Abstract
Unicompartmental Knee Arthroplasty (UKA) is an effective surgical option for managing unicompartmental knee osteoarthritis; it represents 10% of all knee arthroplasties worldwide, increasing 32.5% annually in the United States alone. Despite evolution in surgical technique and implant design, success rate and long-term survivorship of UKA have been historically lower than Total Knee Arthroplasty (TKA). The most common causes of UKA failure leading to revision are polyethylene wear, progression of arthritis, aseptic loosening and patella-femoral symptoms due to poor patient selection in many cases. Historically, UKA revisions have presented technical challenges mainly related to managing residual bone defects and ligament insufficiency ultimately leading to knee instability: the fear of instability has often pushed surgeons to lower the threshold for an increase of the intra-articular level of constraint. Unfortunately, the use of more constrained implants requires sacrificing bone stock and has been related to higher rates of re-revision secondary to recurrence of aseptic loosening. Because of these challenges, the authors developed a surgical technique that could combine balancing the knee during revision surgery with the use of the less constrained polyethylene option. To achieve this, we started evaluating a novel device (VERASENSE, Orthosensor, FL) designed to support soft tissue balancing during primary TKA. This intraoperative sensing technology dynamically quantifies intra-articular loads during TKA trial with the goal of correcting any residual imbalance in real time. Herein we propose a novel surgical technique, which might allow use of a primary TKA design characterized by a lower level of constraint, instead of a constrained or hinged revision knee system, during UKA revision. A key aspect of this technique is the use of sensing technology during intraoperative stability testing.
Key words: TKA, sensor, revision, total knee arthroplasty, instability
Introduction
Unicompartmental Knee Arthroplasty (UKA) is an effective surgical option for managing unicompartmental knee osteoarthritis; it represents 10% of all knee arthroplasties worldwide, increasing 32.5 % annually in the United States alone. Despite evolution in surgical technique and implant design, success rate and long-term survivorship of UKA have been historically lower than Total Knee Arthroplasty (TKA). The most common causes of UKA failure leading to revision are polyethylene wear, progression of arthritis, aseptic loosening and patella-femoral symptoms due to poor patient selection in many cases. Historically, UKA revisions have presented technical challenges mainly related to managing residual bone defects and ligament insufficiency ultimately leading to knee instability: the fear of instability has often pushed surgeons to lower the threshold for an increase of the intra-articular level of constraint. Unfortunately, the use of more constrained implants requires sacrificing bone stock and has been related to higher rates of re-revision secondary to recurrence of aseptic loosening.1
Because of these challenges, the authors developed a surgical technique that could combine balancing the knee during revision surgery with the use of the less constrained polyethylene option. To achieve this, we started evaluating2 a novel device (VERASENSE, Orthosensor, FL) designed to support soft tissue balancing during primary TKA. This intraoperative sensing technology dynamically quantifies intraarticular loads during TKA trial with the goal of correcting any residual imbalance in real time. Herein we propose a novel surgical technique, which might allow use of a primary TKA design characterized by a lower level of constraint, instead of a constrained or hinged revision knee system, during UKA revision. A key aspect of this technique is the use of sensing technology during intraoperative stability testing.
Surgical technique
An accurate preoperative plan is mandatory before any UKA revision: all patients undergo extensive preoperative radiological evaluation, which includes anterior-posterior and lateral weight-bearing radiographs, a weight-bearing pangonogram, and a patella view. A CT study is often required to quantify bone loss following aseptic loosening of the implant, and in all cases of painful UKA to evaluate component malalignment. Note that a Posterior- Stabilized (PS) primary system (Persona, Zimmer-Biomet, USA) and a semi-constrained revision system (Persona Revision Knee System, Zimmer-Biomet, USA) are always available at the time of surgery since the final level of constraint is intraoperatively selected. With the patient in supine position, a standard midline incision following the previous approach and a medial para-patellar capsulotomy are performed.
The first intra-articular surgical gesture is represented by removal of any scar tissue usually present in the suprapatellar pouches and behind the patellar tendon; the fat pad is then removed. The tibial insert is usually removed using a ¾ inch osteotome slided between the polyethylene and the metal component. At this point, all the visible osteophytes are removed from the patella, the distal femur and proximal tibia; the anterior and posterior cruciate ligaments are then removed.
Before removing the other components, the entry point for the intramedullary alignment guide is determined (usually 1cm proximal and 1cm medial to the top of the femoral notch), the guide is inserted and the distal femur cutting gig is secured at an angle according to the preoperative plan. The femoral component (medial or lateral) is addressed first and removed with the subsequent use of straight and flexible osteotomies, oscillating and reciprocating saws, paying extreme attention to conserving the femoral bone-stock. Once the femoral component has been removed, femoral bone loss is quantified. The femoral component is then repositioned on the femur during removal of the tibial component in order to protect the femoral bone stock from iatrogenic damage while working on the tibia (Figure 1). The tibial component is then removed with the subsequent use of flexible osteotomies, stacked osteotomies and oscillating saw, paying extreme attention to conserving the tibial bone stock. Once the tibial component has been removed, tibial bone loss is quantified (Figure 2). When all components have been removed, the level of constraint (primary PS or semi-constrained system) is determined. The general rule followed by the authors is that if the distal femoral and proximal tibial bone loss is no more than 15 mm on each side, a primary PS design is intraoperatively chosen, making the final decision on the stability of the implant and the integrity of the collateral ligaments at the time of sensor-guided trial testing.
The distal femoral cut is then completed and the femoral sizing guide is placed on the distal femur: the rotational alignment of the component is determined in accordance with the surgical trans-epicondylar axis to avoid excessive internal or external rotation of the femoral component due to bone loss, a typical error if the posterior condylar axis is used as a reference. The final, four-inone, cutting jig is then placed on the distal femur after sizing and the final cuts (anterior, posterior, chamfers) are performed. The Persona PS size specific trial femoral component is placed on the femur and the PS box cut is then completed. It must be considered that mild distal condyle bone loss can be present and tolerated, since it will be filled during cementation (Figure 1). Attention is then paid to the tibia. After exposure of the tibial plateau, the initial resection level is set such that the sawblade just fits on top of the area characterized by bone loss, which should be only “refreshed” with an oscillating saw (Figure 2). The varus-valgus alignment of the final tibial cut is determined by an extramedullary rod set at the center of the ankle. The alignment of the knee is checked by placing a 10-15 mm spacer block, keeping the knee in extension. If the alignment is satisfactory, the tibial component size and rotational alignment according to the middle third of the tibial tuberosity are determined; the final preparation of the tibial component is then completed. Please note that this included reaming the tibial canal in order to accept a 30 mm, cemented tibial stem (“stubby”). At this point (Figure 3), the femoral and tibial component trials are inserted and the Postero-Stabilized (PS) Verasense tibial sensor is inserted, the knee is brought to extension (not hyperextension) and the extensor mechanism is temporarily closed with a clamp.2 Please note that the trial is routinely inserted and then removed so that it can be re-zeroed due to the small plastic deformation of the trial that occurs with initial implantation which may alter the load measurements. With the patella relocated in the trochlear groove, load measurements are then documented at 10°, 45°, and 90° of flexion following a uniform data collection protocol. At this point, the distribution of compartment forces during intraoperative Range Of Motion (ROM) drives the selection of the liner and, accordingly, the level of constraint. As previously described,2 the authors consider stable knees those showing a pressure of <50 lbs on the medial compartment, <35 lbs on the lateral compartment, and a mediolateral intercompartmental difference within 15 lbs. The mean intercompartmental force differences during trial ultimately drives our surgical technique and 15 lbs is usually considered as the parameter to differentiate “balanced” from “unbalanced” knees.2 In order to obtain the desired values, the authors routinely perform soft tissue releases [i.e. “pie-crusting” of the lateral compartment or superficial Medial Collateral Ligament (MCL) release of the medial] or bone re-cuts after removal of the trial components. Once these “fine tunings” have been performed, a new sensor trial is performed; considering that the sensor is available with different shim thicknesses (10, 12, 14, 17 mm), multiple trials can be performed in order to reproduce a satisfactory stability. In the scenario of a sensor-detected instability, the authors follow a step-by-step algorithm: i) A medial to lateral intercompartmental difference within 15 lbs is treated using a standard PS insert; ii) An intercompartmental difference between 15-40 lbs suggests it is best to use a PS primary femoral component combined with a Constrained Postero-Stabilized (CPS) Poly; this can be accomplished by recutting the PS box 2 mm deeper into the trochlea. The CPS articular surfaces are designed to provide ±1.5° varus/valgus constraint and ±5.5° internal/external rotation constraint; iii) An intercompartmental difference over 40 lbs is treated by increasing the level of constraint by shifting to a Persona Revision Knee System, characterized by having the possibility of using a Constrained Condylar Knee (CCK) bearing. This shift requires a primary to revision femoral conversion with the need of accessory femoral bone cuts; the primary Persona tibial baseplate, if not Trabecular MetalTM, can still be used in this scenario.
Figure 1.
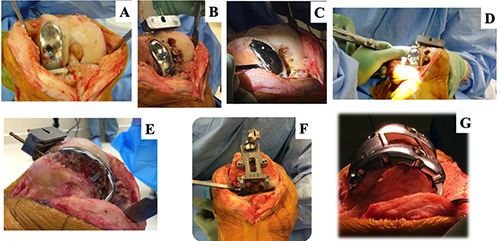
Right Knee. A) Right Unicompartmental Knee Arthroplasty; B) The intramedullary entry point for the intramedullary alignment guide has been determined and the distal femur cutting gig has been secured in accordance with the preoperative plan; C) A ¼ inch straight osteotome is used between the femoral component and cement mantle; D) A flexible osteotome is then used in order to preserve the femoral bone stock; E) The femoral component is removed with minimal bone loss; F) Sizing of the femoral component: a small osteotome is used on the postero-lateral femoral condyle to compensate for the bone loss which may lead to errors in rotational alignment; G) The trial femoral component is finally impacted into place and minimal bone loss is noted; when this gap is minimal (< 5 mm), the authors use bone cement to fill the gap during final cementation.
Figure 2.
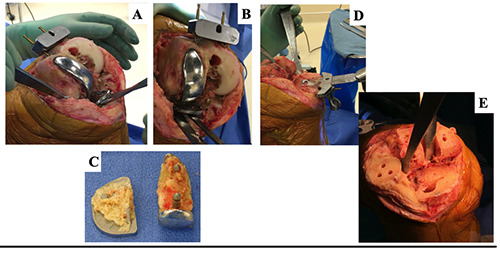
Right Knee. A) and B) A ½ inch or 1inch osteotome are used between the femoral component and cement mantle; C) The femoral and tibial components are removed with minimal bone loss; D) The tibial cut is completed using an extramidollary cutting guide positioned at the center of the ankle and the level of resection is determined according to the lateral tibial plateau bone loss; E) Bone surfaces are ready for cementation.
Once the final implants have been chosen and cemented, the capsular layer is sutured using a knotless barbed suture in a continuous fashion and the subcutaneous fat layer is closed using synthetic bidirectional barbed sutures. Skin closure is then performed using 2-octyl-cyanoacrylate (glue) and a polyester mesh with monocryl running suture.
Expected outcomes
UKA is a very appealing procedure when compared with TKA because it results in less postoperative pain, less peri-operative blood loss and faster discharge. The surgical technique proposed here makes conversion to TKA a more precise salvage procedure for failed UKA. The aim of this technique is to create a standardized UKA to primary TKA revision protocol based on a load scoring system able to suggest accurate surgical steps, setting a specific level of constraint for a specific range of load values. Secondarily, this technique allows surgeons to follow objective and intra-operatively determined parameters, which, when correlated with the standard intra-operative exam, could help surgeons choose the appropriate polyethylene thickness. Finally, this technique might help knee surgeons during complex revisions at the time of deciding on bone loss management and implant fixation; trabecular metal cones, titanium sleeves and stems might be necessary in the scenario of an unbalanced knee with high intercompartmental load differences.
Interestingly, revision of UKA to TKA has been associated with poorer clinical outcomes when compared with primary TKA: patients are usually less satisfied in terms of pain, joint stiffness and physical function. Being a symptom rather than a clinical finding, TKA instability represents a challenging entity to quantify: our technique combines an increase in the polyethylene thickness and an increase of the level of constraint as methods to guarantee the stability of the final, primary implant; it must be noted that, when a final insert with greater than 17 mm thickness is required, the authors recommend the use of a CCK system. The use of this sensing technology has also been proven to intraoperatively help the surgeon select the appropriate thickness of the insert3 and increase the degree of constraint addressing major instability during regular, primary TKA.
A decision-making algorithm on the level of intra-articular constraint during UKA to revision TKA has been published.4,5 Posterior-stabilized components showed superior clinical outcomes in patients with minor bony defects and intact metaphyseal bone; semi-constrained implants showed better outcomes in the setting of an aseptic loosening with major bone defects while a rotating-hinge was preferred to address major bone defects due to septic causes.
The clear advantage of using this sensor- guided technology is to allow an intraoperative evaluation of the medial and lateral compartmental load pressures, tracking soft-tissue balance throughout the entire range of motion arc with trial implants in place, and accordingly, modify any residual imbalance: to the authors knowledge, there are no other reports on this technique and its theoretical advantages.
Complications
Being a surgical technique based on a single-use, non-implantable testing device, no major complications are expected. First, we recognize that being an operator-dependent technique represents a limitation as the learning curve of one experienced surgeon may not immediately translate to surgeons in general. Second, sensor readings are influenced by limb position and rotation; surgeons are invited to use a similar testing technique in their cases. Third, the authors apply this sensing technology to trial components, which may reproduce more instability as they are not cemented to bone as are actual components.
Figure 3.
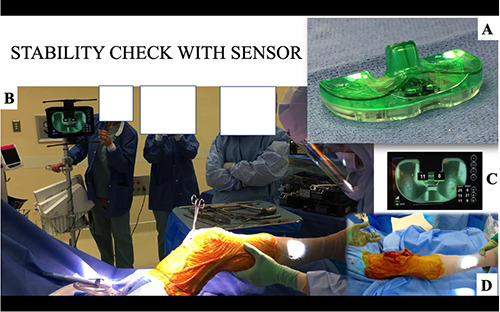
Right Knee. A) Postero-stabilized (PS) Verasense (Orthosensor, FL, USA) tibial sensor. B) Intraoperative testing during assisted range of motion (ROM); C) Load detection (lbs); D) The knee is never hyperextended during sensor testing.
Finally, the authors recognize that this surgical technique has the major limitation of extrapolating intraoperative data from a non-loading situation and may not duplicate in vivo, weight-bearing kinematic of the knee.
Acknowledgements
The authors acknowledge Heather Maughan, PhD for her critical review of this manuscript.
References
- 1.Indelli PF, Giori N, Maloney W. Level of constraint in revision knee arthroplasty. Curr Rev Musculoskelet Med 2015;8:390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Risitano S, Karamian B, Indelli PF. Intraoperative load-sensing drives the level of constraint in primary total knee arthroplasty: Surgical technique and review of the literature. J Clin Orthop Trauma 2017;8:265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghirardelli S, Bala A, Peretti G, et al. Intraoperative sensing technology to achieve balance in primary total knee arthroplasty: a review of the literature. JBJS Rev 2019;7:e4. doi: 10.2106/JBJS.RVW.19.00008. [DOI] [PubMed] [Google Scholar]
- 4.Lunebourg A, Parratte S, Ollivier M, et al. Are revisions of unicompartmental knee arthroplasties more like a primary or revision TKA? J Arthroplasty 2015;30:1985–9. [DOI] [PubMed] [Google Scholar]
- 5.Shen C, Lichstein PM, Austin MS, et al. Revision knee arthroplasty for bone loss: choosing the right degree of constraint. J Arthroplasty 2014;29:127-31. [DOI] [PubMed] [Google Scholar]


