INTRODUCTION
The COVID-19 pandemic has accelerated the expansion of telemedicine, with healthcare systems substituting in-person for virtual visits.1 Yet, not all patients have equal access to these services, potentially widening healthcare disparities.2,3 One barrier to telemedicine services is digital access, defined as having technology at home that supports remote visits with healthcare providers. Older adults with serious illness may benefit most from telemedicine services: they require frequent doctors’ visits and leaving home can be challenging due to functional impairment. It is unknown if digital access has increased among those with serious illness as it has in the general population. We aim to compare digital access over time between older adults with and without serious illness using data from a nationally representative cohort study.
METHODS
We used the 2011–2017 National Health and Aging Trends Study (NHATS), a longitudinal study of Medicare enrollees that is linked to Medicare claims, wherein respondents are annually surveyed regarding their health, function, and technological environment. We included observations of respondents aged ≥70 who were enrolled in fee-for-service Medicare for 6 months prior to their NHATS interview. The primary outcome variable was digital access, defined as having a cellphone, computer, or tablet at home and knowing how to use the device. We defined serious illness using a validated combination of severe medical condition, functional impairment, and prior healthcare utilization.4 We used logistic regression to assess temporal trends in digital access with interview year as a continuous independent variable. All estimates were weighted to account for complex survey design and sampling approach. Respondents could have multiple observations, and we additionally adjusted for person-level clustering of data. As a sensitivity test, we assessed age-adjusted rates of digital access. This study was approved by the Mount Sinai Institutional Review Board.
RESULTS
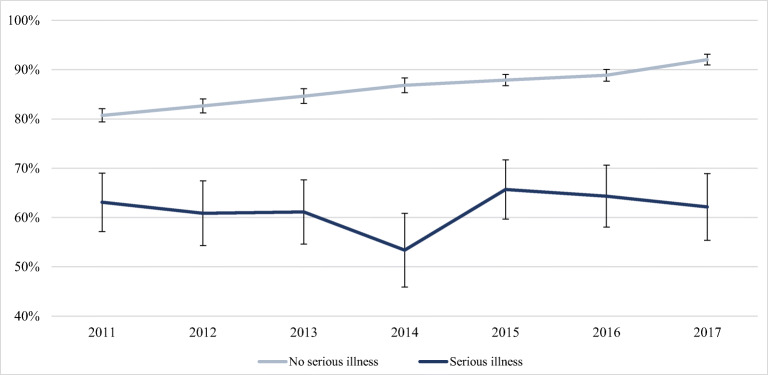
We identified 22,522 observations of 6813 unique older adults from 2011–2017, 8.0% with serious illness. Those with serious illness were older, had lower education and incomes, and were more likely to self-report poor health (p < 0.001). As compared to 20.2% of those without serious illness, 70.7% of those with serious illness were homebound, or never/rarely left home (p <0.001). They went online for all purposes less often (p < 0.001), including to contact medical providers and get information about health conditions (Table 1). While 84.3% of all observations reported digital access, this included 61.4% of those with serious illness as compared to 86.3% of those without serious illness (p<0.001). Rates of device ownership increased over time for those without serious illness (1.6% increase per year, 95% CI 1.4 to 1.9%) but did not increase for observations of those with serious illness (0.04% increase per year, 95% CI − 0.1 to 1.7%) (Fig. 1). When adjusting for age, the temporal trends observed persisted.
Table 1.
Characteristics of Older Adults With and Without Serious Illness (N=22,522)a
| No serious illness (n = 20,519) (%) |
Serious illnessb (n = 2003) (%) |
p valuec | |
|---|---|---|---|
| Proportion | 92.0 | 8.0 | |
| Demographic characteristics | |||
| Age, years | |||
| 70–74 | 41.2 | 21.7 | < .001 |
| 75–80 | 24.7 | 22.0 | |
| 80–85 | 18.1 | 21.5 | |
| 85+ | 16.1 | 34.9 | |
| Female | 56.5 | 62.9 | < .001 |
| Race/ethnicityd | |||
| White, non-Hispanic | 85.6 | 83.7 | .16 |
| Black, non-Hispanic | 6.7 | 8.5 | |
| Other, non-Hispanice | 3.3 | 3.0 | |
| Hispanic | 4.4 | 4.8 | |
| Married or lives with partner | 53.3 | 37.9 | <.001 |
| Lives alone | 34.5 | 48.2 | <.001 |
| College education or more | 28.9 | 17.9 | <.001 |
| Metropolitan region | 79.4 | 80.0 | .69 |
| Lowest income quartilef | 23.1 | 37.6 | < .001 |
| Medicaid | 11.4 | 25.8 | < .001 |
| Fair/poor self-reported health | 21.0 | 54.3 | <.001 |
| Homeboundg | 20.2 | 70.7 | < .001 |
| Digital access characteristics | |||
| Has and knows how to use the following: | |||
| Cellphone | 80.1 | 54.2 | < .001 |
| Computer | 63.0 | 38.5 | < .001 |
| Tableth | 33.0 | 19.1 | < .001 |
| Sends messages by email or textingi | 53.5 | 32.4 | < .001 |
| Goes online besides email and textingi | 44.9 | 66.1 | < .001 |
| Goes online to: | |||
| Shop for groceries or personal itemsi | 20.1 | 11.1 | < .001 |
| Pay bills or do bankingi | 25.9 | 12.5 | < .001 |
| Order or refill prescriptionsi | 12.4 | 6.3 | < .001 |
| Visit social network sitesi | 22.6 | 12.4 | < .001 |
| Contact medical providersj | 12.9 | 6.4 | < .001 |
| Handle health insurance mattersj | 7.5 | 3.6 | < .001 |
| Get information about health conditionsj | 21.7 | 12.0 | < .001 |
aData is presented as percentages, weighted to account for complex survey design
bSerious illness is defined as having at least one severe medical condition and/or functional impairment and at least one hospital admission in the last year and/or residing in a nursing home. Severe medical conditions include cancer, renal failure, dementia, advanced liver disease or cirrhosis, diabetes with severe complications, amyotrophic lateral sclerosis, acquired immune deficiency syndrome, hip fracture, chronic obstructive pulmonary disease or interstitial lung disease on oxygen or requiring hospitalization, and congestive heart failure requiring hospitalization4
cp values are from the univariate comparison
dData was collected by self-report
eCategory includes American Indian, Asian, Native Hawaiian, Pacific Islander, other, do not know, and more than 2 reported race/ethnicity categories
fIncome quartiles are for all Medicare beneficiaries
gHomebound is defined as leaving home never or rarely (1 time per week)
hThis question was first asked in wave 3 (2013–2014) of NHATS survey
iThese questions were asked over the timeframe of the “last month”
jThese questions were asked over the timeframe of the “last year”
Figure 1.
Percent of respondents with digital access by NHATS survey wave. Data source: National Health and Aging Trends Study, 2011–2017. Digital access is defined as having a cellphone, computer, or tablet at home and knowing how to use it. Serious illness is defined as having at least one severe medical condition and/or functional impairment and at least one hospital admission in the last year and/or residing in a nursing home. Severe medical conditions include cancer, renal failure, dementia, advanced liver disease or cirrhosis, diabetes with severe complications, amyotrophic lateral sclerosis, acquired immune deficiency syndrome, hip fracture, chronic obstructive pulmonary disease or interstitial lung disease on oxygen or requiring hospitalization, and congestive heart failure requiring hospitalization.4 Digital access for older adults without serious illness increased by 1.6% per year (95% CI 1.4 to 1.9%). Digital access did not increase for patients with serious illness (0.04% increase per year, 95% CI −0.1 to 1.7%). Error bars represent 95% confidence intervals. All proportions are adjusted for repeated measures, survey design, and sampling approach to be nationally representative of the population age ≥70 for that year.
DISCUSSION
We found large and widening gaps in digital access for older adults with serious illness compared to those without serious illness. While older adults with serious illness are demographically distinct, with older age and lower income, it is unclear why their device ownership has remained static over time while it has increased for older adults without serious illness. Nevertheless, these gaps are an important barrier to healthcare access.
While we do not directly measure how the COVID-19 pandemic impacted digital access, it is unlikely that the significant barriers for those with serious illness would have improved before or during the pandemic. In fact, given economic hardship and social isolation, we may find worsening digital access when pandemic data become available. As health systems expand telemedicine delivery, identification of patients without devices or internet is only the first step in improving access. Many older adults, including those with serious illness, will require support to navigate new technologies due to visual, auditory, or cognitive impairments.3 Individualized approaches, including in-home technical assistance and easy-to-use video applications, may overcome some barriers to telemedicine.5, 6 Furthermore, given existing gaps in digital access, insurers should reimburse telephonic visits equally to video to ensure that those with limited digital access are supported. For the promise of telemedicine to be equitably realized, we must engage the sickest patients.
Funding Sources
LPG – NIA K23AG049930, ASK – NIA K24AG062785, CKA — NIA 1K76AG064427-01A1
Declaration
Conflict of Interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Clancy CM, Kirsh S. Virtual Care and the Pandemic: Are We Reaching All Patients? Ann Intern Med. 2021;174(1):116-7. [DOI] [PMC free article] [PubMed]
- 2.Roberts ET, Mehrotra A. Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine. JAMA Intern Med. 2020;180(10):1386. doi: 10.1001/jamainternmed.2020.2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lam K, Lu AD, Shi Y, Covinsky KE. Assessing Telemedicine Unreadiness Among Older Adults in the United States During the COVID-19 Pandemic. JAMA Intern Med. 2020;180(10):1389. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelley AS, Covinsky KE, Gorges RJ, et al. Identifying Older Adults with Serious Illness: A Critical Step toward Improving the Value of Health Care. Health Serv Res. 2017;52(1):113–131. doi: 10.1111/1475-6773.12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nouri SS, Khoong EC, Lyles CR, Karliner LS. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. NEJM Catal. 2020;1-13. 10.1056/CAT.20.0123.
- 6.Levine DM, Lipsitz SR, Linder JA. Trends in Seniors’ Use of Digital Health Technology in the United States, 2011-2014. JAMA. 2016;316(5):538. doi: 10.1001/jama.2016.9124. [DOI] [PubMed] [Google Scholar]