Abstract
To evaluate the clinical efficiency, feasibility, and safety of computed tomography (CT)-guided trans-scapular coil localization (TSCL) approach to treating scapula-blocked pulmonary nodules (SBPNs).
In total, 105 patients with pulmonary nodules underwent CT-guided CL and subsequent video-assisted thoracoscopic surgery (VATS)-guided wedge resection (WR) between January 2016 and July 2020. Six of these patients (5.7%) had SBPNs that led them to undergo CT-guided TSCL. Rates of technical success and localization-related complications were then recorded and analyzed.
CT-guided TSCL was associated with a 100% technical success rate, with one coil being placed per patient. The median CT-guided TSCL duration was 15 min. No patients experienced any complications associated with this procedure, and subsequent VATS-guided WR of SBPNs was 100% technically successful. In two patients with invasive adenocarcinoma, additional lobectomy was performed. Median VATS duration and intraoperative blood loss were 120 min and 150 mL, respectively.
In summary, these results indicate that CT-guided TSCL could be easily and safely implemented to achieve high success rate when performing the VATS-guided WR of SBPNs.
Keywords: coil, localization, pulmonary nodule, scapular
1. Introduction
Computed tomography (CT)-guided localization has been frequently conducted prior to performing video-assisted thoracoscopic surgery (VATS)-guided wedge resection (WR) for pulmonary nodules (PNs), enabling successful localization in 89.6% to 100% of cases and facilitating successful WR in 97% to 100% of cases with relatively low rates of complications (8.8–12.6%).[1–4] Localization has previously been conducted using coils, methylene blue, hook-wire, or radio-labeling agents.[4] Coil localization (CL) is associated with lower complication rates than these other approaches.[4]
Owing to the advantages associated with this approach, CL is widely used in patients with sub-centimeter PNs, multiple PNs, and sub-fissural PNs.[5–7] While CT-guided lung interventions typically seek to avoid all bony structures, a subset of patients exhibit scapula-blocked PNs (SBPNs).[8–10] In these patients, the scapula must be penetrated when conducting these interventions in order to effectively evaluate and treat SBPNs.[8–10]
Herein, we explore the clinical efficiency, feasibility, and safety of a CT-guided trans-scapular CL (TSCL) approach for SBPNs.
2. Materials and methods
2.1. Study design
The Xuzhou Central Hospital ethics committee (members: Jing Yang, Pei-An Wang, Cong-Hui Han, Hai-Tao Yin, Xian-Chi Li, Bo Bi, Na Zhang, Li-Li Ma, Zhong-Mei Wu, and Xin-Xin Zhang) approved this retrospective study, which was consistent with the Declaration of Helsinki.
As this was a non-interventional retrospective study, the requirement for informed consent was waived. All data were anonymized after removing all personally identifiable data.
In total, 105 patients with PNs were treated via CT-guided CL followed by VATS-guided WR between January 2016 and July 2020, of whom 6 (5.7%) had SBPNs and underwent CT-guided TSCL (Table 1).
Table 1.
Baseline data of the 6 patients.
| Age (y)/Gender | BMI (kg/m2) | Co-morbid | Tumor history | Location | Nature | Diameter (mm) | Lesion-pleura distance (mm) | |
| 1 | 65/male | 23.7 | Mild cerebral infarction | No | Right upper | GGN | 7 | 4 |
| 2 | 50/male | 24.6 | None | No | Right upper | Solid | 8 | 8 |
| 3 | 66/female | 23.1 | None | No | Left upper | Mixed GGN | 18 | 6 |
| 4 | 45/female | 22.5 | None | No | Right upper | GGN | 5 | 0 |
| 5 | 70/female | 20.8 | Mild cerebral infarction | No | Left upper | Solid | 8 | 11 |
| 6 | 45/female | 25.2 | None | No | Left upper | GGN | 6 | 0 |
Inclusion criteria for this analysis were:
-
1.
PNs ≤ 3 cm in diameter, including ground-glass PNs ≤ 3 cm and solid PNs ≤ 1.5 cm;
-
2.
a PN-pleura distance ≤2 cm; and
-
3.
SBPNs for which no needle pathway was available that would enable avoidance of the scapula.
Exclusion criteria were:
-
1.
PNs < 5 mm in diameter;
-
2.
typical benign PNs, including calcifications and nodules that grew smaller upon follow-up; and
-
3.
patients with active bleeding, infections, abnormal coagulatory activity, or reduced cardiopulmonary reserves.
2.2. CT-guided TSCL
All CT-guided interventions were performed with a 16-slice CT device by a skilled radiologist with 14 years of experience performing interventional chest radiology procedures. Patients in the lateral or prone positions were given local anesthesia and directed to remain still and breathe regularly for the course of the procedure.
Preoperative CT scanning was performed to evaluate the needle passage. Scapular puncture was conducted with a 17G needle (DuoSmart, Modena, Italy) using a drill while steadily applying pressure. An 18G needle (Precisa, Roma, Italy) was then advanced coaxially via the 17G needle and gently advanced to the lung parenchyma to within 1 cm of the PN. A coil (length: 5-cm; diameter: 0.038 inches) (Cook, IN) was then advanced until it was almost within the lung parenchyma, and the needle was then removed so that the coil tail was still localized above the visceral pleura (Fig. 1).
Figure 1.
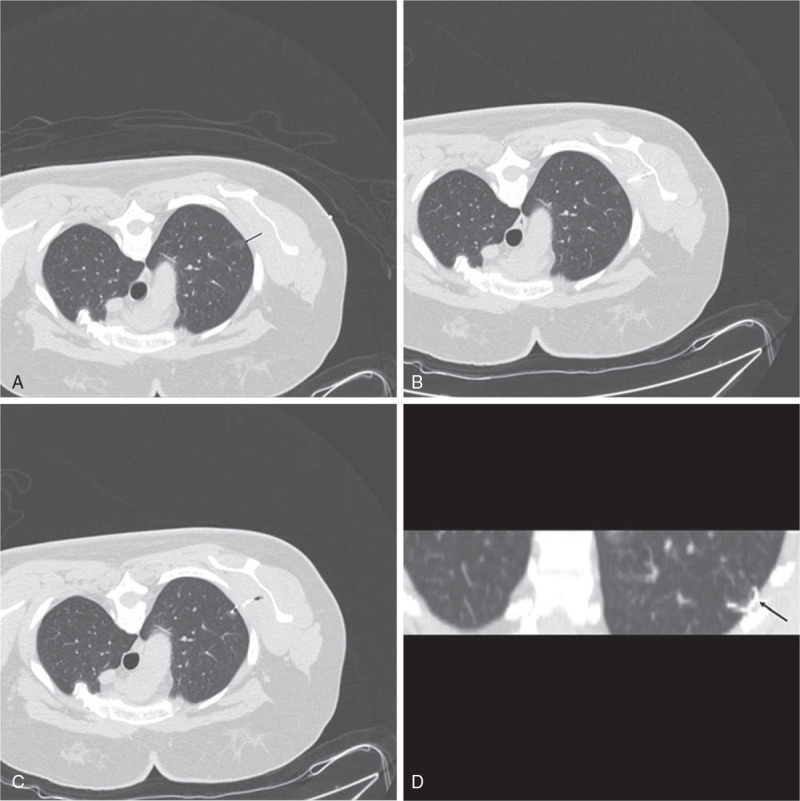
(A) A SBPN (ground glass nodule, arrow) was found in the left upper lobe. (B) The needle was punctured via the trans-scapula approach. (C) The coil was inserted for localization. (D) The coil tail (arrow) remained positioned above the visceral pleura.
Postoperative CT scanning was then conducted to assess patients for procedure-associated complications.
2.3. VATS-guided WR
VATS-guided WR was conducted within 24 h after TSCL, using the coil tail as a guide such that the edge of the resected area was ≥2 cm from the coil. When the coil tail was no longer visible, it was instead located via palpation. When coil tail localization was not possible, lobectomy was performed in lieu of the WR procedure.
High-speed pathological assessments of the resected lesion were performed in the Department of Pathology. In cases where LNs that experienced enhanced further than the mini-invasive adenocarcinoma level, excessive lymph and lobectomy dissection of node were executed.
2.4. Definitions
CT-guided TSCL was considered to be technically successful when the coil could be visualized upon VATS. WR was considered to be successful when the target nodule was located within the resected wedge of tissue.
2.5. Statistical analysis
SPSS v16.0 (SPSS, Inc, IL) was employed for all statistical testing. Quantitative data are given as medians, while categorical data are percentages (number/total).
3. Results
3.1. Baseline data
This study included 6 patients (4 female, 2 male) with a median age of 57.5 years who were treated via this approach (Table 1). Each patient had a single SBPN located behind the central portion of the scapula. These lesions had a median diameter of 7.5 mm and a median lesion-pleura distance of 5 mm. None of these patients had any history of cancer, while two had experienced mild cerebral infarction.
3.2. Localization procedures
CT-guided TSCL was technically successful in 100% of patients. The median duration of CT-guided TSCL was 15 min. A single coil was placed in all patients, and no procedure-related complications were reported (Table 2).
Table 2.
Details of CT-guided coil localization.
| Technical success | Patients’ position | Duration (min) | Complication | |
| 1 | Yes | Prone | 12 | None |
| 2 | Yes | Prone | 20 | None |
| 3 | Yes | Prone | 14 | None |
| 4 | Yes | Prone | 13 | None |
| 5 | Yes | Prone | 16 | None |
| 6 | Yes | Prone | 18 | None |
3.3. VATS procedures
The VATS-guided WR of SBPNs was technically successful in 100% of patients (Table 3). Subsequent lobectomy was conducted in two of these patients owing to the diagnosis of invasive adenocarcinoma. The median VATS duration and intraoperative blood loss were 120 min and 150 mL, respectively. Resected SBPNs were diagnosed as adenocarcinoma (T1N0M0, n = 2) and adenocarcinoma in situ (n = 4).
Table 3.
Details of VATS.
| Successful wedge resection | Additional lobectomy | Duration (min) | Blood loss (mL) | Diagnosis | |
| 1 | Yes | No | 60 | 25 | AIS |
| 2 | Yes | Yes | 270 | 200 | Adenocarcinoma |
| 3 | Yes | Yes | 220 | 200 | Adenocarcinoma |
| 4 | Yes | No | 120 | 200 | AIS |
| 5 | Yes | No | 60 | 50 | AIS |
| 6 | Yes | No | 120 | 100 | AIS |
4. Discussion
Herein, we detailed our clinical experience performing CT-guided TSCL for SBPNs. When conducting CT-guided lung interventional procedures, bony structures have the potential to obstruct the needle pathway.[8–10] Typically, avoiding these bones is considered to be the optimal approach. However, when a viable pathway is not available, it is instead considered acceptable to conduct a trans-bone approach. Herein, we achieved a 100% rate of technical success when performing CT-guided TSCL for SBPNs, in line with similarly high rates that have previously been reported in other studies about CT-guided trans-bone lung interventional procedures (91–100%).[8–10]
When performing CT-guided lung biopsy, a number of potentially acceptable alternative needle pathways need to be evaluated when the most direct pathway is occluded by bone, even though these pathways are likely to increase the pleura–lesion distance. In contrast to biopsy approaches, however, the CL of PNs is intended to facilitate high technical success rates when conducting VATS-guided WR.[1] It is thus important that the coil body by localized proximal to the PN, while the coil tail remains above the pleural surface as near the lesion as possible. Minimizing the pleura-lesion distance is therefore essential to facilitate effective CT-guided CL. As such, a trans-scapular approach was selected in the present study for cases wherein the optimal needle pathway was blocked by the scapula.
No patients exhibited any TSCL-related complications. However, this finding may be attributable to our small study size, given that in prior studies the rates of complications associated with CT-guided localization ranged from 9% to 12.3%,[1–3] and prior studies of the CT-guided trans-scapular biopsy approach reported complication rates of 18.2% to 25%.[8,10]
VATS-guided WR was performed successfully for all patients in this study. In line with results pertaining to most other preoperative CT-guided localization strategies,[1–3] preoperative CT-guided TSCL is capable of achieving high rates of WR success when evaluating SBPNs without compromising pulmonary function.
This study has multiple limitations. For one, it was a single-center retrospective study and thus potentially susceptible to selection bias. Our sample size was also very small, so additional work will be required to validate our conclusions. Furthermore, we did not include a control group in this study. Even so, as this is a specialized technique which is only used when treating a very limited number of specific patients, we believe these data support it being a safe and feasible approach. Lastly, this technique only applies to the sub-pleural PNs. Thus, it cannot be used for the deeper PNs.
In summary, CT-guided TSCL can be conducted to easily and safely achieve high success rates when performing the VATS-guided WR of SBPNs. However, this technique is not suit for the deeper SBPNs.
Author contributions
Data curation: Xia Liu, Wei Cao.
Funding acquisition: Qing-Song Xu.
Methodology: Wei Cao.
Supervision: Qing-Song Xu.
Writing – original draft: Xia Liu.
Writing – review & editing: Qing-Song Xu.
Footnotes
Abbreviations: CL = coil localization, CT = computed tomography, PN = pulmonary nodule, SBPN = scapular-blocked PN, TSCL = trans-scapular CL, VATS = video-assisted thoracoscopic surgery, WR = wedge resection.
How to cite this article: Liu X, Cao W, Xu QS. Computed tomography-guided coil localization for scapula-blocked pulmonary nodules: A trans-scapular approach. Medicine. 2021;100:5(e24333).
Program of 2019 Xuzhou clinical technique research (2109GG002).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
BMI = body mass index, GGN = ground glass nodule.
CT = computed tomography.
AIS = adenocarcinoma in situ, VATS = video-assisted thoracoscopic surgery.
References
- [1].Fu YF, Zhang M, Wu WB, et al. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A 2018;28:292–7. [DOI] [PubMed] [Google Scholar]
- [2].Gruber-Rouh T, Naguib NNN, Beeres M, et al. CT-guided hook-wire localisation prior to video-assisted thoracoscopic surgery of pulmonary lesions. Clin Radiol 2017;72: 898.e7-11. [DOI] [PubMed] [Google Scholar]
- [3].Findik G, Demiröz SM, Apaydin SMK, et al. Computed tomography-guided methylene blue labeling prior to thoracoscopic resection of small deeply placed pulmonary nodules. Do we really need palpation? Thorac Cardiovasc Surg 2017;65:387–91. [DOI] [PubMed] [Google Scholar]
- [4].Park CH, Han K, Hur J, et al. Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules: a systematic review and meta-analysis. Chest 2017;151:316–28. [DOI] [PubMed] [Google Scholar]
- [5].Xia FF, Shi YB, Wang T, et al. Computed tomography-guided transfissural coil localization of lung nodules. Thorac Cardiovasc Surg 2019;68:545–8. [DOI] [PubMed] [Google Scholar]
- [6].Teng F, Wu AL, Yang S, et al. Preoperative computed tomography-guided coil localization for multiple lung nodules. Ther Adv Respir Dis 2020;14:1753466620909762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Refai M, Andolfi M, Barbisan F, et al. Computed tomography-guided microcoil placement for localizing small pulmonary nodules before uniportal video-assisted thoracoscopic resection. Radiol Med 2020;125:24–30. [DOI] [PubMed] [Google Scholar]
- [8].Rossi UG, Seitun S, Ferro C. MDCT-guided transthoracic needle aspiration biopsy of the lung using the transscapular approach. Cardiovasc Intervent Radiol 2011;34:184–7. [DOI] [PubMed] [Google Scholar]
- [9].Iguchi T, Hiraki T, Ishii H, et al. Transosseous route for CT fluoroscopy-guided radiofrequency ablation of lung tumors. J Vasc Interv Radiol 2015;26:1694–8. [DOI] [PubMed] [Google Scholar]
- [10].Rebonato A, Maiettini D, Andolfi M, et al. CT-guided percutaneous trans-scapular lung biopsy in the diagnosis of peripheral pulmonary lesion nodules of the superior lobes using large needles. Cardiovasc Intervent Radiol 2018;41:284–90. [DOI] [PubMed] [Google Scholar]


