Abstract
Purpose:
This study examined trends in the prevalence of cardiovascular disease (CVD) and CVD risk factors among U.S. older adults and workers. We also investigated correlations between the temporal prevalence of CVD and selected risk factors (hypertension, obesity, physical inactivity, smoking, and treated diabetes) among participants.
Methods:
Data were obtained from the National Health Interview Survey (2004–2018) for U.S. adults aged greater than or equal to 50 years (n = 207,539), of which 84,180 were employed. Temporal trends in prevalence were assessed by fitting weighted regression models to the age-standardized prevalence to the 2010 U.S. population. The relationship between temporal prevalence of CVD with each risk factor was assessed using Spearman's correlation coefficient.
Results:
Among all older adults, the prevalence of CVD significantly declined (β = −0.16, P < .001) during 2004–2018; similar decline was observed among employed adults (β = −0.16, P = .001). Temporal prevalence in CVD was positively correlated to physical inactivity (r = 0.73, P = .002) and smoking (r = 0.81, P < .001), but not to any of the other risk factors.
Conclusions:
Among employed adults aged greater than or equal to 50 years, the prevalence of CVD, physical inactivity, and smoking dramatically declined over the past 15 years. The temporal decline in prevalence of CVD was significantly associated with decline prevalence of physical inactivity and smoking.
Keywords: Trend, Prevalence, CVD, Workers, NHIS
Introduction
Cardiovascular disease (CVD), including coronary heart disease and cerebrovascular disease (stroke), has been the leading cause of death in the United States during the past century [1,2]. A report by the U.S. Centers for Disease Control and Prevention showed that the U.S. death rate from CVD reached a peak in 1950 and it declined 60 percent between 1950 and 1999 [2]. Another cohort study reported that the U.S. death rate for heart disease declined 68 percent from 1969 to 2014 [3]. The major risk factors for CVD have been known to include clinical factors (hypertension, diabetes, high blood cholesterol), behavioral factors (obesity, physical inactivity, smoking, and unhealthy diet), and age [1].
CVD is prevalent among the working population in the United States [4]. CVD morbidity and mortality in the workplace has resulted in lost productivity which amounts to an annual loss of $120 billion dollars [5]. The National Institute for Occupational Safety and Health reported that CVD is a leading cause of death and permanent disability among workers, resulting in an average loss of seven years of life expectancy [6]. The National Institute for Occupational Safety and Health study revealed that workers in certain occupations and industry groups were at higher risk of CVD. Workers in community or social services and in transportation or material moving had the worst cardiovascular health among 22 occupational groups [6], and workers aged younger than 55 years in wholesale trade and in public administration sectors had the highest prevalence of CVD among 20 industry groups [7].
We aimed to 1) investigate trends in the prevalence of CVD among U.S. adults (aged 50 years and older) by employment status (employed, unemployed, not in the labor force) during a 15-year period (2004–2018), 2) analyze the trends of selected CVD risk factors (hypertension, obesity, physical inactivity, smoking, and treated diabetes) among U.S. workers during this study period, and 3) investigate which risk factors were correlated with CVD by comparing the trends of the CVD risk factors to that of CVD.
Methods
Data
CVD prevalence data were compiled from the National Health Interview Survey (NHIS) (2004–2018), conducted by the Centers for Disease Control and Prevention's National Center for Health Statistics. The NHIS is the principal source of information on the health of the civilian noninstitutionalized population of the United States. It is a representative cross-sectional survey of in-person household interviews conducted annually. Extensive details about the questionnaire, methodology, data, and documentation are available on the NHIS website https://www.cdc.gov/nchs/nhis/?#.
For the current analyses, we used data from the NHIS core questionnaires (Sample Adult, Family) collected over a 15-year period spanning from 2004 to 2018. The total number of adult respondents during 2004–2018 was 444,743 (an average response rate of 80.1%), of which 207,539 were adults ages 50 years and older (our analytic sample size).
Employment status
We classified the older adults into three categories based on employment status: employed (current workers, n = 84,180), unemployed (n = 4676), and not in the labor force (n = 118,683). The employed were paid workers who were ‘working at a job or business’ or ‘with a job or business but not at work’ during the week before their interview. The unemployed were those who were not working and looking for job. Persons classified as not in the labor force were neither working at a job nor looking for work such as retirees, persons at home due to household responsibilities, ill health, or disability and other similar reasons.
CVD and risk factors
The NHIS questionnaire collected information from participants on CVD and risk factors for CVD (hypertension, treated diabetes, physical inactivity, smoking, and obesity). Prevalence of CVD was based on the number of adults who reported that they had ever been told by a doctor or other health practitioner that they had coronary heart disease, angina pectoris, heart attack, any kind of heart condition or disease, or stroke. Hypertension was based on those who reported that they had ever been told by a doctor or other health professional that they had high blood pressure. Treated diabetes was defined as those who reported that they were taking diabetic pills or taking insulin by shot or pump to lower their blood sugar. Physical inactivity was defined as not participating in any leisure-time aerobic activity that lasted for at least 10 minutes. Smoking was defined as currently smoking cigarettes every day or some days and more than 100 cigarettes in entire life. Obesity was defined as having a body mass index (BMI) higher than 30 kg per m2.
Data analysis
To account for the complex survey design, all prevalence estimates (%) were weighted using the NHIS individual sample adult weights and the estimates were age standardized to the 2010 U.S. population. Prevalence estimates were age standardized to the 2010 U.S. worker population estimates by Bureau of Labor Statistics, using five age groups: 50–54, 55–59, 60–64, 65–69, and 70+ years. Temporal trends in CVD and the selected risk factors were assessed by fitting weighted regression models to the age-standardized prevalence. The temporal relationship between the prevalence of CVD and each risk factor was assessed using Spearman's correlation coefficients. SAS-callable SUDAAN, v11 was used for statistical analyses. All reported P-values were two-sided, and a P-value of less than .05 was considered statistically significant.
Results
Among all U.S. older adults, the age-standardized prevalence of CVD gradually declined (β = −0.16, P < .001) between 2004 and 2018 (Fig. 1). The slopes of the prevalence of CVD for those employed and not in the labor force (β = −0.16, P = .001 and β = −0.18, P = .002, respectively) were similar to those for all older adults.
Fig. 1.
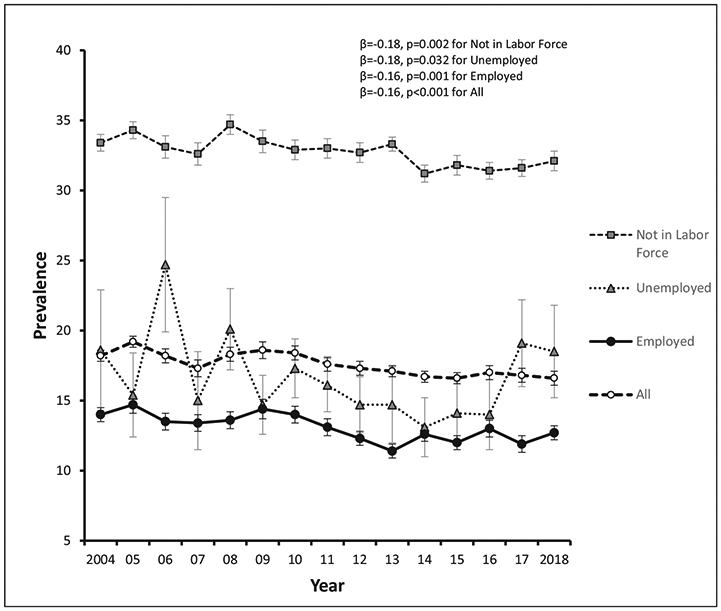
Temporal trends in prevalence of CDV among U.S. oder adults (age ≥ 50 years) by employment status.
Figure 2 presents temporal trends in prevalence of CVD and CVD risk factors among employed U.S. older adults. The age-standardized prevalence of CVD, physical inactivity, and smoking significantly declined during the study period (β = −0.16, P = .001; β = −1.08, P < .001; β = −0.34, P < .001, respectively), whereas the prevalence of hypertension, obesity, and treated diabetes increased (β = 0.17, P = .038; β = 0.42, P < .001; β = 0.21, P < .001, respectively). The prevalence of physical inactivity was drastically reduced from 38% in 2004 to 24% in 2018.
Fig. 2.
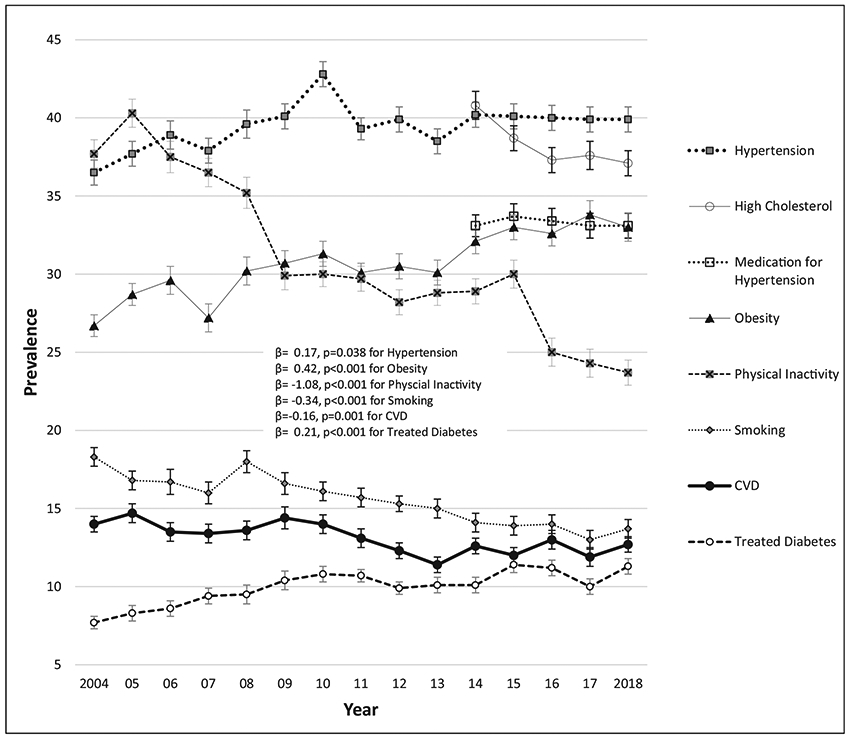
Temporal trends in prevalence of CVD and selected risk factors among U.S. older workers (age ≥50 years). Spearman correlation coefficient between the prevalence of CVD and the CVD risk factors was as follows: physical inactivity (r = 0.73, P = .002), smoking (r = 0.81, P < .001), treated diabetes (r = −0.43, P = .108), hypertension (r = −0.24, P =.388), and obesity (r = −0.57, P = .028).
Spearman correlation coefficient between the prevalence of CVD and the CVD risk factors was as follows: physical inactivity (r = 0.73, P = .002), smoking (r = 0.81, P < .001), treated diabetes (r = −0.43, P = .108), hypertension (r = −0.24, P =.388), and obesity (r = −0.57, P = .028). Correlation coefficients indicated that decline in CVD was positively correlated to decline in physical inactivity (r = 0.73, P = .002) and smoking (r = 0.81, P < .001). Temporal prevalence of CVD was found to be inversely correlated to that of obesity (r = −0.57, P = .028), which is contrary to our expectation.
Discussion
In this study, we investigated temporal trends in CVD and CVD risk factors for the U.S. adults aged 50 or older (overall, and by employment status). The prevalence of CVD had dropped 2.5% between 2004 and 2018. The 2.5% drop means that approximately 142,000 fewer workers were diagnosed with CVD in 2018 than in 2004 based on the U.S. 2010 standardized population. As expected, the decline in prevalence of CVD and that of physical inactivity and smoking were highly and significantly correlated because the prevalence of both physical inactivity and smoking also significantly decreased during the same period.
Although the prevalence of physical inactivity and smoking decreased, the prevalence of hypertension, another major risk factor for CVD, increased during the study period. We noticed, however, that in 2014–2018, the mean prevalence of hypertension leveled off around 40% and the mean prevalence of treated hypertension was 33% during the same period (Fig. 2). Therefore, we can infer that approximately 83% (i.e., 33%/40%) of older workers with hypertension were prescribed and taking medication to lower blood pressure during that period. The proportion of treatment for hypertension in recent years was an improvement compared with that in the late of 1990s, when only 55% were reported as being treated [8,9].
We observed an inverse correlation between the prevalence of obesity and CVD. When obesity is measured as BMI, and those with higher BMI have fewer cardiovascular events or less mortality than those with lower BMI, this unusual finding has been termed the ‘obesity paradox’ [10-13]. Flegal et al. showed that the obesity paradox occurred in older persons [10]. This is one possible explanation for the inverse correlation observed between obesity and CVD in our study because the sample comprised many older workers (age e50 years). Another explanation is that because obesity was assessed as BMI greater than or equal to 30 kg per m2, this measurement does not truly assess an excess of fat mass; it may actually assess an increased amount of lean mass [14]. Nevertheless, obesity is a well-known public health problem and needs effective interventions. It has been suggested that there should be a more aggressive public health campaign against obesity which could include higher taxes on sugary drinks and refined foods among other strategies [15]. This campaign could specifically target certain segments of the population that may have higher consumption of less nutritious food and drink, such as blue-collar workers, persons at the lower end of the socioeconomic ladder, those working irregular shift schedules, and those who are obese and morbidly obese [6,7,16].
The overall trends of CVD and CVD risk factors among older workers mask important differences in trends of prevalence by occupational or industry groups. Occupational or industry groups have unique working environments, and their causes or treatment for CVD may differ. For example, Shockey et al. [6] reported that workers in transportation and material moving had the highest prevalence of hypertension, obesity, and physical inactivity, whereas those in personal care and service had highest levels of blood glucose, and those in farming, fishing, and forestry had the poorest dietary habits. To continue to reduce the burden of CVD, there should be collaboration between the employer and employees in each occupational environment to develop specific prevention strategies in addition to the individual efforts of workers.
There are a few limitations that must be considered in this study. Because linear regression was applied to see the temporal trends for the entire period, there is a potential to overlook the change (increase, decrease, or no change) of prevalence in certain specific periods. For example, we see that the overall trend in prevalence of CVD (β = −0.16) (after analysis in linear regression) decreased over the study period 2004–2018. However, after analysis in joinpoint regression (data results not shown here), the trend in prevalence of CVD looked flat during 2004–2010 (β = −0.04), rapidly decreased during 2010–2013 (β = −0.67), and increased during 2013–2018 (β = 0.18). Because the prevalence of CVD or CVD risk factors was based on self-reported responses, it may be subject to recall bias. It is also possible that several members of high-risk groups did not participate in the survey and that may have underestimated the prevalence. In addition, because of the limits of the data source, we did not investigate other risk factors for CVD, such as dietary habits and medical history (prior history of CVD, clinical treatments by specialists and health care providers, emergency medical services, etc.) [2]. Treatment for high cholesterol is one of the key elements for reducing CVD risk. Because the NHIS data 2004–2013 did not ask if the participants had taken medications to lower lipids or blood pressure, we were unable to include this information in our analysis. For the employed adults, we should have considered occupational risk factors of CVD, such as shift work schedules, work-related stress, severity of workload, total work hours, the organizational environment, and so forth.
Despite these limitations, to our knowledge, this is one of few studies investigating the association between CVD and associated risk factors over the past 2 decades and the only one that used nationally representative data of the working population with a high response rate (80%). This analysis of a nationally representative sample of older workers with information on CVD status and CVD risk factors provides a meaningful reference for future research on heart disease or stroke. Additional years of data on other CVD risk factors are needed to improve our ability to understand these temporal trends and their relationships with CVD.
Acknowledgments
Grant funding: No.
Footnotes
Disclosure: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Conflicts of interest: None of the authors have any conflicts of interest.
References
- [1].Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. , on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics - 2019 update: a report from the American Heart Association. Circulation 2019;139:e56–528. [DOI] [PubMed] [Google Scholar]
- [2].CDC. Decline in deaths from heart disease and stroke, United States, 1990-1999 Washington, DC: MMWR Morb Mortal Wkly Rep 1999;48(30):649–56. [PubMed] [Google Scholar]
- [3].Weir HK, Anderson RN, Coleman King SM, Soman A, Thompson TD, Hong Y, et al. Heart Disease and Cancer Deaths - Trends and Projections in the United States, 1969-2020. Prev Chronic Dis 2016;17(13):E157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Leigh PJ, Miller TR. Job-related diseases and occupations within a large workers' compensation data set. Am J Ind Med 1998;33:197–211. [DOI] [PubMed] [Google Scholar]
- [5].Carnethon M, Whitsel LP, Franklin BA, Kris-Etherton P, Milani R, Pratt CA, et al. , American Heart Association Advocacy Coordinating Committee; Council on Epidemiology and Prevention; Council on the Kidney in Cardiovascular Disease; Council on Nutrition, Physical Activity and Metabolism. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation 2009;120:1725–41. [DOI] [PubMed] [Google Scholar]
- [6].Shockey TM, Sussell AL, Odom EC. Cardiovascular Health Status by Occupational Group - 21 States, 2013. MMWR Morb Mortal Wkly Rep 2016;65: 793–8. [DOI] [PubMed] [Google Scholar]
- [7].Luckhaupt SE, Calvert GM. Prevalence of coronary heart disease or stroke among workers aged <55 years – United States, 2008-2012. MMWR Morb Mortal Wkly Rep 2014;63(30):645–9. [PMC free article] [PubMed] [Google Scholar]
- [8].Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. , on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation 2016;133(4): e38–360. [DOI] [PubMed] [Google Scholar]
- [9].Joint National Committee (JNC) on Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med 1997;157(24):2413–46. [DOI] [PubMed] [Google Scholar]
- [10].Flegal K, Kit B, Orpana H. Association of all-cause mortality with overweight and obesity using standard body mass index categories – a systematic review and meta-analysis. JAMA 2013;309(1):71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Carnethon MR, De Chavez PD, Bigg ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of weight status with morality in adults with incident diabetes. JAMA 2012;308(6):581–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ades PA. The obesity paradox: perception vs knowledge. Mayo Clin Proc 2010;85(2):112–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hainer V, Aldhoon-Hainerova I. Obesity paradox does exit. Diabetes Care 2013;36(S2):S276–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, Lavie CJ. Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag 2019;15:89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jou J, Techakehakij W. International application of sugar-sweetened beverage (SSB) taxation in obesity reduction: Factors that may influence policy effectiveness in county-specific contents. Health Policy 2012;107: 83–90. [DOI] [PubMed] [Google Scholar]
- [16].Elser H, Falconi AM, Bass M, Cullen MR. Blue-collar work and women's health: a systematic review of the evidence from 1990 to 2015. Popul Health 2018;6:195–244. [DOI] [PMC free article] [PubMed] [Google Scholar]


