Abstract
Asthma, a chronic respiratory disease characterized by chronic airway inflammation, bronchial hyperresponsiveness, and reversible airflow obstruction, poses a substantial economic burden on patients and caregivers alike. Moreover, the heterogeneous nature of the disease and the presence of various phenotypes make the treatment of asthma challenging and nuanced. Despite the availability of several approved pharmacological treatments, approximately half of patients with asthma in the United States experienced exacerbations in 2016, highlighting the need for effective add-on treatments. Furthermore, asthma control remains suboptimal due to low adherence to medications, poor inhaler technique, and several patient-related factors. Importantly, the primary care setting, in which pharmacists play an integral role, represents a critical environment for providing long-term follow-up care for the effective management of chronic diseases, such as asthma. Pharmacists are uniquely positioned to ensure optimal clinical outcomes in patients with asthma since they have the clinical expertise to educate patients on their disease state and the role of asthma medications, provide training on inhalation technique, address patients’ concerns about potential side effects of medications, and improve adherence to therapy. Therefore, in this review article, we discuss the overall role of pharmacists in effective asthma care and management.
Keywords: asthma, clinical outcomes, inhaler, pharmacists, primary care
Introduction
Asthma, one of the most common chronic diseases, poses a substantial socioeconomic burden on both patients and caregivers.1 Asthma affects people of all ages, including children, with a considerable negative impact on both school and work performance. In 2017, an estimated 25.2 million people, including 6.2 million children, had asthma in the United States.2 Furthermore, despite a range of available therapies, approximately 11.5 million people, including 3.2 million children, reported having an asthma attack in 2016.3 In addition, poorly controlled asthma is associated with a significant increase in the number of missed school and workdays for children and caregivers alike.4 Consequently, asthma results in a significant economic burden in the United States, with total costs amounting to US$81.9 billion in 2013.1 Despite the availability of effective therapies, the management of asthma remains a challenge as it is dependent on the behaviors of both patients and health care providers (HCPs).5 Notably, pharmacists, who are an integral part of the health care team in the primary care setting,6 can provide long-term follow-up care for the effective management of chronic diseases, such as asthma. Therefore, in this review article, we discuss the crucial role of pharmacists in the management of asthma.
Pathophysiology of Asthma
Asthma is a heterogeneous disease characterized by chronic airway inflammation, bronchial hyperresponsiveness, and reversible airflow obstruction.7,8 The common asthma phenotypes include allergic asthma, nonallergic asthma, late-onset asthma, asthma with fixed airflow limitation, and asthma with obesity.9 Asthma is associated with a strong inflammatory component that primarily affects the larger conducting airways.8 Inflammatory patterns vary according to the phenotypes and involve several cell types, including T cells, mast cells, eosinophils, basophils, neutrophils, and lymphocytes.7 The initial diagnosis of asthma is based on the identification of the pattern of respiratory symptoms characteristic of asthma—fluctuating symptoms of wheezing, shortness of breath, tightness of chest, and cough—and confirmation of variable expiratory airflow limitation using spirometry.9 Depending on the level of treatment required to control symptoms and exacerbations, asthma severity is classified as mild, moderate, or severe.9
Asthma Treatment
The heterogeneous nature of asthma and the presence of various phenotypes present a number of treatment challenges.10 Consequently, there is a need for personalized asthma therapy taking into consideration both the clinical characteristics of patients and their response to medications.10 Overall, the goals of asthma management are to achieve good control of symptoms, maintain normal activity levels, and minimize the risk of future exacerbations and medication side effects.9 Numerous clinical practice guidelines are available worldwide to assist HCPs in making data-driven clinical decisions. In the United States, the National Heart, Lung, and Blood Institute (NHLBI) provides guidelines for the diagnosis and management of asthma, which were last updated in 2007.11 However, many significant developments in the diagnosis and treatment of asthma have been reported since their last update, and recommendations on fraction of exhaled nitric oxide, immunotherapy, indoor allergen reduction, bronchial thermoplasty, and intermittent use of inhaled corticosteroids (ICS) and long-acting muscarinic antagonists (LAMAs) need to be integrated into the NHLBI guidelines.12 The Global Initiative for Asthma (GINA), targeted toward primary care physicians, was launched in 1993 as a collaborative effort between the NHLBI and the World Health Organization.9 The GINA report, which was last updated in 2019, provides an evidence-based global asthma management strategy built-up on a review of recent scientific literature that can be adapted for use in different countries.
Treatment for asthma includes the use of controller and/or reliever medications. Controller medications are used for regular maintenance treatment and include ICS, ICS and long-acting β2-agonist (LABA) combinations, leukotriene receptor antagonists, oral corticosteroids (OCS), tiotropium, and immunomodulator (anti-immunoglobulin E or anti-interleukin-4/5) therapies.13 These drugs control asthma symptoms, reduce airway inflammation, and minimize the risk of future exacerbations. Inhaled corticosteroids are the mainstay of controller therapy and standard of care in long-term asthma treatment, and their use has been shown to decrease exacerbations, hospitalizations, and mortality.7,9 In addition, the use of ICS in combination with a LABA was reported to be more effective than increasing the ICS dose.14 Furthermore, the use of a LAMA, either in addition to LABA + ICS or as an alternative to a LABA added to ICS maintenance therapy, may be needed as add-on treatment in patients whose asthma is not well controlled on ICS and LABA.15,16 Of note, patients with severe asthma are good candidates for treatment with anti-inflammatory therapies, including newer biologic agents that target T-helper type 2 (Th2)–driven inflammatory pathways, because Th2-type inflammation is more common in these patients.17 Add-on therapy with immunomodulators, used in specific asthma populations having a severe asthma phenotype, has been shown to reduce exacerbations18,19 and hospitalizations.19
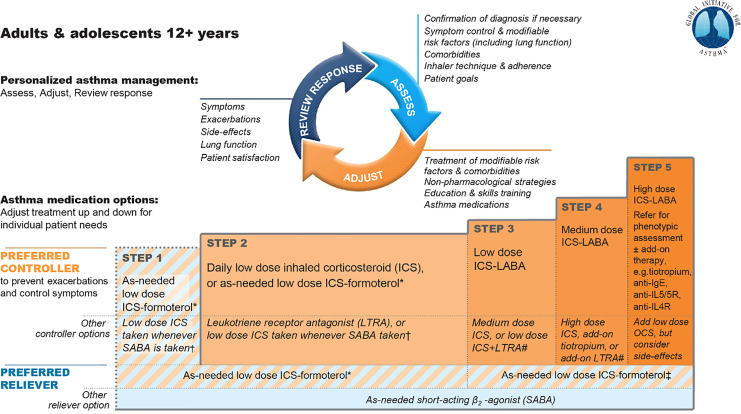
For patients who continue to experience uncontrolled symptoms or exacerbations following a reassessment of asthma diagnosis, inhaler technique, and adherence to medications, HCPs could consider stepping up treatment (Figure 1).13 Similarly, stepping down treatment is an option in patients whose symptoms have been controlled for 3 months and are at a low risk of exacerbations.9 However, stopping ICS completely is not advised. Reliever (rescue) medications are used “as needed” for the relief of breakthrough symptoms during asthma worsening or exacerbations and include SABAs and ICS/formoterol combination therapy.13 Despite the availability of these various treatment options, 46.9% of patients with asthma in the United States reported exacerbations in 2016, underscoring the need for effective add-on treatments.20 In addition to pharmacological therapy, nonpharmacological interventions may be used to improve asthma symptoms and reduce the risk of future exacerbations. These include engaging in regular physical activity; consuming a healthy diet; cessation of smoking; and avoiding indoor allergens, environmental exposure to smoke, occupational exposures, and medications that may worsen asthma.9 Treatment of modifiable risk factors and comorbidities, such as obesity and anxiety, is also recommended.9 Finally, it is important to note that although GINA provides population-based recommendations taking into account therapeutic options that are broadly effective in most patients, HCPs should make individualized treatment decisions following consideration of patient- and disease-related factors.
Figure 1.
Stepwise approach to control symptoms and minimize risk of future exacerbations in adults and adolescents 12 years and older with asthma as per GINA.13 For children 6-11 years, the preferred Step 3 treatment is low dose ICS-LABA or medium dose ICS. *Off-label; data only with budesonide-formoterol †Off-label; separate or combination ICS and SABA inhalers. ‡Low dose ICS-formoterol is the reliever for patients prescribed budesonide-formoterol or BDP-formoterol maintenance and reliever therapy. #Consider adding HDM SLIT for sensitized patients with allergic rhinitis and FEV1 >70% predicted. BDP indicates beclomethasone dipropionate; FEV1, forced expiratory volume in 1 second; GINA, Global Initiative for Asthma; HDM SLIT, house dust mites–sublingual immunotherapy; ICS, inhaled corticosteroids; IgE, immunoglobulin E; IL, interleukin; LABA, long-acting β2-agonist; LTRA, leukotriene receptor antagonist; OCS, oral corticosteroids; SABA, short-acting β2-agonist. Note: Reused with permission from Global Initiative for Asthma pocket guide 2019 (©: 2019 Global Initiative for Asthma, Inc.).
Inhaler devices in asthma treatment
Inhalation therapy is the cornerstone of asthma therapy; it allows delivery of the drug directly to the intended site of action, minimizes systemic side effects, and requires a lower dose of drugs.21 Asthma control depends not only on the pharmacological agent but also on the inhaler used for delivering the medication; hence, it is essential to match the right inhaler with the right patient, taking into consideration the needs, abilities, and preferences of each patient.22 Indeed, it has been observed that inhaler mishandling is common in real life,23 further highlighting the importance of correct inhaler technique. The main classes of asthma inhaler devices are small-volume nebulizers (SVNs), pressurized metered-dose inhalers (pMDIs), breath-actuated inhalers (BAIs), dry powder inhalers (DPIs), and soft mist inhalers (SMIs).21,24 Each device has its own advantages and disadvantages. Small-volume nebulizers use pneumatic or electrical energy to generate a respirable aerosol from aqueous solutions or suspensions.24,25 They do not require coordination between actuation and inhalation, making them suitable for children, the elderly, and nonconscious patients.21 However, SVNs are not easily portable, deliver a lower fraction of the medication to the lungs, can cause considerable drug loss during exhalation, and require a long treatment time and a considerable amount of cleaning and maintenance.25 In contrast to SVNs, pMDIs use propellants as the energy source to generate aerosols from solutions or suspensions.21 Effective use of pMDIs requires coordination between actuation and inhalation, which can be difficult to achieve,21 resulting in insufficient drug delivery.26,27 However, spacers or BAIs can be used to overcome these challenges.21 All DPIs are breath actuated, that is, they utilize the patient’s inspiratory flow to generate the turbulent energy that helps in deagglomeration of the powder into a respirable fine particle size range.28 Thus, coordination between actuation and inhalation is not required. The peak inspiratory flow rate (PIFR) is the maximal airflow generated during the inspiratory cycle, and the minimal and optimal PIFRs required by DPIs vary.29 Additionally, PIFR is known to decrease significantly when symptoms of asthma increase, especially in children. Moreover, all DPIs have an intrinsic airflow resistance. Dry powder inhalers with low resistance require greater inspiratory effort for powder deagglomeration,28 and sufficient inspiratory flow is therefore difficult to achieve in patients such as children and the elderly with advanced respiratory diseases.21 Therefore, appropriate inhaler choice requires consideration of these circumstances.30 Depending on the mechanism employed for storage and dispensation of the drug, DPIs may be categorized as single-unit dose inhalers (each dose is loaded before inhalation), multidose reservoir inhalers (entire supply of drug is preloaded), or multiunit dose inhalers (single doses are individually sealed and released on actuation).21 Multidose reservoir DPIs protect the drug formulation from moisture.31 Soft mist inhalers overcome the limitations of both pMDIs and DPIs by avoiding the use of propellants, reducing inspiratory effort for inhalation, and allowing for consistent delivery of the drug aerosol to the lungs.32 However, coordination with actuation and breath is still required with an SMI.
Factors Influencing Clinical Outcomes in Asthma
Research has demonstrated that asthma control can be achieved in most patients33; however, in real life, asthma control is poor.34 Asthma control is influenced by several factors, including those that are disease related (eg, asthma type, comorbidities, and triggers), patient related (eg, sociodemographic factors, adherence to medications, perceptions, knowledge, and behaviors), and HCP related (eg, misdiagnosis, knowledge of current guidelines, attitude toward guidelines, and implementation of guidelines).33
Patient-related factors affecting clinical outcomes in asthma
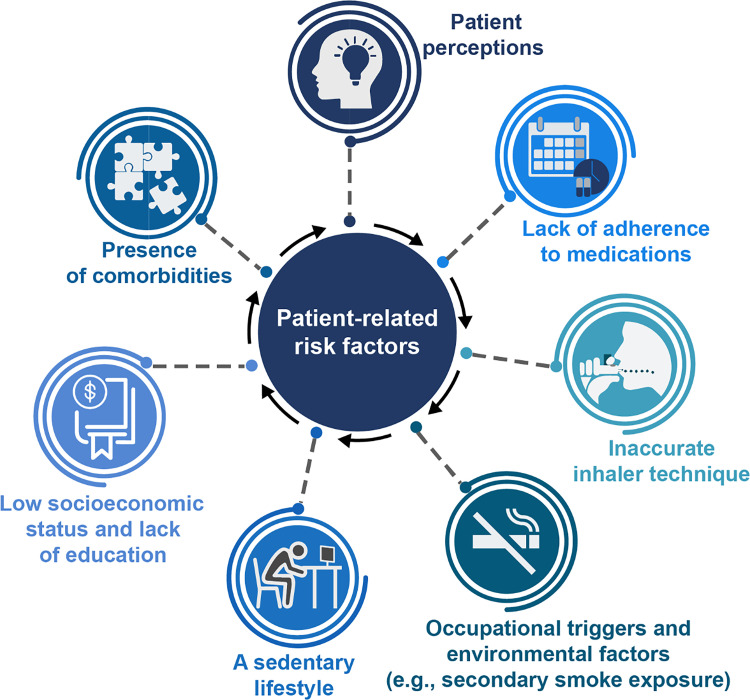
Several patient-related factors affect clinical outcomes in patients with asthma (Figure 2). For instance, patients’ perceptions influence behavioral choices (eg, smoking and lack of treatment adherence), which in turn affect treatment efficacy.35 Adherence is impeded by perceptual barriers, such as doubting the need for medication in the absence of symptoms, underestimating the significance of symptoms, concerns about drug-related side effects, and a lack of understanding of the importance of asthma control.35
Figure 2.
Patient-related factors predisposing them to worsening of asthma.
Lack of adherence to treatment and poor inhaler technique are the most commonly reported patient-related factors associated with poor asthma control.36 Nonadherence can be either “non-intentional” (eg, forgetting to take the medication) or “intentional” (eg, conscious decision to not take the medicine as prescribed due to perceived risks).36 Poor adherence is associated with an increase in costs of care and a discernible reduction in quality of life (QoL).37,38 As the rate of adherence to therapy is low in asthma patients, ranging from 30% to 70% in children and adults,39 poor control of asthma symptoms should alert primary care providers to potential nonadherence in such patient populations. Incorrect inhaler technique is associated with poor asthma control, an increased risk of hospitalizations and emergency room visits, and an increased likelihood of prescription for an OCS course.23,40 Indeed, results of a recent systematic review of pMDI and DPI technique reported that incorrect inhaler technique was very frequent (31%) and had not improved over the period from 1975 to 2014.41 The most frequently reported errors were lack of coordination between actuation and inhalation and incorrect speed and/or depth of inhalation with pMDIs; incorrect preparation of the inhaler device and lack of full expiration before inhalation with DPIs; and lack of postinhalation breath hold, which was common for both pMDIs and DPIs.41 In another study assessing real-life inhaler handling, lack of hand-lung synchronization, lack of cartridge in device, and inhalation despite having dose counter at zero were the most commonly noted errors with an SMI.42
In addition to nonadherence and poor inhaler technique, occupational triggers and environmental factors (eg, secondary smoke exposure) are also associated with uncontrolled asthma.43 Likewise, a sedentary lifestyle also negatively influences asthma control compared with a more active lifestyle.44 Low socioeconomic status is associated with an increase in the incidence and prevalence of asthma,45 poor asthma control,46,47 and increased use of emergency health services.46 Patients with a poor economic status may have higher exposure to indoor or outdoor allergens46 and limited access to health care resources,47 both of which impact asthma control. Furthermore, a patient who is less educated may not understand some asthma symptoms, which could have an impact on adherence to treatment.33 Conversely, a higher education in parents has been found to be associated with better asthma control in children.48 Several comorbidities and conditions, such as allergic rhinitis, obesity, gastroesophageal reflux disease, psychological disturbances, and obstructive sleep apnea, are frequently observed in patients with asthma and may impact the clinical manifestation and severity of asthma.49,50 Of note, the prevalence of psychiatric comorbidities, such as anxiety and depression, is high in patients with asthma.51
Role of Pharmacists
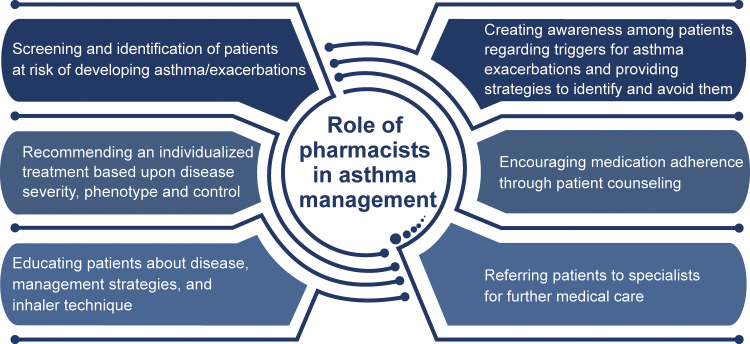
Pharmacists are uniquely positioned to improve outcomes in asthma patients given their clinical expertise in patient management and their ability to educate patients on asthma medications, provide training on inhalation technique, address patients’ concerns around the potential side effects of medications, and improve adherence to treatment.52 Indeed, the National Governors Association highlights the importance of pharmacists in providing direct health care to patients in an integrated health care system.53 Furthermore, pharmacists are more easily accessible than HCPs and are often the first point of contact in community settings.54 As such, pharmacists have the opportunity to provide advice on preventive care for chronic diseases (eg, conduct screenings, educate patients, make referrals to HCPs for follow-up care).55 As pharmacists interact with patients on an ongoing basis during prescription refills, they can play an active role in asthma management given their knowledge and expertise on medications.52 The NHLBI guidelines highlight the role of pharmacists in asthma management through educational interventions and therapeutic management.56 Results of a comprehensive review including 25 studies showed that pharmacist-led interventions improved asthma outcomes (such as asthma severity and health-related QoL) and reduced health care utilization in community pharmacy settings, and improved asthma symptoms and reduced health care utilization in ambulatory clinics as a result of patient education, medication management, and monitoring components of patients’ self-management.57 Studies with pharmacist-led interventions have been conducted in different practice settings (eg, community pharmacies, inpatient admissions, and outpatient clinics) as well as with different practice models (eg, telemedicine and asthma education programs), and results of such interventions can be applied to broader practice settings and models. Figure 3 highlights the role of pharmacists in asthma care and management.
Figure 3.
Role of pharmacists in asthma management.
Educate patients on asthma and treatment options
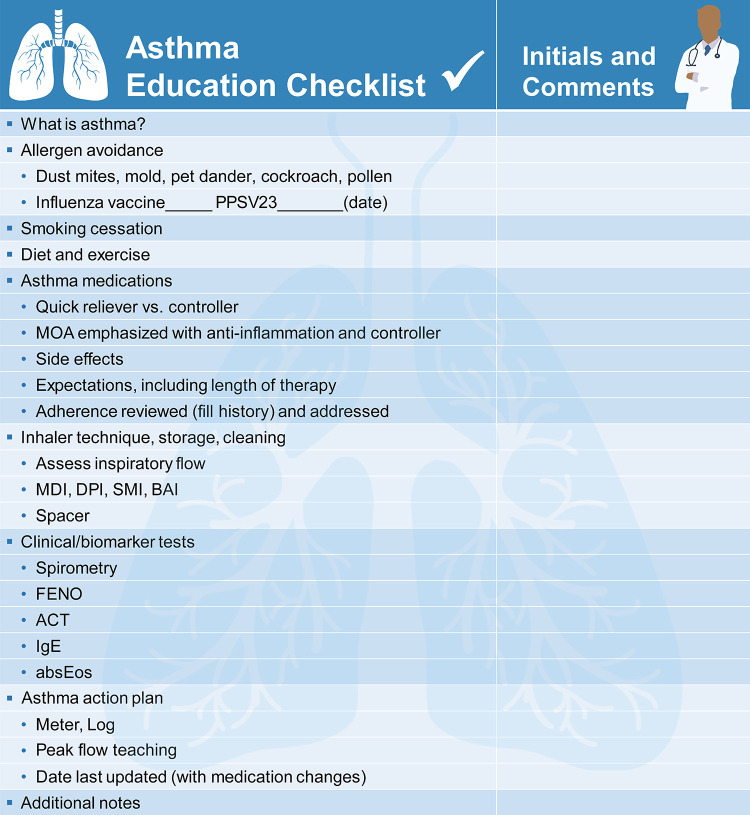
General health literacy is essential for successful asthma management. Studies have shown that low literacy correlates with poor knowledge of asthma and asthma medications and suboptimal pMDI inhaler technique in adults.58,59 A systematic review of 13 studies showed that low parental literacy was associated with poor asthma control in children and increased health care utilization.60 Consequently, providing tailored education can overcome barriers of low literacy and improve asthma self-management.59 A discussion on the patient’s understanding of asthma and treatment goals is often the starting point of asthma education. More importantly, providing patients with medication and inhaler options may help enhance adherence to therapy, thereby improving treatment outcomes. In this context, an asthma education checklist could provide important discussion points for HCPs to aid their interaction with patients (Figure 4).
Figure 4.
Asthma education checklist. absEos indicates absolute eosinophils; ACT, Asthma Control Test; BAI, breath-actuated inhaler; DPI, dry powder inhaler; FENO, fractional exhaled nitric oxide; IgE, immunoglobulin E; MDI, metered-dose inhaler; MOA, mechanism of action; PPSV, pneumococcal polysaccharide vaccine; SMI, soft mist inhaler.
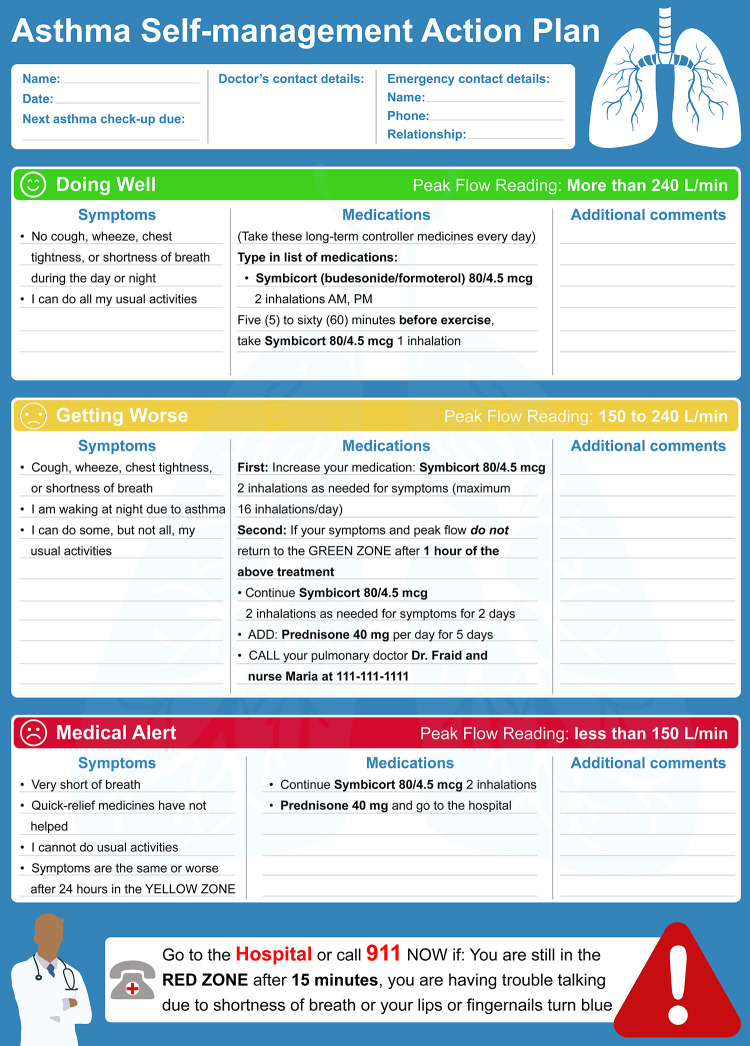
Pharmacists also play an important role in ensuring that patients have an asthma action plan to follow. Written action plans, which can assist with the detection and early treatment of exacerbations, are an important part of self-management.61 Asthma action plans provide information on medications and their dosage, how to recognize symptom worsening, and steps to be followed in the case of an emergency (Figure 5).62 Individualized written action plans (ie, information on when and how to increase the dose, duration of reliever medication treatment, and when to seek medical help) along with information on the increased dosing of ICS and addition of OCS have been shown to improve asthma outcomes61 and should be completed by HCPs to maximize adherence and minimize errors.63 Indeed, results from a community pharmacy-based study in Canada, which incorporated a care protocol, including asthma education on medications, triggers, self-monitoring, and an asthma action plan, reported improvements in clinical and economic outcome measures (reductions in symptom scores, work/school absenteeism, medical visits, and emergency room visits and improvements in lung function, QoL, and asthma knowledge) in patients who received asthma self-management training by specially trained community pharmacists compared with usual care.64
Figure 5.
A prototype asthma action plan.
Train, assess, and correct inhaler technique of patients
Health care providers play a crucial role in the initial training of patients on correct inhaler technique and ensuring that this is maintained over the long term.65 Results from a recent study found that the knowledge of HCPs, including pharmacists, about asthma was significantly associated with inhaler demonstration skills.66 Consequently, providing pharmacists with effective education tools and specific training on asthma and inhaler technique will ensure that they can play a pivotal role in educating patients on correct inhaler techniques.67 Such training is essential because only a small proportion of patients receive information on inhaler use, with an even smaller proportion of patients having their inhaler technique checked over time.68 Pharmacists can also educate patients on how the medication present in their inhalers alleviates the symptoms of asthma and improves lung function.69 However, it is important that pharmacists do not rely on written or verbal instructions alone but also employ a step-by-step demonstration of inhalation technique with periodic reassessments.70,71 Following demonstration, pharmacists can assess patients’ technique and rectify as necessary. Repeating this training during follow-up visits will help consolidate the correct inhaler technique over time and eliminate errors. In addition, HCPs have the option of utilizing audio–visual aids and may instruct patients to use such materials.72 For instance, the American Lung Association and other internet sources provide a number of resources for both patients and caregivers, including videos on correct inhaler technique.73,74
Instruct about the importance of medication adherence
Medication adherence is a multi-phased process including initiation of prescribed therapy, implementation of therapy as prescribed, and subsequent persistence of the treatment regimen.34 Consequently, adherence to therapy remains suboptimal in many chronic diseases, including asthma.34 Owing to a lack of education on the disease state and medications, many patients tend to overestimate the risks related to ICS or may fail to understand the benefits of regular maintenance treatment with ICS due to their relatively slow onset of action compared with easily perceptible effects of SABAs or LABAs.36 Use of these bronchodilators without ICS is associated with adverse events (AEs), including mortality, and may result in poor asthma control.75 Ensuring effective communication between the patient and the pharmacist can help achieve adherence to maintenance ICS medications and prevent both AEs and mortality associated with overuse of bronchodilators in the absence of ICS. As patient counseling and providing drug information form the most common components of pharmacist-led interventions, it is essential that pharmacists focus on improvements in patients’ understanding not only of asthma and inhaler technique but also of treatment regimens and adherence.76 If patients are not satisfied with their treatment regimen, are experiencing AEs and/or are not achieving therapeutic benefit, or are not adhering to their prescribed medications, alternative regimens should be discussed with the patient and recommended to the physician. Interventions by HCPs have been shown to improve medication adherence in asthma, together with a reduction in the dose of controller medications and hospital admissions.77 The involvement of patients in the decision-making, particularly in relation to the choice of medication and inhaler, and the type of training provided have been shown to improve patient satisfaction, QoL, and overall medication adherence in an intervention review of 4 studies.78,79
Identify factors that worsen symptoms and ways to effectively manage triggering factors
Several factors are known to increase asthma attacks and exacerbations, such as tobacco smoke, dust mites, cockroaches, pets, mold, air pollution, infections (flu), physical exercise, bad weather, and fragrances, and pharmacists can help patients identify and manage triggering factors better.80-82 In addition, providing education to smokers with asthma and highlighting how smoking attenuates the effectiveness of certain asthma medications, such as ICS,83 could be of potential benefit. Furthermore, providing patients with detailed explanations on how asthma medications work, together with environmental interventions that could improve asthma control, could be of assistance. Finally, ensuring that patients are aware of treatment options, such as allergen immunotherapy as add-on to immunotherapy for the management of allergic-type asthma, is imperative in enhancing patients’ involvement in decision-making.
Pharmacist-Led Interventions for Improving Clinical Outcomes in Patients With Asthma
Several pharmacist-led interventions conducted worldwide have improved clinical outcomes in asthma patients in different settings (Table 1).
Table 1.
Impact of Pharmacist-Led Interventions on Clinical Outcomes in Patients With Asthma.
| Publication; type of study | Participant characteristics | Interventions | Outcome |
|---|---|---|---|
| Community pharmacy setting | |||
| Maricoto et al,84 meta-analysis | N = 1812 participants aged ≥65 years with asthma or COPD (8 studies) | Physical demonstration of inhaler technique and training with placebo devices in patients with asthma and COPD | A significant reduction in exacerbation rates following pharmacist-led interventions |
| Dokbua et al,85 systematic review and meta-analysis | N = 2121 participants with asthma (12 studies across 8 countries) | Self-management support services (eg, self-monitoring and an action plan) provided by community pharmacists | Improvement in symptom control, QoL, and adherence to treatment |
| Mehuys et al,52 randomized controlled | N = 201 adults from 66 community pharmacies in Belgium | Education on asthma, inhaler technique, and medication adherence | Significant improvements in asthma control, inhaler technique, and adherence compared with usual care in patients with partially controlled asthma |
| Manfrin et al,86 randomized controlled | N = 810 adults from 15 regions of Italy | Systematic and structured consultation with a pharmacist covering asthma symptoms, medication adherence, and pharmacist-identified pharmaceutical care issues | Significant improvements in asthma control and adherence |
| Schulz et al,87 controlled | N = 242 participants from Germany | Education on disease, pharmacotherapy, and self-management; assessment and correction of inhalation technique; and detection of drug- or health-related issues | Significant improvements in evening peak expiratory flow rate, asthma-specific QoL, and inhalation technique in patients with mild to severe asthma |
| Saini et al,88 controlled | N = 102 participants from Australia | Assessment of asthma severity and provision of a written action plan, education, and regular review | A significant reduction in asthma severity and daily dose of reliever medication and a significant improvement in perceived asthma control and asthma knowledge |
| Stergachis et al,90 randomized controlled | N = 330 children from the United States | Structured training to provide individualized asthma management services | No significant effect on health or health service use outcomes |
| Outpatient setting | |||
| Knoell et al,91 controlled | N = 100 participants from the United States | Interaction of pharmacists with physicians and patients regarding self-management plans | A significant increase in patients’ awareness about self-management and likelihood of monitoring peak flow readings |
| González-Martin et al,92 pharmaceutical care program | N = 21 children with stable and moderate asthma from Chile | Education on disease, pharmacotherapy, self-management, and inhalation technique | A significant improvement in QoL reflected in PAQLQ scores |
| Diamond and Chapman,93 nationally coordinated asthma education program | N = 4080 participants from Canada | One-on-one counseling sessions with a pharmacist on self-management behavior and markers of asthma control, tailoring to each patient’s educational needs | A significant decrease in the frequency of daytime and nocturnal asthma symptoms and use of reliever medications, and a significant increase in the use of controller medication in patients with asthma |
Abbreviations: COPD, chronic obstructive pulmonary disease; PAQLQ, Pediatric Asthma Quality of Life Questionnaire; QoL, quality of life.
Community pharmacy settings
A recent meta-analysis including 4 randomized controlled trials and 4 quasi-experimental studies in 1812 participants reported a significant reduction in exacerbation rates in patients with asthma or chronic obstructive pulmonary disease (COPD) following pharmacist-led interventions, including physical demonstration of inhaler technique and training with placebo devices. However, the impact on disease control and QoL was inconsistent and the authors concluded that all the randomized trials revealed uncertain or high risk of bias based on risk of bias assessment recommended by Cochrane.84 Results of a systematic review of 12 studies conducted in 8 countries demonstrated that self-management support services (eg, self-monitoring and an action plan) provided by community pharmacists helped improve symptom control, QoL, and adherence to treatment in patients with asthma.85 Results of a 6-month randomized trial conducted in community pharmacies across Belgium also demonstrated that pharmacist-led interventions, focused on improving inhalation technique and medication adherence, significantly improved asthma control compared with usual care in patients with partially controlled asthma. Furthermore, pharmacist-led interventions reduced reliever medication use and improved inhaler technique and treatment adherence in all patients.52 Similarly, improvements in asthma control and adherence were observed after a community pharmacist-led intervention, which consisted of a systematic, structured face-to-face consultation with pharmacists, covering asthma symptoms, medicines used, attitude toward medicines and adherence, and issues impacting optimal medicine use and asthma control in a cluster randomized controlled trial in Italy.86 A 12-month controlled intervention study in Germany, in which community pharmacists provided education on disease, pharmacotherapy, and self-management; assessed and corrected inhalation technique; and helped detect and resolve drug- or health-related issues, demonstrated a significant improvement in evening peak expiratory flow rate, asthma-specific QoL, and inhalation technique in patients with mild to severe asthma.87 A 6-month community pharmacist-led intervention (assessing asthma severity, helping patients achieve and maintain better lung function by optimal medication use and trigger avoidance, and providing a written action plan, education, and regular review) in Australia reported a significant reduction in asthma severity and daily dose of reliever medication and a significant improvement in perceived asthma control and asthma knowledge.88 The Asthma Friendly Pharmacy model, providing interventions to patients, was shown to be feasible in community settings in the United States.89 Pharmacist-led interventions in this model included educating patients on asthma and medications, emphasizing the importance of the medication regimen and adherence, assessing inhalation technique, implementing an asthma action plan, providing counseling on smoking cessation, and strengthening relationships among pharmacists, patients, and HCPs.89 However, in a randomized controlled trial in the United States, a community pharmacist-led intervention did not demonstrate significant improvements in lung function, QoL, and use of asthma-related health care services in pediatric patients with asthma, likely due to low compliance of pharmacists with the study protocol.90 In summary, most of the studies conducted in community pharmacy settings indicated positive outcomes on health status and overall adherence through different pharmacist-led interventions, ranging from educating patients on disease state, treatment options, and importance of adherence to assessing inhaler technique and the use of written action plans.
Outpatient settings
In an outpatient setting in the United States, patients receiving a pharmacist-provided education program in addition to pulmonologist-provided care had more information on self-management of asthma, were more likely to monitor their peak flow readings, and reported greater satisfaction with asthma care compared with patients receiving pulmonologist care alone.91 An asthma education and monitoring program (providing asthma knowledge, evaluating symptoms and exacerbations, and assessing pharmacotherapy including inhaler technique) in an outpatient pediatric clinic in Chile improved QoL compared with the control group in children with asthma.92
A nationally coordinated pharmacy-based assessment and educational intervention across community pharmacies in Canada demonstrated a significant decrease in the frequency of daytime and nocturnal asthma symptoms and use of reliever medications, along with a significant increase in the use of controller medication in patients with asthma, 30 days following a one-on-one counseling session on self-management behavior and markers of asthma control with a pharmacist.93
Inpatient settings
In an inpatient setting, patients seeking care at emergency departments for an exacerbation of asthma, COPD, or congestive heart failure were assessed for their medication adherence or administration technique, patient-specific concerns with respect to medication use, the need for modification of therapy, access to medications at discharge, contraindicated medications, and vaccinations, if applicable, and subsequently referred by pharmacists to follow-up in either an ambulatory care pharmacy clinic or with the home-based medication management program.94 Although a small exploratory study, it highlighted the potential role of pharmacists in transition-of-care programs at discharge and follow-up opportunities at outpatient clinics or home-based medication management programs. In another study, pharmacists’ intervention in the discharge process increased the proportion of patients discharged in possession of their medications and decreased unplanned visits after discharge in a cohort of 102 children with asthma.95
Other strategies
While pharmacists are often the first point of contact in the primary care setting, it is not always possible for some patients to interact with HCPs on a regular basis. Telemedicine is an approach that allows real-time communication between a patient and a clinician at a remote site.96 It can be used for general asthma management and education for self-management, remote monitoring of a patient’s condition, identifying trends and triggers, and adjusting treatment. Clinical pharmacist-driven telemedicine interventions have demonstrated a positive impact on disease management, patients’ self-management, and adherence to treatment in chronic diseases, such as hypertension, heart failure, asthma, and COPD, among others.97 Furthermore, a telepharmacy-based asthma educational program, in which an independent community pharmacist with telehealth capabilities engaged with patients to assess their perception of asthma control, improved asthma control (Asthma Control Test score) in a majority of the patients after 6 visits in a year.98 The Extension for Community Healthcare Outcomes (ECHO) model uses state-of-the-art telehealth technology to train primary care providers to develop disease-specific knowledge, including inhaler technique, development of asthma action plans, and approach to manage poorly controlled asthma patients, and promises to be an effective way to help rural HCPs improve asthma control in their patients.99 To date, evidence on the impact of pharmacist-led telemedicine interventions is weak, as a majority of the studies had questionable internal and external validity. However, although definitive conclusions about the impact of such pharmacist-led telemedicine interventions cannot currently be made, telepharmacy remains a promising option for pharmacists to assume a more prominent role in asthma management in the ambulatory care setting to deliver asthma education services in rural areas. Moreover, since poor inhaler technique remains a major barrier to asthma control,23 feasible, inexpensive, and scalable approaches, such as inhaler technique reminder labels highlighting patients’ initial errors100 and pictograms,101 have been adopted and these approaches show promise. In addition, reminder labels have significantly improved retention of correct inhaler technique with DPIs,100 and pictogram-incorporated medals have improved inhaler technique compared with verbal counseling alone.101 Pharmacists can assess medication cost and insurance coverage barriers and develop strategies to overcome them. For instance, pharmacists can help patients by identifying medications on formulary, completing prior authorization, and referring them to medication assistance programs to maximize the cost savings.102 Although pharmacists’ limited time and resources might be a barrier in implementation of some of these strategies, potential benefits discussed herein warrant validation in a larger patient population. In addition, pharmacists should keep abreast of asthma management guidelines, including NHLBI,56 GINA,13 and the National Institute for Health and Care Excellence.103 Pharmacists could also be encouraged to pursue multidisciplinary Asthma Educator Certification (AE-C®).104 Asthma education by AE-C® pharmacists improved medication adherence and asthma control as well as reduced hospital utilization in inner-city patients with asthma.105
Conclusion
Despite the availability of therapies, asthma control remains suboptimal due to low adherence, poor inhaler technique, and several patient-related factors. Asthma management depends on several factors, including trigger avoidance, smoking cessation, medication adherence, proper inhalation technique, asthma knowledge, and recognition of worsening of asthma symptoms. Furthermore, patients’ perceptions, socioeconomic status, and health literacy influence asthma-related outcomes. Pharmacists are uniquely positioned to assist with asthma management due to their clinical expertise and frequent contact with patients. Indeed, there is increasing evidence that pharmacist-led interventions improve asthma control. Pharmacists can provide education, assess inhaler technique and provide training when required, and refer patients to specialists when necessary. Therefore, there is a need for proactive and continual pharmacist engagement with asthma patients, physicians, nurses, and specialists to implement best practices in health care and achieve optimal clinical outcomes in patients with asthma.
Acknowledgments
The authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE). Writing, editorial support, and formatting assistance was provided by Sudha Korwar, PhD, Saurabh Gagangras, PhD, and Praveen Kaul, PhD, of Cactus Life Sciences (part of Cactus Communications), which was contracted and funded by Boehringer Ingelheim Pharmaceuticals, Inc. (BIPI). BIPI was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was funded by Boehringer Ingelheim Pharmaceuticals, Inc.
ORCID iD: Mary B. Bridgeman, PharmD, BCPS, BCGP  https://orcid.org/0000-0001-7947-9875
https://orcid.org/0000-0001-7947-9875
References
- 1. Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15(3):348–356. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. 2017 National Health Interview Survey (NHIS) Data. Table 3-1. Compiled March 18, 2019. Accessed June 24, 2019 https://www.cdc.gov/asthma/nhis/2017/table3-1.htm
- 3. Centers for Disease Control and Prevention. 2017 National Health Interview Survey (NHIS) Data. Table 5-1. Compiled March 18, 2019. Accessed June 24, 2019 https://www.cdc.gov/asthma/nhis/2017/table5-1.htm
- 4. Sullivan PW, Ghushchyan V, Navaratnam P, et al. The national burden of poorly controlled asthma, school absence and parental work loss among school-aged children in the United States. J Asthma. 2018;55(6):659–667. [DOI] [PubMed] [Google Scholar]
- 5. Dima AL, de Bruin M, Van Ganse E. Mapping the asthma care process: implications for research and practice. J Allergy Clin Immunol Pract. 2016;4(5):868–876. [DOI] [PubMed] [Google Scholar]
- 6. Scott MA, Heck JE, Wilson CG. The integral role of the clinical pharmacist practitioner in primary care. N C Med J. 2017;78(3):181–185. [DOI] [PubMed] [Google Scholar]
- 7. Ye Q, He X-O, D’Urzo A. A review on the safety and efficacy of inhaled corticosteroids in the management of asthma. Pulmonary Ther. 2017;3(1):1–18. [Google Scholar]
- 8. Barnes PJ. Similarities and differences in inflammatory mechanisms of asthma and COPD. Breathe. 2011;7(3):229–238. [Google Scholar]
- 9. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Updated 2018. Accessed May 31, 2019 https://ginasthma.org/wp-content/uploads/2019/01/2018-GINA.pdf
- 10. Bostantzoglou C, Delimpoura V, Samitas K, et al. Clinical asthma phenotypes in the real world: opportunities and challenges. Breathe (Sheff). 2015;11(3):186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. National Heart, Lung, and Blood Institute. Expert panel report 3: Guidelines for the Diagnosis and Management of Asthma, Clinical Practice Guidelines 2007. Published August 28, 2007. Accessed November 4, 2019 https://www.ncbi.nlm.nih.gov/books/NBK7232/
- 12. Ballas ZK. Asthma clinical practice guidelines: time for an update. J Allergy Clin Immunol. 2018;142(3):787. [DOI] [PubMed] [Google Scholar]
- 13. Global Initiative for Asthma. Pocket guide for asthma management and prevention. Updated 2019 Accessed April 25, 2019 https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket-Guide-wms.pdf
- 14. Pauwels RA, L öfdahl CG, Postma DS, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med. 1997;337(20):1405–1411. [DOI] [PubMed] [Google Scholar]
- 15. Buhl R, FitzGerald JM, Busse WW. Tiotropium add-on to inhaled corticosteroids versus addition of long-acting β2-agonists for adults with asthma. Respir Med. 2018;143:82–90. [DOI] [PubMed] [Google Scholar]
- 16. Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367(13):1198–1207. [DOI] [PubMed] [Google Scholar]
- 17. Peters SP, Busse WW. New and anticipated therapies for severe asthma. J Allergy Clin Immunol Pract. 2017;5(5S):S15–S24. [DOI] [PubMed] [Google Scholar]
- 18. Henriksen DP, Bodtger U, Sidenius K, et al. Efficacy, adverse events, and inter-drug comparison of mepolizumab and reslizumab anti-IL-5 treatments of severe asthma – a systematic review and meta-analysis. Eur Clin Respir J. 2018;5(1):1536097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yancey SW, Ortega HG, Keene ON, et al. Meta-analysis of asthma-related hospitalization in mepolizumab studies of severe eosinophilic asthma. J Allergy Clin Immunol. 2017;139(4):1167–1175.e2. [DOI] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention. Most recent asthma data. Accessed December 19, 2018 https://www.cdc.gov/asthma/most_recent_data.htm#modalIdString_CDCTable_1
- 21. Ibrahim M, Verma R, Garcia-Contreras L. Inhalation drug delivery devices: technology update. Med Devices (Auckl). 2015;8:131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kaplan A, Price D. Matching inhaler devices with patients: the role of the primary care physician. Can Respir J. 2018;2018:9473051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. [DOI] [PubMed] [Google Scholar]
- 24. Gregory KL, Wilken L, Hart MK. Pulmonary Disease Aerosol Delivery Devices: A Guide for Physicians, Nurses, Pharmacists, and Other Health Care Professionals. 3rd ed American Association for Respiratory Care; 2017. [Google Scholar]
- 25. Lavorini F, Fontana GA, Usmani OS. New inhaler devices – the good, the bad and the ugly. Respiration. 2014;88(1):3–15. [DOI] [PubMed] [Google Scholar]
- 26. Roche N, Dekhuijzen PN. The evolution of pressurized metered-dose inhalers from early to modern devices. J Aerosol Med Pulm Drug Deliv. 2016;29(4):311–327. [DOI] [PubMed] [Google Scholar]
- 27. Usmani OS, Biddiscombe MF, Barnes PJ. Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med. 2005;172(12):1497–1504. [DOI] [PubMed] [Google Scholar]
- 28. Dal Negro RW. Dry powder inhalers and the right things to remember: a concept review. Multidiscip Respir Med. 2015;10(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ghosh S, Ohar JA, Drummond MB. Peak inspiratory flow rate in chronic obstructive pulmonary disease: implications for dry powder inhalers. J Aerosol Med Pulm Drug Deliv. 2017;30(6):381–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kamps AW, Brand PL, Roorda RJ. Variation of peak inspiratory flow through dry powder inhalers in children with stable and unstable asthma. Pediatr Pulmonol. 2004;37(1):65–70. [DOI] [PubMed] [Google Scholar]
- 31. Hoppentocht M, Hagedoorn P, Frijlink HW, et al. Technological and practical challenges of dry powder inhalers and formulations. Adv Drug Deliv Rev. 2014;75:18–31. [DOI] [PubMed] [Google Scholar]
- 32. Dalby RN, Eicher J, Zierenberg B. Development of Respimat® Soft Mist™ Inhaler and its clinical utility in respiratory disorders. Med Devices (Auckl). 2011;4(1):145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Braido F. Failure in asthma control: reasons and consequences. Scientifica (Cairo). 2013;2013:549252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Boven JF, Ryan D, Eakin MN, et al. Enhancing respiratory medication adherence: the role of health care professionals and cost-effectiveness considerations. J Allergy Clin Immunol Pract. 2016;4(5):835–846. [DOI] [PubMed] [Google Scholar]
- 35. Horne R, Price D, Cleland J, et al. Can asthma control be improved by understanding the patient’s perspective? BMC Pulm Med. 2007;7:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thomas M. Why aren’t we doing better in asthma: time for personalised medicine? NPJ Prim Care Respir Med. 2015;25:15004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bender BG, Rand C. Medication non-adherence and asthma treatment cost. Curr Opin Allergy Clin Immunol. 2004;4(3):191–195. [DOI] [PubMed] [Google Scholar]
- 38. Côté I, Farris K, Feeny D. Is adherence to drug treatment correlated with health-related quality of life? Qual Life Res. 2003;12(6):621–633. [DOI] [PubMed] [Google Scholar]
- 39. Rand CS, Wise RA. Measuring adherence to asthma medication regimens. Am J Respir Crit Care Med. 1994;149(2 Pt 2):S69–76; discussion S77-68. [DOI] [PubMed] [Google Scholar]
- 40. Levy ML, Hardwell A, McKnight E, et al. Asthma patients’ inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the global initiative for asthma (GINA) strategy: a retrospective analysis. Prim Care Respir J. 2013;22(4):406–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sanchis J, Gich I, Pedersen S. Systematic review of errors in inhaler use: has patient technique improved over time? Chest. 2016;150(2):394–406. [DOI] [PubMed] [Google Scholar]
- 42. Molimard M, Raherison C, Lignot S, et al. Chronic obstructive pulmonary disease exacerbation and inhaler device handling: real-life assessment of 2935 patients. Eur Respir J. 2017;49(2):1601794. [DOI] [PubMed] [Google Scholar]
- 43. Al-Zahrani JM, Ahmad A, Al-Harbi A, et al. Factors associated with poor asthma control in the outpatient clinic setting. Ann Thorac Med. 2015;10(2):100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marques da Silva CCB, Teixeira RN, Freitas PD, et al. Influence of body mass index and sedentary lifestyle in clinical control and health related quality of life in moderate and severe asthmatics. Eur Respir J. 2014;44(suppl 58):P4285. [Google Scholar]
- 45. Ekerljung L, Sundblad BM, Rönmark E, et al. Incidence and prevalence of adult asthma is associated with low socio-economic status. Clin Respir J. 2010;4(3):147–156. [DOI] [PubMed] [Google Scholar]
- 46. Bacon SL, Bouchard A, Loucks EB, et al. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respir Res. 2009;10(1):125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cope SF, Ungar WJ, Glazier RH. Socioeconomic factors and asthma control in children. Pediatr Pulmonol. 2008;43(8):745–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Strömberg Celind F, Wennergren G, Vasileiadou S, et al. Higher parental education was associated with better asthma control. Acta Paediatr. 2019;108 (5):920–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Boulet LP. Influence of comorbid conditions on asthma. Eur Respir J. 2009;33(4):897–906. [DOI] [PubMed] [Google Scholar]
- 50. de Groot EP, Nijkamp A, Duiverman EJ, et al. Allergic rhinitis is associated with poor asthma control in children with asthma. Thorax. 2012;67(7):582–587. [DOI] [PubMed] [Google Scholar]
- 51. de Miguel Díez J, Hernández Barrera V, Puente Maestu L, et al. Psychiatric comorbidity in asthma patients. Associated factors. J Asthma. 2011;48(3):253–258. [DOI] [PubMed] [Google Scholar]
- 52. Mehuys E, Van Bortel L, De Bolle L, et al. Effectiveness of pharmacist intervention for asthma control improvement. Eur Respir J. 2008;31(4):790–799. [DOI] [PubMed] [Google Scholar]
- 53. National Governors Association. The expanding role of pharmacists in a transformed health care system. Published 2015. Accessed January 15, 2019 https://s3.amazonaws.com/cppa/system/rich/rich_files/rich_files/83/original/1501theexpandingroleofpharmacists.pdf
- 54. Manolakis PG, Skelton JB. Pharmacists’ contributions to primary care in the United States collaborating to address unmet patient care needs: the emerging role for pharmacists to address the shortage of primary care providers. Am J Pharm Educ. 2010;74(10):S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kelling SE, Rondon-Begazo A, DiPietro Mager NA, et al. Provision of clinical preventive services by community pharmacists. Prev Chronic Dis. 2016;13(10):e149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. National Heart, Lung, and Blood Institute. National asthma education and prevention program. Expert panel report 3: guidelines for the diagnosis and management of asthma, full report 2007. Published August 28, 2007. Accessed December 19, 2018 https://www.nhlbi.nih.gov/sites/default/files/media/docs/asthgdln_1.pdf
- 57. Benavides S, Rodriguez JC, Maniscalco-Feichtl M. Pharmacist involvement in improving asthma outcomes in various healthcare settings: 1997 to present. Ann Pharmacother. 2009;43(1):85–97. [DOI] [PubMed] [Google Scholar]
- 58. Williams MV, Baker DW, Honig EG, et al. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114(4):1008–1015. [DOI] [PubMed] [Google Scholar]
- 59. Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172(8):980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tzeng Y-F, Chiang B-L, Chen Y-H, et al. Health literacy in children with asthma: a systematic review. Pediatr Neonatol. 2018;59(5):429–438. [DOI] [PubMed] [Google Scholar]
- 61. Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax. 2004;59(2):94–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Asthma and Allergy Foundation of America. Asthma action plan. Published September 2015. Accessed December 19, 2018 https://www.aafa.org/asthma-treatment-action-plan/
- 63. Kouri A, Boulet LP, Kaplan A, et al. An evidence-based, point-of-care tool to guide completion of asthma action plans in practice. Eur Respir J. 2017;49(5):e1602238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. McLean W, Gillis J, Waller R. The BC community pharmacy asthma study: a study of clinical, economic and holistic outcomes influenced by an asthma care protocol provided by specially trained community pharmacists in British Columbia. Can Respir J. 2003;10(4):195–202. [DOI] [PubMed] [Google Scholar]
- 65. Price D, Bosnic-Anticevich S, Briggs A, et al. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respir Med. 2013;107(1):37–46. [DOI] [PubMed] [Google Scholar]
- 66. Basheti IA, Hamadi SA, Reddel HK. Inter-professional education unveiling significant association between asthma knowledge and inhaler technique. Pharm Pract (Granada). 2016;14(1):713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Basheti IA, Armour CL, Reddel HK, et al. Long-term maintenance of pharmacists’ inhaler technique demonstration skills. Am J Pharm Educ. 2009;73(2):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Basheti IA, Reddel HK, Armour CL, et al. Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir Care. 2005;50(5):617–623. [PubMed] [Google Scholar]
- 69. Murphy A. How to help patients optimise their inhaler technique. Pharm J. 2016;297(7891). doi:10.1211/PJ.2016.20201442 [Google Scholar]
- 70. Bosnic-Anticevich SZ, Sinha H, So S, et al. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47(3):251–256. [DOI] [PubMed] [Google Scholar]
- 71. Press VG, Arora VM, Shah LM, et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med. 2012;27(10):1317–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Müller T, Muller A, Hubel C, et al. Optimizing inhalation technique using web-based videos in obstructive lung diseases. Respir Med. 2017;129:140–144. [DOI] [PubMed] [Google Scholar]
- 73. American Lung Association. Asthma patient resources and videos. Updated May 13, 2020. Accessed May 15, 2020 https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/patient-resources-and-videos/
- 74. How to use inhalers: interactive guidance and management. Accessed May 15, 2020 https://use-inhalers.com/
- 75. Sears MR. Safety of long-acting beta-agonists: are new data really required? Chest. 2009;136(2):604–607. [DOI] [PubMed] [Google Scholar]
- 76. Crespo-Gonzalez C, Fernandez-Llimos F, Rotta I, et al. Characterization of pharmacists’ interventions in asthma management: a systematic review. J Am Pharm Assoc. 2018;58(2):210–219. [DOI] [PubMed] [Google Scholar]
- 77. Gamble J, Stevenson M, Heaney LG. A study of a multi-level intervention to improve non-adherence in difficult to control asthma. Respir Med. 2011;105(9):1308–1315. [DOI] [PubMed] [Google Scholar]
- 78. Caress AL, Beaver K, Luker K, et al. Involvement in treatment decisions: what do adults with asthma want and what do they get? Results of a cross sectional survey. Thorax. 2005;60(3):199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kew KM, Malik P, Aniruddhan K, et al. Shared decision-making for people with asthma. Cochrane Database Syst Rev. 2017;10(10):CD012330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kanchongkittiphon W, Mendell MJ, Gaffin JM, et al. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the institute of medicine. Environ Health Perspect. 2015;123(1):6–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Centers for Disease Control and Prevention. Learn how to control asthma. Updated September 6, 2019. Accessed May 15, 2020 https://www.cdc.gov/asthma/faqs.htm
- 82. Gautier C, Charpin D. Environmental triggers and avoidance in the management of asthma. J Asthma Allergy. 2017;10:47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Lazarus SC, Chinchilli VM, Rollings NJ, et al. Smoking affects response to inhaled corticosteroids or leukotriene receptor antagonists in asthma. Am J Respir Crit Care Med. 2007;175(8):783–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Maricoto T, Monteiro L, Gama JMR, et al. Inhaler technique education and exacerbation risk in older adults with asthma or chronic obstructive pulmonary disease: a meta-analysis. J Am Geriatr Soc. 2019;67(1):57–66. [DOI] [PubMed] [Google Scholar]
- 85. Dokbua S, Dilokthornsakul P, Chaiyakunapruk N, et al. Effects of an asthma self-management support service provided by community pharmacists: a systematic review and meta-analysis. J Manag Care Spec Pharm. 2018;24(11):1184–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Manfrin A, Tinelli M, Thomas T, et al. A cluster randomised control trial to evaluate the effectiveness and cost-effectiveness of the Italian medicines use review (I-MUR) for asthma patients. BMC Health Serv Res. 2017;17(1):300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Schulz M, Verheyen F, Mühlig S, et al. Pharmaceutical care services for asthma patients: a controlled intervention study. J Clin Pharmacol. 2001;41(6):668–676. [DOI] [PubMed] [Google Scholar]
- 88. Saini B, Krass I, Armour C. Development, implementation, and evaluation of a community pharmacy-based asthma care model. Ann Pharmacother. 2004;38(11):1954–1960. [DOI] [PubMed] [Google Scholar]
- 89. Berry TM, Prosser TR, Wilson K, et al. Asthma friendly pharmacies: a model to improve communication and collaboration among pharmacists, patients, and healthcare providers. J Urban Health. 2011;88(suppl 1):113–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Stergachis A, Gardner JS, Anderson MT, et al. Improving pediatric asthma outcomes in the community setting: does pharmaceutical care make a difference? J Am Pharm Assoc. 2002;42(5):743–752. [DOI] [PubMed] [Google Scholar]
- 91. Knoell DL, Pierson JF, Marsh CB, et al. Measurement of outcomes in adults receiving pharmaceutical care in a comprehensive asthma outpatient clinic. Pharmacotherapy. 1998;18(6):1365–1374. [PubMed] [Google Scholar]
- 92. González-Martin G, Joo I, Sanchez I. Evaluation of the impact of a pharmaceutical care program in children with asthma. Patient Educ Couns. 2003;49(1):13–18. [DOI] [PubMed] [Google Scholar]
- 93. Diamond SA, Chapman KR. The impact of a nationally coordinated pharmacy-based asthma education intervention. Can Respir J. 2001;8(4):261–265. [DOI] [PubMed] [Google Scholar]
- 94. Hohner E, Ortmann M, Murtaza U, et al. Implementation of an emergency department-based clinical pharmacist transitions-of-care program. Am J Health Syst Pharm. 2016;73(15):1180–1187. [DOI] [PubMed] [Google Scholar]
- 95. Hatoun J, Bair-Merritt M, Cabral H, et al. Increasing medication possession at discharge for patients with asthma: the meds-in-hand project. Pediatrics. 2016;137(3):e20150461. [DOI] [PubMed] [Google Scholar]
- 96. Littauer SL, Dixon DL, Mishra VK, et al. Pharmacists providing care in the outpatient setting through telemedicine models: a narrative review. Pharm Pract (Granada). 2017;15(4):1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm. 2018;14(8):707–717. [DOI] [PubMed] [Google Scholar]
- 98. Brown W, Scott D, Friesner D, et al. Impact of telepharmacy services as a way to increase access to asthma care. J Asthma. 2017;54(9):961–967. [DOI] [PubMed] [Google Scholar]
- 99. Harkins M, Raissy H, Moseley K, et al. Project ECHO: improving asthma care in New Mexico with telehealth technology. Chest. 2011;140(4):861A. [Google Scholar]
- 100. Basheti IA, Obeidat NM, Reddel HK. Effect of novel inhaler technique reminder labels on the retention of inhaler technique skills in asthma: a single-blind randomized controlled trial. NPJ Prim Care Respir Med. 2017;27(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Almomani BA, Mokhemer E, Al-Sawalha NA, et al. A novel approach of using educational pharmaceutical pictogram for improving inhaler techniques in patients with asthma. Respir Med. 2018;143:103–108. [DOI] [PubMed] [Google Scholar]
- 102. Campbell JD. Implications for asthma treatment strategies in managed care. Am J Manag Care. 2017; 23:S12–S19. [Google Scholar]
- 103. National Institute for Health and Care Excellence. Asthma: diagnosis, monitoring and chronic asthma management. Published November 29, 2017. Accessed May 15, 2020 https://www.nice.org.uk/guidance/ng80 [PubMed]
- 104. National Asthma Educator Certification Board. Accessed May 15, 2020 https://naecb.com/about-naecb/
- 105. Abraham TG, Huggins C, Diaz-Fuentes G, et al. Combining pharmacy expertise with asthma educator certification: assessing the impact on inner-city asthma patients. J Asthma. 2019;56(8):891–896. [DOI] [PubMed] [Google Scholar]