Abstract
Purpose:
Child participation in type 1 diabetes (T1D) self-care is needed in developing countries due to lack of resources, especially during school day. This pilot study evaluated the feasibility of a therapeutic play intervention (ITP) vs. standard education (SE) on the ability of children with T1D to correctly perform insulin injection technique.
Design and Methods:
Children with T1D (7–12 years) were recruited at two diabetes clinics in Brazil and randomized to ITP or SE. Registered nurses received protocol training to deliver the intervention and perform data collection. ITP group received education that included a story about a child with T1D who self-injects insulin at school; SE group received routine clinic-based education. Pre-intervention, children were video-recorded giving insulin injections to a doll; post-intervention, children were re-recorded giving the doll an injection. The research team reviewed the videos and assessed injection technique using validated checklists. Parents reported children’s self-injection practices at baseline and 30 days.
Results:
Children (N=20, 40% male) were 9.6 ± 1.3 years old and had T1D for 3.6 ± 2.3 years; HbA1c was 9.1 ± 2.0%; 20% of ITP and 50% of SE children used syringes (vs. pens) for injections. At baseline, 80% of both groups knew how to self-inject; most were taught by a parent/relative. Injection technique scores were low in both groups; ITP group increased their scores significantly post-intervention. Practices of self-injection did not change in either group after 30 days.
Practice Implications:
The play-based intervention appeared to improve injection technique in the short-term. Pilot findings support the development of a larger trial to evaluate the effectiveness of ITP on educating children on insulin injections.
Keywords: Type 1 Diabetes Mellitus, Injections, Subcutaneous, Pilot Projects, Child, Pediatric Nursing, Developing Countries
1. INTRODUCTION
Intensive insulin therapy is essential to ensure normal growth, development and improve glycemic control of children with type 1 diabetes (T1D). Despite worldwide increase in diabetes technology use, including insulin pumps, multiple daily injection regimens remain the most common management approaches, especially in developing countries like Brazil (American Diabetes Association, 2019; Gomes et al., 2019). This type of regimen involves the use of three or more daily injections and is associated with better glycemic control and delayed development of complications in T1D compared to conventional therapy with fewer than three daily injections (The Diabetes Control and Complications Trial Research Group, 1993).
Considering that young people spend a good amount of their day in school and school-based activities, the provision of insulin therapy at school is crucial. When there is inadequate glycemic control, young people may experience compromised learning ability and impaired participation in school-based activities (Goss et al., 2018). In this sense, the health and safety of children with T1D in school requires the presence of a school nurse or a trained adult (Goss et al., 2018). However, not all schools have trained personnel available to assist in the care of children with diabetes (Driscoll et al., 2015).
In low-income countries, this scenario is even more complicated, as there is no policy that guarantees the presence of school nurses, trained adults, or access to technologies that facilitates insulin administration, such as continuous subcutaneous insulin infusion systems (Ogle, von Oettingen, Middlehurst, Hanas, & Orchard, 2019). In this context, children become highly involved in T1D self-care at school-age (Streisand et al., 2002; Chang, Yeh, Lo, & Shih, 2007).
In general, recommendations for diabetes self-management and education for school-aged children include a reliance on adults for performing complex tasks such as insulin dosing and administration (Beckles, Edge, Mugglestone, Murphy, & Wales, 2016; Chiang et al., 2018). Such recommendations are based upon typical cognitive and behavioral expectations of school-aged children (Chiang et al., 2018). In addition, education should give children the opportunity to obtain knowledge and dispel misconceptions about T1D self-care (Koller, Khan, & Barret, 2015).
When choosing an educational approach to teach insulin injection technique to children, health professionals must consider engaging strategies for the pediatric population, such as the use of therapeutic play. Therapeutic play is an instructional modality used by pediatric nurses and child life specialists to teach children about their diabetes and treatment protocols (La Banca et al., 2020a; La Banca, Butler, Volkening, & Laffel, 2020b). This educational strategy helps children to understand invasive procedures, such as injections, through developmentally appropriate explanations and gives children the chance to rehearse procedures using teaching dolls (Ortiz et al., 2019). Overall, therapeutic play interventions have been effective in reducing a child’s pain, anxiety, and distress while promoting cooperation (Silva, Austregesilo, Ithamar, & Lima, 2017; Sanchez Cristal et al., 2018). The use of instructional therapeutic play for children with T1D has been explored in qualitative research and has become a potential tool for diabetes education (La Banca, et al., 2019; Pennafort, Queiroz, Gomes, & Rocha, 2018).
This pilot study evaluated the feasibility of a therapeutic play intervention vs. standard education on the ability of children with T1D to correctly perform insulin injection technique. We hypothesized that insulin injection technique would improve following the therapeutic play intervention.
2. METHODS
2.1. Study Design
This manuscript reports a pilot randomized trial, approved by the Research Ethics Committee of a Brazilian university. The pilot protocol met the 33 items requirement of SPIRIT 2013 Statement (Chan et al., 2013) in which therapeutic play was compared with the standard education offered at two diabetes outpatient clinics in the city of Sao Paulo, Brazil.
2.2. Participants
Children were invited to participate if they met the following criteria: age 7–12 years, T1D duration of at least 6 months, and receiving multiple daily injections using insulin vial and syringe or insulin pen for at least 30 days prior to recruitment. Exclusion criteria included visual impairment (unable to see the syringe, pen, or insulin dosages) and honeymoon stage (period of time shortly following T1D onset when the pancreas is still able to produce some insulin, clinically defined as C-peptide measurement ≥0.01 mg/mL and/or daily insulin dose less than 0.5 U/kg).
2.3. Recruitment and Setting
Potential participants were selected by consulting the electronic schedules of both services, from October 2018 to January 2019. All names of potential participants were replaced by an identification code, generated sequentially by the principal investigator. Further, the codes were entered in SAS 9.4 for the stratified randomization procedure, performed centrally by the study principal investigator. Potential participants were allocated in the instructional therapeutic play group (ITP) or the standard education group (SE) in two age strata: 7–9 years and 10–12 years.
The local research team was comprised of six registered nurses experienced in conducting therapeutic play sessions. The nurses received protocol training by the principal investigator, a pediatric nurse researcher experienced in diabetes education and therapeutic play. The protocol training took place one month before data-collection and standardized all study procedures. The research team had opportunity to review study procedures and ask questions during weekly meetings with the principal investigator.
2.4. Control Condition
Participants in both groups received clinical care at outpatient clinics following the T1D Clinical Protocol and Therapeutic Guidelines of the Brazilian Ministry of Health in which diabetes education is provided by a physician in absence of a multidisciplinary diabetes team. Both outpatient clinics are affiliated with a public university and do not provide patients with structured diabetes education programs like those offered in many developed countries (Hawkes, Willi, & Murphy, 2019; Price et al., 2016). In the control group, participants received only the standard education provided by the physician at the time of their regular appointment.
2.5. The Instructional Therapeutic Play Intervention
At the therapeutic play session, the registered nurse relayed a scripted story to the child with the parent/guardian in attendance. The story described a child who has diabetes and has to self-inject insulin in the school setting. While telling the story, the nurse adapted the gender of the scripted character to match that of the child to facilitate bonding. The nurses presented the materials they would use for the injection: a rag doll, cotton ball with 70% alcohol, a sharps disposal box, a cool box, an insulin syringe with real needle, and a vial (10 ml) or an insulin pen [with pen needle according to the child’s usual insulin delivery modality (see Figure 1). After demonstrating all the steps of injection into the doll, the nurse offered the child the opportunity to inject the doll.
Figure 1.

Materials used for the therapeutic play intervention
2.6. Data Collection
Data collection occurred at two study visits: (1) on the day of the child’s appointment at the diabetes clinic by the research team (“baseline”); (2) through a telephone call after 30 days by the principal investigator. All potentially eligible families were approached by the nurses at their clinic encounters and invited to participate. No study procedures ensued until parents/guardians provided permission (written informed consent) to proceed and children provided assent.
Upon study entry, a nurse asked the child participants in both groups to demonstrate on a doll how to inject 5 units of fast-acting insulin. This demonstration was video recorded, and the nurse did not interrupt the children to correct their technique during the demonstration. In the SE group, data collection was complete after this procedure. In the ITP group, the child then participated in a therapeutic play session conducted by a nurse. Next, the child in the ITP group was asked to perform a second demonstration on the doll. This second demonstration was also video recorded. Parents/guardians received a follow-up call from the research team 30 days following these procedures.
2.7. Outcome Measures
At baseline, parents/guardians answered a demographic questionnaire, and a diabetes-specific questionnaire regarding their child that included date of T1D diagnosis, presence of other conditions, and diabetes management plan. The child’s medical records were reviewed for weight, height, total insulin dose, and most recent HbA1c value, including records up to six months pre-visit.
The parent/guardian also provided data on the child’s insulin injection practices at baseline and 30 days later by telephone, including how many times each week the child self-injected, age of first self-injection and person responsible for teaching the child injection technique.
The parents/guardians in the ITP group answered a question on their satisfaction with the ITP session immediately after the intervention and by telephone. The parents/guardians rated their satisfaction from 1 to 5, in which 1 represented “extremely dissatisfied”, 2 “dissatisfied”, 3 “not sure”, 4 “satisfied” and 5 “totally satisfied”. The flowchart in Figure 2 illustrates the study procedures.
Figure 2.

Study procedures flowchart
The investigators used two checklists to evaluate the child participants’ injection technique. The Syringe Injection Checklist and the Pen Injection Checklist were created by the authors as tools to measure a child’s ability to properly inject insulin. The checklists were designed to be used while reviewing video-recordings of a child’s injection technique. The final checklist score was the mean of scores from three nurses who independently watched and scored the videos. Scores could range from 0–100, with 100 indicating perfect injection technique.
The pilot feasibility trial was assessed for its practicality. The study practicality explores the extent to which an intervention can be delivered when there are limitations of resources or time dedicated to the research (Bowen et al., 2009). In this sense, assessing the pilot study practicality means implementing the study or parts of the study in a way that would mirror future approaches to see whether it could be done in a larger clinical trial (Eldridge et al., 2016).
2.8. Data Analysis
Data were double entered into Excel® and exported to SAS® version 9.4 for statistical analysis. For continuous variables, mean, median, standard deviation, and range were calculated. For categorical variables, percentages were calculated. Differences between groups were assessed by independent t-test and chi-square. In the ITP group, injection technique scores before and after the instructional play were compared by paired t-test. For all analyses, p <.05 was considered statistically significant.
3. RESULTS
3.1. Participant characteristics
Twenty children with T1D participated in the study, with 10 participants planned for each group (see Figure 3). Socio demographic and clinical characteristics of the participating children were mostly balanced between groups (see Table 1). Children had a mean age of 9.6±1.3 years with diabetes duration ranging from 0.5 to 7.8 years. Most were checking blood glucose levels at least 3 times daily (range 3–9); mean HbA1c was above goal at 9.1±2.1% (76±2 mmol/mol), range 6.5–15.5%. The majority of children (65%) received insulin therapy using insulin pens; however, the use of pens was under-represented in the standard education group.
Figure 3.

CONSORT flowchart
Table 1.
Participants characteristics a.
| All participants (N = 20) | Standard Education (n=10) | Instructional Therapeutic Play (n = 10) | P | |
|---|---|---|---|---|
| Age, years | 9.6 ± 1.3 | 9.9 ± 1.5 | 9.4 ± 1.2 | .43 |
| Diabetes duration, years | 3.6 ± 2.3 | 3.4 ± 2.2 | 3.8 ± 2.5 | .70 |
| Female sex, % | 60 | 60 | 60 | 1 |
| Race/ethnicity: white, % | 40 | 40 | 40 | 1 |
| Family structure: two-parent, % | 60 | 40 | 80 | .09 |
| Household income ≥ US$600/month | 35 | 10 | 60 | .02 |
| Parental education: high school level or higher, % | 75 | 70 | 80 | .76 |
| BMI z-scores, SDS | −0.1 ± 1.3 | 0.2 ± 0.9 | −0.4 ± 1.6 | .11 |
| HbA1c | ||||
| mmol/mol | 76 ± 23 | 78 ± 29 | 73 ± 13 | .60 |
| % | 9.1 ± 2.1 | 9.3 ± 2.6 | 8.8 ± 1.2* | |
| BG monitoring, times/day | 5.6 ± 1.9 | 5.8 ± 2.0 | 5.4 ± 1.8 | .47 |
| Daily insulin dose, units/kg | 0.7 ± 0.1 | 0.7 ± 0.1 | 0.6 ± 0.1 | .05 |
| Insulin injection device, % | ||||
| Syringe + vial | 35 | 50 | 20 | .16 |
| Pen | 65 | 50 | 80 | |
| Child performs insulin self-injection sometimes: yes, % | 80 | 80 | 80 | 1 |
| Age of first self-injection, years | 7.7 ± 1.6 | 7.7 ± 1.7 | 7.7 ± 1.7 | 1 |
| Adult supervision of child self-injection: always, % | 70 | 90 | 50 | .07 |
| Who taught the child how to self-inject, % | ||||
| Child never learned | 20 | 20 | 20 | .48 |
| Parent or a relative | 65 | 70 | 60 | |
| Nurse | 15 | 10 | 20 | |
Abbreviations: BG, blood glucose.
All values are expressed as Mean ± SD or %.
Missing value (n=9).
Parents/guardians were mainly mothers (85%) with an overall mean age of 38.5±7.2 years. Most were married or living with a partner (70%) and working either part-time or full time (70%). Family income was higher in the ITP group than in the SE group with 60% compared with 10%, respectively, earning $600 USD monthly (p=0.02).
3.2. Parent/guardian Reports of Child Self-injection
At baseline, most parents/guardians (80%) reported that their children were already performing insulin self-injections and 70% always had adult supervision during the procedure. Most children (65%) had learned from their parents/relatives while 15% had learned from a nurse. The mean age of first self-injection was under 8 years (range 5–10 years old) depicted in Table 1.
At study entry, children were self-injecting insulin 4.3±3.2 times/week (range 0–7). After 30 days, there was no difference observed on the parent/guardian reports of child self-injection frequencies (p=0.53) (see Table 2)
Table2.
Frequency of child self-injections per week at baseline and after 30 days.
| All participants (N=20) | Standard Education (n=10) | Instructional Therapeutic Play (n=10) | ||||
|---|---|---|---|---|---|---|
| Mean±SD | Median (Range) |
Mean±SD | Median (Range) |
Mean±SD | Median (Range) |
|
| Baseline | 4.3 ± 3.2 | 6.5 (0–7) |
5.0 ± 3.0 | 7.0 (0–7) |
3.7 ± 3.3 | 4.5 (0–7) |
| 30 days | 4.5 ± 3.1 | 7 (0–7) |
5.6 ± 2.9 | 7.0 (0–7) |
3.5 ± 3.0 | 3.5 (0–7) |
3.3. Injection technique scores before and after intervention
At baseline, the SE group had a mean injection technique score of 42.1±19.2 (range 18–75), similar to the score in the ITP group, 44.0±11.1 (range 25–62) (p=0.79) (see Figure 3). Injection technique score increased significantly in the ITP group after the intervention to 62.6±18.7 (p=0.01). Injection technique scores improved for both children using vial with syringe and for those using insulin pens (see Figure 4); however, the changes were not statistically significant due to small number of participants. The injection technique score of the ITP group after the therapeutic play session was significantly higher than the score in the SE group at baseline by 20.5±18.9 (p=0.02). There were no statically significant differences between injection technique scores of children aged 7–9 years and children aged 10–12 years (p=.56), although older children had higher scores (41.0±15.5 of youngers vs. 45.1±15.7 of olders).
Figure 4.
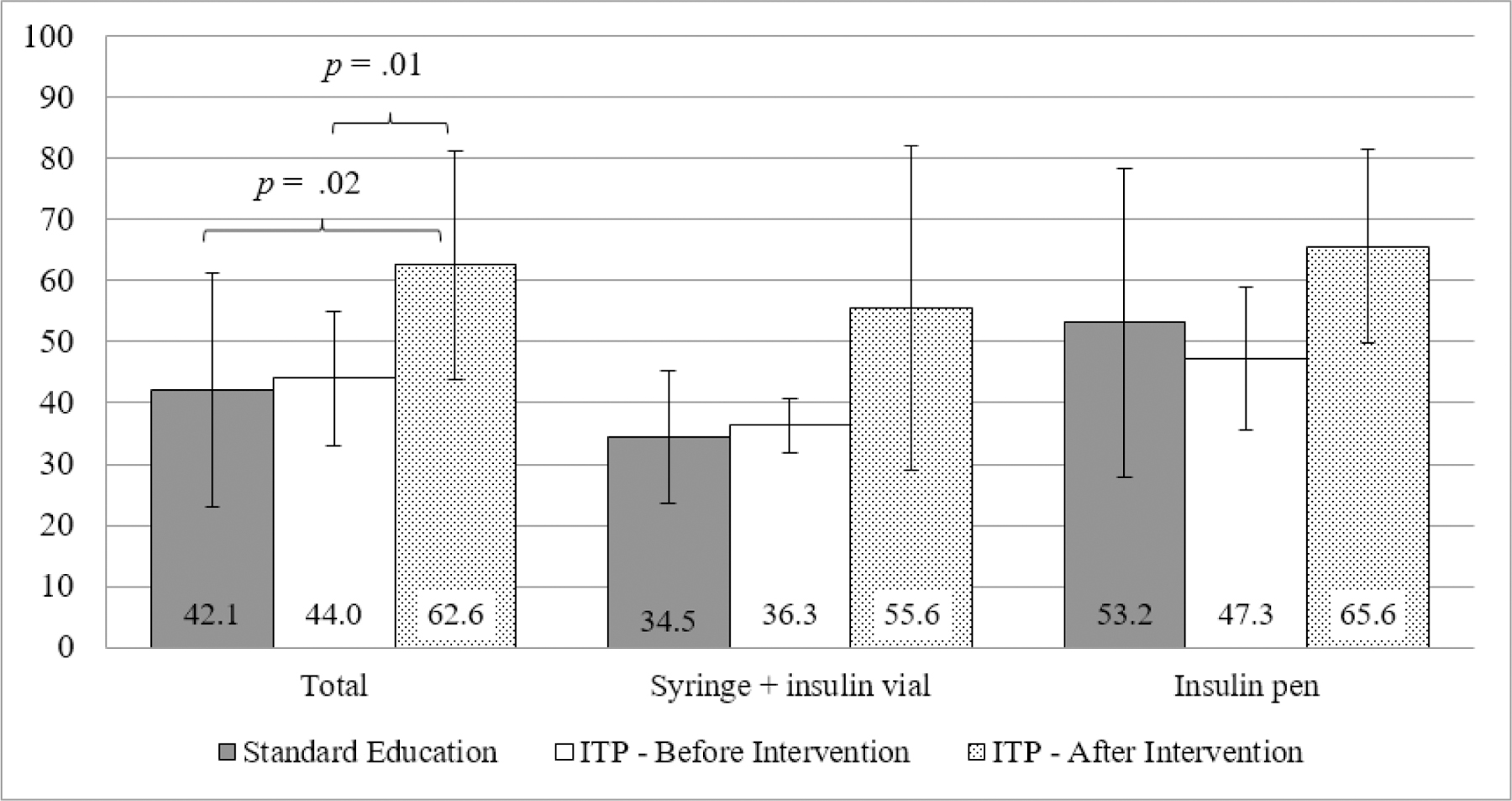
Injection technique scores according to insulin device used by the child.
3.4. Observed insulin technique errors and improvements following ITP
The most common errors regarding injection technique varied according to insulin delivery method. Those using vial and syringe often incorrectly injected air into the vial before drawing up the insulin into the syringe, neglected to inject the air entirely before drawing up the insulin, or incorrectly withdraw the proper dose of insulin. For those using insulin pens, many forgot to roll the pen in their hands to warm it up after removing it from a cool pack. Both groups infrequently inspected the injection sites before giving the injection.
After the ITP intervention, for those using vial and syringe, there were improvements in injection techniques related to checking and removing air bubbles in the syringe, holding and releasing the ‘skin’ of the doll for the injection, and properly disposing of the used syringe in a sharps container. After the ITP intervention, the children treated with insulin pens similarly demonstrated improvements in the areas of hand hygiene, priming of the pen needle before dose selection, cleaning the injection site, waiting for the alcohol to dry before injecting the insulin, and delaying removal of the pen needle for a few seconds after injecting.
3.5. Satisfaction with the ITP intervention
Only parents/guardians of children in the ITP group received the satisfaction survey. Nine caregivers (90%) reported extreme satisfaction (scored of 5) after the ITP intervention while one caregiver (10%) reported satisfaction (score of 4). There was no change in satisfaction scores when the survey was repeated after 30 days.
3.6. Pilot Feasibility
The main finding of this pilot study that may inform a future randomized clinical trial comprise logistics for data collection in outpatient clinics without research facilities, therefore the intervention practicality. Our research team reported coordinating the pilot data collection and medical encounters were challenging. Although the study was approved by the institution’s IRB and approved by the clinic coordinators, the research team needed local support for data collection. The front-desk secretaries of the outpatient clinics and health professionals who worked in the service helped to coordinate the time when the research nurses would approach potential participants and their caregivers. Even though caregivers were informed that participation in the study would not compromise the follow-up in the health service, many families were resistant to participate if the research visit was scheduled to occur after the medical encounter.
In order to organize the environment and prepare for the study procedures, the research team had, on average, to arrive two hours before the start of medical appointments to approach potential participants and end the research visit. It was not possible to bring participants to the research visit other than the day of the medical encounter, as research resources were not available to remunerate the family member for their participation such as transportation reimbursement.
Moreover, since the clinics where the study was carried out were not facilities with specific rooms for research visits, the interview with the caregiver and the ITP intervention depended on the availability of an empty room on the collection days. Many interviews took place in the waiting room, compromising quality of data collection due to the high flow of people and frequent noise and indicating opportunities for improvement in the protocol for conducting the larger trial.
4. DISCUSSION
This pilot study explored the feasibility of a play-based intervention compared with standard education on the ability of children with T1D to correctly perform insulin injection technique. Due to the substantial number of under-resourced countries globally in which there are insufficient numbers of either healthcare professionals or trained adults in the school environment, children with T1D are often expected to begin self-care behaviors at a young age in order to receive midday insulin injections as part of intensive insulin therapy. (Chiang et al., 2018)
Participants in the ITP and SE groups had reasonably similar characteristics, although families from ITP group reported higher income while educational attainment was similar. Additionally, more children in the ITP group used insulin pens rather than vial and syringe for insulin delivery, compared to the SE group. Notably, the Brazilian public health system provides free vials and syringes but does not provide insulin pens. Furthermore, at the time this study was conducted the Brazilian public health system only provided regular and NPH insulin with no coverage for insulin analogs or insulin pens. Children from Brazil are not alone in their needs as families from other under-resourced countries often experience similar deficiencies in supplies for their child’s diabetes care (Gomes et al., 2017; Ogle, Kim, Middlehurst, Silink, & Jenkins, 2016).
The recommended standard of care for diabetes management in children requires intensive insulin therapy using multiple daily injections when there are no resources for insulin pump use (Danne et al., 2018). The demands of intensive treatment of T1D often require that parents rearrange schedules or resign from work in order to care for their children with T1D (Katz, Laffel, Perrin, & Kuhlthau, 2012; Katz, Volkening, Dougher, & Laffel, 2015). In this study, the majority of parents/guardians reported working part-time or full-time. Interestingly, the majority of participating children (80%) knew how to self-inject insulin upon study entry, likely due to their need to self-inject insulin during the day without help from a trained adult.
Previous studies have highlighted the importance of family involvement in the management of T1D in youth (Katz et al., 2015; King, Berg, Butner, Butler, & Wiebe, 2014; Laffel et al., 2003). However, in Brazil and other developing countries, it is often necessary for children to acquire self-care responsibilities at a young age due to deficient resources in the school setting. Furthermore, there are limited data regarding the optimal age at which children should acquire diabetes self-care tasks (La Banca, Volkening, & Laffel, 2019). Nonetheless, the need for midday insulin administration may demand educational approaches to help engage the young child in self-care efforts while simultaneously reminding the parents of the ongoing need for family involvement in the child’s diabetes care when at home.
Premature transfer of diabetes management tasks solely to youth with T1D can result in early diabetes burn-out, which can lead to non-adherence and deteriorating glycemic control during adolescence (American Diabetes Association, 2019; Cameron, Garvey, Hood, Acerini, & Codner, 2018). Further, decreased parental involvement in diabetes management can cause psychosocial problems, such as depressive symptoms and diabetes-related distress (Katz, Volkening, Butler, Anderson, & Laffel, 2014; Wu, Hilliard, Rausch, Dolan, & Hood, 2013). Thus, designing nursing interventions, for example, that include therapeutic play can aid families when there is need to transfer some care tasks to the child with T1D.
In a review on interventions aimed at improving self-care skills in youth with T1D, inclusion of parents helped to improve adherence of youth in their self-care routines and enhances the parents’ perception of their child’s ability to participate in diabetes management (Cahill, Polo, Egan, & Marasti, 2016). Moreover, previous studies have noted the importance of parent support and collaboration with health care providers as a means to facilitate self-care in youth with T1D (Koller, Khan, & Barret, 2014; Kelo, Martikainen, & Eriksson, 2011). Nurses acknowledge the importance of building collaborations with parents and child life specialists to promote play-based strategies in order to create a sense of fun and positive experience for the pediatric clientele (Drayton, Waddups & Walker, 2019). In this sense, Brazilian pediatric nurses can benefit from family-based approaches and the therapeutic play to support the transfer of diabetes self-care tasks from parents to the child such as insulin therapy.
It is important to highlight that most pediatric nurses do not have the same background as possessed by child life specialists. The research team in this study was experienced in developing therapeutic play activities for children with T1D, received protocol training, and was supervised by the principal investigator, a pediatric nurse with expertise in therapeutic play interventions. The awareness of Brazilian nurses in developing play-based strategies has been previously discussed (Maia, Ribeiro, & Borba, 2011). However, we acknowledge that most nurses do not have this type of training and that their role is geared towards the provision of medical care. In this sense, there must be specific training and supervision in order to optimally deliver both diabetes education and therapeutic play in nursing care.
With regard to school support, there have been international efforts to train school personnel about diabetes in developing countries (Bechara et al., 2018; Chinnici et al., 2019). However, it is common that teachers from elementary and middle schools are only authorized to perform blood glucose monitoring or to give insulin injections to youth with T1D in emergencies (Chinnici et al., 2019; Rapp, Arent, Dimmick, & Jackson, 2005). Therefore, the use of play-based interventions such as therapeutic play can provide education and support for the young child who has to self-inject insulin in school.
In this pilot study, children who received the ITP intervention increased their injection technique scores. This was especially evident for older school age children and those using insulin pens. Further, the most common errors in injection technique were observed for youth using insulin vial and syringe. Injections with a pen comprise fewer steps than injections with a syringe and vial; however, access to insulin pens can be challenging in under-resourced countries like Brazil, reinforcing the need to engage the child and family in the proper use of vials and syringes, potentially through play-based interventions (Calliari et al., 2018). Furthermore, literature has shown that children engage better in self-care when real medical equipment is used in the education process (Koller, 2018), what might explain why children who participated in the ITP intervention had higher injection technique scores than children who received standard education.
Of note, there were no observed differences in the frequency of insulin self-injections from baseline to 30 days after the intervention. The therapeutic play activity focused on injection technique without discussion of ongoing efforts by the child in his/her own self-care behaviors. Future play-based interventions might incorporate activities related to encouraging insulin self-injections, particularly in the school setting when there is no trained adult available, to maintain intensive insulin therapy aimed at optimizing glycemic control.
There are a number of limitations to this study related to the small number of participants, the single dose of the play-based intervention, and the limited follow-up period. Furthermore, the SE group only demonstrated insulin injection on the doll a single time although it is unlikely that technique would have changed without any further intervention. Future studies should expand the follow-up duration in order to observe the longitudinal effects of the therapeutic play intervention. Moreover, there is need to include not only parent reported outcomes with regard to insulin injection technique but also the children’s perceived barriers in performing T1D self-care at school as well as their satisfaction with therapeutic play. Future research should consider insulin delivery modality, with randomization in vial/syringe and pen strata or preplanned use of buckets to ensure equal representation of children using insulin vial/syringe and insulin pens.
Nonetheless, this pilot project was the first study to use a play-based strategy to teach school-aged children insulin self-injection technique. The results regarding caregiver satisfaction with the intervention also reinforce the potential use of therapeutic play to promote a child’s participation in diabetes self-care.
HOW MIGHT THIS INFORMATION AFFECT NURSING PRACTICE?
Findings of this paper indicate the potential benefit of a nurse-led therapeutic play intervention for teaching insulin injection to children with T1D. Although challenges observed for data collection in the two outpatient clinics due to lack of research resources, these pilot results support the improvement of a protocol for a larger and longer randomized controlled clinical trial in Brazil to evaluate the effectiveness of therapeutic play compared with standard education on enhancing insulin injection technique, frequency of self-injections, and improved glycemic control in children with T1D.
This study builds on the extant literature by assessing the feasibility of a therapeutic play intervention delivered by nurses following procedures of a rigorous research method such as a randomized trial. The positive effect of the therapeutic play activity might motivate Brazilian and other international nurses to pursue training in play-based strategies, as well as partnering with child life professionals in order to deliver pediatric programs in diabetes education. Therefore, the pilot study results support a feasible nursing intervention to be implemented in pediatric nursing.
What is currently known?
Children with type 1 diabetes from developing countries often participate in self-care during the school day due to lack of resources.
When teaching diabetes self-care tasks, nurses must consider engaging strategies for the pediatric population, such as the use of therapeutic play
What does this article add?
A therapeutic play intervention compared with standard education showed to improve the ability of children with type 1 diabetes to perform insulin injections correctly.
Pediatric nurses might promote a child’s participation in diabetes self-care through therapeutic play, an age-appropriate educational intervention.
References
- American Diabetes Association. (2019). 13. Children and Adolescents: Standards of Medical Care in Diabetes-2019. Diabetes Care, 42(Suppl 1), S148–S164. [DOI] [PubMed] [Google Scholar]
- Bechara GM, Castelo Branco F, Rodrigues AL, Chinnici D, Chaney D, Calliari LEP, & Franco DR (2018). “KiDS and Diabetes in Schools” project: Experience with an international educational intervention among parents and school professionals. Pediatr Diabetes, 19(4), 756–760. [DOI] [PubMed] [Google Scholar]
- Beckles ZL, Edge JA, Mugglestone MA, Murphy MS, & Wales JK (2016). Diagnosis and management of diabetes in children and young people: summary of updated NICE guidance. BMJ, 352, i139. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, …, Fernandez M (2009). How We Design Feasibility Studies. Am J Prev Med. 2009 May; 36(5): 452–457. 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill SM, Polo KM, Egan BE, & Marasti N (2016). Interventions to Promote Diabetes Self-Management in Children and Youth: A Scoping Review. Am J Occup Ther, 70(5), 7005180020p7005180021–7005180028. [DOI] [PubMed] [Google Scholar]
- Calliari LE, Cudizio L, Tschiedel B, Pedrosa HC, Rea R, Pimazoni-Netto A, … Strauss K (2018). Insulin Injection Technique Questionnaire: results of an international study comparing Brazil, Latin America and World data. Diabetol Metab Syndr, 10, 85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron FJ, Garvey K, Hood KK, Acerini CL, & Codner E (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Diabetes in adolescence. Pediatr Diabetes, 19 Suppl 27, 250–261. [DOI] [PubMed] [Google Scholar]
- Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K, … Moher D (2013). SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med, 158(3), 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CW, Yeh CH, Lo FS, & Shih YL (2007). Adherence behaviours in Taiwanese children and adolescents with type 1 diabetes mellitus. Journal of Clinical Nursing, 16(7B), 207–214. 10.1111/j.1365-2702.2005.01541.x [DOI] [PubMed] [Google Scholar]
- Chiang JL, Maahs DM, Garvey KC, Hood KK, Laffel LM, Weinzimer SA, … Schatz D (2018). Type 1 Diabetes in Children and Adolescents: A Position Statement by the American Diabetes Association. Diabetes Care. [DOI] [PMC free article] [PubMed]
- Chinnici D, Middlehurst A, Tandon N, Arora M, Belton A, Reis Franco D, … Cavan D (2019). Improving the school experience of children with diabetes: Evaluation of the KiDS project. J Clin Transl Endocrinol, 15, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danne T, Phillip M, Buckingham BA, Jarosz-Chobot P, Saboo B, Urakami T, … Codner E (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes, 19(Suppl 27), 115–135. [DOI] [PubMed] [Google Scholar]
- Drayton NA, Waddups S, Walker T (2019). Exploring distraction and the impact of a child life specialist: Perceptions from nurses in a pediatric setting. J Spec Pediatr Nurs. 24:e12242 Retrieved from: https://onlinelibrary.wiley.com/doi/abs/10.1111/jspn.12242 [DOI] [PubMed] [Google Scholar]
- Driscoll KA, Volkening LK, Haro H, Ocean G, Wang Y, Jackson CC, … Siminerio LM (2015). Are children with type 1 diabetes safe at school? Examining parent perceptions. Pediatr Diabetes, 16(8), 613–620. [DOI] [PubMed] [Google Scholar]
- Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, & Bond CM (2016). Defining Feasibility and Pilot Studies in Preparation for Randomised Controlled Trials: Development of a Conceptual Framework. PloS one, 11(3), e0150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomes MB, Rodacki M, Pavin EJ, Cobas RA, Felicio JS, Zajdenverg L, & Negrato CA (2017). The impact of ethnicity, educational and economic status on the prescription of insulin therapeutic regimens and on glycemic control in patients with type 1 diabetes. A nationwide study in Brazil. Diabetes Research and Clinical Practice, 134, 44–52. [DOI] [PubMed] [Google Scholar]
- Gomes MB, Santos DC, Pizarro MH, Melo LGN, Barros BSV, Montenegro R, … Negrato CA (2019). Relationship between health care insurance status, social determinants and prevalence of diabetes-related microvascular complications in patients with type 1 diabetes: a nationwide survey in Brazil. Acta diabetologica, 56(6), 697–705. [DOI] [PubMed] [Google Scholar]
- Goss PW, Middlehurst A, Acerini CL, Anderson BJ, Bratina N, Brink S, … Wolfsdorf J (2018). ISPAD Position Statement on Type 1 Diabetes in Schools. Pediatr Diabetes, 19(7), 1338–1341. [DOI] [PubMed] [Google Scholar]
- Hawkes CP, Willi SM, & Murphy KM (2019). A structured 1‐year education program for children with newly diagnosed type 1 diabetes improves early glycemic control. Pediatric Diabetes, 20(4), 460–467. [DOI] [PubMed] [Google Scholar]
- Katz ML, Laffel LM, Perrin JM, & Kuhlthau K (2012). Impact of type 1 diabetes mellitus on the family is reduced with the medical home, care coordination, and family-centered care. J Pediatr, 160(5), 861–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz ML, Volkening LK, Butler DA, Anderson BJ, & Laffel LM (2014). Family-based psychoeducation and Care Ambassador intervention to improve glycemic control in youth with type 1 diabetes: a randomized trial. Pediatr Diabetes, 15(2), 142–150. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz ML, Volkening LK, Dougher CE, & Laffel LM (2015). Validation of the Diabetes Family Impact Scale: a new measure of diabetes-specific family impact. Diabet. Med, 32(9), 1227–1231. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelo M, Martikainen M, & Eriksson E (2011). Self-care of school-age children with diabetes: an integrative review. Journal of advanced nursing, 67(10), 2096–2108. 10.1111/j.1365-2648.2011.05682.x [DOI] [PubMed] [Google Scholar]
- King PS, Berg CA, Butner J, Butler JM, & Wiebe DJ (2014). Longitudinal trajectories of parental involvement in Type 1 diabetes and adolescents’ adherence. Health Psychol, 33(5), 424–432. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23795709. doi:2013-21805-001 [pii];10.1037/a0032804 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koller D (2018). Anxiety and the Hospitalized Child: Best Practices for Guiding Therapeutic Play Charles Schaefer, (Ed). Play-Based Interventions for Childhood Anxieties, Fears, and Phobias. Guilford Press, New York. [Google Scholar]
- Koller D, Khan N, & Barrett S (2015). Pediatric perspectives on diabetes self-care: a process of achieving acceptance. Qualitative health research, 25(2), 264–275. 10.1177/1049732314551057 [DOI] [PubMed] [Google Scholar]
- La Banca RO, Brandão MCM, Sparapani VC, de Souza NS, Neves ET, Cavicchioli MGS, … Nascimento LC (2020a). A fun way to learn about diabetes: Using therapeutic play in a Brazilian camp. Journal of Pediatric Nursing. [DOI] [PubMed]
- La Banca RO, Butler DA; Volkening LK; Laffel LM (2020b). Play-Based Interventions Delivered by Child Life Specialists: Teachable Moments for Youth With Type 1 Diabetes. Journal of Pediatric Health Care. 10.1016/j.pedhc.2020.02.002 [DOI] [PMC free article] [PubMed]
- La Banca RO, Ribeiro CA; Freitas MS; Freitas MAO; Nascimento LC; Monteiro OO; Borba RIH (2019). Therapeutic play in the teaching of insulin therapy to children with diabetes: a qualitative case study. Rev. Eletr. Enf, 21, 52591 10.5216/ree.v21.52591 [DOI] [Google Scholar]
- La Banca RO, Volkening LK, & Laffel LM (2019). Acquisition of Self-Care in Youth with Type 1 Diabetes (T1D) Varies by Age and Task. Diabetes, 68 10.2337/db19-1375-P [DOI] [Google Scholar]
- Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, & Anderson BJ (2003). Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr, 142(4), 409–416. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12712059. [DOI] [PubMed] [Google Scholar]
- Maia EB, Ribeiro CA, & de Borba RI (2011). Compreendendo a sensibilização do enfermeiro para o uso do brinquedo terapêutico na prática assistencial à criança [Understanding nurses’ awareness as to the use of therapeutic play in child care]. Revista da Escola de Enfermagem da USP, 45(4), 839–846. 10.1590/s0080-62342011000400007 [DOI] [PubMed] [Google Scholar]
- Ogle GD, Kim H, Middlehurst AC, Silink M, & Jenkins AJ (2016). Financial costs for families of children with Type 1 diabetes in lower-income countries. Diabet Med, 33(6), 820–826. [DOI] [PubMed] [Google Scholar]
- Ogle GD, von Oettingen JE, Middlehurst AC, Hanas R, & Orchard TJ (2019). Levels of type 1 diabetes care in children and adolescents for countries at varying resource levels. Pediatr Diabetes, 20(1), 93–98. [DOI] [PubMed] [Google Scholar]
- Ortiz GS, O’Connor T, Carey J, Vella A, Paul A, Rode D, & Weinberg A (2019). Impact of a Child Life and Music Therapy Procedural Support Intervention on Parental Perception of Their Child’s Distress During Intravenous Placement. Pediatric emergency care, 35(7), 498–505. 10.1097/PEC.0000000000001065 [DOI] [PubMed] [Google Scholar]
- Pennafort V. P. d. S., Queiroz MVO, Gomes ILV, & Rocha M. d. F. F. (2018). Instructional therapeutic toy in the culture care of the child with diabetes type 1. Revista Brasileira de Enfermagem, 71, 1334–1342. Retrieved from http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0034-71672018000901334&nrm=iso. [DOI] [PubMed] [Google Scholar]
- Price K, Knowles J, Fox M, Wales J, Heller S, Eiser C, … Knowles J (2016). Effectiveness of the Kids in Control of Food (KIC k–OFF) structured education course for 11–16 year olds with Type 1 diabetes. Diabetic Medicine, 33(2), 192–203. [DOI] [PubMed] [Google Scholar]
- Rapp J, Arent S, Dimmick B, & Jackson C (2005). Legal rights of students with diabetes. Alexandria, Va., American Diabetes Association.
- Sanchez Cristal N, Staab J, Chatham R, Ryan S, Mcnair B, & Grubenhoff JA (2018). Child Life Reduces Distress and Pain and Improves Family Satisfaction in the Pediatric Emergency Department. Clinical pediatrics, 57(13), 1567–1575. 10.1177/0009922818798386 [DOI] [PubMed] [Google Scholar]
- Silva RD, Austregesilo SC, Ithamar L, & Lima LS (2017). Therapeutic play to prepare children for invasive procedures: a systematic review. J Pediatr (Rio J), 93(1), 6–16. [DOI] [PubMed] [Google Scholar]
- Streisand R, Respess D, Overstreet S, Gonzalez de Pijem L, Chen RS, & Holmes C (2002). Brief report: self-care behaviors of children with type 1 diabetes living in Puerto Rico. Journal of Pediatric Psychology, 27(8), 759–764. 10.1093/jpepsy/27.8.759 [DOI] [PubMed] [Google Scholar]
- The Diabetes Control and Complications Trial Research Group. (1993). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England Journal of Medicine, 329(14), 977–986. Retrieved from https://www.nejm.org/doi/pdf/10.1056/NEJM199309303291401 [DOI] [PubMed] [Google Scholar]
- Wu YP, Hilliard ME, Rausch J, Dolan LM, & Hood KK (2013). Family involvement with the diabetes regimen in young people: the role of adolescent depressive symptoms. Diabet Med, 30(5), 596–602. [DOI] [PMC free article] [PubMed] [Google Scholar]


