Abstract
Management of periacetabular lesions involves complex clinical decision making. The modified Harrington procedure with total hip arthroplasty can recreate pelvic stability with a cement rebar construct as well as a functional hip. This study analyzes the modified Harrington procedure to assess construct longevity and patient outcomes. We queried a prospectively maintained database to identify all patients at a large academic medical center from 2017 to 2019 with periacetabular metastatic disease treated with a modified Harrington. Medical records were reviewed and complications, patient outcomes, Musculoskeletal Society Tumor (MSTS) scores, and implant survival were recorded. A total of nine patients were treated with the modified Harrington between 2017 and 2019. At maximum follow- up there were zero revisions or longterm complications. The mean preoperative MSTS score was 2.2 (range, 0-18), compared to the mean postoperative MSTS score of 17.7 (range, 9-25) recorded at a mean 4 (range, 1-30) months following surgery (p<0.001). The modified Harrington technique total hip technique for reconstruction in periacetabular metastatic bone disease is a safe procedure with effective symptom relief, improvement in function, and excellent implant survivorship.
Key words: Acetabulum, pelvis, orthopedics, surgery, metastasis
Introduction
The pelvis is one of the most common bony locations of metastatic cancer.1Within the periacetabular region, metastases cause significant pain and functional impairment, often in patients who have a poor prognosis. First-line therapy for periacetabular metastases includes chemotherapy and/or radiotherapy with analgesics, often with interventional radiology procedures.2 However, operative intervention is indicated for some patients with significant structural defects, and those who exhibit functional impairment and are reasonable operative candidates. The decision to operate is complex and often nuanced. Typically, periacetabular reconstruction in this setting is a palliative procedure. Furthermore, these procedures afford a greater quality of end-of-life by increasing mobility and function than that achieved by conservative measures alone.3– 9 However, due to the extensive loss of the bone of the acetabulum, these reconstructions are technically demanding and fraught high rates of complication.
There exist a variety of methods for periacetabular reconstruction in advanced metastasis. These defects are classified according to Kevin Harrington, who in 1981 first described a technique for reconstruction in severe acetabular compromise using a rebar built with acrylic cement and Steinmann pins.10 Since then, periacetabular reconstruction has advanced to intralesional curettage followed by saddle prostheses, allograft or allograft prosthetic composites, pasteurized autografts, porous implants, or custom-made prosthetic components.11-16 Small to medium-sized case series have described the outcomes of periacetabular reconstruction using a combination of these techniques. Additionally, more recent constructs such as trabecular metal augments and three-dimensional [e.g. three-dimensional (3D)] designs have demonstrated high rates of long-term survival.17 However, there is little consensus on which technique demonstrates the highest rate of implant survival and superior patient functioning while achieving the lowest rates of complication and cost.
Purpose
In this study we assessed the surgical, functional, and oncologic outcomes of patients who underwent a modified Harrington procedure for reconstruction of the periacetabular region in the setting of advanced metastasis. We sought to: i) determine the improvement in function and quality of life after the procedure; ii) characterize the complication profile surrounding the modified Harrington technique; and iii) assess implant and overall patient survival.
Materials and Methods
Patient selection
Following Institutional Review Board approval, consecutive patient records from a prospectively maintained surgical database were reviewed retrospectively. Nine patients, all with periacetabular lesions, underwent the modified Harrington procedure within a single, high volume tertiary academic medical center. The inclusion criteria used to identify patients were greater than 18 years of age, and with diagnostic confirmation of metastatic periacetabular disease, including myeloma and lymphoma. Only patients who underwent surgical treatment between 2017 and 2019 using the modified Harrington approach were included. Patients were excluded from subsequent analyses if there was no mention of a modified Harrington approach used. Thus, the decision to reconstruct was patient-specific and varied by case, with no predefined operative criterion. Metastatic lesions were classified according to Harrington: Class I lesions (acetabular lateral cortices and superior/ medial walls intact); Class II (medial wall deficiency); Class III (Figure 1); and Class IV (widespread loss of integrity to the iliac wing).10 Each patient underwent a thorough musculoskeletal workup including a complete physical examination and identification of the primary tumor when possible, with necessary biopsy and imaging prior to surgery.
Surgical procedure
All procedures were carried out by a fellowship trained orthopedic oncologist. A similar approach was utilized for all patients independent of lesion class. Patients were placed in a lateral position and given general or spinal anesthetic. A standard posterior approach to the hip was performed. Short external rotators were dissected, and a capsulotomy was performed after which the hip was dislocated. An osteotomy was made in the femoral neck and then deep acetabular retractors were placed to visualize the metastatic defect. The acetabulum was then reamed. Following identification and curettage of the lesion, the defect was copiously irrigated with hydrogen peroxide followed by a saline solution and treated with our plasma scalpel. For each case, fully threaded 6.5 mm acetabular bone screws (Zimmer Orthopedics, Warsaw, IN, USA) were inserted retrograde through the defect into the ilium, ischium, and superior pubic rami. The depth, direction and number of screws placed were dependent upon the lesion class and extent of bony destruction. The screws acted as a scaffold or rebar into which cement was then placed (Figure 2).
Bone Cement (Zimmer Orthopedics, Warsaw, IN, USA) was interdigitated among the screws and curettaged portion of the acetabulum to create the rebar construct. After an adequate screw-rebar construct was obtained, a fully cemented acetabular cup was placed in the acetabulum in appropriate abduction and version. Femoral components could either be cemented or press fit, depending on the quality of bone, age of the patient, and disease status. All patients were allowed to bear full weight in the immediate post-operative period, and two patients received adjuvant radiation therapy. Follow-up varied by case.
Functional and surgical outcomes
Preoperative and postoperative outcome scores were documented retrospectively to assess the functional outcome of each patient using the Musculoskeletal Tumor Society [e.g. Musculoskeletal Tumor Society (MSTS)] score. The MSTS is a Likert-type scale that assesses areas such as pain, function, emotional state, ability to walk, and gait in patients with metastatic disease of the lower extremity. Due to the small sample size, there was no follow-up threshold (months) before which MSTS scores were omitted. Second, implant survival was recorded and assessed, and revision was recorded if applicable. Revision was defined as surgical intervention for a failed implant in an effort to either restore or remove the implant. Major, minor, and mechanical complications were recorded for each patient, and included perioperative (short-term) and mid to long-term complications when applicable.
Statistics
Continuous and categorial variables of interest were analyzed using descriptive statistics and reported as the mean [standard deviation (SD)] or mean (95% confidence interval, CI) when applicable. Implant and patient survival were assessed using methods proposed by Kaplan and Meier.18 Implant survival was calculated from the date of surgery to the last recorded date of follow-up in the medical record, if no revision had occurred. Overall survival was calculated from the date of surgery to the last recorded follow-up in the medical record if no documentation of death was available. Mean preoperative MSTS scores (allgroup) were compared against postoperative MSTS scores using a comparison of means (t test), and the changes are represented as percent improvements over time. A p<0.05 was considered statistically significant, and all analyses were performed on SPSS version 26.0 (IBM Corp., Armonk, NY, USA).
Figure 1.
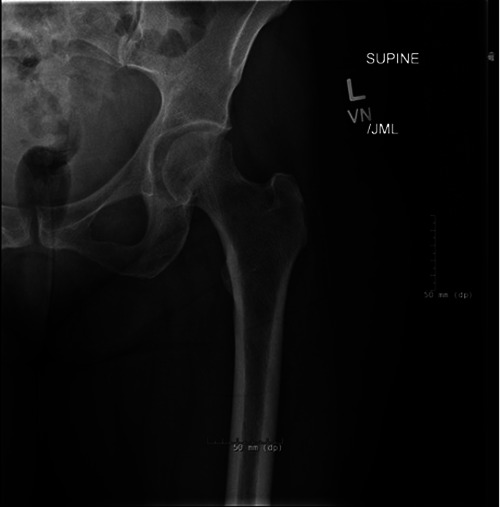
Antero-posterior radiograph of the left hip and pelvis demonstrating posterior acetabular metastases with medial wall insufficiency. This patient had metastatic lung adenocarcinoma to the acetabulum (Class III) and underwent a modified Harrington procedure for periacetabular reconstruction.
Figure 2.
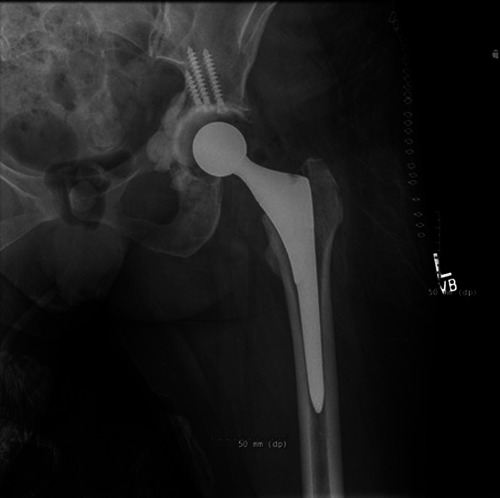
Post-operative radiograph of a patient with metastatic disease demonstrating the modified Harrington technique. In this patient, three acetabular screws were driven retrograde through the acetabular roof, after which cement was interdigitated to create a rebar for medial and posterior acetabular wall reconstruction.
Results
Patient and disease characteristics
Patient demographics are summarized in Table 1.
Nine patients between 2017 and 2019 met the inclusion criteria. The mean age at surgery was 59.7 years (range, 40-81 years), and there was female predominance (78%). The most common diagnosis was metastatic breast carcinoma (3 cases, 67%), followed by 1 case each of multiple myeloma, adenocarcinoma of lung, metastatic soft tissue sarcoma of the pelvis, renal cell carcinoma, adenocarcinoma of the colon, and endometrial carcinoma. One lesion (11%; multiple myeloma) was Class I, 2 (22%; breast and renal cell) were Class II, and the remaining 6 (67%; 2 = breast; 1 = endometrial, spindle cell, lung, colon) were Class III according to the aforementioned Harrington classification system. One patient (multiple myeloma) was treated concomitantly for a pathologic femoral neck fracture that occurred prior to surgery. Six (67%; 2 = breast; 1= lung, spindle, renal cell, multiple myeloma) of the 9 patients received neoadjuvant radiotherapy while 5 (56%) received neoadjuvant chemotherapy (2 = breast, 1 = multiple myeloma, lung, spindle cell). Two (22%; lung, renal cell) received adjuvant radiation while 6 (67%; 2 = breast; 1= lung, spindle, renal cell, multiple myeloma) received adjuvant chemotherapy. The mortality rate was 33% (3 cases) at a mean (range) of 5.3 (3-10) months, and the mean (range) follow-up for all patients was 9 (1-40) months.
Surgical characteristics and implant survival
Surgical characteristics and implantrelated events are summarized in Table 2.
The mean (SD) duration of surgery (minutes) was 153.7 (25.1), and the mean (SD) intraoperative blood loss (mL) was 503.5 (577.7). One patient (metastatic breast carcinoma) experienced an intraoperative calcar split of the femoral neck which was repaired with cerclage wires. The mean (SD) size (cm) of tissue/bone removed at largest dimension was 5.4 (0.8) and surrounding soft tissue invasion was observed in 2 (22%; lung, colon) cases. The mean amount of blood products (packed red cells) received throughout the entire hospital stay was two (range, 0-5), and the mean length of hospital stay was 4.8 days (range, 3-10 days). Zero (0%) patients developed minor or major post-operative complications including wound complication, seroma/hematoma formation, or surgical site infection. Zero patients underwent revision surgery by maximum recorded followup. The implant survivorship was 100% at a mean of 5.9 months (range, 1-43 months) follow-up.
Functional outcomes
Functional outcomes are summarized in Table 3.
The mean (range) preoperative Musculoskeletal Society Tumor (MSTS) score was 2.2 (0-18), compared to the mean (range) postoperative MSTS score of 17.7 (9-25) recorded at a mean (range) 4 (1-30) months following surgery based on available follow-up data (p<0.001). Overall, there was an 88% improvement in scores from the preoperative to postoperative period.
Table 1.
Demographics.
| Characteristics | N. |
|---|---|
| Eligible cases | 9 |
| Sex | |
| Female | 7 |
| Male | 2 |
| Mean/median follow-up (months) (range) | 9.1 (1-43) |
| Mean age at surgery (years) (range) | 61.1 (40-81) |
| Age | |
| >60 | 5 |
| <60 | 4 |
| Radiotherapy | |
| Preoperative | 4 |
| Postoperative | - |
| Pre- and Postoperative | 2 |
| None | 2 |
| Data unavailable | 1 |
| Chemotherapy | |
| Preoperative | 0 |
| Postoperative | 1 |
| Pre- and Postoperative | 5 |
| None | 2 |
| Data unavailable | 1 |
| Primary malignant tumor | |
| Breast | 3 |
| Renal | 1 |
| Myeloma | 1 |
| Endometrial | 1 |
| Colon | 1 |
| Lung | 1 |
| Spindle Cell Sarcoma | 1 |
| Last status | |
| Dead due to cancer | 3 |
| Dead due to other/unknown cause | 0 |
| Alive | 6 |
Table 2.
Surgical characteristics.
| Characteristics | N. |
|---|---|
| Operation | |
| Primary only | 8 |
| Revision | 1 |
| Mean lesion size (cm) (range) | 3.91 (0.8-7) |
| Harrington’s classification | |
| Class I | 1 |
| Class II | 2 |
| Class III | 6 |
| Class IV | - |
| Mean operation blood loss (mL) (range) | 661 (200-2200) |
| Mean operation time (minutes) (range) | 157 (116-191) |
| Mean duration of hospital stays (days) (range) | 5.2 (3-10) |
| Type of prosthesis | |
| Uncemented regular | 4 |
| Cemented longstem | 3 |
| Cemented regular | 1 |
| Revision – Original prosthesis left in place | 1 |
| Head size (mm) | |
| 28 | 2 |
| 32 | 3 |
| 36 | 4 |
Discussion
Our institution has demonstrated consistently high rates of improved patient function in the acute postoperative setting, as well as implant durability. Though a small sample size with limited follow-up, the results are promising. The use of clinically reported (MSTS scores) and patientreported outcomes before and following periacetabular reconstruction is welldescribed. In literature reporting the outcomes of the modified Harrington technique, disability has been measured by a variety of instruments, and each shows consistent improvement from the preoperative to postoperative period.3,5,19–21 Similar improvements in pain and disability have also been observed in studies of other techniques for periacetabular reconstruction. 15,22,23 Typically, patients with metastatic disease to the acetabulum have significant (subjective and objective) impairment before surgery, often with intense, localized pain and other physiologic complications depending on the disease burden. Furthermore, these patients may present with concomitant pathologic fracture as one of our patients did, rendering them immobile and subject to a much poorer quality of life. In this study, each of the patients who underwent surgery had a significantly impaired quality of life beforehand, as evidenced by low mean preoperative MSTS scores. The improvement in the scores in the post-operative period suggests a strong functional benefit of this procedure, and the percent improvement seen in this study aligns with those of the literature. Facilitating independent ambulation and decreasing pain by way of surgery is warranted in select patients, particularly in those with disease refractory to chemotherapy, radiation, interventional radiology techniques, and particularly those with fracture or larger impending lesions. Thus, we believe the modified Harrington technique, when selected for in specific patients, permits excellent short-term functional improvement.
There are relatively few patient series in the literature that document the treatment planning, operative reconstruction, and functional or implant-related outcomes of the modified Harrington in the modern era. In 2000, Nilsson et al. described the outcomes of 32 patients treated with threaded pins and a cemented total hip construct with a mean survival of 11 months.24 They suggest the technique offers a durable, safe solution to patients with advanced periacetabular destruction from metastatic tumor. Then in 2007, Wangsaturaka et al. demonstrated improved function in 14 patients treated with a modified Harrington, though two patients in this study developed hip dislocation and acetabular loosening requiring closed reduction.25 In an attempt to address these complications, various groups have explored constructs such as a three-pin Harrington procedure (cannulated screw placement anterograde through the iliac to acetabular roof), a Burch-Schneider cage for reconstruction, percutaneous acetabuloplasty, and recently, porous tantalum augments and other prosthetic implants, some of which are designed with 3D-printing. 7,15,19,22,26 These constructs likely offer marginally increased stability compared to the modified Harrington, though there are no prospective trials comparing the modified Harrington to these other, often more expensive techniques.
While most periacetabular reconstructions afford adequate functional improvement with better ambulation, the majority of patients portend a poor prognosis regardless. In light of this prognosis, there exists a need for immediate restoration of weightbearing and decreased pain, though at a lower cost given a shorter life expectancy. Recent research has demonstrated a costsavings benefit for the screw-cement rebar scaffold and polyethylene cup reconstruction (modified Harrington variant), with which our institution has had initial success.21 Bernthal et al. suggest this variant is durable and provides sick patients good functional improvement at a lower cost than, for example, porous shells, tantalum cups, cages, and prosthetic components. In their study of 52 acetabular reconstructions, the authors record a 9.6% failure rate (according to the Henderson classification) and a 2% major surgical complication rate.21 Complication profiles in this surgery vary by implant design. Compared to other modern techniques for periacetabular reconstruction, the cement-screw-rebar scaffold with polyethylene cup appears to be safe and durable. The cup-cage reconstruction technique described by Hoell et al. in 2012 demonstrated a relatively high rate of mechanical failure (20%), compared to methods including the porous tantalum (Khan et al., 5%) and rebar with flanged metal cup (Marco et al., 10.9%).15,22,27 Though a small sample size with limited follow-up, the results of our current study suggest a safe option with good short-term reliability (0% revision rate). This advantage is particularly beneficial in patients with a shorter life expectancy.
There are significant limitations to this study. The retrospective nature of this study precludes any meaningful comparative analysis. Thus, we are not able to assess outcomes compared to other commonly utilized techniques for periacetabular reconstruction. Within the current study, the small sample size and relatively short follow- up limit the external validity of the results. However, a majority of these patients unfortunately have limited life expectancy, and regaining immediate, short-term functional outcome is arguably the most clinically important measure. One strength of this study is the consistency in surgical approach as each procedure was performed by the same surgeon. After careful patient selection, each hip was approached in a similar manner, minimizing bias that may be introduced by collecting data from multi-institutions.
Table 3.
Functional outcome scores.
| Characteristics | N. | MSTS scores | ||
|---|---|---|---|---|
| Preoperative mean | Postoperative mean | p | ||
| Eligible cases | 9 | 3.89 | 18.78 | <0.01 |
| Sex | ||||
| Female | 7 | 3.57 | 20.57 | <0.01 |
| Male | 2 | 5 | 12.5 | 0.13 |
| Age | ||||
| >60 | 5 | 1.4 | 19.4 | <0.01 |
| <60 | 4 | 4.25 | 18 | 0.05 |
| Metastatic load | ||||
| Solitary bone | 1 | 0 | 23 | N/A |
| Multiple bones | 3 | 8.33 | 23.67 | 0.13 |
| Bone and other | 5 | 2 | 15 | 0.03 |
| Harrington classification | ||||
| Class I | 1 | 0 | 23 | N/A |
| Class II | 2 | 14 | 20.5 | 0.58 |
| Class III | 6 | 1.17 | 17.5 | <0.01 |
| Alive at 3 months | ||||
| No | 3 | 3.33 | 11.67 | <0.01 |
| Yes | 6 | 4.17 | 22.33 | 0.21 |
MSTS, Musculoskeletal Tumor Society.
Conclusions
Metastatic bone disease to the periacetabular region presents a challenging clinical scenario. For patients that fail conservative measures, surgical management is indicated. The modified Harrington procedure is a surgical reconstructive option used in patients with advanced acetabular bone disease. The results of modern studies suggest the modified Harrington is a standardized procedure with low complication rates. Additional studies have characterized this procedure as one that greatly improves postoperative functional and oncologic outcomes within a group of patients with a very poor prognosis. The current literature suggests both the rate of complications and mortality are high. Furthermore, in addition to the modified Harrington there exist different techniques for periacetabular reconstruction, each with varying success. Results from small series suggest newer prostheses have shown promising early functional and radiographic outcomes. However, other studies have demonstrated a cost-savings benefit with the modified Harrington, by avoiding these newer prostheses in patients with a short life expectancy. In the current study, our institution has demonstrated consistently high rates of improved patient function in the acute postoperative setting, as well as implant durability. At the study conclusion, we report zero revision surgeries with significant improvement in clinical outcome scores. These results are consistent with some of the better- reported outcomes in the literature regarding the modified Harrington. To conclude, the current study, along with data that demonstrate a relatively low complication profile, suggest this procedure is safe and permits favorable short-term functional outcomes in patients with advanced periacetabular metastasis.
References
- 1.Vena VE, Hsu J, Rosier RN, O’Keefe RJ. Pelvic reconstruction for severe periacetabular metastatic disease. Clin Orthop 1999;362:171-80. [PubMed] [Google Scholar]
- 2.Guzik G. Treatment of metastatic lesions localized in the acetabulum. J Orthop Surg 2016;11:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erol B, Aydemir AN, Onay T, Topkar MO. Reconstruction of advanced periacetabular metastatic lesions with modified Harrington procedure. Acta Orthop Traumatol Turc 2016;50:178-85. [DOI] [PubMed] [Google Scholar]
- 4.Shahid M, Saunders T, Jeys L, Grimer R. The outcome of surgical treatment for peri-acetabular metastases. Bone Joint J 2014;96-B:132-6. [DOI] [PubMed] [Google Scholar]
- 5.Kask G, Nieminen J, van Iterson V, et al. Modified Harrington’s procedure for periacetabular metastases in 89 cases: a reliable method for cancer patients with good functional outcome, especially with long expected survival. Acta Orthop 2020;91:341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan T, Zhao Z, Tang X, et al. Improving functional outcome and quality of life for patients with metastatic lesion of acetabulum undergoing cement augmentation. Med (Baltimore) 2019;98: e17029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tillman RM, Myers GJC, Abudu AT, et al. The three-pin modified “Harrington” procedure for advanced metastatic destruction of the acetabulum. J Bone Joint Surg Br 2008;90:84-87. [DOI] [PubMed] [Google Scholar]
- 8.Coomber R, Lopez D, Carrothers AD. Advancement of the Harrington technique for reconstruction of pathological fractures of the acetabulum. BMJ Case Rep 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charles T, Ameye L, Gebhart M. Surgical treatment for periacetabular metastatic lesions. Eur J Surg Oncol 2017;43:1727-32. [DOI] [PubMed] [Google Scholar]
- 10.Harrington KD. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg Am 1981;63:653-64. [PubMed] [Google Scholar]
- 11.Rowell P, Lowe M, Sommerville S, Dickinson I. Is an acetabular cage and cement fixation sufficiently durable for the treatment of destructive acetabular metastases? Clin Orthop 2019;477: 1459-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weisstein JS. CORR Insights®: LUMiC® endoprosthetic reconstruction after periacetabular tumor resection: short-term results. Clin Orthop 2017;475:696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hipfl C, Stihsen C, Puchner SE, et al. Pelvic reconstruction following resection of malignant bone tumours using a stemmed acetabular pedestal cup. Bone Joint J 2017;99-B:841-8. [DOI] [PubMed] [Google Scholar]
- 14.Abolghasemian M, Tangsaraporn S, Drexler M, et al. The challenge of pelvic discontinuity: cup-cage reconstruction does better than conventional cages in mid-term. Bone Joint J 2014; 96-B:195-200. [DOI] [PubMed] [Google Scholar]
- 15.Hoell S, Dedy N, Gosheger G, et al. The Burch-Schneider cage for reconstruction after metastatic destruction of the acetabulum: outcome and complications. Arch Orthop Trauma Surg 2012;132:405-10. [DOI] [PubMed] [Google Scholar]
- 16.Marchetti P, Binazzi R, Vaccari V, et al. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty 2005;20:730-7. [DOI] [PubMed] [Google Scholar]
- 17.Li Q, Chen X, Lin B, Ma Y, et al. Threedimensional technology assisted trabecular metal cup and augments positioning in revision total hip arthroplasty with complex acetabular defects. J Orthop Surg 2019;14:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457-481. [Google Scholar]
- 19.Durfee RA, Sabo SA, Letson GD, et al. Percutaneous acetabuloplasty for metastatic lesions to the pelvis. Orthopedics 2017;40:e170-5. [DOI] [PubMed] [Google Scholar]
- 20.Lozano-Calderon SA, Kaiser CL, Osler PM, Raskin KA. Cemented total hip arthroplasty with retrograde ischioacetabular steinmann pin reconstruction for periacetabular metastatic carcinoma. J Arthroplasty 2016;31:1555-60. [DOI] [PubMed] [Google Scholar]
- 21.Bernthal NM, Price SL, Monument MJ, et al. Outcomes of modified Harrington reconstructions for nonprimary periacetabular tumors: an effective and inexpensive technique. Ann Surg Oncol 2015;22:3921-8. [DOI] [PubMed] [Google Scholar]
- 22.Khan FA, Rose PS, Yanagisawa M, et al. Surgical technique: Porous tantalum reconstruction for destructive nonprimary periacetabular tumors. Clin Orthop 2012;470:594-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benevenia J, Cyran FP, Biermann JS, et al. Treatment of advanced metastatic lesions of the acetabulum using the saddle prosthesis. Clin Orthop 2004;426: 23-31. [DOI] [PubMed] [Google Scholar]
- 24.Nilsson J, Gustafson P, Fornander P, Ornstein E. The Harrington reconstruction for advanced periacetabular metastatic destruction: good outcome in 32 patients. Acta Orthop Scand 2000;71:591-6. [DOI] [PubMed] [Google Scholar]
- 25.Wangsaturaka P, Asavamongkolkul A, Waikakul S, Phimolsarnti R. The results of surgical management of bone metastasis involving the periacetabular area: Siriraj experience. J Med Assoc Thail Chotmaihet Thangphaet 2007;90:1006-13. [PubMed] [Google Scholar]
- 26.Colman MW, Karim SM, Hirsch JA, et al. Percutaneous acetabuloplasty compared with open reconstruction for extensive periacetabular carcinoma metastases. J Arthroplasty 2015;30: 1586-91. [DOI] [PubMed] [Google Scholar]
- 27.Marco RA, Sheth DS, Boland PJ, et al. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am 2000;82:642-51. [DOI] [PubMed] [Google Scholar]


