Abstract
Objective:
Liquid thickeners are commonly recommended in individuals with dysphagia and recurrent aspiration as a strategy for pneumonia prevention. The goal of this study was to examine the effects of small amounts of aspirated liquid thickener on the lungs.
Study design:
Animal model. Prospective small animal clinical trial.
Methods:
Adult Sprague Dawley rats (n = 19) were divided into two groups and underwent three intratracheal instillations of either xanthan gum-based nectar-thick water (0.1–0.25 mL/kg) or water-only control over the course of 8 days. Blood was collected from a peripheral vein on days 1 and 8 and submitted for complete blood count (CBC) analysis. Rats were euthanized 10 days after the last instillation, and the lungs were harvested. Histopathology was conducted on lung specimens by a blinded licensed veterinary pathologist and scored for evidence of lung injury and pneumonia.
Results:
Fifteen animals (8 nectar-thickener group, 7 control group) survived until the endpoint of the study (day 18). Serum CBC did not show abnormalities at any timepoint in either group. Histological evidence of lung inflammation and edema were significantly greater in the nectar-thick group compared to controls (P < .05). Signs of inflammation included aggregates of foamy macrophages, expansion of bronchiolar lymphoid tissue, and large numbers of eosinophilic intraalveolar crystals. Histiocytic and neutrophilic pneumonia was noted in one animal that received thickened liquids.
Conclusion:
Recurrent aspiration of small amounts of thickened water resulted in significant pulmonary inflammation in a murine model of aspiration. Results of this study support the need for further investigation of liquid thickener safety and its efficacy in reducing the pulmonary complications of swallowing disorders.
Keywords: Xanthan gum, dysphagia, liquid thickener, aspiration, pneumonia
INTRODUCTION
Aspiration pneumonia is a major cause of morbidity in older adults and one of the leading causes of death among residents of nursing homes.1,2 Swallowing dysfunction increases the risk of pulmonary aspiration, which can evolve into pneumonia. To reduce the risk of dysphagia-induced aspiration, healthcare providers frequently recommend that patients thicken their liquids with commercially available thickeners, typically to a nectar or honey-like consistency.3 For some patients, thickened liquids may increase the safety of swallowing by slowing liquid flow or increasing bolus cohesiveness, which helps to compensate for a delayed pharyngeal swallow or incomplete airway closure.4–6 Despite the potential of thickened liquids to reduce the risk of aspiration, aspiration still occurs.7,8 Results of our previous study using a lagomorph model of acute aspiration suggest that aspiration of a large amount of thickened water versus water alone results in greater pulmonary inflammation, lung edema, and death.9 Additionally, we observed that cornstarch-based thickeners may pose a greater health risk compared to xanthan gum-based thickeners. The risk of pulmonary injury following recurrent aspiration of thickened liquids is uncertain. In the current study, we examined the effects of recurrent aspiration of small amounts of thickened liquids to simulate the potential of repeated aspiration of liquids in patients with swallowing disorders.
MATERIALS AND METHODS
This study protocol was approved by the Institutional Animal Care and Use Committee of the University of California, Davis (protocol #20118). Adult Sprague Dawley male rats (n = 19) were divided into two groups: thickened-water (n = 10) and water-only controls, henceforth referred to as controls (n = 9). The groups underwent three intratracheal (IT) instillations of either thickened water or water on days 1, 3, and 8.
Viscosity Measurements
Purified water (LIFEWTR, PepsiCo, Harrison, NY) was prepared with xanthan gum-based thickener (Resource Thickenup Clear, Nestle, Vevey, Switzerland) to a consistency of International Dysphagia Diet Standardisation Initiative (IDDSI) level 2, as measured by the IDDSI flow test.10,11 In advance of the study, the rheological properties of test samples of the level 2 xanthan gum-thickened water were measured using a 40-mm parallel plate geometry with a 1 mm gap on an Anton Paar MCR302 rheometer (Graz, Austria). Samples were equilibrated to 22C prior to measurement, and a shear rate sweep from 0.1 to 100 1/sec was performed. At a shear rate of 50 1/sec, typically used to estimate flow properties of fluids during swallowing, the apparent viscosity of the xanthan gum-thickened water was 91 (±1.8) milli-pascal-second (mPa-s).
Prior to the intratracheal instillation procedure, either water (IDDSI level 0) or thickened water (IDDSI level 2) was drawn into a 1-mL syringe (Monoject Kendall/Covidien, Dublin, Ireland) within 5 minutes of preparation at room temperature. Animals received 0.1 mL/kg of instillate on days 1 and 8 and 0.25 mL/kg on day 3 (Fig. 1A). The animals were instilled with small volumes of liquid in order to emulate the occurrence of recurrent aspiration in humans. Instillate volume was increased on day 3 to 0.25 mL/kg. Due to an animal death that occurred with the larger volume, however, the volume was reduced back to 0.1 mL/kg for the final instillation. Rats were anesthetized with ketamine (75 mg/kg) and dexmedetomidine (0.5 mg/kg, intraperitoneal injection (IP). If the animal exhibited signs of wakefulness during the procedure, inhaled 3% isoflurane was administered to effect as needed. The animal was positioned on a rodent work stand (Hollowell EMC, Pittsfield, MA) in the prone position. An otoscope (MDS Inc.,Valrico, FL) with an attached intubation specula (Hollowell EMC, Pittsfield, MA) was inserted into the pharynx transorally, and animals were kept breathing spontaneously. An 18G, 2.5-inch intravenous catheter (B. Braun Medical Inc, Bethlehem, PA) was inserted through the specula into the larynx, and the syringe containing the instillate was attached to the catheter (Fig. 1B). Following the instillation of fluid, animals were immediately injected with an anesthetic reversal agent, atipamezole (1–2.5 mg/kg, IP), and were monitored until recovery. Blood was collected from a peripheral vein on days 1 and 8 and submitted for complete blood count (CBC) analysis. Throughout the study period, animals were monitored for difficulty breathing, abnormal eating behaviors, malaise, and pain. All surviving animals were euthanized on day 18 with pentobarbitol (100 mg/kg, IP). This method of euthanasia was performed in lieu of CO2 inhalation in order to preserve the lung tissue for histological evaluation.
Fig. 1.
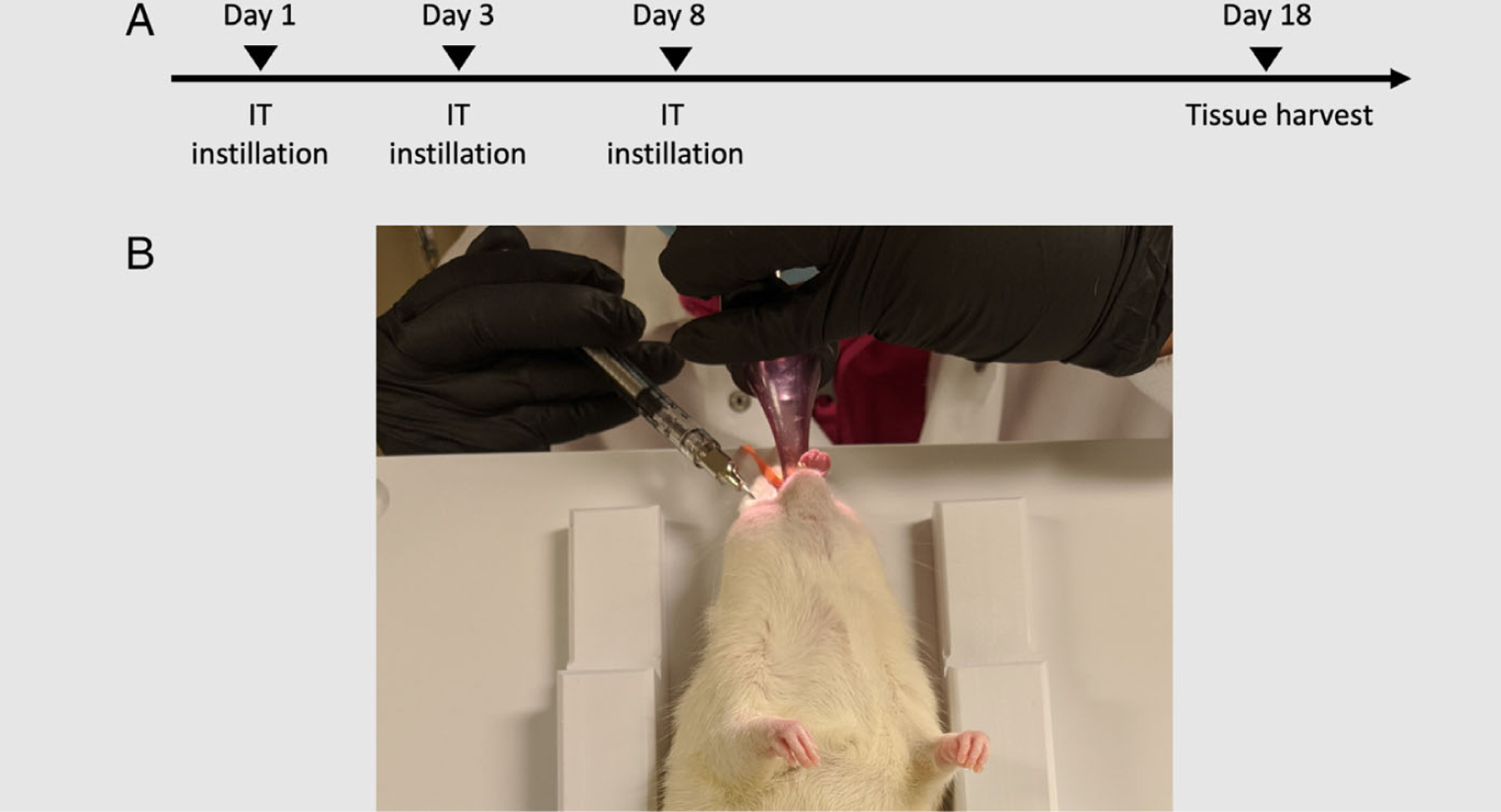
(A) Experimental timeline. (B) IT instillation setup: the animal was positioned on the rodent workstand (Hollowell EMC, Pittsfield, MA) in the prone position. An otoscope (MDSInc., Valrico, FL) with an attached intubation specula (Hollowell EMC, Pittsfield, MA) was inserted into the pharynx transorally, and a 18G 2.5-inch IV catheter was inserted through the specula into the larynx. The instillate was administered via a syringe attached to the catheter. IT instillation = intratracheal instillation; IV = intravenous.
Histological analysis of the lungs was conducted on all animals that survived until the endpoint of the study by a blinded pathologist. Formalin-fixed lung tissue was routinely processed, embedded in paraffin, sectioned at 4- to 5-μm, mounted on glass slides, and stained with hematoxylin and eosin (H&E). The following parameters of lung injury were graded on a 6-point ordinal scoring system from 0 (normal) to 5 (severe change): histiocytic and granulocytic inflammation, alveolar edema, and interstitial fibrosis. Parameter scores were determined by the affected percentage of 1) the total sectional area or 2) the most severely altered 400× field (see Table I for further details). Addition of the scores for airway inflammation and alveolar edema were used to determine an overall lung injury score for each animal.Pulmonary artery medial hypertrophy was recorded using binomial scoring.
TABLE I.
Scoring System of Lung Histology Evaluation.
| Parameter Score | Percentage of Area Affected |
|---|---|
| 0 | Parameter absent |
| 1 | Less than 10% affected |
| 2 | 10%–5% affected |
| 3 | 26%–75% affected |
| 4 | 76%–90% affected |
| 5 | Greater than 90% affected |
Statistical comparisons between groups were conducted by independent sample t tests using SPSS version 26.0 (IBM Inc., Armonk, NY). P values < .05 were considered to be statistically significant.
RESULTS
Fifteen animals (thickened water group = 8, water control group = 7) survived until the endpoint of the study (day 18), and four animals died prior to the endpoint. Two of the animals died from acute respiratory failure immediately following the IT instillation (thickened-water group), and two died of anesthetic complications prior to the procedure (control group).
Animal Deaths
The cause of death in one of the animals from the thickened water group is presumed to be a combination of left-sided congestive heart failure (chronic passive pulmonary congestion) and possible acute aspiration. Necropsy findings included moderate, left ventricular hypertrophic cardiomyopathy with multifocal interstitial fibrosis. Lung evaluation revealed moderate multifocal to regionally extensive congestion and edema with alveolar histiocytosis and cytoplasmic pigment as well as regional fibrinous pneumonia with edema, perivascular neutrophils, and possible intralesional foreign material. The cause of death in the second animal from the thickened water group was not grossly or histologically apparent; however, alveolar histiocytes suggested the presence of edema, and we suspect acute respiratory failure second to airway obstruction. Gross and histopathologic evaluation could not identify any specific cause of the death for either of the control animals. Regional acute congestion and hemorrhage were identified in one of the animal lungs, which the pathologist interpreted as agonal, occurring during the dying process but not a cause of death.
Complete Blood Count
Serum CBC did not show abnormalities at any timepoint in either group.
Lung Histopathology
Mean (±standard deviation [SD]) total lung injury scores were 6.12 (±2.3) for the thickened water group and 2.85 (±1.2) for the control group (P < .01) (Fig. 2A). Mean (±SD) airway inflammation scores were significantly greater in the thickened water group [1.94 (±0.8)] compared to the control group [1.14 (±0.4); P = .03] (Fig. 2B). Mean (±SD) alveolar edema scores were 1.69 (±0.4) in the thickened water group in comparison to only 0.35 (±0.7) in the water control group (P = .02) (Fig. 2C). No evidence of fibrosis was noted for any of the samples. Signs of inflammation included expansion of bronchiolar lymphoid tissue and large numbers of eosinophilic intraalveolar crystals and aggregates of foamy macrophages (Fig. 3). The lungs of four animals from the thickened water group exhibited intrapulmonary crystalline material consistent with the hemoglobin crystals that are often associated with inflammation in rats12,13 (Fig. 4). Inflammation was associated with small amounts of karyorrhectic debris, which surrounded medium- and large-caliber blood vessels. One animal from the thickened-water group had a focally extensive histiocytic and neutrophilic pneumonia confined to a single lobe. No animals from the control group exhibited intrapulmonary crystalline material, karyorrhectic debris, or histiocytic or neutrophilic pneumonia. Pulmonary artery medial hypertrophy was identified in 4 animals from the thickened water group and 3 animals from the control group.
Fig. 2.
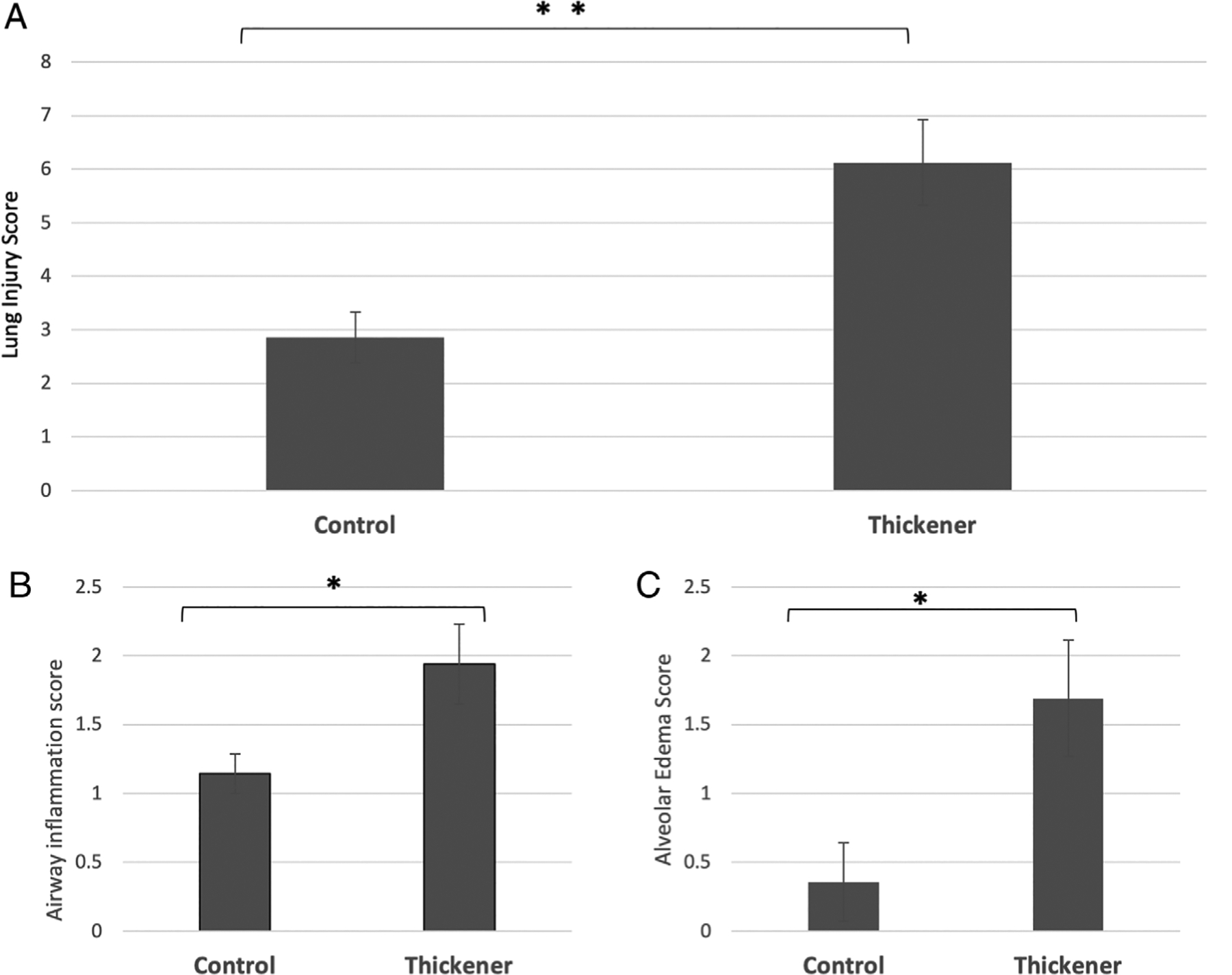
Histological evaluation of the lungs performed by a blinded pathologist using a 6-point (0–5) ordinal scoring system. Mean scores for total lung injury (A), airway inflammation (B), and alveolar edema (C) are presented for each group. *P < .05; **P < .01.
Fig. 3.
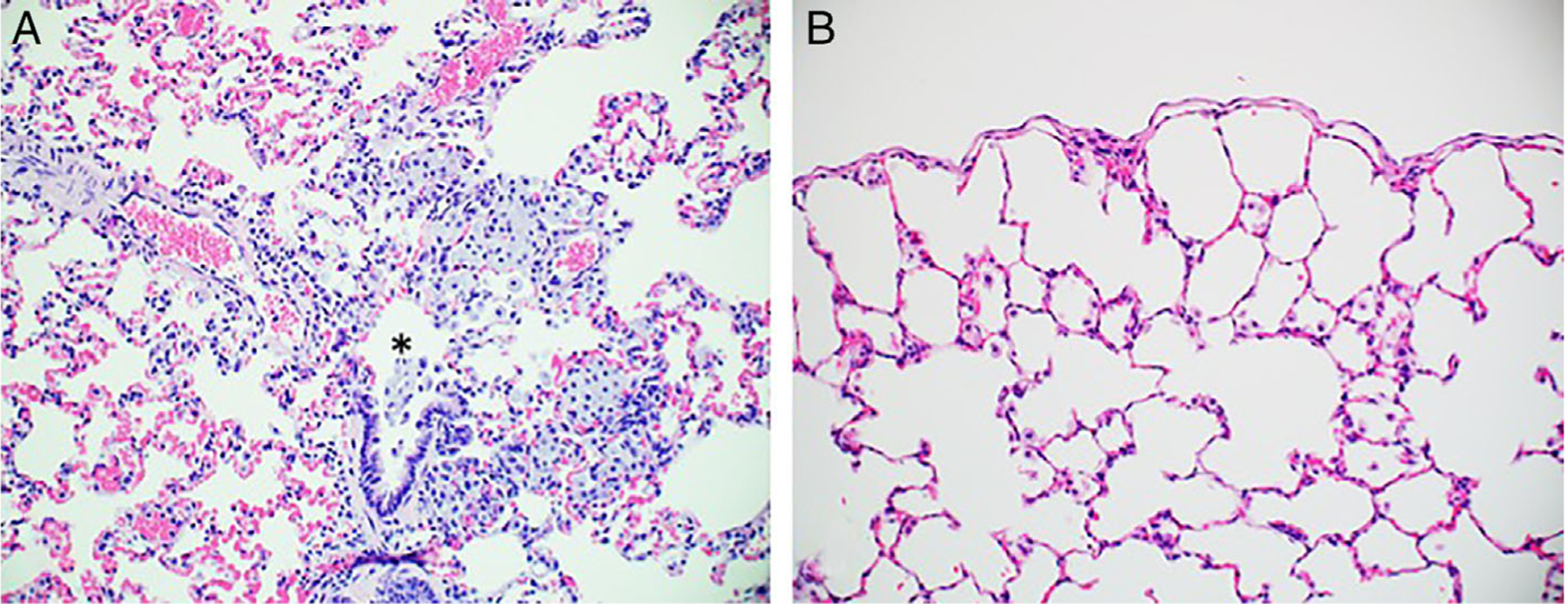
Pulmonary pathology in rats treated with xanthan gum-thickened water (A) and control (water alone) (B). Installation of xanthan gum-thickened water is associated with clusters of intraalveolar macrophage that often extend from alveolar ducts (asterix) and alveolar edema (A). Macrophages contain copious finely granular, lightly basophilic material that is interpreted as the instilled solution. Installation of water alone was associated with small numbers of intraalveolar macrophages. Hematoxylin and eosin: 200× magnification.
Fig. 4.
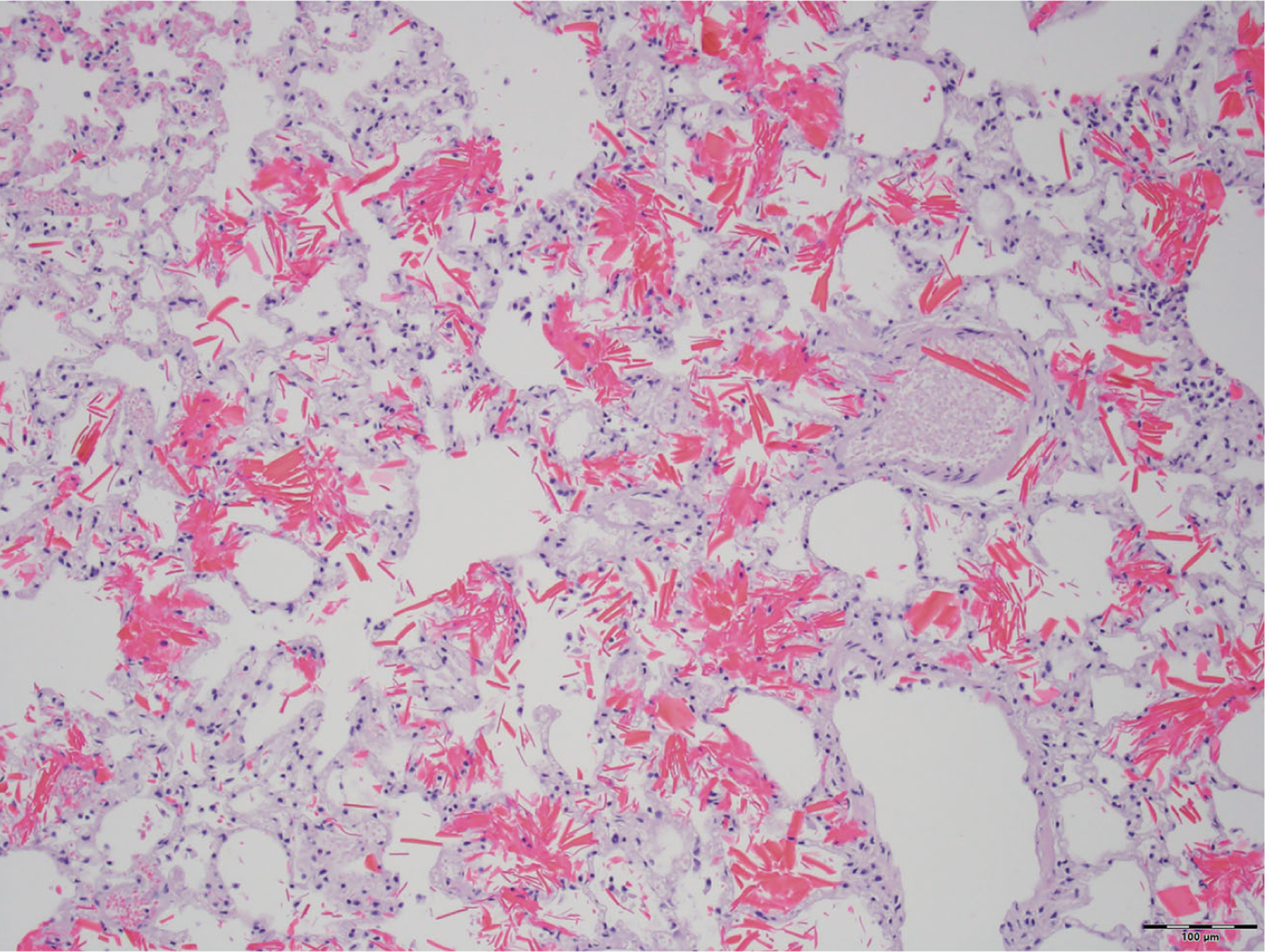
Hemoglobin crystals present in lungs that were instilled with xanthan gum-thickened water. Hemoglobin crystals are often associated with inflammation in rats. Hematoxylin and eosin: 200× magnification.
DISCUSSION
Thickening liquids is a commonly used management strategy for reducing dysphagia-induced liquid aspiration with the goal of preventing the development of aspiration pneumonia. Liquid thickeners are recommended by most speech language pathologists to approximately half of patients with swallowing difficulty14 and are used as a common management strategy in up to 92% of skilled nursing facilities.15 Several studies have demonstrated a reduction in the frequency of supraglottic penetration and aspiration events with increased fluid viscosity5,16–20; however, the effectiveness of this strategy in reducing pneumonia rates is unknown. Although thickeners may reduce the risk of aspiration during swallowing in some populations, they do not eliminate it completely in many patients.7,8 The importance of understanding swallowing physiology in determining the effectiveness of changes in viscosity is essential.21 For example, postswallow residue with thickened liquids may increase the potential for postdeglutitive aspiration.5,19,22 Despite the ubiquitous use of liquid thickeners in patients with aspiration risk, little is known about their effects on the lungs.
Previous work in a rabbit model by our group has demonstrated that 3 consecutive days of large amounts of aspirated thickeners are injurious to the lungs and fatal.9 All animals in the study that were instilled with cornstarch-based thickeners died before the endpoint of the study (day 4). The animals who underwent instillation of xanthan gum-based thickeners survived until the endpoint; however, lung histology demonstrated significantly more pulmonary inflammation, interstitial congestion, and alveolar edema compared to water alone. In this current study, we examined the effects of aspirated thickeners in a rat model of recurrent aspiration events with small amounts of viscous liquid, which are likely more representative of the occurrence of aspiration in persons with swallowing disorders.
Results of this study demonstrate significant pulmonary inflammation in a rat model of recurrent aspiration of small amounts of liquid gel thickener, which was evident in the lungs even after a 10-day recovery period. These findings suggest that aspiration of xanthan gum-based thickened water may be harmful to the lungs even when aspirated occasionally and in small amounts. A recent study in mice demonstrated that thickened saline aspiration caused short-term inflammatory responses and a prolonged increase in alveolar capillary barrier permeability.23 Nishimura et al.24 demonstrated an increase in pulmonary neutrophils from the IT instillation of nonpurified xanthan gum in rats, which the authors attributed to the possibility of endotoxin-related pulmonary injury. Neutrophil count was lower in the commercially available xanthan gum product, likely due to purification processes. Because all fluids in the study were adjusted to a viscosity of 20 mPasec, the authors suggested that chemical rather than physical characteristics of the instillates accounted for differences in lung injury. These studies, as well as the current study, used xanthan gum-based thickeners, which are currently the most commonly used thickeners in the adult population. However, additional studies are needed to examine the effects of other liquid thickeners, particularly those more commonly prescribed for the pediatric population, such as other gum bases or pectin-based thickeners.
In addition to the effects of physical and chemical properties of aspirates, the amount of aspirated material and the frequency of the recurrence of aspiration events may also play a role in the severity of pulmonary outcomes. The possible contribution of these factors is also suggested by the results of a lagomorph study demonstrating that repeated small-volume aspiration of milk in a rabbit model resulted in persistent airway inflammation and increased airway reactivity compared to saline controls.25 Elucidating the effects of volume and frequency of aspiration is important due to the recurrent nature of aspiration secondary to dysfunctional swallowing.
In this study, histologic evidence of pulmonary artery medial hyperthrophy was identified in several animals from both experimental groups. Medial hyperthropy can be a spontaneous finding in laboratory rats and is most often considered a secondary response to hypertension.26 Zhao et al. indicated that they observed this finding in a chronic hypoxia-induced pulmonary hypertension rat model27; however, it is unknown if this could also be caused by an acute hypoxic event. Some strains of rats that are predisposed to hypertension can also develop medial hypertrophy of the pulmonary artery. However, Sprague Dawley rats are not known to demonstrate this finding. Interstitial fibrosis was not identified in any of the groups, although future evaluation of Masson’s Trichrome-stained replicate sections at a later timepoint (90 days or longer) following aspiration-induced inflammation may identify fibrosis that was not discernable in H&E-stained slides at day 18. A longer-term study may demonstrate chronic changes in the lung, including interstitial fibrosis.
Current data on the effectiveness of liquid thickeners in reducing aspiration pneumonia are limited. A recent systematic review and meta-analysis of pneumonia associated with thin liquid versus thickened liquid intake in patients who aspirate concluded that there was no significant difference in the risk of pneumonia in aspirating patients who took thin liquids with safety strategies compared with those who took thickened liquids only.28 The authors noted, however, that these results may be generalizable only for patients with a low risk of pneumonia.28 In recent years, there is growing concern among clinicians who treat patients with dysphagia about the frequent use of thickener despite the limited understanding with regard to their efficacy in pneumonia prevention.29,30 The results of this investigation support this apprehension and support the need for further investigation. Moreover, current investigations have looked at adult animal models; the impact of recurrent aspiration with and without thickeners on the developing lung warrants investigation.
This investigation is not without limitations. The sample size was small, and the rodent is a limited surrogate for the human condition. In addition, the IT instillation does not represent the complexities of the deglutition process and how it may modify aspirated thickened liquid. The results of this experiment should be interpreted with caution. Nonetheless, the data suggest that the intratracheal administration of thickened water causes significantly more pulmonary injury than the intratracheal administration of water alone and support the need for further investigation.
CONCLUSION
Aspiration of small amounts of thickened water at intermittent time points resulted in significant pulmonary inflammation in a murine model of aspiration. Histologic evidence of lung inflammation and edema was still evident 10 days following the last aspiration event. Due to the widespread use of liquid thickeners in persons with aspiration risk, there is a pressing need for further research on the risks and benefits of liquid thickeners and the development of evidence-based recommendations for their use.
Acknowledgments
Supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH) through grant number UL1 TR001860 and linked award KL2 TR001859. Further funding was provided by T32 Cardio NIH T32-HL086350, and Denny & Jeanene Dickenson Fellowship. The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Footnotes
Presented as a poster presentation at the Combined Otolaryngology Spring Meetings (COSM) virtual poster session on May 15, 2020. Originally scheduled for oral presentation at the American Bronchoesophagological Association for COSM, Atlanta, Georgia, U.S.A., April 23, 2020, which was canceled due to the COVID-19 global pandemic.
BIBLIOGRAPHY
- 1.Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003;124:328–336. [DOI] [PubMed] [Google Scholar]
- 2.Ney D, Weiss J, Kind A, Robbins J. Senescent swallowing: impact, strategies and interventions. Nutr Clin Pract 2009;24:395–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garcia JM, Chambers E, Molander M. Thickened liquids: practice patterns of speech-language pathologists. Am J Speech Lang Pathol 2005;14:4–13. [DOI] [PubMed] [Google Scholar]
- 4.Vickers Z, Damodhar H, Grummer C, et al. Relationships among rheological, sensory texture, and swallowing pressure measurements of hydrocolloid-thickened fluids. Dysphagia 2015;30:702–713. [DOI] [PubMed] [Google Scholar]
- 5.Clave P, de Kraa M, Arreola V, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther 2006;24:1385–1394. [DOI] [PubMed] [Google Scholar]
- 6.Newman R, Vilardell N, Clave P, Speyer R. Effect of bolus viscosity on the safety and efficacy of swallowing and the kinematics of the swallow response in patients with oropharyngeal dysphagia: white paper by the European Society for Swallowing Disorders (ESSD). Dysphagia 2016;31:232–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia 2001;16:119–122. [DOI] [PubMed] [Google Scholar]
- 8.Goulding R, Bakheit AM. Evaluation of the benefits of monitoring fluid thickness in the dietary management of dysphagic stroke patients. Clin Rehabil 2000;14:119–124. [DOI] [PubMed] [Google Scholar]
- 9.Nativ-Zeltzer N, Kuhn MA, Imai DM, et al. The effects of aspirated thickened water on survival and pulmonary injury in a rabbit model. Laryngoscope 2018;128:327–331. [DOI] [PubMed] [Google Scholar]
- 10.Hanson B A review of diet standardization and bolus rheology in the management of dysphagia. Curr Opin Otolaryngol Head Neck Surg 2016;24:183–190. [DOI] [PubMed] [Google Scholar]
- 11.International Dysphagia Diet Standardisation Initiative (IDDSI). Complete IDDSI framework: Detailed definitions 2.0 Available at: https://ftp.iddsi.org/Documents/Complete_IDDSI_Framework_Final_31July2019.pdf. Accessed May 20, 2020.
- 12.Paakko P, Anttila S, Sormunen R, et al. Biochemical and morphological characterization of carbon tetrachloride-induced lung fibrosis in rats. Arch Toxicol 1996;70:540–552. [DOI] [PubMed] [Google Scholar]
- 13.Zachary JF, Frizzell LA, Norrell KS, Blue JP, Miller RJ, O’Brien WD. Temporal and spatial evaluation of lesion reparative responses following superthreshold exposure of rat lung to pulsed ultrasound. Ultrasound Med Biol 2001;27:829–839. [DOI] [PubMed] [Google Scholar]
- 14.Garcia JM, Chambers E, Molander M. Thickened liquids practice patterns of speech-language pathologists. Am J Speech Lang Pathol 2016;14:4–13. [DOI] [PubMed] [Google Scholar]
- 15.Castellanos VH, Butler E, Gluch L, Burke B. Use of thickened liquids in skilled nursing facilities. J Am Diet Assoc 2004;104:1222–1226. [DOI] [PubMed] [Google Scholar]
- 16.Logemann JA, Gensler G, Robbins J, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res 2008;51:173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robbins J, Gensler G, Hind J, et al. Comparison of 2 interventions for liquid aspiration on pneumonia incidence: a randomized trial. Ann Intern Med 2008;148:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rofes L, Arreola V, Mukherjee R, Swanson J, Clave P. The effects of a xanthan gum-based thickener on the swallowing function of patients with dysphagia. Aliment Pharmacol Ther 2014;39:1169–1179. [DOI] [PubMed] [Google Scholar]
- 19.Vilardell N, Rofes L, Arreola V, Speyer R, Clave P. A comparative study between modified starch and xanthan gum thickeners in post-stroke oropharyngeal dysphagia. Dysphagia 2016;31:169–179. [DOI] [PubMed] [Google Scholar]
- 20.Leonard RJ, White C, McKenzie S, Belafsky PC. Effects of bolus rheology on aspiration in patients with dysphagia. J Acad Nutr Diet 2014;114: 590–594. [DOI] [PubMed] [Google Scholar]
- 21.Slovarp L, Danielson J, Liss J. Inter-rater agreement of Clinicians’ treatment recommendations based on modified barium swallow study reports. Dysphagia 2018;33:818–826. [DOI] [PubMed] [Google Scholar]
- 22.Bhattacharyya N, Kotz T, Shapiro J. The effect of bolus consistency on dysphagia in unilateral vocal cord paralysis. Otolaryngol Head Neck Surg 2003;129:632–636. [DOI] [PubMed] [Google Scholar]
- 23.Araie T, Minagi HO, Usami Y, et al. Effect of xanthan gum-thickened liquid aspiration on the lungs in a mouse model. Oral Sci Int 2020;17(2):78–85. [Google Scholar]
- 24.Nishimura R, Sugiyama N, Fujishima I. The pulmonary tissue damage associated with the aspiration of gelatinizers in rats. J Med Dent Sci 2013;60:1–8. [PubMed] [Google Scholar]
- 25.Colombo JL, Hallberg TK. Airway reactivity following repeated milk aspiration in rabbits. Pediatr Pulmonol 2000;29:113–119. [DOI] [PubMed] [Google Scholar]
- 26.Johnson CL, Nyska A National Toxicology Program Nonneoplastiv lesion atlas: A guide for standardizing terminology in toxicologic pathology for rodents. Available at: https://ntp.niehs.nih.gov/nnl/cardiovascular/blood_vessel/arhypt/index.htm. Accessed May 20, 2020.
- 27.Zhao L Chronic hypoxia-induced pulmonary hypertension in rat: the best animal model for studying pulmonary vasoconstriction and vascular medial hypertrophy. Drug Discov Today Dis Models 2010;7:83–88. [Google Scholar]
- 28.Kaneoka A, Pisegna JM, Saito H, et al. A systematic review and meta-analysis of pneumonia associated with thin liquid vs. thickened liquid intake in patients who aspirate. Clin Rehabil 2017;31:1116–1125. [DOI] [PubMed] [Google Scholar]
- 29.Morley JE. Dysphagia and aspiration. J Am Med Dir Assoc 2015;16: 631–634. [DOI] [PubMed] [Google Scholar]
- 30.O’Keeffe ST. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified. BMC Geriatr 2018;18:167. [DOI] [PMC free article] [PubMed] [Google Scholar]


