Abstract
This case presents a patient with a remote history of complex posterior urethral repair related to a prior motorcycle accident who presented to the urology clinic in urinary retention with associated lower urinary tract symptoms. Due to his altered anatomy, traditional outlet procedures were deferred due to significant reported risks of post treatment urinary incontinence. Decision was made to proceed with prostatic artery embolization, and at follow up he reported resolution of his urinary retention and significant symptomatic improvement in his voiding without development of urinary incontinence.
Keywords: Prostatic artery embolization, Incontinence, Bladder outlet obstruction, Benign prostatic hyperplasia, Posterior urethroplasty, Supra-crural rerouting
Introduction
Prostatic artery embolization (PAE) is an alternative to traditional interventions for patients with lower urinary tract symptoms (LUTS) interested in more minimally invasive solutions. PAE is not yet part of the standard pathway for treating benign prostatic hyperplasia (BPH) and more studies are needed to improve patient selection for this technically challenging treatment modality. Historically, its use has been in poor surgical candidates with prostatic sizes >40mL and LUTS unrelated to neurologic causes, though the only relative contraindication to PAE is severe atherosclerotic disease.1 A comprehensive literature review suggests that patients with adenomatous dominant BPH or who are catheter dependent prior to PAE could predict a higher likelihood of success as compared to patients otherwise.2
One of the most significant risks with traditional BPH therapies, like transurethral resection of the prostate (TURP) is urinary incontinence. Incontinence is related to sphincter trauma (30%), detrusor irritability (20%), mixed urinary incontinence (30%), incomplete resection (5%), and bladder neck contracture or urethral stricture (10%). Post-TURP incontinence is more common in the setting of posterior urethral reconstruction as these patients have a damaged external sphincter and are dependent on their bladder neck/internal sphincter. The bladder neck is routinely resected during TURP.
We report the evaluation and treatment of BPH related LUTS via PAE in a 77-year-old man with a history of posterior urethroplasty and its implications in maintenance of continence.
Case presentation
A 77-year-old male with remote history of MVA resulting in closed pelvic straddle injury and bulbous urethral stricture presented to the urology clinic with LUTS. Following his injury, the patient developed a long segment posterior urethral defect requiring complex posterior urethroplasty with associated supra-crural urethral rerouting. Rerouting required translocation of the urethra around the lateral side of the right corporal body and through the bony defect created by the pubectomy, allowing the urethra to pass through a small furrow in the pubis to avoid compression between the corpus and the bone. As is typical of posterior urethroplasties, especially those this complex, his continence depended exclusively on the internal sphincter/bladder neck.
Following repair he initially did well, but eventually developed urinary retention. In December 2019, he was found to have a wide-caliber urethral stricture and underwent direct vision internal urethrotomy with placement of indwelling Foley catheter for two weeks. Afterwards, he performed clean intermittent catheterization (CIC) three times daily with no periods of spontaneous urination suggesting that the stricture was not responsible for his symptoms.
He was then referred to our reconstructive urology clinic for evaluation. In addition to urinary retention requiring CIC, he endorsed frequency, nocturia, hesitancy, and weak stream despite medical therapy with tamsulosin and finasteride. He had not had prior outlet procedures. Estimated prostate size was 72g by TRUS. International Prostate Symptom Score (IPSS) was 34 with a quality-of-life (QoL) score of 4. Cystoscopy demonstrated a bulbar urethral narrowing behind the right corpus cavernosum, but easy passage of the 16.5 French flexible cystoscope, as well as bilobar prostate enlargement with apparent outlet obstruction. Urodynamic testing demonstrated normal compliance and obstructive voiding, low peak flow (4 mL/sec) and voiding pressures of up to 73 cm H2O and video images suggestive of BOO, not urethral stricture obstruction.
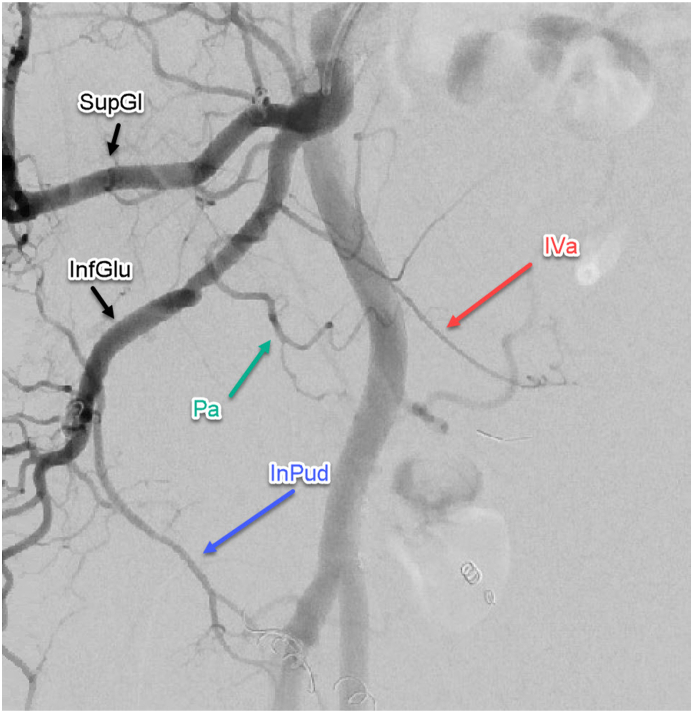
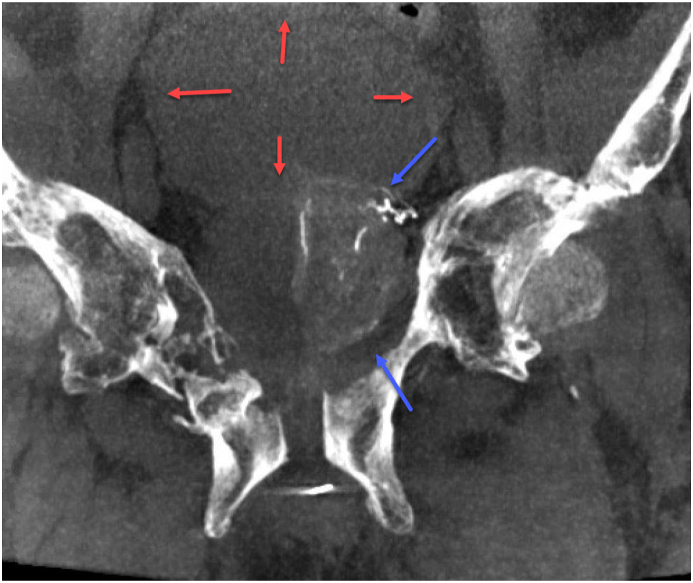
Due to concern for post-TURP incontinence related to his prior PFUDD, traditional outlet procedures were deferred, and he was referred to interventional radiology to discuss PAE (Fig. 1). He subsequently underwent PAE, and at follow up reported significantly improved symptoms without any reported incontinence or CIC requirements at the three and six-month follow ups (Fig. 2). IPSS reduced to 14 with QoL score of 3. He will continue to be followed in clinic at yearly intervals for repeat Uroflow and PVR measures.
Fig. 1.
Right Internal Iliac Angiogram (SVa = Sup Vesicular artery, InPu = Internal Pudendal, SuGl = Superior Gluteal, InfGlu = Inferior Gluteal, PA = Prostate artery).
Fig. 2.
Coronal Cone Beam CT Prostate Enhancement (red arrows = bladder; blue arrows = prostate). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Discussion
The most common cause of posterior urethral injuries is motor vehicle crash, with the most common complications related to repair of these injuries being incontinence and erectile dysfunction. The primary deciding factor in repair of the injury is the length of defect and how to achieve a tension free anastomosis. Patients with defects <2cm can often be repaired with urethral mobilization alone, 29.6% require splitting of the corporal bodies, and 31.6% require inferior pubectomy. Although controversial, corporal re-routing is reserved for very long defects, especially those with compromised bulbar urethras (2–4.7% of cases) with an average defect length of 4.75cm.3
TURP is the gold standard operative intervention for BOO secondary to an enlarged prostate to which other modalities are often compared. PAE has become an increasingly popular modality since the late 2000s as an alternative for patients who are not suitable or are high risk for TURP-related complications. Ray et al. compared 89 patients undergoing TURP to 216 patients undergoing PAE, with subsequent retrograde ejaculation in 24.1% of patients undergoing PAE versus 47.5% of patients undergoing TURP.4 In terms of incontinence, these studies found only 2 patients in each arm developed incontinence, but none of these patients had any history of urethral stenosis or prior reconstruction.4
TURP following posterior urethroplasty carries an increased risk of incontinence, as continence following posterior urethroplasty relies solely on the proximal mechanisms, chiefly the bladder neck, which is often sacrificed during TURP. Even when urethral rerouting is not utilized, the external sphincter must be sacrificed in order to complete the anastomosis, as the most common site of injury is at the membranous urethra. PAE has been demonstrated non-inferior to TURP when performed by highly trained interventional radiologists with proper patient selection.5
Traumatic posterior urethral injury is more likely to occur earlier in life preceding the need for BPH treatments. In counseling these patients, it is important to address the risk of postoperative urinary incontinence associated with outlet procedures that address the bladder neck. PAE can be considered as a possible solution for these patients, though data remains sparse, as well as availability of this modality.
Conclusion
This case presents a novel indication and excellent outcome for PAE in the setting of BOO in a patient with prior posterior urethral repair without development of post treatment urinary incontinence. Further investigation is necessary, though PAE shows promise in this setting.
Declaration of competing interest
All authors have no conflict of interest to declare.
References
- 1.Picel A.C., Hsieh T.C., Shapiro R.M., Vezeridis A.M., Isaacson A.J. Prostatic artery embolization for benign prostatic hyperplasia: patient evaluation, anatomy, and technique for successful treatment. Radiographics. 2019;39(5):1526–1548. doi: 10.1148/rg.2019180195. [DOI] [PubMed] [Google Scholar]
- 2.Sun F., Lucas-Cava V., Sánchez-Margallo F.M. Clinical predictive factors in prostatic artery embolization for symptomatic benign prostatic hyperplasia: a comprehensive review. Transl Androl Urol. 2020;9(4):1754–1768. doi: 10.21037/tau-20-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Webster G.D., Peterson A.C. Simple perineal and elaborated perineal posterior urethroplasty. Arab J Urol. 2015;13(1):17–23. doi: 10.1016/j.aju.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ray A.F., Powell J., Speakman M.J. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study) BJU Int. 2018;122(2):270–282. doi: 10.1111/bju.14249. [DOI] [PubMed] [Google Scholar]
- 5.Napal Lecumberri S., Insausti Gorbea I., Sáez de Ocáriz García A. Prostatic artery embolization versus transurethral resection of the prostate in the treatment of benign prostatic hyperplasia: protocol for a non-inferiority clinical trial. Res Rep Urol. 2018;10:17–22. doi: 10.2147/RRU.S139086. [DOI] [PMC free article] [PubMed] [Google Scholar]