Abstract
Lumbar lateral interbody fusion (LLIF) has been gaining popularity among the spine surgeons dealing with degenerative spinal diseases while LLIF on L5-S1 is still challenging for its technical and anatomical difficulty. OLIF51 procedure achieves effective anterior interbody fusion based on less invasive anterior interbody fusion via bifurcation of great vessels using specially designed retractors. The technique also achieves seamless anterior interbody fusion when combined with OLIF25. A thorough understanding of the procedures and anatomical features is mandatory to avoid perioperative complications.
Keywords: Anterior lumbar interbody fusion (ALIF), Oblique lateral interbody fusion (OLIF), Minimally invasive surgery, complication, vascular injury, retrograde ejaculation
Introduction
Recent advancement in lumbar spine surgery techniques have achieved great proceedings by the development of less invasive anterior interbody fusion procedure, or lateral interbody fusion (LIF) surgery1-3). The LIF technique includes mainly two major techniques: psoas-splitting LLIF (XLIF: eXtreme LIF) and non psoas-splitting LLIF (OLIF: Oblique LIF). Among them, OLIF is less invasive with almost no invasion or compression to the psoas muscle compared with XLIF via the anatomical window called oblique lateral corridor in front of the psoas muscle at L2-5 levels (OLIF25)4). However, the OLIF25 procedure is not enough to approach L5-S1 segment for anatomical reasons with complicated vascular structures such as ascending lumbar vein. Traditional ALIF procedure can access the L5-S1 disc space via the central disc space between the bifurcations of the iliac vessels in a supine or semi-supine position, where OLIF25 can hardly approach by technical and positioning reasons. Recent development has made the area accessible with a modified lateral approach to access to the central portion of L5-S1 disc using specially designed retractors in the decubitus position, that can achieve seamless combination with OLIF25, called OLIF51 that is approved in Japan in 2019 with available implants. The current technical note aimed to describe the indication and techniques of OLIF51 surgery, including case presentation and complication based on literature.
Indications
The indications for OLIF51 are similar to those for traditional anterior lumbar interbody fusion: discogenic lower back pain with unstable degenerative discs with no canal stenosis, spondylolysis, and degenerative spondylolisthesis, and failed back syndromes5-7). Cases with severe synovitis or severe intracanal/intraforaminal bony spur may require direct posterior decompression for ensured enlargement of the neural pathway. OLIF51 has two merits in lumbosacral pathology. Firstly, OLIF51 can provide, like OLIF25 procedure, significant correction in both coronal and sagittal imbalance followed by achievement of proper spinal sagittal balance and improved outcomes8-10) as well as indirect decompression with spontaneous enlargement of spinal canal and foramen. Pathological adjacent segment disease (ASD) at L5-S1 disc, that can be caused by floating lumbar fusion11,12), is also a good indication for OLIF51. Secondly, OLIF51 can provide more lordosis that is expected more in the patients who require more lordotic lumbosacral junction, such as degenerative kyphoscoliosis cases with pelvic malalignment. These features indicate that OLIF51 is one of the viable options for adult degenerative scoliosis13) combined with multilevel OLIF25 fusion.
Preoperative Planning
The OLIF51 procedure requires a thorough understanding of the retroperitoneal anatomy of the patients, as the procedure can associate with significant complications such as great vascular injury or retrograde ejaculation.
X-ray
A careful review of the relationship of the location of the iliac crest and the L5-S1 level is important. Unlike OLIF25, high-iliac crest does not matter in the oblique lateral trajectory for OLIF51 but does sometimes matter when the surgeon plans to perform simultaneous OLIF25 on L4-5 level14).
Magnetic resonance imaging (MRI) and computed tomography (CT) scan
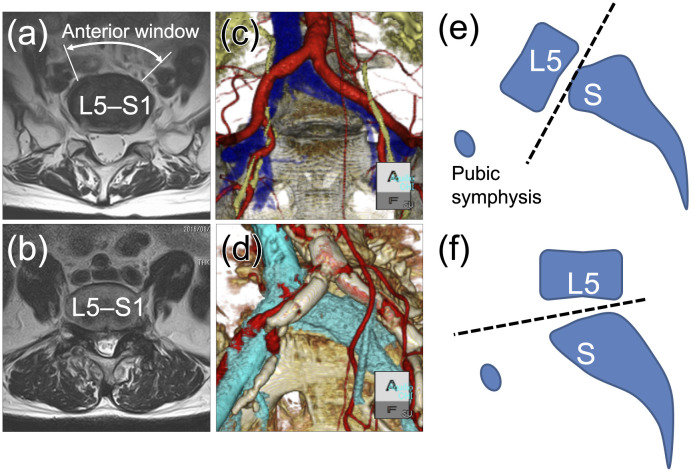
Checking retroperitoneal organs such as the position and shape of the iliopsoas muscle and anterior vasculature, including the location of bifurcation, is mandatory. Preoperative sagittal and axial MRI and CT scan are useful to determine the location of the bifurcation and transitional anatomy. When the iliac vessels, especially left common iliac vein, were congested in front of the L5-S1 disc, the surgeons must be careful in adopting the indication for OLIF51 surgery, as that can lead to vascular injury by excess mobilization and/or interference with the great vessels (Fig. 1 (a, b)). On the other hand, unlike OLIF25, anteriorly located iliopsoas does not matter. Abdominal CT angiography should be performed to evaluate bony factors, vessel trajectory, and urinary tracts. Three-dimension reconstruction provides images on how the possible view of the surgical field as well as its anatomical features (Fig. 1 (c, d)). Furthermore, confirmation of the relative location of L5-S1 space to the pubic symphysis (Fig. 1 (e, f)). These preoperative investigation and planning are quite important to avoid intraoperative complications described later.
Figure 1.
Preoperative planning. Confirmation of the anatomy around the anterior portion of L5-S1 disc is mandatory using MRI (a, b), abdominal CT angiography (c, d), and reconstructed sagittal CT scan (e,f). (a) The anatomical window should be wide enough (a), and OLIF51 should not be performed when the vessels are congested in front of the disc (b). Abdominal CT angiography provides the information around the L5-S1 disc: (c) Adequate opening with good indication for OLIF51. (d) The left common iliac vein runs over the disc, and the indication for OLIF 51 must be carefully discussed. Confirmation of the relative location of L5-S1 space to the pubic symphysis is also essential in evaluating the preoperative approach to the L5-S1 disc space. If the direction of the L5-S1 disc goes under the pubic symphysis (e), OLIF51 approach is impossible compared with the usual direction (f).
Surgical Technical Review for OLIF51
Patient positioning
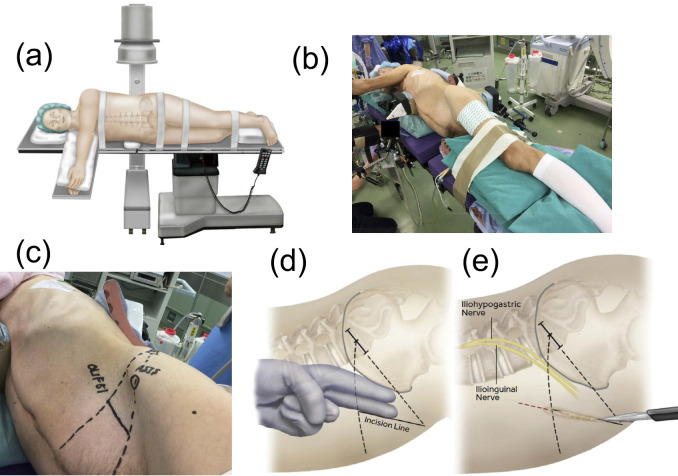
The patient is set up as right lateral decubitus on a radiolucent table just as OLIF25 surgery. The patient should be fixed using lateral boards or tape, as is reported in LLIF procedures6,13,14) (Fig. 2 (a)). Unlike OLIF 25, a lateral board for pubic symphysis should not be placed in the regular position as it can interfere with the instruments such as cage inserters. The board can be used for restraining the thigh, or the procedure can be done even without it only when the patients was fixed firmly (Fig. 2 (b)).
Figure 2.
Patient positioning using (a) tapes or (b) lateral boards. The patient should be fixed using lateral boards or tape. It may be helpful to flex the lower hip for added stability. (c-d) Skin marking. (c) Under fluoroscopic guidance, check and mark the target L5-S1 disc space and the midportion of the disc space, and draw two identical lines: a vertical line projected perpendicular to the floor, and another one extended onto the abdomen in the direction of the disc. (d, e) The incision is made 1-2 finger breadths from the ASIS along the pelvis. The incision can be made in about 3-7 cm in length. The position of the incision depends on the disc level and number of levels.
Place the patient so as to be perpendicular to the floor, not to the surgical table, to obtain a true lateral image. Minor adjustments by table rotation or tilting under fluorescent guidance would be helpful for the successive positioning, and that enables the technique much easier using C-arm. Placing an axillary roll and bending the patient's hips and knees will relax the psoas and nerve fibers inside. Jackknifed position with a table breaking is not necessary15).
Skin marking and incision
After the positioning, identify and mark the location of the anterior superior iliac spine (ASIS), the contour of the iliac crest, and the target L5-S1 disc using fluoroscopy. From the midportion of the L5-S1 disc, draw two identical lines: a vertical line projected perpendicular to the floor, and another one extended onto the abdomen in the direction of the disc (Fig. 2 (c)). The incision is made 1-2 finger breadths from the ASIS along the pelvis to avoid nerve injury of the iliohypogastric and ilioinguinal nerves that exit the abdominal cavity about 20 mm from the ASIS and run toward the groin. The incision can be made in about 3-7 cm in length (Fig. 2 (d, e)), which is flexible according to the patients' physique or necessity of combined other level OLIF (ex. L4-5).
Approaching the retroperitoneal space and the L5-S1 disc
The surgeon can approach the retroperitoneal space using a Kelly Clamp or simply two fingers via blunt dissection of abdominal external oblique muscle, internal oblique muscle, and transversalis muscle with deep transversalis fascia in its back as is described in the OLIF25 procedure. If the incision is located more medial, the entry point can be just close to the rectus abdominis muscle. In this procedure, the external oblique muscle at that level looks like aponeurotic that requires sharp incision.
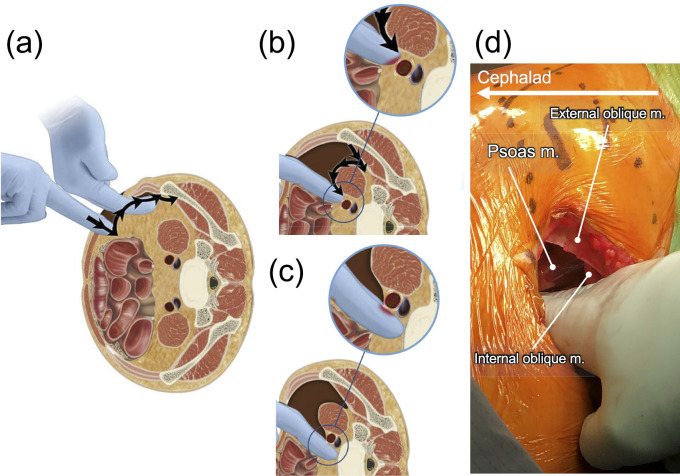
Clean the transversalis fascia off using index fingers and a peanut to find retroperitoneal fat through it. And then, incise a small hole to expose the yellow retroperitoneal fat. This fascia can have been already lacerated during the blunt dissection. Sweep circumferentially around the undersurface of the transversalis fascia to ensure the peritoneum is not adherent to the fascia using two index fingers, and then palpate and follow the internal abdominal wall along with the inside of the pelvis (Fig. 3 (a)). Once touch the iliopsoas muscle that has a soft but tensioned, and pliable feeling, and then sweep the peritoneal contents in all of the direction: cephalad-caudal and dorsal-ventral, which allows the abdominal contents to fall away from the spine, requiring significantly less peritoneal retraction forces than a traditional supine midline exposure. The blunt dissection continues anteriorly from the pelvis while searching for the very palpable common iliac artery pulse. Once palpate the pulse on the finger pad, move the finger medially by keeping to feel the pulse on the dorsal side of the finger (Fig. 3 (b, c)). The surgeon can search and feel the deeply-located sacral promontory there with a possibility of touching the promontory over the common iliac vein medial to the artery. The vein is pulseless and can palpate like just a soft tissue that covers the anterior portion of the L5-S1 disc and the promontory.
Figure 3.
Retroperitoneal approach to the L5-S1 disc. After the circumferential sweep around the undersurface of the transversalis, palpate and follow the internal abdominal wall along with the inside of the pelvis (a). Once touch the iliopsoas, the blunt dissection continues anteriorly from the pelvis while searching for the very palpable common iliac artery pulse (b). Once palpate the pulse on the finger pad, move the finger medially by keeping to feel the pulse on the dorsal side of the finger (c). Direct visualization of the iliopsoas muscle and the common iliac vessels should be established in addition to the tactile feeling. (d) The index finger is touching the promontory by feeling the arterial pulse on the dorsal side of the finger.
To ensure a safe approach to the L5-S1 disc space between the bifurcation, direct visualization of the iliopsoas muscle and the common iliac vessels should be established in addition to the tactile feeling (Fig. 3 (d)). The fat overlying the psoas muscle and L5-S1 disc can be gently swept using fingers, peanuts, and hand-held retractors (The exposed L5-S1 disc is shown later in (Fig. 4 (c)). Especially adventitial layers on the anterior disc and sacrum should be mobilized using extremely gentle blunt dissection, as the layer adheres and tethers the common iliac vein to the annulus with the superior hypogastric neural plexus and sympathetic chain within it, known as the major cause of retrograde ejaculation when injured.
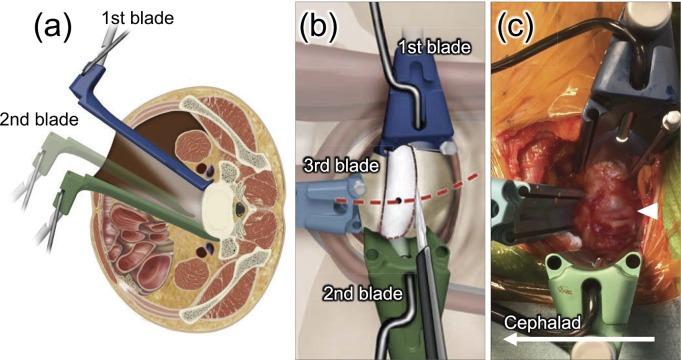
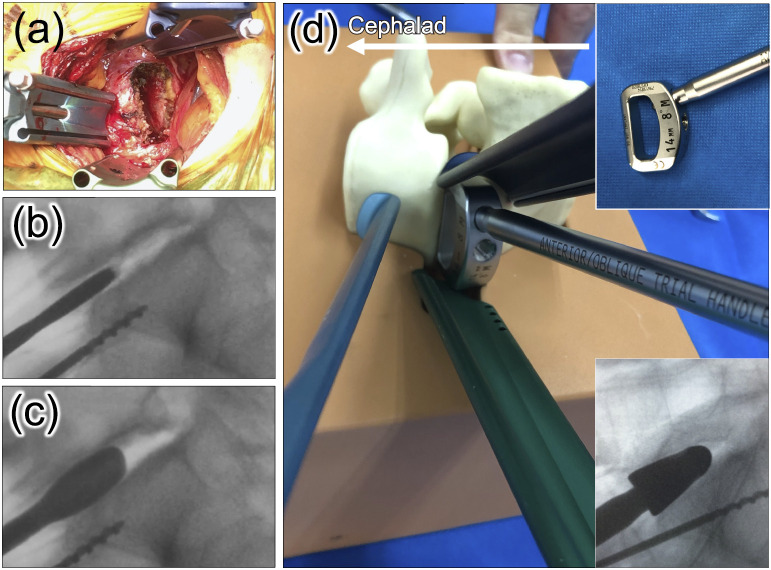
Figure 4.
Exposure of the L5-S1 disc. (a) Placement of 1st and 2nd blades by laterally retracting the common iliac vessels. (b) The L5-S1 disc exposed using three retractor blades. The 1st and the 3rd blades are fixed using pins. The red dot line indicates the midline of the L5-S1 disc. (c) Intraoperative images of the L5-S1 disc. Only the 1st retractor is fixed to the sacrum. White arrowhead indicates the medial sacral vessels.
Exposure of the L5-S1 disc
Once after the establishment of the safe retroperitoneal pathway to the anterior portion of the L5-S1 disc under direct visualization, OLIF51 retractor blades are available, which are length enough and a channel to put a fixation pin to the sacrum or vertebral body, and some of them have backward curvature on their tip to ensure safe retraction (Fig. 4 (a)). Firstly place the retractors between the bilateral common iliac vessels, and retract them gently outward to expose the L5-S1 disc. Continue sequential placement of the retractors by placing the blunt-tipped blade medially that is designed to wrap around the contralateral side of the disc. And then, additional third medial blade can be placed to gently retract and guard the bifurcation on the L5 vertebrae. And then, the retractor blades are attached to the flexible arm fixed to the operative table. The first and third blade can be pinned to sacrum and L5 vertebral body, respectively. Pinning the second blade is not mandatory (Fig. 4 (b)).
Disc preparation
Once the retractors are placed, it is important to confirm the midline of the disc space under AP fluoroscopic view. Medial sacral vessels also can be of help to confirm the anatomical midline. Medial sacral vessels should be ligated or cauterized to assure the thorough exposure of the anterior portion of the L5-S1 disc (Fig. 4 (c)). And then, the annulus including anterior longitudinal ligament is incised to create a portal at least 20 mm in length. The annulotomy should be squarely cut from the edge of the disc and vertebral bodies to avoid a “flapper valve” phenomenon wherein the edges of non-removed annulus catch and tighten as the distractors and final implant move in and out of the disc space (Fig. 5 (a)). After the discectomy, a Cobb and intervertebral distractors are inserted across the disc space for an adequate intervertebral release (Fig. 5 (b, c)). This procedure is vital to allow significant expansion of the L5-S1 disc space.
Figure 5.
Disc preparation and implant trialing. After the disc preparation (a), the disc space is sequentially distracted (b, c) until adequate disc space height, and foraminal size are obtained as well as determining the size of the cage using fluoroscopy (d).
The surgeons should also keep in mind that they are working obliquely within the disc space. Quick checks using fluoroscopy are helpful in avoiding unnecessary invasion of the posterior spinal canal and contralateral foramen.
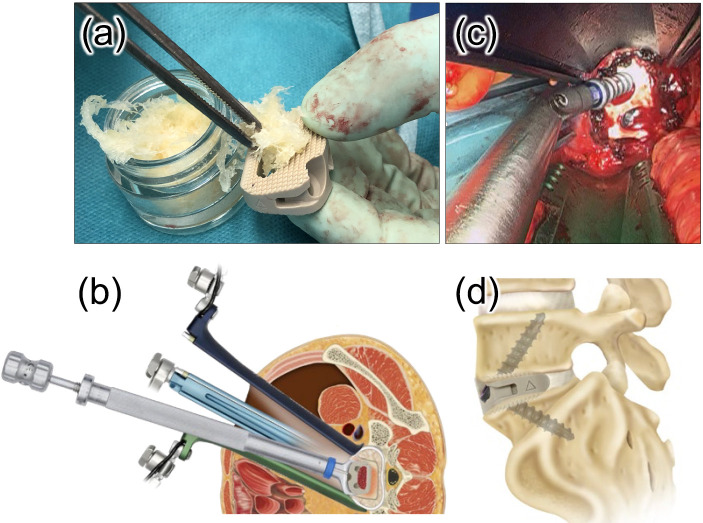
Implant trialing and cage installation
After the disc preparation, the disc space is sequentially distracted with trials with an obliquely-attached handle until adequate disc space height, and foraminal size are obtained as well as determining the size of the cage using fluoroscopy (Fig. 5 (d)). And then an 8º, 12º or 18º lordotic polyether ether ketone cage (OLIF51 Sovereign™ Spinal System; Medtronic Sofamor Danek, Minneapolis, MN, USA), ranging in height from 10 to 16 mm, will be inserted subsequently. Before inserting the cage, place auto/allograft and/or artificial substances such as DBM (demineralized bone matrix), or hydroxyapatite stuff in the implant's central cavity (Fig. 6 (a)). In inserting the cage, confirmation of the A-P and lateral direction using fluoroscopy is mandatory because the obliquely-designed inserter handle can confuse the orientation (Fig. 6 (b)). And then, supplemental screws will be inserted through the screw holes in the anterior portion of the cage as is shown in Fig. 6 (c) and (d). After the implant installation, the retractors will be removed, followed by the closure of the subcutaneous layers and skin. After the OLIF51 procedure, supplemental posterior instrumentation is then placed according to the appropriate surgical techniques such as percutaneous pedicle screw fixation and percutaneous cortical bone screw fixation16). Surgeons can add direct neural decompression depending on the pathology.
Figure 6.
Cage installation. (a) A lordotic intervertebral cage put with DBM (demineralized bone matrix). (b) Cage insertion using an obliquely-designed inserter handle. (c, d) Supplemental screws will be inserted through the screw holes in the anterior portion of the cage.
Representative case presentation
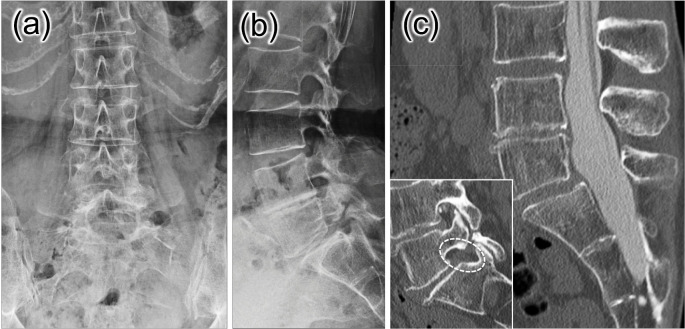
A 65-year-old woman visited our clinic complaining of chronic lower back pain and robust left leg pain, which was refractory to analgesic agents, including opioids. She showed L5 radiculopathy with intermittent neurological claudication at less than 100 meters. Radiological assessment showed L5 spondylolysis with adjacent segment disorder at L4-5 with decreased disc height with impaired local lordosis with no central canal stenosis (Fig. 7). Considering the pathology of her L5 radiculopathy, recovering L5-S foraminal height was mandatory.
Figure 7.
Representative case of a 65-year-old women with spondylolysis. Radiological assessment showed L5 spondylolysis with adjacent segment disorder at L4-5 with decreased disc height with impaired local lordosis with no central canal stenosis. (a, b) Plain X-ray (c) Sagittal and parasagittal CT reconstruction. Dotted circle indicates the impaired left L5-S1 foramen.
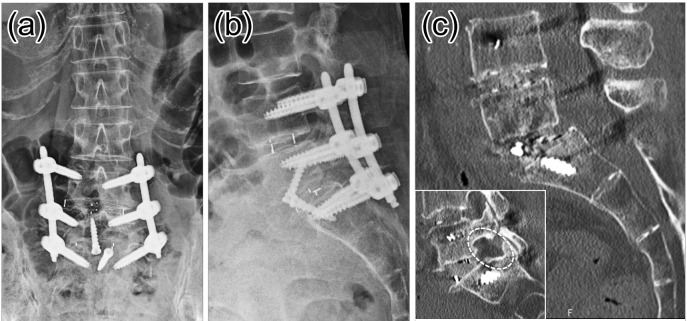
Based on the ensured safety with the wide window in front of the L5-S disc using enhanced CT scan (shown in Fig. 1 (C)), we employed OLIF51 surgery combined with L4-5 OLIF to achieve minimal invasiveness and significant intervertebral and foraminal height recovery, followed by posterior pedicle screw fixation using single position procedure with no patient flipping to a prone position (Fig. 8). Intraoperative bleeding was 40 g with an absolute operative time of 2 hours and 33 min. After the operation, the patient's robust leg pain and lower back pain disappeared with the radiological the L5-S1 foraminal enlargement.
Figure 8.
The patients underwent OLIF51 surgery combined with L4-5 OLIF, followed by posterior pedicle screw fixation using single position procedure with no patient flipping to a prone position. (a, b): Plain X-ray (c) Sagittal and parasagittal CT reconstruction. Dotted circle indicates the impaired left L5-S1 foramen, and note that the foraminal area enlarged compared with the Fig. 7 (c).
Discussion
OLIF51 is essentially a laterally-positioned retroperitoneal ALIF, which has already been proven to be an effective fusion procedure for various lumbar spinal disorders. The goal of OLIF51 is to achieve bony stability, improve alignment, and indirectly decompress the neural elements at L5-S1 level via less invasive procedures together with OLIF25.
OLIF51 surgery requires adequate consideration of indications and preoperative anatomical investigations to ensure perioperative safety as well as better postoperative outcomes. Regarding the fusion rate, a previous retrospective study has reported the fusion rate of OLIF51 as much as 97.9%6), which should be investigated more in future prospective observation. The development of OLIF51 surgery has made it possible to perform lumbar anterior interbody fusion from the upper lumbar spine to L5-S1 seamlessly in a single decubitus position.
Complications
Unlike OLIF25 procedure, OLIF51 procedure causes less neural complications such as thigh numbness, and/or motor weakness in the lower extremities, and urinary injury for anatomical or procedural reasons17,18). In OLIF51 surgery, cage subsidence can happen at the rate of around 10%, and possible significant complications are vascular injury, retrograde ejaculation, and postoperative ileus6). The rate of vascular injury in cases involving OLIF51 is reported to be higher than that for traditional ALIF (4.3% vs. 3.3%, respectively)6). If an access surgeon is available, it should be better for the surgeons to achieve a safer approach to L5-S1 disc by avoiding possible significant vessel injury. However, even in a situation without an access surgeons, spine surgeons can perform the anterior L5-S1 approach with enough knowledge and technique19). In some cases, a central approach via the bifurcation is sometimes tricky as several vascular structures obstruct the operating field, as mobilization of these vascular structures is often technically demanding19-21). Some surgeons perform L5-S1 fusion via oblique lateral corridor in the same way as OLIF25 procedure by medially retracting the iliac vessels22-24). The technique can be sometimes useful in some cases with more congested iliac vessels in front of the L5-S1 junction and less-congested collateral vessels such as ascending lumbar veins in the oblique lateral corridor, but not applicable to all of the L5-S1 pathological patients and should be developed for more established certainty and safety.
Retrograde ejaculation, which is considered to result from neural injury of superior hypogastric nerve plexus5,7), has rarely reported in the OLIF51 surgery cases6). The fact is almost acceptable considering its less invasive procedure of OLIF51. To avoid postoperative sexual dysfunction, especially in male patients, careful and blunt dissection and retraction of structures within the bifurcation of the great vessels are mandatory, as is told in the traditional ALIF5).
Furthermore, the oblique approach to the L5-S1 disc space can sometimes invade contralateral foramen, often followed by a salvage revision surgery25). To avoid the possible invasion, it is important to check where the surgeons are accessing during the surgery using fluoroscopy.
Conclusion
OLIF51 procedure achieves effective anterior interbody fusion with mechanisms of indirect decompression, rigid stability, and alignment correction on the basis of less invasive anterior interbody fusion via bifurcation of great vessels using specially designed retractors. The technique also achieves seamless anterior interbody fusion when combined with OLIF25. A thorough understanding of the procedures and anatomical features is mandatory to avoid perioperative complications.
Disclaimer: Sumihisa Orita is one of the Editors of Spine Surgery and Related Research and on the journal's Editorial Committee. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Ethical Approval: N/A (Review article with a case report with patient's approval)
Author Contributions: SuO, YS, KI, YE,YA, MI, RH, TN and SeO contributed as the primary surgeons in the related surgeries. SuO wrote the manuscript. All the authors reviewed the manuscript. SF, TI, YK, and MT also contributed as the members of the assessment committee with SuO and SeO.
Acknowledgement
The illustrated materials in Fig. 2 to 6 were provided and used under the permission of Medtronic Sofamor Danek.
References
- 1.Fujibayashi S, Hynes RA, Otsuki B, et al. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2015;40(3):E175-82. [DOI] [PubMed] [Google Scholar]
- 2.Shiga Y, Orita S, Inage K, et al. Evaluation of the location of intervertebral cages during oblique lateral interbody fusion surgery to achieve sagittal correction. Spine Surg Relat Res. 2017;1(3):197-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sato J, Ohtori S, Orita S, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. 2017;26(3):671-8. [DOI] [PubMed] [Google Scholar]
- 4.Orita S, Inage K, Furuya T, et al. Oblique Lateral Interbody Fusion (OLIF): Indications and techniques. Oper Tech Orthop. 2017;27:223-30. [Google Scholar]
- 5.Takahashi K, Yamagata M, Moriya H. Sexual dysfunction after anterior lumbar interbody fusion. Chiba Med J. 1998;74:189-92. [Google Scholar]
- 6.Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. The spine journal : official journal of the North American Spine Society. 2017;17(4):545-53. [DOI] [PubMed] [Google Scholar]
- 7.Takahashi K, Kitahara H, Yamagata M, et al. Long-term results of anterior interbody fusion for treatment of degenerative spondylolisthesis. Spine. 1990;15(11):1211-5. [DOI] [PubMed] [Google Scholar]
- 8.Ploumis A, Liu H, Mehbod AA, et al. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine (Phila Pa 1976). 2009;34(15):1581-4. [DOI] [PubMed] [Google Scholar]
- 9.Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024-9. [DOI] [PubMed] [Google Scholar]
- 10.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30(6):682-8. [DOI] [PubMed] [Google Scholar]
- 11.Orita S, Inage K, Eguchi Y, et al. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 2016;26(7):685-93. [DOI] [PubMed] [Google Scholar]
- 12.Orita S, Yamagata M, Ikeda Y, et al. Retrospective exploration of risk factors for L5 radiculopathy following lumbar floating fusion surgery. J Orthop Surg Res. 2015;10(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Regan C, Kang JD. The Role of the Minimally Invasive Extreme Lateral Interbody Fusion Procedure for Complex Spinal Reconstruction. Operative Techniques in Orthopaedics. 2013;23(1):28-32. [Google Scholar]
- 14.Basho R, Chen JH. Lateral Interbody Fusion: Indications and Techniques. Operative Techniques in Orthopaedics. 2011;21(3):204-7. [Google Scholar]
- 15.Davis TT, Hynes RA, Fung DA, et al. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine. 2014;21(5):785-93. [DOI] [PubMed] [Google Scholar]
- 16.Orita S, Inage K, Kubota G, et al. One-Year Prospective Evaluation of the Technique of Percutaneous Cortical Bone Trajectory Spondylodesis in Comparison with Percutaneous Pedicle Screw Fixation: A Preliminary Report with Technical Note. J Neurol Surg A Cent Eur Neurosurg. 2016;77(6):531-7. [DOI] [PubMed] [Google Scholar]
- 17.Abe K, Orita S, Mannoji C, et al. Perioperative Complications in 155 Patients Who Underwent Oblique Lateral Interbody Fusion Surgery: Perspectives and Indications From a Retrospective, Multicenter Survey. Spine (Phila Pa 1976). 2017;42(1):55-62. [DOI] [PubMed] [Google Scholar]
- 18.Kubota G, Orita S, Umimura T, et al. Insidious intraoperative ureteral injury as a complication in oblique lumbar interbody fusion surgery: a case report. BMC Res Notes. 2017;10(1):193. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarrett CD, Heller JG, Tsai L. Anterior exposure of the lumbar spine with and without an “access surgeon”: morbidity analysis of 265 consecutive cases. J Spinal Disord Tech. 2009;22(8):559-64. [DOI] [PubMed] [Google Scholar]
- 20.Bateman DK, Millhouse PW, Shahi N, et al. Anterior lumbar spine surgery: a systematic review and meta-analysis of associated complications. The spine journal : official journal of the North American Spine Society. 2015;15(5):1118-32. [DOI] [PubMed] [Google Scholar]
- 21.Quraishi NA, Konig M, Booker SJ, et al. Access related complications in anterior lumbar surgery performed by spinal surgeons. Eur Spine J. 2013;22 Suppl 1:S16-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanno K, Ohtori S, Orita S, et al. Miniopen oblique lateral L5-s1 interbody fusion: a report of 2 cases. Case Rep Orthop. 2014;2014:603531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakita H, Shiga Y, Ohtori S, et al. Less invasive corrective surgery using oblique lateral interbody fusion (OLIF) including L5-S1 fusion for severe lumbar kyphoscoliosis due to L4 compression fracture in a patient with Parkinson's disease: a case report. BMC Res Notes. 2015;8:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chung NS, Jeon CH, Lee HD. Use of an Alternative Surgical Corridor in Oblique Lateral Interbody Fusion at the L5-S1 Segment: A Technical Report. Clinical spine surgery. 2017;31(7):293-6. [DOI] [PubMed] [Google Scholar]
- 25.Hozumi T, Orita S, Inage K, et al. Successful salvage surgery for failed transforaminal lumbosacral interbody fusion using the anterior transperitoneal approach. Clin Case Rep. 2016;4(5):477-80. [DOI] [PMC free article] [PubMed] [Google Scholar]