Background: Initially projected to be the fourth most at-risk country for coronavirus disease 2019 (COVID-19) because of its close ties with China (1), Taiwan, on 21 December 2020, marked 253 consecutive days without a locally transmitted case, and a cumulative total of 770 cases (675 imported) and 7 deaths (2). Despite imported cases, Taiwan has successfully contained COVID-19 without a national lockdown (Figure 1).
Figure 1. Timeline of imported and locally transmitted, confirmed cases of COVID-19; government measures; and public behavior changes throughout 2020 in Taiwan.
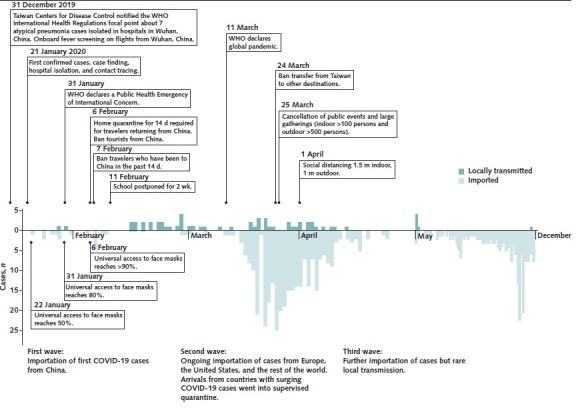
Daily numbers of COVID-19 cases (January to April) and condensed case demonstration (May to December) are plotted by dates of confirmation by reverse transcriptase polymerase chain reaction test. COVID-19 = coronavirus disease 2019; WHO = World Health Organization.
Taiwan's rapid, coordinated, and early response was informed by its experience during the outbreak of severe acute respiratory syndrome in 2003, when it had the third-highest death toll globally and longest-listed endemic travel alert by the World Health Organization (3).
In December 2019, Taiwan's early alert system prompted passenger screening on flights from Wuhan, China. Additional efforts followed, including a ban on all flights from Hubei province, targeted screening of symptomatic travelers using customs data linked to universal health care system electronic records, contact tracing and testing, and mandatory home quarantine for travelers from affected countries (4). From late March, further measures included extensive restrictions on outbound and inbound international travel, a system for universal face mask access, a mandatory face mask policy for public transportation and indoor spaces (with high adherence), physical distancing, large gathering restrictions, and hand sanitizer at most building entrances.
Objective: To assess the possibility of undocumented COVID-19 deaths in Taiwan and whether nonpharmaceutical interventions and behavior changes affected all-cause, pneumonia and influenza, and road traffic deaths in 2020.
Methods: We collected government data from 2008 to 2020 for yearly population, all-cause deaths, weekly pneumonia and influenza deaths, and monthly road traffic deaths (January to October 2020) (Figure 2). Using midyear population and World Health Organization standard population (2000) data, we calculated the corresponding adjusted mortality rates per 100 000 persons and their 95% CIs for each year.
Figure 2. Adjusted all-cause, pneumonia and influenza, and road traffic mortality rates in Taiwan from 2008 to 2020.
Top. All-cause mortality rates are adjusted by sex and 5-y age groups. (Data from Taiwan Ministry of the Interior. Statistical Data Query. Accessed at https://statis.moi.gov.tw/micst/stmain.jsp?sys=100 on 12 January 2021.) Middle. Pneumonia and influenza mortality rates, including bacterial, viral, and unspecified pneumonia, are adjusted by 3 age groups (0 to 49, 50 to 64, and ≥65 y). (Data from Taiwan Centers for Disease Control. Taiwan National Infectious Disease Statistics System. Accessed at https://nidss.cdc.gov.tw/en/Default.aspx on 12 January 2021.) Bottom. Road traffic mortality rates (occurred within 30 d from the accident) are adjusted by 3 age groups (0 to 24, 25 to 64, and ≥65 y). (Data from Taiwan Ministry of Transportation and Communications. Commonly used transportation statistics. Accessed at https://stat.motc.gov.tw/mocdb/stmain.jsp?sys=100&funid=emenu on 12 January 2021.).
Findings: The age- and sex-adjusted all-cause mortality rate per 100 000 persons in 2020 was 399.8 (95% CI, 398.0 to 401.7), which is in line with the decreasing trend seen in recent years and notably lower than the 2019 rate (417.6 [CI, 415.7 to 419.6]) (Figure 2, top). The adjusted pneumonia and influenza mortality rate in 2020 was 48.7 (CI, 48.0 to 49.3), which is significantly lower than the 2019 rate (56.8 [CI, 56.1 to 57.5]) and a deviation from the overall increasing trend (Figure 2, middle). Finally, the adjusted road traffic mortality rate in 2020 was 8.8 (CI, 8.5 to 9.1), which is higher than the 2019 rate (8.4 [CI, 8.1 to 8.8]) but in line with the increasing trend in the past 3 years (Figure 2, bottom).
Discussion: Our results suggest that excess mortality in Taiwan in 2020 is highly unlikely because the adjusted all-cause mortality rate decreased compared with the 2019 rate and does not depart from the ongoing declining trend of previous years.
Excess deaths may occur beyond those directly attributed to COVID-19 (5), and inadequate testing may cause COVID-19 deaths to be underreported or misclassified as pneumonia or influenza because of symptomatic similarity. However, the low pneumonia and influenza mortality rate in 2020 suggests that mask wearing, physical distancing, and restricting large social events may have had a positive spillover effect. During the pandemic, pneumonia may receive greater attention and be more likely to be listed as the cause of death, generating possible overestimation. If so, this would strengthen our results because we found decreased, not increased, pneumonia deaths.
In contrast, recent road traffic deaths are harder to interpret. An overall downward trend since 2008 is disturbed by a slight increase since 2017. The greater number of road traffic deaths during the first 10 months of 2020 may be explained by the recent increasing trend or by behavior changes indirectly triggered by the pandemic, such as shifting from public to private transport, including cars and motorbikes, which have higher risks for accidents. Data from the Ministry of Transportation and Communications (see legend of Figure 2, bottom) show a 23% decrease in the use of Taipei Mass Rapid Transit (the largest public transportation service) from March to May 2020 versus the same period in 2019.
Taiwan's experience shows that nonpharmaceutical measures and mass behavior changes facilitated by nonauthoritarian governments can successfully suppress community spread, which can serve as an example for other countries. These measures will be important for preventing new, more transmissible variants of COVID-19 until vaccines allow for herd immunity.
Footnotes
This article was published at Annals.org on 2 February 2021
References
- 1. Chinazzi M , Davis JT , Ajelli M , et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395-400. [PMID: ] doi: 10.1126/science.aba9757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen W, Chang M, Wu J, et al. Taiwan reports first domestic case of COVID-19 in 253 days (update). Focus Taiwan. 22 December 2020. Accessed at https://focustaiwan.tw/society/202012220013 on 12 January 2021.
- 3. Summers J , Cheng H , Lin H , et al. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg Health West Pac. 2020;4:100044. doi: 10.1016/j.lanwpc.2020.100044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang CJ , Ng CY , Brook RH . Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341-1342. [PMID: ] doi: 10.1001/jama.2020.3151 [DOI] [PubMed] [Google Scholar]
- 5. Faust JS , Krumholz HM , Du C , et al. All-cause excess mortality and COVID-19-related mortality among US adults aged 25-44 years, March-July 2020. JAMA. 2020. [PMID: ] doi: 10.1001/jama.2020.24243 [DOI] [PMC free article] [PubMed] [Google Scholar]



