To the Editor:
The coronavirus disease (COVID-19) pandemic has disproportionately affected ethnic minorities and males in the United States. Through late July, U.S. Centers for Disease Control and Prevention (CDC) data suggest minorities make up nearly two-thirds of all U.S. COVID-19 cases (1) and a similar proportion of intensive care unit (ICU) admissions (2). Critical illness from COVID-19 also appears more common in men than women (1, 2). Recommended care includes supportive therapies identified by previous clinical trials to provide benefit in related critical illnesses (3). Therefore, we evaluated ethnic and sex composition of past critical care trial populations to determine if they are representative of patients with severe COVID-19.
We reviewed multicenter randomized trials of critically ill adults in which mortality was the main endpoint. Eligible trials were published between 2008 and 2018 in The New England Journal of Medicine, JAMA, Lancet, Lancet Respiratory Medicine, American Journal of Respiratory and Critical Care Medicine, Intensive Care Medicine, or Critical Care Medicine. The Medicare definition of critical illness was adopted to select relevant trials. Data were extracted from each trial’s main publication and trial registration website in blinded duplicate, with discrepancies resolved by a third reviewer. Mean trial demographic representation was compared with U.S. COVID-19 population statistics reported by the CDC through July 20, 2020, using the t test for location (the univariate procedure in SAS v9.4; SAS Institute).
Ninety-seven trials were included. Participant ethnicity was reported in 20 trials (combined enrollment: 26,942 patients), 80% of which included U.S. patients. Nonwhites made up a median of 17.8% (interquartile range [IQR], 10.2–26.5%) of trial participants (Figure 1A). Similarly, low nonwhite representation was found in analyses restricted to trials with U.S. participants (median 19.8%; IQR, 16.6–27.3%). Patients with COVID-19 in the ICU were 3.3 times likelier to be nonwhite than critical care trial participants (60.2% vs. 18.2%; P < 0.01). Nonwhite trial enrollment never achieved representation proportionate even to the current U.S. population (39.6%) (4).
Figure 1.
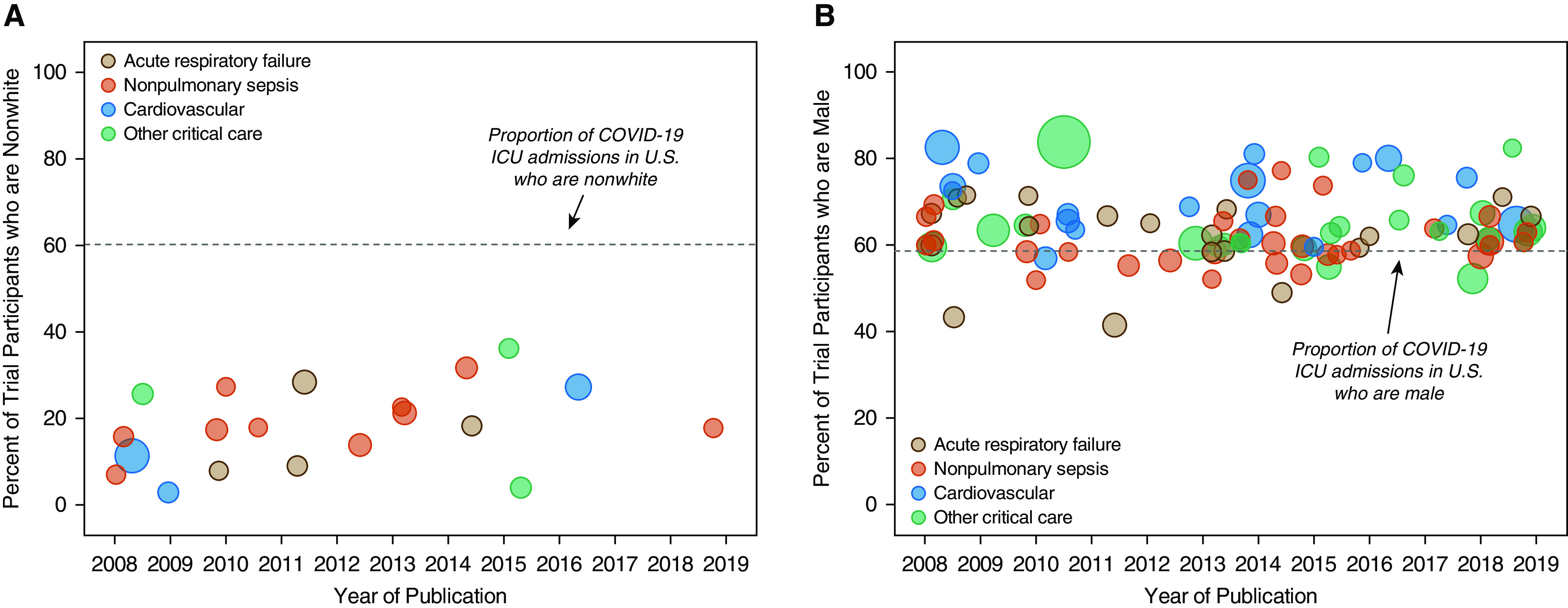
Ethnicity and sex of critical care trial participants compared with hospitalized patients with coronavirus disease (COVID-19). (A) Representation of nonwhites among COVID-19 intensive care admissions (60.2%) far exceeds their representation in multicenter clinical trials of critical illness over the last decade. (B) Representation of males among COVID-19 hospitalizations is mirrored by male preponderance in critical care clinical trials. Bubble size corresponds to trial sample size relative to other included trials. Trials were classified according to their main topical focus as acute respiratory failure (including pneumonia), nonpulmonary sepsis, cardiovascular, or other critical care. ICU = intensive care unit.
Participant sex was reported in 96 trials (combined enrollment: 156,014 patients). Males made up a median of 63.1% (IQR, 59.6–67.8%) of trial participants (Figure 1B). Male enrollment exceeded female enrollment in all but three trials. Patients with COVID-19 in the ICU were less likely to be male than critical care trial participants, although the difference was small and male preponderance was observed for both (58.6% vs. 64.2%; P < 0.01).
Similar findings for ethnicity and sex were observed in analyses restricted to trials studying acute respiratory failure or sepsis (Figure 1).
Our findings on ethnic and sex representation in critical care trials carry twofold significance for COVID-19. First, systematic underrepresentation of ethnic minorities in prior critical care trials creates uncertainty regarding generalizability of findings to patients most severely affected by COVID-19 in the United States. Comorbid, environmental, socioeconomic, and structural factors might influence pulmonary, immune, and vascular responses to injury and timing of presentation for critical illness among ethnic minorities (5). Second, male preponderance was observed not only among patients with severe COVID-19 but also among critical care trial participants. If not entirely due to biased enrollment, these data lend further credence to a biological basis (intrinsic and/or extrinsic) for male predisposition to critical illness from COVID-19 and otherwise. Such factors may influence treatment responsiveness to both COVID-19–specific therapies and to interventions considered best practice based on prior trials.
Supplementary Material
Footnotes
Supported in part by a grant from the U.S. National Institutes of Health (K23-HL133489) (J.R.B.).
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.US Centers for Disease Control and Prevention. CDC COVID data tracker. 2020 [accessed 2020 Jul 20]. Available from: https://www.cdc.gov/covid-data-tracker/index.html.
- 2.COVID-19-Associated Hospitalization Surveillance Network COVID-NET; US Centers for Disease Control and Prevention. COVID-19 laboratory-confirmed hospitalizations. 2020 [accessed 2020 Jul 20]. Available from: https://gis.cdc.gov/grasp/COVIDNet/COVID19_5.html.
- 3.National Institutes of Health. Coronavirus disease 2019 (COVID-19) treatment guidelines. 2020 [accessed 2020 Jul 20]. Available from: https://covid19treatmentguidelines.nih.gov. [PubMed]
- 4.US Census Bureau. US census quick facts. 2020 [accessed 2020 May 6]. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045218.
- 5.Khunti K, Singh AK, Pareek M, Hanif W. Is ethnicity linked to incidence or outcomes of COVID-19? BMJ. 2020;369:m1548. doi: 10.1136/bmj.m1548. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


