Abstract
Background:
There is a lack of research on the effects of a postoperative rehabilitation program on anterior cruciate ligament (ACL) graft rupture.
Hypothesis:
We hypothesized that a hip-focused rehabilitation protocol with graft rupture education and avoidance training (HIP-GREAT program) would demonstrate lower ACL graft rupture rates compared with a traditional physical therapy (PT) program.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This study consisted of young athletes who had undergone ACL reconstruction at a single institution. Postoperatively, 136 participants (mean age, 16.9 ± 2.4 years) were enrolled in a traditional PT protocol between 2006 and 2010, and 153 participants (mean age, 17.0 ± 2.3 years) were enrolled in the HIP-GREAT protocol between 2011 and 2015. Follow-up rates were 31% (42/136) and 27% (41/153) in the traditional PT and HIP-GREAT groups, respectively, at 3 years postoperatively. The hazard ratio was calculated, and absolute risk reduction (ARR) and number-needed-to-treat (NNT) analyses were performed to compare the 2 protocols.
Results:
ACL graft rupture occurred in 10 patients (7.4%) in the traditional PT group and 5 patients (3.3%) in the HIP-GREAT group. This difference was not statistically significant (hazard ratio, 0.39; 95% CI, 0.14 to 1.16; P = .09). The ARR was 0.041 (95% CI, –0.011 to 0.093), and the NNT was 24.5.
Conclusion:
This study did not demonstrate a statistically significant reduction of ACL graft rupture in patients in the HIP-GREAT group. However, high ARR values and low NNT values were found, which suggests the possible effectiveness of the HIP-GREAT protocol to reduce ACL graft ruptures in young athletes.
Keywords: Reinjury, physical therapy, hip, neuromuscular training, education
Anterior cruciate ligament (ACL) injury is considered one of the most traumatic joint injuries. It has been estimated that approximately 80,000 to 350,000 ACL injuries occur annually in the United States alone.9,53,64 ACL tears often happen in physically active youth,35 and several descriptive epidemiological studies have shown an increase of ACL injuries over the past several decades,12,22,26 especially in adolescent athletes.22 Currently, ACL reconstruction (ACLR) remains the standard of care, especially for those who are aiming to return to sport activities. However, returning to sport activities requires substantial time after ACLR; the suggested time duration ranges from 6 to 9 months.18,20 Additionally, even after athletes have been cleared to return to sporting activities, recent evidence has suggested that only 40% return to their preinjury level of sport.2 Furthermore, significant functional deficits including reduced muscular strength,48,55,59,63 diminished postural control,56 altered landing patterns,27 and different gait mechanics1 have been reported after ACLR.
One of the most devastating events after ACLR is a subsequent ACL tear including both ipsilateral graft rupture and contralateral ACL injury. A few studies have reported a relatively high number of subsequent ACL injuries.†† Drawing on the available evidence, Shelbourne et al52 reported that the subsequent ACL injury rate at 5-year follow-up was 9.6%, with an ipsilateral graft rupture rate of 4.3% and contralateral ACL injury rate of 5.3%.52 However, subgroup analysis indicated a 17.4% rate of subsequent ACL injury for patients with ACLR who were younger than 18 years.52 Another study documented a 32% rate of subsequent ACL injury in athletes younger than 18 years at a mean follow-up of 48.3 months.10 Evidence shows that younger athletes are particularly at risk for a subsequent ACL injury.10,38,40,52,61,62 Subsequent ACL injury, either ipsilateral graft rupture or contralateral ACL injury after ACLR, negatively influences knee function and quality of life,14 induces degenerative changes in the knee,15,31 and hinders an athlete’s sport career.2,5,7,15
Several studies have examined timing of subsequent injuries to the ACL.4,40,51,61,62 Webster and Feller61 tracked 354 teenaged patients after ACLR and examined the status of ACL graft ruptures. According to that study, nearly half of the ACL graft ruptures happened within the first year after ACLR, and approximately 75% of all ACL graft ruptures occurred within 2 years.61 In contrast, contralateral ACL injury often occurs between 3 and 5 years after ACLR.40,61 Considering the high risk of ACL graft rupture within 2 years after ACLR, postoperative rehabilitation may play a key role. A few intervention studies have been performed to determine the effects of training programs designed to reduce the risk of primary ACL injury tear.24,39,44,60 However, there is a lack of studies investigating effects of postoperative rehabilitation on ACL graft rupture.58
One of the most recent primary ACL injury prevention training studies implemented hip-focused injury prevention (HIP) training. This training demonstrated significant reduction in the incidence of ACL injury in female collegiate basketball.44 In our clinics, we developed an educational component called graft rupture education and avoidance training (GREAT) and incorporated this with HIP training (HIP-GREAT) as a postoperative rehabilitation program. A positive effect of education on ACL injury reduction was initially documented by Ettlinger et al.13 In that study, the research team provided an educational session to prevent ACL injury in alpine skiers, which resulted in a 62% reduction of ACL injuries.13 Several other primary ACL injury prevention studies have incorporated educational components in their programs and demonstrated ACL injury reduction.36,41,47
The purpose of this study was to determine the effectiveness of the HIP-GREAT rehabilitation program in preventing ACL graft rupture in young athletes after ACLR. Our hypothesis was that patients participating in the HIP-GREAT program would demonstrate lower rates of ACL graft rupture than would patients participating in traditional physical therapy (PT).
Methods
Participants
This study was conducted at a single institution between January 2006 and October 2015. Ethical approval was obtained from the study institution before study commencement. This study consisted of patients who had undergone ACLR by a single orthopaedic surgeon (T.H.) via the same surgical procedure using an anatomic double-bundle hamstring autograft. The postoperative rehabilitation protocol consisted of traditional PT between January 2006 and March 2010 and HIP-GREAT between April 2011 and October 2015.
We used the following inclusion criteria: (1) age between 12 and 22 years at the time of ACLR and (2) participation in middle school, high school, and collegiate varsity athletics. We excluded the following: (1) patients with bony fractures on either the tibia or the femur at the time of ACL injury, any other knee ligament damage (medial collateral ligament, posterior cruciate ligament, lateral collateral ligament) requiring surgical intervention at the time of ACLR, and a history of previous ACL injury; (2) patients who were planning to return to collision sports, such as football, ice hockey, and rugby; (3) those who were planning to return to skiing; and (4) those who were planning to reduce their athletic participation levels after ACLR. We excluded patients who participated in collision sports because potential direct blows to the knee joint might confound the purpose of this study. Skiers were excluded because the HIP-GREAT was primarily designed for athletes who engaged in decelerating, cutting, and pivoting movements. In addition, participants who were planning to reduce their levels of athletic participation were excluded because our focus was on competitive varsity-level athletes.
A total of 496 young male and female athletes were considered for this study (n = 233 for traditional PT and 263 for HIP-GREAT). After we applied the inclusion and exclusion criteria, 289 athletes (136 for traditional PT, 153 for HIP-GREAT) with a mean age of 16.9 ± 2.3 years were ultimately included (Figure 1).
Figure 1.
Flowchart of study patients. ACL, anterior cruciate ligament; HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy.
Postoperative Rehabilitation
The postoperative rehabilitation protocol was the same for both groups during the first several weeks. The focus of the initial stage of rehabilitation was to treat postoperative pain, swelling, and other symptoms associated with ACLR. Ice, rest, and nonsteroidal anti-inflammatory drugs were used to reduce pain and swelling. We usually allowed partial weightbearing at 1 week and full weightbearing at 2 weeks after ACLR. During the first 3 months after ACLR, postoperative bracing was required; between 4 and 9 months, a functional knee brace was worn.
Traditional Physical Therapy Protocol
The traditional PT protocol consisted of a standard rehabilitation program that targets return to sport at 9 months after ACLR (Appendix Table A1).
HIP-GREAT Protocol
In the HIP-GREAT program, we added 16 unique hip-oriented exercises (7 strengthening exercises, 4 balance exercises, and 5 jump-landing exercises) to the traditional PT protocol (see the Appendix). The HIP-GREAT was designed to progressively enhance hip joint function through hip strengthening, balance and postural control exercises, and jump-landing maneuvers. These rehabilitation exercises were developed for the HIP training protocol reported by Omi et al.44 In brief, for hip strengthening, we implemented hip abduction and hip external rotation movements using a flexible band, and those exercises were progressed from open kinetic chain (OKC) (eg, clamshell exercise) to closed kinetic chain (CKC) (eg, standing hip abduction and lateral walk using a flexible exercise band). For balance and postural control training, patients were initially asked to control their posture during double-leg exercises. Next, they were progressed to single-leg exercises. Finally, patients were asked to perform a single-leg hop using controlled motions while maintaining quality of balance (eg, hop and land on Bosu ball [BOSU, Ashland, Ohio] from back to front and from side directions). Additionally, we used a jump-landing maneuver as a part of HIP-GREAT training. During the jump-landing task, we applied a flexible band at the participant’s thigh level to resist against hip adduction, hip internal rotation, and knee valgus motions. We emphasized keeping the flexible band taut while the patient was in the air (before landing) to facilitate protective landing mechanics before contact with the floor. In this particular exercise, patients were instructed to align the knee over the toe to maintain neutral knee alignment during landing. Greater knee and hip flexion were encouraged for a soft landing during the jump-landing task.
Another important feature of the HIP-GREAT was an educational component. We developed an educational brochure, which covered (1) ACLR and the graft remodeling process, (2) key points of rehabilitation exercises and avoidance of potentially risky movements, and (3) risk of reinjury (relatively high incidence rates and hazardous times [within 2 years after ACLR] for ACL graft ruptures). This educational session occurred 3 times: during hospitalization, 3 months after ACLR, and 6 months after ACLR. The educational session was performed in a one-on-one format with a physical therapist, the patient, and his or her family, usually lasting for 30 minutes. The physical therapist explained key points in each educational session and addressed clinical, rehabilitative, and performance-oriented questions from the patient and family members.
Return-to-Play Assessment
We assessed the isokinetic strength of the quadriceps and hamstring at 60 deg/s using an ARIEL-CES 5000 with arm and leg stations (Ariel Dynamics Inc). During the isokinetic strength tests, the average torque value of 3 repetitions was extracted, and the ratio between the involved and uninvolved limbs was calculated as a limb symmetry index (LSI) ([Involved Limb ÷ Uninvolved Limb] × 100%). Mean peak torque values of the hamstring-to-quadriceps (H:Q) ratio were also recorded. We investigated knee laxity using a KT-1000 arthrometer (side-to-side difference, involved knee minus uninvolved knee) at the time of return to sport. Recommendations regarding return to play were made based on the testing results of isokinetic strengthening (≥90% of healthy, contralateral limb), joint laxity (side-to-side difference <3 mm and negative Lachman tests), symptoms (absence of pain and swelling in the surgical knee joint), agility footwork (favorable knee alignment, especially no valgus in cutting), and drop vertical jump (adequate knee flexion without valgus in landing). Functional tests, agility footwork, and drop vertical jump were evaluated by physical therapists upon visual inspection. Final clearance was given based on results of the return-to-sport tests and physician discretion. Most patients received a clearance to return to play at 9 months after ACLR.
Follow-up
Patients were tracked for 3 years after ACLR. An email was sent every 9 months (4 times during 3 years) to identify occurrences of ACL graft rupture. Occasionally, patients voluntarily visited our clinics to provide updates on their knee condition. Physical therapists and affiliated members who were involved in this study were often present at major regional sporting competitions, which allowed us to check the participants’ injury and sport participation status. When we observed that patients were participating at a lower level of sport compared with their pre-ACLR status, they were excluded from the follow-up. In cases where ACL graft ruptures were suspected, orthopaedic physicians who specialized in sports injury initially provided a physical evaluation. Then, all of the ACL graft ruptures were verified using magnetic resonance imaging or arthroscopy. The mechanism of ACL graft tear was confirmed via an in-person interview during a participant’s clinical visits.
Statistical Analysis
Survival analysis was performed based on the number of ACL graft tears over time between traditional PT and HIP-GREAT protocols, and the hazard ratio (HR) was calculated. Absolute risk reduction (ARR) and number-needed-to-treat (NNT) analyses were performed based on calculations described in past studies.19,57 To ensure that key parameters, such as demographics (sex, age, height, weight, and body mass index), comorbidities (meniscal tears, repairs, and meniscectomy), isokinetic strength tests (quadriceps, hamstrings, and H:Q ratio), and KT-1000 arthrometer measurements were comparable between the 2 rehabilitation protocols, an independent t test, Mann-Whitney U test, and chi-square analysis were used. Shapiro-Wilk testing was performed to determine normality of continuous variables and application of a series of t tests (an independent t or Mann-Whitney U test). Statistical significance was set as P ≤ .05, and SPSS Version 24 (IBM Corp) was used for all analyses.
Results
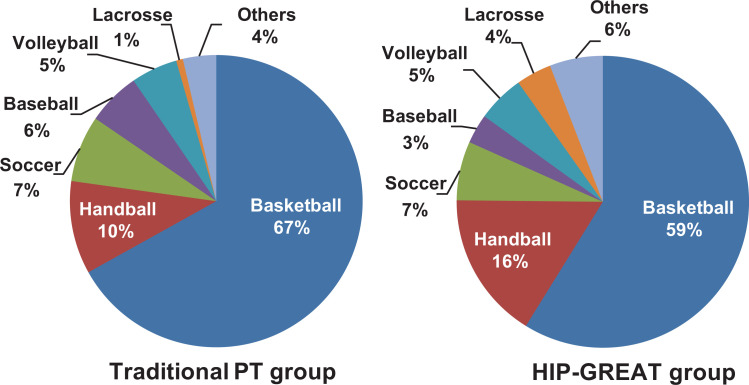
The participants’ characteristics including sex, age, follow-up period, height, weight, body mass index, and meniscal injury status are presented in Table 1. No significant difference between the 2 groups was observed for any characteristic. At 9, 18, 27, and 36 months after ACLR, the follow-up rate for the traditional PT group was 96%, 50%, 37%, and 31%, respectively, and the follow-up rate for HIP-GREAT group was 97%, 65%, 46%, and 27%, respectively. There were no significant differences in isokinetic strength or knee laxity between the 2 groups (Table 2). LSI and H:Q ratio in both groups were approximately 90% and 60%, respectively (Table 2). Participants’ sporting activities at the time of ACL rupture are shown in Figure 2, and no statistically significant differences were detected between the 2 groups (P = .27).
Table 1.
Patient Characteristicsa
| Traditional PT Group (n = 136) | HIP-GREAT Group (n = 153) |
P Value | |
|---|---|---|---|
| All patients | |||
| Sex, n | .09 | ||
| Male | 32 | 24 | |
| Female | 104 | 129 | |
| Age, y | 16.9 ± 2.4 (13-22) | 17.0 ± 2.3 (12-22) | .49 |
| Follow-up, mo | 22.3 ± 11.1 (3.8-36) | 24.2 ± 10.3 (7.1-36) | .21 |
| Male patients | |||
| Age, y | 17.8 ± 2.5 (15-22) | 17.1 ± 2.5 (12-22) | .44 |
| Height, cm | 174.2 ± 8.4 (159.0-190.0) | 175.0 ± 9.0 (154.0-200.0) | .76 |
| Weight, kg | 69.0 ± 9.1 (52.0-86.0) | 69.5 ± 11.1 (49.8-88.0) | .85 |
| BMI | 22.7 ± 2.0 (18.5-26.6) | 22.7 ± 2.9 (17.4-30.3) | .98 |
| Meniscal tears,b n (%) | .48 | ||
| No | 15 (46.9) | 9 (37.5) | |
| Yes | 17 (53.1) | 15 (62.5) | |
| Medial meniscus, n (%) | .80 | ||
| Repair | 7 (87.5) | 2 (100) | |
| Meniscectomy, rasping | 1 (12.5) | 0 (0) | |
| Lateral meniscus, n (%) | .59 | ||
| Repair | 10 (90.9) | 12 (85.7) | |
| Meniscectomy, rasping | 1 (9.1) | 2 (14.3) | |
| Female patients | |||
| Age, y | 16.5 ± 2.3 (13-22) | 16.9 ± 2.2 (12-22) | .15 |
| Height, cm | 162.0 ± 6.5 (145.0-175.0) | 162.5 ± 6.9 (147.0-182.0) | .56 |
| Weight, kg | 56.8 ± 6.6 (41.0-76.0) | 55.7 ± 6.6 (40.0-83.0) | .21 |
| BMI | 21.6 ± 1.9 (18.1-29.1) | 21.1 ± 2.0 (16.6-31.2) | .10 |
| Meniscal tears,c n (%) | .86 | ||
| No | 52 (50.0) | 66 (51.2) | |
| Yes | 52 (50.0) | 63 (48.8) | |
| Medial meniscus, n (%) | .26 | ||
| Repair | 13 (86.7) | 28 (96.6) | |
| Meniscectomy, rasping | 2 (13.3) | 1 (3.4) | |
| Lateral meniscus, n (%) | .26 | ||
| Repair | 41 (91.1) | 40 (83.3) | |
| Meniscectomy, rasping | 4 (8.9) | 8 (16.7) |
aData are presented as mean ± SD (range) unless otherwise indicated. BMI, body mass index; HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy.
bTwo participants in the traditional PT group and 1 participant in the HIP-GREAT group underwent medial and lateral meniscal repair.
cFive participants in the traditional PT group and 12 participants in the HIP-GREAT group underwent medial and lateral meniscal repair; 1 participant in the traditional PT group and 1 participant in the HIP-GREAT group underwent medial meniscal repair and lateral meniscal meniscectomy; 1 participant in the traditional PT group and 1 participant in the HIP-GREAT group underwent lateral meniscal repair and meniscectomy; and 1 participant in the traditional PT group underwent medial and lateral meniscal meniscectomy.
Table 2.
Comparison of Isokinetic Strength Test and Knee Laxitya
| Traditional PT Group | HIP-GREAT Group | P Value | |
|---|---|---|---|
| Limb symmetry index, % | |||
| Quadriceps strength | 91.8 ± 11.5 | 91.5 ± 11.9 | .83 |
| Hamstring strength | 89.3 ± 8.3 | 91.0 ± 11.1 | .14 |
| H:Q ratio, % | |||
| Involved limb | 61.2 ± 11.5 | 62.0 ± 9.9 | .37 |
| Uninvolved limb | 62.1 ± 10.4 | 63.0 ± 11.7 | .78 |
| Knee laxity, mmb | 0.8 ± 2.0 | 0.7 ± 1.8 | .54 |
aData are presented as mean ± SD. HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; H:Q, hamstring to quadriceps; PT, physical therapy.
bKT-1000 arthrometer side-to-side difference, involved knee minus uninvolved knee.
Figure 2.
Distribution of sports participation. No significant differences were seen between the 2 groups (P = .27). HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy.
In the PT group, ACL graft rupture occurred in 10 patients (7.4%; 5 male and 5 female; mean age, 16.0 ± 2.7 years; range, 13-21 years) at a mean of 11.6 ± 4.7 months postoperatively (range, 3.8-17.6 months). In the HIP-GREAT group, 5 patients experienced graft rupture (3.3%; all female; mean age, 15.4 ± 1.1 years; range, 14-17 years) at a mean of 12.9 ± 4.4 months postoperatively (range, 7.1-17.0 months). Although statistical significance was not detected (P = .08), fewer ACL graft ruptures occurred in the HIP-GREAT group during 3 years of follow-up (Figure 3). We noted no statistically significant HR reduction between the 2 groups (HR, 0.39; 95% CI, 0.14-1.16; P = .09) (Figure 3).
Figure 3.

Comparison of anterior cruciate ligament (ACL) graft rupture rate. HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy.
The ARR was 0.041 (95% CI, –0.011 to 0.093) or 4.1%, and the NNT analysis indicated that at least 25 patients with ACLR were necessary to prevent 1 ACL graft rupture (NNT = 24.5) at 3-year follow-up. In the traditional PT group, ACL graft ruptures were observed in 9 basketball players and 1 soccer player. Among participants who received the HIP-GREAT protocol, 4 basketball players and 1 handball player sustained an ACL graft rupture. All ACL graft ruptures occurred under noncontact mechanisms except in 1 case, for which the specific mechanism and timeline were unidentified (Table 3).
Table 3.
Patients With ACL Graft Rupturea
| Patient | Age, y | Sex | Injury Activity | RTS Without Physician’s Permission | Time to Graft Rupture, mo | Mechanism of Primary ACL Injury | Mechanism of Graft Rupture |
|---|---|---|---|---|---|---|---|
| Traditional PT | |||||||
| 1 | 13 | Female | Basketball | – | 15.1 | Noncontact | Noncontact |
| 2 | 19 | Female | Basketball | – | 10.9 | Contact | Noncontact |
| 3 | 14 | Female | Basketball | – | 14.9 | Contact | Noncontact |
| 4 | 14 | Female | Basketball | – | 17.6 | Noncontact | Noncontact |
| 5 | 15 | Male | Basketball | + | 3.8b | Contact | Noncontact |
| 6 | 15 | Female | Basketball | – | 9.4 | Noncontact | Noncontact |
| 7 | 15 | Male | Basketball | + | 4.7c | Noncontact | Noncontact |
| 8 | 15 | Male | Basketball | – | 12.4 | Noncontact | Noncontact |
| 9 | 21 | Male | Soccer | – | 16.3 | Noncontact | Noncontact |
| 10 | 19 | Male | Basketball | – | 10.9d | Noncontact | Unknown |
| HIP-GREAT | |||||||
| 1 | 14 | Female | Basketball | – | 16.0 | Noncontact | Noncontact |
| 2 | 17 | Female | Basketball | – | 9.5 | Noncontact | Noncontact |
| 3 | 15 | Female | Basketball | – | 7.1e | Noncontact | Noncontact |
| 4 | 15 | Female | Handball | – | 17.0 | Noncontact | Noncontact |
| 5 | 16 | Female | Basketball | – | 15.0 | Noncontact | Noncontact |
aACL, anterior cruciate ligament; HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy; RTS, return to sport; +, patient who returned to sports without physician’s clearance; –, patient who returned to sports with physician’s clearance.
bPatient was cleared only for jogging but practiced a layup and was injured on the landing.
cPatient was cleared only for jogging but participated in a basketball lesson and was injured while playing.
dPatient did not know the exact time of graft rupture, so graft rupture was calculated as the date of the examination indicating knee instability.
ePatient was injured during a practice session as she tried to avoid contact with a defender.
Discussion
The primary goal of this study was to investigate the effectiveness of the HIP-GREAT rehabilitation program in preventing ACL graft rupture in young athletes after ACLR. Our analysis did not indicate any statistically significant difference between a traditional PT program and the HIP-GREAT protocol, although 61% of HR reduction was noted (HR, 0.39; 95% CI, 0.14-1.16). An a posteriori power analysis showed that 181 participants were needed to achieve statistical significance in each group. In this study, the ACL graft rupture rate of 7.4% in the traditional PT group was comparable with rates found in several previous studies.17,38,40,61 According to a few studies that investigated ACL graft rupture after ACLR with follow-up periods of 14 to 24 months, the reported rates of ACL graft rupture ranged from 10.0% to 14.3%. Additionally, physical characteristics, quadriceps strength, hamstring strength, H:Q ratio, and KT-1000 arthrometer measurements at the time of return to play were not different between the traditional PT and HIP-GREAT groups. Therefore, we believe that the HIP-GREAT program, which had a graft rupture rate of 3.3%, has the potential to reduce the number of graft ruptures after ACLR. Additionally, the current study showed a relatively high ARR (4.1%) and a notably low NNT (at least 25 patients with ACLR were needed to prevent 1 ACL graft rupture) compared with values from primary ACL injury prevention studies, which have reported ARRs ranging from 0.1% to 5.2%‡‡ and NNTs ranging from 36 to 644, all number-needed-to-treat to benefit.19,57
Historically, several biomechanical and neuromuscular risk factors of primary ACL injury have been reported.25,33,37,42 However, modifiable risk factors of secondary ACL injury have been understudied. Paterno et al46 identified hip internal rotation moment, increased knee valgus movement, greater asymmetry in knee extensor moment during the initial landing phase of a drop vertical jump, and altered postural stability as risk factors for secondary ACL injuries. Studies have documented other risk factors, such as female sex; young age; greater number of athletic exposures; timing of return to play; participation in sports that involve cutting, pivoting, and decelerating; and H:Q ratio.6,18,34,45 Although studies that focused on modifiable risk factors of the ACL graft rupture were scarce, we surmised that strengthening hip muscles, improving awareness of knee position, and enhancing overall balance and postural control during cutting and landing maneuvers would be beneficial during postoperative rehabilitation, especially in terms of reducing ACL graft ruptures. Moreover, several years after ACLR, continuous biomechanical and neuromuscular deficits have been reported.1,8,27,48,55,56,59,63 This evidence supports that incorporating ancillary exercises into a traditional rehabilitation program would be more beneficial than would using traditional rehabilitation alone. Furthermore, a few recent articles have suggested preventive intervention after ACLR.11,23
We considered that training of hip external rotators and hip abductors would facilitate neutral knee alignment. Several investigations have found an association between decreased hip abductor strength and increased knee valgus in dynamic movements.21,28 Additionally, Khayambashi et al29 reported that decreased hip abductor and external rotator strength were associated with greater risk of sustaining a primary noncontact ACL injury. Therefore, in the HIP-GREAT protocol, hip strengthening was performed throughout the entire rehabilitation process. Hip strengthening was performed with OKC exercises at the beginning of rehabilitation. Later, exercises were progressed to CKC styles. During this progression from OKC to CKC in the first several months after ACLR, a flexible band was used at the thigh level to further enhance hip strength with emphasis on neutral knee alignment. At around 5 to 6 months, we focused on enhancing quality of movements and emphasized neuromuscular control of hip, knee, and ankle joints. To facilitate better-quality movements along with the progression of exercise, jump-landing training was incorporated. During this exercise, a flexible band was kept at the thigh level to counterbalance hip adduction, hip internal rotation, and knee valgus movements.
Another focus was placed on enhancing hip mechanics along with balance and postural control during cutting and landing. Koga et al32 reported that the hip joints were flexed, abducted, and internally rotated at the time of ACL injury, especially within 40 milliseconds of the initial phase in cutting and landing maneuvers. The investigators explained that these particular hip positions may hinder the athlete’s ability to attenuate ground-reaction force and may potentially lead to ACL injury.32 Another study supported this finding. According to Pollard et al,50 low knee and hip flexion angles during landing are associated with increased knee valgus angles, increased knee adductor moments, and decreased energy absorption at the knee and hip joints. Therefore, we considered that hip function is vital, especially the hip mechanics before initial contact in landing maneuvers. For this reason, we instructed patients in the HIP-GREAT group to move their hip in a posterior direction while maintaining neutral knee alignment. To optimize this particular movement, we provided verbal cues, such as “use hip before knee.”
Last, patient education was a unique, yet imperative component of the HIP-GREAT program. We developed a structured brochure and 3 educational sessions highlighting the healing process, return-to-play timeline, and graft retear risk after ACLR. The educational session lasted 30 minutes and usually included the patient, his or her family members, and a physical therapist. This initiative was a vital part of the HIP-GREAT program, and we were able to establish specific, short-term goals relative to patients’ recovery. For instance, after ACLR, we focused on explaining the graft remodeling process and the ACLR surgical process. In the meeting, we often stressed that remodeling requires time, emphasizing that return to play is based not only on physical recovery after surgery but also on healing time after ACLR. We were surprised to find that some of the patients and their family members were not aware that insufficient graft maturation may increase the likelihood of ACL graft rupture. One of the most frequently asked questions regarded the most appropriate timeline for return to play, which was addressed in one of the educational sessions. After we implemented the educational sessions in the HIP-GREAT program, there were no cases of premature return to play. We believe this was a reflection of setting short-term goals during the educational sessions. Hence, we believe that educating patients led to realistic expectations with regard to return-to-play timing and understanding the rehabilitation process.
This study has several limitations. First, the follow-up rates may be perceived as low; however, we focused on only those patients who returned to their original sport and continued competing at their original level. Furthermore, the reporting period was 1 year longer than that in previous studies.18,46 Additionally, 1 study2 reported that only 41% of young athletes played at their preinjury level of sport 2 years after ACLR. At 27 months of follow-up in the current study, the follow-up rates were 37% and 46% in traditional PT and HIP-GREAT groups, respectively, which are comparable with previous reports. Second, the current study was not a randomized controlled trial. It was difficult to randomly implement a different rehabilitation protocol in our clinical setting. Thus, we compared 2 different rehabilitation protocols used during 2 different time periods. To ensure that there were no baseline differences between the 2 cohorts, we carefully checked patients’ physical characteristics (Table 1), muscular strength (Table 2), and joint laxity (Table 2). Additionally, to maintain the rigor of this study, 1 orthopaedic surgeon (T.H.) performed all ACLRs using the same surgical procedure. Thus, we believe that there were minimal or no confounding variables between the 2 periods. Third, we did not collect data on postsurgical activity, such as the number of hours the sport or activity was played during the follow-up period. Fourth, HIP-GREAT includes not only a training program but also patient education. It would have been ideal to assess the effectiveness of the ACL graft rupture reduction training program and patient education separately. Future studies are warranted to consider these limitations.
Conclusion
We compared 2 different post-ACLR rehabilitation protocols: a traditional PT protocol versus HIP-GREAT. The rate of graft rupture was 7.4% (10/136) in the traditional ACL rehabilitation group and 3.3% (5/153) in the HIP-GREAT group. This finding was not statistically significant; however, fairly high ARR (4.1%) and low NNT (at least 25 patients with ACLR needed) were recorded in the HIP-GREAT group. There are reports that postoperative rehabilitation protocols improve neuromuscular function, which was theorized to reduce the risk of graft rupture after ACLR.3,11,23 However, the effectiveness of specific rehabilitation programs on ACL graft rupture reduction has not been documented. Although statistical significance was not detected in the current study, the graft rupture reduction observed in the HIP-GREAT group may be clinically valuable. Future studies are needed to identify and develop an ideal post-ACLR rehabilitation protocol to reduce graft rupture in young patients who undergo ACLR.
Acknowledgment
The authors thank the following staff of the Department of Rehabilitation, Nippon Koukan Hospital: Songjo Yun, PT, Kaori Nagatsuma, PT, Masashi Kaneko, PT, Tomohisa Kurihara, PT, Tomomi Doi, PT, Daisuke Seki, PT, Masumi Yoshimoto, PT, Yasuhiro Kunita, PT, MS, Takumi Inoue, PT, and Mizuho Inoue, PT.
Appendix
Table A1.
Traditional PT and HIP-GREAT Postoperative Rehabilitation Protocolsa
| Phase 1: ACLR to discharge (patients were discharged 3 weeks after ACLR) |
| Goals |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Phase 2: 1-3 months after ACLR (continue with phase 1 exercises and increase repetitions and weights) |
| Goal |
|
|
|
|
|
|
| Phase 3: 3-9 months after ACLR (continue with phase 1 and 2 exercises and increase repetitions and weights) |
| Goals |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
aPrograms added only to the HIP-GREAT protocol are shown in italics and underlined. ACL, anterior cruciate ligament; ACLR, ACL reconstruction; HIP-GREAT, hip-focused rehabilitation protocol with graft rupture education and avoidance training; PT, physical therapy.
Appendix Figure A1.
Exercises for hip-focused rehabilitation protocol with graft rupture education and avoidance training: (A) hip external rotation with flexible band, (B) lateral walk with flexible band, (C) standing hip abduction with flexible band, (D) jump landing with flexible band for basketball players, and (E) alternating leg hop on uneven surface.
Footnotes
Final revision submitted June 3, 2020; accepted June 30, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Nippon Koukan Hospital (No. 2006-7).
References
- 1. Abourezk MN, Ithurburn MP, McNally MP, et al. Hamstring strength asymmetry at 3 years after anterior cruciate ligament reconstruction alters knee mechanics during gait and jogging. Am J Sports Med. 2017;45(1):97–105. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43(4):848–856. [DOI] [PubMed] [Google Scholar]
- 3. Arundale AJH, Capin JJ, Zarzycki R, Smith AH, Snyder-Mackler L. Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-SPORTS). Int J Sports Phys Ther. 2018;13(3):422–431. [PMC free article] [PubMed] [Google Scholar]
- 4. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 5. Chicorelli AM, Micheli LJ, Kelly M, Zurakowski D, MacDougall R. Return to sport after anterior cruciate ligament reconstruction in the skeletally immature athlete. Clin J Sport Med. 2016;26(4):266–271. [DOI] [PubMed] [Google Scholar]
- 6. Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. [DOI] [PubMed] [Google Scholar]
- 7. Christino MA, Tepolt FA, Sugimoto D, Micheli LJ, Kocher MS. Revision ACL reconstruction in children and adolescents. J Pediatr Orthop. 2020;40(3):129–134. [DOI] [PubMed] [Google Scholar]
- 8. Chung KS, Ha JK, Yeom CH, et al. Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Two-year follow-up after reconstruction. Am J Sports Med. 2015;43(12):3013–3021. [DOI] [PubMed] [Google Scholar]
- 9. Cimino F, Volk BS, Setter D. Anterior cruciate ligament injury: diagnosis, management, and prevention. Am Fam Physician. 2010;82(8):917–922. [PubMed] [Google Scholar]
- 10. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 11. Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777–792, A771-A711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 13. Ettlinger CF, Johnson RJ, Shealy JE. A method to help reduce the risk of serious knee sprains incurred in alpine skiing. Am J Sports Med. 1995;23(5):531–537. [DOI] [PubMed] [Google Scholar]
- 14. Faltstrom A, Hagglund M, Kvist J. Patient-reported knee function, quality of life, and activity level after bilateral anterior cruciate ligament injuries. Am J Sports Med. 2013;41(12):2805–2813. [DOI] [PubMed] [Google Scholar]
- 15. Gifstad T, Drogset JO, Viset A, Grontvedt T, Hortemo GS. Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2011–2018. [DOI] [PubMed] [Google Scholar]
- 16. Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. [DOI] [PubMed] [Google Scholar]
- 17. Graziano J, Chiaia T, de Mille P, Nawabi DH, Green DW, Cordasco FA. Return to sport for skeletally immature athletes after ACL reconstruction: preventing a second injury using a quality of movement assessment and quantitative measures to address modifiable risk factors. Orthop J Sports Med. 2017;5(4):2325967117700599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train. 2006;41(4):450–456. [PMC free article] [PubMed] [Google Scholar]
- 20. Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37(2):e103–e108. [DOI] [PubMed] [Google Scholar]
- 21. Heinert BL, Kernozek TW, Greany JF, Fater DC. Hip abductor weakness and lower extremity kinematics during running. J Sport Rehabil. 2008;17(3):243–256. [DOI] [PubMed] [Google Scholar]
- 22. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171(8):808–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. [DOI] [PubMed] [Google Scholar]
- 25. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 26. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 27. Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 28. Jacobs CA, Uhl TL, Mattacola CG, Shapiro R, Rayens WS. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train. 2007;42(1):76–83. [PMC free article] [PubMed] [Google Scholar]
- 29. Khayambashi K, Ghoddosi N, Straub RK, Powers CM. Hip muscle strength predicts noncontact anterior cruciate ligament injury in male and female athletes: a prospective study. Am J Sports Med. 2016;44(2):355–361. [DOI] [PubMed] [Google Scholar]
- 30. Kiani A, Hellquist E, Ahlqvist K, Gedeborg R, Michaelsson K, Byberg L. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170(1):43–49. [DOI] [PubMed] [Google Scholar]
- 31. Kievit AJ, Jonkers FJ, Barentsz JH, Blankevoort L. A cross-sectional study comparing the rates of osteoarthritis, laxity, and quality of life in primary and revision anterior cruciate ligament reconstructions. Arthroscopy. 2013;29(5):898–905. [DOI] [PubMed] [Google Scholar]
- 32. Koga H, Nakamae A, Shima Y, Bahr R, Krosshaug T. Hip and ankle kinematics in noncontact anterior cruciate ligament injury situations: video analysis using model-based image matching. Am J Sports Med. 2018;46(2):333–340. [DOI] [PubMed] [Google Scholar]
- 33. Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218–2225. [DOI] [PubMed] [Google Scholar]
- 34. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 35. LaBella CR, Hennrikus W, Hewett TE. Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics. 2014;133(5):e1437–e1450. [DOI] [PubMed] [Google Scholar]
- 36. LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. [DOI] [PubMed] [Google Scholar]
- 37. Leppanen M, Pasanen K, Kujala UM, et al. Stiff landings are associated with increased ACL injury risk in young female basketball and floorball players. Am J Sports Med. 2017;45(2):386–393. [DOI] [PubMed] [Google Scholar]
- 38. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 39. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. [DOI] [PubMed] [Google Scholar]
- 40. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44(2):384–392. [DOI] [PubMed] [Google Scholar]
- 41. Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. [DOI] [PubMed] [Google Scholar]
- 42. Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. [DOI] [PubMed] [Google Scholar]
- 43. Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Omi Y, Sugimoto D, Kuriyama S, et al. Effect of hip-focused injury prevention training for anterior cruciate ligament injury reduction in female basketball players: a 12-year prospective intervention study. Am J Sports Med. 2018;46(4):852–861. [DOI] [PubMed] [Google Scholar]
- 45. Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med. 2017;5(12):2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125(9):614–621. [DOI] [PubMed] [Google Scholar]
- 48. Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134(10):1417–1428. [DOI] [PubMed] [Google Scholar]
- 49. Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88(8):1769–1774. [DOI] [PubMed] [Google Scholar]
- 50. Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech (Bristol, Avon). 2010;25(2):142–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948–957. [DOI] [PubMed] [Google Scholar]
- 52. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 53. Silvers HJ, Mandelbaum BR. Prevention of anterior cruciate ligament injury in the female athlete. Br J Sports Med. 2007;41(suppl 1):i52–i59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football—a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605–614. [DOI] [PubMed] [Google Scholar]
- 55. Sugimoto D, Heyworth BE, Collins SE, Fallon RT, Kocher MS, Micheli LJ. Comparison of lower extremity recovery after anterior cruciate ligament reconstruction with transphyseal hamstring versus extraphyseal iliotibial band techniques in skeletally immature athletes. Orthop J Sports Med. 2018;6(4):2325967118768044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sugimoto D, Howell DR, Micheli LJ, Meehan WP III. Single-leg postural stability deficits following anterior cruciate ligament reconstruction in pediatric and adolescent athletes. J Pediatr Orthop B. 2016;25(4):338–342. [DOI] [PubMed] [Google Scholar]
- 57. Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46(14):979–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Thrush C, Porter TJ, Devitt BM. No evidence for the most appropriate postoperative rehabilitation protocol following anterior cruciate ligament reconstruction with concomitant articular cartilage lesions: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1065–1073. [DOI] [PubMed] [Google Scholar]
- 59. Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47(11):825–833. [DOI] [PubMed] [Google Scholar]
- 60. Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(11):2827–2832. [DOI] [PubMed] [Google Scholar]
- 62. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 63. Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3636–3644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wojtys EM, Brower AM. Anterior cruciate ligament injuries in the prepubescent and adolescent athlete: clinical and research considerations. J Athl Train. 2010;45(5):509–512. [DOI] [PMC free article] [PubMed] [Google Scholar]