Abstract
Background:
It is difficult to predict who will experience prolonged health problems after sustaining a sport-related concussion.
Purpose:
To synthesize the literature and conduct a gap analysis on the association between preinjury mental health problems and clinical outcome from sport-related concussion.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Data sources were PubMed, PsycINFO, MEDLINE (and MEDLINE in Process), CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus, and Web of Science. Studies published before February 2019 that addressed preinjury mental health problems as a possible predictor of worse clinical outcome or clinical recovery from concussion were eligible for inclusion.
Results:
Of 4013 studies screened, 358 full texts were reviewed, and 12 studies involving 3761 participants (n = 471 [12.5%] with preexisting mental health problems) were ultimately included. The participants with a preinjury history of mental health problems were at greater risk for having persistent symptoms or worse outcome in 9 of 12 studies. The studies had major methodological differences, and most studies were not focused on mental health as a primary predictor or prognostic factor. Rather, they included it as a secondary or tertiary predictor. The sample sizes with preinjury mental health problems in most studies were small or very small (ie, <25). The age of onset, type, course, severity, and duration of mental health problems were not defined. The extent to which mental health problems were present before the season, during baseline testing, was not reported.
Conclusion:
Preinjury mental health problems appear to confer risk for worse clinical outcome after sport-related concussion. Future research is needed to (1) examine this risk factor in large representative populations of middle school students, high school students, and collegiate athletes; (2) quantify the risk for each mental health condition; (3) understand the mechanisms underlying this increased risk; and (4) develop more refined treatment and rehabilitation approaches for these student-athletes.
Keywords: concussion, depression, anxiety, mental health, outcome, moderators, age, sports
Preinjury mental health problems, such as depression and anxiety, appear to confer risk for worse clinical outcome in student-athletes after sport-related concussion.17 Moreover, postinjury mental health problems complicate and prolong recovery.25,30 A previously published systematic review prepared for the Berlin Concussion in Sport Consensus Conference26 examined a diverse set of 21 predictors and prognostic factors of clinical recovery after concussion.17 The authors identified 8 studies published before June 2016 that examined preinjury mental health as one of those predictors.2,9,11,13,31,42,45,46 Of these 8 studies, all examined a personal history of mental health problems, and 2 studies examined a family history of mental health problems.13,31 All but 1 of the studies reported that preinjury mental health problems were associated with worse clinical outcome.42 The methodological strengths and weaknesses of those studies were not carefully examined. Moreover, the mechanisms of vulnerability associated with preinjury mental health problems are not well-understood and are likely multifactorial as well as biopsychosocial. The purpose of this study was to conduct a systematic review and knowledge gap analysis of the association between preinjury mental health problems and outcome from sport-related concussion. Through this review we will (1) carefully examine the nature of the findings, magnitude of the findings, and methodological quality of the literature; (2) include studies published since the summer of 2016; (3) identify gaps in the literature; and (4) make recommendations for future research.
Methods
An original systematic review protocol was prospectively registered in the PROSPERO database for systematic reviews (protocol ID: CRD42016041479), and an updated systematic review was also registered (protocol ID: CRD42019128274). This systematic review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.29 We defined outcome as “clinical recovery and return to activities and sports.” Clinical recovery could be defined in many different ways by each individual study, such as by considering improvement in neuropsychological functioning or self-reported resolution of symptoms and/or whether participants had been medically cleared to return to play and/or participate in normal activities.
Search Strategy
We identified articles by searching online databases, hand-searching reference lists, and performing cited reference searches (Figure 1). We conducted 2 partially overlapping literature searches using PubMed, MEDLINE, PsycINFO, CINAHL, Cochrane Library, EMBASE, SPORTDiscus, Scopus, and Web of Science. We included articles published in English from database inception to June 2016 in our first search for a systematic review17 prepared for the Concussion in Sport Group conference in Berlin in 201626 and then from January 1, 2016, to February 1, 2019, in our second search. The search terms were exactly the same for the 2 different time points. Two general categories relating to (1) sport- and athlete-related terms and (2) brain concussion–related terms were used as the key search terms, as follows: sport, sports (MeSH), athletic, athlete, player AND craniocerebral trauma, brain injuries, brain concussion, sports concussion, athletic injuries, mild traumatic brain injury, mTBI, traumatic brain injury, TBI, brain concussion, concussion, multiple concussions, repeated concussion, repetitive concussion, cumulative concussions, concussion history, brain damage, prognosis, outcome, recovery, risk factor, injury incidence, sex differences, gender, genetics, ApoE, BDNF, S100B, GFAP, severity, loss of consciousness, LOC, post-traumatic amnesia, PTA, amnesia, retrograde amnesia, seizure, seizures, learning disorder, ADHD, level of education, migraine, mental health, sleep disorders, medications, cervical injury, vestibular injury, psychological reactions, anxiety, depression, headaches, intractable headaches, magnetic resonance imaging, MRI, computer tomography, and CT. This extraordinarily broad set of search terms was used to replicate the terms used in the previous systematic review because many articles examined multiple predictors. A more focused search could miss articles that do not examine mental health specifically but nevertheless include mental health as one of many predictors.
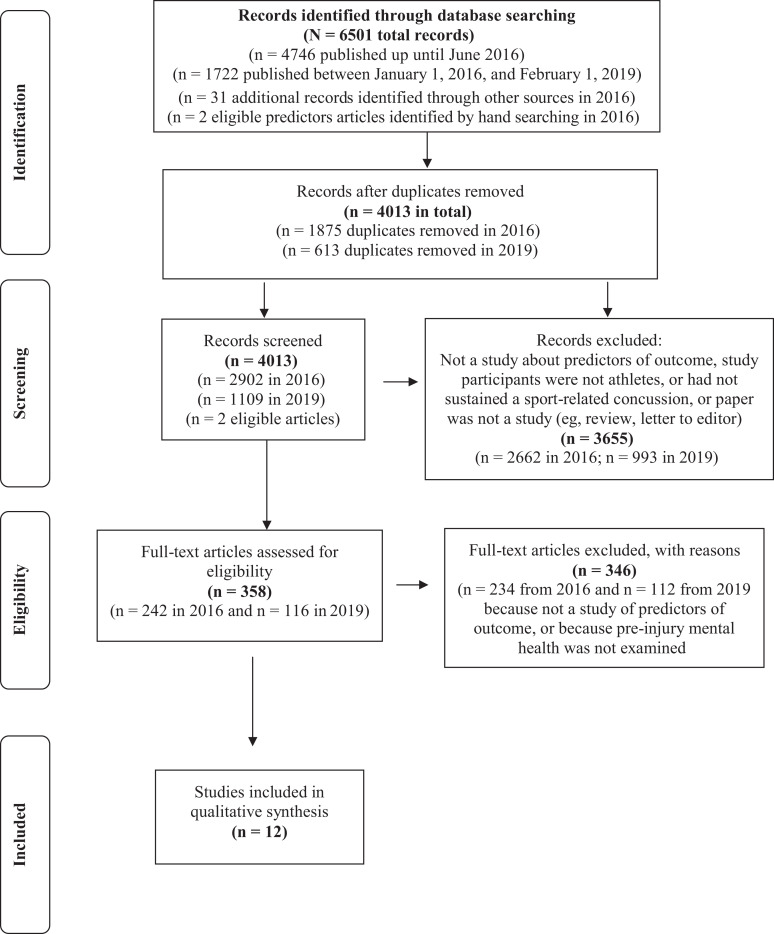
Figure 1.
Systematic literature search utilizing the PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines.
Article Selection and Data Extraction
The search sequence and results are presented in Figure 1. When replicating the search and reviewing documentation, we discovered a mistake in the reporting of the number of records identified in the original search from 2016. The initial search in 2016 yielded 4746 records, as noted in Figure 1, not 7617 records noted in the original article PRISMA figure.17 For the original search, 2 reviewers conducted the initial screening of the titles and abstracts of articles identified (G.L.I. and A.J.G.). For the updated search, the titles and abstracts of the 1109 articles identified (January 1, 2016, to February 1, 2019) were screened by 1 author (G.L.I.). Studies conducted with humans that examined outcome from sport-related concussion >1 week after injury were included. Studies that addressed acute outcome in the initial days after injury but did not address clinical recovery time or risk for persistent symptoms were excluded. When there was uncertainty about whether a study should be included based on the review of the title and abstract, the full article was retrieved and reviewed by 1 of 2 authors during the first search (G.L.I. or A.J.G.) and the second search (A.J.G. or D.P.T.). To supplement the electronic database search, we examined the reference lists from previously published reviews and systematic reviews.
Three authors (M.W.W., A.J.G., and D.P.T.) completed the extraction of information from the 12 articles: that is, first author, year of publication, the PubMed identification number, number of participants, proportion of male participants, age, setting, study design, number with preinjury mental health problem, outcome measures, whether mental health was a primary focus of the study, source of information regarding the mental health problem, medication information (type, dose, duration), the period for assessing the clinical outcome, study findings, and effect sizes. Two reviewers (M.W.W., D.P.T) independently extracted data from each article. A third reviewer (A.J.G.) was sometimes needed to resolve discrepancies. Risk of bias for each article was rated by 2 authors (M.W.W. and D.P.T.) using the Newcastle-Ottawa scale, and differences were resolved by discussion. The Newcastle-Ottawa scale is a risk of bias assessment system used for observational studies, including case-control and cohort studies.44 When rating the Newcastle-Ottawa scale, we considered prior mental health problems as the “exposure” and prolonged concussion recovery as the “outcome.” The level of evidence for each article was rated independently by 2 authors (M.W.W. and D.P.T.) using the Oxford Centre for Evidence-Based Medicine,32 and differences were resolved by discussion.
Applying a Likelihood Ratio Heuristic
We calculated a likelihood heuristic to determine the likelihood of observing a specific number of significant and nonsignificant studies if preinjury mental health problems are an independent vulnerability factor of prolonged recovery after concussion compared with if they are not (see the Appendix for explanation). This likelihood heuristic, developed and published by Lakens and Etz,19 can be applied to a body of systematically reviewed evidence when study results are conflicting and are not amenable to meta-analysis (eg, due to a wide range of reported outcome metrics). Büttner and colleagues6 applied this likelihood heuristic to systematic review data on predictors of prolonged recovery after concussion, illustrating that even when studies were closely conflicting, there was substantial evidence for specific predictors of prolonged recovery. Lakens and Etz provided a detailed explanation of this method and developed an openly available online calculator (https://lakens.shinyapps.io/likelihood/) to perform this analysis. Likelihood ratios of 8 and 32 are proposed as thresholds for moderate and strong evidence, respectively.38
Results
The search revealed 6501 articles (Figure 1). After duplicates were removed, 4013 were screened further by title and abstract for eligibility. Of the 4013 articles, 3655 were excluded on the basis that they did not examine athletes who had sustained a sports concussion, or the citation was not an original study (ie, the citation was a review article, editorial, letter to the editor, or commentary). The PDFs of 358 articles were retrieved and reviewed. We included 12 studies that examined preinjury mental health problems as a predictor of clinical outcome. Information from the studies is summarized in Tables 1 through 3. These studies included 3761 participants, of whom 471 (12.5% of the total sample) had preexisting mental health problems. There were major methodological differences across the studies (see Tables 1 and 2). Research designs were diverse, including retrospective (8/12 studies; 67%), prospective (4/12 studies; 33%), case-control (4/12 studies; 33%), and cohort studies (8/12 studies; 67%). Most of the studies measured outcome based on symptoms (10/12 studies; 83%), but how they conceptualized symptom outcome varied. There was considerable variability in when outcomes were measured, such as within an archival study period (4/12 studies; 33%), length of recovery (3/12 studies; 25%), and defined follow-up period (5/12 studies; 42%). Studies were conducted in multiple different settings, including populations from colleges (3/12 studies; 25%), emergency departments (2/12 studies; 17%), and specialty clinics (7/12 studies; 58%).
TABLE 1.
Cohort Study Characteristics and Findingsa
| Study Characteristics | Findings, Effect Size, Time Period |
|---|---|
| Corwin (2014)9
Total N = 247; 247 concussed; 58% male. Age: mean, 14 (SD, NR); range, 7-18. Total with preinjury mental health problem, n = 24 (10%). Depression, n = 15 (6%). Anxiety, n = 9 (4%). Male/female, NR. Setting: tertiary specialty clinic (often sees slow-to-recover youth). Design: retrospective cohort (77% with sport-related concussions). Outcome: return to school/sports and symptom-free. |
Findings: Took depression history group 2.22 times longer to be symptom free-(Median, 142 vs 64 days) and 1.61 times longer time until fully cleared. Anxiety history yields 2.21 risk of longer time until fully cleared (Median, 121 vs 74 days). No differences in return to school. Time period: symptom-free median, 64 days (IQR, 18-119). Fully cleared for all activities median, 76 days (IQR, 30-153). |
| Eisenberg (2013)11
Total N = 235; 235 concussed; 57% male. Age: mean, 14.3 (SD, NR); range, 11-22. Total with preinjury mental health problems, n = 36 (15.3%). Depression, n = 15 (6.4%). Anxiety, n = 21 (8.9%). Male/female, NR. Setting: emergency department. Design: prospective cohort (64% with sport-related concussions). Outcome: time to symptom resolution |
Findings: Depression history yields longer time until symptom-free. Depression did not predict prolonged recovery in multivariate regression model, but hazard ratio was 1.98. About 48% of the depressed sample was symptomatic at 90 days, compared with 15% of the whole sample. Anxiety was not significant. Time period: 90 days. |
| Ellis (2015)13
Total N = 174; 174 concussed; 62% male. Age: mean, 14.2 (SD, 2.34); range, NR. Total with preinjury mental health problems, n = 23 (13.2%). ADHD, n = 14 (8.0%). Depression, n = 4 (2.3%). Anxiety, n = 5 (2.9%). Tourette syndrome, n = 1 (0.6%). Male/female, NR. Setting: pediatric concussion program. Design: retrospective cohort. Outcome: presence of psychiatric sequelae (ie, worsening of symptoms of a preexisting psychiatric disorder, new suicidal ideation, or presence of a new psychiatric disorder) vs no psychiatric disorder. |
Findings: More people with a history of a psychiatric disorder had a psychiatric outcome after a concussion than those without a preinjury psychiatric disorder (45%-50% vs 7%). Time period: follow-up at 1- to 4-week intervals depending on the severity of their symptoms, trajectory of recovery, and availability. |
| Ellis (2017)12
Total N = 306; 306 concussed; 60% male. Age: mean, 14.3 (SD, 2.3); range, NR. Total with preinjury mental health problem, NR. Setting: pediatric concussion program. Design: retrospective cohort. Outcome: VOD (>1 subjective complaint and >1 objective finding) and development of PCS at 1 month. |
Findings: Preinjury history of depression was a significant predictor of VOD in univariate (RR, 2.45; 95% CI, 1.49-4.05) and multivariate (RR, 1.53; 95% CI, 1.03-2.29) analyses. Preinjury history of depression was a significant predictor of PCS development in univariate (RR, 2.19; 95% CI, 1.57-3.07) and multivariate (RR, 1.50; 95% CI, 1.09-2.05) analyses. Time period: median time until medical clearance in study period for those with PCS was 123 days (IQR, 88-238 days). |
| Fehr (2019)15
Total N = 431; 431 concussed; 55% male. Age: mean, 14.3 (SD, 2.1); range, 10-18. Total with preinjury mental health problems, n = 41 (9.5%). Anxiety, n = 13 (3.0%). Depression, n = 12 (2.8%). Bipolar, n = 5 (1.2%). Other, n = 7 (1.6%). Male/female, NR. Setting: outpatient pediatric sports medicine specialty clinic. Design: retrospective cohort study. Outcome: symptom duration. |
Findings: All mental health findings were nonsignificant (P = .013, but significance was set to P < .01). Bipolar excluded due to limited prevalence. Any psychiatric disorder: HR, 0.61; 95% CI, 0.36-1.02. Anxiety: HR, 0.58; 95% CI, 0.23-1.46. Depression: HR, 0.54; 95% CI, 0.20-1.45. Other: HR, 1.07; 95% CI, 0.40-2.86. Time period: 90 days. |
| Lawrence (2018)20
Total N = 253; 253 concussed; 59% male. Age: median, 17 (IQR, 15.0-20.0); range, NR. Total with preinjury mental health problems, n = 39 (15.4%). Male/female, NR. Setting: academic sports medicine clinic. Design: retrospective cohort study. Outcome: time until full return to sport and school/work. |
Findings: Preinjury psychiatric history was not related to either return to sport or return to school/work. Time period: median, 28 days (IQR, 17.0-43.0). |
| Yang (2015)45
Total N = 71; 71 concussed; 75% male. Age: NR. Total with preinjury mental health problems, n = 58. Anxiety, n = 40. Depression, n = 18. (Number with comorbid anxiety and depression not reported; thus, the total number with preinjury mental health problems might be smaller.) Setting: university. Design: prospective cohort. Outcome: depression and anxiety at 1 week after injury. |
Findings: 18/71 (25%) participants were classified as having depression and 40/71 (56%) were classified as having anxiety at baseline. Baseline depression increased the likelihood of depression symptoms (OR, 4.59; 95% CI, 1.25-16.89) and anxiety symptoms (OR, 3.40; 95% CI, 1.11-10.49) postinjury. Baseline anxiety did not significantly change likelihood of postinjury anxiety (OR, 1.55; 95% CI, 0.56-4.31) or depression (OR, 2.92; 95% CI, 0.73-11.70). Time period: 1-week postinjury. |
| Zemek (2016)46
Total N = 2006; 2006 concussed (1701 with complete data); 61% male. Age: median, 12 (IQR, 9.2-14.6); range, 5-18. Total with preinjury mental health problems with complete data, n = 213. Anxiety, n = 131. Depression, n = 36. Sleep disorder, n = 35. Other, n = 11. Male/female, NR. Setting: multiple pediatric emergency departments. Design: Multicenter cohort. Outcome: PCS at 1 month. |
Findings: Premorbid anxiety history increased risk of PCS (OR, 1.4; 95% CI, 1.0-2.1). The rate of persistent symptoms was 29.3% in those without preinjury anxiety compared with 37.4% of those with preinjury anxiety. Premorbid depression history increased risk of PPCS at 28 days (OR, 2.7; 95% CI, 1.4-5.2). The rate of persistent symptoms was 29.5% in those without preinjury depression compared with 52.8% of those with preinjury depression. Time period: 28 days. |
aADHD, attention-deficit/hyperactivity disorder; HR, hazard ratio; IQR, interquartile range; NR, not reported; OR, odds ratio; PCS, postconcussion syndrome/postconcussion symptoms; PPCS, persistent postconcussion symptoms; RR, relative risk; VOD, vestibulo-ocular dysfunction.
TABLE 2.
Case-Control Study Characteristics and Findingsa
| Study Characteristics | Findings, Effect Size, Time Period |
|---|---|
| Asken (2016)2
Total N = 97; 97 concussed; 77% male. Age: mean, 20.4 (SD, 1.3); range, NR. Total with preinjury mental health problems, n = 8/92 (9%), 5 cases missing. Male/female, n = 2/6. Setting: university. Design: retrospective chart review, cross-sectional case-control. Outcome: days missed from play; normal vs prolonged recovery (>7 days) |
Findings: Those with premorbid psychiatric diagnosis were 2.1 times more likely to have a prolonged recovery than those without it. Effect size reported: ϕ = 0.267. Time period: median, 7 days; range, 3-67 days. |
| Morgan (2015)31
Total N = 120; 120 concussed; 49% male. Age: PCS, mean, 14.9 (SD, 2.1); non-PCS, mean, 14.8 (SD, 2.0); range, 9-18. Total with preinjury mental health problems, n = 13 (10.8%). Mood, n = 8 (6.7%). Psychiatric, n = 5 (4.2%). Male/female, n = NR. Setting: database, high school. Design: retrospective case-control study. Outcome: Development of PCS vs those who had a concussion but recovered within 3 weeks. |
Findings: Athletes with premorbid mood or psychiatric illness were more likely to develop PCS. Mood disorder was a predictor of PCS in logistic regression model. A history of mood disorder yielded an increased risk of developing PCS in multivariate logistic regression model (RR, 17.9; 95% CI, 2.9-113.0). Time period: 3 months. |
| Terwilliger (2016)42
Total N = 42; 42 concussed; 52% male. Age: mean, 14.9 (SD, 0.87); range, 13-16. Total with preinjury mental health problems, n = 4 (9.5%). Anxiety, n = 3 (7.1%). Depression, n = 1 (2.4%). Male/female, NR. Setting: clinic. Design: case-control study. Outcome: symptoms at first clinic visit (mean, 22 days; SD, 16; median, 18); LOR. |
Findings: No significant differences in outcome for those with premorbid mental health. Depression was not related to symptom burden or length of recovery. Anxiety was not related to LOR. Time period: additional-impact LOR (mean, 52.3 days; SD, 26.1; median, 43), Single-impact group LOR (mean, 36.9 days; SD, 19.1; median, 35). |
| Vargas (2015)43
Total N = 126; 84 concussed; 69% male. Age, concussed group: mean, 18.4 (SD, 0.8). Age, control group: mean, 18.9 (SD, 0.9); range, NR. Total with preinjury mental health problems, n = 12/126 (10%). Male/female, NR. Concussed, n = 9/84 (11%). Control, n = 3/42 (7%). Setting: university. Design: case-control study. Outcome: postinjury depression. |
Findings: Using dichotomized depression score, investigators found that more athletes had a meaningful level of depression after a concussion (23%) compared with baseline (11%). Control group showed marginal increase at time 2 (10%) from baseline (7%). Baseline depression symptoms were predictive of postinjury depression symptoms (r = .37; P < .0001). Baseline depression symptoms accounted for 11% of the variance (R 2 = 0.11; P = .03) even when considering history of psychiatric treatment, postconcussion symptoms, and age at first organized sport participation. Time period: concussed group: mean, 6.6 days postinjury (SD, 8.8); up to 41 days. Control group: up to 8.4 weeks post baseline. Mean, 0.14 y (SD, 0.0 y), range, 0.12-0.16 y. |
aLOR, length of recovery; NR, not reported; PCS, postconcussion syndrome/postconcussion symptoms; RR, relative risk.
Level of Evidence and Risk for Bias Assessment
Level of evidence ratings and results of the Newcastle-Ottawa scale are summarized in Table 4. There were 8 cohort studies and 4 case-control studies. The average level of evidence for the 12 studies was 3.5. Of the 12 studies, 6 studies were rated as 3 (ie, cohort studies) and 6 studies were rated as 4 (ie, case-control studies or lower quality prognostic cohort studies). On the Newcastle-Ottawa scale, studies received credit for between 3 and 8 items (mean ± SD, 5.75 ± 1.82). Most studies received credit for drawing the nonexposed cohort (ie, patients without prior mental health problems) from the same community as the exposed cohort (ie, those with prior mental health problems). Few studies received credit for comparability due to lack of statistical or design procedures to control for additional important factors potentially related to outcome from concussion, such as sex, age, or prior concussions. Most studies determined exposure (ie, prior mental health status) based on self-report or provided no description of how prior mental health status was determined. Further, outcome (ie, concussion recovery) was most commonly assessed via self-reported symptoms.
TABLE 4.
Newcastle-Ottawa Quality Assessment Scale Scores and the Level of Evidence of the Included Studies (Listed Alphabetically)a
| Newcastle-Ottawa Scale | ||||||
|---|---|---|---|---|---|---|
| First Author (Year) | Designb | Selection (0-4) | Comparability (0-2) | Outcome/Exposure (0-3) | Total Credits | Level of Evidence (1-5) |
| Asken (2016)2 | Case-control | --** | ** | -** | 6 | 4 |
| Corwin (2014)9 | Cohort | **-* | -- | *** | 6 | 4 |
| Eisenberg (2013)11 | Cohort | **-* | ** | -** | 7 | 3 |
| Ellis (2015)13 | Cohort | -*-* | -- | *-* | 4 | 3 |
| Ellis (2017)12 | Cohort | **-* | ** | *** | 8 | 3 |
| Fehr (2019)15 | Cohort | **-* | -- | **- | 5 | 4 |
| Lawrence (2018)20 | Cohort | **-* | ** | *** | 8 | 3 |
| Morgan (2015)31 | Case-control | -*** | ** | *** | 8 | 4 |
| Terwilliger (2016)42 | Case-control | --** | *- | *** | 6 | 4 |
| Vargas (2015)43 | Case-control | ---* | -- | -** | 3 | 4 |
| Yang (2015)45 | Cohort | **-- | -- | *** | 5 | 3 |
| Zemek (2016)46 | Cohort | -*-* | -- | -*- | 3 | 3 |
aAn asterisk (*) indicates that specific item on the Newcastle–Ottawa Scale was fulfilled. A hyphen (-) indicates that specific item on the Newcastle-Ottawa Scale was not met.
bWe determined the study design in reference to the determination of whether prior mental health problems are a predictor of worse clinical recovery from concussion. Exposure ratings are for case-control studies, and outcome ratings are for cohort studies. In certain circumstances, the original study design (which might have examined many predictors of recovery) might have earned credit on one of the Newcastle-Ottawa Scale parameters, but when we examined the study in relation to its ability to determine whether prior mental health is associated with worse concussion outcome, the study might not have earned credit on that parameter.
Preinjury Mental Health Problems and Clinical Outcome
The vast majority of available studies found significantly worse clinical outcomes after concussion for patients with premorbid mental health problems relative to those without premorbid mental health problems. A prospective cohort study examining the length of recovery (time until symptom resolution) after concussion provided evidence that preinjury depression resulted in longer time until symptom-free in univariate, Kaplan-Meier survival analysis (P = .01).11 It was noted that 87%, 57%, and 48% of those with preinjury depression remained symptomatic at 7, 28, and 90 days postinjury, respectively, compared with 77%, 32%, and 15% of the entire sample who were symptomatic at the same time points. However, depression history was not significant in multivariate model (P = .09). The nonsignificant hazard ratio (1.978) was likely related to small sample size with premorbid depression (n = 15). The largest study (sample size of 2006; 1701 with complete data) included in this review found that premorbid depression increased the odds of developing persistent symptoms at 28 days after concussion (odds ratio, 2.7; 95% CI, 1.4-5.2; P = .002), with 52.5% of those with preinjury depression having persistent symptoms at 28 days postinjury compared with 29.5% of those without preinjury depression.46 Premorbid anxiety was also associated with persistent postinjury depression (odds ratio, 1.4; 95% CI, 1.0-2.1; P = .05).46 Family history of psychiatric illness was included in only 2 of the studies. First, in a retrospective study using data from a specialty concussion clinic, family psychiatric illness was associated with worse psychiatric outcomes after sports-related concussion.13 Second, in a retrospective chart review study from a university-based sport concussion clinic with high school athletes, family history of mood disorders was a significant predictor of postconcussion syndrome in a multivariate logistic regression model (odds ratio, 3.1; 95% CI, 1.1-8.5; P = .026).31
Among the 12 studies included in this review, only 3 studies did not report a statistically significant association between preinjury mental health problems and worse clinical outcome.15,20,42 Of those 3 studies, 2 did not clearly indicate how they determined premorbid mental health problems,15,20 and mental health was not a primary predictor of interest in any of them. One of these studies was a retrospective study using data from a specialty concussion clinic to evaluate risk factors for prolonged symptoms.15 The univariate Cox proportional hazard regression for any psychiatric disorder (hazard ratio, 0.61; 99% CI, 0.36-1.02; P = .013) predicting prolonged (lower hazards of) recovery was nonsignificant due to adjusted alpha being set at .01 amid the large number of other predictors considered in this study.15 As such, psychiatric history was not included in their multivariate model.
Sample Size
The median and mean numbers of participants with preinjury mental health problems included in these studies were 24 and 46.3 (SD, 69.9), respectively. Approximately one-third of the studies (36.4%) had <15 participants, and 55% of the studies had <25 participants with preinjury mental health problems. Across the studies, the participants with preinjury mental health problems represented a median of 10.8% of the total study sample (mean ± SD, 17.8% ± 21.3%; range, 8.2%-81.7%). One study did not report the cell size for this subgroup. This appears to be lower than the prevalence rates from the National Comorbidity Study–Adolescent Supplement, which found that 31.9% of adolescents ages 13 to 18 had a lifetime history of an anxiety disorder and 14.3% had a mood disorder.28
Likelihood Ratios
As shown in Table 5, observing 9 significant and 3 nonsignificant studies is 621 million (ie, 6.21+E08) times more likely if mental health history is a vulnerability factor for prolonged recovery after concussion than if it is not. All analyses of subgroups of studies, assuming 80% power and alpha at 5%, also yielded high to very high likelihood ratios. Repeating the overall likelihood analysis using parameters of much lower statistical power (eg, 45%) and higher alpha level (eg, 25%) across studies generates a revised likelihood ratio that is substantially less in magnitude, but still high (ie, 78.23). This modified likelihood ratio presented in Table 5 might be more representative of the statistical properties of several of the studies included in this review, and thus it would be reasonable to assume that the true likelihood ratios fall somewhere between the 80% power/5% alpha and 45% power/25% alpha values presented in Table 5.
TABLE 5.
Likelihood Ratio Estimates Summarizing Studies Relating to Preinjury Mental Health Problemsa
| Likelihood Ratio | ||||
|---|---|---|---|---|
| Total No. of Studies | No. of “Positive” Studies (P < .05) | 80% Power, 5% Alpha | 45% Power, 25% Alpha | |
| All studies | 12 | 9 | 6.21+E08 | 78.23 |
| Studies with n > 25 participants who had preinjury mental health problems | 5 | 3 | 181.54 | 3.14 |
| Studies that examined duration of postinjury symptoms | 6 | 4 | 2904.64 | 5.65 |
| Studies that examined duration of postinjury symptoms and had n > 25 | 3 | 2 | 53.89 | — |
aLikelihood ratio (LR) estimates are calculated assuming a statistical power of 80% (0.80), an intended alpha level of 5% (.05), and a prior probability of 50% (0.50) that the alternative hypothesis is true before the data are collected (eg, a 50% probability that prior concussion history is associated with worse clinical outcome after sport-related concussion). Alternative LRs are calculated with lower presumed power and inflated alpha levels. When a likelihood ratio >1 is observed for a prognostic factor, this indicates that the data are more likely assuming the alternative hypothesis is true than assuming the null hypothesis is true. The LR for studies with more participants (ie, n > 25) was not calculated under the assumption of low power and inflated alpha because the assumption of low power is less likely to be true for those studies.
Minimal Clinical Information Relating to Preinjury Mental Health Problems
Nearly all the available studies lack important information relevant to understanding preinjury mental health and worse outcome from concussion (Table 3). Regarding the determination and characterization of preinjury mental health status, most commonly, this was based solely on self-report of a prior diagnosis (6/12 studies), or the authors did not specify how preinjury mental health status was determined (2/12 studies). One study described coding prior mental health status based on the participant’s medical chart, from which findings could have been based upon self-report information indicated on a standard health history form. There were 3 studies that allowed parents to provide historical information along with patients, although no study exclusively required that parents uniformly provide historical data. Thus, it remains unclear how much input parents had in determining psychiatric history among these studies. None of the studies confirmed whether participants were identified as having prior mental health problems using structured diagnostic interviews. Information relating to specific diagnoses, age of onset, illness duration, current severity, course (single episode, recurrent, or chronic), family history of mental health problems, or medications (type, dose, or duration) was typically not available in the studies (see Table 3).
TABLE 3.
Information Relating to Preinjury Mental Health Problemsa
| First Author (Year) | Focus? Abstract? Significant?b |
Source | Type | N | Duration | Age of Onset | Episode/Chronicity | Family History | Medications |
|---|---|---|---|---|---|---|---|---|---|
| Asken (2016)2 | No, yes, yes | Self-report | Psychiatric condition | 8 | NR | NR | NR | NR | NR |
| Corwin (2014)9 | Yes, yes, yes | Self-/parent-report | Depression/anxiety | 24 | NR | NR | NR | NR | NR |
| Eisenberg (2013)11 | No, no, yes | Self-/parent-report | Depression/anxiety | 36 | NR | NR | NR | NR | NR |
| Ellis (2015)13 | Yes, yes, yes | Self-report | Psychiatric history and family psychiatric history | 23 | NR | NR | NR | n = 28 (16.1%) | Yesc |
| Ellis (2017)12 | No, yes, yes | Self-report | Depression history | NR | NR | NR | NR | NR | NR |
| Fehr (2019)15 | No, no, no | NR | Anxiety, depression, bipolar, other | 41 | NR | NR | NR | NR | NR |
| Lawrence (2018)20 | No, no, no | NR | NR | 39 | NR | NR | NR | NR | NR |
| Morgan (2015)31 | Yes, yes, yes | Medical records | Psychiatric illness, family history of mood disorder, family history of psychiatric disorder | 13 | NR | NR | NR | Mood disorder, n =11 (9.2%); psychiatric disorder, n =13 (10.8%) | NR |
| Terwilliger (2016)42 | No, no, no | Acute Concussion Evaluation interview, self-report | Depression/anxiety | 4 | NR | NR | NR | NR | NR |
| Vargas (2015)43 | Yes, yes, yes | Self-report | Depression | 12 | NR | NR | NR | NR | NR |
| Yang (2015)45 | Yes, yes, yes | Self-report | Baseline depression and anxiety symptom reporting | 58 | NR | NR | NR | NR | NR |
| Zemek (2016)46 | No, no, yes | Acute Concussion Evaluation interview, by self-/parent-report | Anxiety, depression, and other psychiatric disorder diagnosis | 213 | NR | NR | NR | NR | NR |
aNR, not reported.
bWere preinjury mental health problems a central part, or focus, of the study? Were the results relating to preinjury mental health reported in the abstract? Did the study find a statistically significant association between preinjury mental health problems and worse outcome following concussion?
cAntidepressant, sleep, stimulant, mood stabilizer, antianxiety, and atypical antipsychotic medications.
Discussion
This systematic review identified 12 studies that examined the association between preinjury mental health problems and worse clinical outcome from sport-related concussion. Statistically significant prolonged recovery or worse clinical outcome was reported in 9 of the 12 studies. Clinical outcome was defined in several different ways, such as the duration of concussion symptoms (6/12 studies); time to return to activity, play, school, or work (4/12 studies); and the presence of the postconcussion syndrome (2/12 studies), psychiatric problems (2/12 studies), and vestibulo-ocular dysfunction (1/12 studies) at a certain time point after injury. Some studies had multiple clinical outcomes. The average level of evidence for the 12 studies was 3.5. A number of methodological limitations were identified. The sample sizes of patients with preinjury mental health problems in most studies were small or very small. Only 5 studies had a sample size >25 people with prior mental health problems, and 2 of those studies did not find a significant association between preinjury mental health and outcome. Further, 7 of the articles were not focused on mental health as a primary predictor; they included it as a secondary or tertiary predictor. The age of onset, type, course, severity, and duration of mental health problems typically were not defined. The extent to which the mental health problems were present before the season, during baseline testing, generally was not reported. The effect sizes for the association between mental health history and outcome often were not reported. Nonetheless, this systematic review provides reasonably strong and consistent evidence that preinjury mental health problems confer risk for worse clinical outcome after sport-related concussion.
There were some clinically important findings from 3 specific studies. First, Zemek and colleagues46 examined a cohort of 2006 children and adolescents from emergency departments across Canada (1701 patients with complete data). Of those, 131 reported a preinjury history of anxiety and 36 reported a preinjury history of depression. At 4 weeks postinjury, approximately 53% of youth with preinjury depression reported persistent symptoms and 37% of youth with preinjury anxiety reported persistent symptoms, compared with 29% of youth who did not have either of these conditions. This study illustrates a relatively high prevalence of persistent symptoms in youth presenting to the emergency department after injury and a particularly high prevalence in those with preinjury depression. Second, Eisenberg and colleagues11 reported outcomes from youth seen in a specialty clinic (N = 235); in that sample, only 15 patients had preinjury depression and 21 had preinjury anxiety. At 4 weeks postinjury, 32% of the total sample had persistent symptoms compared with 57% of the subgroup with preinjury depression and 66% of the subgroup with preinjury anxiety. Finally, Corwin and colleagues9 studied a sample of patients from a tertiary specialty clinic (N = 247) who had a high rate of persistent symptoms lasting >4 weeks (ie, 73%). The small sample of patients with preinjury depression (n = 15) or anxiety (n = 9) took twice as long, on average, to recover than did the patients without these conditions.
There are many potential reasons why, and mechanisms by which, preinjury mental health problems might be a risk factor for worse outcome. Both genetic22 and family-environmental3,10 risk factors for mood and anxiety disorders are present in adolescents and young adults. Depression and anxiety in youth are associated with a personal history of adverse events during childhood,14,16,40 attention-deficit/hyperactivity disorder,27,35 greater life stressors,24,33 substance misuse or abuse,18,41 less effective coping skills,8 less emotional awareness,39 and lower resilience.37 In adolescents, changing or decreasing daily activities because of physical illness or injury is associated with depression.21 Moreover, a history of depression or anxiety is associated with increased risk for a future problem with depression or anxiety.40 All of the above factors are potentially relevant in a biopsychosocial vulnerability model that examines how preinjury mental health might relate to postinjury coping strategies, symptom expression, resilience, and clinical outcome.
Limitations
Our systematic review has several important limitations. We reviewed only published articles, so there is a risk for publication bias. We included studies published in English, so there is a potential for language-of-publication bias in our conclusions. Mental health problems were not assessed using gold standard instruments, such as diagnostic interviews (eg, the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders–5) or empirically validated self-report measures (eg, Patient Health Questionnaire–9; General Anxiety Disorder–7). Neither the severity of psychological symptoms nor psychological treatment status at the time of concussion were reported. Another limitation is that many of the original studies did not report specific symptoms endorsed on the postconcussion symptom scale (eg, sadness, nervousness, difficulty concentrating, sleep problems). It is possible that these symptoms were interpreted to be related to the athlete’s concussion but may have been more related to the athlete’s preexisting mental health condition. Most studies were statistically underpowered to detect group differences because of small sample sizes. When examining method and risk for bias, we rated the studies in relation to preinjury mental health as a predictor of worse clinical outcome from concussion—not based on how the original authors designed their studies—which likely resulted in some studies receiving less credit than they would have if they were rated based on their original intent and design. Most importantly, we could not aggregate data across studies or compute meaningful effect sizes to meta-analyze due to substantial variability in the definition of outcome across studies.
Directions for Future Research
There are 5 important directions for future research. First, to date, very few studies have been designed specifically to examine preinjury mental health as a prognostic factor, and most studies have been underpowered. There is a need to conduct better powered studies in samples selected from populations of middle school students, high school students, collegiate athletes, and youth presenting to concussion clinics, preferably using a priori power calculations to determine necessary sample size. Given that pediatricians’ offices are a common initial point of concussion care,1 it would be of interest to enroll injured youth from pediatric and primary care offices as well.
Second, the studies to date are not representative of most student-athletes who sustain concussions, because most studies are based on patients who attend the emergency department acutely or those who present to specialty clinics for health care, most likely due to having persistent symptoms or being at risk for having persistent symptoms. There is a need to study a large representative sample of student-athletes, such as National Collegiate Athletic Association Division I athletes enrolled in the Concussion Assessment, Research and Education Consortium,4 or a large representative sample of high school students.
Third, there is a need to better characterize preinjury mental health problems in concussion studies, because most studies simply collect lifetime history in a binary (yes/no) manner. It would be interesting to determine whether there are differences in outcome for athletes whose prior mental health difficulties either are not present or are well-controlled at the time of baseline testing compared with those experiencing difficulties at the time of baseline testing. We encourage authors of future studies to use empirically validated assessments of mental health and to report current psychological diagnoses, symptom severity, and treatment status.
Fourth, more research is needed on quantifying the risk in clinically relevant terms (eg, how many more days, on average, does it take for someone with a history of mental health conditions to recover from a concussion compared with someone without mental health history?).
Fifth, it will be important to conduct research designed to better understand the mechanisms by which preinjury mental health problems confer risk and whether there are specific subgroups who might benefit from early, or different, treatment and rehabilitation approaches. It is not known, for example, whether youth with preinjury mental health problems have worse or different acute symptoms in the first 72 hours after injury. Acute symptoms are important, and several studies have shown that greater acute symptoms are a risk factor for slower clinical recovery.5,7,23,36 It is also important to determine whether and why preinjury mental health problems might be associated with greater difficulties with return to school. Future studies addressing the knowledge gaps identified in this review will ideally lead to a better understanding of the mechanisms by which preinjury mental health confers risk for worse outcome and will inform earlier intervention and overall better treatment and rehabilitation strategies for at-risk student-athletes.
Conclusion
In this systematic review, most studies found that preexisting mental health conditions were associated with a longer recovery from a concussion, and these studies entailed very different methods and outcomes. Future research is needed to (1) examine this risk factor in large, representative populations of middle school students, high school students, and collegiate athletes; (2) quantify the risk for each mental health condition; (3) understand the mechanisms underlying this increased risk; and (4) develop more refined treatment and rehabilitation approaches for these student-athletes.
Acknowledgment
The authors thank Fionn Büttner for completing the likelihood ratio heuristic analyses.
Appendix
Likelihood Heuristic
In 2017, Lakens and Etz19 published a likelihood heuristic that can be applied to systematic literature reviews. We applied this method, for the first time, to systematic review data in the sport concussion literature.6 This heuristic is applied to a series of studies that examine the same topic but are not amenable to meta-analytic methods. It considers the number of statistically significant and nonsignificant studies and estimates the likelihood of observing a specific number of significant studies if the alternative hypothesis is true relative to if the null hypothesis is true. The probability of observing a specific number of significant results is calculated in 2 ways, assuming that (1) the alternative hypothesis is true and studies had 80% statistical power and (2) the null hypothesis is true and studies had a 5% type I error rate . The formula below is used to calculate a probabilistic estimate for each hypothesis (ie, alternative and null hypotheses):
where n is the sum of significant and nonsignificant studies for the prognostic factor (ie, preinjury mental health problems), k is the number of significant studies, and θ can represent either statistical power or study alpha level. When calculating the probabilistic estimate for whether the alternative hypothesis is true, θ is the parameter for statistical power (0.8; ie, the numerator of the likelihood ratio). When calculating the probabilistic estimate assuming the null hypothesis is true, θ is the parameter value of the alpha level (.05; ie, the denominator of the likelihood ratio). To produce the likelihood ratio, the probability of observing a certain number of significant studies assuming the alternative hypothesis was true (ie, the numerator) is divided by the probability of observing significant studies assuming the null hypothesis was true (ie, the denominator). The likelihood ratio calculations can be performed using an openly available online calculator (https://lakens.shinyapps.io/likelihood/) produced by the authors of the original study on this method.19 Büttner et al6 provided a detailed explanation of the likelihood ratio heuristic method and created separate statistical code, in R,34 establishing agreement between the online calculator and the published formula. Likelihood ratios of 8 and 32 are proposed as thresholds for moderate and strong evidence, respectively.38
Footnotes
Final revision submitted March 28, 2020; accepted April 10, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded in part by the National Football League for a program of research titled “The Spectrum of Concussion: Predictors of Clinical Recovery, Treatment and Rehabilitation, and Possible Long-term Effects.” G.L.I. serves as a scientific advisor for BioDirection, Sway Operations, and Highmark and has received research funding from ImPACT Applications, CNS Vital Signs and Psychological Assessment Resources, and the National Football League. A.J.G. has been a contracted concussion consultant to Rugby Australia and has received grant funding from the NSW Sporting Injuries Committee, the Brain Foundation (Australia), and the Hunter Medical Research Institute; he is currently funded through an NHMRC Early Career Fellowship; the Hunter New England Local Health District, Research, Innovation and Partnerships Health Research & Translation Centre and Clinical Research Fellowship Scheme; an Australian-American Fulbright Commission Postdoctoral Award; and the University of Newcastle’s Priority Research Centre for Stroke and Brain Injury. D.P.T. is a consultant for REACT Neuro, Inc. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Arbogast KB, Curry AE, Pfeiffer MR, et al. Point of health care entry for youth with concussion within a large pediatric care network. JAMA Pediatr. 2016;170(7):e160294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Asken BM, McCrea MA, Clugston JR, et al. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51(4):329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beardslee WR, Gladstone TR, O’Connor EE. Developmental risk of depression: experience matters. Child Adolesc Psychiatr Clin N Am. 2012;21(2):261–278, vii. [DOI] [PubMed] [Google Scholar]
- 4. Broglio SP, McCrea M, McAllister T, et al. A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA-DoD Concussion Assessment, Research and Education (CARE) consortium structure and methods. Sports Med. 2017;47(7):1437–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown NJ, Mannix RC, O’Brien MJ, et al. Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. 2014;133(2):e299–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Büttner F, Terry DP, Iverson GL. Using a likelihood heuristic to summarize conflicting literature on predictors of clinical outcome following sport-related concussion. Clin J Sport Med. Published online September 15, 2020 doi:10.1097/JSM.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 7. Castile L, Collins CL, McIlvain NM, Comstock RD. The epidemiology of new versus recurrent sports concussions among high school athletes, 2005-2010. Br J Sports Med. 2012;46(8):603–610. [DOI] [PubMed] [Google Scholar]
- 8. Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87–127. [PubMed] [Google Scholar]
- 9. Corwin DJ, Zonfrillo MR, Master CL, et al. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. J Pediatr. 2014;165(6):1207–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Devenish B, Hooley M, Mellor D. The pathways between socioeconomic status and adolescent outcomes: a systematic review. Am J Community Psychol. 2017;59(1-2):219–238. [DOI] [PubMed] [Google Scholar]
- 11. Eisenberg MA, Andrea J, Meehan W, Mannix R. Time interval between concussions and symptom duration. Pediatrics. 2013;132(1):8–17. [DOI] [PubMed] [Google Scholar]
- 12. Ellis MJ, Cordingley DM, Vis S, et al. Clinical predictors of vestibulo-ocular dysfunction in pediatric sports-related concussion. J Neurosurg Pediatr. 2017;19(1):38–45. [DOI] [PubMed] [Google Scholar]
- 13. Ellis MJ, Ritchie LJ, Koltek M, et al. Psychiatric outcomes after pediatric sports-related concussion. J Neurosurg Pediatr. 2015;16(6):709–718. [DOI] [PubMed] [Google Scholar]
- 14. Fassett-Carman A, Hankin BL, Snyder HR. Appraisals of dependent stressor controllability and severity are associated with depression and anxiety symptoms in youth. Anxiety Stress Coping. 2019;32(1):32–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fehr SD, Nelson LD, Scharer KR, et al. Risk factors for prolonged symptoms of mild traumatic brain injury: a pediatric sports concussion clinic cohort. Clin J Sport Med. 2019;29(1):11–17. [DOI] [PubMed] [Google Scholar]
- 16. Harkness KL, Lumley MN, Truss AE. Stress generation in adolescent depression: the moderating role of child abuse and neglect. J Abnorm Child Psychol. 2008;36(3):421–432. [DOI] [PubMed] [Google Scholar]
- 17. Iverson GL, Gardner AJ, Terry DP, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Johannessen EL, Andersson HW, Bjorngaard JH, Pape K. Anxiety and depression symptoms and alcohol use among adolescents—a cross sectional study of Norwegian secondary school students. BMC Public Health. 2017;17(1):494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lakens D, Etz AJ. Too true to be bad: when sets of studies with significant and nonsignificant findings are probably true. Soc Psychol Personal Sci. 2017;8(8):875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lawrence DW, Richards D, Comper P, Hutchison MG. Earlier time to aerobic exercise is associated with faster recovery following acute sport concussion. PLoS One. 2018;13(4):e0196062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lewinsohn PM, Gotlib IH, Seeley JR. Depression-related psychosocial variables: are they specific to depression in adolescents? J Abnorm Psychol. 1997;106(3):365–375. [DOI] [PubMed] [Google Scholar]
- 22. Maglione D, Caputi M, Moretti B, Scaini S. Psychopathological consequences of maltreatment among children and adolescents: a systematic review of the GxE literature. Res Dev Disabil. 2018;82:53–66. [DOI] [PubMed] [Google Scholar]
- 23. Makdissi M, Darby D, Maruff P, et al. Natural history of concussion in sport: markers of severity and implications for management. Am J Sports Med. 2010;38(3):464–471. [DOI] [PubMed] [Google Scholar]
- 24. Mazurka R, Wynne-Edwards KE, Harkness KL. Stressful life events prior to depression onset and the cortisol response to stress in youth with first onset versus recurrent depression. J Abnorm Child Psychol. 2016;44(6):1173–1184. [DOI] [PubMed] [Google Scholar]
- 25. McCrea M, Iverson GL, McAllister TW, et al. An integrated review of recovery after mild traumatic brain injury (MTBI): implications for clinical management. Clin Neuropsychol. 2009;23(8):1368–1390. [DOI] [PubMed] [Google Scholar]
- 26. McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016 Br J Sports Med. 2017;51(11):838–847. [DOI] [PubMed] [Google Scholar]
- 27. Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: a meta-analytic review. Clin Psychol Rev. 2014;34(8):595–607. [DOI] [PubMed] [Google Scholar]
- 28. Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Study–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269, W64. [DOI] [PubMed] [Google Scholar]
- 30. Mooney G, Speed J, Sheppard S. Factors related to recovery after mild traumatic brain injury. Brain Inj. 2005;19(12):975–987. [DOI] [PubMed] [Google Scholar]
- 31. Morgan CD, Zuckerman SL, Lee YM, et al. Predictors of postconcussion syndrome after sports-related concussion in young athletes: a matched case-control study. J Neurosurg Pediatr. 2015;15(6):589–598. [DOI] [PubMed] [Google Scholar]
- 32. OCEBM Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine. Accessed June 18, 2019 https://www.cebm.net/index.aspx?o=5653.
- 33. Pan LA, Goldstein TR, Rooks BT, et al. The relationship between stressful life events and axis I diagnoses among adolescent offspring of probands with bipolar and non-bipolar psychiatric disorders and healthy controls: the Pittsburgh Bipolar Offspring Study (BIOS). J Clin Psychiatry. 2017;78(3):e234–e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2014. [Google Scholar]
- 35. Reale L, Bartoli B, Cartabia M, et al. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. 2017;26(12):1443–1457. [DOI] [PubMed] [Google Scholar]
- 36. Resch JE, Brown CN, Macciocchi SN, et al. A preliminary formula to predict timing of symptom resolution for collegiate athletes diagnosed with sport concussion. J Athl Train. 2015;50(12):1292–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Reuben JD, Shaw DS. Resilience in the offspring of depressed mothers: variation across risk, domains, and time. Clin Child Fam Psychol Rev. 2015;18(4):300–327. [DOI] [PubMed] [Google Scholar]
- 38. Royall R. Statistical Evidence: A Likelihood Paradigm. CRC Press; 1997. [Google Scholar]
- 39. Sendzik L, Schafer JO, Samson AC, Naumann E, Tuschen-Caffier B. Emotional awareness in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc. 2017;46(4):687–700. [DOI] [PubMed] [Google Scholar]
- 40. Sousa C, Mason WA, Herrenkohl TI, et al. Direct and indirect effects of child abuse and environmental stress: a lifecourse perspective on adversity and depressive symptoms. Am J Orthopsychiatry. 2018;88(2):180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Strandheim A, Bratberg GH, Holmen TL, Coombes L, Bentzen N. The influence of behavioural and health problems on alcohol and drug use in late adolescence—a follow up study of 2399 young Norwegians. Child Adolesc Psychiatry Ment Health. 2011;5(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Terwilliger VK, Pratson L, Vaughan CG, Gioia GA. Additional post-concussion impact exposure may affect recovery in adolescent athletes. J Neurotrauma. 2016;33(8):761–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vargas G, Rabinowitz A, Meyer J, Arnett PA. Predictors and prevalence of postconcussion depression symptoms in collegiate athletes. J Athl Train. 2015;50(3):250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed June 23, 2019 http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 45. Yang J, Peek-Asa C, Covassin T, Torner JC. Post-concussion symptoms of depression and anxiety in division I collegiate athletes. Dev Neuropsychol. 2015;40(1):18–23. [DOI] [PubMed] [Google Scholar]
- 46. Zemek R, Barrowman N, Freedman SB, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014–1025. [DOI] [PubMed] [Google Scholar]