Abstract
Disorders of consciousness (DOC) result from brain injuries that cause functional changes in vigilance, awareness and behaviour. It is important to correctly diagnose DOC so that the most appropriate rehabilitation treatments can be initiated. Several studies in DOC patients have demonstrated that repetitive transcranial magnetic stimulation (rTMS) has an important role to play in the recovery of consciousness as highlighted by monitoring clinical scale scores. Although studies indicate that rTMS can be used to aid recovery, it is not combined with other rehabilitative cognitive treatments. As of December 2018, there have been no studies published that combined DOC cognitive rehabilitation with TMS. This current review describes the use of rTMS as a form of non-invasive brain stimulation, as distinct from its use as a tool to investigate residual cortical activity, in terms of its possible therapeutic effects including cognitive rehabilitation. Literature searches were undertaken to identify all relevant studies. The available evidence suggests that rTMS may have an important role to play in in monitoring brain function during recovery and making other intensive rehabilitation treatments more effective, such as sensorial stimulations and cognitive training in patients after a severe acquired brain injury. Further research is required to establish the usefulness of rTMS treatment in DOC rehabilitation.
Keywords: Transcranial magnetic stimulation, rehabilitation, disorders of consciousness, cognitive treatments, recovery of consciousness
Introduction
Consciousness is characterized by two important components: vigilance and awareness. Good functioning of these two components stabilizes a normal level of consciousness. Disorders of consciousness (DOC) represent the outcome of brain injuries that can induce functional changes in vigilance, awareness and behaviour.1DOC present an important challenge in terms of misdiagnosis between different levels of consciousness. The correct diagnosis of DOC is important to in order to be able to plan specific rehabilitative treatments.2 A previous study investigated the accuracy of this severe clinical diagnosis using the Coma Recovery Scale-Revised (CRS-R) and it demonstrated that most of the patients with an uncertain diagnosis by clinical consensus were identified as minimally conscious state (MCS) based on their CRS-R scores.3 Magnetic resonance imaging (MRI) and neurophysiological studies showed that MCS and vegetative state (VS) patients could have cortical responses reflecting a level of cognition and awareness.4,5 These results permitted a reclassification of the state of consciousness in some of these patients.4,5 These findings demonstrated that specific examinations could be useful techniques to establish a communication channel with these types of patients that could be classified as unresponsive.6 In recent years, the application of non-invasive techniques to assess the functional state of the cerebral cortex in DOC patients has become an important topic.7 The basis of transcranial magnetic stimulation (TMS) application is diagnosis, prognosis and monitoring biological aspects used in neuroscience studies.8 TMS activates neurons in the grey matter in order to produce a response.9 TMS induces a burst along the corticospinal pathway when it was applied to the primary motor cortex with an adequate intensity.10 This reaction was recorded through motor evoked potentials (MEPs) on the contralateral muscles with respect to the stimulated motor cortex.11 Repetitive TMS (rTMS)consists of a transitory modulation of neural excitability with an effect that depends on the stimulation frequency.12 Continuous low frequency rTMS (≤1Hz) reduced cortical excitability in local stimulated regions and in correlated areas; while, intermittent high frequency rTMS (≥5Hz) seemed to obtain the opposite effect.13 Combined methods have been useful for studying the reactivity and connectivity of the cerebral cortex.14 A previous study enrolled six healthy control subjects and applied real and sham TMS over the left primary motor cortex during electroencephalographic (EEG) registration.15 This study validated the use of the combined techniques of TMS/EEG recording for experimental and clinical purposes.15 TMS was used as a prognostic and diagnostic tool in patients with traumatic brain injury (TBI).16 Online and offline TMS, combined with EEG and functional MRI, can give a positive feedback for functional recovery and cerebral plasticity in patients with a diagnosis of TBI.16The neuromodulative processes that occur during the rehabilitation of patients with subacute TBI remain to be investigated.17 TMS is a useful tool for stimulating recovery in lesioned circuits, but a previous study demonstrated that the focality of TMS might be disadvantageous in the acute stage of diffuse damage, which is frequent in TBI.17 This current review discusses the use of rTMS as a form of non-invasive brain stimulation, as distinct from its use as a tool to investigate residual cortical activity, in terms of its possible therapeutic effects including cognitive rehabilitation.
Literature search methods
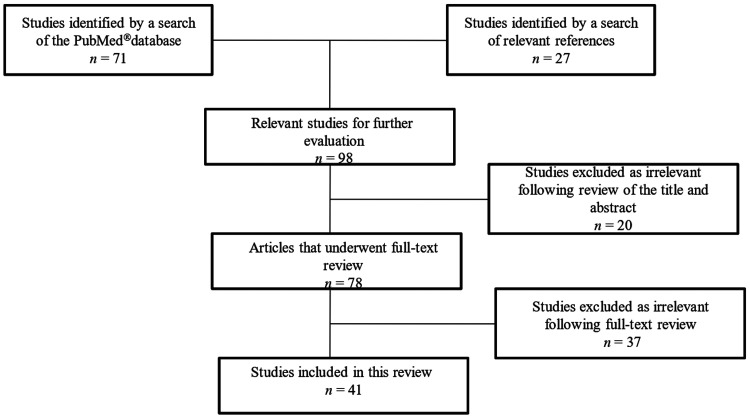
This current review investigated the use of rTMS in patients with DOC. The electronic database PubMed® was searched from January 2003 to December 2018 using the following terms: “Transcranial Magnetic Stimulation” (all field) AND “Consciousness Disorders” (all field) OR “transcranial magnetic stimulation rehabilitative treatment” (all field) AND disorders of consciousness (all field). There was a total of 71 articles identified via PubMed® (Figure 1). An additional 27 articles were identified by screening the reference lists of relevant articles. Articles were selected by screening the title, abstract and full-text using the following inclusion criteria: (i) study population included VS and MCS patients in the rehabilitative phase; (ii) the study investigated TMS in DOC; (iii) the study applied TMS for rehabilitative purposes. In total, 18 articles were selected from the PubMed®database search and 23 from screening the reference lists of relevant articles.
Figure 1.
Flow diagram of eligible studies showing the number of citations identified, screened and included in the review.
TMS in neurorehabilitation
Transcranial magnetic stimulation treatments were used to treat depressive and anxious symptoms because TMS stimulation appears to induce antidepressive effects.18,19 Neuroscientists use TMS to study and understand the relationship between cognitive performance and specific neural pathways.20 A previous review article described the role of TMS in cognitive plasticity.20 rTMS was also used to improve performance in sensory extinction and in unilateral neglect after stroke.21 Hemispatial neglect is defined as a defective spatial orientation. Single-pulse TMS improved spatial performance during a tactile detection task in right brain damage with extinction symptoms.22 High frequency rTMS conducted on the left prefrontal cortex improved cognitive performance.20 In cognitive TMS rehabilitation, it is possible the use EEG alpha-frequency to synchronize the activity and to induce transient improvements in cognitive tasks.23 Recovery of cognitive function might depend on improvements of cortical excitability induced by focal brain stimulation, which is probably facilitated by synaptic plasticity, leading to the recovery of degraded functions, restoration of neural function and regeneration of damaged neurons.24,25 A previous study described the use of a combination of neurophysiological techniques including TMS and EEG to study cerebral complexity in phases of weakness, in deep sleep and during pharmacological or pathological loss of consciousness.22 This new approach seems to provide a good measure of awareness and weakness states; and it is also useful for identifying the cortical mechanisms that underlie both the loss and the recovery of consciousness in pathological conditions.26
TMS as a diagnostic and neurorehabilitative tool in patients with DOC
A recent review assessed the level of cortical excitability and connectivity in DOC patients.26 Based on a neurophysiological approach, TMS has become a specific tool to assess VS and MCS.27 TMS elicited MEP responses in severely brain damaged patients.27 A previous report evaluated the diagnostic, prognostic and therapeutic effects of different neurophysiological techniques such as TMS, TMS-EEG co-registration and event-related evoked potentials.28 The results demonstrated that the use of TMS combined with other techniques (EEG) in DOC patients could differentiate VS from MCS and monitor a possible recovery of consciousness and cortical connectivity.28 Researchers have highlighted the importance of using a combined approach of TMS with high-density EEG as a technique to measure brain changes under physiological, pharmacological and pathological conditions; and to study neural correlates of consciousness.29 In particular, in MCS patients who were unable to stay in contact with their external environment, in whom changes in connectivity corresponding to an early stage in patients with gradual consciousness recovery were observed.30 The pattern of cortical evoked potentials by TMS (TEPs) were measured in 18 VS, 10 MCS and two locked-in syndrome (LIS) patients and the results demonstrated a significant difference among the TEPs patterns of VS and MCS and LIS patients.31The study demonstrated that in patients with VS, TMS induced only ipsilateral responses or no responses at all.31 A combined neurophysiological approach is useful to make a more certain diagnosis of DOC.22,31 A recent study demonstrated the efficacy of 5HzrTMS over the left primary motor cortex and polysomnography followed by TMS for a correct differential diagnosis.32 In particular, MCS patients showed a slow wave activity, which may be an index of cortical plasticity, but this activity perturbation was not found in VS patients.32 Previous research showed that patients with DOC obtained a good outcome in terms of total score on the CRS-R after sessions of stimulation over the dorsolateral prefrontal cortex with a 10HzrTMS.33,34 Another study showed that application of 10HzrTMS on the left dorsolateral prefrontal cortex decreased the low frequency band power and increased high frequency band power especially in MCS.35 In this study, patients were observed also with EEG registration, which might be useful to assess rTMS modulation effects.35 In contrast, a sham-controlled study demonstrated that real 20Hz rTMS applied for five consecutive days over the primary motor cortex did not produce significant behavioural changes and did not show EEG modifications in VS patients.36
A previous study examined the feasibility of a single session of rTMS applied over the dorsolateral prefrontal cortex in patients with unresponsive wakefulness syndrome.37 The results showed that a single session of 10Hz rTMS over the right dorsolateral prefrontal cortex might transiently improve consciousness and partially restore the connectivity within several cortical areas in some patients with DOC.37 These findings might be explained by a functional, but transitory, improvement of connectivity of the residual brainstem-thalamo-cortical and cortico-cortical networks.38
Conclusion
To date, there have been no published studies that have focused on cognitive rehabilitation in patients with DOC, especially in those with a minimal response. There are no standardized rehabilitation programmes for these patients. Therefore, major attention needs to be focused on developing cognitive rehabilitation programmes for patients with DOC that result in a better recovery of consciousness.39 There are few studies related to rehabilitative techniques, especially in terms of cognitive rehabilitative training.39,40 Published studies on the use of TMS in patients with DOC have highlighted how this tool might have an important role to play in the recovery of consciousness and the improvement of cognitive performance.8,20,34 A case study of an MCS patient that combined peripheral stimulation and rTMS demonstrated that peripheral nerve stimulation did not have any effect in terms of clinical, behavioural or electroencephalographic changes.41 However, the results provided evidence that rTMS treatment may improve awareness and arousal in MCS.41
Data obtained from the reviewed published literature indicate that TMS has an important role to play in the recovery of consciousness as highlighted by monitoring clinical scale scores.33,34 These studies demonstrated that TMS was a useful tool for the recovery of consciousness as demonstrated by an improvement in the scores of clinical scales.33,34There have been no studies in published in the literature that combined cognitive rehabilitation and TMS in patients with DOC. For these reasons, this current review recommends research into the use of TMS in conjunction with intensive rehabilitative treatments that include sensorial stimulation (auditory, visual and tactile stimulation) and cognitive training in patients with severe cognitive impairment after a severe brain acquired injury.41 Further research is required to establish the usefulness of TMS treatment in DOC rehabilitation. A limitation of this work was that it was not structured as a systematic review.
Footnotes
Declaration of conflicting interest: The authors declare that there are no conflicts of interest.
Funding: Supported by a grant from the Italian Health Ministry (no. GR-2013-02359341).
ORCID iDs: Simona De Salvo https://orcid.org/0000-0001-9501-3258
Francesco Corallo https://orcid.org/0000-0003-4862-3832
Silvia Marino https://orcid.org/0000-0002-1088-6808
References
- 1.Giacino JT, Fins JJ, Laureys S, et al. Disorders of consciousness after acquired brain injury: the state of the science. Nat Rev Neurol 2014; 10: 99–114. [DOI] [PubMed] [Google Scholar]
- 2.Giacino JT. Disorders of consciousness: differential diagnosis and neuropathologic features. Semin Neurol 1997; 17: 105–111. [DOI] [PubMed] [Google Scholar]
- 3.Schnakers C, Vanhaudenhuyse A, Giacino J, et al . Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol 2009; 9: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marino S, Bonanno L, Ciurleo R, et al . Functional Evaluation of Awareness in Vegetative and Minimally Conscious State. Open Neuroimag J 2017; 11: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Salvo S, Naro A, Bonanno L, et al. Assessment of nociceptive system in vegetative and minimally conscious state by using laser evoked potentials. Brain Inj 2015; 29: 1467–1474. [DOI] [PubMed] [Google Scholar]
- 6.Monti MM, Vanhaudenhuyse A, Coleman MR, et al. Willful modulation of brain activity in disorders of consciousness. N Engl J Med 2010; 362: 579–589. [DOI] [PubMed] [Google Scholar]
- 7.Shou Z, Li Z, Wang X, et al. Non-invasive brain intervention techniques used in patients with disorders of consciousness. Int J Neurosci 2020: 1–15. [DOI] [PubMed] [Google Scholar]
- 8.Miniussi C, Rossini PM. Transcranial magnetic stimulation in cognitive rehabilitation. Neuropsychol Rehabil 2011; 21: 579–601. [DOI] [PubMed] [Google Scholar]
- 9.Ferreri F, Pasqualetti P, Määttä S, et al. Human brain connectivity during single and paired pulse transcranial magnetic stimulation. Neuroimage 2011; 54: 90–102. [DOI] [PubMed] [Google Scholar]
- 10.Capaday C, Lavoie BA, Barbeau H, et al . Studies on the corticospinal control of human walking. I. Responses to focal transcranial magnetic stimulation of the motor cortex. J Neurophysiol 1999; 81: 129–139. [DOI] [PubMed] [Google Scholar]
- 11.Rossini PM, Rossi S. Transcranial magnetic stimulation Diagnostic, therapeutic, and research potential. Neurology 2007; 68: 484–488. [DOI] [PubMed] [Google Scholar]
- 12.Pascual-Leone A, Tormos JM, Keenan J, et al . Study and modulation of human cortical excitability with transcranial magnetic stimulation. J Clin Neurophysiol 1998; 15: 333–343. [DOI] [PubMed] [Google Scholar]
- 13.Pascual-Leone A, Valls-Solé J, Wassermann EM, et al. Responses to rapid-rate transcranial magnetic stimulation of the human motor cortex. Brain 1994; 117: 847–858. [DOI] [PubMed] [Google Scholar]
- 14.Miniussi C, Thut G. . Combining TMS and EEG offers new prospects in cognitive neuroscience. Brain Topogr 2010; 22: 249–256. [DOI] [PubMed] [Google Scholar]
- 15.Bonato C, Miniussi C, Rossini PM. Transcranial magnetic stimulation and cortical evoked potentials: a TMS/EEG co-registration study. Clin Neurophysiol 2006; 117: 1699–1707. [DOI] [PubMed] [Google Scholar]
- 16.Pape TL, Rosenow J, Lewis G. Transcranial magnetic stimulation: a possible treatment for TBI. J Head Trauma Rehabil 2006; 21: 437–451. [DOI] [PubMed] [Google Scholar]
- 17.Demirtas-Tatlidede A, Vahabzadeh-Hagh AM, Bernabeu M, et al. Noninvasive brain stimulation in traumatic brain injury. J Head Trauma Rehabil 2012; 27: 274–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bersani FS, Minichino A, Enticott PG, et al. Deep transcranial magnetic stimulation as a treatment for psychiatric disorders: a comprehensive review. Eur Psychiatry 2013; 28: 30–39. [DOI] [PubMed] [Google Scholar]
- 19.Gross M, Nakamura L, Pascual ‐Leone A, et al. Has repetitive transcranial magnetic stimulation (rTMS) treatment for depression improved? A systematic review and meta‐analysis comparing the recent vs. the earlier rTMS studies. Acta Psychiatr Scand 2007; 116: 165–173. [DOI] [PubMed] [Google Scholar]
- 20.Rossi S, Rossini PM. TMS in cognitive plasticity and the potential for rehabilitation. Trends Cogn Sci 2004; 8: 273–279. [DOI] [PubMed] [Google Scholar]
- 21.Brighina F, Bisiach E, Oliveri M, et al . 1 Hz repetitive transcranial magnetic stimulation of the unaffected hemisphere ameliorates contralesional visuospatial neglect in humans. Neurosci Lett 2003; 336: 131–133. [DOI] [PubMed] [Google Scholar]
- 22.Sarasso S, Rosanova M, Casali AG, et al. Quantifying cortical EEG responses to TMS in (un) consciousness. Clin EEG Neurosci 2014; 45: 40–49. [DOI] [PubMed] [Google Scholar]
- 23.Klimesch W, Sauseng P, Gerloff C. Enhancing cognitive performance with repetitive transcranial magnetic stimulation at human individual alpha frequency. Eur J Neurosci 2003; 17: 1129–1133. [DOI] [PubMed] [Google Scholar]
- 24.Sharma N, Classen J, Cohen LG. Neural plasticity and its contribution to functional recovery. Handb Clin Neurol 2013; 110: 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faralli A, Bigoni M, Mauro A, et al. Noninvasive strategies to promote functional recovery after stroke. Neural Plast 2013; 2013: 854597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lapitska N, Gosseries O, Delvaux V, et al. Transcranial magnetic stimulation in disorders of consciousness. Rev Neurosci 2009; 20: 235–250. [DOI] [PubMed] [Google Scholar]
- 27.De Salvo S, Bramanti P, Marino S. . Clinical differentiation and outcome evaluation in vegetative and minimally conscious state patients: the neurophysiological approach. FunctNeurol 2012; 27: 155–162. [PMC free article] [PubMed] [Google Scholar]
- 28.Ragazzoni A, Cincotta M, Giovannelli F, et al. Clinical neurophysiology of prolonged disorders of consciousness: from diagnostic stimulation to therapeutic neuromodulation. Clin Neurophysiol 2017; 128: 1629–1646. [DOI] [PubMed] [Google Scholar]
- 29.Napolitani M, Bodart O, Canali P, et al. Transcranial magnetic stimulation combined with high-density EEG in altered states of consciousness. Brain Inj 2014; 28: 1180–1189. [DOI] [PubMed] [Google Scholar]
- 30.Rosanova M, Gosseries O, Casarotto S, et al. Recovery of cortical effective connectivity and recovery of consciousness in vegetative patients. Brain 2012; 135: 1308–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ragazzoni A, Pirulli C, Veniero D, et al. Vegetative versus minimally conscious states: a study using TMS-EEG, sensory and event-related potentials. PLoS One 2013; 8: e57069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pisani LR, Naro A, Leo A, et al. Repetitive transcranial magnetic stimulation induced slow wave activity modification: A possible role in disorder of consciousness differential diagnosis? Conscious Cogn 2015; 38: 1–8. [DOI] [PubMed] [Google Scholar]
- 33.Bai Y, Xia X, Kang J, et al. Evaluating the effect of repetitive transcranial magnetic stimulation on disorders of consciousness by using TMS-EEG. Front Neurosci 2016; 10: 473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xia X, Bai Y, Zhou Y, et al. Effects of 10 hz repetitive transcranial magnetic stimulation of the left dorsolateral prefrontal cortex in disorders of consciousness. Front Neurol 2017; 8: 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xia X, Liu Y, Bai Y, et al. Long-lasting repetitive transcranial magnetic stimulation modulates electroencephalography oscillation in patients with disorders of consciousness. Neuroreport 2017; 28: 1022–1029. [DOI] [PubMed] [Google Scholar]
- 36.Cincotta M, Giovannelli F, Chiaramonti R, et al . No effects of 20 Hz-rTMS of the primary motor cortex in vegetative state: a randomised, sham-controlled study. Cortex 2015; 71: 368–376. [DOI] [PubMed] [Google Scholar]
- 37.Naro A, Russo M, Leo A, et al. A single session of repetitive transcranial magnetic stimulation over the dorsolateral prefrontal cortex in patients with unresponsive wakefulness syndrome: preliminary results. Neurorehabil Neural Repair 2015; 29: 603–613. [DOI] [PubMed] [Google Scholar]
- 38.Hampstead BM, Sathian K, Bikson M, et al. Combined mnemonic strategy training and high-definition transcranial direct current stimulation for memory deficits in mild cognitive impairment. Alzheimers Dement (N Y) 2017; 3: 459–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.La Gattuta E, Corallo F, Buono VL, et al. Techniques of cognitive rehabilitation in patients with disorders of consciousness: a systematic review. Neurol Sci 2018; 39: 641–645. [DOI] [PubMed] [Google Scholar]
- 40.Miniussi C, Cappa SF, Cohen LG, et al. Efficacy of repetitive transcranial magnetic stimulation/transcranial direct current stimulation in cognitive neurorehabilitation. Brain Stimul 2008; 1: 326–336. [DOI] [PubMed] [Google Scholar]
- 41.Piccione F, Cavinato M, Manganotti P, et al. Behavioral and neurophysiological effects of repetitive transcranial magnetic stimulation on the minimally conscious state: a case study. Neurorehabil Neural Repair 2011; 25: 98–102. [DOI] [PubMed] [Google Scholar]