Abstract
Large bowel perforation is an acute abdominal emergency requiring rapid diagnosis for proper treatment. The high mortality rate associated with large bowel perforation underlines the importance of an accurate and timely diagnosis. Computed tomography is useful for diagnosis of ingested foreign bodies, and endoscopic repair using clips can be an effective treatment of colon perforations. We herein describe a 78-year-old man with sigmoid colon perforation caused by accidental swallowing of a jujube pit. The jujube pit had become stuck in the wall of the sigmoid colon and was successfully removed by colonoscopy, avoiding an aggressive surgery. As a result of developments in endoscopic techniques, endoscopic closure has become a feasible option for the management of intestinal perforation.
Keywords: Perforation, foreign body, jujube, colonoscopy, computed tomography, endoscopic repair
Introduction
The overall mortality rate from large bowel perforation reportedly ranges from 16.9% to 19.6%, emphasizing the importance of an accurate and timely diagnosis.1,2 Computed tomography is considered the method of choice for identifying ingested foreign bodies and their complications because of to its high-quality multiplanar capabilities and high resolution.3 Endoscopic repair using clips can be effective for the treatment of colon perforations that occur during diagnostic colonoscopy.4 Most foreign bodies can pass through the gastrointestinal tract without any complications, but a small proportion can cause complications involving perforation, obstruction, and fistula formation, which may be fatal.5,6 We herein present a rare case of successful diagnosis and treatment of sigmoid colon perforation due to a jujube pit.
Case presentation
A 78-year-old male farmer presented to the emergency department of our hospital with a 13-day history of umbilical abdominal pain, nausea, and vomiting. The patient had received medical treatments for presumed gastroenteritis at a local hospital. However, 1 day before presentation to our hospital, his abdominal pain had gradually increased and he had developed anal exhaust reduction and bloody stools. He had a history of chronic bronchitis but was otherwise clinically well. Physical examination revealed moderate obesity with a distended abdomen and umbilical abdominal tenderness. Fresh blood was observed on anal examination.
Laboratory examination revealed evidence of peritoneal irritation: the white blood cell count was 13.6 × 109/L (reference range, 3.5–10.5 × 109/L), and the C-reactive protein concentration was 50.3 mg/L (reference range, <10 mg/L). Abdominal computed tomography (CT) showed a high-density lesion (foreign body) in the colon, evidence of abdominal infection and an incomplete jejunal obstruction (Figures 1, 2). Colonoscopy showed a circumferential ulcer in the sigmoid colon and a 3-cm jujube pit piercing the wall of the sigmoid colon (Figures 3, 4).
Figure 1.
Computed tomography scan of the abdomen revealing a hyperdense lesion within the colon (black arrow).
Figure 2.
Computed tomography scan of the abdomen revealing a high-density lesion (foreign body) in the colon, evidence of abdominal infection, and an incomplete jejunal obstruction (black arrow).
Figure 3.
A jujube pit was observed piercing the wall of the sigmoid colon.
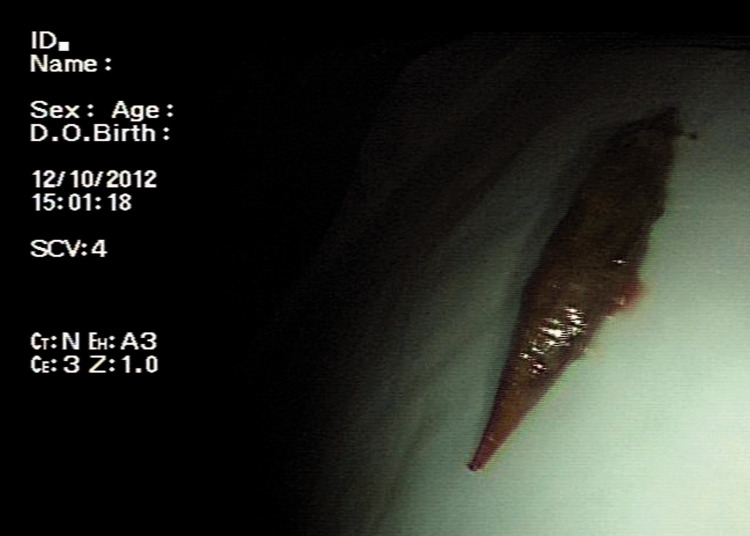
Figure 4.
The 3-cm jujube pit.
Using colonoscopy, we firmly grasped the sharp end of the jujube pit and covered it by a snare. We then drew it toward the scope, with the bowel lumen maintained at the center of the visual field to avoid mucosal injury. Once the object was removed, a second-look colonoscopic examination was performed to check for complications, thereby avoiding an aggressive surgery. The patient was treated with antibiotics for 7 days and discharged from the hospital with no early complications.
Discussion
A large bowel perforation is an abdominal emergency with multiple etiologies. Foreign body inhalation is a common cause of colonic perforation.7 Most foreign bodies that reach the gastrointestinal tract will pass spontaneously, although impaction may occur at areas of anatomical narrowing (upper esophageal sphincter, lower esophageal sphincter, pylorus, ileocecal valve, and anus).8–12 Fraga et al.13 analyzed the frequency of perforation according to its location in 236 patients. The most common location was the small bowel (39.8%), followed by the duodenum (22.0%), colon (20.3%), rectum (10.6%), and sigmoid colon (5.5%).
The overall mortality rate from large bowel perforation reportedly ranges from 16.9% to 19.6%, emphasizing the importance of an accurate and timely diagnosis.2,7 However, localizing the perforation site can be challenging. Multidetector CT is the most reliable imaging method for the diagnosis of large bowel perforation, predicting the perforation site with an accuracy of 82% to 90%.14 In our case, CT revealed wall thickening and an abscess of the sigmoid colon, consistent with perforation of the large intestine.
Most foreign bodies will pass through the gastrointestinal tract uneventfully, but long and pointy foreign bodies such as toothpicks, fish bones, and sharp jujube pits as in the present case are more likely to require surgical or endoscopic removal. Perforation of the sigmoid colon caused by a jujube pit is rare. Surgery is usually inevitable if foreign bodies cannot be extracted endoscopically.15
Large bowel perforation is a common acute abdominal disease that requires rapid diagnosis and effective treatment. In our case, a jujube pit that had become stuck in the wall of the sigmoid colon was successfully removed by colonoscopy, thereby avoiding an aggressive surgical strategy. In the absence of peritoneal signs or clinical instability, a minimally invasive approach via colonoscopy can be a safe, efficient means of removing sharp objects, reducing the risk of distal perforation and the need for surgery.16 As a result of developments in endoscopic techniques, endoscopic closure has become a feasible option for the management of perforation.
Footnotes
Ethics: This study was approved by the hospital ethics committee of HwaMei Hospital, University of Chinese Academy of Sciences. The patient provided written informed consent.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Bielecki K, Kaminski P, Klukowski M. Large bowel perforation: morbidity and mortality. Tech Coloproctol 2002; 6: 177–182. [DOI] [PubMed] [Google Scholar]
- 2.Kriwanek S, Armbruster C, Beckerhinn P, et al. Prognostic factors for survival in colonic perforation. Int J Colorectal Dis 1994; 9: 158–162. [DOI] [PubMed] [Google Scholar]
- 3.Venkatesh SH, Venkatanarasimha Karaddi NK. CT findings of accidental fish bone ingestion and its complications. Diagn Interv Radiol 2016; 22: 156–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JS, Kim BW, Kim JI, et al. Endoscopic clip closure versus surgery for the treatment of iatrogenic colon perforations developed during diagnostic colonoscopy: a review of 115,285 patients. Surg Endosc 2013; 27: 501–504. [DOI] [PubMed] [Google Scholar]
- 5.Pinero Madrona A, Fernandez Hernandez JA, Carrasco Prats M, et al . Intestinal perforation by foreign bodies. Eur J Surg 2000; 166: 307–309. [DOI] [PubMed] [Google Scholar]
- 6.Pulat H, Karakose O, Benzin MF, et al. Small bowel perforation due to fish bone: a case report. Turk J Emerg Med 2015; 15: 136–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown CV. Small bowel and colon perforation. Surg Clin North Am 2014; 94: 471–475. [DOI] [PubMed] [Google Scholar]
- 8.Pavlidis TE, Marakis GN, Triantafyllou A, et al. Management of ingested foreign bodies. How justifiable is a waiting policy? Surg Laparosc Endosc Percutan Tech 2008; 18: 286–287. [DOI] [PubMed] [Google Scholar]
- 9.Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002; 55: 802–806. [DOI] [PubMed] [Google Scholar]
- 10.O'Donnell ME, Gibson N, Sharif MA, et al. Crohn's disease of the terminal ileum: a cheap diagnosis. Ir J Med Sci 2008; 177: 401–403. [DOI] [PubMed] [Google Scholar]
- 11.Abraham B, Alao AO. An unusual foreign body ingestion in a schizophrenic patient: case report. Int J Psychiatry Med 2005; 35: 313–318. [DOI] [PubMed] [Google Scholar]
- 12.Murshid KR, Khairy GE. Laparoscopic removal of a foreign body from the intestine. J R Coll Surg Edinb 1998; 43: 109–111. [PubMed] [Google Scholar]
- 13.Fraga M, Nydegger A, Abdelrahman K, et al. [Digestive foreign body management]. Rev Med Suisse 2015; 11: 1592–1595. [PubMed] [Google Scholar]
- 14.Kim SH, Shin SS, Jeong YY, et al. Gastrointestinal tract perforation: MDCT findings according to the perforation sites. Korean J Radiol 2009; 10: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho MK, Lee MS, Han HY, et al. Fish bone migration to the urinary bladder after rectosigmoid colon perforation. World J Gastroenterol 2014; 20: 7075–7078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hershman M, Shamah S, Mudireddy P, et al. Pointing towards colonoscopy: sharp foreign body removal via colonoscopy. Ann Gastroenterol 2017; 30: 254–256. [DOI] [PMC free article] [PubMed] [Google Scholar]