Abstract
People with chronic obstructive pulmonary disease, cardiovascular disease, or hypertension have a high risk of developing severe coronavirus disease 2019 (COVID-19) and of COVID-19 mortality. However, the association between long-term exposure to air pollutants, which increases cardiopulmonary damage, and vulnerability to COVID-19 has not yet been fully established. We collected data of confirmed COVID-19 cases during the first wave of the epidemic in mainland China. We fitted a generalized linear model using city-level COVID-19 cases and severe cases as the outcome, and long-term average air pollutant levels as the exposure. Our analysis was adjusted using several variables, including a mobile phone dataset, covering human movement from Wuhan before the travel ban and movements within each city during the period of the emergency response. Other variables included smoking prevalence, climate data, socioeconomic data, education level, and number of hospital beds for 324 cities in China. After adjusting for human mobility and socioeconomic factors, we found an increase of 37.8% (95% confidence interval [CI]: 23.8%–52.0%), 32.3% (95% CI: 22.5%–42.4%), and 14.2% (7.9%–20.5%) in the number of COVID-19 cases for every 10-μg/m3 increase in long-term exposure to NO2, PM2.5, and PM10, respectively. However, when stratifying the data according to population size, the association became non-significant. The present results are derived from a large, newly compiled and geocoded repository of population and epidemiological data relevant to COVID-19. The findings suggested that air pollution may be related to population vulnerability to COVID-19 infection, although the extent to which this relationship is confounded by city population density needs further exploration.
Keywords: Coronavirus disease 2019, COVID-19, Air pollution, Chronic exposure
Graphical abstract
This research reported a national-level association with long-term exposure to air pollutants and COVID-19 cases covering 324 cities in China.
1. Introduction
Coronavirus disease 2019 (COVID-19) has rapidly spread across the world. To date, the virus that causes COVID-19, severe acute respiratory disease coronavirus 2 (SARS-CoV-2), has infected more than 103 million people and led to approximately 2.23 million fatalities, according to John Hopkins University. Currently, several reports suggest that air pollution is associated with an increased risk of death or severe illness among people with COVID-19 infection (Magazzino et al., 2020; Wu et al., 2020; Yao et al., 2020; Travaglio et al., 2021), on the basis of a biologically plausible pathway that might lead to serious deterioration (Conticini et al., 2020a; Frontera et al., 2020). SARS-CoV-2 can induce respiratory distress, so individuals with a compromised respiratory system are expected to be more vulnerable to infection (Qu et al., 2020), and people with pre-existing conditions are more vulnerable to severe infection. A meta-analysis showed that chronic obstructive pulmonary disease (COPD), cardiovascular disease, and hypertension are associated with severe COVID-19 infection and admission to the intensive care unit (ICU) (Jain and Yuan 2020).
Long-term exposure to air pollution affects lung function and is associated with the risk of many lung diseases, including an increased prevalence of COPD, acute lower respiratory illness, and lung cancer (Götschi et al., 2008; Lelieveld et al., 2015; Doiron et al., 2019; Liu et al., 2019). Moreover, recent research has put forth potential biological mechanisms of alveolar angiotensin-converting enzyme 2 (ACE-2) and population susceptibility to COVID-19 infection (Paital and Agrawal 2020). Additionally, chronic lung exposure to pollutants may lead to injury owing to pulmonary damage from oxidative stress, macrophage disfunction, and a disrupted epithelial barrier, thereby increasing susceptibility of the upper airways (Ciencewicki and Jaspers 2007; Frontera et al., 2020; Zhu et al., 2020). This implies that long-term exposure might increase vulnerability to lung diseases, thereby affecting the risk of COVID-19 infection in the whole population. However, recent studies tend to ignore the broad implications of long-term effects on the lungs. Furthermore, few studies have considered the important role of human travel and movement in the spatial spread of COVID-19, which might serve as a critical confounding variable in evaluating the effects of air pollution. We must understand the impact of air pollution exposure on COVID-19 infection and disease severity (Villeneuve and Goldberg 2020) in the general public, to help improve future modeling and disease burden calculations in countries around the world.
During the first epidemic wave of COVID-19 in China, to prevent further dissemination of the disease, officials in Wuhan prohibited all transport in and out of the city on January 23, 2020. In the following days, cities across mainland China launched the highest level emergency response and were able to control the epidemic outside of Wuhan by March 6, 2020. These measures substantially reduced air pollution, as confirmed by a significant reduction in pollution levels observed across cities in China between January and March 2020 (Chen et al., 2020a, ; Villeneuve and Goldberg 2020). These data from Chinese cities (excluding Wuhan) were ideal to assess the relationship between long-term average air pollution exposure and COVID-19 risk because these cities had widely distributed COVID-19 cases and highly variable historical air quality, which had been comprehensively surveyed under consistent criteria and data standards across the country. Air pollution produces both acute and long-term health effects, so a reduction in air pollution levels can serve as a natural experiment in how to offset potential acute effects of air pollution.
Considering the proven link between air pollution and the high risk of severe COVID-19 infection, we suspected that long-term exposure to air pollutants, which increases cardiopulmonary damage, would be associated with increased vulnerability to COVID-19. To test this hypothesis, we identified sociodemographic and behavioral confounders through a literature search. We first investigated the effect of travel and movement from Wuhan city, the location where COVID-19 was first recorded and from where it spread across China. During the Spring Festival holiday in 2020, approximately 4.3 million people traveled from Wuhan to other cities in China (Tian et al., 2020). These travel patterns were strongly associated with the total number of cases reported in each city, suggesting that the outbreaks across China were mainly seeded in Wuhan city.
2. Methods
2.1. Epidemiological and demographic data
We collected epidemiological data from official reports of the health commissions of 324 cities, excluding Wuhan (Table 1 ). These included daily reports from December 31, 2019 to March 6, 2020, but excluded newly reported, locally acquired infections. Data on the proportion of severe COVID-19 cases were obtained from official reports of Provincial Health Committees and used to interpolate the city-level values. The National Health Commission of the People’s Republic of China defined uniform diagnosis and treatment criteria of “2019 novel coronavirus pneumonia”, to measure the number of outbreaks. The reporting system was supported by local health-related departments, including hospitals and Centers for Diseases Control and Prevention (CDCs) at the provincial or county level (Zanin et al., 2020). In the first wave of the COVID-19 epidemic, these local CDCs sought to detect the largest possible number of infections, but people with a fever and a travel history to Wuhan were the priority groups for testing. Socioeconomic data, including the gross domestic product (GDP) per capita and number of hospital beds, were obtained from the China City Statistical Yearbook 2019. The age structure and illiteracy rate of people aged 15 years and older in each city were obtained from the Sixth National Population Census of the People’s Republic of China, which was conducted by the National Bureau of Statistics of People’s Republic of China in 2013. The prevalence of smoking and secondhand smoking among non-smokers was obtained from the Chinese National Nutrition and Health Survey (Wu et al., 2008; Xia et al., 2019). These were ecological and not individual data, which did not involve personal information; therefore, an ethics review was not required.
Table 1.
Databases and sources of coronavirus disease 2019 (COVID-19) and air pollution data.
| Database | data provider | Source |
|---|---|---|
| COVID-19 | ||
| Confirmed COVID-19 cases | Provincial Health Committees which contained data of each city | Official website of health commission of 34 provincial-level administrative units and 342 city-level units |
| Severe COVID-19 cases | Provincial Health Committees which contained data of each city | Official website Health commission of 34 provincial-level |
| COVID-19 deaths | Provincial Health Committees which contained data of each city | Official website of health commission of 34 provincial-level administrative units and 342 city-level units |
| Human mobility data | ||
| Outflow from Wuhan | Baidu location-based services mobile phone data provided by the telecommunications operators | https://qianxi.baidu.com/ |
| Within-city movements | The activities index of human mobility with a city | https://qianxi.baidu.com/ |
| Meteorological data | ||
| PM2.5, PM10, SO2, CO, NO2, and O3 | China National Environmental Monitoring Centre,2015–2019 | http://www.cnemc.cn/ |
| Temperature | Mean Temperature of Warmest/Coldest Quarter (2015–2019) | https://www.worldclim.org/data/bioclim.html |
| Rainfall | Precipitation of Warmest/Coldest Quarter (2015–2019) | https://www.worldclim.org/data/bioclim.html |
| Relative Humidity | National Meteorological Information Center (CMA Meteorological Data Center, 2015–2019) | http://data.cma.cn/ |
| Demographic data | ||
| Gross domestic product (GDP) | China City Statistical Yearbook 2019 | http://www.stats.gov.cn/tjsj/ndsj/2019/indexeh.htm |
| Age structure | Sixth National Population Census of the People’s Republic of China (2013) | http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm |
| Smoking and second-hand smoking prevalence | Chinese National Nutrition and Health Survey (NNHS) | PMID: 24698853 |
| Hospital beds | China City Statistical Yearbook 2019 | http://www.stats.gov.cn/tjsj/ndsj/2019/indexeh.htm |
| Illiteracy rate | Sixth National Population Census of the People’s Republic of China (2013) | http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm |
COVID-19, coronavirus disease 2019; PM2.5, particulate matter ≤ 2.5 μm; PM10, particulate matter ≤ 10 μm; SO2, sulfur dioxide; CO, carbon monoxide; NO2, nitrogen dioxide; O3, ozone; CMA, China Meteorological Administration.
2.2. Human mobility data
Human movements were tracked using mobile phone data from Baidu location-based services and telecommunications operators (Table 1). The number of recorded movements from Wuhan to other cities across China was calculated from 11 to January 23, 2020. On 23 January, movements from Wuhan dropped to nearly zero because of the travel ban. Movements within each city were recorded daily until 6 March. The within-city movement index was extracted from the same operators and was measured, to reflect the average times people traveled from their location inside each city every day. This database was developed to describe people’s compliance with physical distancing policies, which included suspending intracity public transport, closing entertainment venues, and banning public gatherings.
2.3. Source of air pollution and meteorological data
Original daily data for air pollutant concentrations, including particulate matter ≤2.5 μm and ≤10 μm and (PM2.5 and PM10, respectively), sulfur dioxide (SO2), carbon monoxide (CO), nitrogen dioxide (NO2), and ozone (O3) for each city, were obtained from air quality stations across China from January 2015 to March 2020. For each city, the average concentration for each pollutant before the COVID-19 outbreak (January 2020) was calculated across the entire available period. The data for temperature and precipitation during the coldest and warmest quarter in each city were extracted from WorldClim (Table 1), and the annual mean relative humidity was obtained from the National Meteorological Information Center.
2.4. Statistical methods
To quantify the effect of air pollution on COVID-19 risk, we used historical data for air quality between 2015 and 2019 and COVID-19 case reports. Sociodemographic and behavioral confounders were identified in a literature search. We searched PubMed and preprint servers (medRxiv) using the terms “air pollution”, “COVID-19”, and “SARS-CoV-2”, regardless of language and date. Among 74 studies identified, 55 were unrelated to public health. Of the remaining 19 studies, 6 used statistical models to investigate the relationship between air pollution and COVID-19 risk. Three papers involved large-scale and nationwide data from the United States (US), United Kingdom (UK), Italy, Spain, France, and Germany. The association between long-term exposure to air pollutants and COVID-19 risk was assessed using regression with a generalized linear model (GLM):
| (1) |
| (2) |
where Flow i is the passenger volume from Wuhan to city i during the Spring Festival 2020, before the Wuhan travel ban; Peak time of flow reflects the corresponding peak time. Within-city movements i shows the effect of social distancing within a city between the travel ban and March 6, 2020 in city i. GDP is the gross domestic product per capita of city i. Smoking prevalence and second-hand smoking prevalence in non-smokers was extracted from the published literature. The proportion of residents older than 65 years, illiteracy rate, number of hospital beds, population, and population density of city i were extracted from census data. Climate conditions are represented by temperature and rainfall in summer and winter. The relative humidity is the annual mean in city i. Latitude and longitude show the spatial distribution of city i. PM 2.5, PM 10, SO 2, CO, NO 2, and O 3 are the daily average concentration data of air pollutants in city i between January 1, 2015 and December 31, 2019. Air pollution variables were included in the model separately because of the high multicollinearity among them. βs are regression coefficients. The variation per unit (VPU) = [exp(variable coefficient) – 1] × 100% was used to describe the effect. The VPU can be interpreted as the percentage increase in the number of COVID-19 cases associated with a 10-μg/m3 increase in long-term average air pollutant exposure. We used the R software version 3.6.3, MASS package in the analyses (The R Foundation for Statistical Computing, Vienna, Austria).
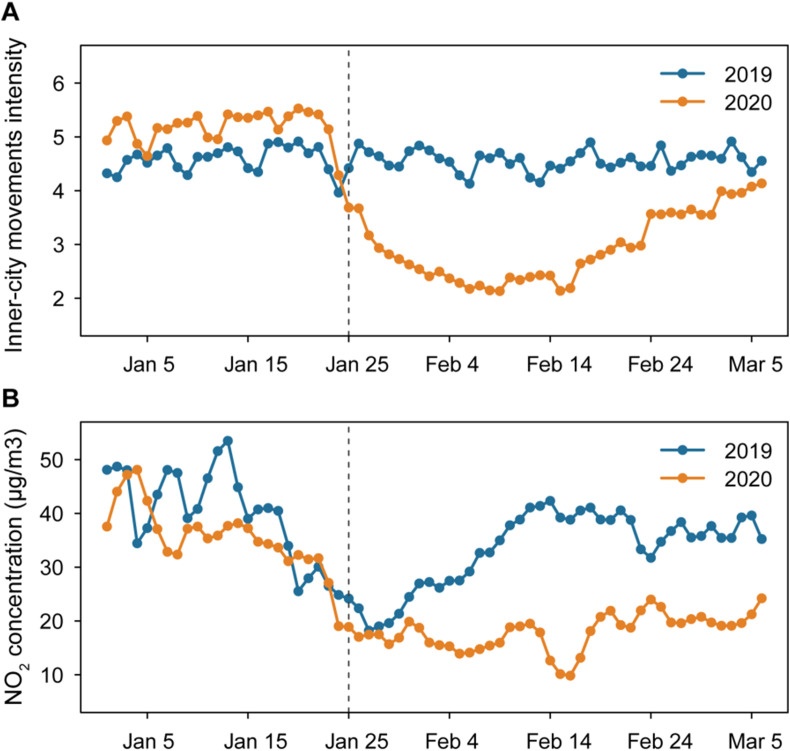
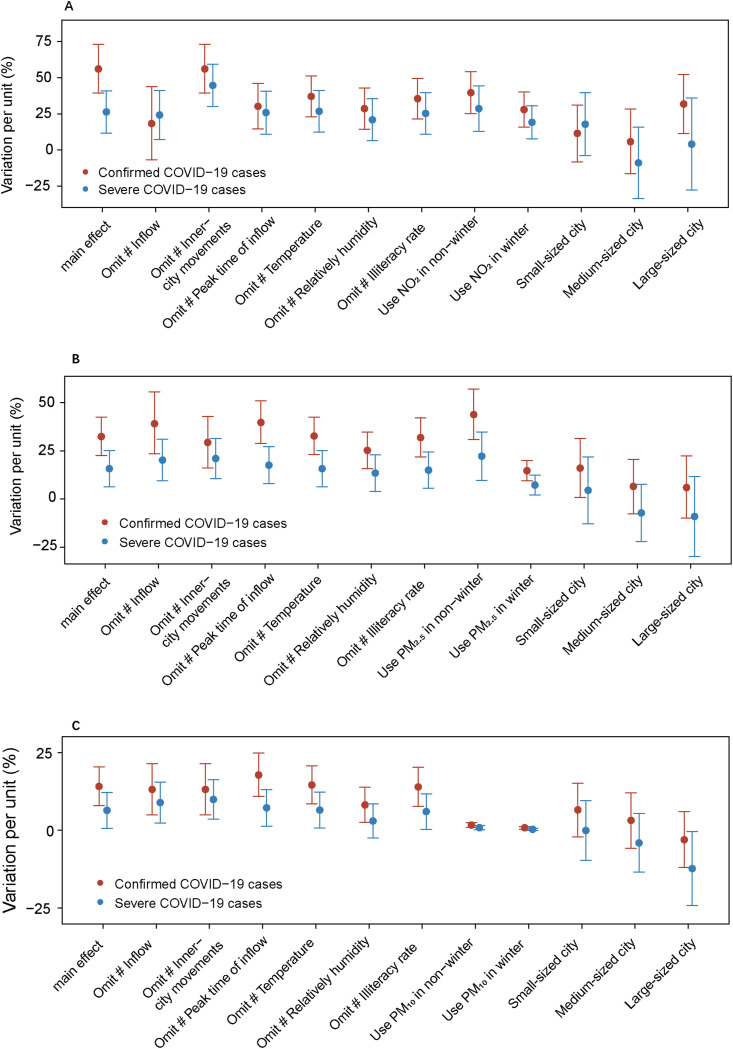
2.5. Sensitivity analysis
We conducted additional sensitivity analyses to assess the robustness of our results. We fit models, omitting adjusted variables separately and air pollutant concentrations in winter and non-winter seasons. To examine the associations after adjusting all other confounders, cities were categorized into three separate groups according to population size: small-sized (0–2.68 million population, n = 98), medium-sized (2.68–4.67 million, n = 97), and large-sized (4.67–30.75 million, n = 98) cities.
3. Results
3.1. Analysis of COVID-19 in China
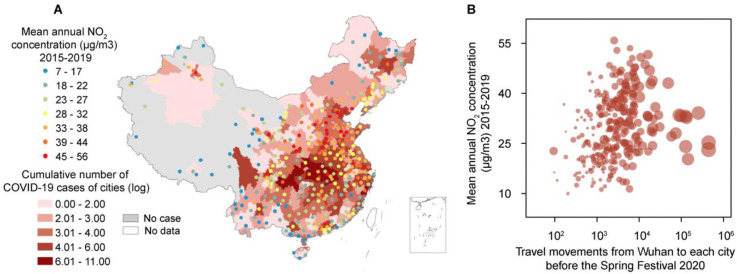
Between December 31, 2019 and March 6, 2020, a total of 81,132 cases of COVID-19 were reported across China. Of these, 62.6% (50,783/81,132) of cases were clustered in Wuhan city; the remaining 37.4% (30,349/81,132) of cases were distributed across 324 other cities. After March 6, 2020, there were very few locally acquired infections outside Wuhan city during the first wave. There was sustained local transmission of COVID-19 in Wuhan city, so data from that city were not included in the subsequent analysis. Fig. 1 shows that the 324 cities had widely distributed COVID-19 cases from December 31, 2019 to March 6, 2020. Additionally, with more travelers from Wuhan before the Spring Festival and more numerous COVID-19 cases reported in each city.
Fig. 1.
Air pollution exposure, coronavirus disease 2019 (COVID-19) cases, and travel movements in 324 cities of China during Spring Festival 2020. (A) Distribution of cities with data on nitrogen dioxide (NO2) concentrations and COVID-19 cases. Shading from light red to dark red represents cumulative number of confirmed COVID-19 cases in each city, from low to high, respectively, from December 31, 2019 to March 6, 2020; white area represents no data, and grey area represents no cases. Points colored from blue to red represent historic mean annual NO2 concentrations (μg/m3), from low to high, respectively, during January 2015 and December 2019, prior to the COVID-19 epidemic. (B) Association between the cumulative number of confirmed cases, the number of human movements from Wuhan to each city, and historic mean annual NO2 concentration. The area of the circles represents the cumulative number of cases reported by March 6, 2020. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
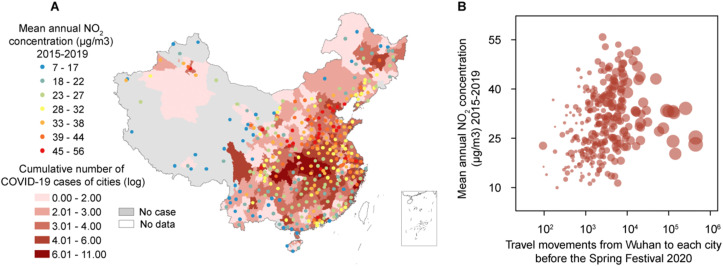
3.2. Air pollution reduction and travel restrictions
The average daily concentrations of PM2.5, PM10, SO2, CO, NO2, and O3 during the first wave of the COVID-19 epidemic were 52.13 μg/m3, 69.58 μg/m3, 0.93 mg/m3, 24.58 μg/m3, and 51.29 μg/m3among the 324 cities, respectively (Supplemental Table 1). On January 23, 2020, China banned travel movement from and to Wuhan, in an attempt to control the epidemic. After that date, a series of social distancing and lockdown policies were implemented throughout China to control the COVID-19 epidemic. During the lockdown period, air pollution emissions were markedly reduced. In particular, average levels of SO2, PM2.5, and PM10 were decreased by 21%, 18%, and 16%, respectively, compared with levels before implementation of the restriction policies. NO2 experienced a reduction of 8.17 μg/m3, which was one of the most significant changes among all examined air pollutants after the social distancing measures came into force. The results also indicated that these measures significantly reduced movement within cities during 2020 in comparison with that during 2019 (Fig. 2 ). The air quality in 2020 was also significantly improved, compared with that during the same period in 2019. The changes in average daily concentrations of PM2.5, PM10, SO2, CO, NO2, and O3 were −7.02% ± 32.9%, −19.25% ± 22.03%, −15.06% ± 20.56%, −5.46% ± 18.73%, −20.17% ± 29.56%, and 5.01% ± 16.01%, respectively, from 31 December to March 6, 2020.
Fig. 2.
(A) Average within-city movement intensity and (B) air pollutant concentration in 324 cities of China during the 2020 COVID-19 outbreak (orange line), compared with the same period in 2019 (blue line). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Effect of long-term exposure to air pollutants on COVID-19 cases and severe infections We collected data on a range of confounding variables, such as GDP per capita, smoking prevalence, climate data, illiteracy rate, and age composition (age > 65 years), together with travel movements from Wuhan and within-city movements (as measures of compliance with social distancing). These variables were adjusted in the statistical analysis. The population size of each city and number of COVID-19 deaths and hospital beds were not included in the model because of high multicollinearity with travel movements from Wuhan. The movements of approximately 4.3 billion people during the Spring Festival holiday also induced uncoordinated changes in actual population sizes across cities (Simiao et al., 2020). As expected, the number of COVID-19 cases in each city increased with increased population inflow from Wuhan; more infections were reported in cities that had more travelers from Wuhan. Overall, we observed positive and significant associations between confirmed cases of COVID-19 with historical air pollutant concentrations (Fig. 1A). In the 324 cities (except Wuhan) that had data on air quality, an increase of 10 μg/m3 in the NO2, PM2.5, and PM10 concentrations was associated with a 37.8% (95% confidence interval [CI]: 23.8%–52.0%), 32.3% (95% CI: 22.5%–42.4%), and 14.2% (7.9%–20.5%) increase in COVID-19 cases. We also examined the relationship between the number of severe COVID-19 cases and air pollutant levels. An increase of 10 μg/m3 in NO2, PM2.5, and PM10 concentrations was associated with a 26.3% (95% CI: 11.7%–40.8%), 15.7% (95% CI: 6.3%–25.2%), and 6.43% (95% CI: 0.6%–12.2%) increase in severe COVID-19 cases. The results were statistically significant and robust in sensitivity analyses (Table 2 and Fig. 3 ). The analysis was also carried out using separate datasets. Cities were categorized according to population size into small, medium, and large cities. There was no significant effect of long-term exposure to most of the air pollutants on susceptibility to COVID-19 infection when the data were stratified by population size. While, the effect persisted after stratification in NO2 and PM2.5 on confirmed COVID-19 cases among large cities and small cities, and the impact of PM10 in severe COVID-19 cases among large cities. This shows the importance of population as a confounding variable in the analysis.
Table 2.
Impact of historical air pollution exposure on cases of COVID-19.
| Confirmed COVID-19 cases |
Severe COVID-19 cases |
|||||
|---|---|---|---|---|---|---|
| Covariates | Coefficient (95%CI) | std | P | Coefficient (95%CI) | std | P |
| NO2 | 0.378(0.238,0.52) | 0.072 | <0.001 | 0.263(0.117,0.408) | 0.074 | <0.001 |
| Intercept | −1.697(-3.436,0.021) | 0.882 | 0.055 | −1.919(-3.437,-0.401) | 0.771 | 0.013 |
| Inflow from Wuhan | 0.007(0.007,0.008) | <0.001 | <0.001 | 0.016(0.013,0.019) | 0.002 | <0.001 |
| Within-city movements | −1.14(-1.382,-0.901) | 0.123 | <0.001 | −0.853(-1.098,-0.609) | 0.124 | <0.001 |
| Peak of inflow from Wuhan | 0.175(0.133,0.218) | 0.022 | <0.001 | 0.086(0.043,0.13) | 0.022 | <0.001 |
| Mean temperature of coldest quarter | −0.023(-0.045,-0.001) | 0.011 | 0.040 | 0.006(-0.014,0.027) | 0.010 | 0.528 |
| Relatively humidity | 0.048(0.029,0.067) | 0.010 | <0.001 | 0.028(0.012,0.045) | 0.008 | 0.001 |
| Illiteracy rate | 0.053(0.014,0.09) | 0.019 | <0.001 | 0.0188(-0.017,0.055) | 0.018 | 0.305 |
| PM2.5 | 0.323(0.225,0.424) | 0.051 | <0.001 | 0.157(0.063,0.252) | 0.048 | 0.001 |
| Intercept | −1.237(-2.841,0.329) | 0.809 | 0.128 | −1.313(-2.689,0.062) | 0.699 | 0.061 |
| Inflow from Wuhan | 0.007(0.006,0.007) | <0.001 | <0.001 | 0.015(0.012,0.018) | 0.002 | <0.001 |
| Within-city movements | −1.376(-1.617,-1.139) | 0.122 | <0.001 | −0.961(-1.192,-0.731) | 0.117 | <0.001 |
| Peak of inflow from Wuhan | 0.137(0.096,0.179) | 0.021 | <0.001 | 0.077(0.033,0.121) | 0.022 | 0.001 |
| Mean temperature of coldest quarter | −0.003(-0.027,0.022) | 0.012 | 0.790 | 0.01(-0.01,0.03) | 0.010 | 0.329 |
| Relatively humidity | 0.052(0.032,0.071) | 0.010 | <0.001 | 0.026(0.01,0.042) | 0.008 | 0.002 |
| Illiteracy rate | 0.049(0.008,0.087) | 0.020 | 0.016 | 0.019(-0.017,0.056) | 0.018 | 0.293 |
| PM10 | 0.142(0.079,0.205) | 0.032 | <0.001 | 0.0643(0.006,0.122) | 0.032 | <0.001 |
| Intercept | −1.183(-3.023,0.609) | 0.927 | 0.203 | −1.183(-2.861,0.217) | 0.927 | 0.203 |
| Inflow from Wuhan | 0.007(0.006,0.007) | <0.001 | <0.001 | 0.007(0.012,0.018) | <0.001 | <0.001 |
| Within-city movements | −1.346(-1.604,-1.092) | 0.131 | <0.001 | −1.346(-1.208,-0.742) | 0.131 | <0.001 |
| Peak of inflow from Wuhan | 0.148(0.104,0.194) | 0.023 | <0.001 | 0.148(0.037,0.126) | 0.023 | <0.001 |
| Mean temperature of coldest quarter | −0.009(-0.033,0.016) | 0.013 | 0.455 | −0.009(-0.011,0.03) | 0.013 | 0.455 |
| Relatively humidity | 0.054(0.032,0.076) | 0.011 | <0.001 | 0.054(0.012,0.046) | 0.011 | <0.001 |
| Illiteracy rate | 0.046(0.003,0.086) | 0.021 | 0.033 | 0.046(-0.021,0.053) | 0.021 | 0.033 |
COVID-19, coronavirus disease 2019; PM2.5, particulate matter ≤ 2.5 μm; PM10, particulate matter ≤ 10 μm; NO2, nitrogen dioxide; CI, confidence interval.
Fig. 3.
Variation per unit and 95% confidence intervals, (A) NO2, (B) PM2.5, and (C) PM10. The variation per unit (VPU) = [exp(variable coefficient) – 1] × 100%. The VPU can be interpreted as the percentage increase in the number of COVID-19 cases associated with a 10-μg/m3 increase in long-term average NO2 and PM2.5. The VPU from the main analysis was adjusted for confounding factors. In the sensitivity analyses, we omitted each confounding factor separately, and used seasonal air pollutant concentrations.
COVID-19, coronavirus disease 2019; PM2.5, particulate matter ≤2.5 μm; PM10, particulate matter ≤10 μm; NO2, nitrogen dioxide.
4. Discussion
In the present study, we clarified the association between long-term exposure to air pollution and vulnerability to COVID-19 infection during the first epidemic wave in China. The present results were derived from a large, newly compiled and geocoded repository of population and epidemiological data relevant to COVID-19. Indeed, several studies have evaluated the association between air pollution exposure and COVID-19 risk (Copat et al., 2020). Our finding was in line with studies based on large-scale nationwide data, including from the US (Wu et al., 2020), UK (Konstantinoudis et al., 2020; Travaglio et al., 2020; Travaglio et al., 2021), Italy (Conticini et al., 2020a; Fattorini and Regoli 2020), The Netherlands (Andree 2020), Spain, France, and Germany (Ogen 2020), as well as various provinces of China (Yongjian et al., 2020). Because the first COVID-19 wave was contained in China, meaning that we were able to investigate the impact of historical air pollution on COVID-19 risk and severity.
In the present study, we found statistically significant evidence that an increase in long-term exposure to NO2, PM2.5, or PM10 corresponded to an increase in the number of COVID-19 cases and severe infections. The findings are comparable to the results of previous studies in the US (Wu et al., 2020) and Northern Europe (Andree 2020), where levels of PM2.5 were also found to be strongly associated with COVID-19 incidence, after adjusting for multiple confounders. However, ours was the first study to use complete data from the first wave of the COVID-19 epidemic in China and to identify the association between long-term exposure to air pollution and COVID-19 risk, after controlling for many meteorological and demographic variables as well as human mobility data. The effects of NO2 and PM10 exposure were also clearly shown in our analysis model, which was a relatively new result. The effects of different components of air pollutants on COVID-19 should be further studied and confirmed.
Our results highlight the importance of air quality improvements with respect to health in China. In an attempt to control the epidemic, on January 23, 2020, non-essential travel was prohibited in and out of Wuhan city, a major transport hub and megacity of 11 million people. Subsequently, the highest level of emergency response was implemented throughout all of China, to reinforce containment of the COVID-19 epidemic. Interventions included the closure of entertainment venues, suspension of within-city public transport, and prohibition of travel to and from other cities in China. These stringent intervention measures significantly reduced air pollution levels in each city during this period (Le et al., 2020), which was confirmed in our monitoring results (Fig. 2). To some extent, the interventions provided an excellent opportunity to examine the benefits of improved air quality (Chen et al., 2020a). Reducing air pollutant concentrations would reduce the incidence of acute respiratory diseases and people’s susceptibility to numerous infectious diseases. Even assuming that problems existed within the multiple interventions, these results were in line with our expectations. Previous studies have demonstrated that exposure to air pollutants is associated with poorer lung function, often measured using forced vital capacity and forced expiratory volume in 1 s (Ackermann-Liebrich U, Leuenberger P et al., 1997, Forbes LJ, Kapetanakis V et al., 2009, Urman R, McConnell R et al., 2014, Adam M, Schikowski T et al., 2015). Exposure to particulate matter may be associated with an increased risk of cardiopulmonary diseases (Chen et al., 2019), aggravation of the case fatality rate of SARS (caused by SARS-CoV, another strain of coronavirus) (Cui et al., 2003), and impaired immune response (Wei and Tang 2018). Oxidant pollutants could also damage the innate immune response and increase host susceptibility to viruses by interfering with the function of macrophages(Karan et al., 2020; Qu et al., 2020). Nitrogen oxides (NOX) cause inflammatory responses and worsen pre-existing lung inflammation, resulting in a direct effect on the risk of respiratory diseases (Takahashi Y, Mochitate K et al., 1986, Conticini et al., 2020a), which is also shown in the Comparative Toxicogenomics Database (http://ctdbase.org). NO2 is primarily produced by traffic and factories and is less influenced by climatic conditions, so there were reductions in the concentration of NOX with a decline in within-city movements during the COVID-19 outbreak throughout China. Increased O3 and SO2 concentrations were associated with lower COVID-19 risk, which was also consistent with previous studies (Travaglio et al., 2020; Yongjian et al., 2020). However, the mechanisms underlying the impact of these pollutants on COVID-19 risk remain uncertain.
The association between long-term exposure to air pollution and vulnerability to COVID-19 may be affected by some confounders. We considered many variables for inclusion in the initial model, such as population, inflow from Wuhan, and the number of COVID-19 deaths and hospital beds. However, owing to the collinearity among these four variables, we retained only one of these variables. We believe that in the first COVID-19 wave, the population inflow from Wuhan was the most important factor affecting development of the epidemic. Therefore, only the variable of inflow from Wuhan was retained and the other three were eliminated from the final model. However, we believe that the variable of population is also very important; thus, a hierarchical analysis for the population variable was conducted separately. We found that the association between long-term exposure to air pollutants and vulnerability to COVID-19 differed among different-sized cities. In large-sized cities, the association was more obvious, which may be owing to better health care, better case reporting, and better testing policies in large cities. Therefore, the effect of population size is complex and needs further analysis.
As with other novel infectious diseases, there were many challenges in the diagnosis of COVID-19 during the first epidemic wave (Arons et al., 2020; Li et al., 2020). Concern has been expressed about the sensitivity and specificity of the tests initially used to identify people infected with SARS-CoV-2. The performance of the detection methods has improved over time (Carter et al., 2020). At the same time, there is a lack of adequate testing in most countries, and treatment of patients with COVID-19 in many jurisdictions is inadequate owing to overburdened health systems. As a result, many cases and deaths that were attributable to COVID-19 have not been confirmed. These issues may have some influence on the findings of this study. For example, this situation would lead to inaccuracies in the number of confirmed cases or severe cases of COVID-19 infection, which would cause some bias in the results. This may also be a reason that rates of greater severity of the disease are consistently lower. However, early studies during the epidemic can draw on the results of a pure transmission model. The present study focused on the association between air pollution and COVID-19 in the first wave in Wuhan, China. The variables included important human mobility data, such as inflow from Wuhan and peak time of inflow from Wuhan. These data would well reflect some important scientific problems in the early stages of an outbreak of a new infectious disease.
Several important caveats are worth mentioning. First, the data included here were all from mainland China; it is therefore unclear whether the findings can be generalized to other countries without data on historic air pollution exposure. Second, there are currently no high-quality records at city level regarding severe COVID-19 infections and ICU admissions, although we have attempted to fill this gap by using province-level reports. Third, air pollution data from ambient air quality stations across China do not necessarily reflect exposure to indoor air pollution; this may therefore bias the results. Finally, we do not know the exact number of cases because we do not know the number of asymptomatic and mildly symptomatic cases that may not have been recorded. These data will not be available until there has been a systematic survey of infection (e.g., via serological testing) across China. However, we reported a national-level disease pattern covering 324 cities and its potential association with long-term exposure to air pollutants.
5. Conclusions
In the present study, we found a significant positive association between long-term exposure levels to PM2.5, PM10, NO2, and the risk and severity of COVID-19 infection in China. Our findings suggest that air pollution may be related to population vulnerability to COVID-19. Interventions to control the COVID-19 outbreak in China successfully reduced air pollution levels and potentially prevented further cases of acute respiratory disease. Improved air quality may be conducive to reducing the hazards of respiratory infectious diseases. The link between COVID-19 and air pollution deserves more definitive and global data analysis.
Author contributions
Pai Zheng, designed the study, wrote and revised the manuscript. Zhangjian Chen, edited the manuscript, wrote and revised the manuscript. Yonghong Liu, collected the statistical data, conducted the analyses. Hongbin Song, collected and processed the LBS data. Chieh-Hsi Wu, conducted the analyses, edited the manuscript. Bingying Li, collected the statistical data. Moritz U.G. Kraemer, edited the manuscript. Huaiyu Tian, designed the study, edited the manuscript. Xing Yan, collected the statistical data. Yuxin Zheng, edited the manuscript. Nils Chr. Stenseth, designed the study. Guang Jia, designed the study, All authors read and approved the manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank the thousands of CDC staff and local health workers in China who collected data and continue to work to contain the COVID-19 pandemic in China and elsewhere.
Footnotes
This paper has been recommended for acceptance by Da Chen.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2021.116682.
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 91743114, 91643203, 82073616, 81673234]; the Research Council of Norway, which contributed to this work through the COVID-19 Seasonality Project [grant number 312740]; the Beijing Science and Technology Planning Project [grant number Z201100005420010]; the Beijing Natural Science Foundation [grant number JQ18025]; the Beijing Advanced Innovation Program for Land Surface Science; and the Young Elite Scientist Sponsorship Program by CAST (YESS) [grant number 2018QNRC001]. H.T. and M.U.G.K. acknowledge support from the Oxford Martin School; HT acknowledges support from the Military Logistics Research Program. The funders had no role in the study design; data collection, analysis, and interpretation; preparation of the manuscript; or the decision to submit the manuscript for publication.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ackermann-Liebrich U., Leuenberger P., Schwartz J., Schindler C., Monn C., Bolognini G., Bongard J.P., Brändli O., Domenighetti G., Elsasser S., Grize L., Karrer W., Keller R., Keller-Wossidlo H., Künzli N., Martin B.W., Medici T.C., Perruchoud A.P., Schöni M.H., Tschopp J.M., Villiger B., Wüthrich B., Zellweger J.P., Zemp E. Lung function and long term exposure to air pollutants in Switzerland. Study on air pollution and lung diseases in adults (SAPALDIA) team. Am. J. Respir. Crit. Care Med. 1997;155(1):122–129. doi: 10.1164/ajrccm.155.1.9001300. [DOI] [PubMed] [Google Scholar]
- Adam M., Schikowski T., Carsin A.E., Cai Y., Jacquemin B., Sanchez M., Vierkötter A., Marcon A., Keidel D., Sugiri D., Al Kanani Z., Nadif R., Siroux V., Hardy R., Kuh D., Rochat T., Bridevaux P.O., Eeftens M., Villani S., Phuleria H.C., Birk M., Cyrys J., Cirach M., de Nazelle A., Nieuwenhuijsen M.J., Forsberg B., de Hoogh K., Declerq C., Bono R., Piccioni P., Quass U., Heinrich J., Jarvis D., Pin I., Beelen R., Hoek G., Brunekreef B., Schindler C., Sunyer J., Krämer U., Kauffmann F., Hansell A.L., Künzli N., Probst-Hensch N. Adult lung function and long-term air pollution exposure. ESCAPE: a multicentre cohort study and meta-analysis. Eur. Respir. J. 2015;45(1):38–50. doi: 10.1183/09031936.00130014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andree P.J. Incidence of COVID-19 and connections with air pollution exposure: evidence from The Netherlands. Policy Research Working Paper. 2020:9221. [Google Scholar]
- Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R., Taylor J., Spicer K., Bardossy A.C., Oakley L.P.J.N.E. 2020. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter L.J., Garner L.V., Smoot J.W., Li Y., Zhou Q., Saveson C.J., Sasso J.M., Gregg A.C., Soares D.J., Beskid T.R. ACS Publications; 2020. Assay Techniques and Test Development for COVID-19 Diagnosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K., Wang M., Huang C., Kinney P.L., Anastas P.T. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4(6):e210–e212. doi: 10.1016/S2542-5196(20)30107-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Yin P., Meng X., Wang L., Liu C., Niu Y., Liu Y., Liu J., Qi J., You J., Kan H., Zhou M. Associations between coarse particulate matter air pollution and cause-specific mortality: a nationwide analysis in 272 Chinese cities. Environ. Health Perspect. 2019;127(1) doi: 10.1289/EHP2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J., Jaspers I.J. I.t. Air pollution and respiratory viral infection. 2007;19(14):1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Santo Signorelli S., Conti G.O., Ferrante M.J.E.R. 2020. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review; p. 110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ. Health. 2003;2:15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doiron D., de Hoogh K., Probst-Hensch N., Fortier I., Cai Y., De Matteis S., Hansell A.L. Air pollution, lung function and COPD: results from the population-based UK Biobank study. Eur. Respir. J. 2019;54(1):1802140. doi: 10.1183/13993003.02140-2018. [DOI] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264:114732. doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes L.J., Kapetanakis V., Rudnicka A.R., Cook D.G., Bush T., Stedman J.R., Whincup P.H., Strachan D.P., Anderson H.R. Chronic exposure to outdoor air pollution and lung function in adults. Thorax. 2009;64(8):657–663. doi: 10.1136/thx.2008.109389. [DOI] [PubMed] [Google Scholar]
- Frontera A., Cianfanelli L., Vlachos K., Landoni G., Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J. Infect. 2020;81(2):255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Götschi T., Heinrich J., Sunyer J., Künzli N. Long-term effects of ambient air pollution on lung function: a review. Epidemiology. 2008;19(5):690–701. doi: 10.1097/EDE.0b013e318181650f. [DOI] [PubMed] [Google Scholar]
- Jain V., Yuan J.-M. Systematic review and meta-analysis of predictive symptoms and comorbidities for severe COVID-19 infection. medRxiv. 2020 doi: 10.1101/2020.1103.1115.20035360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karan A., Ali K., Teelucksingh S., Sakhamuri S.J. G.h. r., policy The impact of air pollution on the incidence and mortality of COVID-19. 2020;5(1):1–3. doi: 10.1186/s41256-020-00167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantinoudis G., Padellini T., Bennett J.E., Davies B., Ezzati M., Blangiardo M. Long-term exposure to air-pollution and COVID-19 mortality in England: a hierarchical spatial analysis. medRxiv. 2020 doi: 10.1016/j.envint.2020.106316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le T., Wang Y., Liu L., Yang J., Yung Y.L., Li G., Seinfeld J.H. Unexpected air pollution with marked emission reductions during the COVID-19 outbreak in China. 2020;369(6504):702–706. doi: 10.1126/science.abb7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelieveld J., Evans J.S., Fnais M., Giannadaki D., Pozzer A.J.N. The contribution of outdoor air pollution sources to premature mortality on a global scale. 2015;525(7569):367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- Li X., Geng M., Peng Y., Meng L., Lu S.J.J. 2020. Molecular immune pathogenesis and diagnosis of COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Chen R., Sera F., Vicedo-Cabrera A.M., Guo Y., Tong S., Coelho M.S., Saldiva P.H., Lavigne E., Matus P. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 2019;381(8):705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magazzino C., Mele M., Schneider N.J.A.E. The relationship between air pollution and COVID-19-related deaths: an application to three French cities. 2020;279:115835. doi: 10.1016/j.apenergy.2020.115835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paital B., Agrawal P.K.J. 2020. Air pollution by NO 2 and PM 2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review; pp. 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu G., Li X., Hu L., Jiang G. An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19) Environ. Sci. Technol. 2020;54(7):3730–3732. doi: 10.1021/acs.est.0c01102. [DOI] [PubMed] [Google Scholar]
- Simiao C., Juntao Y., Weizhong Y., Chen W., Till B. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395(10226):764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi Y., Mochitate K., Miura T. Subacute effects of nitrogen dioxide on membrane constituents of lung, liver, and kidney of rats. Environ. Res. 1986;41(1):184–194. doi: 10.1016/s0013-9351(86)80180-3. [DOI] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.-H., Chen B., Kraemer M.U., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O.N., Yang R., Grenfell B.T., Pybus O.G., Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., Popovic R., Yu Y., Leal N., Martins L.M. medRxiv; 2020. Links between Air Pollution and COVID-19 in England. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M., Yu Y., Popovic R., Selley L., Leal N.S., Martins L.M. Links between air pollution and COVID-19 in England. Environ. Pollut. 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urman R., McConnell R., Islam T., Avol E.L., Lurmann F.W., Vora H., Linn W.S., Rappaport E.B., Gilliland F.D., Gauderman W.J. Associations of children’s lung function with ambient air pollution: joint effects of regional and near-roadway pollutants. Thorax. 2014;69(6):540–547. doi: 10.1136/thoraxjnl-2012-203159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeneuve P.J., Goldberg M.S.J. Methodological considerations for epidemiological studies of air pollution and the sars and COVID-19 coronavirus outbreaks. 2020;128(9) doi: 10.1289/EHP7411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei T., Tang M. Biological effects of airborne fine particulate matter (PM2.5) exposure on pulmonary immune system. Environ. Toxicol. Pharmacol. 2018;60:195–201. doi: 10.1016/j.etap.2018.04.004. [DOI] [PubMed] [Google Scholar]
- Wu X., Nethery R., Sabath M., Braun D., Dominici F.J. S.a. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. 2020;6(45) doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Huxley R., Li L., Anna V., Xie G., Yao C., Woodward M., Li X., Chalmers J., Gao R., Kong L., Yang X. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118(25):2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- Xia C., Zheng R., Zeng H., Zhou M., Wang L., Zhang S., Zou X., Sun K., Yang Z., Li H., Parascandola M., Islami F., Chen W. Provincial-level cancer burden attributable to active and second-hand smoking in China. Tobac. Contr. 2019;28(6):669–675. doi: 10.1136/tobaccocontrol-2018-054583. [DOI] [PubMed] [Google Scholar]
- Yao Y., Pan J., Wang W., Liu Z., Kan H., Qiu Y., Meng X., Wang W. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci. Total Environ. 2020;741:140396. doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yongjian Z., Jingu X., Fengming H., Liqing C. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanin M., Xiao C., Liang T., Ling S., Zhao F., Huang Z., Lin F., Lin X., Jiang Z., Wong S.-S. The public health response to the COVID-19 outbreak in mainland China: a narrative review. J. Thorac. Dis. 2020;12(8):4434–4449. doi: 10.21037/jtd-20-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.