The authors examined the factors that were associated with county-level novel coronavirus disease 2019 case and death rates in the state of Georgia. They found that county percent Black population was associated with both case and death rates even after adjustment for socioecologic and health system factors. Primary care health professional shortage areas were associated with higher novel coronavirus death rates, even when adjusted for other factors.
Supplemental digital content is available in the text.
Key Words: COVID-19, ecologic analysis, primary care, racial disparities
Abstract
Objectives
We hypothesized that the proportion of Black individuals in a county would be associated with higher rates of coronavirus disease 2019 (COVID-19) cases and deaths, even after accounting for other high-risk socioecologic factors such as poverty, population density, and household crowding, and uninsured rates. We also expected that counties designated as primary care health professional shortage areas (PCHPSAs) would be associated with higher COVID-19 death rates, and the lack of primary care access would exacerbate racial disparities in death rates. We undertook this study to test these hypotheses and discern the independent effects of racial composition, socioecologic characteristics, and healthcare system factors on COVID-19 cases and deaths in Georgia counties.
Methods
We used county-level COVID-19 cases and deaths on April 23, 2020 from the Johns Hopkins Coronavirus Resource Center and estimates of 2019 county-level populations from the US Census Bureau to calculate the cumulative event rates for the state of Georgia. We used multiple regression models to examine crude and adjusted associations of socioecologic and health system variables with county-level COVID-19 case and mortality rates.
Results
After adjustment, a 1% increase in the proportion of Black people in the county resulted in a 2.3% increase in the county COVID-19 confirmed case rate and a 3.0% increase in the death rate (relative risk 1.03, 95% confidence interval 1.01–1.05, P < 0.001). Primary care shortage areas had a 74% higher death rate (relative risk 1.74, 95% confidence interval 1.00–3.00, P = 0.049).
Conclusions
These results highlight the impact of racial disparities on the spatial patterns of COVID-19 disease burden in Georgia, which can guide interventions to mitigate racial disparities. The results also support the need for robust primary care infrastructure throughout the state.
Key Points
Counties in Georgia with a higher percentage of Black residents had higher coronavirus disease 2019 (COVID-19) case and death rates, even after adjusting for socioecologic and health system factors.
Counties designated as primary care health professional shortage areas had higher rates of COVID-19.
Further study is needed to determine what factors are responsible for the higher rate of COVID outcomes in counties with a higher percentage of Black residents.
The study highlights the need to recruit and retain primary care providers in counties where there is a shortage of primary care providers.
Coronavirus disease 2019 (COVID-19) has disproportionately affected minority communities in terms of cases and severity of outcomes across the United States.1–3 In particular, non-Hispanic Black (Black) populations bear disproportionate burdens of COVID-19 cases and deaths.4,5 This disproportionate impact has been particularly acute in Georgia. In the early part of the pandemic, many counties in Georgia led the nation in cases and deaths, and Albany, Georgia had the second-highest COVID-19 death rate in the country for a metropolitan area behind New York City.6 Hypothesized explanations for these disparities have been attributed to structural and social inequities that exist in these communities, including disproportionate employment in high-exposure fields, disproportionate burden of underlying chronic health conditions, disproportionate burdens of poverty, inadequate access to health care, and higher rates of uninsured status.4,7,8 There is strong evidence that the broad range of racial health disparities experienced by the Black community exists independently of the risk conferred by socioeconomic disadvantage and other social determinants of health.9–11 One ecologic factor that has been associated with more equitable health outcomes across disparate groups is robust access to primary care.12,13
Racial and ethnic disparities in COVID-19 disease burden at the individual level have been identified in epidemiologic studies; however, there are limited COVID-19 ecologic data with complete information for race/ethnicity. As such, it has been difficult to assess the spatial patterns of these racial/ethnic population health disparities. In response, there have been some ecologic analyses that describe spatial patterns of COVID-19 burden in relationship to other socioecologic variables nationally and in Georgia.14 These studies, however, have been primarily descriptive with respect to contextualization of other sociodemographic factors such as poverty, rurality, and hospital capacity. To date, no studies have modeled the independent effects of these ecologic and sociodemographic and healthcare system variables on COVID-19 cases and deaths, and no studies have examined the impact of access to primary healthcare services that influence population health in the context of COVID-19.15–18
Georgia was the first state to allow nonessential businesses to open, on April 24, 2020, after a prolonged shutdown period and shelter-in-place orders. A recent study using data of cumulative cases and deaths up to April 24, demonstrated that counties in Georgia with higher case rates had a higher percentage of Black residents and were different in regard to other factors, including percent uninsured and percent living in poverty.19 Based on this preliminary study, we hypothesized that the proportion of Blacks in a county would be associated with higher rates of COVID-19 cases and deaths even after accounting for other high-risk socioecologic factors such as poverty, population density, household crowding, and uninsured rates. In addition, given the positive impact of primary care access on the health of populations,13 we expected that counties designated as primary care health professional shortage areas (PCHPSAs) would be associated with higher COVID-19 death rates and that lack of primary care access would exacerbate racial disparities in death rates. We undertook this study to test these hypotheses and discern the independent effects of racial composition, socioecologic characteristics, and healthcare system factors on COVID-19 cases and deaths in Georgia counties.
Methods
We obtained county-level COVID-19 cases and deaths on April 23, 2020 from the Johns Hopkins Coronavirus Resource Center20 and estimates of 2019 county-level populations from the US Census Bureau21 for the state of Georgia. PCHPSA designation in 2020 and number of hospital beds per population in 2017 were obtained from Area Health Resource Files of the Health Resources and Services Administration.22 Sociodemographic characteristics were obtained from 2018 estimates of 2014–2018 American Community Survey Data.23 Counties were included in this study if they met the following criteria: they were located in the state of Georgia and they had at least 10 COVID-19 cases on April 23, 2020.
There were two main outcomes in this study: the COVID-19 case rate was calculated and presented as number of cases per 100,000 people and the COVID-19 death rate was calculated and presented as number of deaths per 100,000 people. Exposure variables included the percentage of Black people, the percentage of Asian/Pacific Islanders, the percentage of crowded households (defined as the proportion of households in the county with more than one person per room, excluding bathrooms and kitchens), the percentage of uninsured people, the percentage of people living under the federal poverty level, population density presented as number of people per square mile, number of hospital beds per 1000 people, and percentage of people aged 65 years and older, all of which are continuous variables. PCHPSA designation is the only categorical variable and was categorized as yes/no. Exposure variables were explored based on findings from the published literature.
Descriptive statistics were calculated for outcome variables and exposure variables with means and standard deviations (SDs) or number and proportion reported. As the distribution of COVID-19 case rates was highly right-skewed, it was log-transformed before fitting in linear models. Then, we performed unadjusted and adjusted linear regressions using log-transformed COVID-19 case rates as outcomes, and we reported exponentiated coefficients, exponentiated 95% confidence intervals (CIs), and P values for each exposure variable. Using COVID-19 death numbers as outcome variables and total population in the county as offsets, we conducted unadjusted and adjusted negative binomial regression, with rate ratios, 95% CIs, and P values reported for each exposure variable. All P values were two-sided, and a P < 0.05 was considered statistically significant. SAS version 9.4 (SAS Institute, Cary, NC) was used to perform all of the analyses. We also used ArcGIS Pro (Esri, Redland, CA) to create county-level maps for the two outcomes and nine exposure variables in this study.
Results
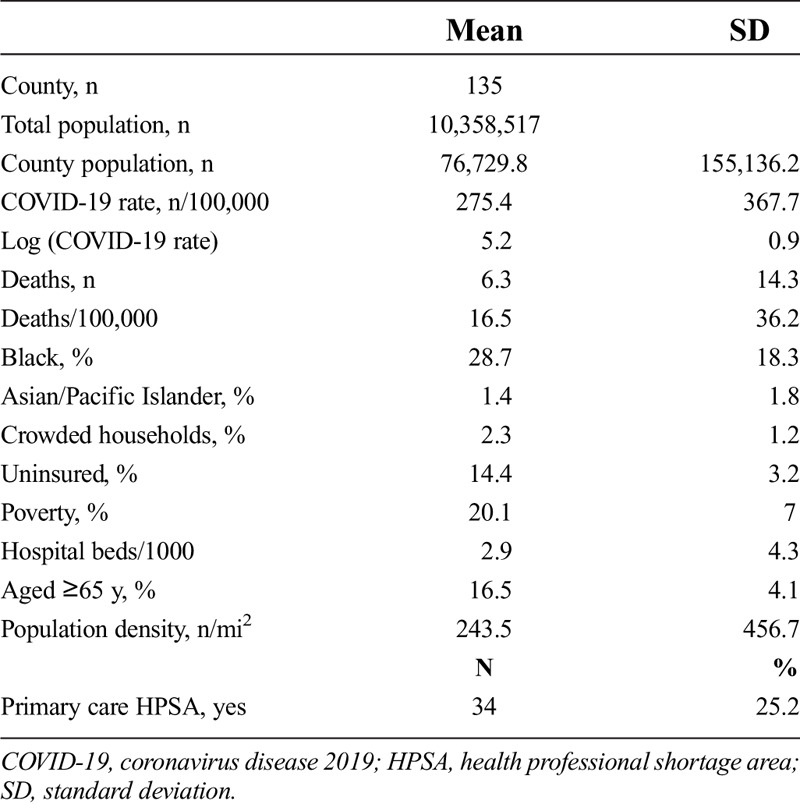
There were 135 of 159 Georgia counties that had at least 10 confirmed COVID-19 cases included. The 135 counties included 10,358,517 people, which represent 97.6% of Georgia’s population. The mean population for a county was 76,729.8 (SD 155,136.2). The overall state COVID-19 confirmed case rate was 188.3/100,000, with county level rates ranging from 33.4 to 2198.3/100,000. The mean number of confirmed COVID-19 cases per 100,000 population for counties was 275.4 (SD 367.7). The mean COVID-19 deaths per 100,000 population was 6.3 (SD 14.3). Descriptive statistics for the sample of counties are presented in Table 1.
Table 1.
Description of sociodemographic characteristics, healthcare accessibility, and confirmed COVID-19 cases and deaths in Georgia, N = 135
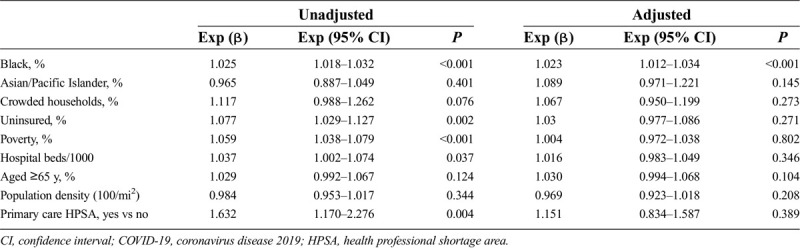
In a bivariate analysis, an increase of 1% of the Black population in the county was associated with a 2.5% increase in the county COVID-19 confirmed case rate. One percent increases in percentage uninsured and percentage of households living below the poverty line were associated with 7.7% and 5.9% increases in case rates, respectively. An increase of 1 hospital bed per 1000 population was associated with a 3.7% increase in case rates. PCHPSAs were associated with a 63.2% greater case rate. A 1/100 mi2 increase in population density was associated with a 1.6% decrease in case rate; however, after mutual adjustment in the same model, only percentage Black population in the county remained significant. After adjustment, a 1% increase in the proportion of Black people in the county resulted in a 2.3% increase in the county COVID-19 confirmed case rate. The complete results of the adjusted and unadjusted linear regression models are presented in Table 2.
Table 2.
Unadjusted and adjusted linear regression models of the association between sociodemographic characteristics, healthcare accessibility, and log-transformed confirmed COVID-19 case rates in Georgia counties, N = 135
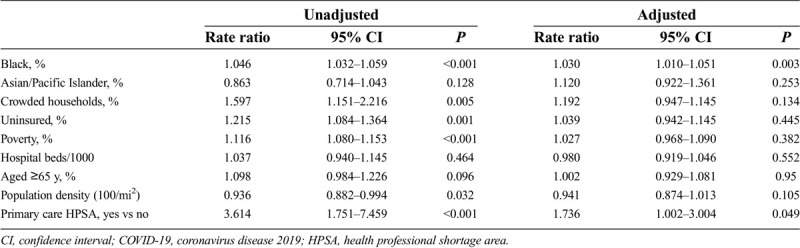
COVID-19 death rates were significantly and positively associated with percentage Black population, percentage of crowded households, percentage of uninsured, percentage living in poverty, and PCHPSA were significantly and negatively associated with population density in unadjusted models (Table 3). After mutual adjustment, only percentage Black and PCHPSA were associated with the COVID-19 mortality rate. A 1% increase in county Black population was associated with a 3.0% increase in the death rate (relative risk [RR] 1.03, 95% CI 1.01–1.05, P < 0.001). Primary care shortage areas had a 74% higher death rate (RR 1.74, 95% CI 1.00–3.00, P = 0.049).
Table 3.
Unadjusted and adjusted negative binomial regression models of the association between sociodemographic characteristics, healthcare accessibility, and confirmed COVID-19 death rates in Georgia counties, N = 135
Maps of case and death rates are shown in Figure 1. High rates of cases and deaths have occurred in southwest Georgia. Other additional counties around the state have experienced high death rates. Maps for the factors (Black percentage and PCHPSA) significantly associated with the outcomes in fully adjusted models are shown in Figure 2. Although not significantly associated in the models, many of the high-rate counties in southwest Georgia also have high rates of uninsured, poverty, crowded housing, and people older than 65 years. Maps for these and other factors are presented as in Supplemental Digital Content Figure A (http://links.lww.com/SMJ/A210).
Fig. 1.
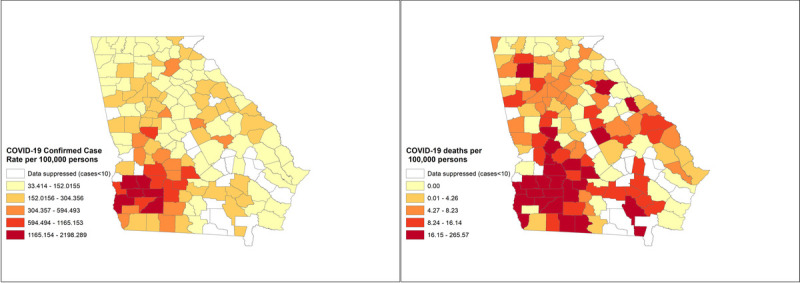
Maps of COVID-19 cases (A) and deaths (B) per 100,000 population in Georgia counties. COVID-19, coronavirus disease 2019.
Fig. 2.
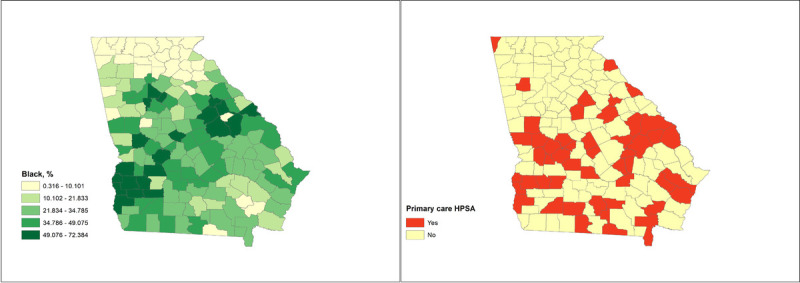
Maps of sociodemographic characteristics with significant associations with COVID-19 cases and deaths per 100,000 population in Georgia counties. COVID-19, coronavirus disease 2019; HPSA, health professional shortage area.
Discussion
On April 24, 2020, Georgia became the first state in the United States to reopen after a mandated shelter-in-place order was lifted. This ecologic analysis of Georgia county COVID-19 data explores cumulative COVID-19 cases and deaths just before the reopening. We examined the impact of county-level sociodemographic factors and access to health care on county COVID-19 case and death rates. Although many factors were associated with both case rate and deaths, only the proportion of Black people in a county was found to be associated with both outcomes in fully adjusted models. In addition, the lack of primary care access was associated with a substantially higher rate of COVID-19 deaths in fully adjusted models. None of the other factors we examined were significant predictors of either outcome in the mutually adjusted models.
We conducted a recent national county-level analysis, which also showed that proportion Black in a county was positively and significantly associated with COVID-19 case and death rate in the spring and fall of 2020. Other studies have found higher numbers of hospital beds and more health system capacity associated with better COVID-19 outcomes14,23; however, we found that these factors were not associated with COVID-19. To our knowledge, no studies have looked at the impact of lack of access to primary care (PCHPSA) on COVID-19 outcomes. One hypothesis in need of further exploration is that people living in communities with more access to primary care may be healthier, with better managed chronic conditions, when infected with COVID-19, resulting in better outcomes and fewer deaths. This is also supported by our finding that PCHPSA was not associated with COVID-19 cases, only deaths. This study sheds light on the important role that primary care access plays in community health. Primary care access has been associated with many positive outcomes,13 and this study demonstrates its positive effect during a public health emergency.
This is the first study (along with our national analysis) to explore the role that access to primary care has on COVID-19 outcomes, finding that primary care access may be protective against COVID-19 deaths. There is a large evidence base that supports the salutary ecologic impact of robust access to primary care on a broad range of health outcomes.12,13,24,25 There are several mechanisms by which adequate access to primary care may be associated with lower COVID-19 case and death rates in Georgia counties, including effective management of chronic conditions that worsen the severity of COVID-19 disease,26 access to timely care,27 and the active role that local primary care clinicians play in local public health efforts.28
These findings reinforce the magnitude of the disproportionate impact that COVID-19 is having on Black communities in Georgia, as supported by several other local, state, and national studies.14 These findings reject the notion that poverty, uninsured rates, and other social determinants are the main drivers of the observed racial disparities in COVID-19 outcomes. The independent association between percentage of Black residents and COVID-19 case and death rates in US counties may be caused by institutionalized racism in the healthcare system, segregation and environmental injustice in communities of color, and disproportionate representation of Black people in high-risk, front-line service work.29,30 It is important to note that structural inequities that lead to disparities in education, access to housing, poverty, and wealth are factors that must be considered in context in mounting efforts to mitigate the observed racial disparities.
This work has several limitations. We lacked the ability to examine race-specific outcomes because large numbers of cases had an unknown race field, and it is not known whether the accuracy of race reporting varied by county or testing location. As race reporting of COVID-19 cases and deaths become more standardized and complete, an analysis should be done to examine whether within-county racial disparities vary at the county level and what factors are associated with mitigating these disparities. We chose to do this analysis as a snapshot of the state of COVID-19 disparities before the reopening of Georgia’s economy on April 24, 2020. Since that time the course of the pandemic has worsened in Georgia, and periodic cross-sectional analyses as well as analysis of rate trajectories of the pandemic in Georgia should be done to document how disparities are either worsening or dissipating. Another major limitation of this analysis is that the number of cases detected is partly a function of the number of tests that have been administered. In areas that lacked adequate testing capacity, case rates may appear lower than they actually are. We did not examine rural-urban classifications of counties even though there are specific susceptibilities to COVID-19 in rural versus urban places that could have warranted using rural-urban categorization; instead we use population density as a proxy for rural status. We did this because population density was a way to measure crowding in public spaces that may promote more opportunities for disease transmission, and we also accounted for household crowding in this analysis, which produced results similar to those of a national county-level analysis using these variables.31 Lastly, this model cannot reliably account for the variation in health behaviors that exist across counties such as Blacks being more likely to socially distance and rural populations being less likely to wear masks than urban populations.32
Conclusions
This study provides a snapshot of the landscape of COVID-19 disparities in Georgia in the first 7 weeks of the pandemic before the reopening of the state. It is the first study to model the independent associations of county sociodemographic and health system characteristics on COVID-19 cases and deaths in Georgia. We found two key factors to be associated with increased COVID-19 case and death rates in Georgia: the proportion of the Black population in a county and designation as a PCHPSA. These results are important because they highlight the impact of racial disparities on the spatial patterns of COVID-19 disease burden in Georgia in a data environment that has not prioritized or standardized the consistent collection of race/ethnicity in COVID-19 epidemiologic data. In addition, this study points to the potential importance of robust access to primary care in reducing mortality from COVID-19. This is especially important because many primary care practices across the country and state face dire financial and operational strain.33,34 These results can guide interventions to mitigate racial disparities in COVID-19 disease burden in Georgia and support the need for robust primary care infrastructure throughout the state.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://sma.org/smj).
P.B. has received compensation from the National Institutes of Health (National Center for Advancing Translational Sciences, National Institute on Minority Health and Health Disparities, and National Institute on Aging). L.C. has received compensation from Walden University.
The remaining authors did not report any financial relationships or conflicts of interest.
Contributor Information
Megan Douglas, Email: mdouglas@msm.edu.
Chaohua Li, Email: cli@msm.edu.
Lee S. Caplan, Email: lcaplan@msm.edu.
Mitchell Blount, Email: mblount@msm.edu.
Dominic Mack, Email: dmack@msm.edu.
Anne H. Gaglioti, Email: agaglioti@msm.edu.
References
- 1.Garg S Kim L Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suleyman G Fadel RA Malette KM, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open 2020;3:e2012270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The COVID Tracking Project. Home page. https://covidtracking.com/about-data. Accessed April 27, 2020.
- 4.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020;323:2466–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Curtice K, Choo E. Indigenous populations: left behind in the COVID-19 response. Lancet 2020;395:1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang CH, Schwartz GG. Spatial disparities in coronavirus incidence and mortality in the United States: an ecological analysis as of May 2020. J Rural Health 2020;36:433–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities 2020;7:398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yancy CW. COVID-19 and African Americans. JAMA 2020;323:1891–1892. [DOI] [PubMed] [Google Scholar]
- 9.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann NY Acad Sci 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 10.Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol 2015;11:407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health 2019;40:105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi L, Starfield B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am J Public Health 2001;91:1246–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83:457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moore JX Langston ME George V, et al. Epidemiology of the 2020 pandemic of COVID-19 in the state of Georgia: inadequate critical care resources and impact after 7 weeks of community spread. J Am Coll Emerg Physicians Open 2020;1:527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Renahy E Mitchell C Molnar A, et al. Connections between unemployment insurance, poverty and health: a systematic review. Eur J Public Health 2018;28:269–275. [DOI] [PubMed] [Google Scholar]
- 16.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health 2004;94:1675–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macinko J, Starfield B, Shi L. Quantifying the health benefits of primary care physician supply in the United States. Int J Health Serv 2007;37:111–126. [DOI] [PubMed] [Google Scholar]
- 18.Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health 2006;96:1300–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaglioti AH Douglas M Li C, et al. County-Level Proportion of Non-Hispanic Black Population is Associated with Increased County Confirmed COVID-19 Case Rates after Accounting for Poverty, Insurance Status, and Population Density. Atlanta, GA: National Center for Primary Care at Morehouse School of Medicine; 2020. [Google Scholar]
- 20.Johns Hopkins University & Medicine . COVID-19 United States cases by county. https://coronavirus.jhu.edu/us-map. Accessed May 1, 2020.
- 21.US Census Bureau . County population totals: 2010-2019. https://www.census.gov/data/datasets/time-series/demo/popest/2010s-counties-total.html.
- 22.data.HRSA.gov. Area Health Resources Files. https://data.hrsa.gov/topics/health-workforce/ahrf. Accessed May 1, 2020.
- 23.US Census Bureau . American Community Survey Data. https://www.census.gov/programs-surveys/acs/data.html. Accessed May 1, 2020.
- 24.Gupta S Hayek SS Wang W, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med 2020;180:e203596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basu S Berkowitz SA Phillips RL, et al. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med 2019;179:506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reynolds R Dennis S Hasan I, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 2018;19:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radley DC, Schoen C. Geographic variation in access to care—the relationship with quality. N Engl J Med 2012;367:3–6. [DOI] [PubMed] [Google Scholar]
- 28.Gruen RL, Campbell EG, Blumenthal D. Public roles of US physicians: community participation, political involvement, and collective advocacy. JAMA 2006;296:2467–2475. [DOI] [PubMed] [Google Scholar]
- 29.Campbell C Greenberg R Mankikar D, et al. A case study of environmental injustice: the failure in Flint. Int J Environ Res Public Health 2016;13:951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thakur N Lovinsky-Desir S Bime C, et al. The structural and social determinants of the racial/ethnic disparities in the US COVID-19 pandemic: what’s our role? Am J Respir Crit Care Med 2020;202:943–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Millett GA Jones AT Benkeser D, et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol 2020;47:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Czeisler M Tynan MA Howard ME, et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5-12, 2020. MMWR Morb Mortal Wkly Rep 2020;69:751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The Larry A. Green Center and Primary Care Collaborative . Primary care & COVID-19 survey: series 1-15 national executive summary. https://www.green-center.org/covid-survey. Accessed July 30, 2020.
- 34.Basu S Phillips RS Phillips R, et al. Primary care practice finances in the United States amid the COVID-19 pandemic: study estimates the potential impact of COVID-19 on operating expenses and revenues of primary care practices. Health Affairs (Millwood) 2020;39:1605–1614. [DOI] [PubMed] [Google Scholar]


