Abstract
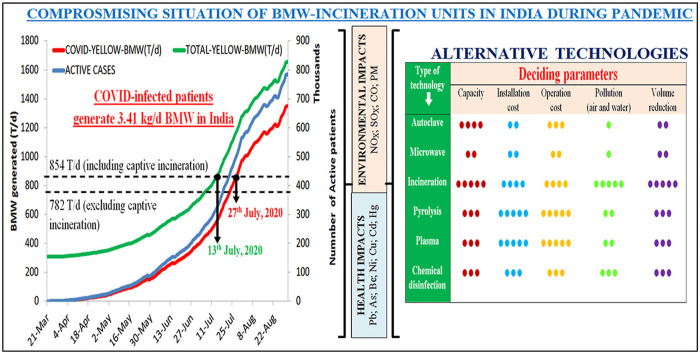
COVID-19 induced pandemic situations have put the bio-medical waste (BMW) management system, of the world, to test. Sudden influx, of COVID-infected patients, in health-care facilities, has increased the generation of yellow category BMW (Y-BMW) and put substantial burden on the BMW-incineration units of India. This study presents the compromising situation of the BMW-incineration units of India, in the wake of COVID-19 pandemic, from 21st March 2020 to 31st August 2020. This analysis revealed that on an average each COVID-infected patient in India generates approximately 3.41 kg/d of BMW and average proportion of Y-BMW in it is 50.44%. Further, it was observed that on 13th July 2020, the total Y-BMW, generated by both the normal and COVID-infected patients, fully utilized the BMW-incineration capacity of India. Also, it was made evident that, during the study period, BMW-incineration emitted several pollutants and their concentration was in the order: NOx > CO > SOx > PM > HCl > Cd > Pb > Hg > PCBs > Ni > Cr > Be > As. Subsequently, life time cancer risk assessment depicted that with hazard quotient >10−6, Cd may induce carcinogenic health impacts on both the adults and children of India. Therefore, to mitigate the environmental-health impacts associated with the incineration of BMW, evaluation of various options, viz., alternative technologies, substitution of raw materials and separate treatment of specific wastes, was also done. It is expected that the findings of this study may encourage the global auditory comprising scientific community and authorities to adopt alternate BMW-management strategies during the pandemic.
Keywords: COVID-19, Bio-medical waste, Incineration, Health risk assessment, Alternative technology, Heavy metals
Graphical abstract
Generation of yellow-BMW in India, during pandemic, was estimated to assess the compromising capacity of its incineration units and associated environmental-human health impacts.
Credit author statement
Parteek Singh Thind: Conceptualization, statistical Formal analysis, Writing – original draft. Arjun Sareen: Data compilation and data analysis, Writing – review & editing Dapinder Deep Singh: Writing – review & editing. Sandeep Singh: Writing – review & editing. Siby John:Visualization, Writing – review & editing.
1. Introduction
On 11th March 2020, World Health Organization (WHO) declared the outbreak of COVID-19, as a pandemic and since then there was a substantial global-burden on management of health care system. This pandemic has inflated the health care facilities with a large number of infected patients. Consequently, global health-care system demanded special provisions such as, setting up of quarantine camps, isolation buildings, research facilities, increased production of personal protective equipment (PPE) kits, chemicals, reagents and medicines etc. Moreover, perception of hygienic-superiority of PPE kits, among the domestic population, has also added to their demand. Same can also be inferred from the fact that, from 2016 to 2020, the production of PPE kits has increased only by 6.5%, however, during pandemic, WHO has indicated a monthly increase of 40% in the production of PPE kits (Market Reports, 2019; WHO, 2020).
An unprecedented demand, of the PPE kits and other single-use medical-care equipment, to counter the highly infectious nature of COVID-19, has led to an enormous generation of yellow category of biomedical waste (Y-BMW) (Ogunseitan, 2020). It is anticipated that, during pandemic period, per capita daily disposal of a single-use face mask, may generate 66 kT of Y-BMW within a year (Allison et al., 2020). Such a sudden increase in the amount of Y-BMW, during the pandemic outbreak of COVID-19, has disturbed even the most reputed waste management systems of the world (European Commission, 2020). In Wuhan, China, during peak of the pandemic, the generation of Y-BMW increased by 6 folds i.e., 240 tons per day. Consequently, regional authorities of China decided to implement other waste management strategies (SCMP 2020). It has also been estimated that, due to COVID-19 infections, the waste generation in USA will increase from 5 MT/y to 300 MT/y. Therefore, authorities of US may also have to take substantial efforts to manage such a huge amount of medical waste (Reuters, 2020).
In developing countries, even before outbreak of COVID-19, management of Y-BMW was under stress. Situation induced by pandemic outbreak of COVID-19 may further deteriorate their waste management system. It is reported that from 20th January 2020 to 30th May 2020, approximately, 2000 T of Y-BMW was generated in Republic of South Korea (ESCAP (United Nation Economic and Social Commission for Asia and the Pacific), 2020). Although, India’s health care sector is expanding at 15% CAGR, yet only 28% of its hospitals segregate the BMW properly and 40% of its Y-BMW is not being treated as per the regional guidelines (MoEFCC, 2016; WHO, 2019; Ilyas et al., 2020). The increase in generation of Y-BMW also calls for an equivalent increase in environmental risks, especially, in the developing nations where incineration is the most preferable way of treating the Y-BMW (Datta et al., 2020). During incineration several health-deteriorating pollutants are emitted, which have the potential to transport to long distances (Mallapur, 2020). Recently, studies have also derived the relationship between air pollution and increased susceptibility to COVID-19 infection (Zhu et al., 2020; Gupta et al., 2020; Comunian et al., 2020; Li et al., 2020). Therefore, it is advised that while addressing the infected patients and stressing on medical research, the issue of waste management should not be neglected. Otherwise, all the efforts, taken by the global community, to sustain the environmental conditions, may nullify (Shaha et al., 2019; Cutler, 2020). Moreover, with the announcement of the pandemic situation the number of scientific publications on reduced air pollution has increased dramatically, around the world. However, studies reporting the increased emissions of the toxic pollutants from incineration of Y-BMW are scanty. Therefore, during the current pandemic-crisis, studies, highlighting an association between the enhanced emissions, due to incineration of Y-BMW, and the human health, are required.
This study intends to bring forward the compromising situation of India’s BMW-incineration capacity, during pandemic outbreak of COVID-19 with specific reference to associated emissions and health impacts. Efforts were also made to compare the generation of Y-BMW in India, during the pandemic situation, with the installed capacity of its Common Biomedical Waste Treatment Facilities (CBWTFs). In this way, estimation of the time, during which the present incineration-capacity of India will be compromised, is done. This study also highlights the carcinogenic and non-carcinogenic health impacts associated with the emission of harmful substances during incineration of Y-BMW. Further, emphasis is also given on recommending the strategies which should be adopted in order to handle the deteriorating situation of current BMW management system. The studies, which could comprehensively address the issue of BMW management in India and associated environmental-health impacts, are scanty. Hence, this study may prove beneficial in building an appropriate framework for efficient management of the BMW during the pandemic outbreak of COVID-19.
2. Study area
Starting from 22nd March 2020, in order to control the spread of COVID-19 infections, the authorities of India initially imposed nation-wide lockdown for 21 days. Since after, several consecutive relaxations were given in the lockdown and consequently, the number of COVID-19 infected patients was also reported to increase (Somani et al., 2020). BMW generated, during this period, inflated the CBWTFs of India. In India, BMW is managed as per BMW legislation, 2016 and according to this legislation, there are four categories of the BMW i.e., red, yellow, white and blue (MoEFCC, 2016). Among these categories of BMW, yellow BMW (Y-BMW) is treated using incinerators. As per latest report of Central Pollution Control Board (CPCB), India, there are 198 CBWTFs with installed incineration capacity of 782 T/d, with additional capacity of 72 T/d from captive incineration (CPCB, 2020). Till 31st May 2020 these CBWTFs were managing 710 T/d of the BMW out of which 101 T/d is generated from COVID-infected patients. Therefore, it was presumed that, with the increasing number of patients, incineration-capacity of the CBWTFs of India may soon get compromised. The number of CBWTFs in each state of India and their respective incineration-capacity is described in Supplementary Table S1.
3. Materials and methods
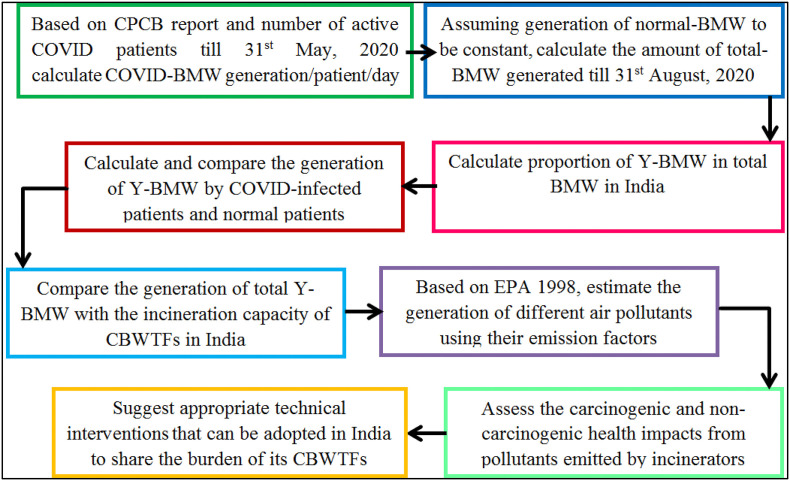
A brief methodology adopted for conducting the present study is described in Fig. 1 .
Fig. 1.
Brief lay-out of the methodology adopted in present study.
The step-wise explanation of the methodology, depicted in Fig. 1, is as following:
3.1. Estimating the generation of total BMW (T-BMW)
Methodology, adopted in the present study, used the following information from the two datasets i.e., the CPCB report (CPCB, 2020) and https://www.worldometer.com.
-
a.
Incineration capacity of the CBWTFs in India (as shown in Supplementary Table S1)
-
b.
Amount of COVID-BMW (C-BMW) generated in India till 31st May
-
c.
Amount of normal-BMW (N-BMW) generated in India till 31st May.
-
d.
Day-to-day data on the number of COVID-infected patients
To estimate the amount of generation of C-BMW per patient per day, data on C-BMW generation and the number of COVID-infected patients from March 21, 2020 to May 31, 2020, was used (as shown in Supplementary Table S1). Further, it was assumed that till 31st August 2020 the amount of generation of C-BMW (kg/patient/d) would remain constant. Subsequently, the amount of C-BMW generated till 31st August 2020 was calculated. Assuming that the generation of N-BMW will remain constant after 31st May 2020, N-BMW was added with C-BMW to calculate the total-BMW (T-BMW). The findings of this estimation are in line with the predictions made in a joint report of Associated Chambers of Commerce and Industry of India (ASSOCHAM) and Velocity (ASSOCHAM India, 2018).
3.2. Estimating the proportion of Y-BMW in T-BMW
To calculate the proportion of Y-BMW in T-BMW for India, CPCB annual reports of seven states of India were accessed and analyzed. In this way, the proportion Y-BMW in each of these states was estimated and its average was used as a representative for whole nation. The findings, of this analysis, were further used to calculate the daily generation of total Y-BMW (T-Y-BMW), including both the COVID Y-BMW (C–Y-BMW) and normal Y-BMW (N–Y-BMW), from 21st March 2020 to 31st August 2020 in India. Further, to estimate the compromising situation of the incineration capacity of India, the amount of generation of T-Y-BMW was compared with the net incineration capacity of the CBWTFs in India.
3.3. Estimating the emissions from incineration of T-Y-BMW
Incineration of T-Y-BMW emitted several pollutants into the atmosphere of India, during the study period. The amount of these pollutants was estimated using their specific emission factors which were adopted from EPA (1995). The net amount of pollutants emitted during this time duration was assumed to stay over India for the given study period. Further, considering the mixing depth of pollutants to be 1000 m (Devara et al., 2002), the concentration of these pollutants (in mg/m3) was calculated.
3.4. Assessing the health risks associated with emissions from BMW-incineration
Incineration of Y-BMW may emit several toxic pollutants such as, heavy metals, gases and other xenobiotic compounds (Gupta et al., 2020; Comunian et al., 2020; Li et al., 2020). On inhalation, these pollutants may pose carcinogenic and non-carcinogenic health impacts on human body. Therefore, in present study, efforts were also made to assess the non-carcinogenic and carcinogenic health impacts associated with exposure of humans to the pollutants emitted during incineration of T-Y-BMW. Life time cancer risk, associated with inhalation of such pollutants, was calculated using Eq. (1) and Eq. (2). Further, Eq. (3) was used to calculate the Hazard Index (HI) as a representing parameter for non-carcinogenic health risks assessment.
| (1) |
| (2) |
| (3) |
Where, Intake(inhalation) defines the average amount of toxic pollutants being inhaled daily per unit weight (mg/kg/d); C is the concentration of the pollutants emitted by the incinerators (mg/m3); IR represents the amount of air inhaled by adults and children, of India, in a day. EF and ED stands for exposure frequency and exposure duration, respectively. BW and AT represent the average body weights and time required for carcinogenic impacts, respectively. A brief description of all these parameters is also given in Table 1 .
Table 1.
Description of exposure parameters of ingestion and inhalation (Department of Environmental Affairs (DoEA), 2010)
| Denotations | Exposure Parameter (units) | Standard values | References |
|---|---|---|---|
| C | Concentration (inhalation: μg/m3) | – | – |
| BW | Body Weight (kg) | Adult = 70; Children = 15 | Miguel et al. (2007) |
| EF | Exposure Frequency (d/y) | 350 (for both adults and children) | U.S. Environmental Protection Agency and U.S. EPA (1998) |
| ED | Exposure Duration (y) | Adult = 30; Children = 6 | United Nations Environment Protection (UNEP) (2005) |
| LT | Life Time (y) | 70 (for both adults and children) | U.S. Department of Energy (USDoE) (2011) |
| AT | Average exposure Time (y) | For Non-carcinogenic: ED ∗ 365; For carcinogenic: LT ∗ 365 |
U.S. Environmental Protection Agency and U.S. EPA (1998) |
| IRj | Rate of inhalation (/d) | 20 for adults and 10 for children | MoHFW (2010); Van den Berg (1995); Shihabudeen et al. (2004) |
After calculating the Intake(inhalation), the life time cancer risk was calculated by multiplying the Intake(inhalation) with the respective cancer slope factors (CSFs) of different pollutants. Similarly, HI was calculated by dividing the Intake(inhalation) with the reference dose (RfD) of the different pollutants. The pollutants selected for this analysis were poly-chlorinated biphenyls (PCBs), Arsenic (Ar), Berrylium (Bl), Cadmium (Cd), Chromium (Cr), lead (Pb) and mercury (Hg) and Nickel (Ni). The values of CSFs ((mg/kg/d)−1) and RfDs (mg/kg/d) for these pollutants were acquired from USEPA (2004) and are mentioned in Table 2 .
Table 2.
Reference doses and slope factors of the pollutantsa.
| S.No. | Pollutants | Reference Dose (mg/kg/d) | Slope Factor (mg/kg/d)−1 |
|---|---|---|---|
| 1 | PCBs | – | 2 |
| 2 | As | 3.00E-04 | 15.1 |
| 3 | Be | – | 8.4 |
| 4 | Cd | 5.70E-05 | 6.3 |
| 5 | Cr6+ | 3.00E-05 | 41 |
| 6 | Ni | 2.50E-02 | 0.84 |
| 7 | Pb | 3.50E-03 | 0.042 |
| 8 | Hg0 | 8.60E-05 | – |
Acquired from US EPA region III (2007); http://www.epa.gov/reg3hwmd/risk/human/index.htm.
4. Results and discussion
4.1. Proportion of Y-BMW in T-BMW of India
The seven states of India chosen for estimating the proportion of Y-BMW in T-BMW of India were Delhi, Haryana, Rajasthan, Madhya Pradesh, Maharashtra, Mizoram and Uttrakhand. These states were chosen on the basis of the availability of annual reports. The amount of Y-BMW generated in each of these states was evaluated from their respective annual reports. These annual reports are submitted annually by their respective state pollution control boards, to the CPCB, India and are available online. The details of the proportion of Y-BMW in each state are mentioned in Table 3 .
Table 3.
Proportion of Y-BMW in India.
| S.No. | State name | Proportion of Y-BMW (%) |
|---|---|---|
| 1 | Mizoram | 34.5 |
| 2 | Delhi | 47 |
| 3 | Maharashtra | 44 |
| 4 | Uttrakhand | 44.97 |
| 5 | Haryana | 69.5 |
| 6 | Madhya Pradesh | 69.05 |
| 7 | Rajasthan | 44.09 |
| Average | 50.44 |
From Table 3, it is evident that the proportion of Y-BMW in T-BMW of India ranges from 34.5% to 69.5% and its average is 50.44%. Therefore, for further investigations, 50.44% was considered as an average proportion of Y-BMW in India. It can also be depicted that the composition of BMW in India is highly variable and it depends on several regional-level and national-level factors. The various factors affecting the composition of BMW are, availability of the CBWTFs, different facilities provided by the CBWTFs, ideology of local administration, central and state-level legislations, knowledge, attitude and practice of the health care workers etc (Askarian et al., 2004; Bdour et al., 2007; Mohee, 2005; Shinee et al., 2008; Shaner and McRae, 2002). Several studies have also pointed that the generation of the amount and type of the BMW is also dependent on various parameters of the health care facilities (HCFs) such as, use of reusable items, number of patients treated every day, number of different departments, kind of departments, availability of insurance-based reimbursement facility, location etc. (Almuneef and Memish, 2003; Tudor et al., 2005; Cheng et al., 2010; Alvim-Ferraz and Afonso, 2005; Oweis et al., 2005; Marinkovic et al., 2008; Prüss et al., 1999).
4.2. Generation of different types of BMW in India during pandemic
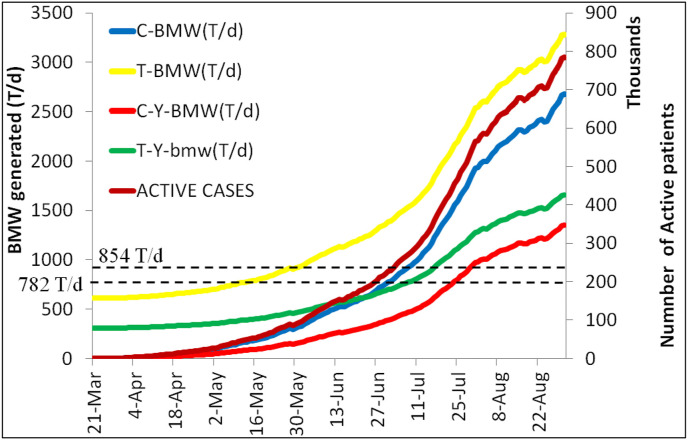
On analyzing the number of COVID-infected patients from March 21, 2020 to May 31, 2020, it was observed that ∼2.1 million citizens of India were infected with COVID-19. It was also estimated that each COVID-infected patient in India generates about 3.41 kg/d of COVID-BMW (C-BMW), which is almost double than the BMW generated during normal days (Manasi, 2017; Ranjan et al., 2016). This information was further used to estimate the generation of different types of BMW during the pandemic outbreak of COVID-19 and its findings are shown in Fig. 2 .
Fig. 2.
Daily generation of different types of BMW in India during pandemic.
In Fig. 2, two horizontal dotted-lines depicted the incineration capacity of India’s CBWTFs including captive incineration (854 T/d) and excluding captive incineration (782 T/d). It can be seen that after May 31, 2020, the number of COVID-infected patients rose exponentially which can be attributed to the substantial relaxations in the nation-wide lockdown. Under such circumstances, the generation of T-Y-BMW also increased and by 13th July 2020 and 10th July 2020, it was observed that the incineration capacity, of India’s CBWTFs, while including captive incineration and excluding captive incineration, respectively, was fully utilized. Moreover, with further spread in COVID-infection, more and more Indian citizens got infected. Subsequently, the amount of C–Y-BMW alone was able to cross India’s Y-BMW incineration capacity on 27th July 2020. It can also be observed that, under pandemic conditions, the rate of generation of C–Y-BMW remained constant till 31st August 2020. On 31st August 2020 it can be seen that generation of T-Y-BMW and C–Y-BMW was 1657 T/d and 1350 T/d, respectively. Under such circumstances, inefficient management of BMW and over-use of incineration units can also be speculated. In this way, uncontrolled spread of COVID-19 infection and other associated environmental-health impacts were also expected. Hence, in this study, efforts were also made to estimate the contribution of the incineration units of India in regional air pollution. This analysis may assist in comprehensively understanding the need of efficient BMW-management during the pandemic situation.
4.3. Emissions from CBWTFs of India during pandemic
The incineration of T-Y-BMW during 21st March 2020 to 31st August 2020, emitted several pollutants into the atmosphere of India. The net amount of pollutants generated during this treatment of T-Y-BMW, is mentioned in Table 4 .
Table 4.
Emission of pollutants during incineration of T-Y-BMW in India.
| S.No. | Pollutants | Emission factors (kg/T) | Emissions on incineration (mg/m3/d) |
|
|---|---|---|---|---|
| C–Y-BMW | T-Y-BMW | |||
| 1 | NOx | 1.78 | 3.63E-05 | 6.36E-05 |
| 2 | CO | 1.48 | 3.02E-05 | 5.29E-05 |
| 3 | SOx | 1.04 | 2.12E-05 | 3.71E-05 |
| 4 | PM | 0.74 | 1.51E-05 | 2.65E-05 |
| 5 | HCl | 0.07 | 1.42E-06 | 2.49E-06 |
| 6 | PCB | 0.02 | 4.75E-08 | 8.32E-08 |
| 7 | Be | 0.003 | 6.36E-09 | 1.11E-08 |
| 8 | Cr | 0.0005 | 1.05E-08 | 1.84E-08 |
| 9 | Ni | 0.001 | 2.59E-08 | 4.54E-08 |
| 10 | As | 0.0002 | 3.34E-10 | 5.86E-10 |
| 11 | Cd | 0.03 | 7.58E-07 | 1.33E-06 |
| 12 | Pb | 0.04 | 7.12E-07 | 1.25E-06 |
| 13 | Hg | 0.09 | 1.76E-07 | 3.09E-07 |
From Table 4, it is evident that incineration of T-Y-BMW during pandemic has added a significant amount of gases, heavy metals and PCBs into India’s atmosphere. The order in which pollutants were emitted during the incineration of T-Y-BMW was observed to be NOx > CO > SOx > PM > HCl > Cd > Pb > Hg > PCBs > Ni > Cr > Be > As. Several studies have estimated the environmental-health impacts associated with these pollutants and their brief description is given in Table 5 .
Table 5.
Environmental and health impacts associated with emissions from BMW-incineration.
| S.No. | Environmental impacts | Causative pollutant(s) | Reference(s) |
|---|---|---|---|
| 1 | Global warming | CO2 | Sharma et al. (2013) |
| 2 | Acidification and damage to monuments | H2SO4 and HNO3 | Sharma et al. (2013) |
| 3 | Water and soil pollution | Cl, Pb, Cu and Zn | Sharma et al. (2013) |
| 4 | Smog formation | SO2 and NO2 | Sharma et al. (2013) |
| Health Impacts | |||
| 5 | Different types of malignancy viz., skin cancer, lung cancer, brain cancer, breast cancer, kidney cancer, prostate cancer, soft-tissue sarcoma, Non-Hodgkin lymphoma | Cd, PCBs | McGregor et al. (1998); Elliot et al. (2000); Viel et al. (2000); Biggeri et al. (1996); Diggle (1990); Knox (2000) |
| 6 | Decreased proportion of male births | PCBs | Mocarelli et al. (2000) |
| 7 | Respiratory issues | PM, CO, SO2 and NO2 | Ayres (1998); Wang et al. (1992); Zmirou et al. (1984) |
| 8 | Hormonal imbalance | PM and PCB | Osius and Karmaus (1998); Osius et al. (1999) |
| 9 | Congenital abnormality | PM and heavy metals | Ten et al. (2000); Lloyd et al. (1988) |
As mentioned in Table 5, PM, CO, SO2 and NO2 can significantly impact the respiratory organ system of the humans. Also, respiratory organs are major target of COVID-19 and hence, exposure of humans to such pollutants may make them prone to have COVID-induced respiratory damage. Several studies, around the world, have proven a significant correlation between the increased ambient concentrations of the air pollutants such as, PM, CO, SO2 and NO2, and surging rate of COVID-19-induced-mortality (Zhu et al., 2020; Gupta et al., 2020; Comunian et al., 2020; Li et al., 2020). Hence, with upcoming events of stubble burning in North-India i.e., during the months of September and October, and exponentially growing emissions from incineration of Y-BMW, the possibility of reduced tolerance of Indian citizens, to COVID-19, is speculated. Table 4, Table 5 also showed that several heavy metals such as, Pb, Zn, Cd, Cu, Ni and As, are emitted during incineration of Y-BMW, which can cause various carcinogenic and non-carcinogenic health impacts. Therefore, in order to discourage the over-dependence of India on BMW-incineration, it is imperative to assess the associated carcinogenic and non-carcinogenic health risks.
4.4. Health risk assessment
The carcinogenic and non-carcinogenic health risks, associated with the exposure of adults and children of India to different pollutants, emitted during incineration of T-Y-BMW, are described in Table 6 .
Table 6.
Non-carcinogenic and carcinogenic health risk assessment.
| S.No. |
Pollutants |
Non-carcinogenic risk assessment |
Carcinogenic risk assessment |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard index | Riskcarcinogenic | ||||||||
| C–Y-BMW | T-Y-BMW | C–Y-BMW | T-Y-BMW | C–Y-BMW | T-Y-BMW | C–Y-BMW | T-Y-BMW | ||
| Adults | Adults | Children | Children | Adults | Adults | Children | Children | ||
| 1 | PCB | – | – | – | – | 1.33E-08 | 2.33E-08 | 7.60E-08 | 1.33E-07 |
| 2 | Be | 1.16E-04 | 2.02E-04 | 3.50E-04 | 6.13E-04 | 7.48E-09 | 1.31E-08 | 4.27E-08 | 7.46E-08 |
| 3 | Cr6+ | – | – | – | – | 6.03E-08 | 1.06E-07 | 3.44E-07 | 6.04E-07 |
| 4 | Ni | 3.42E-07 | 5.99E-07 | 1.04E-06 | 1.82E-06 | 3.05E-09 | 5.34E-09 | 1.74E-08 | 3.05E-08 |
| 5 | As | 3.67E-07 | 6.45E-07 | 1.11E-06 | 1.95E-06 | 7.06E-10 | 1.24E-09 | 4.03E-09 | 7.08E-09 |
| 6 | Cd | 4.39E-03 | 7.70E-03 | 1.33E-02 | 2.33E-02 | 6.69E-07 | 1.17E-06 | 3.82E-06 | 6.70E-06 |
| 7 | Pb | 6.71E-05 | 1.18E-04 | 2.03E-04 | 3.57E-04 | 4.19E-09 | 7.35E-09 | 2.39E-08 | 4.20E-08 |
| 8 | Hg | 6.75E-04 | 1.19E-03 | 2.05E-03 | 3.59E-03 | – | – | – | – |
It is evident from Table 6 that heavy metals and PCBs emitted during incineration of the T-Y-BMW do not pose any non-carcinogenic health impacts. However, inhalation of Cd was observed to cause carcinogenic health risks among adults and children of India, as its Riskcarcinogenic was observed to be > 10−6. Moreover, increasing trend of emissions from BMW-incinerators and collaborative impacts of the emissions from other sources such as, stubble burning and vehicular emissions, may further deteriorate the health of Indian citizens. Therefore, to minimize the health risks associated with management of Y-BMW, it is recommended to incorporate and encourage less-polluting technologies in the BMW management system of India.
5. Alternative strategies for mitigation
5.1. Alternative technologies
It is evident from the results present in Section 4, of this study, that the pandemic outbreak of COVID-19 has increased the burden on BMW-incineration units of India, which may further give rise to several environmental-health issues. Therefore, it is imperative for the authorities to take review of the current situation, identify the alternative options, frame new policies and efficiently implement them. The various alternative technologies, that can bring a comprehensive improvement in the environmental-health aspects of the current system of BMW management include, autoclaving, pyrolysis, plasma, microwave and chemical disinfection. The brief comparison, of the various alternative technologies with the conventional incineration-based BMW disposal method, is described in Table 7 .
Table 7.
Comparison of different BMW management technologies.
| Type of technology | Capacity | Installation cost | Operation cost | Pollution (air and water) | Volume reduction |
|---|---|---|---|---|---|
| Autoclave | ●●●● | ●● | ●●● | ● | ●● |
| Microwave | ●● | ●● | ●● | ● | ●● |
| Incineration | ●●●●● | ●●●● | ●●●● | ●●●●● | ●●●●● |
| Pyrolysis | ●●● | ●●●●● | ●●●●● | ●● | ●●● |
| Plasma | ●●● | ●●●●● | ●●●●● | ●● | ●●● |
| Chemical disinfection | ●●● | ●●● | ●●● | ●●● | ●●● |
Efficacy, of all the BMW-disposal technologies mentioned in Table 7, has been assessed under the State and Territorial Association of Alternate Treatment Technologies (STAATT) criteria (WHO, 2014). As per this assessment, all the technologies, except chemical disinfection, fall under the level 4 technologies and are efficient in sterilizing the C-BMW. However, as applicability of chemical disinfection is limited only to disinfection of BMW, it falls in the category of level 3 technologies.
Findings of present investigation have illustrated that during the pandemic outbreak of COVID-19, the amount of T-BMW has increased significantly. Hence, during these unprecedented times, it is imperative to identify an alternative treatment technology which could efficiently treat large quantity of infectious waste, within a short span of time. From Table 7, it can be seen that other than conventional method of incineration, autoclave technology is another technology that can handle large amount of BMW. In autoclave-based treatment, 5–3000 kg of BMW waste can be treated within 1 h (WHO, 2019). Also, in this technique, the environmental emissions and operational costs are comparatively low. This technology is considered suitable for the treatment of disposables, microbiological waste and sharps (MoEFCC, 2016). However, it is not considered efficient in treatment of anatomical wastes, radioactive waste, chemicals and chemotherapy waste. The only disadvantage reported in the autoclave process is that the volume reduction of BMW is lower than incineration and this, which can increase the influx of waste on landfill disposal sites.
Similar to autoclave process, microwave-based treatment also emit very less amount of pollutants. In microwave treatment of BMW, electromagnetic waves of wavelength: 1 to 1000 mm, and frequency: 900 MHz–2500 MHz, are used to disinfect the waste (Neto et al., 1999). Considering the utility of microwave and autoclave-based treatment of BMW, there are now convincing evidences that, in combination with mechanical shredding, equipment can be designed to disinfect the COVID-infected waste (MEE, 2006). In China, a mobile facility, based on microwave treatment, has shown promising results while treating 80 kg/h of the BMW (Resilient Environmental Solutions, 2020; BMW, 2020). Rapid action, high energy efficiency, low emission rate and efficient disinfection may prove autoclave and microwave treatments as effective alternative treatment technology (Ohtsu et al., 2011). However, high operational and installation cost discourages their use in low-income group of countries (Datta et al., 2020).
Just like conventional incineration treatment, pyrolysis is also a thermal process that sterilizes the BMW at high temperature. However, in pyrolysis, treatment takes place in the absence of oxygen. In this way, combustion of the waste is limited and emissions are also low (Zhu et al., 2008). However, volume reduction of waste is compromised. Similarly, in plasma-pyrolysis, BMW is treated in the absence of oxygen and at high temperature. Although its capacity is also high and emissions are low, yet, because of its high operational and installation cost, its applicability in pandemic situation is not favored (Messerle et al., 2018).
During pandemic outbreak of COVID-19, chemicals have played significant role in disinfecting the surfaces and certain body parts. Therefore, applicability of chemical disinfection also needs to be evaluated for treatment of COVID-infectious waste. Chemical treatment involves moderate operating cost as compared to other treatment options. As efficiency of chemical treatment is only limited to disinfection and it could not reduce the volume of the waste, therefore, it has been recognized only as a preventive or preliminary measure. However, recently, their applications in reprocessing and re-using a specific COVID waste viz., PPEs, have been reported (Barcelo, 2020). Compatibility of vaporous H2O2 with the polymer-based materials and reduced time has brought its disinfecting properties forward for treating the PPE kits (Barcelo, 2020). Its utilization in disinfecting the used N95 masks under controlled conditions has also shown promising results (Price et al., 2020; Chin et al., 2020).
Therefore, it can be concluded that although, alternative technologies have certain advantages over incineration, yet they cannot completely substitute it. It has also been suggested by literature that incineration may remain the most favorable treatment technique for infectious waste (Ilyas et al., 2020; Lee et al., 2004). It is recommended that the discussed alternative technologies can be made to work, side-by-side, to share the increased amount of BMW during pandemic period. However, for this purpose segregation needs to be done efficiently.
5.2. Segregation and treatment of specific waste
During pandemic outbreak of COVID-19, it has been reported that the amount of only a certain type of waste viz., single-use plastic, masks, chemicals, PPEs etc., has increased. Therefore, these types of waste should be segregated from the rest of the BMW. In this way, they could be treated by other environmental-friendly techniques. A brief description, of the waste materials that could be segregated for specific type of treatment, is mentioned in Table 8 .
Table 8.
Treatment of specific wastes and its benefits.
| S.No. | Waste type | BMW categorya | Alternate treatment | Benefits |
|---|---|---|---|---|
| 1 | Sharps (comprising plastic and metal) | Yellow, red and blue |
|
|
| 2 | Anatomical waste | Yellow |
|
|
| 3 | Pathological waste | Yellow |
|
|
| 4 | Pharmaceutical and chemical waste | Blue, red |
|
|
| 5 | PPE kits | Yellow, blue and red |
|
|
As per MoEFCC (2016)
5.3. Substitution
Avoiding the use of certain types of raw material while manufacturing the health-care equipment may significantly reduce toxic emissions from incinerators (Lee et al., 2004). For an instance, medical equipment/products, comprising PVC, are the major source of chlorine emissions from the incineration units. Moreover, incineration of the PVC-containing medical products also leads to emissions of dioxins and furans (Thorton et al., 1996). Therefore, while emphasizing on efficient segregation of the BMW, it is also advised to encourage the substitution of PVC material in medical products, with bio-based plastics (Silva et al., 2020). Legislations, for assisting the faster transition from general plastic to bio-based plastic, need to be implemented at a larger scale. In this way, all the progress made to achieve the United Nation’s Sustainable Development Goals (SDGs) viz., SDG 3, SDG 8, SDG 12, SDG 13 etc., could be sustained (PlasticsEurope, 2019; HCWH, 2020).
Materials, used for making masks, also comprise of polypropylene and polyethylene. These masks could increase the content of microplastics in the fresh water bodies, further leading to several health-related consequences (NGO Oceans Asia, 2020; Prata et al., 2020; Silva and Nanny, 2020). Therefore, un-controlled use and disposal of masks have also become a controversial issue during recent pandemic situations (WHO 2020). In this context, substitution of the masks, consisting of polypropylene and polyethylene, with textile-made masks has been highlighted by Somani et al. (2020).
Similarly, there are several products, such as, thermometers and sphygmomanometers, in current health-care system, which rely on use of mercury. In the end of their life-cycle these products get incinerated and become a cause of mercury emissions. Several countries have already banned the use of mercury containing products from their health-care system (O’Brien 2000). Also, increased use of contact-less infra-red radiations-based thermometers has given India also an opportunity to remove the mercury based thermometers from its health-care system.
6. Conclusions
The findings of this study revealed that, in India, a COVID-infected patient generates approximately 3.41 kg/d of BMW. Under pandemic conditions, 609 T/d BMW and 101 T/d BMW are generated by normal and COVID-infected patients, respectively. It is also estimated that Y-BMW constitutes 50.4% of the BMW generated. Exponential increase, in the number of COVID-infected patients since 21st March 2020, has inflated the incineration units of India with Y-BMW and this study revealed that by 14th July 2020, the incineration capacity of all the CBWTFs of India would have been fully utilized. Subsequently, assessment of environmental-health impacts, associated with emissions from incineration of BMW, revealed that emissions of Cd may prove fatal for adults and children of India. Therefore, it is recommended to side-by-side use available alternative technologies for the treatment of BMW. In this way, burden on BMW-incineration units of India could be minimized. Also, to reduce the emissions of the harmful chemicals from incineration units, segregation should be encouraged and different treatment options for specific wastes should be adopted. Substitution of harmful raw materials with other harmless substances may also assist in reducing the toxic emissions from incineration units.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
This paper has been recommended for acceptance by Dr. Da Chen.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envpol.2021.116621.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Allison A.L., Ambrose D.E., Domenech A.T., Bawn M., Casas A.M., Chau C., Chandler K., Dobrijevic D., Hailes H., Lettieri P., Liu C., Medda F., Michie S., Miodownik M., Purkiss D., Ward J. The environmental dangers of employing single-use face masks as part of a COVID-19 exit strategy. UCL Open: Environ. Times. 2020 doi: 10.14324/111.444/000031.v1. [DOI] [Google Scholar]
- Almuneef M., Memish Z. Effective medical waste management: it can be done. Am. J. Infect. Contr. 2003;31(3):188–192. doi: 10.1067/mic.2003.43. [DOI] [PubMed] [Google Scholar]
- Alvim-Ferraz M.C.M., Afonso S.A.V. Incineration of healthcare wastes: management of atmospheric emissions through waste segregation. Waste Manag. 2005;25(6):638–648. doi: 10.1016/j.wasman.2004.07.017. [DOI] [PubMed] [Google Scholar]
- Askarian M., Vakili M., Kabir G. Results of a hospital waste survey in private hospitals in Fars Province, Iran. Waste Manag. 2004;24(4):347–352. doi: 10.1016/j.wasman.2003.09.008. [DOI] [PubMed] [Google Scholar]
- ASSOCHAM India. 2018. Unearthing the Growth Curve and Necessities of Bio Medical Waste Management of India. [Google Scholar]
- Ayres J.G. In: Hester R.E., Harrison R.M., editors. vol. 10. 1998. Health effects of gaseous air pollutants; pp. 1–20. (Air Pollution and Health. Issues in Environmental Science and Technology). [Google Scholar]
- Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8:104006. doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bdour A., Altrabsheh B., Hadadin N., Al-Shareif M. Assessment of medical wastes management practice: a case study of the northern part of Jordan. Waste Manag. 2007;27(6):746–759. doi: 10.1016/j.wasman.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Biggeri A., Barbone F., Lagazio C., Bovenzi M., Stanta G. Air pollution and lung cancer in Trieste, Italy: spatial analysis of risk as a function of distance from sources. Environ. Health Perspect. 1996;104:750–754. doi: 10.1289/ehp.96104750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BMW . 2020. China Chooses the Sterilwave Solution for On-Site Treatment of Waste Contaminated by the Coronavirus.https://www.bertin-medical-waste.com/chinachooses-the-sterilwave-solution-for-on-site-treatment-of-waste-contaminated-bythe-coronavirus/ [Google Scholar]
- Cheng Y.W., Li K.C., Sung F.C. Medical waste generation in selected clinical facilities in Taiwan. Waste Manag. 2010;30(9):1690–1695. doi: 10.1016/j.wasman.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peiris M., Poon L.L.M. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comunian S., Dongo D., Milani C., Palestinin Air Pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19’s morbidity and Mortality. Int. J. Environ. Res. Publ. Health. 2020;17(12):4487. doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CPCB . Central Pollution Control Board; New Delhi, India: 2020. Scientific Disposal of Bio-Medical Waste Arising Out of COVID-19 Treatment- Compliance of BMWM Rules, 2016.https://greentribunal.gov.in/sites/default/files/news_updates/Status%20Report%20in%20O.A%20No.%2072%20of%202020.pdf [Google Scholar]
- Cutler S. Mounting medical waste from COVID-19 emphasizes the need for a sustainable waste management strategy. 2020. https://ww2.frost.com/frost-perspectives/managing-the-growing-threat-of-covid-19-generated-medical-waste/
- Datta P., Mohi G.K., Chander J. Biomedical waste management in India: critical appraisal. J. Lab. Phys. 2020;1(10):6–14. doi: 10.4103/JLP.JLP_89_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Environmental Affairs (DoEA) 2010. The Framework for the Management of Contaminated Land, South Africa.http://sawic.environment.gov.za/documents/562.pdf [Google Scholar]
- Devara P.C.S., Maheskumar R.S., Raj P.E., Pandithurai G., Dani K.K. Recent trends in aerosol climatology and air pollution as inferred from multi-year lidar observations over A tropical urban station. Int. J. Climatol. 2002;22:435–449. [Google Scholar]
- Diggle P.J. A point process modeling approach to raised incidence of a rare phenomenon in the vicinity of a pre specified point. J. Roy. Stat. Soc. A. 1990;153:349–362. [Google Scholar]
- Elliot P., Eaton N., Shaddick G., Carter R. Cancer incidence near municipal solid waste incinerators in Great Britain. Part 2: histopathological and case-note review of primary liver cancer cases. Br. J. Canc. 2000;82:1103–1106. doi: 10.1054/bjoc.1999.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA . fifth ed. vol. 1. 1995. Medical waste incineration. In compilation of air pollutant emission factors. (Stationary Point and Area Emission Units (AP-42)). (Chapter 13).2.4. Research Triangle Park, NC. [Google Scholar]
- ESCAP (United Nation Economic and Social Commission for Asia and the Pacific) 2020. The Safe Waste Treatment for COVID-19: Lessons from the Republic of Korea.https://www.unescap.org/resources/safe-waste-treatment-covid-19-lessons-republic-korea [Google Scholar]
- Gupta A., Bherwani H., Gautam S., Anjum S., Musugu K., Kumar N., Anshul A., Kumar R. Air pollution aggravating COVID-19 lethality? Exploration in Asian cities using statistical models. Environ. Dev. Sustain. 2020 doi: 10.1007/s10668-020-00878-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HCWH . 2020. Health Care Waste Management and the Sustainable Development Goals.https://noharm-global.org/issues/global/healthcare-waste-management-and-sustainable-development-goals accessed 2020/5/11. [Google Scholar]
- Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020;749:141652. doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox E.G. Childhood cancers, birth-places, incinerators and landfill sites. Int. J. Epidemiol. 2000;29:391–397. [PubMed] [Google Scholar]
- Lee B.K., Ellenbecker M.J., Moure-Ersaso R. Alternatives for treatment and disposal cost reduction of regulated medical waste. Waste Manag. 2004;24:143–151. doi: 10.1016/j.wasman.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Li H., Xu X., Dai D., Huang Z., Ma Z., Guan Y. Air pollution and temperature are associated with increased COVID-19 incidence: a time series study. Int. J. Infect. Dis. 2020;97:278–282. doi: 10.1016/j.ijid.2020.05.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd O.L., Lloyd M.M., Williams F.L.R., Lawson A. Twinning in human populations and in cattle exposed to air pollution from incinerators. Br. Med. J. 1988;45:556–560. doi: 10.1136/oem.45.8.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallapur C. 2020. Sanitation Workers at Risk from Discarded Medical Waste Related to COVID-19.https://www.indiaspend.com/sanitation-workers-at-risk-from-discarded-medical-waste-related-to-covid-19/ [Google Scholar]
- Manasi S. Challenges in biomedical waste management in cities: a ward level study of Bangalore. Adv. Recycling Waste Manag. 2017;2(1):1–8. [Google Scholar]
- Marinkovic N., Vitale K., Holcer N.J., Dzakula A., Pavic T. Management of hazardous medical waste in Croatia. Waste Manag. 2008;28(6):1049–1056. doi: 10.1016/j.wasman.2007.01.021. [DOI] [PubMed] [Google Scholar]
- McGregor D.B., Partensky C., Wilbourn J., Rice J.M. An IARC evaluation of polychlorinated dibenzo-p-dioxins and polychlorinateddibenzofurans as risk factors in human carcinogenesis. Environ. Health Perspect. 1998;106:755–760. doi: 10.1289/ehp.98106755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MEE . 2006. Technical Specifications for Steam-Based Centralized Treatment Engineering on Medical Waste (On Trial). China.http://english.mee.gov.cn/Resources/standards/Solid_Waste/other_standards1/200710/t20071024_111967.shtml [Google Scholar]
- Messerle V.E., Mosse A.L., Ustimenko A.B. Processing of biomedical waste inplasma gasifier. Waste Manag. 2018;79:791–799. doi: 10.1016/j.wasman.2018.08.048. [DOI] [PubMed] [Google Scholar]
- Miguel D., Iribarren E., Chacon I., Ordonez E., Charlesworth S.A. Risk-based evaluation of the exposure of children to trace elements in playgrounds in Madrid (Spain) Chemosphere. 2007;66:505–513. doi: 10.1016/j.chemosphere.2006.05.065. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare (MoHFW) 2010. Annual Report to the People on Health.http://mohfw.nic.in/WriteReadData/l892s/9457038092.pdf [Google Scholar]
- Mocarelli P., Gerthoux P.M., Ferrai E., Patterson D.G., Keszak S.M., Brambilla P., Vincoli N., Signorini S., Tramacere P., Carreri V., Sampson E.J., Turner W.E., Needham L.L. Paternal concentrations of dioxin and sex ratio of offspring. Lancet. 2000;355:1858–1863. doi: 10.1016/S0140-6736(00)02290-X. [DOI] [PubMed] [Google Scholar]
- MoEFCC . MoEFCC; 2016. Biomedical Waste Management Rules.https://dhr.gov.in/sites/default/files/Bio-medical_Waste_Management_Rules_2016.pdf 2016. [Google Scholar]
- Mohee R. Medical wastes characterization in healthcare institutions in Mauritius. Waste Manag. 2005;25(6):575–581. doi: 10.1016/j.wasman.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Neto A.G., Carvalho J.N.D., Fonseca J.A.C.D., Carvalho A.M.D.C., Castro M.M.D.M.V. SBMO/IEEE MTT-S International Microwave and Optoelectronics Conference. IEEE; 1999. Microwave medical waste disinfection: a procedure to monitor treatment quality; pp. 63–65. [Google Scholar]
- NGO Oceans Asia. 2020. No Shortage of Surgicalmask at the Beach.http://oceansasia.org/beach-mask-coronavirus/ [Google Scholar]
- O’Brien E. Replacing the mercury sphygmomanometer. Br. Med. J. 2000;815 doi: 10.1136/bmj.320.7238.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogunseitan O.A. The materials genome and COVID-19 pandemic. J. Occup. Med. 2020 doi: 10.1007/s11837-020-04207-3. [DOI] [Google Scholar]
- Ohtsu Y., Onoda K., Kawashita H., Urasaki H. A comparison of microwave irradiation, electric, and hybrid heating for medical plastic-waste treatment. J. Renew. Sustain. Energy. 2011;3:435. [Google Scholar]
- Osius N., Karmaus W. Thyroid hormone level in children in the area of a toxic waste incinerator in South Essen. Gesundheitswesen. 1998;60:107–112. [PubMed] [Google Scholar]
- Osius N., Karmaus W., Kruse H., Witten J. Exposure to polychlorinatedbiphenyls and levels of thyroid hormones in children. Environ. Health Perspect. 1999;107:843–849. doi: 10.1289/ehp.99107843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oweis R., Al-Widyan M., Al-Limoon O. Medical waste management in Jordan: a study at the king hussein medical center. Waste Manag. 2005;25(6):622–625. doi: 10.1016/j.wasman.2005.03.011. [DOI] [PubMed] [Google Scholar]
- PlasticsEurope . 2019. Plastics - the Facts 2019. An Analysis of European Plastics Production, Demand and Waste Data. (PlasticsEurope Brussels, Belgium) [Google Scholar]
- Price A., Cui Y., Liao L., Xiao W., Yu X., Wang H., Zhao M., Wang Q., Chu S., Chu L. 2020. Is the Fit of N95 Facial Masks Affected by Disinfection? A Study of Heat and UV Disinfection Methods Using the OSHA Protocol Fit Test. medRxiv. [DOI] [Google Scholar]
- Prüss A., Giroult E., Rushbrook P. WHO; Geneva: 1999. Safe Management of Wastes from Health-Care Activities.https://www.who.int/water_sanitation_health/medicalwaste/itoxiv.pdf?ua=1 [Google Scholar]
- Ranjan R., Pathak R., Singh D.K., Jalaluddin M., Kore S.A., Kore A.R. Awareness about biomedical waste management and knowledge of effective recycling of dental materials among dental students. J. Int. Soc. Prev. Community Dent. 2016;6:474–479. doi: 10.4103/2231-0762.192941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reports Market. 2019. Personal Protective Equipment Market by Type (Hands & Arm Protection, Protective Clothing, Foot & Leg Protection, Respiratory Protection, Head Protection), End-Use Industry (Manufacturing, Construction, Oil & Gas, Healthcare) - Global Forecast to 2022.https://www.marketsandmarkets.com/Market-Reports/personal-protective-equipment-market-132681971.html [Google Scholar]
- Resilient Environmental Solutions . 2020. Environmental Assessment for the Proposed Establishment of STERILWAVE Apparatus for Treatment of Medical Waste at Rhino Park Private Hospital, Windhoek Screening Report.http://www.eia.met.gov.na/screening/1371_a_screening_report_rhinopark_hospital_sterilwave.pdf accessed22 May 2020. [Google Scholar]
- Reuters . 2020. Discarded Corona Virus Masks Clutter Hong Kong’s Beaches, Trails.https://www.reuters.com/article/us-healthcoronavirus-hongkong-environme/discarded-coronavirus-masksclutter-hong-kongs-beaches-trails-idUSKBN20Z0PP accessed: 2020/5/11. [Google Scholar]
- Shaha R., Hardinga J., Browna J., McKinlaya C. Neonatal glycaemia and neuro developmental outcomes: a systematic review and meta-analysis. Neonatology. 2019;115:116–126. doi: 10.1159/000492859. [DOI] [PubMed] [Google Scholar]
- Shaner H., McRae G. Revised ed. CGH Environment Strategies Inc; USA: 2002. Eleven Recommendations for Improving Health Care Waste Management. [Google Scholar]
- Sharma R., Sharma M., Sharma R., Sharma V. The impact of incinerators on human health and environment. Rev. Environ. Health. 2013;28(1):67–72. doi: 10.1515/reveh-2012-0035. [DOI] [PubMed] [Google Scholar]
- Shihabudeen M.M., Eldon R.R., Philip L., Swaminathan T. Performance of BTX degraders under substrate versatility conditions. J. Hazard Mater. 2004;B109:201–211. doi: 10.1016/j.jhazmat.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Shinee E., Gombojav E., Nishimura A., Hamajima N., Ito K. Healthcare waste management in the capital city of Mongolia. Waste Manag. 2008;28(2):435–441. doi: 10.1016/j.wasman.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Silva P.M., Nanny M.A. Impact ofmicroplastic fibers from the degradation of non- woven synthetic textiles to the Magdalena river water column and river sediments by the city of Neiva, Huila (Colombia) Water. 2020;12:1210. doi: 10.3390/w12041210. [DOI] [Google Scholar]
- Silva A.L.P., Prata J.C., Walker T.R., Campos D., Duarte A.C., Soares A.M.V.M., Barcelo D., Santos T.R. Rethinking and optimizing plastic waste management under COVID-19 pandemic: policy solutions based on redesign and reduction of single-use plastics and personal protective equipment. Sci. Total Environ. 2020;742:140565. doi: 10.1016/j.scitotenv.2020.140565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somani M., Srivastava A.N., Gummadivalli S.K., Sharma A. Indirect implications of COVID-19 towards sustainable environment: an investigation in Indian context. Bio. Tech. Rep. 2020;11:100491. doi: 10.1016/j.biteb.2020.100491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorton J., McCally M., Orris P., Weinberg J. Hospitals and plastics. Dioxin prevention and medical waste incinerators. Publ. Health Rep. 1996, July;111(4):298–308. [PMC free article] [PubMed] [Google Scholar]
- Tudor T.L., Noonan C.L., Jenkin L.E.T. Healthcare waste management: a case study from the national health service in cornwall, United Kingdom. Waste Manag. 2005;25(6):606–615. doi: 10.1016/j.wasman.2004.10.004. [DOI] [PubMed] [Google Scholar]
- United Nations Environment Protection (UNEP) 2005. E-waste: “The Hidden Side of IT Equipment’s Manufacturing and Use: Early Warnings on Emerging Environmental Threats No. 5.https://archive-ouverte.unige.ch/unige:23132 [Google Scholar]
- U.S. Department of Energy (USDoE) U.S. Department of Energy’s Oak Ridge Operations Office (ORO); 2011. The Risk Assessment Information System (RAIS)https://rais.ornl.gov/ [Google Scholar]
- U.S. Environmental Protection Agency (U.S. EPA) vol. 1. 1998. Risk assessment guidance for superfund.https://www.epa.gov/sites/production/files/2015-09/documents/rags_a.pdf (Human Health Evaluation Manual). [Google Scholar]
- US Environmental Protection Agency (USEPA) 2004. Risk Assessment Guidance for Superfund Volume I: Human Health Evaluation Manual. [Google Scholar]
- Van-den-Berg R. National Institute for Public Health and the Environment RIVM; 1995. Human Exposure to Soil Contamination: a Qualitative and Quantitative Analysis towards Proposals for Human Toxicological Intervention Values. [Google Scholar]
- Viel J.F., Arveux P., Baverel J., Cahn J.Y. Soft-tissue sarcoma and non-Hodgkin’s lymphoma clusters around a municipal solid waste incinerator with high dioxin emission levels. Am. J. Epidemiol. 2000;152:13–19. doi: 10.1093/aje/152.1.13. https://doi:10.1093/aje/152.1.13 [DOI] [PubMed] [Google Scholar]
- Wang J.Y., Hsiue T.R., Chen H.I. Bronchial responsiveness in an area of air pollution resulting from wire reclamation. Arch. Dis. Child. 1992;67:488–490. doi: 10.1136/adc.67.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2014. Safe Management of Wastes from Health Care Activities.http://www.who.int/water_sanitation_health/publications/wastemanag/en/ accessed June 2020. [Google Scholar]
- WHO . World Health Organization; Geneva: 2019. Overview of Technologies for the Treatment of Infectious and Sharp Waste from Health Care Facilities.https://apps.who.int/iris/bitstream/handle/10665/328146/9789241516228-eng.pdf?ua=1 [Google Scholar]
- WHO . 2020. Shortage of Personal Protective Equipment Endangering Health Workers Worldwide.https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangeringhealth-workers-worldwide accessed 2020/5/11. [Google Scholar]
- Zhu H.M., Yan J.H., Jiang X.G., Lai Y.E., Cen K.F. Study on pyrolysis of typical medical waste materials by using TG-FTIR analysis. J. Hazard Mater. 2008;153:670–676. doi: 10.1016/j.jhazmat.2007.09.011. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection- Evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmirou D., Parent B., Potelon J.L. Etude epidemiologique deseffetssur la sante des rejetsatmospheriqued ’uneusined ’inceneration de dechetsindustriels et menagers. Rev. Epidemiol. Sante. 1984;32:391–397. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.