yes) | limited data | yes |
| Thrombotic microangiopathy (TMA) | (yes) | (yes) | nd | yes |
| Burns patients | yes | yes | nd | yes |
| Improved survival in cancer | yes | yes | (yes)2 | nd |
| Virus induced mortality reduction | yes | yes | nd | nd |
| ARDS mortality reduction | yes | yes | nd | nd |
1 true frequency unknown & reported frequency confounded by residual or concomitant heparin, underdosing.
2 no direct data but possibly on the basis of heparanase inhibition.
3 possibly on the basis of structural requirements for heparanase inhibition by GAGs.
() = some effect but not first-line treatment.
The bracketed responses in Table 5 either indicate a weaker effect or data limited to a specific cancer. Clinical trial and routine real-world experience have shown that all 4 products are safe and effective for thrombosis prevention and treatment when used at recommended dosing regimens. However, in extreme clinical situations differences appear that may have a bearing on their suitability for use in COVID-19 patients, particularly in the later, more severe stages of the infection.
Overall Tables 1 -6 reveal some interesting differences and similarities in product characteristics that could impact on their potential value in COVID-19. Figure 2 illustrates which of these GAG antithrombotics (in the assessment of the reviewer) might have a positive, moderate (bracketed) or no/unlikely (absent from the box) influence on the proposed management target.
Figure 2.
Potential value of the 4 GAG antithrombotics in the management of COVID-19 infection. In vitro and in vivo actions demonstrated for various GAG antithrombotics in relation to potential use in the management of COVID-19 infection and its complications.
The overall “scores” for each product are summarized in Table 7 (based on Figure. 2).
Table 7.
Summary of Possible Treatment Values Form Figure 2.
| GAG antithrombotic | Potential treatment value1 | ||
|---|---|---|---|
| Likely value | Possible value | No or unlikely value | |
| Unfractionated heparin | 10 | 3 | 5 |
| Low molecular weight heparin | 9 | 5 | 4 |
| Sulodexide | 9 | 7 | 3 |
| Danaparoid | 13 | 2 | 4 |
1 assessed from Figure 2 based on reported clinical experience.
Heparin is known to change the immunogenicity of many proteins to which it binds and allosterically alters.139 It also has multiple effects on immune and inflammatory responses, inhibits NETosis,140 is a powerful antithrombotic and for safety reasons (bleeding risk especially if thrombolytics are required) is preferred over the LMWHs.141 Hence it would appear to be an ideal for use in severely ill COVID-19 patients were it not for the possibility of causing HIT, and the requirement for therapeutic dosing for anticoagulation142 and most of the actions that might benefit COVID-19 patients. These higher dosing levels might increase its tendency to induce bleeding and HIT particularly in patients admitted to the ICU. The LMWHs offer a similar palate of therapeutic advantages and disadvantages. On the other hand both sulodexide and danaparoid appear to induce less bleeding in high risk situations and neither has so far been reported to cause spontaneous HIT. Sulodexide has the stronger antithrombin activity, via activation of HCII by its high molecular weight DS chains, whereas danaparoid inhibits thrombin generation via a combination of acceleration of AT inhibition of Factor Xa and inhibition of thrombin activation of Factor IX. Oral sulodexide (v placebo) and i.v. danaparoid (v UFH) have been shown to be effective for the long-term prevention of recurrent VTE after standard therapy and for the treatment and short term (3 months) prevention of recurrence in patients presenting with an acute VTE, respectively. Danaparoid is approved for VTE prevention and in Japan for DIC treatment. Both drugs have extensive use in renal disorders-sulodexide in diabetic patients and danaparoid in HIT patients requiring ECC use. Both reduce the proteinuria associated with vascular angiopathy and prevent complement binding to the GBM in renal disorders, prevent reperfusion injury, angiogenesis, organ damage and protect the endothelium.
Table 8 summarizes the main differences between sulodexide and danaparoid. Despite their long half-lives and lack of an antidote sulodexide and danaparoid are safe in terms of bleeding with only small differences from the best of the LMWHs.
Table 8.
Summary of Main Clinical Differences Between Sulodexide and Danaparoid.
| Potential risk situation | Of potential value based on clinical experience | |
|---|---|---|
| Danaparoid | ||
| DIC/hyperfibrinolysis | unknown | yes |
| Increased heparin-binding proteins/heparin resistance | unknown | yes |
| HIT | unknown | yes |
| DIC | unknown | yes |
| Reduced AT levels | unknown | yes |
| Increased platelet sensitivity and activation | (yes) | yes |
| Excessive thrombin | yes | yes |
| Excessive thrombin generation | (yes) | yes |
| Transplant associated thrombotic microangiopathy | nd | yes |
| Heparanase activity | yes | no |
| Mainly acute or chronic disorders | chronic | acute |
| Long half-life1 | yes | yes |
| Hepatic dysfunction/failure | no | yes |
| Renal dysfunction/failure | yes | yes |
| Bleeding risk | yes | yes |
| Thrombophilia | (yes) | yes |
| Clear dosage regimen available | no | yes2 |
1 for sulodexide half-life is dose and administration route dependent, for danaparoid half-life is independent of both. For sulodexide no half-life data for individual components, for danaparoid half-life of individual components known (Table 3).
2 therapeutic i.v. infusion regimen following an i.v. loading dose for all patients.
The heparins appear to suppress thrombin generation more strongly than danaparoid and hence APC production is also reduced resulting in the reported “rebound thrombosis” that can occur following treatment discontinuation).143,144 Danaparoid with its very low anti-IIa activity of danaparoid, and relatively low anti-Xa potency compared with the heparins allows sufficient thrombin to be generated, even at therapeutic levels, for normal APC generation and hence is not associated with “rebound thrombosis.”
Discussion
The effects of COVID 19 infection are full of unpleasant surprises in part due to the direct effect of the virus taking over essential cell receptors, in part due to its attack on the vascular system as a way of accessing the rest of the body and in part due to the confusion it sows in the body’s 2 important defense mechanisms—the immune and hemostasis systems. The latter 2 systems normally co-operate in such a way that intrusive threats are managed with no or little damage to the host. However, progression of COVID-19 is governed by the viral load, virulence and specific risk host factors that in turn determine the interplay and its extent between specific tissue and systemic reactions. Many participants in these reactions are Janus molecules with both protective and damaging actions. Which action predominates depends on the balance between their concentration and that of often many interacting species, but the SARS-CoV-2 virus is able to use them to increase its invasiveness and virulence. Subjects requiring hospital admission for COVID 19 infection already have to some extent dysregulation and disruption of the body’s defense systems, particularly in the lungs or GI tract, which if not treated urgently and effectively can rapidly spread to other organs. Thus early recognition and preventative treatment are required to reduce the need for hospital admission or limit the period required in hospital.
Of the many potential drug treatments available for SARS-Cov-2 infection, it would appear that the natural GAG antithrombotics, including heparins and heparinoids, might offer special advantages because they combine anticoagulant with immune-modulating activities that are both dependent and independent of each other. Although their immune modulatory activities are largely based on animal experiments or surrogate end-points in healthy volunteer and fewer patient studies, there is a possibility that they might seriously reduce morbidity.110 They also have the advantage of being relatively cheap compared with other products with similar actions. This is particularly important in poorer countries and socio-economically deprived communities, in many other countries, who have high infection rates. African, Native and African American, Hispanic and Indian communities are disproportionately represented in these communities and suffer more disease and greater disease severity due to poor nourishment and crowded conditions. They also have a higher risk of hypertension, obesity, non-insulin dependent diabetes mellitus. As a result they are more prone to SARS-CoV-2 infection and are disproportionately represented in the number of hospital admissions, ICU occupancy and deaths from COVID-19.145,146
Demonstration of various immune-mediated activities and their relationship to the physicochemical characteristics of either pure synthetic or GAG mixtures on both the macro scale, i.e. chain length and constituent hexoses, and micro scale, i.e. degree and clustering of side chain sulphate and acid groups, does not mean efficacy will or can follow in the disease setting. This is because of the great heterogeneity of GAGs, and variability of their interaction with their ligands in different tissues and organs and between different animal species117 used for most of the non-human experiments. Thus information of their effects on relevant clinical outcomes, such as prevention of disease progression, organ preservation, restoration of organ function, adverse events generally and mortality rate in particular, can only be obtained from clinical trials.
Furthermore, the chemical effects of and physicochemical restrictions imposed by the extraction procedures (required to remove many kinds of contaminant) have created end products consisting of unphysiological GAG mixtures with anticoagulant and immune-modulatory actions that likely differ from those of the original GAG chains in their tissue of origin. Therefore efforts are now being made to (semi)synthesize made-to-measure GAGs with less variability and more reproducible chemical content that can either be used singly or as well defined mixtures in given clinical scenarios. However, there is also a real possibility that GAGs (single types or mixtures) with immune-modulating and antiviral activity but safer anticoagulant activity, are being left behind in the tissues of origin or discarded during the isolation of heparin and the heparinoids. However, with the urgent need to identify possible treatments for COVID-19 infections the focus is currently on what is available now—UFH, LMWHs, sulodexide and danaparoid. As “combination therapy” they offer a worthwhile attempt at ameliorating the effects of COVID-19. A recent review of potential candidates considered danaparoid as the most appropriate for clinical exploration in COVID 19 patients.147 However consideration of the potential value of in-vitro and in-vivo evidence suggests 2 products: sulodexide and danaparoid, that appear to offer less risk than the heparins of:
Spontaneous development of HIT,
Cross-reactivity with any HIT or HIT-like anti-platelet antibody (although the risk appears higher with sulodexide than with danaparoid148),
Bleeding in high risk situations (both have low bleeding inducing capacity despite the fact that sulodexide does149 and danaparoid does not150,151 affect platelet activation/aggregation (a surrogate for primary hemostasis).
More immunological information is known for sulodexide than for danaparoid.152-155 Both products are reported to reduce angiopathy and both effectively reduce proteinuria in diabetic kidney disease although they appear to do so by different mechanisms—heparanase inhibition by sulodexide156 and HS replacement by danaparoid,157,158 although the picture is incomplete. Much data on immunogenic activity particularly for danaparoid including its effect in blocking the HIT antibody,159 is based on in-vitro studies, animal experiments, small pilot studies or extrapolated from structure/effect results from experiments with (semi)synthetic or chemically modified (e.g. desulphated at various sites) GAGs. Some activities of sulodexide and danaparoid may favor treatment of the hemostasis complications of COVID-19 but may not favorably impact anti-inflammatory activity. Danaparoid has virtually no effect on platelet activation except for a weak inhibition of thrombin as a platelet agonist (hence its low bleeding inducing capacity and lack of interference with primary hemostasis), but the high level of platelet activation from many sources in COVID-19 (see Figure 1) is one of the drivers of the hyper-inflammatory reaction. Hence danaparoid, at least, may require adjunct use of anti-platelet therapy. However, as well as evidence of a unique immune modulating activity in patients with HIT,159,160 therapeutic dosing with danaparoid has been used successfully to treat acutely ill patients161,162 and problems similar to those that complicate COVID-19, e.g. DIC163–165 (including a hyperfibrinolytic variant166), HIT,167 patients with renal168–170 and varying degrees of hepatic failure in patients with cirrhosis, or hepatoma complicated by portal vein thrombosis113,171,172 and patients with autoimmune diseases (such as PNH173,174 and SLE/APL syndromes175,176) and also to prevent chemotherapy-induced TMA177,178 that like viral associated TMA also appears to be complement mediated.179 Encouragingly, for many drugs in the past extrapolation from even in-vitro experimental data has yielded successes for many clinical problems. Hence the immune-modulatory data derived from animals and use of surrogate end-points in clinical studies for both danaparoid and sulodexide should be viewed in that light, even though the balance and level of information available about the anticoagulant and immune-modulatory activities for these 2 products is very different. Once a patient develops the first symptoms and signs of COVID-19 infection there is a need for a treatment strategy preferably aimed at prevention of the acute, serious clinical challenges the virus poses. Many hospitalized patients already present with serious complications that require urgent therapeutic intervention. Despite the advice of the ISTH,180 but in keeping with data from COVID-19 patients treated with UFU or LMWH,72 data from in-vitro studies and experience in the treatment of acute HIT181,182 and ICU patients,161–165,167 therapeutic infusions of danaparoid would appear to be the best approach for all COVID-19 patients, unless there is a high risk of bleeding (exacerbation). It is not clear from publications what the optimal dose and administration route of sulodexide should be. The extremes of clinical presentation of COVID-19 infection will require different management strategies and only randomized clinical trials will determine whether or not either antithrombotic can prevent or ameliorate complications. Obviously, all the factors identified cannot be controlled for in a single study but the urgency of the current situation with COVID-19 demands hard end-point answers e.g. prevention of death and organ failure, correction of fibrinolysis shutdown or DIC, correction of thrombocytopenia and platelet activation, restoration of blood-flow to hypoxic areas, reduction in ICU stay etc. as soon as possible. The need to either “kill” the virus or reduce the viral load not only in diseased patients but also in asymptomatic subjects to reduce their chance of transmitting SARS-CoV-2 to susceptible individuals means that whichever antithrombotic is used it will be part of a “cocktail” including steroids, antiplatelet drugs, anti-viral therapy and thrombolytics required to control COVID-19.183
Figure 1.
Some of the many potential consequences of “cross-talk” disruption in COVID-19 infection. This figure shows some of the many potentially pathological consequences of cross-talk breakdown between the immune/inflammatory and hemostasis systems that some of the more severely affected COVID-19 patients develop. It reflects the chaos that develops both locally and systemically when the body’s defenses can no longer match the damaging effects of the virus. APC = activated Protein C, DIC = disseminated intravascular coagulation, HIT = heparin-induced thrombocytopenia, HS = heparan sulphate, PAI-1 = plasminogen activation inhibitor, PF4 = platelet factor 4, TAFI = thrombin activated fibrinolysis inhibitor, TMA = thrombotic microangiopathy.
Conclusion
It is clear that both disruption of immune reactions to inflammatory responses and hemostatic changes play a great role in the development of severe morbidity in COVID-19. While many drugs may prevent one or other of the responses those that combine both actions, such as many of the currently available GAG antithrombotics, may offer more effective and safer prophylaxis and/or treatment. Given the extreme complexity of the immune and hemostasis interactions to infection by the COVID-19 virus it is probably unlikely that a single GAG antithrombotic with immune-modulatory activity could fit into the management plan for all patients. Two possible GAG candidates, taking-into-account their safety in comparison with the heparins, are sulodexide and danaparoid with (possibly) different effects on hemostasis and the immune/inflammatory systems. Animal and ex-vivo/in-vitro experiments offer useful information but direct extrapolation to infected patients is confounded by uncertainties concerning whether either of these purified antithrombotics compares chemically and physiologically with their natural unextracted counterparts, tissue specificity of structure/function relationships and species differences in responses to the various stimuli used to mimic the pathophysiological changes seen in patients. While both drugs on paper offer interesting insights danaparoid has been used in more of the acute critical clinical situations that arise in COVID-19 infection than sulodexide. The other advantage is their relatively low cost. Whether sulodexide would be more useful in the early stages as preventative therapy and danaparoid more useful once complications are threatening or emerging, or indeed neither or both eventualities, requires a well-designed clinical trial that includes the whole clinical spectrum of COVID-19 patients otherwise treated according to accepted recommendations for the extent and severity of their disease.183
Acknowledgments
I would like to thank Professor J Fareed and Dr C Carter for their encouragement and excellent advice.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The author led the clinical development of danaparoid sodium until his retirement in 1999 and has since worked as an independent clinical consultant with an interest in anticoagulants.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Harry N. Magnani  https://orcid.org/0000-0001-8357-8286
https://orcid.org/0000-0001-8357-8286
References
- 1. Mycroft-West CJ, Su D, Li Y, et al. Glycosaminoglycans induce conformational change in the SARSCoV-2 Spike S1 Receptor Binding Domain. 2020. doi:10.1101/2020.04.29.068767
- 2. European Centre for Disease Prevention and Control. Clinical characteristics of COVID-19 ISARIC COVID-19 Database. 2020. [Google Scholar]
- 3. Ampomah PB, Kong WT, Zharkova O. Annexins in influenza virus replication and pathogenesis. Front Pharmacol. 2018;9:1282 doi:10.3389/fphar.2018.01282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Capila I, Herniaz MJ, Mo YD, et al. Annexin V-heparin oligosaccharide complex suggests heparan sulfate mediated assembly on cell surfaces. Structure. 2001;9(1):57. [DOI] [PubMed] [Google Scholar]
- 5. Price E. Could the severity of COVID-19 be increased by low gastric acidity? Crit Care. 2020;24(1):456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Foley JH, Conway EM. Cross-talk pathways between coagulation and inflammation. Circ Res. 2016;118(9):1392 doi:10.1161/CIRCRESAHA.116.306853 [DOI] [PubMed] [Google Scholar]
- 7. Chen L, Deng H, Cui H, et al. Inflammatory responses and inflammation associated diseases in organs. Oncotarget. 2020;9(6):7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Henry BM, Vikse J. Clinical characteristics of COVID-19 in China. N Engl J Med. 2020;382(19):1859 doi:10.1056/NEJMc2005203 [DOI] [PubMed] [Google Scholar]
- 10. Guan GW, Gao L, Wang JW, et al. Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia. Chin J Hepatol. 2020;28(2):100 doi:10.3760/cma.j.issn.1007-3418.2020.02.002 [DOI] [PubMed] [Google Scholar]
- 11. Qiu H, Wander P, Bernstein D, Satapathy SK. Acute on chronic liver failure from novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Liver Int. 2020;40(7):1590–1593. doi:10.1111/liv.14506 [DOI] [PubMed] [Google Scholar]
- 12. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;393(10234):1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zehnder J, Galli S. Mast-cell heparin demystified. Nature. 1999;400(6746):714–715. doi:10.1038/23360 [DOI] [PubMed] [Google Scholar]
- 14. Merrill JT, Erkan D, Winakur J, James JA. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol. 2020;16(10):581–589. doi:10.1038/s41584-020-0474-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Clarke D, Katoh O, Gibbs RV, Griffiths SD, Gordon MY. Interaction of interleukin 7 (IL-7) with glycosaminoglycans and its biological relevance. Cytokine. 1995;7(4):325 doi:10.1006/cyto.1995.0041 [DOI] [PubMed] [Google Scholar]
- 16. Kolarova H, Ambruzova B, Sindlerova L, Klinke A, Kubala L. Modulation of endothelial glycocalyx structure under inflammatory conditions. Mediators Inflamm. 2014;2014:694312 doi:10.1155/2014/694312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haeger SM, Yang Y, Schmidt EP, et al. Heparan sulfate in the developing, healthy, and injured lung. Am J Respir Cell Mol Biol. 2016;55(1):5–11. doi:10.1165/rcmb.2016-0043TR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine storm’ in COVID-19. J Infection. 2020;80(6):607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Magro C, Mulvey JJ, Berlin B, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Van de Veerdonk FL, Netea MG, van Deuren M. Kallikrein-kinin blockade in patients with COVID 19 to prevent acute respiratory distress syndrome. eLife. 2020;9:e57555 doi:10.7554/eLife.57555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Java A, Apicelli AJ, Liszewski KM, et al. The complement system in COVID-19: friend and foe? JCI Insight. 2020;5(15):e140711 doi:10.1172/jci.insight.140711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sobczak AIS, Pitt SJ, Stewart AJ. Glycosaminoglycan neutralization in coagulation control. Arteriosclerosis Thromb Vasc Biol. 2018;38(6):1258–1270. doi:10.1161/ATVBAHA.118.311102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Conway EM. Thrombomodulin and its role in inflammation. Semin Immunopathol. 2012;34(1):107 doi:10.1007/s00281-011-0282-8 [DOI] [PubMed] [Google Scholar]
- 24. Mosnier LO. Platelet factor 4 inhibits thrombomodulin dependent activation of thrombin activatable fibrinolysis inhibitor (TAFI) by thrombin. J Biol Chem 2011;286(1):502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis and angiogenesis in COVID-19. NEJM. 2020;383(2):120–128. doi:10.1056/NJEMoa2015432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. White D, MacDonald S, Bull T, et al. Heparin resistance in COVID-19 patients in intensive care units. J Thromb Thrombolys. 2020;50(2):287–291. doi:10.10007/S11239-020-02145-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Renaudineau Y, Revelen R, Bordron A, Mottier D, Youinou P, Le Corre R. Two populations of endothelial cell antibodies cross-react with heparin. Lupus. 1998;7(2):86. [DOI] [PubMed] [Google Scholar]
- 28. Visentin GP, Ford SE, Scott JP, Aster RH. Antibodies from patients with heparin-induced thrombocytopenia/thrombosis are specific for platelet factor 4 complexed with heparin or bound to endothelial cells. J Clin Invest. 1994;93(1):81–88. doi:10.1172/JCI116987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yang Y, Tang H. Aberrant coagulation causes a hyper-inflammatory response in severe influenza pneumonia. Cell Molec Immunol. 2016;13(4):432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gavriilaki E, Brodsky RA. Severe conid-19 infection and thrombotic angiopathy: success does not come easily. Brit J Haematol. 2020;189(6):e227–e230. doi:10.111/bjh.16783 [DOI] [PubMed] [Google Scholar]
- 31. Java A, Edwards A, Rossi A, et al. Cytomegalovirus- induced thrombotic microangiopathy after renal transplant successfully treated with eculizumab: case report and review of the literature. Transpl Int. 2015;28(9):1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Griffin JH. The thrombin paradox. Nature. 1995;378(6555):337–338. [DOI] [PubMed] [Google Scholar]
- 33. Coccheri S. COVID-19: The crucial role of blood coagulation and fibrinolysis. Intern Emerg Med. 2020;15(8):1369–1373. doi:10.1007/s11739-020-02443-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Esmon CT. Regulation of blood coagulation. Biochimica et Biophysica Acta. 2000;1477(1-2):349–360. [DOI] [PubMed] [Google Scholar]
- 35. Wright FL, Vogler TO, Moore EE, et al. Fibrinolysis shutdown correlation with thromboembolic events in severe COVID-19 infection. J Am Coll Surg. 2020;231(2):193–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Medcalf RL, Keragala CB, Myles PS. Fibrinolysis and COVID-19: a plasmin paradox. J Thromb Haemost. 2020. doi:10.1111/jth.1496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ji H-L, Zhao R, Matalon S, Matthay MA. Elevated plasmin(ogen) as a common risk factor for COVID-19 susceptibility. Physiol Rev. 2020;100(3):1065 doi:10.1152/physrev.00013.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tang N, Li D, Wang X, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi:10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hunt BJ, Levi M. Re The source of elevated plasma D-dimer levels in COVID-19 infection. Br J Haematol. 2020;190(3):e133–e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Levi M, Thachill J, Iba T, et al. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet. 2020;7(6):e438–e440. doi:10.1016S2353-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zlokovic BV, Griffin JH. Cytoprotective protein C pathways and implications for stroke and neurological disorders. Trends Neurosci. 2011;34(4):198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Posma JJ, Grover SP, Hisada Y, et al. Roles of coagulation proteases and PARs (protease-activated receptors) in mouse models of inflammatory diseases. Arterioscler Thromb Vasc Biol. 2019;39(1):13–24. doi:10.1161/ATVBAHA.118.311655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Grey ST, Tsuchida A, Hau H, Orthner CL, Salem HH, Hancock WW. Selective inhibitory effects of the anticoagulant activated protein C on the responses of human mononuclear phagocytes to LPS, IFN-gamma, or phorbol ester. J Immunol. 1994;153(8):3664–3672. [PubMed] [Google Scholar]
- 44. Street ME. HMGB1: a possible crucial therapeutic target for COVID-19? Horm Res Paediatr. 2020;93(2):73–75. doi:10.1159/000508291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Barnes BJ, Adrover JM, Baxter-Stoltzfus A, et al. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J Exp Med. 2020;217(6):e20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mozzini C, Girelli D. The role of neutrophil extracellular traps in COVID-19: only an hypothesis or a potential new field of research? Thromb Res. 2020;191:26–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lim CH, Adav SS, Sze SK, et al. Thrombin and plasmin alter the proteome of neutrophil extracellular traps. Front Immunol. 2018;9:1554 doi:10.3389/fimmu.2018.01554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chen R, Kang R, Fan X-G, Tang D. Release and activity of histones in diseases. Cell Death Dis. 2014;5(8):e1370 doi:10.1038/cdds.2014.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Longstaff C, Hogwood J, Gray E, et al. Neutralisation of the anticoagulant effects of heparin by histones in blood plasma and purified systems. Coagulation Fibrinol. 2016;115(3):591–599. [DOI] [PubMed] [Google Scholar]
- 50. Wildhagen KCAA, de Frutos PG, Reutelingsperger CP, et al. Non-anticoagulant heparin prevents histone-mediated cytotoxicity in vitro and improves survival in sepsis. Blood. 2014;123(7):1098–1101. [DOI] [PubMed] [Google Scholar]
- 51. Xu J, Zhang X, Pelayo R, et al. Extracellular histones are mediators of cell death in sepsis. Nat Med. 2009;15(11):1318–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ashar HK, Mueller NC, Rudd JM, et al. The role of extracellular histones in influenza virus pathogenesis. Am J Pathol. 2018;188(1):135 doi:10.1016/j.ajpath.2017.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ekaney ML, Otto GP, Sossdorf M, et al. Impact of plasma histones in human sepsis and their contribution to cellular injury and inflammation. Crit Care. 2014;18(5):543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bartoszewski R, Dabrowski XM, Jakiela B, et al. SARS-CoV-2 may regulate cellular responses through depletion of specific host miRNAs. Am J Physiol Lung Cell Mol Physiol. 2020;319(3):L444–L455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Thachill J. What do monitoring platelet counts in COVID-19 teach us? Letter to the editor. Thomb Haemost. 2020;18(8):2071–2072. doi:10.111/JTH.14879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rapkiewicz AV, Mai X, Carsons SE, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. Research Paper EClinicalMedicine. 2020;24:100434 doi:10.1016/j.eclinm.2020.100434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bomhof GK, Mutsaers PGMJ, Leebeek FWG, et al. COVID-19 associated immune thrombocytopenia. bhj correspondence. Br J Haematol. 2020;190(2):e61–e64. doi:10.1111/bjh.16850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020;506:145 doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Matsuo T, Matsuo M, Sugimoto T, Wanaka K. Anti-heparin/PF4 complexes by ELISA in patients with disseminated intravascular coagulation. Pathophysiol Haemost Thromb. 2007;36(6):305–310. doi:10.1159/000296281. Epub 2010. [DOI] [PubMed] [Google Scholar]
- 60. Dragonetti D, Guarini G, Pizzuti M. Detection of anti-heparin-PF4 complex antibodies in COVID-19 patients on heparin therapy. Blood Transfus. 2020;18(4):328 doi:10.2450/2020.0164-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Warkentin TE, Basciano PA, Knopman J, Bernstein RA. Spontaneous heparin-induced thrombocytopenia syndrome: 2 new cases and a proposal for defining this disorder. Blood. 2014;123(23):3651–3654. [DOI] [PubMed] [Google Scholar]
- 62. Liu X, Zhang X, Xiao Y, et al. Heparin-induced thrombocytopenia is associated with a high risk of mortality in critical COVID-19 patients receiving heparin-involved treatment. doi:10.1101/2020.04.23.20076851
- 63. Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094–1099. published online March 27. doi:10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Qiao X, Waybill K, Jernigan A, et al. 320: Evaluation of the 4 T score in medical intensive care unit for a preclinical diagnosis of HIT. Crit Care Med. 2019;47(1):141 Abstract 320. doi:10.1097/01.ccm.0000551074.48101.e2 [Google Scholar]
- 65. Warkentin TE, Greinacher A. Management of heparin-induced thrombocytopenia. Curr Opin Hematol. 2016;23(5):462 PMID:27380556. doi:10.1097/MOH.0000000000000273 [DOI] [PubMed] [Google Scholar]
- 66. Ferner RE, Levi M, Sofat R, et al. Thrombosis in COVID-19: clinical outcomes, biochemical and pathological changes, and treatments. On behalf of the Oxford COVID-19 Evidence Service Team.
- 67. Maier CL, Truong AD, Auld SC, Polly DM, Tanksley C-L, Duncan A. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? Lancet. 2020;395(10239):1758–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Buisjers B, Yanginlar C, de Nooijer A. Increased plasma heparanase activity in COVID-19 patients. medRxiv 2020. doi:10.1101/2020.06.12.20129304 [DOI] [PMC free article] [PubMed]
- 69. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Klok FA, Kruip MJ, van der Meer NJ, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020. pii: S0049-3848(20)30120-1 doi:10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1995–2002. doi:10.1111/jth.14888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ciavarella A, Peyvandi F, Martinelli I. Where do we stand with thrombosis prophylaxis in patients with COVID-19? Thromb Res. 2020;191:29 doi:10.1016/j.thromres.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Amelot AA, Tagzirt M, Ducouret G, et al. Platelet factor 4 (CXCL4) seals blood clots by altering the structure of fibrin. JBC. 2007;282(1):710–720. http://www.jbc.org/cgi/doi/10.1074/jbc.M606650200 [DOI] [PubMed] [Google Scholar]
- 74. Weisel JW. Structure of fibrin: impact on clot stability. Thromb Haemost. 2007;5(suppl 1):116. [DOI] [PubMed] [Google Scholar]
- 75. Dorgalaleh A. Bleeding and bleeding risk in COVID-19. Semin Thromb Hemost. 2020;46(7):815–818. doi:10.1055/s-0040-1713434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sudre CH, Steves C, Ourselin S, et al. Symptom clusters in COVID19: a potential clinical prediction tool from the COVID Symptom study app. medRxiv 2020. doi:10.1101/2020.06.12.20129056 [DOI] [PMC free article] [PubMed]
- 77. Hussain A, Bhowmik B, do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142 doi:10.1016/j.diabres.2020.108142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Rabelink TJ, van den Berg BM, Garsen M, Wang G, Elkin M, van der Vlag J. Heparanase: roles in cell survival, extracellular matrix remodelling and development of kidney disease. Nat Rev Nephrol. 2017;13(4):201–212. doi:10.1038/nrneph.2017.6 [DOI] [PubMed] [Google Scholar]
- 79. van den Hoven MJ, Rops AL, Bakker MA, et al. Increased expression of heparanase in overt diabetic nephropathy. Kidney Int. 2006;70(12):2100–2108. doi:10.1038/sj.ki.5001985 [DOI] [PubMed] [Google Scholar]
- 80. van den Hoven MJ, Rops AL, Vlodavsky I, Levidiotis V, Berden JH, van der Vlag J. Heparanase in glomerular diseases. Kidney Int. 2007;72(5):543–548. doi:10.1038/sj.ki.5002337 [DOI] [PubMed] [Google Scholar]
- 81. Arokiasamy S, King R, Boulaghrasse H, et al. Heparanase-dependent remodelling of initial lymphatic glycocalyx regulates tissue-fluid drainage during acute inflammation in vivo. Front Immunol. 2019;10:2316 doi:10.3389/fimmu.2019.02316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Biscetti F, Rando MM, Nardella E, et al. High mobility group Box-1 and diabetes mellitus complications: state of the art and future perspectives. Int J Mol Sci. 2019;20(24):6258 doi:10.3390/ijms20246258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Abbas AM, Fathy SK, Fawzy AT, Salem AS, Shawky MS. The mutual effects of COVID-19 and obesity. Obesity Med. 2020;19 doi:10.1016/j.obmed.2020.100250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sattar N, McInnes IB, McMurray JJV. Obesity a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020;142(1):4–6. doi:10.1161/CIRCULATIONAHA.120.047659 [DOI] [PubMed] [Google Scholar]
- 85. Schiffrin EL, Flack JM, Ito S, Muntner P, Webb RC. Hypertension and COVID-19. Am J Hypertension. 2020;33(5):373–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Cancarevic I, Malik BH. SARS-Cov-2 (COVID 19) infection in hypertensive patients and in patients with cardiac disease. Cureus. 2020;12(6):e8557 doi:10.7759/cureus.8557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Abboud H, Abboud FZ, Kharbouche H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 infection: pathophysiology and clinical effects on the central nervous system. World Neurosurg. 2020;140:49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. doi:10.1021/acschemneuro.0c00122 [DOI] [PubMed] [Google Scholar]
- 89. Ellul MA, Benjamin L, Singh B, et al. Neurological associations of COVID-19. Lancet. 2020. doi:10.1016/S1474-442(20)30221-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Giefing-Kroll C, Berger P, Lepperdinger G. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 2015;14(3):309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Zecchin A, Kalucka J, Dubois C, Carmeliet P. How endothelial cells adapt their metabolism to form vessels in tumors. Front Immunol. 2017;8:1750 doi:10.3389/fimmu.2017.01750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020;20(4):411–412. S1473-3099(20)30113-4. doi:10.1016/S1473-3099(20)30113-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Naicker S, Yang CW, Hwang S-J, Liu B-C, Chen J-H, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97(5):824–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. O’Sullivan ED, Hughes J, Ferenbach DA. Renal aging: causes and consequences. J Am Soc Nephrol. 2017;28(2):407–420. doi:10.1681/ASN.2015121308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Batlle D, Soler MJ, Sparks MA, et al. Acute kidney injury in COVID-19: emerging evidence of a distinct pathophysiology. J Am Soc Nephrol. 2020;31(7):1380–1383. doi:10.1681/ASN.2020040419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Scully EP, Haverfield J, Ursin RL, Tannenbaum C, Klein SL. Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol 2020;20(7):442–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. van der Made CI, Simons A, Schuurs-Hoeijmakers J, et al. Presence of genetic variants among young men with severe COVID-19. JAMA. 2020;324(7):1–11. doi:10.1001/jama.2020.13719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Thachil J, Tang N, Gando S, et al. DOACs and ‘newer’ haemophilia therapies in COVID-19. J Thromb Haemost. 2020;18(7):1795 doi:10.1111/jth.14841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Milewska A, Zarebski M, Nowak P, Stozek K, Potempa J, Pyrc K. Human coronavirus NL63 utilizes heparan sulfate proteoglycans for attachment to target cells. J Virol. 2014;88(22):13221–13230. doi:10.1128/JVI.02078-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Shriver Z. Heparin and heparan sulfate: analyzing structure and microheterogeneity. Handb Exp Pharmacol. 2012;297:159–176. doi:10.1007/978-3-642-23056-1_8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Zhang W, Swanson R, Izaguirre G, Xiong Y, Lau LF, Olson ST. The heparin-binding site of antithrombin is crucial for antiangiogenic activity. Blood. 2005;106(5):1621–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Weitz JI. Heparan sulfate: antithrombotic or not? J Clin Invest. 2003;111(7):952–954. doi:10.1172/JCI200318234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Trowbridge JM, Gallo RL. Dermatan sulphate: new functions from an old glycosaminoglycan. Glycobiology. 2002;12(9):117R–125R. [DOI] [PubMed] [Google Scholar]
- 104. He L, Giri TK, Vicente CP, Tollefsen DM. Vascular dermatan sulphate regulates the antithrombotic action of heparin cofactor II. Blood. 2008;111(8):4118–4125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Raghuraman A, Mosier PD, Desai UR. Understanding dermatan sulfate-heparin cofactor II. ACS Med Chem Lett. 2010;1(6):281 doi:10.1021/ml100048y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Maimone MM, Tollefsen DM. Structure of a dermatan sulfate hexasaccharide that binds to heparin cofactor II with high affinity. J Biol Chem. 1991;266(22):14830. [PubMed] [Google Scholar]
- 107. Blinder MA, Andersson TR, Abildgaard U, Tollefsen DM. Heparin cofactor II Oslo. Mutation of Arg-189 to His decreases the affinity for dermatan sulfate. J Biol Chem. 1989;264(9):5128–5133. [PubMed] [Google Scholar]
- 108. Huntington JA. Mechanisms of glycosaminoglycan activation of the serpins in hemostasis. Thromb Haemost. 2003;1(7):1535–1549. [DOI] [PubMed] [Google Scholar]
- 109. Hoffman M, Pratt CW, Corbin LW, Church FC. Characteristics of the chemotactic activity of heparin cofactor II proteolysis products. J Leukocyte Biol. 1990;48(2):156–162. [DOI] [PubMed] [Google Scholar]
- 110. Song J-C, Wang G, Zhang W, et al. Chinese expert consensus on diagnosis and treatment of coagulation dysfunction in COVID-19. Mil Med Res. 2020;7(1):19 doi:10.1186/s40779-020-00247-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Lindahl U, Couchman J, Kimata K, et al. Proteoglycans and sulfated glycosaminoglycans In: Varki A, Cummings RD, Esko JD, et al. eds. Chapter 17: Essentials of Glycobiology [Internet]. 3rd ed Cold Spring Harbor Laboratory Press; 2015. [Google Scholar]
- 112. Gardini C, Urso E, Guerrini M, van Herpen R, de Wit P, Naggi A. Characterisation of danaparoid complex extractive drug by an orthogonal analytical approach. Molecules. 2017;22(7):1116 doi:10.3390/molecules 22071116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Fujiyama S, Saitoh S, Kawamura Y, et al. Portal vein thrombosis in liver cirrhosis. BMC Gastroenterol. 2017;17:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. The TIFDED Study Group. Thromboprophylaxis in hip fracture surgery: a pilot study comparing danaparoid, enoxaparin and dalteparin. Haemostasis. 1999;29(6):310–317. [DOI] [PubMed] [Google Scholar]
- 115. Adizguel C, Iqbal O, Hoppensteadt D, et al. Comparative anticoagulant and platelet modulatory effects of enoxaparin and sulodexide. Clin Appl Thromb Hemost. 2009;15(5):501–511. [DOI] [PubMed] [Google Scholar]
- 116. Cassinelli G, Torri G, NaggiI A. Non-anticoagulant heparins as heparanase inhibitors chapter 20 In: Vlodavsky I, Sanderson RD, Ilan N, eds. Heparanase, Advances in Experimental Medicine and Biology. 1221 2020. doi:10.1007/978-3-030-34521-1_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Boittier ED, Gandhi NS, Ferro V, Coombe DR. Cross-species analysis of glycosaminoglycan binding proteins reveals some animal models are “more equal” than others. Molecules. 2019;24(5):924 doi:10.3390/molecules24050924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Tuinman PR, Dixon B, Levi M, Juffermans NP, Schultz MJ. Nebulized anticoagulants for acute lung injury—a systematic review of preclinical and clinical investigations. Crit Care. 2012;16(2):R70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Wang L, Brown JR, Varki A, et al. Heparin’s anti-inflammatory effects require glucosamine 6-O sulphation and are mediated by blockade of L- and P-selectins. J Clin Invest. 2002;110(1):127–136. doi:10.1172/JC10214996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Garg HG, Yu L, Hales CA, Toida T, Islam T, Linhardt RJ. Sulphation patterns in heparin and heparan sulphates: effects on the proliferation of bovine pulmonary artery bovine smooth muscle cells. Biochem Biophys Acta. 2003;1369(3):225–231. [DOI] [PubMed] [Google Scholar]
- 121. Griffin KL, Fischer B, Kumarapurugu AB, et al. 2-O, 3-O-desulfated heparin inhibits neutrophil elastase-induced HMGB-1 secretion and airways inflammation. Am J Resp Cell Mol Biol. 2014;50(4):684–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Bai X, Bame KJ, Habuchi H, Kimata K, Esko JD. Turnover of heparan sulfate depends on 2-O-sulfation of uronic acids. J Biol Chem. 1997;272(37):23172–23179. [DOI] [PubMed] [Google Scholar]
- 123. Pikas DS, Li J-P, Vlodavski I, Lindahl U. Substrate specificity of heparanases from human hepatoma and platelets. J Biol Chem. 1998;273(30):18770–18777. [DOI] [PubMed] [Google Scholar]
- 124. Harris EN, Liu J, Miller C, et al. 3-O sulfation of heparin is required for hepatic accumulation. FASEB. 2016. Experimental biology meeting. [Google Scholar]
- 125. Agelidis AM, Shukla D. Cell entry mechanisms of HSV: what we have learned in recent years. Future Virol. 2015;10(10):1145–1154. doi:10.2217/fvl.15.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Kaltenbach DD, Jaishankar D, Hao M, et al. Sulfotransferase and heparanase: remodeling engines in promoting virus infection and disease development. Front Pharmacol. 2018;9:1315 doi:10.3389/fphar.2018.01315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Stanford KI, Wang L, Castagnola J, et al. Heparan sulfate 2-O-sulfotransferase is required for triglyceride-rich lipoprotein clearance. J Biol Chem. 2010;285(1):286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Stringer SE, Gallagher JT. Specific binding of the chemokine platelet factor 4 to heparan sulphate. J Biol Chem. 1997;272(33):20508–20514. [DOI] [PubMed] [Google Scholar]
- 129. Glass CA. Recombinant heparin—new opportunities. Front Med. 2018;5:341 doi:10.3389/fmed.2018.00341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Hallak LK, Spillmann D, Peeples ME. Glycosaminoglycan sulfation requirements for respiratory syncytial virus infection. J Virol. 2000;74(22):10508 doi:10.1128/jvi.74.22.10508-10513.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Dong LQ, Wang XQ, Guo YN, et al. HS N-sulfation and iduronic acids play an important role in the infection of respiratory syncytial virus in vitro. Eur Rev Med Pharmacol Sci. 2013;17(14):1864–1868. [PubMed] [Google Scholar]
- 132. Fluhr H, Spratte J, Heidrich S, Ehrhardt J, Greinacher A, Zygmunt M. The molecular charge and size of heparins determine their impact on the decidualisation of endometrial stromal cells. Mol Human Repro. 2011;17(6):354–359. [DOI] [PubMed] [Google Scholar]
- 133. Presanis JS, Hajela K, Ambrus G, Gál P, Sim RB. Differential substrate and inhibitor profiles for human MASP-1 and MASP-2. Mol Immunol. 2004;40(13):921–929. [DOI] [PubMed] [Google Scholar]
- 134. van Bruggen MCJ, Walgreen B, Rijke TP, et al. Heparin and heparinoids prevent the binding of immune complexes containing nucleosomal antigens to the GBM and delay nephritis in MRL/lpr mice. Kidney Int. 1996;50(5):1555–1564. [DOI] [PubMed] [Google Scholar]
- 135. Capila I, Linhardt RJ. Heparin-protein interactions. Angew Chem Int Ed Engl. 2002;41(3):390–412. [DOI] [PubMed] [Google Scholar]
- 136. Takahashi H, Ebihara S, Okazaki T, Asada M, Sasaki H, Yamaya M. A comparison of the effects of unfractionated heparin, dalteparin and danaparoid on vascular endothelial growth factor-induced tumour angiogenesis and heparanase activity. B J Pharmacol. 2005;146(3):333–343. doi:10.1038/sj.bjp.0706344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Hacker U, Gerner F, Büning H, et al. Standard heparin, low molecular weight heparin, low molecular weight heparinoid, and recombinant hirudin differ in their ability to inhibit transduction by recombinant adeno-associated virus type 2 vectors. Gene Ther. 2001;8(12):966–968. doi:10.1038/sj.gt.3301466 [DOI] [PubMed] [Google Scholar]
- 138. Fluhr H, Seitz T, Zygmunt M. Heparins modulate the IFN-γ-induced production of chemokines in human breast cancer cells. Breast Cancer Res Treat. 2013;137(1):109–118. [DOI] [PubMed] [Google Scholar]
- 139. Chudasama SL, Espinasse B, Hwang F, et al. Heparin modifies the immunogenicity of positively charged proteins. Blood. 2010;116(26):6046–6053. doi:10.1182/blood-2010-06-292938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Leppkes M, Knopf J, Naschberger E, et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine. 2020;58;102925 doi:10.1016/j.ebiom.2020.102925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Barrett CD, Moore HB, Yaffe MB, Moore EE. ISTH interim guidance on recognition and management of coagulopathy in COVID-19: a comment. Thromb Haemost. 2020;18(8):2060 doi:10.1111/jth.14860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Shi C, Wang C, Wang H, et al. Clinical observations of low molecular weight heparin in relieving inflammation in COVID-19 patients: a retrospective cohort study. medRxiv 2020. doi:10.1101/2020.03.28.20046144.t [DOI] [PMC free article] [PubMed]
- 143. Granger CB, Miller JM, Bovill EG, et al. Rebound increase in thrombin generation and activity after cessation of intravenous heparin in patients with acute coronary syndromes. Circulation. 1995;91(7):1929–1935. [DOI] [PubMed] [Google Scholar]
- 144. Bijsterveld NR, Moons AH, Meijers JCM, et al. Rebound thrombin generation after heparin therapy in unstable angina. J Am Coll Cardiol. 2002;39(5):811–817. [DOI] [PubMed] [Google Scholar]
- 145. Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi:10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Pana D, Szec S, Minhasc JS, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EclinMed. 2020:23 doi:10.1016/j.eclinm.2020.100404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Bikdeli B, Madhavan MV, Gupta A, et al. Pharmacological agents targeting thrombo-inflammation in COVID-19: review and implications for future research. Thromb Haemost. 2020;120(7):1004–1024. doi:10.1055/s-0040-1713152.ISSN 0340-6245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Farooqui A, Hoppensteadt D, Iqbal O, et al. Comparative studies on the interaction of unfractionated heparin and sulodexide with functional anti-heparin platelet factor 4 antibodies. Blood. 2019;134(supplement1):2446. [Google Scholar]
- 149. Adizguel C, Iqbal O, Hoppensteadt D, et al. Sulodexide mediated inhibition of tissue factor activation of platelets. A potential mechanism for the observed therapeutic effects in diabetic nephropathy. FASEB. 2008;22:1118. [Google Scholar]
- 150. Burgess JK, Chong BH. The platelet pro-aggregating and potentiating effects of unfractionated heparin, low molecular weight heparin and heparinoid in intensive care patients and healthy controls. Eur J Haematol. 1997;58(4):279–285. [DOI] [PubMed] [Google Scholar]
- 151. Meuleman D. Orgaran (Org 10172): its pharmacological profile in experimental models. Haemostasis. 1992;22(2):58–65. [DOI] [PubMed] [Google Scholar]
- 152. Coccheri S, Mannello F. Development and use of sulodexide in vascular diseases: implications for treatment. Drug Des Devel Ther. 2014:8 49–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Dou H, Song A, Jia S, Zhang L. Heparinoids sulodexide and danaparoid as clinically useful drugs. Prog Mol Biol Translational Sci. 2019;163:55–74. doi:10.1016/bs.pmbts.2019.02.005 [DOI] [PubMed] [Google Scholar]
- 154. Ciszewicz M, Polubinska A, Antoniewicz A, Suminska-Jasinska K, Breborowicz A., sulodexide suppresses inflammation in human endothelial cells and prevents glucose cytotoxicity. Transl Res. 2009;153(3):118–123. [DOI] [PubMed] [Google Scholar]
- 155. Mannello F, Ligi D, Canale M, Raffetto JD. Sulodexide down regulates the release of cytokines, chemokines and leukocyte colony stimulating factors from human macrophages: role of glycosaminoglycans in inflammatory pathways of chronic venous disease. Curr Vasc Pharmacol. 2014;12(1):173–185 . [DOI] [PubMed] [Google Scholar]
- 156. Masola V, Onisto M, Zaza G, Lupo A, Gambaro G. A new mechanism of action of sulodexide in diabetic nephropathy: inhibits heparanase-1 and prevents FGF-2-induced renal epithelial-mesenchymal transition. J Translational Med. 2012;10(1):213 doi:10.1186/1479-5876-10-213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. van de Pijl JW, van de Woude F, Swart W, van Es LA, Lemkes HHPJ. Effect of danaparoid sodium on hard exudates in diabetic retinopathy. Lancet. 1997;350(9093):1743–1745. [DOI] [PubMed] [Google Scholar]
- 158. van de Pijl JW, Lemkes HHPJ, Frölich M, van de Woude F, van der Meer FJM, van Es LA. Effect of danaparoid sodium on proteinuria, von Willebrand factor and hard exudates in patients with diabetes mellitus type 2. J Am Soc Nephrol. 1999;10(6):1331–1336. [DOI] [PubMed] [Google Scholar]
- 159. Greinacher A, Michels I, Mueller-Eckhardt C. Heparin associated thrombocytopenia: the antibody is not heparin specific. Thromb Haemost. 1992;67(5):545–549. [PubMed] [Google Scholar]
- 160. Krauel K, Furll B, Warkentin TE, et al. Heparin-induced thrombocytopenia—therapeutic concentrations of danaparoid, unlike fondaparinux and direct thrombin inhibitors, inhibit formation of platelet factor 4-complexes. J Thromb Haemost. 2008;6(12):2160–2167. [DOI] [PubMed] [Google Scholar]
- 161. Tardy-Poncet B, Tardy B, Reynaud J, et al. Efficacy and safety of danaparoid sodium (Org 10172) in critically ill patients with heparin-associated thrombocytopenia. Chest. 1999;115(6):1616–1620. [DOI] [PubMed] [Google Scholar]
- 162. Trehel-Tursis V, Louvain-Quintard V, Zarrouki Y, Imbert A, Doubine S, Stéphan F. Clinical and biological features of patients suspected or confirmed to have heparin-induced thrombocytopenia in a cardiothoracic ICU. Chest. 2012;142(4):837–844. [DOI] [PubMed] [Google Scholar]
- 163. Nakahara M, Yasuda T, Taniguchi J, Kakihama Y, Kanmura Y. Efficacy of danaparoid on sepsis with DIC in patients admitted to the ICU. Proc Am Soc Anesthesiol. Annual Meeting October 2009. Abstract A913. [Google Scholar]
- 164. Ikeda K, Ikeda T, Taniuchi H, et al. Effect of danaparoid sodium combined with antithrombin for the patients with systemic inflammatory response syndrome (SIRS) associated coagulopathy (SAC). Intens Care Med. 2008;34:S266, Abstract 1043. [Google Scholar]
- 165. Minakata D, Fujiwara S, Hayakawa J, et al. Comparison of danaparoid sodium and synthetic protease inhibitors for the treatment of disseminated intravascular coagulation associated with hematological malignancies: a retrospective analysis. Acta Haematol. 2020;143(3):250–259. [DOI] [PubMed] [Google Scholar]
- 166. Nieuwenhuis HK, Sixma JJ. Treatment of disseminated intravascular coagulation in acute promyelocytic leukaemia with low molecular weight heparinoid Org 10172. Cancer. 1986;58(3):761–764. [DOI] [PubMed] [Google Scholar]
- 167. Magnani HN, Gallus A. Heparin induced thrombocytopenia: a report of 1478 clinical outcomes of patients treated with danaparoid (Orgaran®) from 1982 to mid-2004. Thromb Haemost. 2006;95(6):967–981 [DOI] [PubMed] [Google Scholar]
- 168. Magnani HN. A review of 122 published outcomes of danaparoid anticoagulation for intermittent haemodialysis. Thromb Res. 2005;125(4):e171–176. [DOI] [PubMed] [Google Scholar]
- 169. Magnani HN, Wester JPJ. Is danaparoid anticoagulation suitable for patients with HIT and ARF requiring CVVRT? An analysis of case reports. Open Access Sci Rep. 2012;1(9):1. [Google Scholar]
- 170. Lasocki S, Piednoir P, Ajzenberg N, Geffroy A, Benbara A, Montravers P. Anti-PF4/heparin antibodies associated with repeated hemofiltration-filter clotting: a retrospective study. Critical Care. 2008;12(3):R84 doi:10.1186/cc6937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Ohtake T, Tsuji K, Kawanishi T, et al. A multicentre survey of the efficacy and safety of danaparoid sodium treatment for portal vein thrombosis. Hepatology. 2014;60(4):399A Abstract 402. 24807046 [Google Scholar]
- 172. Hayashi T, Takatori H, Horii R, et al. Danaparoid sodium-based anticoagulation therapy for portal vein thrombosis in cirrhosis patients. BMC Gastroenterol. 2019;19(1):217 doi:10.1186/s12876-019-1140-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. de Guibert S, de Latour RP, Varoqueaux N, et al. Paroxysmal nocturnal haemoglobinuria and pregnancy before the eculizumab era. Haematologica. 2011;96(9):1276–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Meppiel E, Crassard I, Peffault de Latour R, et al. Cerebral venous thrombosis in paroxysmal nocturnal hemoglobinuria: a series of 15 cases and review of the literature. Medicine. 2015;94(1):e362 doi:10.1097/MD.0000000000000362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Adachi M, Nakatsuka M, Sakasi A, et al. Effect of danaparoid on Antiphospholipid antibody positive infertile patients. copy via Organon Nippon 2006 now Aspen Pharma.
- 176. Yoshihara H, Sugiura-Ogasawara M, Kitaori T, Katano K, Ozaki Y. Danaparoid is effective and safe for patients with obstetric antiphospholipid syndrome. Mod Rheumatol. 2020;30(2):332–337. doi:10.1080/14397595.2019.1602241 [DOI] [PubMed] [Google Scholar]
- 177. Kato K, Sakaguchi H, Muramatsu H, et al. Danaparoid reduces transplant-related mortality in stem cell transplantation for children. Pediatr Transplant. 2018;22(2):e13099 doi:10.1111/petr.13099 [DOI] [PubMed] [Google Scholar]
- 178. Machida S, Onizuka M, Toyosaki M, et al. Danaparoid reduces the incidence of hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Bone Marrow Transplantation. 2017;52(2):307–309. [DOI] [PubMed] [Google Scholar]
- 179. Hausberg M, Felten H, Pfeffer S. Treatment of chemotherapy-induced thrombotic microangiopathy with eculizumab in a patient with metastatic breast cancer. Case Rep Oncol. 2019;12(1):1–6. ePub 2019 Jan 3. doi:10.1159/000495031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Thachill J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18(5):1023–1026. doi:10.111/jth.14810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Farner B, Eichler P, Kroll H, Greinacher A. A comparison of lepirudin and danaparoid in patients with heparin-induced thrombocytopenia (HIT). Thromb Haemost. 2001;85(6):950–957. [PubMed] [Google Scholar]
- 182. Lubenow N, Warkentin TE, Greinacher A, et al. Results of a systematic evaluation of treatment outcomes for heparin-induced thrombocytopenia in patients receiving danaparoid, ancrod and/or coumarin explain the rapid shift in clinical practice during the 1990s. Thromb Haemost. 2006;117(5):507–515. [DOI] [PubMed] [Google Scholar]
- 183. COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health; 2021. Accessed January, 2021 https://www.COVID19treatmentguidelines.nih.gov/ [PubMed] [Google Scholar]