Abstract
Foodborne pathogens cause diseases and death, increasing the economic burden. It needs to identify incident places, media food and pathgens. Our aim is to survey empirical data that provide a retrospective historical perspective on foodborne diseases and explore the causes and trends of outbreaks.
We examined publicly available annual summary data on reported foodborne disease outbreaks in Taiwan from 2014 to 2018. We calculated the percentage of places, media food, bacteria and natural toxin sources in foodborne diseases and performed a chi-square test for difference evaluation. The higher risk of places and causes in 2018 compared with 2014 was empolyzed with univariate logistic regression.
There were 26847 patients with foodborne diseases during the period from 2014 to 2018. The top 2 primary source locations of the foodborne diseases were schools and restaurants. The top 2 primary food media classifications of the foodborne diseases were boxed meals and compounded foods. The top 2 primary incident bacterial classifications of the observed foodborne diseases were Bacillus cereus and Staphylococcus aureus. The top 2 primary natural toxin classifications of the foodborne diseases were plants and histamines. The incidence of foodborne disease in military facilities, fruits and vegetables, and Staphylococcus aureus was increased in our study.
Our study confirmed the high risk and increased incidence of foodborne diseases, food media classifications, bacterial classifications, and natural toxins in Taiwan. It is worthy of attention for the government health department-designed policy to promote disease prevention.
Keywords: foodborne diseases, outbreak, surveillance
1. Introduction
In 2015, the World Health Organization published a forecast of the global impact of foodborne diseases based on 2010 data.[1] The data showed that there are approximately 600 million cases of foodborne disease and 420,000 related deaths every year due to 31 major known pathogens.[2] Approximately 9.4 million cases of foodborne disease are estimated to occur every year in the United States.[3] Although foodborne disease is rarely associated with established disease outbreaks,[4] the data collected during the outbreak investigation can be used to confirm the mediators and pathogens that cause the disease, highlighting the vulnerability of the food delivery system. Once this vulnerability is confirmed, public health officials and supervisory agencies can design targeted interventions to reduce the risk of food contamination during production and distribution.[4,5]
Foodborne diseases in contaminated foods are monitored in many countries because they are a major cause of morbidity and mortality and impact economic burden.[6–8] Foodborne diseases are defined as diseases that “result from the ingestion of contaminated foods and food products and include a broad range of illnesses caused by parasites, chemicals and pathogens which contaminate food at different points in the food production and preparation process.”[9] The foodborne disease surveillance system aims to reduce the burden of disease by monitoring disease trends, estimating burden, identifying and controlling outbreaks, identifying high-risk foods and poor food preparation practices, identifying vulnerable groups, identifying foodborne routes of specific pathogens, evaluating food safety programmes, and providing information and empirical medical evidence to help decision makers develop public health precautions.[10]
Approximately 500 foodborne disease events occurred every year.[11] The number of actual cases is often several times higher than the number of reported cases; people need to pay more attention to food hygiene. The pathogenic causes of foodborne diseases vary due to different eating places and eating habits.[12] The proportion of outdoor food consumption is increasing rapidly and, in turn, increases the chance of pathogenic microorganisms with improper storage.[12,13] Since 2007, the Public Health Service of the Food and Drug Administration of Taiwan's Ministry of Health and Welfare has begun to publish a summary of the food contamination epidemic. From this dataset, the collection and reporting of foodborne disease outbreaks have indicated in terms of type, quantity, completeness, timeliness and comprehensiveness.[11] The purposes of this study are to validate the empirical data of the Taiwanese Food-Borne Disease Surveillance Reporting System over the past 5 years, to provide a retrospective historical perspective of foodborne diseases and to explore the causes and trends of epidemiological changes that cause outbreaks of disease.
2. Methods
2.1. Data source
We examined publicly available annual summary data on reported Foodborne disease outbreaks in Taiwan from 2014 to 2018.[11] The total number of foodborne outbreaks reported annually included all outbreaks due to seafood, meat, egg products, other sources (which included any other known food), or unknown sources. The outbreak settings were determined based on the places where the food was eaten (2014–2018), depending on the data available during those periods. Setting was categorized as restaurants (which included cafeterias, delicatessens, or any restaurant subtype), home (which included the patient's home or a private residence), other (which included any other known setting), or unknown. The outbreak factors of food media were classified as seafood, aquatic processing, meat and processed meat products, eggand processed egg products, cereals and processed cereal products, fruits and vegetables and their processed products, cakes and candy, boxed meals, and compounded foods. The outbreak aetiologic factors were classified as bacterial pathogens, chemicals, natural toxins, or unknown. When data were available, the aetiology was further classified by pathogen, including Vibrio vulnificus, Salmonella, enteropathogenic Escherichia coli, Staphylococcus aureus, Bacillus cereus, and Clostridium botulinum (botulism). The unknown food media classification and unknown cause classification were excluded. The higher risk of places and causes about foodborne disease in 2018 compared with first year of this study performed by logistic regression, the data of places and causes about foodborne disease in 2014 was used as control. The flowchart of this study is shown in Figure 1.
Figure 1.
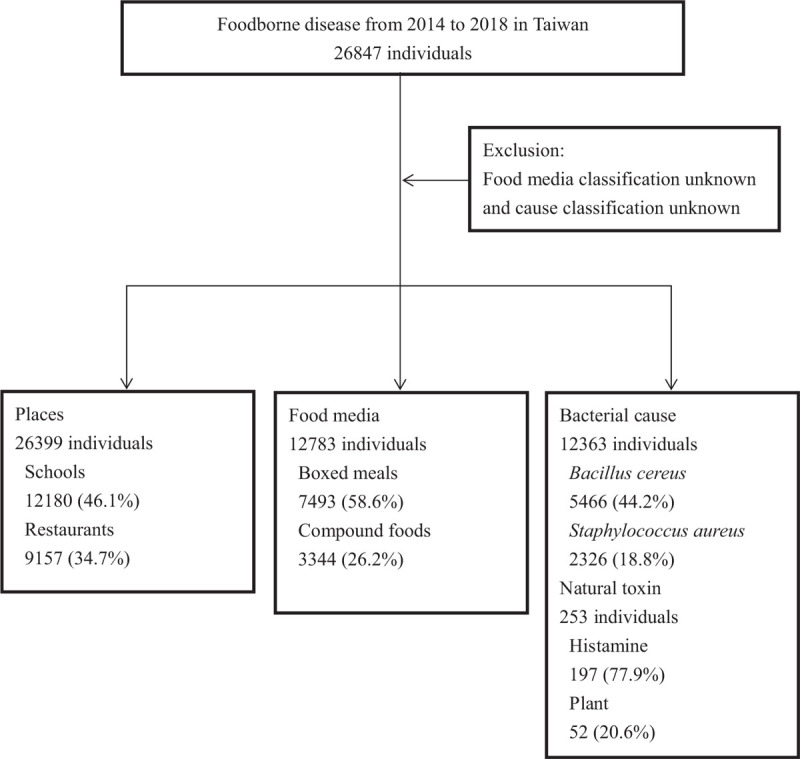
The flowchart of this study.
This study that does not require ethical approval includes those involving information freely available in the public domain and the analysis of open dataset sources, where the data are properly anonymised.
2.2. Statistical analyses
We calculated the percentage of foodborne disease outbreaks and outbreak-associated illnesses relative to all foodborne disease outbreaks. Chi-square tests were 2-sided, with a significance threshold of P < .05. The higher risk of places and causes in 2018 compared with 2014 were identified by crude odds ratio (OR) using univariate logistic regression without adjusting for other factors to evaluate the risk because individual data were unavailable. The analysis used IBM SPSS version 22 (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Released 2013).
3. Results
There were 26,847 patients, and no deaths were assessed by the public health service department website of the Welfare Food and Drug Administration during the period from 2014 to 2018. The classification of the places of food consumption was conducted. The top 2 places of foodborne disease were shools and restaurants. There was a significant difference in cases classified by place of foodborne disease from 2014 to 2018 (P < .001). (Table 1)
Table 1.
The places of foodborne disease acquisition from 2014 to 2018 in Taiwan.
| Places | Total 26399 | 2014 (4426) | 2015 (6166) | 2016 (5171) | 2017 (6181) | 2018 (4455) | P |
| Home | 1166 | 198 (4.5%) | 192 (3.1%) | 423 (8.2%) | 199 (3.2%) | 154 (3.5%) | <.001 |
| Restaurant | 9157 | 1,245 (28.1%) | 2,774 (45.0%) | 1,638 (31.7%) | 2,441 (39.5%) | 1,059 (23.8%) | |
| School | 12180 | 1,994 (45.1%) | 2,525 (41.0%) | 2,499 (48.3%) | 2,677 (43.3%) | 2,485 (55.8%) | |
| Office | 1559 | 635 (14.3%) | 191 (3.1%) | 95 (1.8%) | 191 (3.1%) | 447 (10.0%) | |
| Hospital | 234 | 36 (0.8%) | 87 (1.4%) | 50 (1.0%) | 37 (0.6%) | 24 (0.5%) | |
| Transportation vehicles | 64 | 0 (0%) | 34 (0.6%) | 17 (0.3%) | 6 (0.1%) | 7 (0.2%) | |
| Military facilities | 784 | 68 (1.5%) | 36 (0.6%) | 94 (1.8%) | 390 (6.3%) | 196 (4.4%) | |
| Outdoor | 167 | 10 (0.2%) | 8 (0.1%) | 105 (2.0%) | 17 (0.3%) | 27 (0.6%) | |
| Vendors | 409 | 74 (1.7%) | 89 (1.4%) | 155 (3.0%) | 55 (0.9%) | 36 (0.8%) | |
| Exterior | 324 | 85 (1.9%) | 129 (2.1%) | 81 (1.6%) | 25 (0.4%) | 4 (0.1%) | |
| Prison | 355 | 81 (1.8%) | 101 (1.6%) | 14 (0.3%) | 143 (2.3%) | 16 (0.4%) |
The primary top 2 food media classifications of incident foodborne diseases were boxed meals and compounded foods. (Table 2) The incidence decreased in seafood and increased in fruits and vegetables and their processed products compared in 2018 with the rates in 2014. In our study, the cases classified by food media of foodborne disease with contamination rates varied and were significantly different from 2014 to 2018 (P < .001).
Table 2.
The food media of foodborne diseases from 2014 to 2018 in Taiwan.
| Food media | Total 12783 | 2014 (2103) | 2015 (2257) | 2016 (2472) | 2017 (3523) | 2018 (2428) | P |
| Seafood | 744 | 206 (9.8%) | 287 (12.7%) | 189 (7.6%) | 56 (1.6%) | 6 (0.2%) | <.001 |
| Aquatic processing | 45 | 2 (0.1%) | 7 (0.3%) | 4 (0.2%) | 9 (0.3%) | 23 (0.9%) | |
| Meat and processed meat products | 218 | 33 (1.6%) | 7 (0.3%) | 157 (6.4%) | 19 (0.5%) | 2 (0.1%) | |
| Eggs and processed egg products | 374 | 62 (2.9%) | 135 (6.0%) | 131 (5.3%) | 0 (0%) | 46 (1.9%) | |
| Cereals and processed cereal products | 174 | 48 (2.3%) | 26 (1.2%) | 0 (0%) | 100 (2.8%) | 0 (0%) | |
| Fruits and vegetables and their processed products | 326 | 13 (0.6%) | 37 (1.6%) | 8 (0.3%) | 130 (3.7%) | 138 (5.7%) | |
| Cakes, candy | 65 | 14 (0.7%) | 14 (0.6%) | 35 (1.4%) | 0 (0%) | 2 (0.1%) | |
| Boxed meals | 7493 | 1130 (53.7%) | 954 (42.3%) | 1553 (62.8%) | 1909 (54.2%) | 1947 (80.2%) | |
| Compounded foods | 3344 | 595 (28.3%) | 790 (35.0%) | 395 (16.0%) | 1300 (36.9%) | 264 (10.9%) |
The primary bacterial classifications responsible for the observed incident foodborne diseases were Bacillus cereus, Staphylococcus aureus, enteropathogenic Escherichia coli, and Salmonella. The incidence of Bacillus cereus, Staphylococcus aureus and enteropathogenic Escherichia coli increased in 2018 compared with the rates in 2014. The incidence rates of Vibrio vulnificus and Salmonella were reduced in 2018 compared with the rates in 2014. Our study found varied bacterial food media infections from 2014 to 2018 (P < .001). (Table 3) The primary natural toxin classifications associated with incident foodborne diseases were plants and histamines. The cases of natural toxins in food poisoning were indeed different from 2014 to 2018, with statistically significant differences (P < .001). (Table 4)
Table 3.
The bacterial causes of foodborne diseases from 2014 to 2018 in Taiwan.
| Bacterial causes | Total 12363 | 2014 (2368) | 2015 (1725) | 2016 (1916) | 2017 (2614) | 2018 (3740) | P |
| Vibrio vulnificus | 995 | 565 (23.9%) | 177 (10.3%) | 71 (3.7%) | 132 (5.0%) | 10 (0.3%) | <.001 |
| Salmonella | 1733 | 649 (27.4%) | 294 (17.0%) | 341 (17.8%) | 235 (8.9%) | 214 (5.7%) | |
| Enteropathogenic Escherichia coli | 1875 | 183 (7.7%) | 49 (2.8%) | 50 (2.6%) | 979 (37.5%) | 614 (16.4%) | |
| Staphylococcus aureus | 2326 | 356 (15.0%) | 369 (21.4%) | 191 (10.0%) | 140 (5.4%) | 1270 (34.0%) | |
| Bacillus cereus | 5466 | 615 (26.0%) | 834 (48.3%) | 1257 (65.6%) | 1128 (43.2%) | 1632 (43.6%) | |
| Botox | 8 | 0 (0%) | 2 (0.1%) | 6 (0.3%) | 0 (0%) | 0 (0%) |
Table 4.
The natural toxin causes of foodborne diseases from 2014 to 2018 in Taiwan.
| Natural toxin | Total 253 | 2014 (173) | 2015 (22) | 2016 (8) | 2017 (22) | 2018 (28) | P |
| Plant | 52 | 9 (5.2%) | 15 (68.2%) | 8 (100%) | 13 (59.1%) | 7 (25%) | <.001 |
| Histamine | 197 | 160 (92.5%) | 7 (31.8%) | 0 (0%) | 9 (40.9%) | 21 (75%) | |
| Puffer poison | 4 | 4 (2.3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
We surveyed the higher risk of foodbornde disease in 2018 compared with 2014 in places, food media, bacterial causes and natural toxin causes. The crude OR was 1.539 (95% confidence interval [CI]: 1.415–1.673, P < .001) in school, 2.949 (95% CI: 2.231–3.899, P < .001) in military facilities, 2.693 (95% CI: 1.302–5.57, P = .008) outdoors. The crude OR was 9.688 (95% CI: 5.47–17.161, P < .001) by fruit and vegetables and their processed products, 3.163 (95% CI: 2.769–3.613, P < .001) by boxed meals. The crude OR was 2.345 (95% CI:1.971–2.791, P < .001) by Escherichia coli, 2.906 (95% CI:2.548–3.314, P < .001) by Staphylococcus aureus, 2.207 (95% CI: 1.972–2.469, P < .001) by Bacillus cereus. The crude OR was 6.074 (95% CI:2.048–18.015, P = .001) by plants.
4. Discussion
According to the Food and Drug Statistics Monitoring Network of the Ministry of Health and Welfare of Taiwan in 2019, there are at least 300 foodborne disease events every year, affecting more than 4500 patients and no deaths. The foodborne cases had different empirical data due to different places of food consumption, media foods and pathogenic aetiologies. These historical retrospective data were properly summarized and statistically analysed; these results allow appropriate inferences about epidemiological characteristics of the causes and trends of foodborne disease in the public health or clinical set.
The top 2 places of foodborne disease were schools and restaurants from 2014 to 2018. This outcome is similar to the findings from the literature.[12] The nutritious lunch was provided in elementary school, and boxed meals were provided for high school. The potential reasons were inappropriate food stores and bacteria contaminated by dietary staff. Foodborne disease occurred in restaurants, hotels, ice fruit rooms, and bakeries. The possible reasons include food manufacturers or practitioners who suffered from upper respiratory tract diseases or wound infection during the period of food production, or the food industry provided foods contaminated with pathogenic organisms.[14] The palce of foodborne disease occurred in the home, and the possible reasons included eating leftovers from restaurants at home, insufficient storage temperature, or cross-contamination between raw and cooked foods. There was a negative relationship between the events of foodborne disease (see Table, Suppplement Content, which illustrates the higher rate of events occurring in restaurants) and the number of individuals in the restaurants and schools; this relationship possibly occurs because there are more restaurants estibilished than schools. The number of consumers is lower in restaurants than in schools, which reflects and is consistent with the social phenomenon in Taiwan. The majority of foodborne diseases occurred in the restaurants, but the impact on the people infected in the school was more serious, as these events resulted in outbreaks of disease in homes or offices. It is more obvious that the food poisoning process may involve a group infection caused by eating the same contaminated foods in the same place. Our study showed that the rate of foodborne disease from vendors declined year by year with government improved health habits and environments, and the rate of foodborne disease in military units increased year by year in the past 3 years. The advanced management policy for vendors had benefits for the prevention of foodborne disease and promoted hyiene education and training for dietary staff in militaty units.
Foodborne disease was caused by eating the same infectious food, indicating the importance of proper food handling and hygiene, as well as the understanding of food classification.[13] From 2014 to 2018, the cases of foodborne disease were the highest for boxed meals, followed by compounded foods. The boxed meals were unique to Chinese diet behaviours for lunch and dinner, and compounded foods were eaten for breakfast in Taiwan. The compounded foods and aquatic products were likely to cause foodborne disease outbreaks, as seen in past studies.[15,16] We infer that this outcome reflects the high proportion of eating food outside in Taiwan; the majority of eating outside involved the consumption of boxed meals, which directly cause food poisoning. In addition, the cases caused by fruits and vegetables and their processed products increased significantly. Because of changes in dietary habits for advanced health conditions, people have increased their intake of fruits and vegetables containing abundant vitamins B and C in recent years. These results show that fruits and vegetables and their processed products are a new type of foodborne disease food media in Taiwan. More attention needs to be paid to educating factories on the storage and processing of fruit and vegetable products in the future. The government health department should propose preventive measures and monitors. Food handlers must support preservation methods to avoid bacterial breeding.
Media foods are poisoned with pathogenic bacteria, chemicals or natural toxins. Bacterial foodborne disease cases mainly include Vibrio vulnificus, Staphylococcus aureus, pathogenic Escherichia coli, Bacillus cereus and Salmonella.[13] The majority of the bacterial pathogens resulted in collective infections and outbreaks through human transmission. According to a past study, shellfish products such as oysters and clams are susceptible to contamination by Vibrio vulnificus or other pathogens in the growing environment. Ingestion of shellfish from contaminated waters often causes vomiting, abdominal pain, and diarrhoea, and some patients are more likely to have fever, which may cause the spread of foodborne disease.[17] Important pathogenic infections are often the main cause of large-scale foodborne disease outbreaks. Previous studies have found that Salmonella, which is common in food poisoning cases in many countries, usually comes from infected chickens and eggs, while raw eggs and plates that are not properly cleaned are accidentally contaminated with Salmonella, increasing the chance of infection.[18,19] In food poisoning cases, there may be different distributions depending on the type of food. For example, improper storage of poultry, meat, rice and processed products may cause the growth of Bacillus ceretus and its toxins.[20] The pathogenic infections with the highest proportion of cases were Salmonella in 2014 and Bacillus cereus from 2015 to 2018. Vibrio vulnificus and Salmonella infections declined over the study period, which may be related to the increase in education regarding cooked seafood and eggs by health departments. The potential reason for this discrepancy was that Vibrio vulnificus and Staphylococcus aureus have higher infectivity than other pathogens despite only affecting a small number of patients; the number of Salmonella and Bacillus cereus cases was relatively high compared with the number of events. The findings were similar to those of a previous study.[13] The comparative relationship of the pathogenicity of food poisoning is worthy of attention from infectious disease experts for future clinical adjustment. The bacterial foodborne diseases occurred during warmer months in Taiwan.[21] The causes of foodborne disease by Staphylococcus aureus were the contamination with unhygienic conditions during food preparation, processing, and transferring stages. The enterotoxin secreting by Staphylococcus aureus with heat resistant characteristics were removed difficultly by cooking.[22] The prevalence of Staphylococcus aureus in the chicken eggshell surface was 10.45% in past study.[23] The previous survey found the highest incidence rate of ready to eat foods by Staphylococcus aureus was 20.5% in fresh-cut fruit.[24] The Staphylococcus aureus could not grow during 4°C in ready to eat food.[25] The significantly increased the incidents of foodborne diseases were noted in offices, food media by aquatic processing, egg and processed egg products, slightly increased in fruit or vegetable products and boxed meals between years 2017–2018 (Tables 1 and 2). There was a spiking incident of Staphlococcus aureus between years 2017 to 2018, the potential reasons were the higher ambient temperature during summer cause more cases of bacterial foodborne diseases (Table 3), the event of food safety with contaminated egg liquid without cold chain maintained[26] and ready to eat foods with incomplete refrigerated. Dietary staff should pay attention to wound care and education to avoid contact with food without gloves and encourage the separation of raw and cooked food.
The source of food poisoning by chemical substances is mainly pesticides or heavy metals. The official monitoring data were unavailable in Taiwan from 2014 to 2018, and it was impossible to determine the epidemiological significance. Food poisoning caused by natural toxins[27] is mainly based on plants and histamines.[28] The main causes of poisoning by ingestion of natural plant toxins are as follows:
-
(1)
Edible or medicinal poisoning, such as adverse reactions caused by ingestion of germinated potatoes. Plants such as almonds and ginkgo that are ingested or supplemented with excessive amounts of natural toxins may also be poisoned.
-
(2)
Ingestion of toxic plants with a similar appearance to food, such as edible large wild donkeys, or the mistaken collection of poisonous herbs.
The cases of natural toxins were highest for plant toxins. The cases of histamine toxicity were higher than the cases of poisoning from other natural toxins in 2014 and 2018, and the cases of poisoning by other plant-based natural toxins were higher from 2015 to 2017. The cases of natural toxin poisoning were caused by food contamination or accidential ingestion, and most of them were isolated cases.
Foodborne disease outbreaks could influence productivity, tourism and trade by healthcare system stress. In the frequently interconnective world, local foodborne disease outbreaks will become a potential threat to the entire globe across the national border. Human-to-human infectious diseases are often spread through international tourism and seriously incur the health problem of the population. There were tons of international travellers who visited Taiwan every year, including 8,923,902 visitors from Asia, 766,254 from the Americas, 386,752 from Europe and 134,860 from Oceania in 2019.[29] Therefore, displaing of the recent epidemic characteristics of food poisoning in Taiwan provided foodborne disease awareness and useful epidemic information to prevent food infectious diseases during visiting periods.
Food safety is the focus of public health and social concern of livelihood. It is the most critical issue across the entire world to keep people away from the risks of poisons and diseases, improving nutrition and health promotion. Therefore, the government performed cross-domain management, including food quality inspection, monitoring, proper treatment, packaging, and preservation of foods with international regulations and standards, industrial self-discipline, and private participation to achieve food security.[30] The biotechnological strategies such as agricultural genome editing, ribonucleic acid spraying technology enhance disease-resistant production of food, crop, and grain. Also, these strategies raise food production and ensuring food security, nutritional value, prevent plant-based foodborne illnesses, and bioremediation, and environmental conservation.[31,32] The government needs to strengthen international cooperation to promote sustainable agriculture and eliminate hunger.
It is useful for annual summaries released by the government agency, but it needs to explore the change and meanings. We used statistical methods from public information to explore the epidemiological and trends of foodbornr disease within 5 years. Our study was convinced that the added value did not exceed the scope of public information. However, we identified empirical medical evidence and provided epidemiological knowledge for the prevention and control of foodborne disease.
5. Limitations
There are some limitations in this study. First, the monitoring values had a higher proportion of unidentified categories of media food, and only half of the cases of all datasets were reported from bacterial sources in our study. However, it does not affect the observation worth about foodbrone diseases. Second, there were unavailable viral or parasitic pathogenic infectious and chemical substances with incomplete information. This suggests that the government must collect more detailed pathological causes of foodborne disease with in-depth analysis. Third, if foodborne disease occurred with more than 2 patients in the same place, the medical institutions needed to report the breakout of foodborne disease. We used the reported data from the Ministry of Health and Welfare of Taiwan, it included the whole reported population of Taiwan. It is relatively convenient to seek medical help in Taiwan and some patients searched for medical treatment individually without involvement. Patients with gastrointestinal upset can seek medical treatment by themselves without reporting to the government department, which may underestimate the prevalence of foodborne diseases.
6. Conclusions
To our knowledge, this is the first study to explore the epidemiological characteristics of foodborne disease outbreaks over 5 years using the government's open dataset in Taiwan to address recent data gaps. The rate of foodborne disease showed an increasing trend year by year in military facilities, in the infection of fruits and vegetables and their processed foods and in pathogenic bacteria Bacillus cereus and a decreasing trend in Vibrio vulnificus and Salmonella infections. Gastrointestinal symptoms are common features of foodborne disease, and the association between air temperature or pollution and diarrhea is worthy of exploring in the future. It is recommended that government departments continue to develop optimal laboratory techniques and diagnostic standards to increase complete epidemiological characteristics and to track the risk factors.
Author contributions
Conceptualization: Chia-Peng Yu, Chun-An Cheng.
Data curation: Chia-Peng Yu.
Formal analysis: Chia-Peng Yu.
Funding acquisition: Ding-Chung Wu.
Investigation: Chun-Gu Cheng, Chun-An Cheng.
Methodology: Yu-Ching Chou.
Project administration: Ding-Chung Wu, Chun-Gu Cheng.
Software: Yu-Ching Chou.
Supervision: Chun-An Cheng.
Validation: Yu-Ching Chou.
Visualization: Ding-Chung Wu, Chun-Gu Cheng.
Writing – original draft: Chia-Peng Yu.
Writing – review & editing: Chun-Gu Cheng, Chun-An Cheng.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, OR = odds ratio.
How to cite this article: Yu CP, Chou YC, Wu DC, Cheng CG, Cheng CA. Surveillance of foodborne diseases in Taiwan: a retrospective study. Medicine. 2021;100:5(e24424).
CGC and CAC contributed equally to this work.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
Supplemental digital content is available for this article.
References
- [1]. Organization WH. Estimates of the Global Burden of Foodborne Diseases 2015, 9789241565165. [ http://apps.who.int/iris/bitstream/10665/199350/1/9789241565165_eng.pdf?ua=1/]. Accessed 14 Feb 2019. [Google Scholar]
- [2].Hoelzer K, Switt AIM, Wiedmann M, et al. Emerging needs and opportunities in foodborne disease detection and prevention: from tools to people. Food Microbiol 2018;75:65–71. [DOI] [PubMed] [Google Scholar]
- [3].Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gould LH, Walsh KA, Vieira AR, et al. Surveillance for foodborne disease outbreaks—United States, 1998–2008. MMWR Surveill Summ 2013;62:1–34. [PubMed] [Google Scholar]
- [5].Lynch M, Painter J, Woodruff R, Braden C. Surveillance for foodborne-disease outbreaks; United States, 1998--2002. 2006. [PubMed] [Google Scholar]
- [6].Flint JA, Van Duynhoven YT, Angulo FJ, et al. Estimating the burden of acute gastroenteritis, foodborne disease, and pathogens commonly transmitted by food: an international review. Clin Infect Dis 2005;41:698–704. [DOI] [PubMed] [Google Scholar]
- [7].Buzby JC, Roberts T. The economics of enteric infections: human foodborne disease costs. Gastroenterology 2009;136:1851–62. [DOI] [PubMed] [Google Scholar]
- [8].Hoffmann S, Batz MB, Morris JG., Jr Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens. Journal of food protection 2012;75:1292–302. [DOI] [PubMed] [Google Scholar]
- [9].Organization WH. First formal meeting of the Foodborne Disease Burden Epidemiology Reference Group (FERG): implementing strategy, setting priorities and assigning the tasks 2008. 9241596767. [Google Scholar]
- [10].Borgdorff MW, Motarjemi Y. Surveillance of foodborne diseases: what are the options?:. Geneva: World Health Organization; 1997. [PubMed] [Google Scholar]
- [11].Foodborne diseases in Taiwan. 2019; Available at: https://dep.mohw.gov.tw/DOS/lp-1729-113.html. Accessed 8 Aug, 2019. [Google Scholar]
- [12].Jones TF, Yackley J. Foodborne disease outbreaks in the United States: a historical overview. Foodborne Pathog Dis 2018;15:11–5. [DOI] [PubMed] [Google Scholar]
- [13].Nguyen VD, Bennett SD, Mungai E, et al. Increase in multistate foodborne disease outbreaks—United States, 1973–2010. Foodborne Pathog Dis 2015;12:867–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Barrett KA, Nakao JH, Taylor EV, et al. Fish-associated foodborne disease outbreaks: United States, 1998–2015. Foodborne Pathog Dis 2017;14:537–43. [DOI] [PubMed] [Google Scholar]
- [15].de Oliveira Elias S, Tomasco PV, Alvarenga VO, et al. Contributor factors for the occurrence of salmonellosis during preparation, storage and consumption of homemade mayonnaise salad. Food Res Int 2015;78:266–73. [DOI] [PubMed] [Google Scholar]
- [16].Haendiges J, Jones J, Myers RA, et al. A nonautochthonous US strain of Vibrio parahaemolyticus isolated from Chesapeake Bay oysters caused the outbreak in Maryland in 2010. Appl Environ Microbiol 2016;82:3208–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Taylor M, Cheng J, Sharma D, et al. Outbreak of Vibrio parahaemolyticus associated with consumption of raw oysters in Canada, 2015. Foodborne Pathog Dis 2018;15:554–9. [DOI] [PubMed] [Google Scholar]
- [18].Borges KA, Furian TQ, De Souza SN, et al. Spread of a major clone of Salmonella Enterica serotype enteritidis in poultry and in Salmonellosis outbreaks in southern Brazil. J Food Prot 2016;80:158–63. [DOI] [PubMed] [Google Scholar]
- [19].Al-Rifai RH, Chaabna K, Denagamage T, et al. Prevalence of enteric non-typhoidal Salmonella in humans in the Middle East and North Africa: A systematic review and meta-analysis. Zoonoses Public Health 2019;66:701–28. [DOI] [PubMed] [Google Scholar]
- [20].McDowell RH, Sands EM, Friedman H. Bacillus Cereus. StatPearls. Treasure Island (FL): StatPearls Publishing; 2019. [PubMed] [Google Scholar]
- [21].Pan T-M, Wang T-K, Lee C-L, et al. Food-borne disease outbreaks due to bacteria in Taiwan, 1986 to 1995. J Clin Microbiol 1997;35:1260–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kadariya J, Smith TC, Thapaliya D. Staphylococcus aureus and staphylococcal food-borne disease: an ongoing challenge in public health. Biomed Res Int 2014. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pondit A, Haque ZF, Sabuj AAM, et al. Characterization of Staphylococcus aureus isolated from chicken and quail eggshell. J Adv Vet Anim Res 2018;5:466–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang Y-T, Lin Y-T, Wan T-W, et al. Distribution of antibiotic resistance genes among Staphylococcus species isolated from ready-to-eat foods. J Food Drug Anal 2019;27:841–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lu K-H, Sheen Y-J, Huang T-P, et al. Effect of temperature on the growth of Staphylococcus aureus in ready-to-eat cooked rice with pork floss. Food Microbiol 2020;89:103374. [DOI] [PubMed] [Google Scholar]
- [26].Agency CN. The contaminated egg in Taoyuan. 2018; Available at: https://www.cna.com.tw/news/firstnews/201808120106.aspx. [Google Scholar]
- [27].Tsunematsu S. Natural toxin poisoning. Nihon rinsho. Nihon Rinsho 2012;70:1391–4. [PubMed] [Google Scholar]
- [28].Feng C, Teuber S, Gershwin ME. Histamine (scombroid) fish poisoning: a comprehensive review. Clin Rev Allergy Immunol 2016;50:64–9. [DOI] [PubMed] [Google Scholar]
- [29].Inbound visitors in Taiwan. 2020; Available at: https://stat.taiwan.net.tw/inboundSearch. Accessed 10 May, 2020. [Google Scholar]
- [30].De S. Food safety: steps of rising concern. Everyman's Science 2010;45:219–22. [Google Scholar]
- [31].De S. Strategies of plant biotechnology to meet the increasing demand of food and nutrition in India. Int Ann Sci 2020;10:7–15. [Google Scholar]
- [32].De S. Identification and Cloning of Putative Serine Protease Inhibitor (Serpin) Genes in Rice (Oryza sativa) and a Preliminary Approach to Generate RNAi using the Cloned Sequences. 2019:1–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


