Abstract
Background
Several randomized clinical trials have shown that non-invasive ventilation (NIV) applied immediately after extubation may prevent reintubation in patients at high-risk of extubation failure. However, most of studies included patients with chronic respiratory disorders as well as patients without underlying respiratory disease. To date, no study has shown decreased risk of reintubation with prophylactic NIV after extubation among patients with chronic obstructive pulmonary disease (COPD). We hypothesized that prophylactic NIV after extubation may decrease the risk of reintubation in COPD patients as compared with high-flow nasal oxygen. We performed a post hoc subgroup analysis of COPD patients included in a multicenter, randomized, controlled trial comparing prophylactic use of NIV alternating with high-flow nasal oxygen versus high-flow nasal oxygen alone immediately after extubation.
Results
Among the 651 patients included in the original study, 150 (23%) had underlying COPD including 86 patients treated with NIV alternating with high-flow nasal oxygen and 64 patients treated with high-flow nasal oxygen alone. The reintubation rate was 13% (11 out of 86 patients) with NIV and 27% (17 out of 64 patients) with high-flow nasal oxygen alone [difference, − 14% (95% CI − 27% to − 1%); p = 0.03]. Whereas reintubation rates were significantly lower with NIV than with high-flow nasal oxygen alone at 72 h and until ICU discharge, mortality in ICU did not differ between groups: 6% (5/86) with NIV vs. 9% (6/64) with high-flow nasal oxygen alone [difference − 4% (95% CI − 14% to 5%); p = 0.40].
Conclusions
In COPD patients, prophylactic NIV alternating with high-flow nasal oxygen significantly decreased the risk of reintubation compared with high-flow nasal oxygen alone.
Trial registration The study was registered at http://www.clinicaltrials.gov with the trial registration number NCT03121482 (20 April 2017)
Keywords: Airway extubation, Weaning, Non-invasive ventilation, High-flow nasal oxygen, Chronic obstructive pulmonary disease
Background
In intensive care units (ICUs), extubation failure rates leading to reintubation approximate 20–30% in patients with chronic respiratory disorders [1–7]. Several randomized clinical trials have shown that non-invasive ventilation (NIV) applied immediately after extubation may prevent reintubation in patients at high-risk of extubation failure [2, 7]. However, the patients in these studies considered at high-risk have been heterogeneous and included patients with chronic respiratory disorders as well as patients without underlying respiratory disease. Whether prophylactic application of NIV after extubation reduces reintubation rate in patients with chronic obstructive pulmonary disease (COPD) has been poorly assessed. Previous clinical trials have shown that NIV could be particularly effective to prevent post-extubation respiratory failure in patients with chronic respiratory disorders, but again, these studies did not specifically focus on COPD patients and showed beneficial effects of NIV only in hypercapnic patients [3, 4]. To date, only one small-scale trial has compared NIV with standard oxygen exclusively in COPD patients, and this study failed to highlight the beneficial effects of NIV [8]. Conversely, high-flow nasal oxygen could be as effective as NIV in preventing reintubation in patients at high-risk [9]. Therefore, we performed a post hoc subgroup analysis of a recent large-scale randomized controlled trial showing that prophylactic NIV alternating with high-flow nasal oxygen significantly reduced the risk of reintubation as compared to high-flow nasal oxygen alone in a heterogeneous population of patients at high-risk of extubation failure [7].
We hypothesized that prophylactic NIV alternating with high-flow nasal oxygen after extubation may be particularly effective in COPD patients and may decrease the risk of reintubation in this subgroup of patients as compared with high-flow nasal oxygen alone.
Methods
Study design and patients
The present study is a post hoc analysis of a multicenter, randomized, controlled trial comparing prophylactic use of NIV alternating with high-flow nasal oxygen versus high-flow nasal oxygen alone immediately after extubation in 641 patients at high-risk of reintubation in ICUs [7]. The present analysis focused on the subset population of COPD patients. Underlying COPD could be either documented by spirometry or highly suspected by physician team. Patients who were considered as having underlying COPD without previous spirometry needed to have been intubated for acute hypercapnic respiratory failure and for no other reason, and to have a history of smoking with dynamic hyperinflation during mechanical ventilation and/or emphysema on chest X-ray or scanner. Patients with long-term treatment with NIV or continuous positive airway pressure at home for sleep obstructive apnea syndrome were excluded. The original study was approved by the central ethics committee (Ethics Committee Ouest III, Poitiers, France) with registration number 2016-A01078-43. Written informed consent was obtained from all patients or next of kin before inclusion. According to French law, this post hoc analysis did not require further ethics approval.
Treatment groups
All patients were extubated after successful spontaneous breathing trial and received prophylactic NIV alternating with high-flow nasal oxygen or high-flow nasal oxygen alone during the first 48 h following extubation. In the two groups, treatment could be continued beyond the first 48 h following extubation until complete recovery of respiratory status. Patients assigned to the control group were continuously treated by high-flow nasal oxygen alone with a flow of 50 L/min and fraction of inspired oxygen (FiO2) adjusted to obtain adequate oxygenation, with a pulse oximetry (SpO2) at least 92%. Patients assigned to the interventional group were treated by NIV alternating with high-flow nasal oxygen. Non-invasive ventilation was initiated immediately after extubation with a first session of at least 4 h and minimal duration of at least 12 h a day during the 48 h following extubation. NIV was carried out with an ICU ventilator with NIV mode or dedicated bi-level ventilator, in pressure-support mode with a minimal pressure-support level of 5 cm H2O targeting a tidal volume around 6–8 ml/kg of predicted body weight, a positive end-expiratory pressure level between 5 and 10 cmH2O and a FiO2 adjusted to obtain adequate oxygenation (SpO2 ≥ 92%). Between non-invasive ventilation sessions, high-flow nasal oxygen was delivered as in the control group.
Outcomes
The main outcome was reintubation rates within the 7 days following extubation according to oxygenation strategy. Secondary outcomes included post-extubation respiratory failure within the 7 days following extubation, reintubation rates at 48 h, 72 h and up until ICU discharge, and mortality in ICU.
Severe respiratory failure leading to reintubation was defined by the presence of at least two criteria among the following: respiratory rate > 35 breaths per minute, clinical signs of respiratory distress, respiratory acidosis defined as pH < 7.25 units and PaCO2 > 45 mm Hg, hypoxemia defined as FiO2 ≥ 80% to maintain SpO2 ≥ 92% or a PaO2/FiO2 ≤ 100 mm Hg.
An episode of post-extubation respiratory failure was defined by the presence of at least two criteria among the following: respiratory rate > 25 breaths per minute, clinical signs of respiratory distress, respiratory acidosis defined as pH < 7.35 units and PaCO2 > 45 mm Hg, and hypoxemia defined as FiO2 ≥ 50% to maintain SpO2 ≥ 92% or a PaO2/FiO2 ≤ 150 mm Hg.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) or median [interquartile range, 25–75th percentiles], and qualitative variables were expressed as number and percentage. Patients’ characteristics were compared between the NIV group and the high-flow nasal oxygen group by means of the χ2 tests or Fisher exact test for categorical variables and Student’s t-test or Wilcoxon rank-sum test for continuous variables as appropriate. Primary and secondary outcomes were compared between the two groups by means of the χ2 test. Kaplan–Meier curves were plotted to assess the time from extubation to reintubation and were compared by means of the log-rank test at day 7. The results were presented as odds ratio (OR) with 95% confidence interval (95 CI). A two-tailed p value of less than 0.05 was considered statistically significant. We used SAS software, version 9.4 (SAS Institute), for all the analyses.
Results
Among the 651 patients extubated in the 30 participating ICUs, 150 (23%) had underlying COPD including 102 patients (68%) with COPD confirmed by spirometry. Median forced expiratory volume during the first second (FEV1) was 58% [interquartile range, 42–71%] expressed in percentage of predicted value according to sex and age. Among the 86 patients in whom FEV1 was available, 44% (38 of 86 patients) had severe COPD (stage 3 or 4 according to the Gold classification, i.e., FEV1 < 50% of predicted value).
In overall population, the main reason for intubation at admission was acute respiratory failure in 102 patients (68%), with as main diagnosis bacterial pneumonia in 35% of cases (n = 36), severe acute exacerbation without identified diagnosis in 33% (n = 34), viral pneumonia in 14% (n = 14), cardiogenic pulmonary edema in 11% (n = 11), and another reason in 7% (pulmonary embolism, pneumothorax, pleural effusion, hemoptysis, airway obstruction, and aspiration). Among the 102 patients intubated for acute respiratory failure, 36% (n = 37) had been intubated prior to ICU admission.
Of the 150 COPD patients, weaning was considered as simple in 102 patients (68%), difficult in 44 (29%), and prolonged in 4 (3%). At time of extubation, 53 patients (35%) had hypercapnia (PaCO2 > 45 mm Hg). After extubation, 86 patients were treated with prophylactic NIV alternating with high-flow nasal oxygen and 64 with high-flow nasal oxygen alone. The characteristics of the patients at inclusion were similar in the two groups aside from a higher proportion of patients with ineffective cough in the NIV group (Table 1).
Table 1.
Baseline patient characteristics according to the oxygenation strategy used after extubation
| High-flow nasal oxygen alone (n = 64) | Non-invasive ventilation (n = 86) | p value | |
|---|---|---|---|
| Characteristics of the patients at admission | |||
| Age, years | 66 ± 9 | 66 ± 9 | 0.900 |
| Male sex, n (%) | 48 (75%) | 61 (71%) | 0.580 |
| Body mass index (BMI), kg/m2 | 27 ± 6 | 27 ± 7 | 0.875 |
| Obesity (BMI ≥ 30 kg/m2), n (%) | 14 (22%) | 25 (29%) | 0.326 |
| COPD confirmed by spirometry, n (%) | 43 (67%) | 53 (62%) | 0.483 |
| FEV1, % of predicted value | 58 ± 18 | 57 ± 17 | 0.834 |
| Underlying chronic cardiac disease, n (%) | 14 (22%) | 28 (33%) | 0.149 |
| Ischemic heart disease | 9 (14%) | 15 (17%) | 0.577 |
| Atrial fibrillation | 4 (6%) | 9 (10%) | 0.364 |
| Left ventricular dysfunction | 5 (8%) | 7 (8%) | 0.942 |
| SAPS II at admission, points | 53 ± 17 | 52 ± 18 | 0.874 |
| Main reason for intubation, n (%) | |||
| Acute respiratory failure | 43 (67%) | 59 (69%) | 0.099 |
| Coma | 6 (9%) | 10 (12%) | |
| Shock | 9 (14%) | 3 (3%) | |
| Cardiac arrest | 4 (6%) | 4 (5%) | |
| Surgery | 2 (3%) | 9 (10%) | |
| Other reasons | 0 (0%) | 1 (1%) | |
| Characteristics of the patients on the day of extubation | |||
| SOFA score, points | 4.0 ± 2.5 | 3.8 ± 2.0 | 0.639 |
| Median duration of mechanical ventilation, days | 5.5 [3.0–10.5] | 6.5 [3.0–13.0] | 0.504 |
| Difficult or prolonged weaning#, n (%) | 20 (33%) | 28 (32%) | 0.865 |
| Ineffective cough, n/n total (%) | 7/59 (12%) | 26/82 (32%) | 0.006 |
| Abundant secretions, n/n total (%) | 31/60 (52%) | 37/83 (45%) | 0.402 |
| Administration of steroids before extubation, n (%) | 12 (19%) | 20 (23%) | 0.505 |
| Ventilator settings before the spontaneous breathing trial (SBT) | |||
| Pressure support ventilation, n (%) | 58 (91%) | 75 (87%) | 0.514 |
| Pressure support level, cm H2O | 9.6 ± 2.5 | 9.6 ± 3.0 | 0.997 |
| Positive end-expiratory pressure, cm H2O | 5.6 ± 1.7 | 6.0 ± 1.7 | 0.225 |
| Tidal volume, ml/kg | 7.8 ± 2.2 | 7.9 ± 2.4 | 0.687 |
| Respiratory rate, breaths/min | 23 ± 7 | 22 ± 6 | 0.767 |
| FiO2, % | 34 ± 8 | 37 ± 13 | 0.228 |
| PaO2/FiO2, mm Hg | 248 ± 70 | 247 ± 87 | 0.916 |
| pH, units | 7.45 ± 0.05 | 7.44 ± 0.05 | 0.529 |
| PaCO2, mm Hg | 44 ± 9 | 43 ± 8 | 0.373 |
| PaCO2 > 45 mm Hg, n (%) | 26 (41%) | 30 (35%) | 0.542 |
| Characteristics of the spontaneous breathing trial (SBT) | |||
| Type of SBT, n (%) | 0.807 | ||
| T-piece, n (%) | 37 (58%) | 48 (56%) | – |
| Low level of pressure-support ventilation, n (%) | 27 (42%) | 38 (44%) | – |
| Median duration of the SBT, min | 60 [30–62] | 60 [30–60] | 0.432 |
| Respiratory rate at the end of SBT, breaths/min | 24 ± 7 | 24 ± 6 | 0.782 |
| PaO2 at the end of SBT, mm Hg (n = 109) | 78 ± 18 | 79 ± 22 | 0.735 |
| pH at the end of SBT, units (n = 109) | 7.45 ± 0.05 | 7.46 ± 0.05 | 0.586 |
| PaCO2 at the end of SBT, mm Hg (n = 109) | 44 ± 10 | 42 ± 9 | 0.398 |
| Hypercapnia at time of extubation‡, n (%) | 22 (34%) | 31 (36%) | 0.832 |
Italic means that there is a significant difference (p < 0.05)
Continuous variables are given in mean ± standard deviation or median [interquartile range, IQR 25–75th percentiles] according to their distribution
COPD chronic obstructive pulmonary disease, FEV1 forced expiratory volume during the first second (expressed in % of predicted value according to sex and age), SAPS Simplified Acute Physiology Score, SOFA Sepsis-Related Organ Failure Assessment, SBT Spontaneous Breathing Trial
#Difficult or prolonged weaning refer to patient who failed the first spontaneous breathing trial and were not extubated the day of the first trial
‡Hypercapnia (defined as PaCO2 > 45 mm Hg) was assessed according to the PaCO2 level measured at the end of the spontaneous breathing trial (109 patients) or at the end of or under mechanical ventilation before the trial if this latter was not measured (41 patients)
Ventilator settings using NIV were the following: pressure-support level of 7.9 ± 2.4 cm H2O, PEEP level of 5.2 ± 1.3 cm H2O, and FiO2 of 0.34 ± 0.9, resulting in a tidal volume of 8.8 ± 3.6 ml per kilogram of predicted body weight. Patients treated with high-flow nasal oxygen alone received a gas flow rate of 50 ± 3 L/min with FiO2 of 0.42 ± 0.13. NIV was delivered for a median of 14 h [interquartile range, 10–16] within the first 24 h following extubation and for 23 h [interquartile range, 14–29] within the first 48 h. In the NIV group, NIV was continued beyond the first 48 h for incomplete recovery of respiratory status in 28 patients (33%) whereas in the high-flow nasal oxygen group, high-flow nasal oxygen was continued in 26 patients (41%) (difference − 8%; 95 CI, − 23% to 7%; p = 0.309).
Outcomes
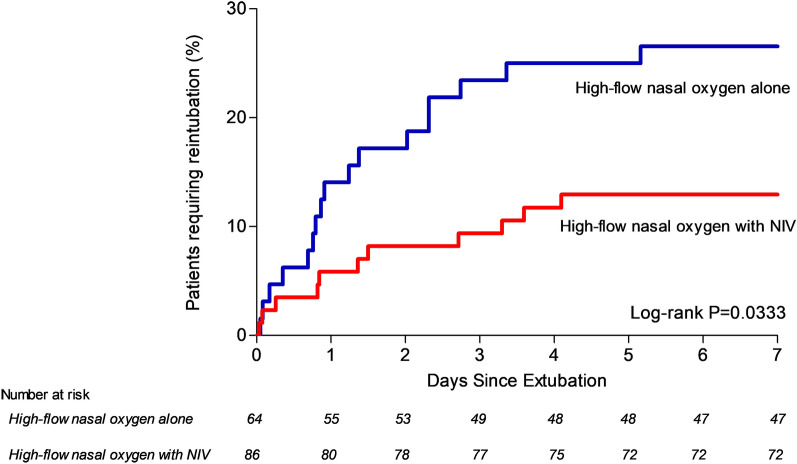
The reintubation rate at day 7 was 13% (11 out of 86 patients) with NIV and 27% (17 out of 64 patients) with high-flow nasal oxygen alone [difference − 14% (95% CI − 27% to − 1%); p = 0.03] (Fig. 1). Reintubation rates were significantly lower with NIV than with high-flow nasal oxygen alone at 72 h and until ICU discharge (Table 2).
Fig. 1.
Kaplan–Meier analysis of time from extubation to reintubation according to oxygenation strategy. Reintubation rates were significantly lower in patients treated with non-invasive ventilation (red bars) than in those treated with high-flow nasal oxygen alone (blue bars). The reintubation rate within the 7 days following extubation was 13% (11 out of 86 patients) with NIV and 27% (17 out of 64 patients) with high-flow nasal oxygen alone [difference, − 14% (95% CI − 27% to − 1%); p = 0.033 using log-rank test]
Table 2.
Primary and secondary outcomes
| Non-invasive ventilation (n = 86) | High-flow nasal oxygen alone (n = 64) | Absolute difference % (95% CI) | p value | |
|---|---|---|---|---|
| Primary outcome | ||||
| Reintubation at day 7, n (%) | 11 (13%) | 17 (27%) | − 14 (− 27 to − 1) | 0.032 |
| Secondary outcomes | ||||
| Post-extubation respiratory failure, n (%) | 22 (26%) | 23 (36%) | − 10 (− 25 to 4) | 0.171 |
| Use of NIV to treat post-extubation respiratory failure, n (%) | 19/22 (86%) | 6/23 (26%) | 60 (32 to 76) | < 0.001 |
| Reintubation at day 7 among patients with post-extubation respiratory failure, n (%) | 10/22 (45%) | 14/23 (61%) | − 15 (− 40 to 13) | 0.300 |
| Reintubation at 48 h, n (%) | 7 (8%) | 11 (17%) | − 9 (− 21 to 2) | 0.092 |
| Reintubation at 72 h, n (%) | 8 (9%) | 15 (23%) | − 14 (− 27 to − 2) | 0.018 |
| Reintubation in ICU, n (%) | 11 (13%) | 18 (28%) | − 15 (− 28 to − 2) | 0.019 |
| Length of stay in ICU, median (IQR), days | 13 [8–21] | 12 [8-19] | – | 0.908 |
| Length of stay in hospital, median (IQR), days | 26 [14–47] | 23 [16–32] | – | 0.406 |
| Mortality in ICU, n (%) | 5 (6%) | 6 (9%) | − 4 (− 14 to 5) | 0.408 |
| Mortality in hospital, n (%) | 15 (17%) | 8 (12%) | 5 (− 7 to 16) | 0.406 |
Italic means that there is a significant difference (p < 0.05)
NIV non-invasive ventilation, CI confidence interval, ICU intensive care unit, IQR interquartile range (25–75th percentiles)
The proportion of patients with post-extubation respiratory failure did not significantly differ between groups. The proportion of patients who received NIV to treat post-extubation respiratory failure was 86% (19 of 22 patients) in the NIV group and 26% (6 of 23 patients) in the high-flow oxygen group [difference 60% (95% CI 32–76%); p < 0.001]. However, the proportion of patients reintubated among those who experienced post-extubation respiratory failure did not significantly differ between the 2 groups.
Mortality in ICU did not differ between groups: 6% (5/86) with NIV vs. 9% (6/64) with high-flow nasal oxygen alone [difference − 4% (95% CI − 14% to 5%); p = 0.40].
Discussion
In this post hoc analysis of a randomized controlled trial focusing on COPD patients, prophylactic use of NIV alternating with high-flow nasal oxygen immediately after extubation significantly decreased the rate of reintubation as compared with high-flow nasal oxygen alone.
This trial is the largest one reporting the effects of prophylactic NIV after extubation in COPD patients. Previously, only one small-scale trial comparing NIV with standard oxygen exclusively in COPD patients failed to highlight the beneficial effects of NIV [8]. Another clinical trial showing decreased risk of post-extubation respiratory failure in patients with chronic respiratory disorders treated with NIV included a majority of COPD patients (74 of 106 patients) [4]. However, the risk of reintubation was not significantly lower with NIV than with standard oxygen and all patients had hypercapnia at time of extubation. Here, we report for the first time decreased risk of reintubation in COPD patients treated with prophylactic NIV after extubation.
Limitations
The main limitation of this study is the post hoc nature of the analysis. However, characteristics of the patients were similar between the 2 groups and the reintubation rates observed are very close to reintubation rates reported in previous studies (around 10% with NIV and between 20 and 30% with standard oxygen) reinforcing external validity [5, 7–9]. The only imbalance between groups was a higher proportion of patients with ineffective cough in the NIV group, situation associated with an increased risk of extubation failure [10, 11]. Despite this unfavorable imbalance, prophylactic NIV was associated with a decreased risk of reintubation. This is in keeping with a previous study reporting that NIV may avoid reintubation in patients with weak cough as compared with standard oxygen [12].
Another major limitation is that more than one-third of patients had suspected but not confirmed COPD using spirometry. These patients were admitted for their first acute exacerbation of COPD or never underwent pulmonary function tests planned after hospital discharge, as is often the case. Indeed, several studies have reported the difficulty for follow-up of these patients and their reluctance to come back for pulmonary explorations after hospital discharge [13, 14]. However, all these patients were admitted for acute hypercapnic respiratory failure and had common risk factors of COPD. Consequently, it is likely that the majority of patients with suspected obstructive spirometric pattern actually had underlying COPD.
Although NIV was the one additional treatment in the interventional group, the decreased risk of reintubation observed in the NIV group might be due to the combination of NIV with high-flow nasal oxygen between NIV sessions. Although the beneficial effects of NIV on oxygenation, alveolar ventilation, and work of breathing are well-demonstrated [15, 16], continuation of high-flow nasal oxygen between NIV sessions may provide further clinical improvement by decreasing work of breathing [17, 18]. Whereas prophylactic NIV could be strongly recommended in patients at high-risk of extubation failure and especially in COPD patients, whether NIV alternating with high-flow nasal oxygen is a better oxygenation strategy than NIV alternating with standard oxygen is a question that requires further investigation.
Lastly, the proportion of patients who experienced post-extubation respiratory failure as well as the proportion of patients reintubated among those with respiratory failure did not significantly differ. However, both rates were reduced, resulting in a significant decreased risk of reintubation with NIV as compared with high-flow nasal oxygen alone. Patients receiving prophylactic NIV were more likely to be treated with NIV in case of post-extubation respiratory failure than those receiving high-flow nasal oxygen alone. As a result, NIV may prevent post-extubation respiratory failure and subsequently avoid reintubation among patients with respiratory failure. Even though the most recent international clinical practice guidelines suggest that NIV should not be used in the treatment of patients with established post-extubation respiratory failure [19], NIV as rescue therapy may avoid reintubation in a number of cases, especially in patients with chronic obstructive pulmonary disease [3–5, 20].
Clinical implications
Several studies have suggested that prophylactic NIV after extubation may be particularly effective in hypercapnic patients [3, 4, 7]. However, less than 40% of patients included in our study had hypercapnia, and the majority of patients had moderate underlying COPD with a mean forced expiratory volume during the first second (FEV1) above 50% of predicted value. It should be emphasized that patients had not necessarily been intubated for acute exacerbation of COPD and that nearly one-third of them had been intubated for another reason than acute respiratory failure (cardiac arrest, shock, coma, or surgery). Prophylactic NIV may decrease the risk of reintubation even in patients with mild or moderate COPD and regardless of the level of PCO2 before extubation, and thereby, NIV should be applied in all COPD patients to prevent extubation failure in the ICU.
Conclusion
Prophylactic use of NIV alternating with high-flow nasal oxygen immediately after extubation of COPD patients was associated with decreased risk of reintubation compared with high-flow nasal oxygen alone.
Acknowledgements
We thank Jeffrey Arsham (CHU de Poitiers, Poitiers, France) for reviewing and editing the original English-language manuscript.
Collaborators list to be indexed in PubMed
Florence Boissier (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Maeva Rodriguez (Centre Hospitalier Universitaire de Poitiers, Faustine Reynaud (Centre Hospitalier Universitaire de Poitiers, Delphine Chatellier (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Céline Deletage (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Carole Guignon (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Florent Joly (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Anne Veinstein (Centre Hospitalier Universitaire de Poitiers, Médecine Intensive Réanimation, Poitiers), Dalila Benzekri-Lefevre (Groupe Hospitalier Régional d’Orléans, Médecine Intensive Réanimation, Orléans), Thierry Boulain (Groupe Hospitalier Régional d’Orléans, Médecine Intensive Réanimation, Orléans), Grégoire Muller (Groupe Hospitalier Régional d’Orléans, Médecine Intensive Réanimation, Orléans), Yves Le Tulzo (Centre Hospitalier Universitaire de Rennes, Hôpital Ponchaillou, Service des Maladies Infectieuses et Réanimation Médicale, Rennes), Jean-Marc Tadié (Centre Hospitalier Universitaire de Rennes, Hôpital Ponchaillou, Service des Maladies Infectieuses et Réanimation Médicale, Rennes), Adel Maamar (Centre Hospitalier Universitaire de Rennes, Hôpital Ponchaillou, Service des Maladies Infectieuses et Réanimation Médicale, Rennes), Suela Demiri (Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Pneumologie et Réanimation Médicale, AP-HP, Paris), Julien Mayaux (Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Pneumologie et Réanimation Médicale, Paris), Alexandre Demoule (Groupe Hospitalier Pitié-Salpêtrière Charles Foix, Service de Pneumologie et Réanimation Médicale, Paris), Lila Bouadma (Hôpital Bichat—Claude Bernard, Médecine Intensive Réanimation, Paris), Claire Dupuis (Hôpital Bichat—Claude Bernard, Médecine Intensive Réanimation, Paris), Pierre Asfar (Centre Hospitalier Universitaire d’Angers, Département de Médecine Intensive Réanimation, Angers), Marc Pierrot (Centre Hospitalier Universitaire d’Angers, Département de Médecine Intensive Réanimation, Angers), Gaëtan Béduneau (Centre Hospitalier Universitaire de Rouen, Hôpital Charles Nicolle, Département de Réanimation Médicale, Rouen), Déborah Boyer (Centre Hospitalier Universitaire de Rouen, Hôpital Charles Nicolle, Département de Réanimation Médicale, Rouen), Benjamin Delmas (Centre Hospitalier Universitaire Félix Guyon, Service de Réanimation Polyvalente, Saint Denis de la Réunion), Bérénice Puech (Centre Hospitalier Universitaire Félix Guyon, Service de Réanimation Polyvalente, Saint Denis de la Réunion), Konstantinos Bachoumas (Centre Hospitalier Universitaire de Clermont-Ferrand, Hôpital Gabriel Montpied, Clermont-Ferrand), Edouard Soum (Centre Hospitalier Universitaire de Clermont-Ferrand, Hôpital Gabriel Montpied, Clermont-Ferrand), Séverin Cabasson (Centre Hospitalier de La Rochelle, Service de Réanimation, La Rochelle), Marie-Anne Hoppe (Centre Hospitalier de La Rochelle, Service de Réanimation, La Rochelle), Saad Nseir (Centre Hospitalier Universitaire de Lille, Center de Réanimation, Lille), Olivier Pouly (Centre Hospitalier Universitaire de Lille, Center de Réanimation, Lille), Gaël Bourdin (Hôpital Saint-Joseph Saint-Luc, Réanimation Polyvalente, Lyon), Sylvène Rosselli (Hôpital Saint-Joseph Saint-Luc, Réanimation Polyvalente, Lyon), Anthony Le Meur (Centre Hospitalier Universitaire de Nantes, Médecine Intensive Réanimation, Nantes), Charlotte Garret (Centre Hospitalier Universitaire de Nantes, Médecine Intensive Réanimation, Nantes), Maelle Martin (Centre Hospitalier Universitaire de Nantes, Médecine Intensive Réanimation, Nantes), Guillaume Berquier (Hôpital Louis Mourier, Réanimation Médico-Chirurgicale, Colombes), Abirami Thiagarajah (Hôpital Louis Mourier, Réanimation Médico-Chirurgicale, Colombes), Guillaume Carteaux (Hôpitaux Universitaires Henri Mondor, Service de Réanimation Médicale, Créteil), Armand Mekontso-Dessap (Hôpitaux Universitaires Henri Mondor, Service de Réanimation Médicale, Créteil), Antoine Poidevin (Groupe Hospitalier Régional Mulhouse Sud Alsace, site Emile Muller, Service de Réanimation Médicale, Mulhouse), Anne-Florence Dureau (Groupe Hospitalier Régional Mulhouse Sud Alsace, site Emile Muller, Service de Réanimation Médicale, Mulhouse), Marie-Ange Azais (Centre Hospitalier Départemental de Vendée, Service de Médecine Intensive Réanimation, La Roche Sur Yon), Gwenhaël Colin (Centre Hospitalier Départemental de Vendée, Service de Médecine Intensive Réanimation, La Roche Sur Yon), Emmanuelle Mercier (Centre Hospitalier Régional Universitaire de Tours, Médecine Intensive Réanimation, Tours), Marlène Morisseau (Centre Hospitalier Régional Universitaire de Tours, Médecine Intensive Réanimation, Tours), Caroline Sabatier (Centre Hospitalier de Pau, Service de Réanimation, Pau), Walter Picard (Centre Hospitalier de Pau, Service de Réanimation, Pau), Marc Gainnier (CHU La Timone 2, Médecine Intensive Réanimation, Marseille), Thi-My-Hue Nguyen (Centre Hospitalier Henri Mondor d’Aurillac, Service de Réanimation, Aurillac), Gwenaël Prat (Centre Hospitalier Universitaire de Brest, Médecine Intensive Réanimation, Brest), Carole Schwebel (Centre Hospitalier Universitaire Grenoble Alpes, Médecine Intensive Réanimation, Grenoble), Matthieu Buscot (Centre Hospitalier Universitaire de Nice, Réanimation Médicale Archet 1, Université Cote d’Azur, Nice).
Authors’ contributions
Pr. AWT had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. AWT designed the study and wrote the manuscript. SR provided substantial contributions to the conception and design of the study, and performed statistical analysis. All authors contributed to drafting of the work, revising it critically for important intellectual content and approved the final version of the manuscript. All authors give their agreement to be accountable for all aspects of the work, and ensure the accuracy and integrity of any part of the work. All authors read and approved the final manuscript.
Funding
The study was conducted with the support of the “Programme Hospitalier de Recherche Clinique National 2015” from the French Ministry of Health (Grant Number 15-0060). The firm Fisher & Paykel provided to all the participating centers the high-flow nasal oxygen equipment and masks for non-invasive ventilation, but has no other involvement in the study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study has been approved by the central ethics committee (Ethics Committee Ouest III, Poitiers, France) with the registration number 2016-A01078-43 (06 September 2016).
Consent for publication
Written informed consent was obtained from all patients or next of kin before inclusion. According to French law, this post hoc analysis did not require further ethics approval.
Competing interests
Dr Thille reported receiving grants from the French Ministry of Health and personal fees and nonfinancial support from Fisher & Paykel Healthcare during the conduct of the study and personal fees from Maquet-Getinge, GE Healthcare, and Covidien outside the submitted work. Dr Sonneville reported receiving grants from the French Ministry of Health, the European Society of Intensive Care Medicine, and the French Society of Intensive Care Medicine and personal fees from Baxter outside the submitted work. Dr Beloncle reported receiving personal fees from Lowenstein Medical and nonfinancial support from GE Healthcare, Getinge Group, and Covidien outside the submitted work. Dr Girault reported receiving grants, personal fees, and nonfinancial support from Fisher & Paykel Healthcare during the conduct of the study and grants and nonfinancial support from ResMed outside the submitted work. Dr Ricard reported receiving travel and accommodation expenses from Fisher & Paykel Healthcare outside the submitted work. Dr Ehrmann reported receiving grants, nonfinancial support, and other funding from Fisher & Paykel Healthcare during the conduct of the study; grants, personal fees, nonfinancial support, and other funding from Aerogen; grants from Hamilton; personal fees from La Diffusion Technique Française; and personal fees from Baxter outside the submitted work. Dr Terzi reported receiving personal fees from Boehringer Ingelheim and Pfizer outside the submitted work. Dr Demoule reported receiving personal fees from Medtronic, Baxter, Hamilton, and Getinge; grants, personal fees, and nonfinancial support from Philips and Lungpacer; personal fees and nonfinancial support from Fisher & Paykel Healthcare; and grants from the French Ministry of Health and Respinor outside the submitted work. Dr Frat reported receiving personal fees and nonfinancial support from Fisher & Paykel Healthcare during the conduct of the study and personal fees and nonfinancial support from SOS Oxygen outside the submitted work. No other disclosures were reported.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Arnaud W. Thille, Email: aw.thille@gmail.com
Rémi Coudroy, Email: r.coudroy@yahoo.fr.
Mai-Anh Nay, Email: mai-anh.nay@chr-orleans.fr.
Arnaud Gacouin, Email: arnaud.gacouin@chu-rennes.fr.
Maxens Decavèle, Email: maxens.decavele@aphp.fr.
Romain Sonneville, Email: romain.sonneville@aphp.fr.
François Beloncle, Email: francois.beloncle@chu-angers.fr.
Christophe Girault, Email: christophe.girault@chu-rouen.fr.
Laurence Dangers, Email: laurence.dangers@chu-reunion.fr.
Alexandre Lautrette, Email: alexandre.lautrette@gmail.com.
Quentin Levrat, Email: quentin.levrat@ch-larochelle.fr.
Anahita Rouzé, Email: anahitarouze@gmail.com.
Emmanuel Vivier, Email: evivier@ch-stjoseph-stluc-lyon.fr.
Jean-Baptiste Lascarrou, Email: jeanbaptiste.lascarrou@chu-nantes.fr.
Jean-Damien Ricard, Email: jean-damien.ricard@aphp.fr.
Keyvan Razazi, Email: keyvan.razazi@aphp.fr.
Guillaume Barberet, Email: barberetg@ghrmsa.fr.
Christine Lebert, Email: christine.lebert@chd-vendee.fr.
Stephan Ehrmann, Email: stephanehrmann@gmail.com.
Alexandre Massri, Email: alexandre.massri@ch-pau.fr.
Jeremy Bourenne, Email: jeremy.bourenne@ap-hm.fr.
Gael Pradel, Email: gaelpradel@hotmail.com.
Pierre Bailly, Email: pierre.bailly@chu-brest.fr.
Nicolas Terzi, Email: nterzi@chu-grenoble.fr.
Jean Dellamonica, Email: jean.dellamonica@unice.fr.
Guillaume Lacave, Email: glacave@ch-versailles.fr.
René Robert, Email: rene.robert@chu-poitiers.fr.
Stéphanie Ragot, Email: stephanie.ragot@univ-poitiers.fr.
Jean-Pierre Frat, Email: jean-pierre.frat@chu-poitiers.fr.
for the HIGH-WEAN Study Group, for the REVA Research Network:
Florence Boissier, Maeva Rodriguez, Faustine Reynaud, Delphine Chatellier, Céline Deletage, Carole Guignon, Florent Joly, Anne Veinstein, Dalila Benzekri-Lefevre, Thierry Boulain, Grégoire Muller, Yves Le Tulzo, Jean-Marc Tadié, Adel Maamar, Suela Demiri, Julien Mayaux, Alexandre Demoule, Lila Bouadma, Claire Dupuis, Pierre Asfar, Marc Pierrot, Gaëtan Béduneau, Déborah Boyer, Benjamin Delmas, Bérénice Puech, Konstantinos Bachoumas, Edouard Soum, Séverin Cabasson, Marie-Anne Hoppe, Saad Nseir, Olivier Pouly, Gaël Bourdin, Sylvène Rosselli, Anthony Le Meur, Charlotte Garret, Maelle Martin, Guillaume Berquier, Abirami Thiagarajah, Guillaume Carteaux, Armand Mekontso-Dessap, Antoine Poidevin, Anne-Florence Dureau, Marie-Ange Azais, Gwenhaël Colin, Emmanuelle Mercier, Marlène Morisseau, Caroline Sabatier, Walter Picard, Marc Gainnier, Thi-My-Hue Nguyen, Gwenaël Prat, Carole Schwebel, and Matthieu Buscot
References
- 1.Thille AW, Richard J-CM, Brochard L. The decision to extubate in the intensive care unit. Am J Respir Crit Care Med. 2013;187(12):1294–1302. doi: 10.1164/rccm.201208-1523CI. [DOI] [PubMed] [Google Scholar]
- 2.Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005;33(11):2465–2470. doi: 10.1097/01.CCM.0000186416.44752.72. [DOI] [PubMed] [Google Scholar]
- 3.Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. 2006;173(2):164–170. doi: 10.1164/rccm.200505-718OC. [DOI] [PubMed] [Google Scholar]
- 4.Ferrer M, Sellares J, Valencia M, Carrillo A, Gonzalez G, Badia JR, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet (London, England) 2009;374(9695):1082–1088. doi: 10.1016/S0140-6736(09)61038-2. [DOI] [PubMed] [Google Scholar]
- 5.Girault C, Bubenheim M, Abroug F, Diehl JL, Elatrous S, Beuret P, et al. Noninvasive ventilation and weaning in patients with chronic hypercapnic respiratory failure: a randomized multicenter trial. Am J Respir Crit Care Med. 2011;184(6):672–679. doi: 10.1164/rccm.201101-0035OC. [DOI] [PubMed] [Google Scholar]
- 6.Vargas F, Clavel M, Sanchez-Verlan P, Garnier S, Boyer A, Bui HN, et al. Intermittent noninvasive ventilation after extubation in patients with chronic respiratory disorders: a multicenter randomized controlled trial (VHYPER) Intensive Care Med. 2017;43(11):1626–1636. doi: 10.1007/s00134-017-4785-1. [DOI] [PubMed] [Google Scholar]
- 7.Thille AW, Muller G, Gacouin A, Coudroy R, Decavele M, Sonneville R, et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: a randomized clinical trial. JAMA. 2019;322(15):1465–1475. doi: 10.1001/jama.2019.14901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khilnani GC, Galle AD, Hadda V, Sharma SK. Non-invasive ventilation after extubation in patients with chronic obstructive airways disease: a randomised controlled trial. Anaesth Intensive Care. 2011;39(2):217–223. doi: 10.1177/0310057X1103900210. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez G, Vaquero C, Colinas L, Cuena R, Gonzalez P, Canabal A, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316(15):1565–1574. doi: 10.1001/jama.2016.14194. [DOI] [PubMed] [Google Scholar]
- 10.Thille AW, Boissier F, Ben Ghezala H, Razazi K, Mekontso-Dessap A, Brun-Buisson C. Risk factors for and prediction by caregivers of extubation failure in ICU patients: a prospective study. Critical Care Med. 2015;43(3):613–620. doi: 10.1097/CCM.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 11.Vivier E, Muller M, Putegnat JB, Steyer J, Barrau S, Boissier F, et al. Inability of diaphragm ultrasound to predict extubation failure: a multicenter study. Chest. 2019;155(6):1131–1139. doi: 10.1016/j.chest.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Duan J, Han X, Huang S, Bai L. Noninvasive ventilation for avoidance of reintubation in patients with various cough strength. Crit Care (London, England). 2016;20(1):316. doi: 10.1186/s13054-016-1493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thille AW, Cordoba-Izquierdo A, Maitre B, Boyer L, Brochard L, Drouot X. High prevalence of sleep apnea syndrome in patients admitted to ICU for acute hypercapnic respiratory failure: a preliminary study. Intensive Care Med. 2018;44(2):267–269. doi: 10.1007/s00134-017-4998-3. [DOI] [PubMed] [Google Scholar]
- 14.Adler D, Pepin JL, Dupuis-Lozeron E, Espa-Cervena K, Merlet-Violet R, Muller H, et al. Comorbidities and subgroups of patients surviving severe acute hypercapnic respiratory failure in the intensive care unit. Am J Respir Crit Care Med. 2017;196(2):200–207. doi: 10.1164/rccm.201608-1666OC. [DOI] [PubMed] [Google Scholar]
- 15.Brochard L, Isabey D, Piquet J, Amaro P, Mancebo J, Messadi AA, et al. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. New England J Med. 1990;323(22):1523–1530. doi: 10.1056/NEJM199011293232204. [DOI] [PubMed] [Google Scholar]
- 16.Vitacca M, Ambrosino N, Clini E, Porta R, Rampulla C, Lanini B, et al. Physiological response to pressure support ventilation delivered before and after extubation in patients not capable of totally spontaneous autonomous breathing. Am J Respir Crit Care Med. 2001;164(4):638–641. doi: 10.1164/ajrccm.164.4.2010046. [DOI] [PubMed] [Google Scholar]
- 17.Pisani L, Fasano L, Corcione N, Comellini V, Musti MA, Brandao M, et al. Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax. 2017;72(4):373–375. doi: 10.1136/thoraxjnl-2016-209673. [DOI] [PubMed] [Google Scholar]
- 18.Di Mussi R, Spadaro S, Stripoli T, Volta CA, Trerotoli P, Pierucci P, et al. High-flow nasal cannula oxygen therapy decreases postextubation neuroventilatory drive and work of breathing in patients with chronic obstructive pulmonary disease. Critical Care (London, England) 2018;22(1):180. doi: 10.1186/s13054-018-2107-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 20.Hilbert G, Gruson D, Portel L, Gbikpi-Benissan G, Cardinaud JP. Noninvasive pressure support ventilation in COPD patients with postextubation hypercapnic respiratory insufficiency. Eur Respir J. 1998;11(6):1349–1353. doi: 10.1183/09031936.98.11061349. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.