Abstract
Background:
Lateral patellar dislocation can become a recurrent problem after the first episode. Identifying those patients who are at increased risk of redislocation is important for the treatment decision-making process.
Purpose:
To identify clinical and radiologic risk factors for recurrence of patellar dislocation after a first episode.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The study included patients with lateral patellar dislocation and a 1-year minimum follow-up who were seen between 2011 and 2018. Patients aged 10 to 65 years were included. Patient characteristics, physical examination (patellar apprehension, J sign), and radiographs were reviewed. The Caton-Deschamps and Insall-Salvati ratios were used to evaluate patella alta. High-grade trochlear dysplasia was defined as Dejour types B, C, and D.
Results:
A total of 130 patients (139 knees) with primary lateral patellar dislocation were included. Recurrent dislocation was seen in 83 knees (59.71%). Stepwise logistic regression analysis demonstrated that Caton-Deschamps ratio ≥1.15 (OR, 2.39; 95% CI, 1.09-5.22; P = .029), age <21 years (OR, 2.53; 95% CI, 1.11-5.77; P = .027), and high-grade trochlear dysplasia (OR, 4.17; 95% CI, 1.90-9.17; P < .001) were significantly associated with patellar redislocation. Based on the presence of these factors, the probability of dislocation after a first lateral patellar dislocation was 31.2% with no factors present, 36.6% with any 1 factor present, 71.7% with any 2 factors present, and 86.2% if all 3 conditions were present.
Conclusion:
The results of this study indicated that patella alta, high-grade trochlear dysplasia, and age <21 years were independent risk factors for patellar redislocation after a first episode, with an additive effect when they were present together. This may help to guide the type of treatment for these patients.
Keywords: patellar dislocation, trochlear dysplasia, patella alta, patellar instability, risk factors
Patellar dislocation is a relatively common knee injury, with an incidence ranging from 2.3 to 77 per 100,000 people per year.6,13,18,34,38,39,45 At least one-third of skeletally mature patients will experience recurrent instability over time after a primary patellar dislocation.13,24,27,28,30 Patellofemoral stability depends on multiple factors, such as limb alignment, the torsional profile, soft tissue constraints, and the shape of the trochlear groove.46 Some of the predisposing factors that have been associated with patellar redislocation are trochlear dysplasia, patella alta, malalignment, elevated tibial tubercle–trochlear groove (TT-TG) distance, and skeletal immaturity.§ However, there continues to be controversy regarding the type of management a patient should receive after a first episode of lateral patellar dislocation. There is a trend toward conservative treatment with few absolute indications for surgery, such as an associated acute osteochondral fracture.2,32,40,42
It has been difficult to predict which patients will go on to have recurrent instability.13 The multifactorial nature of patellar instability requires a clinician to understand the individual risk factors for recurrence and recognize that certain combinations of factors may considerably increase the risk of redislocation.30 There are risk factors for recurrence that have been identified in recent studies. Jaquith and Parikh24 identified the following: skeletal immaturity, patella alta (measured using the Caton-Deschamps ratio), history of contralateral dislocation, and any type of trochlear dysplasia (according to the Dejour classification). Meanwhile, Arendt et al2 showed that patella alta (measured using the Insall-Salvati ratio), trochlear dysplasia (measured as an increased sulcus angle), and skeletal immaturity were predictors of recurrence. A recent meta-analysis found that younger age and elevated TT-TG distance were also risk factors for recurrence.22
Given the high rate of recurrence after a first episode, it is important to better understand the risk factors involved. The ability to recognize the factors that predispose a patient to an increased risk of patellofemoral dislocation recurrence can be a useful clinical tool for making treatment decisions. The purpose of this study was to identify clinical and radiologic risk factors for the recurrence of patellar dislocation after a first episode.
Methods
This study was conducted at a tertiary-care center with specialists trained in the care of patients with complex orthopaedic injuries, making this institution an orthopaedic referral center for the region. This study was approved by the institution’s biomedical research and ethics committee.
Study Population
Eligible patients were those aged 10 to 65 years who had sustained a lateral patellar dislocation and were seen at our institution after their first episode. The study period was between January 2011 and June 2018. A search was conducted in the medical chart database for patients with the appropriate ICD-10 (International Classification of Diseases, 10th Revision) diagnostic codes for patellar dislocation (S830, M220, M221), their medical charts were evaluated, and all these patients were contacted for inclusion in the study. Patients with a history of tibial tubercle osteotomy were not included in the patellar height analysis, and no radiographs were taken for patients who were pregnant during the follow-up visit.
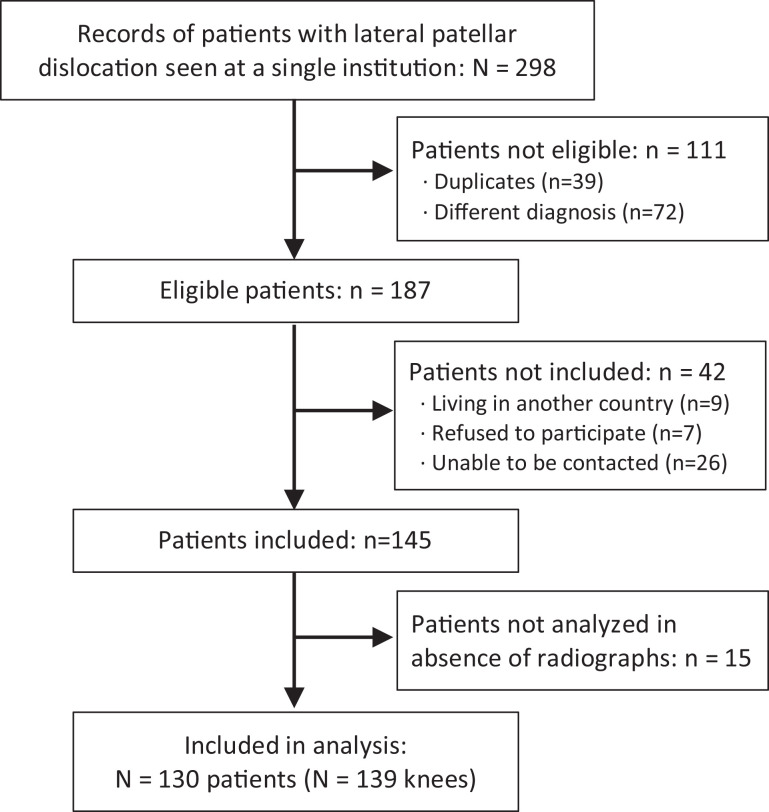
Patients with at least 1 year of follow-up were invited to participate in the study during 2019. There were 187 patients who met the inclusion criteria. Of these, 145 patients were contacted and agreed to participate in the study, and 130 patients (139 knees) underwent radiographic assessment, for a 70% follow-up. Patients lost to follow-up were older (median age, 20 years) than study participants (median age, 16 years). Figure 1 shows the flow diagram of patient inclusion and exclusion.
Figure 1.
STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) flow diagram showing the sampling and inclusion of patients in the study.
Assessment
Data were retrospectively collected from electronic medical records and included patient and clinical characteristics. The main outcome was recurrence of patellar dislocation. The presence of trochlear dysplasia, patellar height, sulcus angle, tilt, and skeletal maturity were assessed by a radiologist (M.R.). This information was recorded in an electronic database used exclusively by our institution (BDClinic).
All study patients were evaluated by an orthopaedic sports medicine surgeon (J.P.M.-C.). This included questions about their first episode and further dislocations, type of treatment received, and physical examination, with emphasis on an apprehension test and the presence of the J sign. After patients provided written informed consent, a comparative radiograph of both knees was taken.
Radiographic Measurements
Anteroposterior, true lateral view (with superimposed dorsal condyles),29 and Merchant view radiographs were used for assessments. Radiographs were obtained and then evaluated by the radiologist, who was blinded to the clinical data and outcomes. For trochlear dysplasia, the Dejour classification system was used.8,14,15 Radiographs were evaluated for the presence of a crossing sign, a supratrochlear spur, and a double contour sign. According to the literature, high-grade trochlear dysplasia includes types B, C, and D, while low-grade trochlear dysplasia is considered type A.29 Patella alta was assessed on the lateral radiographs using the Caton-Deschamps ratio and the Insall-Salvati ratio.11,16,23,43 Skeletal maturity was evaluated based on the distal femoral and proximal tibial physes using one of the following categories: open, closing, or closed. Patients with open or closing physes were considered skeletally immature, and those with closed physes were considered skeletally mature.31
Statistical Analysis
To group data from certain variables, the medians and interquartile ranges for the Insall-Salvati ratio, Caton-Deschamps ratio, sulcus angle, and body mass index (BMI) were used because there was no normal distribution as verified using the Shapiro-Wilk test. Qualitative variables were presented as distributions of relative and absolute frequencies.
A comparison between knees with and knees without patellar redislocation in relation to quantitative variables was made using the Mann-Whitney U test; for qualitative nominal variables, the chi-square or Fisher exact test was used, depending on the expected frequency in the categories. Subsequently, a logistic regression model was used to identify variables that were associated with patellar redislocation (variables with P < .2). Variables with P < .05 were allowed to remain in the model. A new variable was created in which the number of risk factors was defined, and logistic regression was performed to calculate the predicted risk of dislocation.
The goodness of fit of the model was verified using the chi-square Hosmer-Lemeshow test.17 The discriminative capacity of the models was determined using the area under the receiver operating characteristic curve method, and the Akaike information criterion was used to select the best model.44 All analyses and sample size calculations were performed using Stata 14 statistical software (StataCorp).
Results
Table 1 shows a description of the characteristics for the overall study population by outcome of interest. Overall, 83 of the 139 knees (59.71%) had recurrent patellar dislocation during follow-up (minimum follow-up, 1 year; median follow-up, 6.3 years). When comparing these characteristics between cases of redislocation and cases of no redislocation, a significant difference was found for median age, with the redislocation group being younger (16 vs 17.5 years; P = .008). The recurrent patellar dislocation group also exhibited a higher rate of patella alta (Caton-Deschamps ratio, 1.19 vs 1.1; P = .003). There was no significant sex-based difference between the redislocation and no redislocation groups. The redislocation group had a significantly lower BMI compared with the no redislocation group (median, 21.9 vs 23.7; P = .021). Recurrent patellar dislocation was associated with a higher rate of positive J sign (36.14% vs 19.64%; P = .032) and apprehension (61.45% vs 33.93%; P = .001) during physical examination.
Table 1.
Characteristics of Knees With and Knees Without Patellar Redislocationa
| Variable | All (N = 139 Knees) | Redislocation (n = 83 Knees; 59.71%) | No Redislocation (n = 56 Knees; 40.29%) | P Valueb |
|---|---|---|---|---|
| Baseline measurements | ||||
| Sex | ||||
| Female | 75 (54) | 46 (55.42) | 29 (51.79) | .673 |
| Male | 64 (46) | 37 (44.58) | 27 (48.21) | |
| Median age, y | 16 (14-24) | 16 (13-20) | 17.5 (15-27) | .008 |
| Side | ||||
| Left | 74 (53.24) | 45 (54.22) | 29 (51.79) | .431 |
| Right | 65 (46.76) | 38 (45.78) | 27 (48.21) | |
| Follow-up measurements | ||||
| Median BMI | 22.5 (20.1-25.4) | 21.9 (19.5-25.1) | 23.7 (20.45-25.95) | .021 |
| Median Insall-Salvati ratio | 1.34 (1.18-1.47) | 1.38 (1.22-1.47) | 1.29 (1.14-1.44) | .069 |
| Median Caton-Deschamps ratio | 1.16 (1.03-1.24) | 1.19 (1.09-1.26) | 1.1 (0.97-1.22) | .003 |
| Median sulcus angle, deg | 17 (7-26) | 17 (7-26) | 17 (7.5-27) | .718 |
| Apprehension test | 70 (50.36) | 51 (61.45) | 19 (33.93) | .001 |
| J sign | 41 (29.5) | 30 (36.14) | 11 (19.64) | .032 |
| Trochlear dysplasia | 114 (82.01) | 70 (84.34) | 44 (78.57) | .378 |
| Type of dysplasiac | ||||
| A | 51 (36.69) | 22 (26.51) | 29 (51.79) | .002 |
| B | 27 (19.42) | 21 (25.30) | 6 (10.71) | .033 |
| C | 23 (16.55) | 16 (19.28) | 7 (12.5) | .291 |
| D | 13 (9.35) | 11 (13.25) | 2 (3.57) | .047 |
aData are presented as n (%) or median (interquartile range). Boldface P values indicate a statistically significant difference between study groups (P < .05). BMI, body mass index.
bFrom the 2-group t test and Mann-Whitney U test for continuous variables and the chi-square test and Fisher exact test for categorical variables.
cAccording to Dejour classification.
The logistic regression model showed that the factors associated with redislocation were a Caton-Deschamps ratio ≥1.15 (P = .029), age <21 years (P = .027), and high-grade trochlear dysplasia (P < .001). The results of the logistic regression analysis are shown in Table 2. This model was adequately adjusted to the data (P = .59 for the chi-square Hosmer-Lemeshow test) and showed a discriminative capacity of 75% (area under the receiver operating characteristic curve) and an Akaike information criterion of 139.
Table 2.
Logistic Regression Analysis of Patellar Redislocation Group
| Variable | Regression Model | |
|---|---|---|
| OR (95% CI) | P Value | |
| Caton-Deschamps ratio ≥1.15 | 2.39 (1.09-5.22) | .029 |
| Age <21 y | 2.53 (1.11-5.77) | .027 |
| High-grade trochlear dysplasiaa | 4.17 (1.90-9.17) | <.001 |
aDejour types B, C, and D. OR, odds ratio.
In this study, the probability of redislocation based on the presence of these specific factors ranged from 31.2% when no factors were present to 86.2% when all 3 factors were present. The probability of redislocation is detailed in Table 3.
Table 3.
Probability of Redislocation by Number of Positive Factorsa
| No. of Risk Factorsb | Redislocation (n = 83 Knees) |
No Redislocation (n = 56 Knees) |
Predicted Probability of Redislocation, % |
|---|---|---|---|
| 0 | 5 (6.02) | 11 (19.64) | 31.2 |
| 1 | 15 (18.07) | 26 (46.43) | 36.6 |
| 2 | 38 (45.78) | 15 (26.79) | 71.7 |
| 3 | 25 (30.12) | 4 (7.14) | 86.2 |
aData are presented as n (%) unless otherwise indicated.
bThe 3 risk factors are Caton-Deschamps ratio ≥1.15, age <21 years, and high-grade trochlear dysplasia (Dejour types B, C, and D).
Discussion
This study confirms high recurrence of patellar dislocation after a first episode, especially when certain risk factors are present. Despite extensive publications about patellar instability, there is still controversy regarding how to best treat these patients and when to operate on them after the first episode.18,21,24,26,28 The following were found to be independent risk factors for lateral patellar redislocation: patella alta as measured using a Caton-Deschamps ratio ≥1.15, age <21 years, and high-grade trochlear dysplasia (Dejour types B, C, and D). These variables were used to create a risk prediction model for redislocation, which showed a 31.2% risk of redislocation without risk factors, a 36.6% risk with 1 positive criterion, a 71.7% risk with 2 criteria, and an 86.2% risk with 3 positive criteria. This finding coincides with previous risk factors identified in the literature.2,24 There was no association between recurrence and female sex or increased BMI; in contrast, the redislocation group had a slightly lower BMI (P = .02).
We found a 59.7% recurrence after a first episode of patellar dislocation in our study population. This is a high recurrence rate that could be related to the retrospective nature of the study, making it prone for selection bias. However, this value is in the range of what has been reported in the literature36,46 (15%-81%), with a similar distribution among retrospective studies, such as those of Balcarek et al7 (66%), Gravesen et al20 (23%), Buchner et al9 (27%), and Kaewkongnok et al25 (27%), compared with prospective studies, such as those of Fithian et al18 (17%), Nikku et al35 (36%), Askenberger et al4 (43%), and Palmu et al37 (71%). There is a significant burden of disease for these patients, with limitations for daily life and even more for sports participation.33 Today, part of our duty is to better understand who could benefit from early surgery and stratifying by risk factors may be a useful tool.
Patella alta has been associated with an increased risk of recurrence and is one of the abnormalities for which correction can alter the success of treatment in patellofemoral instability.41 The association between patella alta and recurrence is likely caused by delayed entry of the patella into the trochlear groove (the normal osteoarticular constraint) during early knee flexion, allowing for instability to occur.13 Not addressing patella alta is one of the causes of failure for patients after isolated medial patellofemoral ligament reconstruction.41 However, the threshold to correct patella alta has not been well defined, and it has not been established whether the Caton-Deschamps or Insall-Salvati ratio should be used to measure it. Arendt et al2 found a statistically significant difference for recurrence using an Insall-Salvati ratio ≥1.3 as an independent factor. Those patellar height measurements were made using magnetic resonance imaging (MRI), which can explain the difference with our findings, which are from radiographs.48 Jaquith and Parikh24 found that the risk increased using a Caton-Deschamps ratio >1.45 in children and adolescents. We only had 5 knees with a Caton-Deschamps ratio >1.45, 4 of which were in the redislocation group, making that cutoff point very rare for our study population, which included both children and adults. In our study, the redislocation group had higher values than did the no redislocation group for the Caton-Deschamps ratio (1.19 vs 1.1; P = .003). For the Insall-Salvati ratio, there was a nonsignificant difference (1.38 vs 1.29; P = .069). After logistic regression, a Caton-Deschamps ratio ≥1.15 remained a significant cutoff point. This point is in the upper normal limit of what has been used to define patella alta (Caton-Deschamps ratio, >1.2).16,48 It makes sense, then, to consider knees with patellar heights above this normal value to be at increased risk for patellar redislocation.
Since 1915, trochlear dysplasia has been recognized as a risk factor for patellar instability.1,16 In fact, previous studies have shown that trochlear dysplasia might be one of the strongest risk factors for patellar instability and recurrence.3,13,19,28 This is explained by the lack of constraint in the lateral wall of the groove and is consistent with our findings, where high-grade trochlear dysplasia increased the likelihood of patellar redislocation. Jaquith and Parikh24 found an association between patellar dislocation recurrence and trochlear dysplasia using the Dejour classification. Arendt et al2 showed an association with sulcus angles >154° on MRI scans. Our data support dividing dysplasia into low-grade (Dejour type A) and high-grade (Dejour types B, C, and D) groups, with an increased risk of recurrence for the high-grade group. Dividing dysplasia into low- and high-grade groups also improves interobserver reliability.29
Skeletal immaturity was identified by both Arendt et al2 and Jaquith and Parikh24 as a predictive risk factor for patellar redislocation after a first episode. In our retrospective study, there was an incomplete number of patients with radiographs from the first dislocation. Therefore, chronological age at the time of the first dislocation was used as a proxy measurement for skeletal maturity. The logistic regression showed a significantly increased risk for recurrence in patients who had their first episode of patellofemoral dislocation before they were 21 years of age. This age threshold could be explained by skeletal immaturity in some of the patients but not in all because most would have closed physes by 17 or 18 years of age; there are other characteristics indicative of a younger population, such as returning more frequently to strenuous sports, similar to what occurs with anterior cruciate ligament rerupture in younger patients.47
The current study and those of Arendt et al,2 and Jaquith and Parikh24 have in common a lower incidence of recurrence in patients without risk factors, ranging between 7.7% and 31.2%. Risk increases when patella alta, skeletal immaturity/age <21 years, or trochlear dysplasia is present. The chance of redislocation is between 22.7% and 36.6% with 1 risk factor present, between 50.9% and 71.7% with 2 risk factors present, and between 74.8% and 86.2% when there are 3 present. This can definitely help the clinician decide, in conjunction with the patient and his or her family, what type of treatment to choose according to the number of risk factors present. It seems logical to consider surgery when 2 or more of these risk factors are present, keeping in mind that this might include not only a medial patellofemoral ligament reconstruction, but also the correction of the other modifiable risk factors that are present, such as patella alta or trochlear dysplasia. While there are risk factors that can predict recurrence, it continues to be a challenge to define the timing of surgery and the type of surgery to perform.
The main limitation of this study was the retrospective nature of the design. Patients were considered eligible only when the diagnosis of patellar dislocation was registered during their consultation at the emergency department or clinic. Then, during follow-up, they were asked again about their episode in the questionnaire to confirm that they did have a real episode of dislocation. For controlling selection bias, all patients during the study period in the hospital database were eligible, and we actively tried to reach them through telephone calls and email. Most patients lost to follow-up were patients who could not be contacted or lived in another country; only 7 refused to participate. This decreases the chance for selection bias, considering that there are no reasons to consider that most of those patients would have different characteristics or outcomes compared with the main sample. We could not measure recurrence, trochlear dysplasia, or patellar height in patients lost to follow-up, but we did calculate the median age for them, finding a slightly higher value (20 years) compared with the median age of study participants (16 years). This could skew the recurrence to a higher value. Meanwhile, radiographs were obtained during the follow-up visit because there was no high-quality initial radiograph for most patients; this ensured that we could have a true lateral view of the knee, which is important for trochlear dysplasia assessment, but could introduce information bias in some cases where the radiographs might have changed over time. For clinical measurements, such as the J sign or apprehension test, we did not have the initial status (after the first episode) for all patients; therefore, this limited the possibility of including those variables on the analytical model. The study did not include skeletal maturity status but rather a proxy measurement of age. Finally, computed tomography and MRI scans were not available to measure other possible risk factors, such as the TT-TG distance or lateral trochlear inclination angle.12
Conclusion
The results of this study indicated that patella alta, high-grade trochlear dysplasia, and age <21 years were independent risk factors for patellar redislocation after a first episode, with an additive effect when they were present together. Surgical treatment may be considered when 2 or more factors are present.
Acknowledgment
Juan Pablo Martinez-Cano acknowledges Dr. Elizabeth Arendt, Dr. Marc Tompkins, and Dr. Lee Pace for their mentoring and friendship in the patellofemoral path. The authors thank the patients who happily participated in this research, improving the way in which we understand and treat patellar instability. Finally, the authors thank Diana Marcela Martinez, Claudia Montes, and Ramiro Manzano for their assistance with the statistical analysis.
Footnotes
Final revision submitted October 8, 2020; accepted November 19, 2020.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Fundación Valle del Lili (protocol No. 1183).
References
- 1. Albee FH. The bone graft wedge in the treatment of habitual dislocation of the patella. Med Record. 1915;88:257–259. [Google Scholar]
- 2. Arendt EA, Askenberger M, Agel J, Tompkins MA. Risk of redislocation after primary patellar dislocation: a clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med. 2018;46(14):3385–3390. [DOI] [PubMed] [Google Scholar]
- 3. Arendt EA, England K, Agel J, Tompkins MA. An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3099–3107. [DOI] [PubMed] [Google Scholar]
- 4. Askenberger M, Bengtsson Moström E, Ekström W, et al. Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: a randomized controlled trial. Am J Sports Med. 2018;46(10):2328–2340. [DOI] [PubMed] [Google Scholar]
- 5. Askenberger M, Janarv PM, Finnbogason T, Arendt EA. Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med. 2017;45(1):50–58. [DOI] [PubMed] [Google Scholar]
- 6. Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472–479. [DOI] [PubMed] [Google Scholar]
- 7. Balcarek P, Oberthür S, Hopfensitz S, et al. Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2308–2314. [DOI] [PubMed] [Google Scholar]
- 8. Bollier M, Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19(1):8–16. [DOI] [PubMed] [Google Scholar]
- 9. Buchner M, Baudendistel B, Sabo D, Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62–66. [DOI] [PubMed] [Google Scholar]
- 10. Camp CL, Heidenreich MJ, Dahm DL, et al. Individualizing the tibial tubercle—trochlear groove distance: patellar instability ratios that predict recurrent instability. Am J Sports Med. 2016;44(2):393–399. [DOI] [PubMed] [Google Scholar]
- 11. Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera. Apropos of 128 cases [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 12. Cheng C, Joseph SM, Solomito MJ, Pace JL. The effect of trochlear dysplasia on commonly used radiographic parameters to assess patellar instability. Orthop J Sports Med. 2019;7(3)(suppl):2325967119S2325900048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Christensen TC, Sanders TL, Pareek A, et al. Risk factors and time to recurrent ipsilateral and contralateral patellar dislocations. Am J Sports Med. 2017;45(9):2105–2110. [DOI] [PubMed] [Google Scholar]
- 14. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2018;26(1):8–15. [DOI] [PubMed] [Google Scholar]
- 15. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15(1):39–46. [DOI] [PubMed] [Google Scholar]
- 16. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 17. Fagerland MW, Hosmer DW. A generalized Hosmer–Lemeshow goodness-of-fit test for multinomial logistic regression models. Stata J. 2012;12(3):447–453. [Google Scholar]
- 18. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 19. Fitzpatrick CK, Steensen RN, Tumuluri A, et al. Computational analysis of factors contributing to patellar dislocation. J Orthop Res. 2016;34(3):444–453. [DOI] [PubMed] [Google Scholar]
- 20. Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW. High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1204–1209. [DOI] [PubMed] [Google Scholar]
- 21. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The natural history. Am J Sports Med. 1986;14(2):117–120. [DOI] [PubMed] [Google Scholar]
- 22. Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA. Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med. 2020;48(10):2552–2562. [DOI] [PubMed] [Google Scholar]
- 23. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. [DOI] [PubMed] [Google Scholar]
- 24. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop. 2017;37(7):484–490. [DOI] [PubMed] [Google Scholar]
- 25. Kaewkongnok B, Bøvling A, Milandt N, et al. Does different duration of non-operative immobilization have an effect on the redislocation rate of primary patellar dislocation? A retrospective multicenter cohort study. Knee. 2018;25(1):51–58. [DOI] [PubMed] [Google Scholar]
- 26. Kim HK, Shiraj S, Kang CH, et al. Patellofemoral instability in children: correlation between risk factors, injury patterns, and severity of cartilage damage. AJR Am J Roentgenol. 2016;206(6):1321–1328. [DOI] [PubMed] [Google Scholar]
- 27. Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg. 2015;28(4):303–309. [DOI] [PubMed] [Google Scholar]
- 28. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41(3):575–581. [DOI] [PubMed] [Google Scholar]
- 29. Lippacher S, Dejour D, Elsharkawi M, et al. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med. 2012;40(4):837–843. [DOI] [PubMed] [Google Scholar]
- 30. Martin RK, Leland DP, Krych AJ, Dahm DL. Treatment of first-time patellar dislocations and evaluation of risk factors for recurrent patellar instability. Sports Med Arthrosc Rev. 2019;27(4):130–135. [DOI] [PubMed] [Google Scholar]
- 31. McCarroll JR, Shelbourne KD, Porter DA, Rettig AC, Murray S. Patellar tendon graft reconstruction for midsubstance anterior cruciate ligament rupture in junior high school athletes. An algorithm for management. Am J Sports Med. 1994;22(4):478–484. [DOI] [PubMed] [Google Scholar]
- 32. Mehta VM, Inoue M, Nomura E, Fithian DC. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc Rev. 2007;15(2):78–81. [DOI] [PubMed] [Google Scholar]
- 33. Ménétrey J, Putman S, Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2320–2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14(4):513–515. [DOI] [PubMed] [Google Scholar]
- 35. Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76(5):699–704. [DOI] [PubMed] [Google Scholar]
- 36. Pagliazzi G, Napoli F, Previtali D, et al. A meta-analysis of surgical versus nonsurgical treatment of primary patella dislocation. Arthroscopy. 2019;35(8):2469–2481. [DOI] [PubMed] [Google Scholar]
- 37. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. [DOI] [PubMed] [Google Scholar]
- 38. Sanders TL, Pareek A, Hewett TE, et al. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health. 2018;10(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. [DOI] [PubMed] [Google Scholar]
- 40. Sillanpää PJ, Mäenpää HM. First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc Rev. 2012;20(3):128–135. [DOI] [PubMed] [Google Scholar]
- 41. Smith MK, Werner BC, Diduch DR. Avoiding complications with MPFL reconstruction. Curr Rev Musculoskelet Med. 2018;11(2):241–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2015;2:CD008106. [DOI] [PubMed] [Google Scholar]
- 43. Thévenin-Lemoine C, Ferrand M, Courvoisier A, et al. Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am. 2011;93(8):e35. [DOI] [PubMed] [Google Scholar]
- 44. Wagenmakers E-J, Farrell S. AIC model selection using Akaike weights. Psychon Bull Rev. 2004;11(1):192–196. [DOI] [PubMed] [Google Scholar]
- 45. Waterman BR, Belmont PJ, Owens BD. Patellar dislocation in the United States: role of sex, age, race, and athletic participation. J Knee Surg. 2012;25(1):51–57. [DOI] [PubMed] [Google Scholar]
- 46. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 47. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 48. Yue RA, Arendt EA, Tompkins MA. Patellar height measurements on radiograph and magnetic resonance imaging in patellar instability and control patients. J Knee Surg. 2017;30(9):943–950. [DOI] [PubMed] [Google Scholar]