Abstract
Purpose
To report the changes over time in ocular blood flow quantified by laser speckle flowgraphy (LSFG) in a treated large retinal arterial macroaneurysm (RAM).
Observations
A 72-year old female presented with sudden decreased vision in the left eye. Fundus examination revealed a RAM and vitreous hemorrhage (VH), which worsened over one month. A vitrectomy was performed to remove the VH, with 20% sulfur hexafluoride injected into the vitreous cavity. The VH recurred two weeks later and the RAM was found to have enlarged from one-quarter disc diameter (DD) to three DDs during a second vitrectomy. The RAM subsequently shrunk spontaneously to one DD without recurrent VH during the following 2 weeks. Beginning 4 weeks after the second vitrectomy we performed serial LSFG examinations of the RAM and found that the mean blur rate (MBR) of the RAM and retinal flow volume (RFV) in both the feeding arteriole and draining venule decreased as the RAM continued to involute.
Conclusions and importance
MBR and arteriolar and venular RFV measured by LSFG decreased with RAM involution. Longitudinal followup of blood flow by LSFG may be useful for noninvasive evaluation of the stability of RAMs.
Keywords: Retinal artery macroaneurysm, Followup, Blood flow, Laser speckle flowgraphy
1. Introduction
Retinal arterial macroaneurysm (RAM) was firstly reported by Robertson et al., in 1973.1 It occurs often in older women with hypertension.2, 3, 4 RAM is associated with vitreous hemorrhage and exudative change,3, 4, 5, 6, 7, 8, 9, 10, 11 but can naturally regress. Since severe visual dysfunction can occur in the event of aneurysm rupture in some cases, careful management to evaluate the activity of RAM over time is needed. Surgical excision may be needed if a RAM enlarges.5 RAM can be detected with fluorescein angiography (FA), indocyanine angiography (ICGA), or optical coherence tomography (OCT).6, 7, 8 Recently, it has been reported that optical coherence tomographic angiography (OCTA) may be useful for RAM.9,10 FA/ICGA and OCTA are used to visualize blood flow.4,6,7,9,10 Laser speckle flowgraphy (LSFG) is another noninvasive examination that can visualize blood flow. There have been no reports of LSFG assessment of the blood flow in RAMs. We report the change in ocular blood flow over time as measured by LSFG in a patient with a large treated RAM.
1.1. Case report
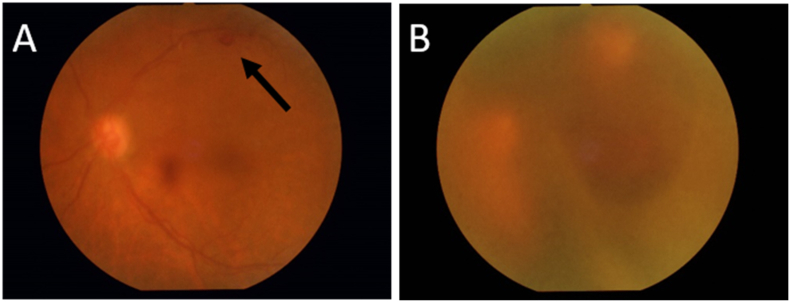
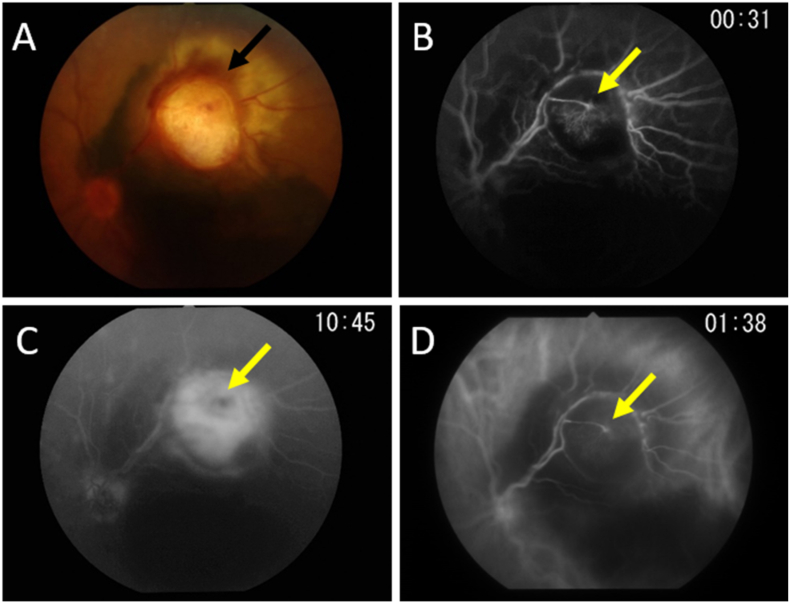
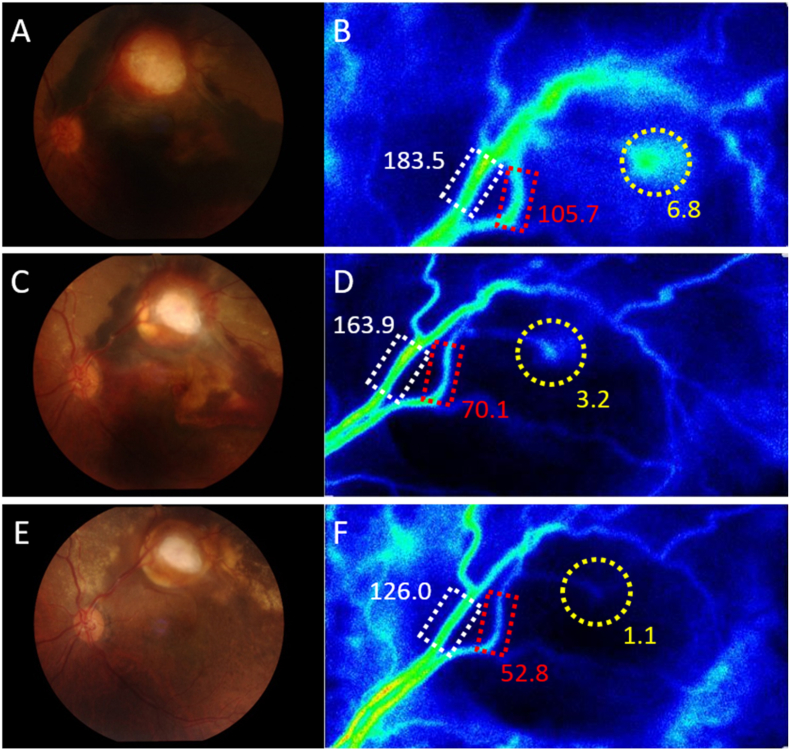
A 72-year old female with a history of systemic hypertension presented with decreased vision in the left eye. Her best-correct visual acuity was 20/40. Funduscopy revealed a one-quarter-disc diameter (DD) RAM with a small amount of vitreous hemorrhage (Fig. 1A). One month later, VA had decreased to counting fingers and the vitreous hemorrhage had enlarged (Fig. 1B). We performed a vitrectomy, finding subretinal hemorrhage in the macula. We injected 20% sulfur hexafluoride into the vitreous cavity. Recurrent VH occurred two weeks after the first surgery, so we performed a second vitrectomy, finding that the RAM had enlarged to three DD in size (Fig. 2A). We did not remove or puncture the RAM to prevent massive bleeding. One week after the second vitrectomy, FA/ICGA showed that the RAM had enlarged as well as intraoperative finding (Fig. 2B, C, D). No bleeding was seen subsequently, and the RAM began to shrink 2 weeks after reoperation (Fig. 3A). Beginning 4 weeks after the second vitrectomy we began performing serial ocular blood flow examinations using LSFG (Softcare Co., Ltd., Fukutsu, Japan). The region of interest (ROI) interrogated with LSFG was the same size at each measurement. Funduscopic examination at 7 weeks revealed the RAM to measure one DD in size (Fig. 3C). LSFG revealed the mean blur rate (MBR) of blood flow in the RAM to be 6.8 arbitrary units (AU). Four months after reoperation, there was no recurrent expansion of the RAM (Fig. 3E). We observed the longitudinal changes in ocular blood flow in the RAM and a retinal feeding arteriole and an adjacent venule on serial LSFG examinations. The MBR of the RAM and the retinal flow volumes (RFV) in both the feeding arteriole and draining venule gradually decreased during the followup period (Fig. 3B, D, F). In contrast, the MBR of the vessels in the disc area, which reflect the entire retinal circulation, were 26.9, 26.3, and 25.2 (AU) in the affected eye at two weeks, seven weeks and four months after reoperation, respectively, indicating preservation of the retinal circulation overall.
Fig. 1.
A. Color fundus photograph: 1/4 disc diameter (DD) retinal arterial macroaneurysm (RAM) with a small vitreous hemorrhage (arrow). B. One month later, the vitreous hemorrhage has worsened. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
A. Color fundus photograph: The RAM has enlarged to 3 DD in size (black arrow). B. Fluorescein angiography (FA) in the early phase, staining the RAM (yellow arrow). C. FA in late phase: extravasation around the RAM (yellow arrow). D. Indocyanine angiography (ICGA) in early phase: the appearance is identical to that in the FA early phase (yellow arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
A. Two weeks after reoperation, no bleeding is seen and the RAM has decreased in size. B. Four weeks after reoperation. The mean blur rates (MBR) in the RAM (yellow circle) and retinal flow volumes (RFVs) in an arteriole (red rectangle) and venule (white rectangle) were 6.8/105.7/183.5 arbitrary units (AU), respectively. C. Seven weeks after reoperation, the RAM has reduced to one DD in size. D. Seven weeks after reoperation, MBR in the RAM and RFVs were reduced to 3.2/70.1/163.9 AU. E. Four months after reoperation, there is no recurrent expansion of the RAM. F. Four months after reoperation, MBR in the RAM and both RFVs showed further reductions to 1.1/52.8/126.0 AU. The MBR of the RAM and RFVs of the arteriole and venule had decreased by −83.4/−50.0/−31.3%, respectively, at 4 months after reoperation compared with those at 4 weeks after reoperation. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
2. Discussion
VH and exudative changes may occur with RAM, and macular edema may result. Laser photocoagulation and intravitreal injection of anti-VEGF agents have been used to treat it.3,4,6,10, 11, 12 Vitrectomy and Nd:YAG laser subinternal limiting membrane hemorrhage drainage have been used in the treatment of vitreous and preretinal hemorrhage.6,12,13 Some cases of RAM can resolve spontaneously.2,3,7 FA/ICGA, OCT and OCTA have been used to diagnose RAM and evaluate the stability of RAM to prevent the visual loss by the hemorrhage and macular edema. Because surgical excision may be required in cases of enlarging RAMs,5,7 FA/ICGA is often used to evaluate the activity of the RAM, but FA/ICGA are slightly invasive examinations due to the rare side effect of the fluorescein. It has been reported that OCTA is able to evaluate RAM before and after treatment.9,10 Unlike FA/ICGA, OCTA requires a minimum constant rate of blood flow in order to visualize blood flow. LSFG allows noninvasive and quantitative evaluation of ocular blood flow. In our case, we confirmed the changes over time in blood flow by LSFG following the second vitrectomy. Seven weeks after the second vitrectomy, the RAM had spontaneously shrunk to one DD in size. Four weeks after the second vitrectomy, we first observed its flow characteristics with LSFG as expressed as MBR. LSFG revealed that the MBR of blood flow in the RAM decreased from 6.8 AU at 7 weeks to 1.1 AU at 4 months after the second vitrectomy as the RAM diminished, suggesting that LSFG can evaluate the stability of RAM noninvasively and quantitatively. RAMs often require multiple treatments due to rebleeding and exudative changes,2,3,5,10 necessitating periodic evaluation. Because LSFG enables noninvasive quantitative measurement of ocular blood flow, it may be useful to follow changes over time in ocular blood flow in RAMs. The shrinkage of this RAM indicated that the stability of RAM had subsided. Thus, the amount of blood flow as measured by LSFG might be a noninvasive prognostic index of RAM behavior.
Because this is a report of a single case and most RAMs do not enlarge to these dimensions, further studies with multiple cases are needed to confirm whether LSFG is an effective tool for their evaluation.
3. Conclusion
We were able to noninvasively evaluate ocular blood flow using LSFG in a large RAM following treatment. The blood flow decreased with the decreasing size of the RAM. LSFG may be a useful tool to evaluate the activity of RAM by measuring blood flow.
Funding
No funding.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Patient consent
The patient gave written informed consent for publication.
Declaration of competing interest
All authors report no financial disclosures.
Acknowledgment
We thank Libby Cone, MD, MA, from Yamada Translation Bureau, Inc. (https://www.ytrans.com/home.html) for editing drafts of this manuscript.
References
- 1.Robertson D.M. Macroaneurysms of the retinal arteries. Trans Am Acad Ophthalmol Otolaryngol. 1973;77(1):OP55–67. [PubMed] [Google Scholar]
- 2.Panton R.W., Goldberg M.F., Farber M.D. Retinal arterial macroaneurysms: risk factors and natural history. Br J Ophthalmol. 1990;74(10):595–600. doi: 10.1136/bjo.74.10.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavin M.J., Marsh R.J., Peart S., Rehman A. Retinal arterial macroaneurysms: a retrospective study of 40 patients. Br J Ophthalmol. 1987;71(11):817–825. doi: 10.1136/bjo.71.11.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes E.L., Dooley I.J., Kennelly K.P. Angiographic features and disease outcomes of symptomatic retinal arterial macroaneurysms. Graefes Arch Clin Exp Ophthalmol. 2016;254(11):2203–2207. doi: 10.1007/s00417-016-3388-9. [DOI] [PubMed] [Google Scholar]
- 5.Oie Y., Emi K. Surgical excision of retinal macroaneurysms with submacular hemorrhage. Jpn J Ophthalmol. 2006;50(6):550–553. doi: 10.1007/s10384-006-0369-2. [DOI] [PubMed] [Google Scholar]
- 6.Koinzer S., Heckmann J., Tode J., Roider J. Long-term, therapy-related visual outcome of 49 cases with retinal arterial macroaneurysms: a case series and literature review. Br J Ophthalmol. 2015;99(10):1345–1353. doi: 10.1136/bjophthalmol-2014-305884. [DOI] [PubMed] [Google Scholar]
- 7.Ohno-Matsui K., Hayano M., Futagami S. Spontaneous involution of a large retinal arterial macroaneurysm. Acta Ophthalmol Scand. 2000;78(1):114–117. doi: 10.1034/j.1600-0420.2000.078001114.x. [DOI] [PubMed] [Google Scholar]
- 8.Miura M., Muramatsu D., Hong Y.J. Noninvasive vascular imaging of ruptured retinal arterial macroaneurysms by Doppler optical coherence tomography. BMC Ophthalmol. 2015;15(1):79–83. doi: 10.1186/s12886-015-0077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alnawaiseh M., Schubert F., Nelis P. Optical coherence tomography (OCT) angiography findings in retinal arterial macroaneurysms. BMC Ophthalmol. 2016;16(1):120–125. doi: 10.1186/s12886-016-0293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang V.S., Schwartz S.G., Flynn Optical coherence tomography angiography of retinal arterial macroaneurysm before and after treatment. Case Rep Ophthalmol Med. 2018 doi: 10.1155/2018/5474903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown D.M., Sobol W.M., Folk J.C., Weingeist T.A. Retinal arteriolar macroaneurysms: long term visual outcome. Br J Ophthalmol. 1994;78(7):534–538. doi: 10.1136/bjo.78.7.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen Y.Y., Lin L.Y., Chang P.Y. Laser and anti-vascular endothelial growth factor Agent treatments for retinal arterial macroaneurysm. Asia Pac J Ophthalmol. 2017;6(5):444–449. doi: 10.22608/APO.201766. [DOI] [PubMed] [Google Scholar]
- 13.Sonmez K., Ozcan P.Y. Nd:YAG laser photodisruption for multilevel premacular hemorrhage due to isolated retinal venous macroaneurysm. Case Rep Ophthalmol Med. 2017 doi: 10.1155/2017/4630187. [DOI] [PMC free article] [PubMed] [Google Scholar]