Abstract
Background
Given the serious impact of the COVID-19 outbreak on the mental health of Chinese adolescents, this study aimed to examine the proportion of anxiety and its correlates among Chinese adolescents with depression during the pandemic.
Methods
This cross-sectional online survey was conducted from February 20th to February 27, 2020 in China. Symptoms of depression and anxiety were assessed by the 20-item Center for Epidemiological Studies-Depression (CES-D) and 7-item Generalized Anxiety Disorder (GAD-7), respectively.
Results
In this study, 3,498 adolescents with depression were identified. Of them, the proportion of anxiety was 45.1% (95% confidence interval [CI]=43.5%-46.8%). Multiple logistic regression analysis revealed that being concerned about graduation (OR=1.25, P=0.002, 95% CI=1.09-1.43), sleep duration <6hr/day (OR=1.80, P<0.001, 95% CI=1.38-2.34), study duration >8hr/day (OR=1.21, P=0.02, 95% CI=1.03-1.42), and quantity of homework higher than before (OR=1.68, P<0.001, 95% CI=1.40-2.02) were positively associated with anxiety; the number of confirmed COVID-19 cases at a provincial level of 100-999 (OR=0.70, P<0.001, 95% CI=0.59-0.83) and 1,000-9,999 (OR=0.69, P=0.001, 95% CI=0.55-0.87) were negatively related to anxiety in adolescents with depression.
Limitations
Because this was a cross-sectional online study, the causality between variables and anxiety could not be examined among depressed adolescents. The use of self-reported scales may lead to an underestimation of the proportion of anxiety among adolescents with depression.
Conclusions
The symptoms of anxiety were common in adolescents with depression during the COVID-19 outbreak. Timing screening and targeted interventions are necessary to mitigate the risks of mental illness of adolescents.
Keywords: Adolescent, Anxiety, Depression, COVID-19, Chinese
1. Introduction
Since its first case was reported in Wuhan, China at the end of 2019, Coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) and raised international concern (World Health Organization, 2020a). By the end of February 2020, there were 85,405 confirmed cases and 2,924 deaths globally (World Health Organization, 2020b). To minimize the transmission of COVID-19, the Chinese government instituted a range of containment and mitigation strategies, such as the Chinese Ministry of Education suggested the primary and secondary schools postpone 2020 spring semester on January 27, 2020 (China's Ministry of Education, 2020). Implementation of society lockdown, household quarantine, and school closures resulted in a negative impact on mental health (Golberstein et al., 2020; Lee, 2020; Wang et al., 2020a).
Adolescents are a vulnerable and often overlooked population during the COVID-19 outbreak. Several studies have shown that COVID-19 might cause mental health issues such as depression, anxiety, and comorbidity (Duan et al., 2020; Guessoum et al., 2020). Chinese adolescents have endured various stressors in the period of COVID-19, such as home quarantine, fear of infection, conflicts with parents, isolation, and great changes in life circumstance, which were related with higher prevalence of depression, anxiety, and other mental health disorders (Guessoum et al., 2020; Xie et al., 2020; Zhou et al., 2020).
Symptoms of anxiety and depression often occur concurrently or sequentially in adolescents (Chavira et al., 2004; Garber and Weersing, 2010). Previous studies showed 25% to 50% of adolescents with a primary depression also had anxiety, while 10% to 15% of adolescent who met criteria for anxiety suffered from depression, which were generally lower (Garber and Weersing, 2010; Angold et al., 1999; Axelson and Birmaher, 2001; Costello et al., 2003; Cummings et al., 2014). Adolescents who comorbid of depression and anxiety were associated with various negative consequences, such as more severe mental health issues, suicidal thoughts and attempts, academic difficulties, and conflicts with parents (Cummings et al., 2014; Kessler et al., 2015; Melton et al., 2016). Zhou et. al (Zhou et al., 2020) conducted a cross-sectional study from March 8 to March 15, 2020 among Chinese students and found the prevalence of a combination of depressive and anxiety symptoms was 31.3%, however, the factors associated with depression comorbid with anxiety were not explored among the adolescents during the COVID-19 outbreak.
Therefore, we conducted this study to investigate the proportion and associated factors of anxiety among Chinese adolescents with depression during the COVID-19 pandemic. We hypothesized that academic pressures, irregular life and study behaviors and other epidemic related factors were associated with anxiety among adolescents with depression during COVID-19 outbreak.
2. Methods
2.1. Study design and participants
This study was part of a cross-sectional, national online survey conducted from February 20th to 27th, 2020 based on the collaborative research network of the National Clinical Research Center for Mental Disorders (Qi et al., 2020). Data collection was performed by the WeChat-based “QuestionnaireStar” program (Changsha Ranxing Science and Technology, Shanghai, China) using the snowball sampling method widely used by researchers during the outbreak (El-Zoghby et al., 2020; Liu et al., 2020a; Reuben et al., 2020). Voluntary participants were recruited from 34 provinces of China. Inclusion criteria included being 11-20 years of age, living in mainland China, and studying in junior or senior secondary school during the COVID-19 epidemic (Qi et al., 2020). Out of these adolescents, those who had depressive symptoms based on their 20-item Center for Epidemiological Studies-Depression (CES-D) scores were included in the study. Ethics approval for this study was obtained from the Medical Ethical Committee of Beijing Anding Hospital. All participants and their guardians provided informed consent before participating in the study.
2.2. Measurements
The online questionnaires included the following: (1) demographical data, such as age, gender, grade, residence; (2) attitudes and behaviors towards COVID-19, including mask-wearing and hand hygiene, number of confirmed cases of COVID-19 in the participant's province, either parents as frontline workers, acquaintance contracting COVID-19, concern about COVID-19, and concern about graduation; (3) impacts of COVID-19 on study and lifestyles, such as sleep duration, study duration, exercise duration, quantity of homework, and participation in distance learning; (4) depression and anxiety symptoms during the COVID-19 epidemic. The spread of the pandemic was determined by the number of confirmed COVID-19 cases in participants’ provinces; corresponding data were obtained from the website of the National Health Commission of the People's Republic of China. Additionally, Mainland provinces and autonomous regions were classified into 7 regions according to the geography, cultures and economics: Eastern (Shandong, Jiangsu, Anhui, Zhejiang, Fujian and Shanghai), Southern (Guangdong, Guangxi Zhuang Autonomous Region and Hainan), Central (Hubei, Hunan, Henan and Jiangxi), Northern (Beijing, Tianjin, Hebei, Shanxi and Inner Mongolia Autonomous Region), Northwest (Ningxia Hui Autonomous Region, Xinjiang Uygur Autonomous Region, Qinghai, Shaanxi and Gansu), Southwest (Sichuan, Chongqing, Yunnan, Guizhou and Tibet Autonomous Region) and Northeast (Liaoning, Jilin and Heilongjiang) (Fang et al., 2017).
The CES-D is a self-reported questionnaire that assesses the symptoms of depression during the past week (Radloff, 1977), including 20 items. Each items of CES-D ranges from 0 (none of the time) to 3 (almost all the time), and a total score ranges from 0-60. A cut-off score of 16 indicated the individual ‘having depressive symptoms’ (Radloff, 1991). The Chinese version of the CES-D has satisfactory internal reliability among adolescents (Sun et al., 2017; Zhao et al., 2019).
A self-report questionnaire of 7-item Generalized Anxiety Disorder (GAD-7) was applied to assess the symptoms of anxiety during the past two weeks. This scale includes 7 questions to reflect the frequency of anxiety symptoms. The total score ranges from 0 to 21; a value greater than 5 indicated potential risk for generalized anxiety symptoms (Spitzer et al., 2006). The Chinese version of GAD-7 had good reliability and validity in Chinese adolescents (Liu et al., 2017).
Furthermore, Cronbach's alpha values of GAD-7 and CES-D were 0.90 and 0.77 in the current sample, respectively, indicating the GAD-7 and CES-D have satisfactory psychometric properties in this study.
2.3. Statistical analysis
All the statistical analyses were performed with SPSS software version 21.0. To compare the difference between the depressed adolescents with and without anxiety, Chi-square test, independent two-sample t-test and Mann-Whitney U test were used, as appropriate. To explore the associated factors of anxiety in the adolescents with depression, multiple logistic regression models using the “enter” method were performed with the significant variables of univariate analysis as independent variables. Several factors were adjusted in multiple logistic regression models to further explore the interactions among the factors. In model 1, gender and grade were adjusted. In model 2, we further adjusted for COVID-19 related factors, such as parents as frontline workers, concerned about graduation, and so on. In model 3, lifestyle and academic factors, including study and sleep duration, quantity of homework, participating in distance learning were adjusted. And in model 4, COVID-19 related factors as well as lifestyle and academic factors were adjusted. P<0.05 was considered statistically significant (two-tailed).
3. Results
A total of 9,744 adolescents are invited to participate in the whole survey. There were 9,554 met the study criteria, of whom, 3,498 (36.6%) with depression (CES-D16) were included in the current study. The proportion of anxiety was 45.1% (95% CI= 43.5%-46.8%) among Chinese adolescents with depression during the COVID-19 outbreak. The sociodemographic characteristics of the adolescents with depression are shown in Table 1 .
Table 1.
Sociodemographic characteristics of adolescents with depression.
| Variables | Total (N=3,498) | With anxiety (N=1,579) | Without anxiety (N=1,919) | χ2 | P | |||
| N | % | N | % | N | % | |||
| Female | 1984 | 56.7 | 937 | 59.3 | 1047 | 54.6 | 8.07 | 0.005 |
| Age (years) | ||||||||
| 11-15 | 1,745 | 49.9 | 739 | 46.8 | 1,006 | 52.4 | 10.95 | 0.001 |
| 16-20 | 1,753 | 50.1 | 840 | 53.2 | 913 | 47.6 | ||
| Grade | ||||||||
| Junior secondary school | 1,693 | 48.4 | 719 | 45.5 | 974 | 50.8 | 9.45 | 0.002 |
| Senior secondary school | 1,805 | 51.6 | 860 | 54.5 | 945 | 49.2 | ||
| Number of confirmed COVID-19 cases at provincial level | ||||||||
| 10-99 | 825 | 23.6 | 442 | 28.0 | 383 | 20.0 | 32.00 | <0.001 |
| 100-999 | 1,932 | 55.2 | 817 | 51.7 | 1,115 | 58.1 | ||
| 1,000-9,999 | 545 | 15.6 | 230 | 14.6 | 315 | 16.4 | ||
| >10,000 | 196 | 5.6 | 90 | 5.7 | 106 | 5.5 | ||
| Geographical regions | ||||||||
| Eastern | 844 | 24.1 | 341 | 21.6 | 503 | 26.2 | 46.82 | <0.001 |
| Southern | 124 | 3.5 | 52 | 3.3 | 72 | 3.8 | ||
| Central | 646 | 18.5 | 259 | 16.4 | 387 | 20.2 | ||
| Northern | 758 | 21.7 | 359 | 22.7 | 399 | 20.8 | ||
| Northwest | 733 | 21.0 | 403 | 25.5 | 330 | 17.2 | ||
| Southwest | 270 | 7.7 | 111 | 7.0 | 159 | 8.3 | ||
| Northeast | 123 | 3.5 | 54 | 3.4 | 69 | 3.6 | ||
| Acquaintance with COVID-19 | 143 | 4.1 | 68 | 4.3 | 75 | 3.9 | 0.35 | 0.55 |
| Parents as frontline workers | 312 | 8.9 | 162 | 10.3 | 150 | 7.8 | 6.36 | 0.01 |
| Concern about graduation | 1,955 | 55.9 | 933 | 59.1 | 1022 | 53.3 | 11.95 | 0.01 |
| Concern about COVID-19 | 2,580 | 73.8 | 1,182 | 74.9 | 1,398 | 72.9 | 1.8 | 0.18 |
| Strict mask-wearing and hand hygiene | 3,199 | 91.5 | 1,767 | 92.1 | 1,432 | 90.7 | 2.14 | 0.14 |
| Sleep duration/day | ||||||||
| <6h | 283 | 8.1 | 179 | 11.3 | 104 | 5.4 | 48.07 | <0.001 |
| 6-8h | 2,089 | 59.7 | 946 | 59.9 | 1,143 | 59.6 | ||
| >8h | 1,126 | 32.2 | 454 | 28.8 | 672 | 35.0 | ||
| Exercise duration/day | ||||||||
| <30min | 1,924 | 55.0 | 893 | 56.6 | 1,031 | 53.7 | 4.46 | 0.11 |
| 30-60min | 1,289 | 36.8 | 552 | 35.0 | 737 | 38.4 | ||
| >60min | 285 | 8.1 | 134 | 8.5 | 151 | 7.9 | ||
| Study duration/day | ||||||||
| <4h | 704 | 20.1 | 316 | 20.0 | 388 | 20.2 | 12.54 | 0.006 |
| 4-8h | 1,711 | 48.9 | 731 | 46.3 | 980 | 51.1 | ||
| >8h | 1083 | 31.0 | 532 | 33.7 | 551 | 28.7 | ||
| Participation in distance learning | 3,181 | 90.9 | 1,446 | 91.6 | 1,735 | 90.4 | 1.43 | 0.23 |
| Quantity of homework | ||||||||
| Lower than before | 903 | 25.8 | 376 | 23.8 | 527 | 27.5 | 54.12 | <0.001 |
| About the same | 1,946 | 55.6 | 826 | 52.3 | 1,120 | 58.4 | ||
| Higher than before | 649 | 18.6 | 377 | 23.9 | 272 | 14.2 | ||
| Residence | ||||||||
| Dorm | 33 | 0.9 | 10 | 0.6 | 23 | 1.2 | 2.96 | 0.09 |
| Other | 3,465 | 99.1 | 1,569 | 99.4 | 1,896 | 98.8 | ||
| Scale | Mean | SD | Mean | SD | Mean | SD | T/Z | P |
| CES-D | 25.87 | 8.15 | 29.52 | 8.96 | 22.88 | 5.93 | -26.24 | <0.001 |
| GAD-7 | 4.81 | 4.45 | 8.59 | 3.90 | 1.70 | 1.46 | -51.26a | <0.001 |
a. Mann-Whitney U test; Bolded P-values: <0.05; COVID-19: Coronavirus Disease 2019; CES-D: 20-item Center for Epidemiological Studies-Depression; GAD-7: 7-item Generalized Anxiety Disorder; SD: standard deviation.
Univariate analysis found that the combination of anxiety and depression was significantly associated with gender, age, grade, number of confirmed COVID-19 cases in the participant's province, geographical regions, parents as frontline workers, daily sleep duration, daily study duration, quantity of homework, concern about graduation, CES-D total score, and GAD-7 total score (P<0.001 for all).
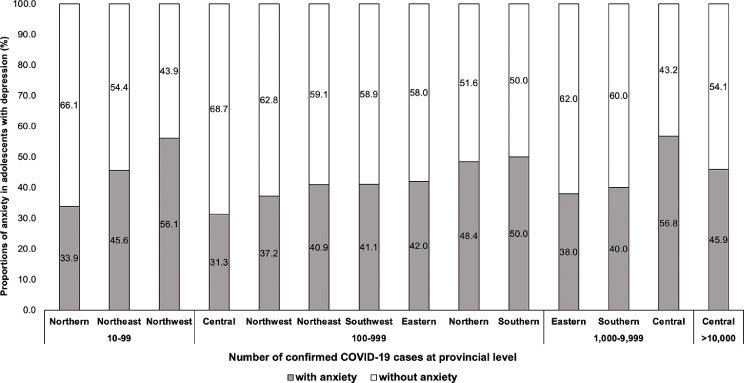
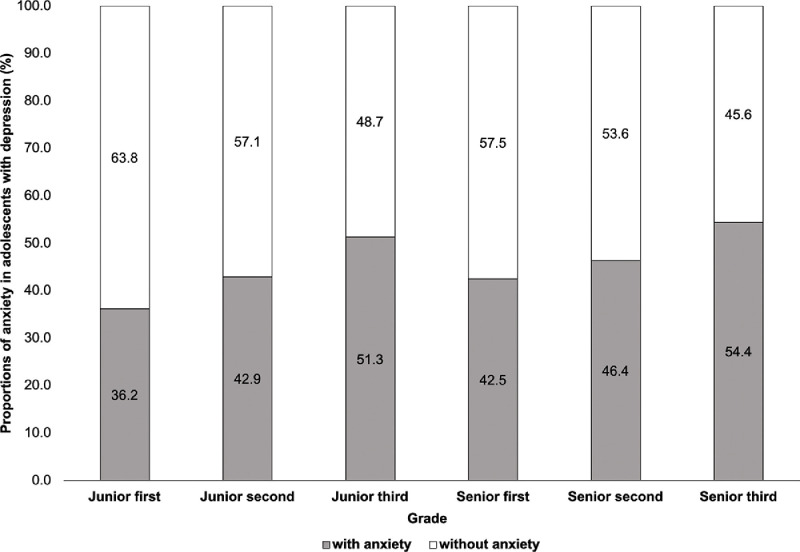
Figure 1 showed the distributions of anxiety in adolescents with depression at the provincial level. For the provinces with 10-99 COVID-19 confirmed cases, the proportions of anxiety were higher in Northwest region (56.1%) than other regions. For the provinces with 100-999 confirmed cases, the proportions were higher in Southern region (50.0%). Furthermore, depressed students who lived in Central region with 1,000-9,999 COVID-19 confirmed cases had the relatively higher proportion of anxiety (56.8%). Figure 2 showed the distributions of anxiety among depressed adolescents in different grades. Depressed adolescents who were in junior (51.3%) and senior (54.4%) third grades presented higher proportions of anxiety than other grades.
Figure 1.
The distributions of anxiety in adolescents with depression at the provincial level during the COVID-19 outbreak. Regions with no anxiety individuals among depressed adolescents were not presented.
Figure 2.
The distributions of anxiety in adolescents with depression at different grades during the COVID-19 outbreak.
Table 2 was the multiple logistic regression analyses among adolescents with depression. The age-adjusted and grade-adjusted models revealed that being female (OR=1.20, P=0.008, 95% CI=1.05-1.38) and studying at the senior secondary school (OR=1.22, P=0.004, 95% CI=1.07-1.40) were positively associated with anxiety symptoms; these associations remained significant after adjusting for COVID-19 and lifestyle-related factors. Being concerned about graduation was positively associated with anxiety symptoms when adjusting for age and grade (OR=1.27, P=0.001, 95% CI=1.11-1.46), and further adjusting for lifestyle factors (OR=1.25, P=0.002, 95% CI=1.09-1.43). The number of confirmed COVID-19 cases at a provincial level of 100-999 and 1,000-9,999 were negatively associated with anxiety symptoms when adjusting for age and grade (OR=0.67, P<0.001, 95% CI=0.56-0.79; OR=0.65, P<0.001, 95% CI=0.52-0.81), and further adjusting for lifestyle factors (OR=0.70, P<0.001, 95% CI=0.59-0.83; OR=0.69, P=0.001, 95% CI=0.55-0.87). Lifestyle factors such as daily sleep duration <6 hours, daily study duration >8 hours, and more homework than before the pandemic were positively associated with anxiety symptoms when adjusting for age and grade (OR=1.91, P<0.001, 95% CI=1.47-2.48; OR=1.19, P=0.03, 95% CI=1.01-1.39; OR=1.72, P<0.001, 95% CI=1.43-2.06), and additionally adjusting for COVID-19 related factors (OR=1.80, P<0.001, 95% CI=1.38-2.34; OR=1.21, P=0.02, 95% CI=1.03-1.42; OR=1.68, P<0.001, 95% CI=1.40-2.02).
Table 2.
Independent correlates of anxiety in adolescents with depression by multivariate logistical regression analysis.
| Variables | P | OR | 95% CI for OR | |
| Lower | Upper | |||
| Model 1 | ||||
| Female | 0.008 | 1.20 | 1.05 | 1.38 |
| Senior secondary school | 0.004 | 1.22 | 1.07 | 1.40 |
| Model 2 | ||||
| Female | 0.01 | 1.20 | 1.04 | 1.38 |
| Senior secondary school | 0.008 | 1.21 | 1.05 | 1.39 |
| Parents as frontline worker | 0.12 | 1.21 | 0.95 | 1.53 |
| Concern about graduation | 0.001 | 1.27 | 1.11 | 1.46 |
| Number of confirmed COVID-19 cases at provincial level | ||||
| 10-99 | – | 1 | – | – |
| 100-999 | <0.001 | 0.67 | 0.56 | 0.79 |
| 1,000-9,999 | <0.001 | 0.65 | 0.52 | 0.81 |
| >10,000 | 0.21 | 0.82 | 0.59 | 1.12 |
| Model 3 | ||||
| Female | 0.006 | 1.21 | 1.06 | 1.39 |
| Senior secondary school | 0.04 | 1.16 | 1.01 | 1.33 |
| Sleep duration/day | ||||
| 6-8h | – | 1 | – | – |
| <6h | <0.001 | 1.91 | 1.47 | 2.48 |
| >8h | 0.05 | 0.86 | 0.74 | 1.00 |
| Study duration/day | ||||
| 4-8h | – | 1 | – | – |
| <4h | 0.79 | 1.03 | 0.85 | 1.23 |
| >8h | 0.03 | 1.19 | 1.01 | 1.39 |
| Quantity of homework | ||||
| About the same | – | 1 | – | – |
| Lower than before | 0.95 | 1.01 | 0.86 | 1.18 |
| Higher than before | <0.001 | 1.72 | 1.43 | 2.06 |
| Model 4 | ||||
| Female | 0.009 | 1.20 | 1.05 | 1.38 |
| Senior secondary school | 0.03 | 1.18 | 1.02 | 1.36 |
| Sleep duration/day | ||||
| 6-8h | – | 1 | – | – |
| <6h | <0.001 | 1.80 | 1.38 | 2.34 |
| >8h | 0.13 | 0.89 | 0.77 | 1.04 |
| Study duration/day | ||||
| 4-8h | – | 1 | – | – |
| <4h | 0.56 | 1.06 | 0.88 | 1.27 |
| >8h | 0.02 | 1.21 | 1.03 | 1.42 |
| Quantity of homework | ||||
| About the same | – | 1 | – | – |
| Lower than before | 0.80 | 1.02 | 0.87 | 1.20 |
| Higher than before | <0.001 | 1.68 | 1.40 | 2.02 |
| Parents as frontline worker | 0.32 | 1.13 | 0.89 | 1.44 |
| Concern about graduation | 0.002 | 1.25 | 1.09 | 1.43 |
| Number of confirmed COVID-19 cases at provincial level | ||||
| 10-99 | – | 1 | – | – |
| 100-999 | <0.001 | 0.70 | 0.59 | 0.83 |
| 1,000-9,999 | 0.001 | 0.69 | 0.55 | 0.87 |
| >10,000 | 0.25 | 0.83 | 0.60 | 1.14 |
Note: Bolded P-values: <0.05; COVID-19: Coronavirus Disease 2019; OR: odds ratio; CI: confidence interval. Multiple logistic regression models with the “enter” method were used. Model 1 was gender-adjusted and grade-adjusted. Model 2 was adjusted for gender, grade, parents as frontline workers, concern about graduation, and residence. Model 3 was adjusted for gender, age, daily sleep duration, daily study duration, and quantity of homework. Model 4 was adjusted for all factors mentioned above. Due to the collinearities, age and geographical regions were not included in the multiple logistic regressions.
4. Discussion
The main focus of this study was to investigate the proportion of anxiety and associated factors in Chinese adolescents with depression during the COVID-19 outbreak. This study found the proportion of anxiety was 45.1% (95% CI = 43.5%-46.8%) among adolescents with depressive symptoms, which was lower than the prevalence of anxiety (55.3%) among depressed middle school students in Changsha (Ma et al., 2013), and 50.1% among Chinese junior secondary students with depressive symptoms (Qu and Zhang, 2018). Apart from different measures on anxiety and depression, sampling methods, and sample size among studies, we speculated some reasons resulted in difference. First, the survey was conducted during the winter holidays, in which the students might have lower levels of academic pressures and mental health symptoms (Wang et al., 2020b). Second, since the outbreak of COVID-19, the government had delivered the knowledge of epidemic through various channels, such as television, internet, and WeChat (Gao et al., 2020), which could help adolescents mitigate their fears and anxiety toward the COVID-19 pandemic.
The study found that adolescents with depression in senior secondary school, especially in third grade were more vulnerable to experience the comorbid of anxiety and depression. Of note, senior secondary students face tremendous academic pressures while preparing for the college entrance examination, which is considered to be of great importance for Chinese students (Li et al., 2008; Liu and Lu, 2011; Tang et al., 2019). The COVID-19 pandemic disrupted their stressful study regimen and decreased their interactions with teachers and classmates (Lee, 2020; Zhou et al., 2020), which could increase the risks of anxiety and pressure. Moreover, the adolescents with depression tend to be more anxious than the adolescents without depression when faced the stressful events (Garber and Weersing, 2010).
Additionally, sleep less than 6 hours/day, study more than 8 hours/day, and higher quantity of homework were positively associated with anxiety among adolescents with depression. Long hours of studying might indicate heavy burdens of homework and insufficient sleep, which had negative impacts on the mental health of students and parent-adolescent relationships (Boers et al., 2019; Brown et al., 2018; Liu et al., 2020b; Liu et al., 2019; McMakin and Alfano, 2015; Stiglic and Viner, 2019; Sun et al., 2012). In line with previous study (Zhou et al., 2020), female adolescents were more likely to have anxiety and depressive symptoms. The gender differences would be explained by the higher levels of fears, shyness and co-rumination of girls (Olino et al., 2013).
Interestingly, we found that provinces with higher numbers of confirmed COVID-19 cases were negatively associated with anxiety symptoms in adolescents with depression. We inferred that the provinces with more confirmed cases had imposed stricter lockdown measures to control the spread of infection, provided more timely mental health services, and popularized more knowledge about COVID-19, which could reduce anxiety in adolescents (Xiang et al., 2020; Zhong et al., 2020). Meanwhile, the study revealed that the depressed students who lived in Northwest areas showed higher proportions of anxiety, which was consistent with a cross-sectional study that the anxiety levels of adolescents were highest in Qinghai (Northwest) than other provinces (Liu et al., 2018). The regional differences of mental health problems might be associated with the inequality of socioeconomic status among regions (Pedrosa et al., 2020; McLaughlin et al., 2012), the adolescents from poorer regions and families tended to have higher levels of anxiety (Najman et al., 2010). Our results could be useful on designing targeted policies across areas and vulnerable populations to reduce anxiety in Chinese adolescents with depression.
Several limitations should be noted in this study. First, this is an online study, those with no access to the internet could not participate in the study. However, during the COVID-19 outbreak, remote learning was adopted nationwide, and few adolescents did not have internet access. Second, some data pertaining to important factors associated with depression, such as physical health and social support, were not available due to logistical reasons. Third, this study only used self-report scales to estimate the symptoms of depressive and anxiety, which may lead to an underestimation of the proportions of anxiety in adolescents with depression. Clinical diagnostic instruments should be utilized in future studies. Fourth, this study found some variables (i.e. concern about school, grades, and sleep) were related to the anxiety, however, they also might be a consequence of anxiety in adolescents with depression. The bi-directional relationships between the variables and symptoms of anxiety/depression should be explored in the future. Fifth, due to the cross-sectional study design, causality between variables and anxiety could not be examined, such as the reverse causality between sleep and anxiety among depressed adolescents. Ideally, a longitudinal study should be performed to examine the changes in proportions of anxiety and its associated factors during the course of the COVID-19 pandemic. Finally, the number of participants varied a lot among different provinces, so the findings could not be generalized to the country.
In conclusion, the symptoms of anxiety were common in adolescents with depression during the COVID-19. These findings suggested the female and higher-grade students were vulnerable to anxiety, indicating the positive academic stress and routine behaviors would be beneficial to the mental health of the adolescents during the COVID-19 outbreak. The government, schools and parents could adopt several measures to create a friendly and positive environment to increase peer support, decrease the academic stress, and establish routines and schedules for consistency and a sense of normalcy.
Contributors
Study design: Xu Chen, Han Qi, Gang Wang.
Data collection, analysis and interpretation: Xu Chen, Han Qi, Rui Liu.
Drafting of the manuscript: Rui Liu, Xu Chen, Han Qi.
Critical revision of the manuscript: Rui Liu, Xu Chen, Han Qi, Christine Pao, Yuan Feng, Le Xiao.
Approval of the final version for publication: all co-authors.
Role of funding
The study was supported by the National Key R&D Program of China (2017YFC1311100); the National Science and Technology Major Project for investigational new drug (2018ZX09201-014); the Beijing Municipal Science & Technology Commission (Z181100001518005, D171100007017001); the National Natural Science Foundation of China (81901368).
Declaration of Competing Intrests
The authors have no conflicts of interest to declare.
Acknowledgements
We wish to thank all the participants in this study.
References
- Angold A., Costello E.J., Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Axelson D.A., Birmaher B. Relation between anxiety and depressive disorders in childhood and adolescence. Depression and anxiety. 2001;14:67–78. doi: 10.1002/da.1048. [DOI] [PubMed] [Google Scholar]
- Boers E., Afzali M.H., Newton N., Conrod P. Association of Screen Time and Depression in Adolescence. JAMA Pediatrics. 2019;173:853–859. doi: 10.1001/jamapediatrics.2019.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown W.J., Wilkerson A.K., Boyd S.J., Dewey D., Mesa F., Bunnell B.E. A review of sleep disturbance in children and adolescents with anxiety. J Sleep Res. 2018;27:e12635. doi: 10.1111/jsr.12635. [DOI] [PubMed] [Google Scholar]
- Chavira D.A., Stein M.B., Bailey K., Stein M.T. Comorbidity of generalized social anxiety disorder and depression in a pediatric primary care sample. J Affect Disord. 2004;80:163–171. doi: 10.1016/S0165-0327(03)00103-4. [DOI] [PubMed] [Google Scholar]
- China's Ministry of Education, 2020. MOE postpones start of 2020 spring semester. http://en.moe.gov.cn/news/press_releases/202001/t20200130_417069.html (access January 29 2020).
- Costello E.J., Mustillo S., Erkanli A., Keeler G., Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cummings C.M., Caporino N.E., Kendall P.C. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014;140:816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. Journal of Affective Disorders. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Zoghby S.M., Soltan E.M., Salama H.M. Impact of the COVID-19 Pandemic on Mental Health and Social Support among Adult Egyptians. J Community Health. 2020;45:689–695. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang C.L., Liu H.M., Luo K., Yu X.H. Comprehensive regionalization of human geography in China (in Chinese) Acta Geographica Sinica. 2017;72:179–196. [Google Scholar]
- Gao H., Hu R., Yin L., Yuan X., Tang H., Luo L., Chen M., Huang D., Wang Y., Yu A., Jiang Z. Knowledge, attitudes and practices of the Chinese public with respect to coronavirus disease (COVID-19): an online cross-sectional survey. BMC Public Health. 2020;20:1816. doi: 10.1186/s12889-020-09961-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J., Weersing V.R. Comorbidity of Anxiety and Depression in Youth: Implications for Treatment and Prevention. Clin Psychol. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. New York. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA pediatrics. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Sampson N.A., Berglund P., Gruber M., Al-Hamzawi A., Andrade L., Bunting B., Demyttenaere K., Florescu S., De Girolamo G. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiology and psychiatric sciences. 2015;24:210–226. doi: 10.1017/S2045796015000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Ang R.P., Lee J. Anxieties in Mainland Chinese and Singapore Chinese adolescents in comparison with the American norm. Journal of Adolescence. 2008;31:583–594. doi: 10.1016/j.adolescence.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Liu Y., Lu Z. The Chinese high school student’s stress in the school and academic achievement. Educational Psychology. 2011;31:27–35. [Google Scholar]
- Liu Y., Zhang W.B., Cai J. Relation of anxiety and depression to lifestyle in junior high school students (in Chinese) Chinese Mental Health Journal. 2017;31:235–240. [Google Scholar]
- Liu H., Shi Y., Auden E., Rozelle S. Anxiety in Rural Chinese Children and Adolescents: Comparisons across Provinces and among Subgroups. Int J Environ Res Public Health. 2018;15:2087. doi: 10.3390/ijerph15102087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Wang N., Tian L. The Parent-Adolescent Relationship and Risk-Taking Behaviors Among Chinese Adolescents: The Moderating Role of Self-Control. Front Psychol. 2019;10:542. doi: 10.3389/fpsyg.2019.00542. 542-542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Luo W.T., Li Y., Li C.N., Hong Z.S., Chen H.L., Xiao F., Xia J.Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infectious Diseases of Poverty. 2020;9:58. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B.P., Wang X.T., Liu Z.Z., Wang Z.Y., An D., Wei Y.X., Jia C.X., Liu X. Depressive symptoms are associated with short and long sleep duration: A longitudinal study of Chinese adolescents. Journal of Affective Disorders. 2020;263:267–273. doi: 10.1016/j.jad.2019.11.113. [DOI] [PubMed] [Google Scholar]
- Ma J., Su L.Y., Yu S.Y., Liang S., Ding J., Feng Z., Yang F., Gao W., Lin J., Huang C., Liu X., Su L. An Anxious and Non-anxious Survey among Depressive Middle School Students in Changsha (in Chinese) Chinese Journal of Clinical Psychology. 2013;21:708–712. [Google Scholar]
- McLaughlin K.A., Costello E.J., Leblanc W., Sampson N.A., Kessler R.C. Socioeconomic status and adolescent mental disorders. Am J Public Health. 2012;102:1742–1750. doi: 10.2105/AJPH.2011.300477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin D.L., Alfano C.A. Sleep and anxiety in late childhood and early adolescence. Curr Opin Psychiatry. 2015;28:483–489. doi: 10.1097/YCO.0000000000000204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton T.H., Croarkin P.E., Strawn J.R., Mcclintock S.M. Comorbid anxiety and depressive symptoms in children and adolescents: a systematic review and analysis. Journal of psychiatric practice. 2016;22:84. doi: 10.1097/PRA.0000000000000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najman J.M., Hayatbakhsh M.R., Clavarino A., Bor W., O'Callaghan M.J., Williams G.M. Family poverty over the early life course and recurrent adolescent and young adult anxiety and depression: a longitudinal study. Am J Public Health. 2010;100:1719–1723. doi: 10.2105/AJPH.2009.180943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino T.M., Durbin C.E., Klein D.N., Hayden E.P., Dyson M.W. Gender differences in young children's temperament traits: comparisons across observational and parent-report methods. J Pers. 2013;81:119–129. doi: 10.1111/jopy.12000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrosa A.L., Bitencourt L., Froes A.C.F., Cazumba M.L.B., Campos R.G.B., de Brito S., Simoes E.S.A.C. Emotional, Behavioral, and Psychological Impact of the COVID-19 Pandemic. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.566212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Liu R., Chen X., Yuan X.F., Li Y.Q., Huang H.H., Zheng Y., Wang G. Prevalence of anxiety and associated factors for Chinese adolescents during the COVID-19 outbreak. Psychiatry Clin Neurosci. 2020;74:555–557. doi: 10.1111/pcn.13102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu M., Zhang C. Study on comorbid anxiety and deprssion of 1335 junior high school students in Kuitun City of Xinjiang (in Chinese) Chin J School Doctor. 2018:666–668. [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977:385–401. [Google Scholar]
- Radloff L.S. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of youth and adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Reuben R.C., Danladi M.M.A., Saleh D.A., Ejembi P.E. Knowledge, Attitudes and Practices Towards COVID-19: An Epidemiological Survey in North-Central Nigeria. J Community Health. 2020;7:1–14. doi: 10.1007/s10900-020-00881-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stiglic N., Viner R.M. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ open. 2019;9 doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun J., Dunne M.P., Hou X.Y. Academic stress among adolescents in China. Australasian Epidemiologist. 2012;19:9–12. [Google Scholar]
- Sun X.Y., Li Y.X., Yu C.Q., Li L.M. Reliability and validity of depression scales of Chinese version: a systematic review (in Chinese) Chinese Journal of Epidemiology. 2017;38:110–116. doi: 10.3760/cma.j.issn.0254-6450.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Tang X., Tang S., Ren Z., Wong D. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: A systematic review and meta-analysis. Journal of Affective Disorders. 2019;245:498–507. doi: 10.1016/j.jad.2018.11.043. [DOI] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z.H., Yang H.L., Yang Y.Q., Liu D., Li Z.H., Zhang X.R., Zhang Y.J., Shen D., Chen P.L., Song W.Q., Wang X.M., Wu X.B., Yang X.F., Mao C. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. J Affect Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) 2020 https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (access January 20 2020) [Google Scholar]
- World Health Organization, 2020b. Coronavirus disease 2019 (COVID-19) Situation. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200229-sitrep-40-covid-19.pdf?sfvrsn=849d0665_2 (access February 29 2020).
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatrics. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., Ding N., Song S., Liu Y., Wen D. Association between depression and overweight in Chinese adolescents: a cross-sectional study. BMJ open. 2019;9 doi: 10.1136/bmjopen-2018-024177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong B.L., Luo W., Li H.M., Zhang Q.Q., Liu X.G., Li W.T., Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16:1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]