Abstract
Since the first infected case of Coronavirus Disease 2019 (COVID-19) was reported in Wuhan, China in December 2019, the virus has spread swiftly, inflicting upon millions of people around the globe. The objective of the study is to investigate and analyze the clinical characteristics and outcomes of patients infected with COVID-19 in Wuxi, China.
Cross-sectional study.
The Fifth People's Hospital of Wuxi, China.
A total of 48 COVID-19 patients were enrolled in the study from 23 January 2020 to 8 March 2020, and the clinical data of these subjects were collected.
Epidemiological, clinical, laboratory, and radiologic characteristics, as well as treatment and outcome data, were collected and analyzed.
Of these 48 patients with confirmed COVID-19, 3 were mild cases (6.3%), 44 were moderate cases (91.7%), 1 was severe case (2.1%). The median age of the subjects was 45 years (interquartile range [IQR], 24–59; range, 5–75 years). Twenty-five of the patients (52.1%) were male and 23 (47.9%) were female. Twenty-eight cases (58.3%) returned to Wuxi, Jiangsu Province. Thirty-four (70.8%) cases were infected due to clustering epidemic and 29 cases (85.3%) were attributable to family-clustering epidemic. No obvious clinical symptoms were observed in the cohort of patients, except for 3 mild cases. The most common symptoms include fever (41 [85.4%]), cough (28 [58.3%]), asthenia (13 [27.1%]), expectoration (11 [22.9%]), diarrhea (10 [20.8%]), and dyspnea (5 [10.4%]). Seventeen (35.4%) patients had lower lymphocyte values than baseline, 31 patients (64.6%) had higher d-dimers to exceed the normal range. The distribution of high-resolution computed tomography (HRCT)-positive lesions were as follows: left lung in 5 cases (10.4%), right lung in 9 cases (18.8%), and bilateral lungs in 31 cases (64.6%). In terms of density of lesions: 28 cases (58.3%) showed ground glass shadows in the lung, 7 cases (14.6%) showed solid density shadows, and 10 cases (20.8%) showed mixed density shadows. Extrapulmonary manifestations found that mediastinal lymph nodes were enlarged in 2 cases (4.2%) and that pleural effusion was present in 1 case (2.1%). All patients underwent treatment in quarantine. Forty-five (93.8%) patients received antiviral treatments, 22 (45.8%) patients received antibacterial treatments, 6 (12.5%) patients received glucocorticoid treatments, 2 (4.2%) patients received high flow oxygen inhalation treatments, and 6 (12.5%) patients received noninvasive ventilation treatments. As of 8 March 2020, all 48 patients included in this study were cured. The average time of hospitalization of the 48 patients was 18 ± 6 (mean ± SD) days, the average time of the lesion resorption was 11 ± 4 days, and the average time taken to achieve negativity in the result of nucleic acid examination was (10 ± 4) days.
The epidemiological characteristics of 48 COVID-19 patients in Wuxi were mainly imported cases and clustered cases. The clinical manifestations of these patients were mainly fever and cough. Laboratory results showed that the lymphocytopenia and increased d-dimer are positively correlated with disease severity. Pulmonary imaging showed unilateral or bilateral ground glass infiltration. Most of the patients entered clinical recovery stage within 15 days after hospitalization.
Keywords: clinical characteristics, COVID-19, epidemiology
1. Introduction
As a new type of coronavirus-related pneumonia (SARS-CoV-2), novel coronavirus pneumonia (NCP) has not been previously documented in humans or animals,[1] until recently WHO has officially named the disease as Coronavirus Disease 2019 (COVID-19).[2] Since the first novel coronavirus patient was admitted to hospital on December 12, 2019, China has reported a total of 85,973 confirmed cases of NCP, and a death toll of 4634.[3] In the meantime, a total of 45,632,406 confirmed cases have been reported in countries and regions outside of China.[4] At present, most of the patients have mild symptoms and manifest favorable prognoses. However, the mortality rate of some patients with severe pneumonia, pulmonary edema, acute respiratory distress syndrome (ARDS), or multiple organ failure remains frustrating.[5,6]
In late January 2020, with the advent of the Chinese Lunar New Year, a large-scale flow of people returned from Wuhan severely aggravated the virus infections in other areas of China. Recently, Japan, South Korea, and other neighboring countries have also attracted worldwide attention. Owing to the increased mobility of such a large population, megacities are prone to have increased prevalence of infected cases. At present, COVID-19 has been reported in Wuhan, Beijing, and other major cities, while the epidemiological characteristics of a large number of megacities are seldom reported. In this study, we describe the clinical characteristics and laboratory test results of 48 patients with COVID-19 infection diagnosed in Wuxi, China, so as to advance the understanding of the disease and to provide useful reference for the prevention and intervention of COVID-19 in other megacities.
2. Methods
2.1. Study design and participants
The study was approved by the Ethics Committee of The Fifth People's Hospital of Wuxi (No.: 2020-003-1). All patients diagnosed with COVID-19 between January 23, 2020 and March 8, 2020 were enrolled in this study. “The novel coronavirus pneumonia diagnosis and treatment plan (trial version 7)” was approved by the National Health Commission of China.[7] The Fifth People's Hospital of Wuxi, located in Wuxi City, Jiangsu Province, is 1 renowned “3rd Grade, Class A” teaching hospitals designated by the government to attend to local patients with COVID-19, and to monitor the clinical outcomes of the said patients (i.e., discharge, mortality, and length of stay) as of the most recent date of follow-up since March 8, 2020.
2.2. Data collection
According to “the novel coronavirus pneumonia diagnosis and treatment plan (trial version 7),” 48 patients with COVID-19 infections in total were divided into mild, moderate, severe, and critical subtypes. The respiratory research team of our hospital analyzed the patients’ medical records. Information on epidemiological, clinical, laboratory, and radiologic characteristics, as well as treatment and outcome data, were obtained by using data collection tables in the EMR, and were then reviewed by the team consisting of professional doctors.
2.3. CT examination and image analysis
The enrolled patients were imaged in a supine position during a suspended inspiration by using a 256-slice multi-detector computed tomography (MDCT) scanner (Brilliance iCT, Philips Healthcare, Cleveland, OH), the scanned area covered the region from the apex of the lung to the top of the diaphragm. High-resolution computed tomography (HRCT) scanning technology was used, and the scanning parameters were set as follows: tube voltage 120 kV, tube current 210 Ma, slice spacing 5 mm, and slice thickness 0.625 mm.
Two experienced cardiothoracic radiologists analyzed the films independently. In the event of differing opinions, they would reach a unanimous judgment through consultation with a third cardiothoracic radiologist. The CT manifestations of each patient were described according to the following characteristic parameters:
-
(1)
distribution of lesions: left lung, right lung, bilateral lungs;
-
(2)
density of lesions: ground glass, solid, mixed type;
-
(3)
extrapulmonary manifestations: whether there was lymphadenopathy or pleural effusion.
2.4. Statistical analysis
All data were analyzed by using SPSS (version 17.0, IBM Corporation, Armonk, NY). Categorical variables were described in terms of frequency, ratio, and percentage; continuous variables were described using the values of mean, median, and interquartile range (IQR). The baseline and CT features of patients in the mild, moderate, severe groups were compared by using Fisher's exact probability test. The age and laboratory indexes of these groups were compared by using Kruskal–Wallis rank sum test, and P < .05 was considered to indicate statistical significance.
3. Results
3.1. Baseline characteristics of enrolled patients
According to the clinical classification of the COVID-19 released by the National Health and Health Commission of China (Table 1), of 48 COVID-19 cases, 3 cases were mild (6.3%), 44 cases were moderate (91.7%), 1 case was severe (2.1%). The median age was 45 years (IQR, 24–59; range, 5–75 years). Twenty-five of the patients (52.1%) were male and 23 (47.9%) were female. Twenty-eight cases (58.3%) returned to Wuxi from other areas. The incidence of clustering epidemic was 34 (70.8%), and the incidence of family-clustering epidemic was 29 (85.3%). Of the 48 included patients, 21 (43.8%) had one or more pre-existing comorbidities. Hypertension (12 [25%]) and diabetes (7 [14.6%]) were the relatively common comorbidities of the subjects (Table 2).
Table 1.
Clinical classification of the COVID-19 released by the National Health and Health Commission of China.
| Mild | Common | Severe | Critically severe |
| Mild clinical manifestation, none imaging performance | Fever, respiratory symptoms, pneumonia performance on X-ray or CT | Meet any of the followings: 1. Respiratory distress, RR ≥ 30/min;2. Oxygen saturation ≤ 93% at rest state;3. Arterial partial pressure of oxygen (PaO2)/fraction of inspiration O2 (FiO2) ≤ 300 mm Hg, 1 mm Hg = 0.133 kPa. | Meet any of the followings:1. Respiratory failure needs mechanical ventilation;2. Shock;3. Combined with other organ failure, patients need ICU monitoring and treatment. |
Table 2.
Baseline characteristics of patients with SARS-CoV-2 infection.
| No. (%) | ||||
| Total (N = 48) | Mild type (N = 3) | Moderate type (N = 44) | Severe type (N = 1) | |
| Age, median (IQR), yr | 45 (24–59) | 15 (14–16) | 47 (25–58) | 71 |
| Sex | ||||
| Male | 25 (52.1) | 3 (100) | 21 (47.7) | 1 (100) |
| Female | 23 (47.9) | 0 (0) | 23 (52.3) | 0 (0) |
| Imported case | 28 (58.3) | 3 (100) | 24 (54.5) | 1 (100) |
| Clustered disease | 34 (70.8) | 3 (100) | 30 (68.2) | 1 (100) |
| Comorbidities | 21 (43.8) | 0 (0) | 20 (45.5) | 1 (100) |
| Diabetes | 7 (14.6) | 0 (0) | 6 (13.6) | 1 (100) |
| Hypertension | 12 (25) | 0 (0) | 11 (25) | 1 (100) |
| Anemia | 1 (2.1) | 0 (0) | 1 (2.3) | 0 (0) |
| Epilepsy | 1 (2.1) | 0 (0) | 1 (2.3) | 0 (0) |
| Chronic liver disease | 1 (2.1) | 0 (0) | 1 (2.3) | 0 (0) |
| Cardiovascular diseases | 2 (4.2) | 0 (0) | 1 (2.3) | 1 (100) |
| Chronic kidney disease | 1 (2.1) | 0 (0) | 0 (0) | 1 (100) |
| Hypothyroidism | 1 (2.1) | 0 (0) | 1 (2.3) | 0 (0) |
| Lumbar fracture | 1 (2.1) | 0 (0) | 1 (2.3) | 0 (0) |
| Symptoms | ||||
| Fever | 41 (90.9) | 0 (0) | 40 (90.9) | 1 (100) |
| Cough | 28 (60) | 1 (33.3) | 26 (59.1) | 1 (100) |
| Asthenia | 13 (27.3) | 0 (0) | 12 (27.3) | 1 (100) |
| Expectoration | 11 (23.6) | 0 (0) | 10 (22.7) | 1 (100) |
| Phlegm blood | 2 (54.5) | 0 (0) | 2 (4.5) | 0 (0) |
| Dyspnea | 5 (12.7) | 0 (0) | 4 (9.1) | 1 (100) |
| Myalgia | 2 (5.5) | 0 (0) | 2 (4.5) | 0 (0) |
| Headache | 1 (5.5) | 0 (0) | 0 (0) | 1 (100) |
| Chest pain | 1 (1.8) | 0 (0) | 0 (0) | 1 (100) |
| Diarrhea | 10 (23.6) | 0 (0) | 10 (22.7) | 0 (0) |
No obvious clinical symptoms could be observed in the patients, except for 3 mild cases. The most common symptoms included fever (41 [85.4%]), cough (28 [58.3%]), asthenia (13 [27.1%]), expectoration (11 [22.9%]), diarrhea (10 [20.8%]), and dyspnea (5 [10.4%]). The less common symptoms included bloody phlegm, myalgia, headache, and chest pain (Table 2).
Compared with mild and moderate patients, patients with severe symptom were significantly older (mild: 15 years old [median], moderate: 47 years old [median], severe: 71 years old; P = .021). Moreover, the proportion of basic diseases was higher (mild: 0 cases [0%], moderate: 20 cases [45.5%], severe: 1 case [100%]; P = .156) in the severe subgroup. The moderate patients had low-to-moderate degree of fever (<39.1°C), while the severe patients had higher degree of fever (≥39.1 °C).
3.2. Results of laboratory tests
During the hospitalization, we observed 4 moderate patients (8.3%) had white blood cell (WBC) counts below the normal range, and 1 severe patient (2.1%) had WBC counts above the normal range. Seventeen patients (35.4%), including 3 mild cases and 14 moderate cases, had lower neutrophil counts than the normal range. One severe case (2.1%) had neutrophils above the normal range. Seventeen (35.4%) patients, including 3 mild cases and 14 moderate cases had lower lymphocytes than the normal range. Platelet counts of the patients were within the normal range. Thirty-one patients (64.6%) had d-dimers higher than the normal range, and their thrombin time was in the normal range, and they had normal concentration of albumin. Moreover, notably higher concentrations of alanine transaminase (ALT), aspartate transaminase (AST), and total bilirubin than normal range were observed in 6 cases (12.5%), 4 cases (8.3%), and 3 cases (6.3%), respectively. C-reactive protein was higher than the normal range in 18 cases (37.5%). Five patients (10.4%) had hypokalemia, yet their sodium content was in the normal range. The subjects had normal concentration of creatine kinase (Table 3).
Table 3.
Laboratory findings of patients infected with SARS-CoV-2 infection on admission to hospital.
| Median (IQR) | ||||||
| Normal range | Total (N = 48) | Mild type (N = 3) | Moderate type (N = 44) | Severe type (N = 1) | P | |
| WBC count, ×109/L | 3.5–9.5 | 5.3 (4.5–6.2) | 6.6 (5.8–6.7) | 5.1 (4.4–5.9) | 12.4 | .116 |
| Neutrophil count, ×109/L | 1.8–6.3 | 3.4 (2.6–4.1) | 4.3 (3.7–4.6) | 3.4 (2.5–3.9) | 7.9 | .108 |
| Lymphocyte count, ×109/L | 1.1–3.2 | 1.3 (1.0–1.9) | 0.9 (0.7–1.0) | 1.4 (1.0–1.9) | 1.32 | .912 |
| Platelet count, ×109/L | 125–350 | 186.5 (154.0–215.3) | 222 (206–223) | 184 (153–210) | 220 | .185 |
| d-Dimers, μg/mL | 0–0.23 | 0.32 (0.22–0.65) | 0.22 (0.21–0.23) | 0.33 (0.22–0.65) | 10.2 | .03 |
| Thrombin time, s | 12.0–18.0 | 16.2 (15.4–17.2) | 13.5 (13.4–13.6) | 16.3 (15.8–17.2) | 15.1 | .016 |
| Albumin, g/L | 35.0–55.0 | 42.0 (38.3–45.8) | 51.0 (49.5–52.5) | 42.0 (38.3–45.0) | 36 | .019 |
| ALT, U/L | 5.0–50.0 | 20.0 (16.0–43.8) | 15.0 (13.5–32.5) | 20.0 (16.0–42.0) | 87 | .203 |
| AST, U/L | 5.0–50.0 | 25.0 (21.0–31.0) | 23.0 (21.0–27.0) | 25.0 (21.0–31.0) | 139 | .205 |
| Total bilirubin, μmol/L | 3.4–20.6 | 7.0 (4.3–10.8) | 7.0 (5.5–11.0) | 7.0 (4.3–10.0) | 63 | .229 |
| C-reactive protein, mg/L | 0–10 | 6.8 (1.8–26.2) | 8.5 (8.5–8.8) | 5.7 (1.2–26.2) | 108.1 | .344 |
| Potassium, mmol/L | 3.50–5.30 | 4.1 (3.7–4.6) | 3.8 (3.7–3.9) | 4.1 (3.7–4.6) | 3.9 | .494 |
| Sodium, mmol/L | 136.0–145.0 | 142.0 (140.0–143.0) | 142.0 (141.0–142.5) | 142.0 (140.0–143.0) | 145 | .288 |
| Creatine kinase, U/L | 25–200 | 68.5 (53.3–96.0) | 71.0 (66.0–73.0) | 67.5 (51.5–96.0) | 101 | .615 |
3.3. Imaging features
HRCT was performed in all 48 patients during their first visit to the hospital, figuring out 3 negative cases and 45 positive cases to varying degrees of severity. The distribution of HRCT positive lesions was as follows: left lung in 5 cases (10.4%), right lung in 9 cases (18.8%), bilateral lungs in 31 cases (64.6%); density of the lesions: 28 cases (58.3%) showed ground glass shadows in the lung (Fig. 1A), including 7 cases (14.6%) with solid density shadows (Fig. 2A), and 10 cases (20.8%) with mixed density shadows (Fig. 3A). After treatment, the lesion area has varying degrees of absorption (Figs. 1B, 2B, and 3B). Extrapulmonary manifestations: enlarged mediastinal lymph nodes in 2 cases (4.2%), and the presence of pleural effusions in 1 case (2.1%) (Table 4).
Figure 1.
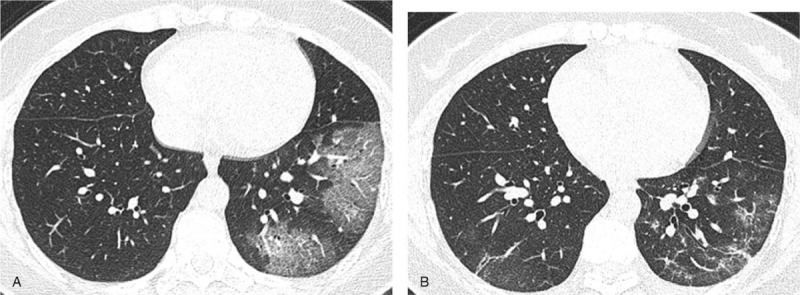
Transverse thin-section serial CT scans from a 49-year-old woman: (A) CT image of the 2th day of hospitalization: ground glass shadow visible in left lower lung, (B) CT image analysis on the 13th day of hospitalization: shows healing of the ground glass shadow.
Figure 2.
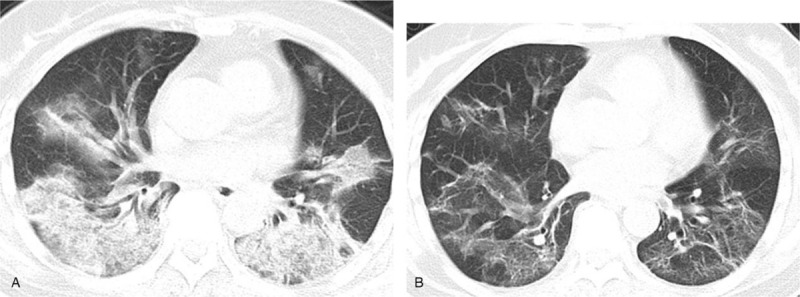
Transverse thin-section serial CT scans from a 61-year-old woman: (A) CT image of the 1th day of hospitalization: solid density shadows visible in both lungs, (B) CT image analysis on the 24th day of hospitalization: shows healing of the solid density shadows.
Figure 3.
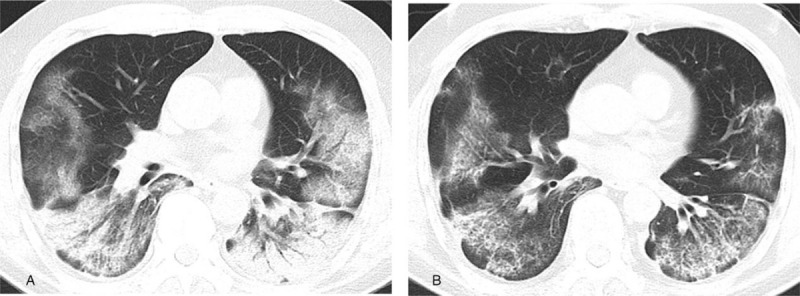
Transverse thin-section serial CT scans from a 53-year-old man: (A) CT image of the 9th day of hospitalization: mixed density shadows visible in both lungs, (B) CT image analysis on the 16th day of hospitalization: shows healing of the mixed density shadows.
Table 4.
CT features of patients with SARS-CoV-2 infection in different clinical types.
| The distribution of HRCT positive lesions | The density of HRCT positive lesions | Extrapulmonary manifestations | |||||||
| Typing | N (%) | Left lung | Right lung | Bilateral lungs | Ground glass shadows | Solid density shadows | Mixed density shadows | Mediastinal lymphadenopathy | Pleural effusions |
| Moderate type | 44 | 5 (11.4) | 9 (20.5) | 30 (68.2) | 28 (63.6) | 6 (13.6) | 10 (22.7) | 1 (2.3) | 0 (0) |
| Moderate type | 1 | 0 (0) | 0 (0) | 1 (100) | 0 (0) | 1 (100) | 0 (0) | 1 (100) | 1 (100) |
| P | .798 | .012 | .044 | .022 | |||||
3.4. Main treatment measures
All patients were subject to treatment in quarantine. Among them, 45 (93.8%) patients received antiviral treatment, 22 patients (45.8%) underwent antibacterial treatments, 6 (12.5%) patients received glucocorticoid treatments, 2 (4.2%) patients received high flow oxygen inhalation treatments, and 6 (12.5%) patients received noninvasive ventilation treatments.
3.5. Discharge status
As of 8 March 2020, all the 48 patients included in this study were cured, hence reaching a satisfying cure rate of 100%. The average time of hospitalization of the 48 patients was 18 ± 6 days, the average time of lesion resorption lasted 11 ± 4 days, and the average time for the result of nucleic acid examination to turn negative amounted to 10 ± 4 days.
4. Discussion
This descriptive study intends to analyze the epidemiological and clinical characteristics of COVID-19 patients in major cities outside Wuhan (i.e., Wuxi, Jiangsu). Wuxi is a typical megacity with a permanent population of about 6.55 million. Thanks to its well-developed transportation and boosting economy, Wuxi is a key second-tier city next to Beijing, Shanghai, and Shenzhen. Due to the superior medical infrastructures, the well-trained medical professionals and the rigorous disease control standards in megacities, the prevention and control pressure of COVID-19 pandemic is enormous in industrialized megacities. Moreover, the city's traffic network connecting numerous dots and reaching out to all directions further amplify the anti-pandemic pressure of people returning to work, therefore it is necessary to study the patterns and characteristics of new coronavirus cases in these cities.
In the current study, we report gratifying outcome: as of 8 March 2020, all 48 patients were cured and there was no death toll. Our data found that the COVID-19 incidence showed neither male predominance nor female predominance, except for 1 critical case was men. Combining the results of the previous study, we suggest that SARS-CoV-2 is more likely to infect adults with chronic comorbidities, especially elderly men.[8,9] According to our data, most of the infected patients once lived in Wuhan for a long time, and an apparent correlation between family gathering and the event of infection could be established to corroborate the human-to-human transmission route of COVID-19.[10] Such transmission route has also well justified the decision and the resolution made by the authorities to extend the Spring Festival holiday, to postpone the date of resumption of work, and to implement a series of preventive measures, such as home quarantine. None of the 48 patients were medical professionals. Thanks to the strict execution of preventive measures to contain the spread of the virus, no new cases have been reported in the city of Wuxi for 21 consecutive days since 25 March 2020.
The common clinical symptoms of COVID-19 include fever, cough, fatigue, expectoration, diarrhea, and dyspnea. The less common clinical symptoms are bloody phlegm, myalgia, headache, and chest pain. In the present study, 1 patient with severe symptom was also infected with bacteria and fungi. Another group of patients had diarrhea symptoms. During the previous outbreak of SARS and the Middle East respiratory syndrome (MERS), nearly a quarter of the patients had diarrhea.[11] One previous study, published in the New England Journal of Medicine (involving 1099 cases), also found the virus in fecal samples. Hence, the possibility of fecal transmission could not be ruled out.[12] We found that most of the patients in Wuxi City, Jiangsu Province had less severe symptoms than those in Wuhan. This finding is consistent with the results of the patients hospitalized in Zhejiang Province, which were reported by professor Lanjuan Li's team.[13]
The most common laboratory examination abnormalities found in this study are lymphocytopenia and increased d-dimer values, suggesting that SARS-CoV-2 infection may be related to cell immune deficiency and coagulation activation. Numerous studies have suggested that SARS-CoV-2, like SARS CoV, may mainly inflict on lymphocytes, especially T lymphocytes.[14] However, our team put forth that in the daily prevention and control work, more attention should be paid to people with simple bacterial infection. In the event of increased counts of leukocytes and neutrophils, the percentage of lymphocytes will increase while the lymphocyte count (absolute value) is often lowered. We should study the results from all patients. Elevated d-dimer level indicates the presence of hypercoagulable state and secondary fibrinolysis in the system, which is a sensitive marker of acute thrombosis. Zhou et al[15] showed that the parameter of d-dimer level >1 mg/L in COVID-19 patients was closely related to higher fatality rate. Xu et al[16] showed that increased d-dimer in COVID-19 patients was related to up-regulated IL-10 level. IL-10 is a multi-cell source and pluripotent cytokine that regulates cell growth and differentiation. It is also an inflammatory and immunosuppressive factor that plays a pivotal role in mediating tissue fibrosis, which indicates more obvious immunosuppression. The high mortality of critically ill COVID-19 patients may be associated with multiple organ failure caused by diffuse microvascular damage.[17] Some researchers believe that cytokines are the mediators of atherosclerosis, which directly lead to plaque rupture, ischemia, and thrombosis through local inflammation, the induction of procoagulant factors and changes in hemodynamics. This is highly attributable to increased coagulation activity and organ function damage in COVID-19 patients.[18] In summary, patients with COVID-19 are characterized by remarkably higher expression of proinflammatory cytokines, increased coagulation activity, and increased d-dimer levels. Elevated d-dimer levels in COVID-19 patients on admission indicate an increased risk of organ functional injury, and require additional clinical attention.
In our study, single or multiple lung lobes had developed lesions, and the patchy shadows were mostly seen in the outer zone of both lungs under the pleura, which can appear as a large area of ground glass shadow. It was found that the area of the density plaque would increase as the disease further progresses. When the patient's clinical condition is improved, some fibrous stripes may appear. On the contrary, if the patient's condition worsens, diffuse lesions will appear throughout the lungs, manifesting significantly higher density and scope of the lesions, as well as the appearance of “white lung,” which seriously sabotage the lung function of the patient.[19] CT examination can help to continuously monitor the progression of the disease.[20] We found that the time when the lesions began to reabsorb on CT was highly consistent with the time when the result of nucleic acid examination turned negative. The combination of imaging evaluation with clinical and laboratory results is of great help to the diagnosis and treatment of COVID-19.
The epidemiological characteristics of COVID-19 cases in Wuxi were mainly imported cases and clustered cases. The clinical manifestations mainly include fever and cough. Laboratory results showed that lymphocyte count and d-dimer are significantly correlated with the severity of the disease. Pulmonary imaging showed unilateral or bilateral ground glass infiltration. Most patients entered clinical recovery stage 15 days after hospital admission. In this study, only the clinical data of only 48 cases were collected, and the patients included in the study were all from Wuxi, Jiangsu Province. Hence, the limitation in sample size and spatial condition due to the timely and effective epidemic prevention and control should be noted. “The novel coronavirus pneumonia diagnosis and treatment plan” issued by the National Health Protection Commission has been tested from the first version to the sixth version, covering all the diagnostic methods relate to viral nucleic acid detection. With the development of technology and advanced understanding of the disease, the detection method of new coronavirus-specific serum antibody (IgM and IgG) has been found, and has a positive diagnosis rate of 100%. The method of diagnosis can also increase the risk of infection transmission during the collecting of nasopharyngeal swab samples; however, the procedure of blood sample collection is simplistic and safe. In the seventh edition, these particular antibodies are added as the diagnostic standard. Yet our study found that there was still a certain false-positive rate in its clinical application, hence it needs to be combined with other detection methods to ensure comprehensive and accurate evaluation.
Author contributions
Each author of this research has contributed to this research and will assume public responsibility for the appropriate portion of the content. This study was initiated and designed by Yigang Chen and Meiping Chu. Linjie Bian and Danping Wu collected the relevant clinical data. Jiehui Huang completed the clinical trial registration and ethical approval procedures. Hao Wang conducted statistical analysis (SPSS). This paper was written by Meiping Chu and Linjie Bian, and all authors jointly revised it and finally approved the manuscript.
Formal analysis: Danping Wu, Hao Wang.
Project administration: Jiehui Huang.
Writing – original draft: MeiPing Chu, Linjie Bian.
Writing – review & editing: Yigang Chen.
Footnotes
Abbreviations: ALT = alanine transaminase, ARDS = acute respiratory distress syndrome, AST = aspartate transaminase, COVID-19 = Coronavirus Disease 2019, HRCT = high-resolution computed tomography, IQR = interquartile range, MDCT = multi-detector computed tomography, MERS = Middle East respiratory syndrome, NCP = novel coronavirus pneumonia, WBC = white blood cell.
How to cite this article: Chu M, Bian L, Huang J, Chen Y, Wu D, Wang H. Clinical characteristics and outcomes of 48 patients hospitalized for COVID-19 infection in Wuxi: A retrospective cohort study. Medicine. 2021;100:5(e23991).
Study on the Key Techniques of Nebulization of Mesenchymal Stem Cell Exosomes for the Treatment of Novel Coronavirus Pneumonia (N2020X008).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
COVID-19 = Coronavirus Disease 2019.
IQR = interquartile range.
ALT = alanine transaminase, AST = aspartate transaminase, IQR = interquartile range, WBC = white blood cell.
HRCT = high-resolution computed tomography.
References
- [1].WHO. Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. Jan11, 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. [Google Scholar]
- [2].WHO. Clinical management of severe acute respiratory infection when Novel coronavirus (nCoV) infection is suspected: interim guidance. Jan 11, 2020. https://www.who.int/internal-publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed Jan 20, 2020). [Google Scholar]
- [3].National Health Commisson of the People's Republic of China. Update on new coronavirus pneumonia epidemic as of 24:00 on October30. http://www.nhc.gov.cn/xcs/yqtb/202010/accc28f30e574f13a9f1b8e5546b5a52.shtml. [Google Scholar]
- [4].Epidemic real-time big data report. https://ncov.dxy.cn/ncovh5/view/pneumonia?from=timeline&isappinstalled=0. [Google Scholar]
- [5].Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. DOI 10.1016/S0140-6736 (20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China 2019. N Engl J Med 2020;382:727–33. DOI 101056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].National Health Commisson of the People's Republic of China. The novel coronavirus pneumonia diagnosis and treatment plan (trial version 7[EB/OL]). [2020-02-18]. http://www.nhc.gov.cn/xcs/zhengcwj/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml. [Google Scholar]
- [8].Channappanavar R, Fett C, Mack M, et al. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol 2017;198:4046–53. DOI 10.4049/jimmunol.1601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Sébastien J, Kevin B, Cecilia G. Sexual dimorphism in innate immunity. Clin Rev Allergy Immunol 2019;56:308–21. DOI 10.1007/s12016-017-8648-x. [DOI] [PubMed] [Google Scholar]
- [10].Leung WK, To KF, Chan PK, et al. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology 2003;125:1011–7. DOI 10.1016/s0016-5085(03)01215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020;395:514–23. DOI 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. DOI 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Xu X-W, Wu X-X, Jiang X-G, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 2020;368:m606.DOI 10.1136/bmj.m606 (published 19 February 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. January 28, 2020. (https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf). [Google Scholar]
- [15].Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. DOI 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Xu Y, Qian Y, Gu Q, et al. Relationship between d-dimer concentration and inflammatory factors or organ function in patients with coronavirus disease 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2020;32:559–63. [DOI] [PubMed] [Google Scholar]
- [17].Li Y, Zhao K, Wei H, et al. Dynamic relationship between d-dimer and COVID-19 severity. Br J Haematol 2020;190:e24–7. DOI 10.1111/bjh.16811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Choi Justin J, Wehmeyer Graham T, Li Han A, et al. d-Dimer cut-off points and risk of venous thromboembolism in adult hospitalized patients with COVID-19. Thromb Res 2020;196:318–21. DOI 10.1016/j.thromres.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. DOI 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia: an official clinical practice guideline of the American Thoracic Society and Infectious Disease Society of America. Am J Respir Crit Care Med 2019;200:e45–67. [DOI] [PMC free article] [PubMed] [Google Scholar]


