Abstract
The COVID-19 crisis has forced a sudden and dramatic shift in the way that clinicians interact with their patients, from outpatient encounters to telehealth visits utilizing a variety of internet-based videoconferencing applications. Although many aspects of pre–COVID-19 outpatient sports medicine care will ultimately resume, it is likely that telehealth will persist because of its practicality and because of patient demand for access to efficient and convenient health care. Physical examination is widely considered a critical obstacle to a thorough evaluation of sports medicine patients during telehealth visits. However, a closer reflection suggests that a majority of the examination maneuvers are possible virtually with limited, if any, modifications. Thus, we provide a comprehensive shoulder and knee physical examination for sports medicine telehealth visits, including (1) verbal instructions in layman’s terms that can be provided to the patient before or read verbatim during the visit, (2) multimedia options (narrated videos and annotated presentations) of the shoulder and knee examination that can be provided to patients via screen-share options, and (3) a corresponding checklist to aid in documentation.
Keywords: telemedicine, telehealth, physical examination, virtual examination, knee examination, shoulder examination
The COVID-19 crisis has resulted in a sudden and dramatic shift in the delivery of clinical care for patients with sports medicine injuries, away from in-person outpatient clinic visits to remote telehealth evaluations.48,62 Web-based videoconferencing platforms are widely available, are user-friendly, and enable face-to-face patient-clinician interaction.23 As a consequence of social distancing measures and imposed restrictions on in-person evaluations, clinicians and patients have been forced to embrace videoconferencing regardless of their previous notions. Several studies across an array of medical disciplines have reported that, compared with in-person visits, telehealth visits have similar patient satisfaction levels while concomitantly reducing travel costs, visit times, wait times, and overall health care costs.3,46,50,71,72 Despite its increasing utilization in other health care disciplines, telehealth was not widely adopted by sports medicine practitioners before the COVID-19 crisis.38 However, we now recognize that telehealth is an effective option for musculoskeletal care and will likely endure even after the pandemic, driven by physician and patient demand for efficiency and convenience.38,44,48,62 One common stance was that musculoskeletal telehealth visits are limited without an in-person physical examination.9,28,29,66,67 Although 1 recently published study described basic physical examination components,62 to our knowledge, we provide below the first comprehensive description of a shoulder and knee physical examination for telehealth purposes.
The purpose of this article was to provide clinicians with a comprehensive shoulder and knee physical examination for the telehealth visit, including (1) verbal instructions in layman’s terms that can be provided to the patient before or read verbatim during the visit, (2) multimedia options (narrated videos and annotated presentations) of the shoulder and knee examination that can be provided to patients via screen share options, and (3) a corresponding checklist for documentation.
PREPARATION FOR TELEHEALTH VISIT
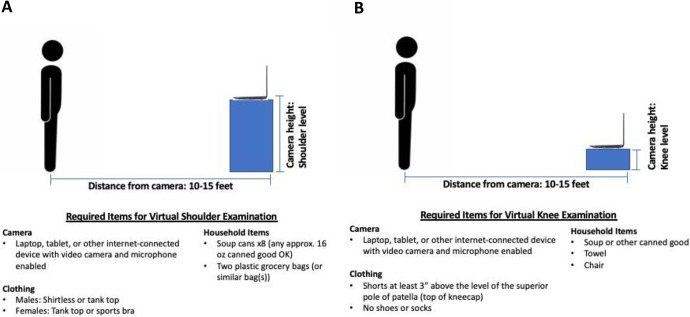
Before the telehealth visit, baseline information should be provided by the patient, including specific questions regarding their chief complaint, history of present illness, medical and surgical history, allergies, home medications, social history, and a review of systems. The patient should also review instructions on how to set up one’s camera to adequately visualize the affected joint or area of interest. At the start of the visit, the patient should be seated with his or her camera at eye level. During the physical examination, patients will be asked to reposition themselves and their camera based on the body part being examined. The required distance and angle of the camera will vary by the type of camera and patient position (Figure 1). Furthermore, it is important for the patient to be dressed in appropriate clothing in preparation for the telehealth visit. Guidelines for appropriate clothing, exam space, patient positioning, camera positioning, and required common household items are provided. Available support from information technology is helpful for troubleshooting any technical difficulties.
Figure 1.
Schematic of a virtual examination for the (A) shoulder and (B) knee.
SHOULDER EXAMINATION
Before the start of the shoulder exam, the patient should review the guidelines provided in Appendix Table A1 (available as supplemental material). The shoulder exam should include an evaluation of the cervical spine, including an assessment of range of motion and the location of pain as well as the Spurling test.28,68,69 When a patient presents with undifferentiated shoulder and neck pain, it is important to rule out a neurological or cervical cause of the patient’s symptoms.28,29,76 The Spurling test can be helpful in suggesting a diagnosis of cervical disc disease.28,68,69
The shoulder exam can be broadly divided into a core exam and abnormality-specific special testing. The core exam includes an overall inspection, assessment of the localization of pain, range of motion testing, motor testing, sensory testing, and peripheral vascular exam. Further special testing can be tailored by the clinician depending on the patient’s suspected injury.28,29,66,67 A comprehensive description of the entire virtual shoulder exam is available in Appendix Table A1, and illustrated examples of each shoulder physical examination component along with written instructions is available in Appendix 1 (available as supplemental material). Video examples of the core exam and abnormality-specific special testing are also available (see Video Supplements 1-4). Each of these items may be shared with patients.
Core Shoulder Examination
The core shoulder examination components are shaded in blue in Appendix Table A1. An inspection of both shoulders should evaluate for obvious muscle atrophy, deformities, prior incisions, scars, skin lesions or rashes, swelling, ecchymosis, or erythema. The patient should be asked to turn so that the camera is able to visualize the front, side, and back of the affected shoulder for a thorough inspection (Appendix 1). The latter view may be particularly useful for identifying rotator cuff atrophy. The patient will be asked to identify the location of maximal pain by pointing to the area with a single finger. Range-of-motion testing should be performed, assessing for symmetry and limitations due to pain. Shoulder forward flexion should be visualized from the side, external rotation and abduction with the patient directly facing the camera, and internal rotation with the patient’s back to the camera (see Video Supplement 1). Previous studies have leveraged technologies, including smartphone applications, virtual goniometers, and motion-sensing devices, such as accelerometers and gyroscopes, to evaluate shoulder range of motion.7,75,78 Strength testing should be performed against gravity and with the use of common household items.62 Sensory testing and a peripheral vascular examination can be performed independently by the patient and should be compared with the contralateral extremity. For sensory testing, the patient will be asked if he or she has any areas of numbness, burning, or tingling and may be asked about specific anatomic locations. For the peripheral vascular exam, the patient can be asked if one hand feels cooler than the other and may also perform an assessment of capillary refill. Scapulothoracic kinematics and dynamic motion are often associated with shoulder injuries.29,35,45,63 Bilateral scapulae can be assessed using the Kibler test, which is performed by assessing bilateral scapular motion during shoulder elevation in the sagittal and scapular planes and may be graded as “normal” or “scapular dyskinesis.”5
Special Testing
Abnormality-specific special testing can be subdivided into impingement/rotator cuff injury, glenohumeral instability, acromioclavicular (AC) joint arthrosis, biceps-labrum complex (BLC) disease, thoracic outlet syndrome, and generalized ligamentous laxity.28,29,66,67 Most special tests can be completed independently by the patient with only minor alterations to the originally described techniques (Figure 2).
Figure 2.
Modifications to common maneuvers for a virtual shoulder examination. (A) The Jobe test (thumbs down in abduction) with soup cans in a grocery bag for resistance. (B) Resisted external rotation testing. (C) Resisted internal rotation testing. (D) The Hawkins test using the contralateral hand to push the abducted shoulder into internal rotation. (E) Cross-body adduction using the contralateral arm. (F) The O’Brien (active compression) test with the thumb pointed down and resistance provided by soup cans in a grocery bag. (G) The O’Brien test with the thumb pointed up.
An additional remote examiner, such as a family member, can help facilitate the performance of these provocative maneuvers but is not a prerequisite. The patient will be guided through each test by a detailed verbal explanation in real time. The sensitivity, specificity, and likelihood ratios for the in-person version of these exams are provided for each test, where available.
Rotator Cuff and Impingement
See Appendix Table A1 (available as supplemental material). The Neer and Hawkins tests are useful screening tests for rotator cuff injuries and can be performed by having the patient use one’s contralateral extremity for assistance.26–28,31,39,46,66 Rotator cuff strength testing can be performed using household items (Table 1).
TABLE 1.
Common Household Items for Strength Testing
| Approximate Weight, lb/kg | Preferred Household Item(s)a | Alternative Household Item(s)b |
|---|---|---|
| 1.0/0.5 | 1 canned good | 12- to 16-oz bottle of water, soda, or juice |
| 4.0/2.0 | 4 canned goods | 2-L bottle of soda; carton of milk |
| 8.0/4.0 | 8 canned goods | Gallon of water or milk; large bottle of laundry detergent or bleach |
aApproximately 12-16 fl oz per canned good (soup, beans, diced tomatoes, etc).
bAvoiding glass objects.
We recommend using 2 plastic grocery bags (double bag) and cans of soup or vegetables weighing approximately 16 oz each. The addition of more cans to the grocery bag increases the resistance during strength testing and allows for a modified strength grade. The grocery bag handles allow strength testing to be performed with the thumb pointed upward or downward. We have developed a modification of the Jobe test in which the patient holds a grocery bag with soup cans with the thumb pointed down at shoulder level in the scapular plane (see Video Supplement 2).26–28,31,39,46,66 To evaluate the teres minor, the hornblower or Patte test can be performed with the patient directly facing the camera.13,26,27,73 The belly press and liftoff tests can be performed entirely by the patient, with the affected side facing the camera.4,26,27,31,60,77
AC Joint and BLC
See Appendix Table A1 (available as supplemental material). A useful screening tool for identifying AC joint injuries is the assessment of tenderness to palpation over the AC joint, which may be performed by the patient using the contralateral hand.26–28,66,74 The cross-body adduction test can also be performed independently by the patient.12,26,27,74
The Speed and Yergason tests are good confirmatory tests for proximal biceps injuries that can be modified to be performed entirely by the patient.5,6,21,28,30,66 Tenderness to palpation of the biceps tendon and the O’Brien active compression test are also screening tests for BLC disease including the extra-articular bicipital tunnel.64 We have modified the O’Brien test to be performed by the patient alone using a grocery bag with soup cans (see Video Supplement 3).
Glenohumeral Instability
See Appendix Table A1 (available as supplemental material). The anterior apprehension test is an excellent screening and confirmatory test for diagnosing anterior shoulder instability,18,28,66 and this can be performed by instructing the patient to place the affected shoulder in a thrower’s position (abduction and 90° of external rotation). The posterior stress test for posterior instability and the sulcus test for inferior or multidirectional instability have also been modified to be performed entirely by the patient (see Video Supplement 4).
The maneuvers comprising the Beighton score (Appendix Table A1) and Roos test can be performed independently by the patient to evaluate for generalized joint hypermobility and thoracic outlet syndrome, respectively.8,33
Postoperative Shoulder Examination
The postoperative virtual shoulder examination is a condensed version of the core shoulder exam intended for patients during the first 6 postoperative weeks. This is intended to evaluate for any concerning findings that would suggest the necessity for an in-person evaluation. The camera must be positioned to fully visualize the operative shoulder so that the clinician can assess for incisional wound healing, surrounding erythema, drainage, ecchymosis, or rashes. Range of motion (testing when appropriate) can be compared with the contralateral side as outlined above. A virtual goniometer can be particularly useful to assess range of motion and assess progress between postoperative visits.19,62
KNEE EXAMINATION
Before the start of the knee examination, the patient should review the guidelines provided in Appendix Table A2 (available as supplemental material). When a patient presents with undifferentiated lower extremity pain and low back pain, it is important to rule out a neurological cause of the patient’s symptoms. Hip or vascular injuries should also be considered in the evaluation of undifferentiated lower extremity pain.
The knee exam can be broadly divided into a core exam and abnormality-specific special testing. The core exam includes an overall inspection, palpation, range-of-motion testing, motor testing, sensory testing, and peripheral vascular exam.9 Special testing can be tailored by the clinician depending on the patient’s suspected abnormality (Figure 3). A comprehensive description of the entire virtual knee exam is available in Appendix Table A2, and illustrated examples of each knee physical exam component along with written instructions is available in Appendix 2 (available as supplemental material). Video examples of the core exam and abnormality-specific special testing are also available (see Video Supplements 5-8). Each of these items may be shared with patients.
Figure 3.
Modifications to common maneuvers for a virtual knee examination. (A) The lever test for anterior cruciate ligament integrity. A soup can is placed beneath the calf, and the distal femur is pushed downward with both hands. A positive test result is an objective and visual finding in which the patient’s heel does not rise off of the table. (B) The bounce test with a soup can placed beneath the heel. The patient is asked to slightly bend the knee and then allow it to bounce down so that it is completely straight, repeating this several times quickly. (C) Patellar apprehension test with the ankle of the affected leg crossed over the contralateral ankle and both thumbs used to apply a lateral directed force on the medial facet of the patella. (D) Hyperflexion test with a towel wrapped around the anterior ankle, which is used to pull the knee into hyperflexion. The towel is allowed to relax and then pulled back again several times quickly.
Core Knee Examination
The core knee exam components are shaded in blue in Appendix Table A2. The knee exam should include an evaluation of the patient’s gait. An inspection of the bilateral lower extremities should evaluate for alignment, obvious muscle atrophy, deformities, incisions, scars, skin lesions or rashes, swelling, ecchymosis, or erythema. The patient should be asked to turn so that the camera is able to visualize the front, sides, and back of the knee for a thorough inspection (Appendix 2). The patient should be asked to identify the location of maximal pain by pointing to that area with a single finger. Range-of-motion testing should be performed while assessing for symmetry and pain (see Video Supplement 5). The use of a virtual goniometer can aid in the evaluation of alignment and range of motion.19,62 Sensory testing and a peripheral vascular exam can be performed by the patient and should be compared with the contralateral side. Strength testing requires a remote examiner such as a family member.
Special Testing
Abnormality-specific special testing can be subdivided into ligamentous instability, meniscal injury, and patellofemoral joint injury.
Ligamentous Instability
See Appendix Table A2 (available as supplemental material). The lever test has been shown to be more sensitive than other tests for the diagnosis of anterior cruciate ligament (ACL) injuries, including the Lachman test.9,37 The modification of the lever test, in which the examiner presses downward on the distal femur of the leg with the examiner’s other fist positioned beneath the calf, is particularly well suited for a telehealth evaluation.32 A positive test result is an objective and visual finding in which the patient’s heel does not rise off of the table; this does not rely on a subjective determination such as the Lachman and anterior drawer tests. To evaluate for posterior cruciate ligament injuries, the posterior sag test53 and quadriceps active test9,15,53 can be used. Both tests should be performed with the camera viewing the knee from the side with the patient supine (see Video Supplement 6).
Meniscal Injury
See Appendix Table A2 (available as supplemental material). Several tests have been described to evaluate for meniscal injuries, and we have modified some of them to be performed by the patient alone, including the bounce test and hyperflexion test.9,40 The Thessaly test can be performed by the patient independently while directly facing the camera (see Video Supplement 7).9,22,25
Patellofemoral Joint Injury
See Appendix Table A2 (available as supplemental material). The J-sign indicates patellar maltracking and can be observed with the patient directly facing the camera in a seated position.9,40,47,57 Patellofemoral crepitation is easily assessed by patients independently. Crepitus is typically enhanced by knee extension against resistance, and thus, the patient is encouraged to do this with the help of a family member. We have modified the patellar apprehension test to be performed entirely by the patient in a supine position (see Video Supplement 8).9,40 A single-leg squat performed with the patient directly facing the camera can demonstrate valgus, internal rotation collapse indicative of neuromuscular imbalance, or a hip injury that may contribute to knee pain. The maneuvers comprising the Beighton score (knee and elbow recurvatum, thumb to forearm apposition, and lumbar flexion) can be performed by the patient to evaluate for generalized joint hypermobility (Appendix Table A2).33
Postoperative Knee Examination
The postoperative virtual knee exam is a condensed version of the core knee exam. Depending on the procedure performed, time point postoperatively, and weightbearing status, the patient’s gait can be assessed. The camera must be positioned to fully visualize the operative knee so that the clinician can assess for wound healing, surrounding erythema, drainage, ecchymosis, or rashes. The camera should be positioned so that bilateral knees are visible to compare and assess swelling and the presence or absence of effusion. Range of motion (testing when appropriate) can be compared with the contralateral side as outlined above. A virtual goniometer can be particularly useful to assess range of motion and assess progress between postoperative visits.19,62
IMPLEMENTATION OF VIRTUAL PHYSICAL EXAMINATION
Similar to an in-person new patient visit, our recommendation is that the physical examination for a telehealth patient start with the “core exam,” followed by additional abnormality-specific special testing as clinically appropriate. The specific special tests performed during a virtual physical exam should be directed by the patient’s history of present illness and basic exam findings. The clinician can select specific physical exam tests from the menu of maneuvers pertinent to the presenting shoulder or knee chief complaint. The time required to perform an exam can vary based on a variety of factors. In our experience, the core knee and shoulder exams as listed require approximately 5 minutes to complete, and the problem-focused exam takes approximately 5 to 10 minutes to complete. The efficiency of the virtual exam can be optimized by choosing a sequence of exam maneuvers that minimize the number of times that the patient has to change between standing, sitting, and supine positions, and this has been incorporated into our core shoulder and knee exams. Three clinical workflow strategies may be implemented by clinicians:
Exam reveal: The clinician exposes the patient to the requisite physical exams for the first time during the telehealth visit. While this has the advantage of eliminating the need for an extensive review of data by the clinician and/or office staff before the telehealth visit, it often adds time to the visit itself because of the need for the clinician to explain, review, and clarify the different physical exam maneuvers.
Comprehensive preview: The clinician may choose to review the patient’s intake form, including a history of the present illness, in advance of the scheduled telehealth visit and use this information to generate a differential diagnosis. The clinician can then send the patient the video demonstrations and written instructions for both the core exam and any indicated abnormality-specific special tests. This strategy allows patients the opportunity to review and perhaps practice the physical exam maneuvers in advance of the visit. We have found, however, that this volume of information is often overwhelming to the patient and is ultimately not effective. This results in the patient’s presenting to a telehealth visit with the same familiarity as those in the “exam reveal” group.
Core exam preview: The patient is supplied with video demonstrations and written instructions for only the “core exam” of the affected joint to be reviewed in preparation for one’s scheduled telehealth visit. The clinician’s staff simply provides the patient with information for the relevant joint-specific core exam. From a clinical workflow and logistics perspective, we have found this to be the most time-efficient approach, as this strategy does not require a detailed chart review as with the “exam reveal” strategy. Additionally, patients are more likely to successfully complete the preview because they are only asked to review limited information and written instructions. This approach thereby improves patients’ familiarity with the format of the exam and improves visit efficiency for the patient, clinician, and ancillary office staff. Abnormality-specific special testing is conducted in real time during the telehealth visit, with explanations and clarifications provided by the clinician using available screen share options.
Regardless of the strategy selected by the clinician, the tools provided here offer a comprehensive and standardized approach to the virtual shoulder and knee exam, including office workflow, previsit setup, and physical exam testing. Improved standardization of these modified virtual exam tests will likely result in better reliability and validity of the virtual exam.
Limitations
There is no doubt that an in-person exam offers the most comprehensive opportunity for a musculoskeletal evaluation, including detailed passive range of motion, focused palpation, tactile recognition of crepitation, accurate strength assessment, and determination of ligamentous instability. We recognize that it is impossible to replace the ability of an experienced musculoskeletal clinician to perform certain physical exam maneuvers such as the Lachman and pivot-shift tests for ACL integrity or load and shift testing for glenohumeral instability. However, we also recognize that many aspects of the physical exam for sports medicine patients can be efficiently and accurately performed via an internet-based telehealth platform. In fact, in a randomized controlled trial of orthopaedic visits performed via telehealth compared with in-person consultations, physicians rated their ability to examine patients as good or very good in 98% of telehealth visits, with no significant differences between groups and no adverse safety events.11 By expanding our menu of exam maneuvers to include alternatives such as the lever test for the ACL,9,37 as well as minor modifications to classic maneuvers to be self-performed such as the Jobe test,26–28,31,39,46,66 we can still obtain useful data, albeit imperfect, via the virtual exam to allow for reasonable, remote clinical decision making.
While we provide recommendations regarding proper positioning of the patient and camera, we acknowledge that certain camera angles and patient positions may not allow the clinician to interpret certain tests with the same accuracy as an in-person exam. Additionally, tests that utilize a remote examiner may be performed by someone who is not trained in performing a musculoskeletal exam. While the layman’s instructions and video demonstrations provided for each test allow the remote examiner and patient to help the clinician identify certain abnormalities when present, it is possible that test findings may be incorrectly interpreted or reported by the examiner or patient despite uniform instructions. The sensitivity, specificity, and diagnostic accuracy of these tests when performed by a patient or untrained remote examiner and interpreted by a clinician have yet to be defined, but they are likely lower than published values for the same tests performed by an experienced examiner in person. As such, treatment plans should be formulated only when findings of the virtual physical exam corroborate the patient’s history and imaging studies. Conflicting findings should prompt a formal in-person evaluation before clinical decision making.34
We have found that a virtual assessment of knee ligamentous injuries, patellar instability, and glenohumeral instability generally provides a more limited amount of diagnostic information compared with in-person exams. When patients present with a history suggestive of these conditions, we still perform an initial virtual physical exam as outlined above but have a low threshold to obtain advanced imaging (typically in the form of magnetic resonance imaging) and a subsequent in-person visit. Similarly, glenohumeral instability testing including apprehension and sulcus tests also seems to be limited when compared with an in-person exam. Finally, some patients may be uncomfortable with telehealth consultations or postoperative follow-up visits. One study demonstrated a 12.1% dropout rate of patients randomized to telehealth visits after rotator cuff surgery, with similar rates in other previously published studies.11,41–43 While a virtual exam has many inherent limitations compared with an in-person exam performed by a trained clinician, we have attempted to utilize the best available resources to optimize the assessment of the shoulder and knee for telehealth purposes.
Current and Future Directions for Telehealth in Sports Medicine
Telehealth in orthopaedics has been shown to be effective for remote consultations, outpatient care, and rehabilitation.10,11,34,54,70 Telehealth has also been shown to improve access to care for patients with musculoskeletal complaints.65 While telehealth visits will not entirely replace in-person visits for sports medicine patients, they offer a wide array of advantages. These visits can offer alternative, cost-effective, and convenient access to musculoskeletal surgical and nonsurgical care. Additionally, these visits can screen and identify patients who need emergency room evaluations, surgical consultations, and advanced imaging. In particular, we envision telehealth visits replacing certain postoperative and follow-up visits, which might require a clinician-patient discussion, imaging review, and abbreviated virtual physical exam as detailed above. Multiple recent studies have suggested that the use of telehealth for postoperative follow-up after joint replacement surgery is safe and economically beneficial.42,43 Sharareh and Schwarzkopf56 reported that telehealth visits after total joint arthroplasty were actually associated with increased patient satisfaction compared with traditional outpatient visits, and this has been consistent with the recent experience of the senior author (S.A.T.) in the setting of a high-volume total shoulder arthroplasty practice. Kane et al34 performed a randomized controlled trial of patients after rotator cuff repair, showing that these patients were able to receive safe and effective follow-up care using telehealth when compared with traditional outpatient visits. Abel et al1 compared in-office visits with telehealth visits conducted within 24 hours of one another after arthroscopic orthopaedic surgery in adolescent patients, demonstrating that both types of visits had similar results when assessing range of motion, incision characteristics, and effusion size. Patients expressed a preference for telehealth appointments. A review of telehealth in upper extremity orthopaedic surgery demonstrated that postoperative wound complications can be easily recognized during telehealth encounters.23
With an increasing emphasis on value-based health care,51 the cost savings associated with telehealth visits will likely drive an increase in the number of telehealth patient encounters in the coming years. Multiple studies on telehealth visits in orthopaedics have demonstrated reduced costs and similar clinical outcomes when compared with traditional outpatient visits.20,58,59,61 In 1 study on the use of telehealth in pediatric sports medicine patients, Atanda et al3 reported significantly shorter visit and wait times for telehealth virtual visits for the purposes of follow-up, postoperative checkup, and imaging review. On average, families saved 85 miles of driving and $50 in visit costs, with a satisfaction rate of greater than 90% as well as 99% recommending telehealth to other patients. Those authors also reported significant savings for the hospital system. Harno et al24 reported that in-person outpatient orthopaedic visits cost 45% more than a teleconsultation when considering equipment costs, maintenance, and staffing. In a randomized controlled pilot study, Sathiyakumar et al55 found that no telehealth patients missed work for follow-up of nonsurgical orthopaedic trauma injuries, compared with 56% of patients who had traditional visits. Multiple other studies have corroborated these findings, suggesting that most telehealth systems reduce costs, including in orthopaedic care specifically.10,16,17,42 These socioeconomic savings are especially important given rising health care costs and the increasing emphasis on value-based care.34
The advent, use, and access of technologies and video-based online platforms have changed the landscape of telehealth visits. Over the past decade, leveraging new technologies to better understand and treat patients has become an increasing focus of health care.2 With increased patient access to video-based online platforms, we feel that using these technologies specifically in the area of musculoskeletal care has many advantages, including standardizing the patient encounter, helping to identify at-risk patients, and improving the reliability and accuracy of the virtual physical exam. Multiple studies have evaluated the interobserver and intraobserver reliability and validity of assessing different physical exam data points such as range of motion, acceleration, and velocity using wearable accelerometers, gyroscopes, camera-based motion software, and inertial sensor monitoring units.49 In the future, we envision the use of a combination of video-based online platforms, motion sensing technologies, and data analytic software to supplement the virtual physical exam.
The COVID-19 crisis and imposed social distancing mandates have forced orthopaedic surgeons to adopt new and unfamiliar ways to evaluate patients including telehealth visits. As we have become increasingly facile and comfortable with this video-based communication platform, many physicians have realized that we can effectively perform a virtual history, conduct a physical exam, and review imaging studies in a similar manner to in-office visits.44 We believe that telehealth visits will endure well beyond the resolution of the current COVID-19 crisis as a result of patient and clinician satisfaction and will be integrated into our collective “new normal.” In fact, our institution has encouraged clinicians to continue telehealth visits at least one-half day per week in perpetuity to accommodate patients with limited geographical availability and those requiring flexible scheduling times.14,36,52
Conclusion
Virtual telehealth platforms for care delivery are likely to endure, in part because of patient and clinician satisfaction, health care savings, geographical expansion, and improved time efficiency. The physical examination is long considered by clinicians to be a cornerstone in the evaluation of musculoskeletal patients, and this has resulted in the slow adoption of virtual telehealth visits. However, further consideration reveals that the majority of a traditional shoulder and knee examination can be accomplished virtually with little to no modification of tests and still enable clinical decision making. We have provided the first comprehensive description of a shoulder and knee physical exam for the purpose of telehealth virtual visits, including several abnormality-specific special tests. Specifically, we provided (1) verbal instructions in layman’s terms that can be provided to the patient before or read verbatim during the virtual visit, (2) video demonstrations of the general shoulder and knee exam as well as special tests accompanied by audio instructions that can be shown to patients via screen-share options, and (3) a corresponding checklist for documentation. These tools improve the patient’s understanding of what is being asked and, in return, will likely improve the reliability and accuracy of the virtual physical exam. Future studies will aim to validate the virtual physical exam components presented here.
Video supplements for this article are available at http://journals.sagepub.com/doi/suppl/10.1177/2325967120962869
Supplemental Material
Supplemental Material, DS_10.1177_2325967120962869 for The Virtual Shoulder and Knee Physical Examination by Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren Young, Scott A. Rodeo and Samuel A. Taylor in Orthopaedic Journal of Sports Medicine
SUPPLEMENTAL MATERIAL
The appendices for this article are available at http://journals.sagepub.com/doi/suppl/10.1177/2325967120962869
Footnotes
Final revision submitted August 17, 2020; accepted September 3, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.S.D. has received research support, consulting fees, and speaking fees from Arthrex and royalties from Linvatec, Thieme, and Wolters Kluwer Health–Lippincott Williams & Wilkins. S.A.R. has received consulting fees from Flexion Therapeutics and Teladoc and has stock/stock options in Ortho Regenerative Technologies. S.A.T. has received consulting fees from DJ Orthopedics and Mitek. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abel KC, Baldwin K, Chuo J, et al. Can telemedicine be used for adolescent postoperative knee arthroscopy follow-up? JBJS J Orthop Phys Assist. 2017;5(4):e26. [Google Scholar]
- 2. Anoushiravani AA, Patton J, Sayeed Z, El-Othmani MM, Saleh KJ. Big data, big research: implementing population health-based research models and integrating care to reduce cost and improve outcomes. Orthop Clin North Am. 2016;47(4):717–724. [DOI] [PubMed] [Google Scholar]
- 3. Atanda A, Pelton M, Fabricant PD, et al. Telemedicine utilisation in a paediatric sports medicine practice: decreased cost and wait times with increased satisfaction. J ISAKOS. 2018;3(2):94–97. [Google Scholar]
- 4. Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22(10):1076–1084. [DOI] [PubMed] [Google Scholar]
- 5. Ben Kibler W, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37(9):1840–1847. [DOI] [PubMed] [Google Scholar]
- 6. Bennett WF. Specificity of the Speed’s test: arthroscopic technique for evaluating the biceps tendon at the level of the bicipital groove. Arthroscopy. 1998;14(8):789–796. [DOI] [PubMed] [Google Scholar]
- 7. Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29–35. [DOI] [PubMed] [Google Scholar]
- 8. Brantigan CO, Roos DB. Diagnosing thoracic outlet syndrome. Hand Clin. 2004;20(1):27–36. [DOI] [PubMed] [Google Scholar]
- 9. Bronstein RD, Schaffer JC. Physical examination of the knee: meniscus, cartilage, and patellofemoral conditions. J Am Acad Orthop Surg. 2017;25(5):365–374. [DOI] [PubMed] [Google Scholar]
- 10. Buvik A, Bergmo TS, Bugge E, et al. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21(2):e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chronopoulos E, Kim TK, Park HB, Ashenbrenner D, McFarland EG. Diagnostic value of physical tests for isolated chronic acromioclavicular lesions. Am J Sports Med. 2004;32(3):655–661. [DOI] [PubMed] [Google Scholar]
- 13. Collin P, Treseder T, Denard PJ, et al. What is the best clinical test for assessment of the teres minor in massive rotator cuff tears? Clin Orthop Relat Res. 2015;473(9):2959–2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;2:CD002098. [DOI] [PubMed] [Google Scholar]
- 15. Daniel DM, Stone ML, Barnett P, Sachs R. Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70(3):386–391. [PubMed] [Google Scholar]
- 16. de la Torre-Diez I, Lopez-Coronado M, Vaca C, Aguado JS, de Castro C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: a systematic review. Telemed J E Health. 2015;21(2):81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Elbert NJ, van Os-Medendorp H, van Renselaar W, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16(4):e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Farber AJ, Castillo R, Clough M, Bahk M, McFarland EG. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am. 2006;88(7):1467–1474. [DOI] [PubMed] [Google Scholar]
- 19. Ferriero G, Vercelli S, Sartorio F, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(2):146–151. [DOI] [PubMed] [Google Scholar]
- 20. Fusco F, Turchetti G. Telerehabilitation after total knee replacement in Italy: cost-effectiveness and cost-utility analysis of a mixed telerehabilitation-standard rehabilitation programme compared with usual care. BMJ Open. 2016;6(5):e009964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gill HS, El Rassi G, Bahk MS, Castillo RC, McFarland EG. Physical examination for partial tears of the biceps tendon. Am J Sports Med. 2007;35(8):1334–1340. [DOI] [PubMed] [Google Scholar]
- 22. Goossens P, Keijsers E, van Geenen RJ, et al. Validity of the Thessaly test in evaluating meniscal tears compared with arthroscopy: a diagnostic accuracy study. J Orthop Sports Phys Ther. 2015;45(1):18–24, B11. [DOI] [PubMed] [Google Scholar]
- 23. Grandizio LC, Foster BK, Klena JC. Telemedicine in hand and upper-extremity surgery. J Hand Surg Am. 2020;45(3):239–242. [DOI] [PubMed] [Google Scholar]
- 24. Harno K, Arajarvi E, Paavola T, Carlson C, Viikinkoski P. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare. 2001;7(4):219–225. [DOI] [PubMed] [Google Scholar]
- 25. Harrison BK, Abell BE, Gibson TW. The Thessaly test for detection of meniscal tears: validation of a new physical examination technique for primary care medicine. Clin J Sport Med. 2009;19(1):9–12. [DOI] [PubMed] [Google Scholar]
- 26. Hegedus EJ, Goode A, Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42(2):80–92. [DOI] [PubMed] [Google Scholar]
- 27. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46(14):964–978. [DOI] [PubMed] [Google Scholar]
- 28. Hippensteel KJ, Brophy R, Smith MV, Wright RW. A comprehensive review of physical examination tests of the cervical spine, scapula, and rotator cuff. J Am Acad Orthop Surg. 2019;27(11):385–394. [DOI] [PubMed] [Google Scholar]
- 29. Hippensteel KJ, Brophy R, Smith MV, Wright RW. Comprehensive review of provocative and instability physical examination tests of the shoulder. J Am Acad Orthop Surg. 2019;27(11):395–404. [DOI] [PubMed] [Google Scholar]
- 30. Holtby R, Razmjou H. Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy. 2004;20(3):231–236. [DOI] [PubMed] [Google Scholar]
- 31. Hughes PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008;54(3):159–170. [DOI] [PubMed] [Google Scholar]
- 32. Jarbo KA, Hartigan DE, Scott KL, Patel KA, Chhabra A. Accuracy of the Lever sign test in the diagnosis of anterior cruciate ligament injuries. Orthop J Sports Med. 2017;5(10):2325967117729809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Juul-Kristensen B, Rogind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford). 2007;46(12):1835–1841. [DOI] [PubMed] [Google Scholar]
- 34. Kane LT, Thakar O, Jamgochian G, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29(4):775–783. [DOI] [PubMed] [Google Scholar]
- 35. Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20(6):364–372. [DOI] [PubMed] [Google Scholar]
- 36. Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lelli A, Di Turi RP, Spenciner DB, Domini M. The “lever sign”: a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2794–2797. [DOI] [PubMed] [Google Scholar]
- 38. Loeb AE, Rao SS, Ficke JR, et al. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000;9(4):299–301. [DOI] [PubMed] [Google Scholar]
- 40. Malanga GA, Andrus S, Nadler SF, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84(4):592–603. [DOI] [PubMed] [Google Scholar]
- 41. Marsh J, Bryant D, MacDonald SJ, et al. Are patients satisfied with a web-based followup after total joint arthroplasty? Clin Orthop Relat Res. 2014;472(6):1972–1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Marsh J, Hoch JS, Bryant D, et al. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014;96(22):1910–1916. [DOI] [PubMed] [Google Scholar]
- 43. Marsh JD, Bryant DM, MacDonald SJ, et al. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J Arthroplasty. 2014;29(9):1723–1728. [DOI] [PubMed] [Google Scholar]
- 44. Massey PA, McClary K, Zhang AS, Savoie FH, Barton RS. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID-19) pandemic. J Am Acad Orthop Surg. 2020;28(11):436–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Parker S, Prince A, Thomas L, et al. Electronic, mobile and telehealth tools for vulnerable patients with chronic disease: a systematic review and realist synthesis. BMJ Open. 2018;8(8):e019192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy. 1999;15(8):841–851. [DOI] [PubMed] [Google Scholar]
- 48. Rao SS, Loeb AE, Amin RM, et al. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020;6(3):617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rawashdeh SA, Rafeldt DA, Uhl TL. Wearable IMU for shoulder injury prevention in overhead sports. Sensors (Basel). 2016;16(11):1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rigamonti L, Albrecht UV, Lutter C, et al. Potentials of digitalization in sports medicine: a narrative review. Curr Sports Med Rep. 2020;19(4):157–163. [DOI] [PubMed] [Google Scholar]
- 51. Ring D, Bozic KJ. Value-based healthcare: the value of considering patient preferences and circumstances in orthopaedic surgery. Clin Orthop Relat Res. 2016;474(3):633–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rowell PD, Pincus P, White M, Smith AC. Telehealth in paediatric orthopaedic surgery in Queensland: a 10-year review. ANZ J Surg. 2014;84(12):955–959. [DOI] [PubMed] [Google Scholar]
- 53. Rubinstein RA, Jr, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22(4):550–557. [DOI] [PubMed] [Google Scholar]
- 54. Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(2):113–120. [DOI] [PubMed] [Google Scholar]
- 55. Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29(3):e139–e145. [DOI] [PubMed] [Google Scholar]
- 56. Sharareh B, Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29(5):918–922.e1. [DOI] [PubMed] [Google Scholar]
- 57. Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468(1):266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Shukla H, Nair SR, Thakker D. Role of telerehabilitation in patients following total knee arthroplasty: evidence from a systematic literature review and meta-analysis. J Telemed Telecare. 2017;23(2):339–346. [DOI] [PubMed] [Google Scholar]
- 59. Sinha N, Cornell M, Wheatley B, Munley N, Seeley M. Looking through a different lens: patient satisfaction with telemedicine in delivering pediatric fracture care. J Am Acad Orthop Surg Glob Res Rev. 2019;3(9):e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Somerville LE, Willits K, Johnson AM, et al. Clinical assessment of physical examination maneuvers for rotator cuff lesions. Am J Sports Med. 2014;42(8):1911–1919. [DOI] [PubMed] [Google Scholar]
- 61. Sultan AA, Acuna AJ, Samuel LT, et al. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. 2020;40(8):e712–e715. [DOI] [PubMed] [Google Scholar]
- 62. Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102(12):e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tate AR, McClure P, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Taylor SA, Newman AM, Dawson C, et al. The “3-pack” examination is critical for comprehensive evaluation of the biceps-labrum complex and the bicipital tunnel: a prospective study. Arthroscopy. 2017;33(1):28–38. [DOI] [PubMed] [Google Scholar]
- 65. Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9(5 suppl):S51–S58. [DOI] [PubMed] [Google Scholar]
- 66. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination, part I: the rotator cuff tests. Am J Sports Med. 2003;31(1):154–160. [DOI] [PubMed] [Google Scholar]
- 67. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination, part II: laxity, instability, and superior labral anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31(2):301–307. [DOI] [PubMed] [Google Scholar]
- 68. Tong HC, Haig AJ, Yamakawa K. The Spurling test and cervical radiculopathy. Spine (Phila Pa 1976). 2002;27(2):156–159. [DOI] [PubMed] [Google Scholar]
- 69. Viikari-Juntura E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine (Phila Pa 1976). 1989;14(3):253–257. [DOI] [PubMed] [Google Scholar]
- 70. Vuolio S, Winblad I, Ohinmaa A, Haukipuro K. Videoconferencing for orthopaedic outpatients: one-year follow-up. J Telemed Telecare. 2003;9(1):8–11. [DOI] [PubMed] [Google Scholar]
- 71. Vyas KS, Hambrick HR, Shakir A, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg. 2017;78(6):736–768. [DOI] [PubMed] [Google Scholar]
- 72. Vyas KS, Morrison SD, Vasconez HC, et al. Teledermatology: is it beneficial to patients? Ann Plast Surg. 2017;79(4):415–416. [DOI] [PubMed] [Google Scholar]
- 73. Walch G, Boulahia A, Calderone S, Robinson AH. The “dropping” and “hornblower’s” signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80(4):624–628. [DOI] [PubMed] [Google Scholar]
- 74. Walton J, Mahajan S, Paxinos A, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am. 2004;86(4):807–812. [DOI] [PubMed] [Google Scholar]
- 75. Werner BC, Holzgrefe RE, Griffin JW, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23(11):e275–e282. [DOI] [PubMed] [Google Scholar]
- 76. Wu WT, Chang KV, Han DS, Lin CP, Ozcakar L. Cross-talk between shoulder and neck pain: an imaging study of association between rotator cuff tendon tears and cervical foraminal stenosis. Medicine (Baltimore). 2018;97(36):e12247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yoon JP, Chung SW, Kim SH, Oh JH. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg. 2013;22(9):1186–1192. [DOI] [PubMed] [Google Scholar]
- 78. Zulkarnain RF, Kim GY, Adikrishna A, et al. Digital data acquisition of shoulder range of motion and arm motion smoothness using Kinect v2. J Shoulder Elbow Surg. 2017;26(5):895–901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, DS_10.1177_2325967120962869 for The Virtual Shoulder and Knee Physical Examination by Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren Young, Scott A. Rodeo and Samuel A. Taylor in Orthopaedic Journal of Sports Medicine