Version Changes
Updated. Changes from Version 1
This update of our living systematic reviews includes literature up to October 2020 whereas our last was up to 7th June 2020. Searches identified 6,226 articles. Seventy-eight articles met our revised inclusion criteria, 49 more than in our previous review. All were still based on observational studies. The majority of studies remained case series but there are now an increased number of service utilisation studies from across the world. There were still no studies were based on populations from sub-saharan Africa. In contrast to the last update in which no studies reported on the change in incidence of suicide or suicidal behaviour after the onset of the pandemic compared with beforehand, we identified nine papers in this update, presenting data on studies from four countries which investigated the impact of COVID-19 on suicide rates. To date, the highest quality data come from Japan which utilises suicide records covering the entire population; these data indicate that the impact of COVID-19 on suicides rates may change over time and have varying effects on different sections of the population. There was no consistent evidence of a rise in suicide but many studies noted adverse economic effects were evolving. There was evidence of a rise in community distress, fall in hospital presentation for suicidal behaviour and early evidence of an increased frequency of suicidal thoughts in those who had become infected with COVID-19. We have updated the author order to reflect contribution to this update, predominately related to oversight of specific tables and drafting specific sections of text. We have added new authors who have joined the screening team.
Abstract
Background: The COVID-19 pandemic has caused considerable morbidity, mortality and disruption to people’s lives around the world. There are concerns that rates of suicide and suicidal behaviour may rise during and in its aftermath. Our living systematic review synthesises findings from emerging literature on incidence and prevalence of suicidal behaviour as well as suicide prevention efforts in relation to COVID-19, with this iteration synthesising relevant evidence up to 19 th October 2020.
Method: Automated daily searches feed into a web-based database with screening and data extraction functionalities. Eligibility criteria include incidence/prevalence of suicidal behaviour, exposure-outcome relationships and effects of interventions in relation to the COVID-19 pandemic. Outcomes of interest are suicide, self-harm or attempted suicide and suicidal thoughts. No restrictions are placed on language or study type, except for single-person case reports. We exclude one-off cross-sectional studies without either pre-pandemic measures or comparisons of COVID-19 positive vs. unaffected individuals.
Results: Searches identified 6,226 articles. Seventy-eight articles met our inclusion criteria. We identified a further 64 relevant cross-sectional studies that did not meet our revised inclusion criteria. Thirty-four articles were not peer-reviewed (e.g. research letters, pre-prints). All articles were based on observational studies.
There was no consistent evidence of a rise in suicide but many studies noted adverse economic effects were evolving. There was evidence of a rise in community distress, fall in hospital presentation for suicidal behaviour and early evidence of an increased frequency of suicidal thoughts in those who had become infected with COVID-19.
Conclusions: Research evidence of the impact of COVID-19 on suicidal behaviour is accumulating rapidly. This living review provides a regular synthesis of the most up-to-date research evidence to guide public health and clinical policy to mitigate the impact of COVID-19 on suicide risk as the longer term impacts of the pandemic on suicide risk are researched.
Keywords: COVID-19, Living systematic review, Suicide; Attempted suicide, Self-harm, Suicidal thoughts
Introduction
The COVID-19 pandemic is causing widespread societal disruption, morbidity and loss of life globally. By the end of December 2020 over 85 million people had been infected and over 1.8 million had died ( Worldometers, 2020). There are concerns about the impact of the pandemic on population mental health ( Holmes et al., 2020). These stem from the impact of the virus itself on people infected ( Taquet et al., 2021), as well as frontline workers caring for them ( Kisely et al., 2020) and increases in bereavement. Other concerns relate to the impact on population mental health of the public health measures that have been implemented to minimise the spread of the virus – in particular physical distancing, leading to social isolation, disruption of businesses, services and education and threats to peoples’ livelihoods. Physical distancing measures and lockdowns have resulted in substantial rises in unemployment, falls in GDP and concerns that many nations will enter a prolonged period of deep economic recession.
There are concerns that suicide and self-harm rates may rise during and in the aftermath of the pandemic ( Gunnell et al., 2020; Reger et al., 2020). Time-series modelling indicated that the 1918–20 Spanish Flu pandemic, which caused well over 20 million deaths worldwide, led to a modest rise in the national suicide rate in the USA ( Wasserman, 1992) and Taiwan ( Chang et al., 2020). Likewise, there is some evidence that previous epidemics and pandemics were associated with rises in suicide and suicidal behaviour ( Zortea et al., 2020). Suicide rates increased briefly amongst people aged over 65 years in Hong Kong during the 2003 SARS epidemic, predominantly amongst those with more severe physical illness and physical dependency ( Cheung et al., 2008).
The current context is, however, very different from previous epidemics and pandemics. The 2003 SARS epidemic was restricted to relatively few countries. Furthermore, during the 100-year period since the 1918–20 influenza pandemic, global and national health systems have improved, international travel and the speed of communication of information (and disinformation) have increased, antibiotics are available to treat secondary infection, and national economies have become globally inter-dependent. The availability of the internet and technological advancement has made it far easier for people to communicate and engage in home working and home schooling. However, there are marked social inequalities in relation to access to technology and ability to stay safe and continue to work, within and between countries. Public health policies and responses, and the degree of access to technology to facilitate online clinical assessments and treatments differ greatly between countries.
Key concerns in relation to suicide prevention during the pandemic include: encouraging help-seeking in those with suicidal thoughts and behaviours e.g. people who have attempted suicide may not attend hospitals because they are worried about contracting COVID-19 or being a burden on the healthcare system at this time; uncertainty regarding how best to assess and support people with suicidal thoughts and behaviours, whilst maintaining physical distancing and addressing any impacts of remote consultation; diminished access to community-based support; exposure to traumatic experiences; long term effect of infection with the virus on mental health ( Taquet et al., 2021) and an economic recession may have an adverse impact on suicide rates ( Chang et al., 2013; Stuckler et al., 2009). There have been increases in bereavement (with many being unusually complicated during the crisis), sales of alcohol ( Finlay & Gilmore, 2020) and domestic violence ( Mahase, 2020) – all risk factors for suicide ( Turecki et al., 2019); the insensitive or irresponsible media reporting of suicide deaths associated with COVID-19 may be harmful ( Hawton et al., 2021); and in some countries access to highly lethal suicide methods such as firearms and pesticides may rise ( Anestis et al., 2021; Gunnell et al., 2020). However early findings from high income countries with ‘real-time’ suicide trend data, indicates there was no rise in suicide rates in the early months of the pandemic ( John et al., 2020a). Japan is the exception to this rule, falls in Japanese suicide rates in the early months of the pandemic have since been replaced by rises above pre-pandemic levels July/August 2020 and beyond ( John et al., 2020a; Tanaka & Okamoto, 2021; Ueda et al., 2021). The longer-term impact of the pandemic on suicide deaths and suicidal behaviour remains uncertain.
In the context of the COVID-19 pandemic there is a rapidly expanding evidence base on its impact on suicide rates, and how best to mitigate such effects. It is therefore important that the best available knowledge is made rapidly available to policymakers, public health specialists and clinicians. To facilitate this, we are conducting a living systematic review focusing on incidence and prevention of suicide and self-harm in relation to COVID-19. Living systematic reviews are high-quality, up-to-date online summaries of research that are regularly updated, using efficient, often semi-automated, systems of production ( Elliott et al., 2014). Our first report covered the period up to the 7 th June 2020. This paper reports the second set of findings from the review, based on relevant articles identified up to 19 th October 2020.
Aim
The overarching aim of the review is to identify and appraise any newly published evidence from around the world that assesses the impact of the COVID-19 pandemic on suicide deaths, suicidal behaviours, self-harm and suicidal thoughts, or that assesses the effectiveness of strategies to reduce the risk of suicide deaths, suicidal behaviours, self-harm and suicidal thoughts, associated with the COVID-19 pandemic.
Methods
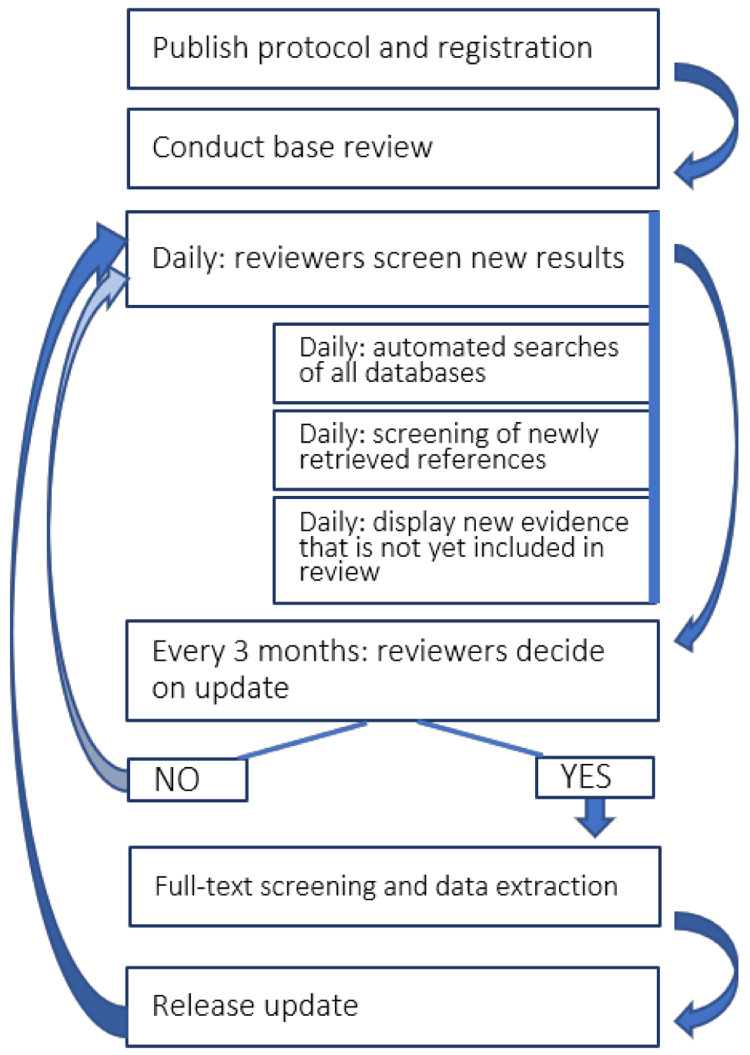
This living systematic review ( Figure 1) follows published guidance for such reviews and for how expedited ‘living’ recommendations should be formulated where relevant ( Akl et al., 2017; Elliott et al., 2017). The review was prospectively registered (PROSPERO ID CRD42020183326; registered on 1 st May 2020). An overview of our living review process is provided in Figure 1. A protocol ( John et al., 2020b) was published in line with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols guideline ( Moher et al., 2015) along with the first update of our review which summarised articles identified up to 7 th June 2020 ( John et al., 2020c). Since publication of our protocol we have amended our methodology to: 1) search additionally the PsyArXiv and SocArXiv open access paper repositories; 2) include modelling studies within the scope of our review (e.g. to predict the likely impact of the pandemic on suicide rates); 3) update our research questions to include studying the impact of adult self-neglect and parental neglect and fear of losing livelihood on suicide-related outcomes; 4) update our searches with any new citations from PsycINFO prior to each update; 5) exclude from data extraction and presentation in results tables single-wave, cross-sectional surveys unless they explicitly make comparisons with appropriate pre-pandemic measures or include comparative data between COVID-19 positive and unaffected individuals for pragmatic reasons, due to the volume of such studes but also issues to do with sampling and generalisability of such studies. Surveys that meet the original inclusion criteria are included as an appendix to the update.
Figure 1. Workflow for updating the living systematic review review.
The process will be supported using automation technology and at three-monthly intervals the team will update the published version of the review.
Eligibility criteria
Study participants may be adults or children of any ethnicities living in any country. Outcomes of interest are:
-
1.
Deaths by suicide
-
2.
Self-harm (intentional self-injury or self-poisoning regardless of motivation and intent) or attempted suicide (including hospital attendance and/or admission for these reasons)
-
3.
Suicidal thoughts/ideation
Studies must address one of the following research questions:
(i) What is the prevalence/incidence?
Prevalence/incidence of each outcome during pandemic (including modelling studies)
(ii) What is the comparative prevalence/incidence?
Prevalence/incidence of each outcome during pandemic vs not during pandemic
(iii) What are the effects of interventions?
Effects of public health measures to combat COVID-19 (including physical distancing, school closures, interventions to address loss of income, interventions to tackle domestic violence) on each outcome
Effects of changed and new approaches to clinical management of (perceived) elevated risk of self-harm or suicide risk on each outcome (any type of intervention is relevant)
(iv) What are the effects of other exposures?
Impact of media portrayal on each outcome and misinformation attributed to the pandemic on each outcome
Impact of bereavement from COVID-19 on each outcome
Impact of any COVID-19 related behaviour changes (domestic violence, alcohol, adult self-neglect, parental neglect, cyberbullying, isolation) on each outcome
Impact of COVID-19-related workload on crisis lines on each outcome
Impact of infection with COVID-19 (self or family member) on each outcome
Impact of changes in availability of analgesics, firearms and pesticides on each outcome (method-specific and overall suicide rates)
Impact of COVID-19 related socio-economic exposures (changes in fiscal policy; recession/depression: unemployment, debt, fear of losing livelihood, deprivation at the person-, family- or small-area level) on each outcome
Impact on health and social care professionals: the stigma of working with COVID-19 patients or the (perceived) risk of infection/being a ‘carrier’, as well as work-related stress on each outcome
Impact of changes in/reduced intensity of treatment for patients with mental health conditions, in particular those with severe psychiatric disorders.
Impact of any other relevant exposure on our outcomes of interest.
Qualitative research
We included any qualitative research addressing perceptions or experiences around each outcome in relation to the COVID-19 pandemic (e.g. stigma of infection, isolation measures, complicated bereavement, media reporting, experience of delivering or receiving remote methods of self-harm / suicide risk assessment or provision of treatment; experience of seeking help for individuals in suicidal crisis); narratives provided for precipitating factors for each outcome.
No restrictions were placed on the types of study design eligible for inclusion, except for the exclusion of single-person case reports. Pre-prints will be re-assessed at the time of publication and the most current version included. There was no restriction on language of publication. We drew on a combination of internet-based translation systems and network of colleagues to translate reports in languages other than English.
Identification of eligible studies
We searched the following electronic databases: PubMed; Scopus; medRxiv, PsyArXiv; SocArXiv; bioRxiv; the COVID-19 Open Research Dataset (CORD-19) by Semantic Scholar and the Allen Institute for AI, which includes relevant records from Microsoft Academic, Elsevier, arXiv and PMC; and the WHO COVID-19 database. A sample search strategy (for PubMed) appears in Box 1 from 1 st January 2020 to 19 th October 2020. We have developed a workflow that automates daily searches of these databases, and the code supporting this process can be found at https://github.com/mcguinlu/COVID_suicide_living). Searches are conducted daily via PubMed and Scopus application programme interface and the bioRxiv and medRxiv RSS feeds. Conversion scripts for the daily updated WHO and the weekly updated CORD-19 corpus are used to collect information from the remaining sources. The software includes a systematic search function based on regular expressions to search results retrieved from the WHO, CORD-19 and preprint repositories (search strategy available in extended data). Our review is ongoing and we continue to investigate the use of other databases and to capture articles made available prior to peer review and assess eligibility and review internally. For this update we therefore included PsyArXiv and SocArXiv repositories in our search strategy via their own open access platforms as we developed our automated system. PsycINFO searches were carried out retrospectively on 6 th January 2021, using a publication date filter for 1 st January 2020 to 19 th October 2020.
Box 1. Search terms for PubMed.
((selfharm*[TIAB] OR self-harm*[TIAB] OR selfinjur*[TIAB] OR self-injur*[TIAB] OR selfmutilat*[TIAB] OR self-mutilat*[TIAB] OR suicid*[TIAB] OR parasuicid*[TIAB) OR (suicide[TIAB] OR suicidal ideation[TIAB] OR attempted suicide[TIAB]) OR (drug overdose[TIAB] OR self?poisoning[TIAB]) OR (self-injurious behavio?r[TIAB] OR self?mutilation[TIAB] OR automutilation[TIAB] OR suicidal behavio?r[TIAB] OR self?destructive behavio?r[TIAB] OR self?immolation[TIAB])) OR (cutt*[TIAB] OR head?bang[TIAB] OR overdose[TIAB] OR self?immolat*[TIAB] OR self?inflict*[TIAB]))) AND ((coronavirus disease?19[TIAB] OR sars?cov?2[TIAB] OR mers?cov[TIAB]) OR (19?ncov[TIAB] OR 2019?ncov[TIAB] OR n?cov[TIAB]) OR ("severe acute respiratory syndrome coronavirus 2" [Supplementary Concept] OR "COVID-19" [Supplementary Concept] OR COVID-19 [tw] OR coronavirus [tw] OR nCoV[TIAB] OR HCoV[TIAB] OR ((virus*[Title] OR coronavirus[Title] OR nCoV[Title] OR infectious[Title] OR HCoV[Title] OR novel[Title])AND (Wuhan[Title] OR China[Title] OR Chinese[Title] OR 2019[Title] OR 19[Title] OR COVID*[Title] OR SARS-Cov-2[Title] OR NCP*[Title]) OR “Coronavirus”[MeSH]))))
A two-stage screening process was undertaken to identify studies meeting the eligibility criteria. First, two authors (either CO or EE) assessed citations from the searches and identified potentially relevant titles and abstracts. Second, either DG, AJ or RW assessed the full texts of potentially eligible studies to identify studies to be included in the review. This process was managed via a custom-built online platform (Shiny web app, supported by a MongoDB database). The platform allowed for data extraction via a built-in form.
Data collection and assessment of risk of bias
One author (DG, AJ or RW) extracted data from each included study using a piloted data extraction form, and the extracted data were checked by one other author (DG, KH, EA, RC, AJ, or EE where AJ extracted data, AJ where DG extracted data). Disagreements were resolved through discussion, and where this failed, by referral to a third reviewer (KH, NK or PM). Irrespective of study design, data source and outcome measure examined, the following basic information were extracted: citation; study aims and objectives; country/setting; characteristics of participants; methods; outcome measures (related to self-harm / suicidal behaviour and COVID-19); key findings; strengths and limitations; reviewer’s notes. For articles where causal inferences are made - i.e. randomised or non-randomised studies examining the effects of interventions or aetiological epidemiological studies of the effects of specific exposures – we plan to use a suitable version of the ROBINS-I or a preliminary similar tool for exposure studies to assess risk of bias as appropriate based on the research question and study design ( Morgan et al., 2017; Sterne et al., 2016).
Data synthesis
We synthesised studies according to themes based on research questions and study design, using tables and narrative. Results were synthesised separately for studies in the general population, in health and social care staff and other at-risk occupations, and in vulnerable populations (e.g. people of older age or those with underlying conditions that predispose them to becoming severely ill or dying after contracting COVID-19) where relevant. Where multiple studies addressed the same research questions, we assessed whether meta-analysis was appropriate and would conduct it where suitable, following standard guidance available in the Cochrane Handbook ( Deeks et al., 2019). The current document is the second iteration of our review. We have not considered it appropriate to combine any results identified so far in a meta-analysis due to quality and heterogeneity.
Results
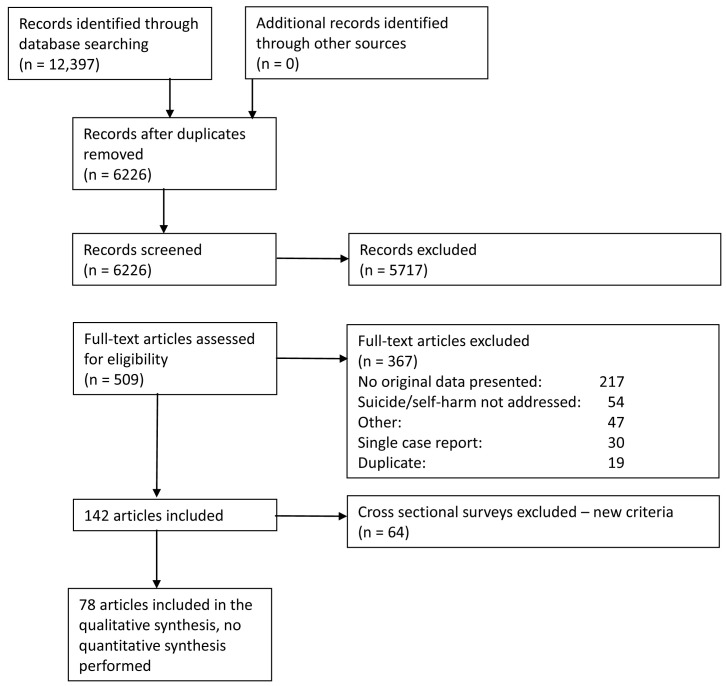
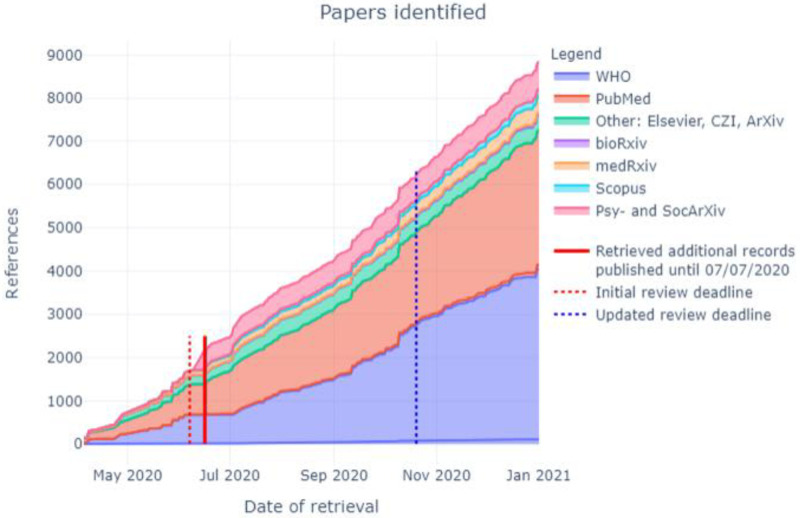
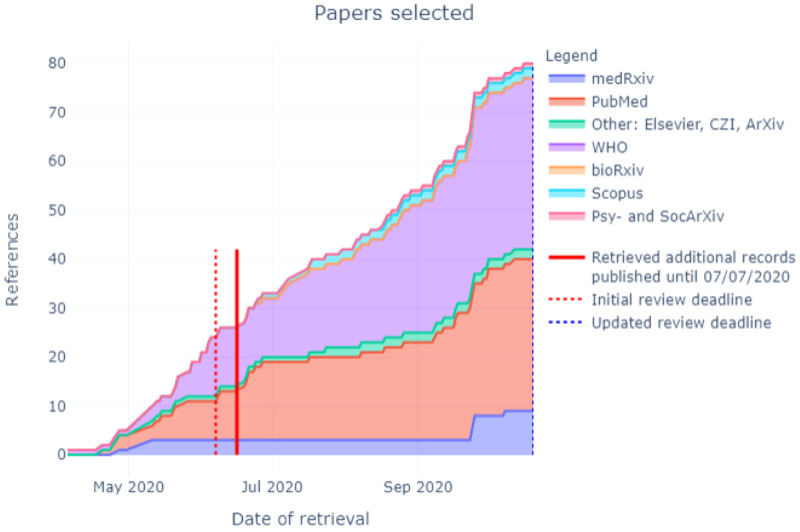
In total, 12,397 citations were identified by 19 th October 2020 from all electronic searches, after duplicates were removed ( Figure 2). The cumulative numbers of articles over time that were identified by the search and included in the review are shown in Figure 3 and Figure 4. The majority of studies identified in the review (5105; 82%) were sourced from two databases, PubMed and WHO; a further 10% (n=622) were drawn from pre-print sites such as MedRxiv.
Figure 2. PRISMA flow diagram.
Figure 3. Number of articles identified by database and repository over time.
Figure 4. Number of articles selected by database and repository over time.
Description of included studies
We included 78 articles in the review. We have highlighted in Table 1– Table 6 where new citations have updated existing studies. Sixty-four cross sectional surveys are included in Appendix 1. In total, six studies spanned several countries or were worldwide, including one using a Reddit mental health dataset (almost half of users are from the USA); 13 were from the United States; seven from China; nine from India; five from the United Kingdom; four each from Japan and Nepal; and between one and three each from Australia, Bangladesh, Canada, Czech Republic, Denmark, France, Germany, Greece, Iran, Ireland, Israel, Italy, Pakistan, Peru, Poland, Portugal, Spain, Qatar and Switzerland. All articles were based on observational studies: twenty-five were case series with a sample of two or more (although Jefson et al., 2020 and Rohde et al., 2020 were based on the same case series); thirteen were cross sectional surveys; two were based on social media posts; six were modelling studies; twenty were service utilisation studies; and nine assessed suicide rates. Studies are summarised by these study types in Table 1 through Table 6. Three other relevant articles were identified, two of these described mixed methods studies ( Evans et al., 2020; Son et al., 2020) and one a case-control study ( Cai et al., 2020). Almost half (n=34) of the articles did not appear to have been peer- reviewed of which ten were pre-prints and 21 were published as research letters to the Editor.
Table 1. Summary of included case series.
| Authors | Geography | Data used | Outcome | Conclusions | Comment/ Limitations |
|---|---|---|---|---|---|
| Ahmed et al., 2020 | India | Suicide cases linked with alcohol
withdrawal syndrome (AWS) reported in newspapers or news channels’ websites from 25 March (start of national lockdown) to 5 May 2020. All cases were in the states of the southern part of India: Kerala, Tamil Nadu, Telangana, and Karnataka. ( n=23) |
Suicide death | AWS seems implicated in a number of
suicides in southern India but, on the basis of the empirical information that is presented here, we do not know whether these deaths were caused by the COVID-19 lockdown, and whether these deaths occurred at a higher frequency during the observation period than they normally occur. |
We cannot be sure whether any of the
suicides occurred primarily as a direct consequence of AWS, or were brought about due to the unavailability of alcohol during lockdown. Study uses news reports as their data source. Letter to the editor, so unlikely to be peer reviewed. |
| Bhuiyan et al., 2020 | Bangladesh | News reports of COVID-19 related
suicide deaths (n=8) |
Suicide death | Job loss, debt and difficulties obtaining
food because of financial difficulties reported in all cases |
Small sample size (n=8)
Study uses news reports as their data source. Letter to editor, probably not peer reviewed. |
| Boshra & Islam, 2020a | Bangladesh | Suicide cases relating to COVID-19 taken
from Bangladeshi online media INITIAL REPORT: 1 March to 31 July 2020 (n=32) UPDATED REPORT published October 27th (Boshra & Islam 2020b): 1 March to 30 Sept 2020 ( n=37). 65% of the cases were male. |
Suicide death | 45.9% were due to economic reasons
attributed to lockdown-related unemployment. |
Although they examined only cases
relating to COVID-19, the authors recognize they do not know how many cases would have occurred if the pandemic had not happened. Study uses news reports as their data source. Pre-print, not peer reviewed. |
| Buschmann & Tsokos, 2020a | Germany | Case series of 10 individuals identified at
autopsy who died by suicide during the pandemic up to March 25 th 2020 UPDATED REPORT ( Buschmann & Tsokas, 2020b) Individuals identified at autopsy who died by suicide associated with the effects of the pandemic up to 29 May 2020 ( n=11) |
Suicide death | All had pre-existing mental health issues.
No evidence of COVID-19. Authors conclude that the effects of the lockdown and media reporting influenced the suicide. |
It is unclear what circumstances of the
deceased persons were brought about directly due to the COVID-19 crisis. Both are Letters to editor, probably not peer reviewed. |
| Dsouza et al., 2020 | India | News reports (n=69) of COVID-19 related
suicide deaths including n=72 cases from March to 24 May 2020. Age range 19–65 years; 63 (88%) males. |
Suicide death | The most common reported factors
were: 1) Fear of infection (n=21); 2) Financial crisis (n=19); 3) COVID-19 related stress (n=9); 4) Positive test for COVID-19 (n=7); 5) Isolation related issues (n=5) 6)Social boycott (n=4); and 7) Migrant unable to return home (n=3). |
Study uses news reports as their data
source. Overlaps with other publications based on news reports from same country e.g. Rajkumar, 2020; Shiob et al., 2020. Letter to editor, probably not peer reviewed. |
| Griffiths & Mamun, 2020 | Global
-Bangladesh, India, Malaysia, USA |
News reports of couples (
n=6) engaging
in COVID-19-related suicidal behaviour includes one murder suicide identified via Searches of seven English- Indian online papers from March to 24 May. |
Suicide attempt
and/or death (couples) |
Details several potential reasons:
1) Fear of infection; 2) Money problems (due to recession associated with lockdowns); 3) Harassment or victimisation by others due to (possibly perceived) infection status; 4) Stress of being in isolation or quarantine; and 5) Uncertainty of when the pandemic will end. |
Small sample size (n=6)
Study uses news reports as their data source. Letter to editor, probably not peer reviewed. |
| Iqbal et al., 2020 | Qatar | Referrals of patients with a positive
COVID-19 test to consultant liaison psychiatry service from a ward or A&E in three hospitals in Doha, . Median age 39.5; 48 male ( n=50) |
Suicide
attempts/self- harm |
Three of the 50 referrals had self
harmed. The self-harm was apparently a reaction to the pandemic. Two were asymptomatic for COVID-19, and one had a mild case. |
Focus is on psychiatric presentations in
people with acute infections, the long term impact of COVID-19 infection on psychiatric morbidity requires further study. Peer reviewed. |
|
Jefsen
et al., 2020a
Rohde et al., 2020 |
Denmark | Review of notes of adult patients from
the psychiatric services of the Central Denmark Region (catchment area: 1.3 million people). Notes between 1 Feb and 23 March 2020 reviewed to identify those describing "pandemic-related psychiatric symptoms" (including "self harm / suicidality", n=74). Median age 29.8 years; 77% female Note full case series n=1357 relevant records found from 412,804, reported in Rohde et al.,, 2020. |
Suicide
attempts/self- harm, suicidal thoughts |
Of the 74 patients identified, 14 (19%)
had self-harm thoughts; 10 (14%) had self-harmed; 34 (46%) had suicidal thoughts; 10 (14%) had made suicide attempts and 13 (18%) had a passive wish to die from COVID-19. |
Findings restricted to suicidal / self-harm
related outcomes in 74 patients with these outcomes. No data on the overall percentage of adult psychiatry patients with these outcomes during or pre-pandemic. Peer-reviewed letter to the editor. |
| Jefsen et al., 2020b | Denmark | All clinical notes from patients below
18 years old in the Central Danish psychiatric service between 1 Feb and 23 March 2020. Pandemic‐related psychopathology identified in 94 children and adolescents. |
Suicide
attempts/self- harm |
8 notes from 5 of the 94 patients
specifically described self‐harm or suicidality related to the pandemic |
No baseline data for individuals.
No data on the overall percentage of child psychiatry patients with these outcomes during or pre-pandemic. Editorial perspective; probably not peer reviewed. |
| Jolly et al., 2020 | USA | Child and adolescent psychiatry
inpatients, age range 11–17 years; 3 female, 1 male; ( n=4). |
Suicide
attempts/self- harm, Suicidal thoughts |
One suicide attempt; one suicidal plan
and two with suicidal thoughts Stressors described included: 1. Unable to see friends/ partner (all cases) 2. Arguments with parents 3. Misunderstanding within friendship group that could not be resolved well over social media 4. Academic worries- performance declined since move to distance learning 5. Feeling isolated |
Detailed descriptive study of very small
sample. Peer reviewed journal. |
| Kapilan, 2020 | India | News reports about two nurses drawn
from news reports ( n=2) |
Suicide death,
Suicide attempts/self- harm |
1 suicide: a nurse who treated COVID-19
patients, and died reportedly due to “ extreme stress and mental disturbance” 1 suicide attempt: a nurse who contracted COVID-19 |
Small sample size (n=2)
Information drawn from news reports. Similar to Rahman et al., 2020. Letter to the editor; possibly not peer reviewed. |
| Kar et al., 2020 | India | News reports of deaths by suicide
among film stars in India, 28 May to 30 July 2020 ( n=7). |
Suicide death | 7 Indian film stars who died by suicide.
Media reports claimed three of these were related to financial problems associated with COVID-19. |
It is unclear whether any of the deaths
were strongly linked with COVID-19 and its indirect impact on people's lives, or whether the individuals were already experiencing mental health difficulties. Study uses news reports as their data source. Appears to use the same data as Mamun et al., 2020b. Letter to the editor; probably not peer reviewed. |
| Mamun et al., 2020a | Bangladesh | News report of suicide pact in mother
and 22 year old son, 11 Jun 2020 ( n=2) |
Suicide death | University student aged 22 and his
mother aged 47 died by suicide. The father had insisted the day before that the student complete online exams as an internet connection was arranged. |
Study uses news reports as their data
source. Only a single pact reported Suggests that online teaching in LMIC may create real tensions due to digital poverty Letter to the editor; possibly not peer reviewed. |
| Mamun et al., 2020b | India | News reports of deaths by suicide
among film stars in India ( n=7 in 2020 vs. n=16 in 2002–2019) |
Suicide death | The frequency of celebrity suicides
in India appears to have increased markedly during the COVID-19 era. The authors highlight the dangers of sensationalised media reporting of celebrity suicides triggering immitative events in the general population. |
Study uses news reports as their data
source. Appears to use the same data as Kar et al., 2020 Letter to the editor; possibly not peer reviewed. |
| Mamun & Ullah, 2020 | Pakistan | News reports of COVID-19 related
suicide deaths in Pakistan, Jan 2020 to end April 2020 ( n=12, a further 4 reports of suspected suicide were not presented). |
Suicide death | Economic concerns reported in 8/12
cases, and fear of infection in the remaining 4. There were 13 other reports of suicides (and attempted suicide) during this period not reported to be linked to COVID-19. |
Highlights the potential importance of
the economic impact of COVID-19 and/or public health measures on influencing suicide in low- and middle-income countries. Study uses news reports as their data source. Peer reviewed journal; paper accepted on same day as received. |
| Nalleballe et al., 2020 | World | Adult COVID-19 patients (inpatients and
outpatients) with records held on the TriNetX database ( trinetx.com), 20 Jan to 10 June 2020 (n= 40,469, 76% living in USA |
Suicidal
thoughts |
9,086 (22.5%) had a neuropsychiatric
coded diagnosis within 1 month of COVID-19 diagnosis. 62 (0.2%) had suicidal thoughts recorded. |
Large clinical database of people with
clinical diagnosis of COVID-19. It is possible that suicidal thoughts were not asked about systematically by clinicians and so there is likely to be marked under-recording. Peer reviewed journal. |
| Pirnia et al., 2020 | Iran | Suicide of members of one family ( n=2). | Suicide death | Son died by suicide three weeks after his
father died of COVID-19. Two days after the son, the mother also killed herself. |
Small sample size (n=-2).
Letter to the editor; probably not peer reviewed. |
| Rahman et al., 2020 | Worldwide | News reports of nurse suicide deaths
( n=6, 2 from Italy, 1 each from UK, Mexico, USA and India) |
Suicide death | Factors reported as associated with
deaths included: fear they had become infected; positive test result; being in quarantine; fearful of becoming infected. |
Study uses news reports as their data
source. Small sample size (n=6). Similar to Kapilan, 2020. Peer reviewed letter to the editor. |
| Rajkumar, 2020 | India | 49 English-language news reports of
COVID-19 related suicides in India, 12 March to 11 April 2020 ( n=23 deaths) |
Suicide death | 6 of the deaths occurred amongst
patients hospitalised / in isolation In 7 cases a diagnosis was mentioned - in 4 this was depression, in 3 alcohol dependence. Precipitating / contributing factors included fear of acquiring infection (9/23); developing influenza-like symptoms (7/23); bereavement (n=5) |
Study uses news reports In English as
their data source. Provides interesting observations, useful for hypothesis testing. Probable overlap with others e.g. Dsouza et al., 2020; Shiob et al., 2020 Letter to the editor, possibly not peer reviewed. |
| Sahoo et al., 2020 | India | Clinical case reports of COVID-19 related
suicide attempts presenting to the ED ( n=2) |
Suicide attempts | Both cases were related to the fear
and stigma of COVID-19. One case was ordered to self-isolate due to being in contact with a known case. |
Small sample size (n=2)
Letter to editor; probably not peer reviewed. |
| Shoib et al., 2020 | India | News reports in 22 English and local
newspapers published in India, identified from Google and reporting on suicides in relation to COVID-19 Search period 25 Jan to 18 April 2020 ( n=34 suicides) |
Suicide death | 18 (52.9%) aged 18–35 years; 28 (82.4%)
male Most frequent reasons given: Fear of infection: 16 (47.1%); misinterpreted fever as COVID-19: 9 (26.5%); Depression and loneliness: 7 (20.6%); personal stigma of COVID-19: 4 (11.8%) Authors mapped number of reports vs number of suicides over the 8 week study period. Rise in COVID-19 related suicides mirrored the rise in number of cases - in first 3 weeks there was 1 report per week, whereas in the last 3 weeks there were 23 reports |
Large case series of news reports,
but probably overlaps with others e.g. Dsouza et al., 2020; Rajkumar, 2020. Study uses news reports as their data source. Letter to the editor, possibly not peer reviewed. |
| Syed et al., 2020 | India | Reports of alcohol-related suicides from
India, extracted from recent media reports, using Google News, retrieving reports of suicide cases from Indian online English language newspapers between 25 March and 17 May 2020 (during India’s national lockdown). Age range 25–70 years; all males ( n=27) |
Suicide death,
Suicide attempts |
27 cases suicide or suicide attempts.
Alcohol restrictions were reported as leading to an increase in attempts and deaths, because of alcohol withdrawal syndrome. |
Case reports from newspapers in English
in Indian news. Underreporting possible because of stigma. Similar to Shiob et al., 2020. Letter to the editor; possibly not peer reviewed. |
| Thakur & Jain, 2020 | World | News reports of COVID-19 related
suicide deaths ( n=7) |
Suicide death | Identified 4 types of suicide risks:
1) Social isolation; 2) Economic; 3) Stress in health professionals; 4) Stigma |
Small sample size (n=7)
Study uses news reports as their data source. Peer reviewed journal; paper accepted 1 day after received. |
| Valdés-Florido et al., 2020 | Spain | Patients admitted to two hospitals in
Spain with reactive psychoses in the context of the COVID-19 crisis during the first two weeks of lockdown ( n=4) |
Suicide attempts | Stress from the pandemic thought to
have triggered reactive psychoses in four patients two of whom presented with severe suicidal behaviour |
Small sample size (n=4)
Peer reviewed journal. |
Table 2. Summary of cross sectional surveys and cohort studies.
| Authors | Geography | Data used | Outcome | Conclusions | Comment/ Limitations |
|---|---|---|---|---|---|
| Debowska et al., 2020 | Poland | University students recruited via 10 Polish
universities and the Students’ Parliament of the Republic of Poland. N = 7228, 81% female; Mean age = 22.78. Data collection occurred in five waves, during the first two months of the COVID- 19 pandemic in Europe (March – April 2020). The waves differed from one another in the amount and type of lockdown-type measures, with wave 4 being characterised by the strictest restrictions |
Suicidal thoughts | No statistical evidence of differences
in suicidal thoughts over the 5 stages of data collection or of gender differences in prevalence. |
Representativeness of sample unclear
Frequency and intensity of suicidal thoughts and impulses in the past 24 h were measured using the Depressive Symptom Inventory-Suicidality Subscale ( Joiner et al., 2002) Letter to editor, probably not peer reviewed |
| Hamm et al., 2020 | USA | Subset of adults aged >60 years who
were participating in an RCT of treatment resistant depression and agreed to a qualitative interview. N=73 (of total 743 RCT participants) |
Suicide and self-harm
thoughts |
5(7%) had suicidal thoghts at the time
of the interview (April 1–23 2020), but not pre-pandemic; 7 (10%) had had a reduction in pre-existing suicidal thoughts. The rest had no suicidal thoughts pre or post pandemic |
Used PHQ-9 pre and post pandemic
(validated measure) Those agreeing to interview self- selecting, perhaps less likely to have experienced untoward effects. Small sample Peer reviewed |
| Hamza et al., 2021 | Canada | Students at a single university in Canada
Surveyed using the same survey tool in May 2019 and May 2020. n=773 (74% female; mean age 18.5 years) ( 964 responders to 2019 survey) |
Suicide attempts/
self-harm |
No statistical evidence evidence of rise
in NSSI: score at T1 (May 2019) 0.18 (SD 0.38) and T 2 (May 2020) 0.20 (SD 0.40) Likewise no difference when analysis stratified according to presence of absence of pre-existing mental health concerns |
Used adapted version of the Inventory
of Statements about Self-Injury (ISAS; Klonsky & Glenn, 2009) to assess non-suicidal self-harm in relation to 7 behaviours e.g. cutting / biting. Reported average score on ISAS scale rather than prevalence of each / any behaviour Peer reviewed |
| Iob et al., 2020 | UK | General population sample recruited on-
line via media / social media. Survey data from 21 March – 20 April 2020. Participants included individuals who provided data on abuse, self-harm and thoughts of suicide or self-harm on at least one occasion n = 44 775 Weighted to represent UK population (age, sex, ethnicity, education) |
Suicide attempts/
selfharm, suicide and self-harm thoughts Help seeking |
7984 (18%) reported suicidal / self-
harm thoughts; 2174 (5%) had self harmed at least once. Suicide/self-harm thoughts higher in those with a COVID-19 diagnosis vs. without (33% vs 17%); likewise for suicide attempts (14% vs. 5%). 57% of those engaging in SH and 40% with thoughts had sought some professional support. Compared with previous UK survey data, levels of help-seeking from MH professionals (14.5% for thoughts / 4.7% SH/SA) were lower. (14.5% for thoughts / 4.7% SH/SA) were lower. |
Suicidal / self-harm thoughts
measured via PHQ-9. Self harm via asking participants whether they’d self-harmed or deliberately hurt themselves. Index period was the last week. Large sample but convenience sampling Use of sample weighting to take account of selection bias Report on outcomes in relation to COVID-19 diagnosis but may be confounded by sociodemographic differences between groups Peer reviewed |
| Raifman et al., 2020 | USA | Two nationally representative surveys
of US adults: 1) The 2017–2018 National Health and Nutrition Examination Survey (NHANES)- 5085 (86.8%) of 5856 NHANES participants responded to suicidal ideation questions and were included in the analyses; 2) 2020 COVID-19 and Life Stressors Impact on Mental Health and Wellbeing study (CLIMB) - conducted 31st March to 13th April 2020. 1415 (96.3%) of 1470 CLIMB participants responded to all questions relevant to the analysis |
Suicidal thoughts | Suicidal ideation increased more than
fourfold, from 3.4% in the 2017–2018 NHANES to 16.3% in the 2020 CLIMB survey, and from 5.8% to 26.4% among participants in low-income households. Suicidal ideation was more prevalent among people facing difficulty paying rent (31.5%), job loss (24.1%), and loneliness (25.1%). |
Survey methods for NHANES and
CLIMB were not identical, but two large population-based surveys conducted at two points. Characteristics of participants in CLIMB and NHANES differed. Respondents may have differed from those who did not, particularly if the stressors examined affected survey participation. Pre-print, not peer reviewed |
| Sueki & Ueda, 2020 | Japan | Two wave population survey of Japanese
people aged >20. Recruited via Internet Survey company to reflect census population of Japan. 6683 completed both waves of the survey (out of 125,011 people selected (5%) and 67% of the 9982 who completed the wave 1 survey) 51% male; mean age 46.5 years. Surveyed Jan 24 2020 (when there were just 2 covid-19 cases in Japan) and again 27–30 April, 3 weeks after state of emergency declared. |
Suicidal thoughts | Suicidal thoughts score was lower
during the pandemic (mean = 1.59) than before it (mean = 1.71),t(6682) = 5.87, p < .001. People in their 30s, and people: a) with unstable employment status (part-time, temporary worker), b) without children, c) with relatively low annual household income and d) those currently receiving psychiatric care had higher suicidal thoughts scores at T2 vs. the reference group, after controlling for suicidal ideation at T1 |
Short-form suicide ideation scale"
( Sueki, 2019). 6 questions, overall scores ranges from 0–12. Low response rate from selected sample (5%) And at T2 vs T1 (67%). Pre-print, not peer reviewed |
| Wang et al., 2020a | China | COVID 19 patients and controls January 2,
2020 to March 10, 2020. 376 COVID-19 patients (including 95 male and 281 female patients) hospitalized between January 2 and March10, 2020,with 501 controls without COVID 19 (including 110 men and 391 women) recruited from different social media platforms |
Suicidal thoughts | In Covid-19 patients moderate or high
suicide risk in 27 % COVID-19 patients vs. 8 % in control (sig difference). High or very high suicide risk similarly higher in Covid group 10% vs. 4%. Age, anxiety, depression and poor sleep quality were all risk factors for high suicide risk in COVID-19 patients. |
Online or face to face interview
assessment by psychiatrists using the Nurses’ Global Asesment of Suicide Risk scale(NGASR). Convenience sampled controls Unlikely to be peer reviewed |
| Wang et al., 2020b | China | Repeat cross sectional study. Participants
who completed survey via “Wenjuanxing,” a Chinese online platform providing functions equivalent to Qualtrics. The data were from two studies, one conducted during the outbreak stage from (N=2540, mean age = 25.28 ± 8.07) and one conducted during the after peak stage (N=2543, mean age = 22.03 ± 6.30) |
Symptom networks
illustrating the relationship between depression and anxiety symptoms were estimated Suicidal thoughts showed a decreased connection with “inability to relax” and “guilty” symptoms, whereas suicidal thoughts showed an increased connection with the “too much worry” symptom over time |
The association between symptoms
changed over the course of the pandemic in China Some changes in connections between some symptoms of suicidal thoughts and other symptoms of depression/anxiety If generalizable, could point to some treatment targets that are more central to suicide risk |
Limitation: anxiety and depression
assessed via self-report not diagnoses Used PHQ-9 Not certain how generalizable networks are to other phases of the pandemic or to other countries Peer reviewed |
| Winkler et al., 2020 | Czech
Republic |
Covid-19 survey 6th to 20th May 2020.:
N=3021 respondents interviewed either by computer-assisted telephone interview or computer assisted web interviewing. General population aged 18–64 years. The survey was representative in relation to national population (age, sex, education and region) Comparable baseline data were obtained from the 2017 Czech Mental Health Survey. |
Suicide risk | Marked increase in respondents with
moderate/high suicide risk from 3.9% (95% CI 3.2, 4.5) in 2017 to 12.3 (11.1, 13.4) in 2020. Having been tested for Covid-19 (with a positive or negative result) was linked with elevated perceived suicide risk (OR 2.1; 1.1, 3.8) as was Covid-19 health worries (OR 1.4; 1.1, 2.1) and Covid-19 economic worries (OR 1.4; 1.2, 1.7). |
Mini International Neuropsychiatric
Interview (MINI) Large nationally representative survey with comparable baseline data but Covid-19 survey was conducted remotely whereas the baseline survey was face-to-face interviewing, so information bias cannot be ruled out. Computer- assisted telephone interviewing had a low participation rate. Peer reviewed |
| Wu et al., 2020a | China | Survivors of COVID-19, followed up
median 22 days (IQR 20–30d) post hospital discharge. N=370 |
Suicide and Self-harm
thoughts |
4 (1.1%) reported experiencing
suicidal / self-harm thoughts over several days |
Large survey of hospital admitted
COVID-19 No pre-illness baseline measure. Used PHQ-9 (standardised measure). Letter to editor, probably not peer reviewed. |
| Wu el al., 2020b | China | 4124 pregnant women during their third
trimester from 25 public hospitals in 10 provinces Jan 1 st-Feb 9 th 2020 1285 assessed after January 20, 2020 when the coronavirus epidemic was publicly announced and 2839 were assessed before this time point. |
Self-harm thoughts | A multi-centre study to
identify mental health concerns in pregnancy The risk of self- harm thoughts was higher after 20 th January compared to before (aRR=2.85, 95% CI: 1.70, 8.85, P=0.005). |
Pre-existing data collection system.
Thoughts of self-harm in the last 7 days from the Edinburgh Postnatal Depression Scale (EPDS, Cox et al.,., 1987) The findings indicate a need for enhanced levels of psychological support for pregnant women during a major infectious disease epidemic / pandemic. Pregnant women in Wuhan, Hubei Province (the epicentre of the epidemic) were not included in the sample. Peer reviewed |
| Zhao et al., 2020 | China | Survey of COVID-19 patients (n=106), 46
male, range 35–92 years at Tongji Hospital, Wuhan from Carried out February 2nd- 16 th, 2020 |
Suicide and Self-harm
thoughts |
24.5% (26/106) of COVID-19 patients
had self-harming or suicidal thoughts, which were "significantly higher percentages than those of the general population." |
Highlights the potential mental health
support needs, and the risk faced by recovering COVID-19 patients. Used PHQ-9. Peer reviewed |
| Zhang et al., 2020 | China | Repeated survey in cohort of primary and
secondary school children / adolescents from two counties before the outbreak started (wave 1, early November 2019) and 2 weeks after school reopening (wave 2, mid-May 2020) in an area of China with low risk of COVID-19. 1389 children recruited 1271 completed info for W1. 1241 W2, response rate 93.1%. Mean [SD] age, 12.6 [1.4] years; age range, 9.3–15.9 years; 736 [59.3%] male). |
NSSI
Suicidal thoughts Suicide plans |
NSSI (42.0% in 2020 vs 31.8% in
2019; aOR, 1.35 [95% CI, 1.17-1.55]; P < .001), suicide ideation (29.7% vs 22.5%; aOR, 1.32 [95% CI, 1.08-1.62]; P = .008), suicide plan (14.6% vs 8.7%; aOR, 1.71 [95% CI, 1.31-2.24]; P < .001), and suicide attempt (6.4% vs 3.0%; aOR, 1.74 [95% CI, 1.14-2.67]; P < .001). OR adjusted for sex, body mass index, self-perceived household economic status, family cohesion, parental conflict, academic stress, parental educational level, family adverse life events, self-perceived health, sleep duration, and sleep disorders |
For NSSI, asking ‘In the past 12 months,
have you ever harmed yourself in a way that was deliberate, but not intended to take your life?’. Suicidal ideation, plans and attempts- from the 2013 Youth Risk Behaviour Surveillance System in the USA Pre-covid data Total number of children in years 4–8 not given so not sure of % recruited and therefore representativeness Seasonal variations and secular trends not accounted for. Peer reviewed |
Table 3. Summary of social media platform posts studies.
| Authors | Geography | Data used | Outcome | Conclusions | Comment/ Limitations |
|---|---|---|---|---|---|
| Low et al., 2020 | Demographic information
is unknown but Reddit users are predominantly American (49.9%) |
Reddit Mental Health Dataset
including posts from 826,961 unique users from 2018 to 2020. |
Using unsupervised clustering,
they found the suicidality and loneliness clusters more than doubled in the number of posts during the pandemic. The Reddit support groups for borderline personality disorder and posttraumatic stress disorder became significantly associated with the suicidality cluster The suicidality cluster doubled in size and a new cluster surrounding self-harm emerged. |
Using natural language
processing (NLP) on text from some of the world’s largest mental health support groups it is possible to identify mental health problems as they emerge in real time and to identify vulnerable sub-groups |
Such approaches could help
subreddit moderators track who is in need of assistance as well as well the concerns of specific communities are No formal diagnoses are made, reliant on what authors post Selection bias related to who posts as well as when they post and how they cope under different circumstances Peer reviewed |
| Saha et al., 2020 | USA | ∼60M Twitter streaming
posts originating from the U.S. from 24 March-24 May 2020, and compare these with ∼40M posts from the comparable period in 2019 |
A 20% increase in frequency of
posts that made reference to suicidal ideation was observed during 2020. |
Suicide risk is multifaceted.
More attention directed at population-scale mental healthcare, such as universal screening approaches |
Analysis of Twitter content makes
good use of readily available data and may reveal patterns and trends that are not easily discernible by conducting research using more traditional methods but what state in their posts does not necessarily reflect trends in suicidality in the population. Not peer reviewed. Pre-print. |
Table 4. Summary of studies using modelling approaches to estimate the possible impact of the pandemic on suicide rates.
| Authors | Country
/ region |
Data used to inform estimate | Model prediction | Comment / Limitations |
|---|---|---|---|---|
| Bhatia, 2020a | USA | Previous research modelling the association of
unemployment with suicide in the USA indicating a 1% rise in unemployment was associated with a 1% rise in suicide. Assumes unemployment in the USA has risen from 3.8% to over 20% |
7444 additional suicides in the following 2
months There were approximately 48,000 suicides in USA in 2018, so this equates to a predicted 15% rise in suicides in the USA. |
No account for potential impacts of pandemic other
than via unemployment rises Duration of unemployment rises uncertain Pre-print, not peer reviewed. |
| Bhatia, 2020b | USA | Meta-analysis of longitudinal studies investigating
the association of duration of unemployment with risk of suicide: used estimate of 2.5 fold increase in risk during 1–5 years of unemployment, derived from one Swedish and one Finnish cohort. National bureau of Health statistics: age adjusted suicide rates US Dept of Labour: weekly unemployment claims US Bureau of Labour Statistics: are distribution of workforce |
Estimated 9,786 additional suicides per year
There were approximately 48,000 suicides in USA in 2018, so this equates to a predicted 20% rise in suicides in the USA |
Estimate of the association between unemployment
and suicide derived from person-based studies investigating long-term unemployment and risk of suicide; this may over-estimate association in the context of economic recession Unclear whether age specific suicide risks were applied to the unemployment data – these were not reported in meta-analysis and text of paper contradictory No account for potential impacts of pandemic other than via unemployment rises Pre-print, not peer reviewed. |
| Kawohl & Nordt, 2020 | World | Previous research modelling the association of
unemployment with suicide in 63 countries (2000– 2011). International Labour Organisations (ILO) Predicted job losses (March 2020) of between 5.3 to 24.7 million |
Between 2135 and 9570 extra suicides per
year worldwide. i.e. a 0.3% to 1.2% rise |
No account for potential impacts of pandemic other
than via unemployment rises Duration of unemployment rises uncertain Research letter, probably not peer reviewed. |
| McIntyre & Lee, 2020a | USA | The authors analysed theassociation of
unemployment with suicide in the USA (1999–2018) and reported a 1% rise in unemployment was associated with a 1% rise in suicide. Three scenarios for changes in level of unemployment a) unchanged at 3.6%(2020), 3.7% (2021); b) rise to 5.8% (2020) and 9.3% (2021); c) rise to 24% (2020) and 18% (2021). |
Scenario b) associated with a 3.3% rise in
suicide in 2020–21 Scenario c) associated with an 8.4% rise in suicide in 2020–21. |
Usefully models the potential impact of two different
unemployment rate rises. No account for potential impacts of pandemic other than via unemployment rises Duration of unemployment rises uncertain Peer reviewed |
| McIntyre & Lee, 2020b | Canada | The authors analysed the association of
unemployment with suicide in Canada (2000–2018) and reported a 1% rise in unemployment was associated with a 1% rise in suicide. Three scenarios for changes in level of unemployment a) minimal change at 5.9%(2020), 6.0% (2021); b) rise to 8.3% (2020) and 8.1% (2021); c) rise to 16.6% (2020) and 14.9% (2021). |
Scenario b) associated with a 5.5% rise in
suicide in 2020–21 Scenario c) associated with a 27.7% rise in suicide in 2020–21. |
Usefully models the potential impact of two different
unemployment rate rises. No account for potential impacts of pandemic other than via unemployment rises Duration of unemployment rises uncertain Peer reviewed |
| Moser et al., 2020 | Switzerland | Used published data on increased risk of
suicide amongst a) prisoners in shared cells (3 fold increased risk) and b) prisoners in solitary confinement (27 fold increased risk) as indicators of risk of lock down on a) multi-person households and; b) single person households. Data on the annual number of suicides in Switzerland and the proportion of Swiss people living alone (16%) and in shared households (84%). |
Estimate 1523 additional suicides.
Based on an estimate the 1043 recorded suicides in Switzerland in 2017 this equates to a more than doubling in suicides deaths |
The team modelled the impact of COVID-19
pandemic on multiple outcomes as well as suicide. Prison confinement is probably not a good proxy for effects of lockdown. High suicide rates in prisoners are due to multiple factors e.g. age and gender profile; high levels of psychiatric morbidity rather than impacts of confinement. Other potential factors e.g. rises in unemployment not included in models Pre-print, not peer reviewed. |
Table 5. Summary of studies assessing service utilisation.
| Authors | Country /
region |
Data used | Outcome | Findings | Comment / Limitations |
|---|---|---|---|---|---|
| Capuzzi et al., 2020 | Italy | Emergency psychiatric evaluations at
psychiatric emergency rooms in two centres in Lombardy, serving a population of approx. 850,000 in two equivalent periods pre (Fri 22 Feb 2019-Sun 5 May 2019) and following the first COVID-19 case in Italy up to end of first phase of lock-down (Fri 21 Feb 2020 to Sun 3rd May 2020). Data obtained from hospital registers. |
Suicide
attempts/self- harm |
Period A (2019) 388 total attendances,
including 68 (17.5%) for self-harm/suicide attempt Period B (2020) 225 total attendances, including 59 (26.2%) for self-harm/suicide attempt. Whilst absolute number of SH/SA cases lower, the difference in number as a proportion of total cases was somewhat higher in age/sex adjusted models (aOR 1.48 (0.97 to 2.28) |
Hospital based study from two
centres Peer reviewed |
| Chen et al., 2020 | England, UK | Data obtained from Trust hospitals clinical
record systems. People using or referred to inpatient and community MH services (including psychological therapy services) in Cambridge and Peterborough - population approx 860,000. Data for Liaison psychiatry referrals for SH/Suicide attempt/ cover 11 March 2014 - 30 August 2020. Data also presented for suicidal thoughts, but data were combined with “low mood” |
Intentional drug
overdose and self-harm |
A marked reduction (p<0.001) in liaison
psychiatry referrals for intentional drug overdose, self-harm and suicidal thoughts occurred after 23 March (lockdown). The proportion of referrals returned to pre-lockdown levels by May/June 2020. |
Liaison team referral only (not all ED
attendances) at a single hospital. Liaison psychiatry referral pathways may have changed as a result of COVID-19 No detailed demographic analysis of referrals as the paper focused on a wide range of mental and physical health presentations. Single area in England. Peer reviewed |
| Dragovic et al., 2020 | Australia | Western Australia (WA) North Metropolitan
Health Services EDs were extracted from the Emergency Department Data Collection database. These 3 EDs serve a population of approx. 800,000 persons. Attendances over the period January to May 2020 were compared to those that occurred over the same calendar month periods during 2019. |
Suicide
attempts/self- harm |
7140 attendances (5522 persons) over the
two study periods. Suicidal and self-harm presentation decreased by 26% to previous year |
Attendances at three hospitals but
WA has low population density and went into stringent lockdown early - hence findings may not be generalisable to other Australian states or other countries; routinely collected healthcare data are large and complete, but they lack rich contextual detail. Peer reviewed |
| Gonçalves-Pinho et al., 2021 | Portugal l | People attending a Psychiatric Emergency
Department in a tertiary hospital in North Portugal serving a population of approximately 3 million people. Attendance between March 19th and May 2nd 2020 (when "emergency state" / restriction of movement existed in Portugal in response to COVID-19) compared with same dates in 2019 |
“Suicide
and self- inflicted injury presentations” to psychiatric ED |
Between March 19
th and May 2
nd 2020,
a significant reduction was identified in presentations of “suicide and intentional self-inflicted injury” to a metropolitan psychiatric ED, compared to the same period in 2019: N=36 v 81, a 55.6% reduction. |
Based on attendances at a single
hospital. Unclear if codes include people with suicidal thoughts as well as acts. Peer reviewed |
| Hernández-Calle et al., 2020 | Spain | Electronic health records examined at a major
general hospital in Madrid, Spain: November 2018 to April 2020. |
Suicidal
thoughts |
During March-April 2020, significantly
fewer psychiatric emergency department visits due to suicidal ideation were reported compared to the same period in 2019. |
Data only shown in a graph.
Single centre study - findings may have limited generalisability. Peer reviewed |
| Hewson et al., 2020 | UK | 31 prisons in UK
Internal reports from Safer Custody Units in 31 prisons where healthcare is provided by CareUK (Russell Green, personal communication) |
Suicide
attempts/self- harm |
After lockdown there were fewer
implementations of Assessment, Care in Custody and Teamwork (ACCT) processes; to initiate care- plans for prisoners considered at risk of self-harm or suicide. Across the 31 prisons, there were 1079 ACCTs implemented in February 2020 compared to 828 in April 2020, a fall of just under 25%. Analysis of data for 8 prisons indicated that there were falls in incidents of self-harm, decreasing by a third from 324 in February 2020 to 214 in April 2020. |
No gender breakdown (female
prisoners in the UK generally have much higher rates of self-harm than male prisoners) Unclear the basis of the selection of the 8 prisons with self-harm data Peer reviewed editorial |
| Jacob et al., 2020 | Australia | Single trauma centre in Australia, serving a
population of 1.5 million. Compared mean number of trauma admissions during March and April during years 2016 to 2020 |
Self-harm | During March and April 2020 a significant
decrease in total number of trauma- related admissions was observed, but no significant difference in admissions following self-harm was seen. |
Mean no. of admissions examined
before and during the Covid-19 public health emergency. Findings from a single centre may not be generalisable. The study was evidently under-powered for examination of mean monthly self- harm admissions. Peer reviewed |
| Karakasi et al., 2020a | Greece | Records of psychiatric emergency cases
presenting at the psychiatric emergency department of AHEPA University General Hospital of Thessaloniki during the following equal time intervals: 1 March to 15-May 2019, 15November 2019 to 31 January 2020, 1 March to 15 May 2020. |
Suicide
attempts/self- harm |
During the restrictive measures in Greece
(March – May 2020), the number of hospital presenting emergency psychiatric incidents fell by half (p < 0.01). The number of suicide attempts was higher in March- May 2020 (n=7) compared to the same period in 2019 (n= 5) and Nov 2019-Jan 2020 (n=4) |
Data from a single hospital
Small numbers Letter. Uncertain if peer-reviewed |
| Lersch, 2020 | USA | Emergency calls (911) to Detroit Police
Department for services between 26th Feb (first reported case COVID in city) and 27th April 2020. Comparison with 2017–2019 and also number of COVID-19 cases in the city. |
Suicide threats
and suicides in progress |
In the time period of interest during the
pandemic in 2020, the number of 911 calls for mental health issues was the lowest of the 4 years (2017–2020), declining by 16% from 2019 to 2020. However, the number of calls for suicide threats declined in 2020, while the number of calls for suicides in progress remained relatively stable over the 4-year period. No significant correlations between daily number of COVID-19 cases in the city and the number of calls from mentally ill persons, but as the number of COVID-19 cases increased there was a decline in calls for suicides in progress, but a significant inverse correlation between numbers of COVID-19 cases and threats of suicide calls (Pearson’s r=0.394) and a similar but non-significant relationship with calls for suicides in progress. In local area analysis, “some of the ‘hotspots’ for suicide threats were in areas of higher rates of COVID-19 cases”. |
Interesting analysis by numbers
of COVID-19 cases, including by locality. Single city. Data are early and may not be complete for COVID-19 cases. Unclear if peer-reviewed |
| McAndrew et al., 2020 | Ireland | Electronic health records for the emergency
department (ED) of a large teaching hospital in Dublin were examined during the first 8 weeks of the Covid-19 emergency (from 16th March to 10th May 2020). Comparative data for 2018 and 2019 were also examined. |
Suicide
attempts/self- harm, Suicidal thoughts |
A 21% reduction in the frequency of
psychiatric emergency presentations was observed, although the proportion of presentations with suicidal ideation or self-harm as factors remained unchanged. The observed reduction was largely due to a reduce attendance frequency during 'normal' hours. |
Electronic health record studies are
not prone to selection or self-report information biases. Further research examining patterns of emergency psychiatry presentations during COVID-19 could identify risky / vulnerable groups of people who have not been seeking help during a crisis. Similar studies from other countries and with extended follow-up periods are needed to build up a comprehensive picture of these temporal patterns. Peer reviewed |
| McIntyre et al., 2020 | Ireland | Self-harm referrals to Liaison Psychiatry team
in a single tertiary care hospital in Gallway Ireland. Contrast 1 March 2020–31 May 2020 with the same period in 2017–2019 |
Self-harm
presentations to a general hospital. |
Between March-April 2020, a significantly
lower proportion of self-harm presentations (-35%) to the hospital was reported, compared to the same period for 2017–2019. At the end of May, similar proportions of self-harm presentations were reported compared to previous years. |
Single hospital study. Incidence
based on referrals to liaison psychiatry - may under-estimate total hospital presenting cases. Liaison psychiatry referral pathways may have changed as a result of COVID-19. Peer reviewed |
| Olding et al., 2021 | England, UK | Trauma patients with penetrating injuries
who were treated at King's College Hospital in London, 23rd March to 29th April 2020 compared to the same period in 2018 and 2019. |
Self-harm (self-
inflicted injuries |
Whilst the incidence of all types of
penetrating trauma appeared to have fallen by 35% during the early lockdown period), the number of self-harm episodes increased from n=1 in 2018 to 5 in 2019 and 8 in 2020 |
Small, single site study. Crude
analytical approach. Number of self- harm cases too small to draw any strong conclusions Peer reviewed |
| Pignon et al., 2020a | France | Emergency psychiatric consultations from
three psychiatric emergency centres from first four weeks of lockdown (started March 17th 2020) and corresponding weeks 2019 |
Suicide
attempts |
During the four first weeks of lockdown,
553 emergency psychiatric consultations were carried out, less than half (45.2%) of the corresponding weeks in 2019 (1224 consultations). Total suicide attempts decreased in 2020 to 42.6% of those in 2019. |
Peer reviewed publication now
published, Pignon et al., 2020b |
| Rajput et al., 2020 | England, UK | Trauma admissions to a single level 1 trauma
centre in Liverpool using data from a trauma research network database. Compared three 7-week periods: (1) Lockdown: 23 March 2020–10 May 2020) (2) Pre-lockdown: 7 weeks prior to lockdown (27 January 2020–15 March 2020) (3) Pre-lockdown 2019: 7 week equivalent period in 2019 (25 March 2019–12 May 2019) |
Suicide
attempts/self- harm |
Total trauma centre attendances fell
during lockdown: 2019: n=194; 7 weeks pre lockdown 2020 n=173; during lockdown n=121 Equivalent numbers for self-harm were: 20 (2019); 24 (pre-lockdown 2020); 14 (lockdown 2020): i.e. 30% fall vs 2019. |
Small sample size; no assessment of
any change in socio-demographic characteristics of self-harm; possible changes due to service re-configurations in response to COVID. Peer reviewed |
| Rhodes et al., 2020 | USA | Trauma registry data of attendees at a Level 1
trauma centre in S Carolina, USA Jan 1-May 1 2019 compared to Jan 1 - May 1 2020 (lockdown April 8 th – May 1 st 2020). |
Suicide
attempts and self-harm, including specific methods |
Some evidence of rise in suicide attempts:
2019: 6 (0.6% of all presentations); 2020: 11 (1.4%) (p=0.079), including ‘self- harm by jumping’: 2019: 0 (0%); 2020: 5 (0.6%); p=0.011). No change in other ‘self-harm’ presentations: gun: 2019: 4 (0.4%); 2020: 4 (0.5%) (p=0.716); knife: 2019: 2 (0.2%); 2020: 1 (0.1%) (p=0.719), nor in acts of ‘Undetermined intent’: 2019: 18 (1.8%); 2020: 6 (0.8%) (p=0.064). |
Most of the period studied (15 of
the 18 weeks) in 2020 preceded lockdown. Small numbers and no specific data on suicide attempts during the post-lockdown period. The statistical comparison of suicide/SH episodes compared these episodes as a % of total attendances, rather than changes in absolute numbers. Peer reviewed |
| Sade et al., 2020 | Israel | Pregnant women admitted to high risk
pregnancy units between 19 March 2020 and 26 May 2020 (the strict isolation period of the pandemic) (n=90) compared to those hospitalised to these units between November 2016 and April 2017 (n=279) |
Suicidal
thoughts assessed using the Edinburgh postnatal depression scale (EPDS) |
Prevalence of suicidal thoughts was similar
pre (5.0%) vs during (8.6%) pandemic (p = 0.221). OR in multivariable logistic regression model, controlling for maternal age, adjusted OR 1.8, 95% CI 0.71–4.85, p = 0.203. |
Admission criteria may have
changed post pandemic (although admissions per month similar ~ 45/month Relatively small sample Select sample - pregnant women - generalisability to wider population uncertain. Pre-pandemic data collected in Nov 2016-April 2017 - 3 years previously - no account of any secular trends (also seasonal difference in collection period). Peer reviewed |
| Sheridan et al., 2021 | USA | Emergency department visits for mental
health issues to a single tertiary care pediatric hospital in Portland, Oregon April 1 2019 up to 29 April 2020 |
Suicidal patients | Department dealt with 14108 patients in
2019. 16 suicidal patients seen in April 2020 vs. 46 in April 2020 (a 65% fall) |
Before / after lock down
comparison, time trend analysis Used routinely available data Data on suicidal patients only specified for 1 month. One tertiary centre so not generalisable. Peer-reviewed |
| Smalley et al., 2021 | USA | Attendees with suicidal thoughts and alcohol
issues across 20 diverse EDs in a large Midwest integrated healthcare system with >750,000 ED visits annually. All behavioural health (BH) visits were collected for 1-month (March 25 th to April 24, 2020) following “stay at home” orders (lockdown). ICD-10 codes were used to identify visits associated with suicidal thoughts. The same parameters were used to collect data for the same time period for 2019. |
Suicidal
thoughts ICD coded by hospital staff |
Comparing 2020 with the same period in
2019, there was 44.4% decrease in overall ED visits and 28.0% decrease in BH visits. Attendances of individuals with suicidal thoughts decreased by 60.6% in 2020 (n=451) vs. 2019 (n=1144). As a percentage of all ED attendances, suicidal thoughts attendances decreased from 2.03% in 2019 to 1.44% in 2020. |
Alternative avenues for help-
seeking not included. But highlights importance of improving access for vulnerable populations during a pandemic. Included only one month in 2019 and one in 2020. Letter to editor, probably not peer reviewed |
| Titov et al., 2020 | Australa | Callers / website visits to "Mindspot" - national
digital MH service in Australia. Compared caller volume and characteristics 1- 28 Sept 2019 (n=1650) vs. 19 March - 15 April 2020 (n=1668) |
Suicidal
thoughts question from PHQ-9 |
No change in prevalence of: a) suicidal
thoughts (30.6% in September 2019 vs. 27.5% in March-April 2020; p=0.08), or b) suicidal intentions or plans (3.7% v 2.9% post p=0.27) |
Clinical / helpline sample - not
population based. Possible seasonal differences- September contacts vs. March-April Evidence of increased contact volume to a digital service. Peer reviewed |
| Walker et al., 2020 | USA | ED attendances (adult and pediatric) from
an integrated multiple hospital / ED system. n=18 EDs across several states. Diagnoses via electronic health records. Pandemic period (17 March 2020 to 21 April 2020) compared to same period in 2019 (17 March 2019 to 21 April 2019) and 36 day pre- pandemic period in 2020 (9 Feb 2020 to 16 March 2020) |
Suicide
attempts/self- harm |
Total ED attendances fell by around 50% during the period
of "the broad institution of distancing measures in response to the COVID-19 pandemic". Likewise, total ED attendances with "suicide" diagnosis fell by around one third during pandemic period: 17 March 2020 to 21 April 2020: n=36 (0.2% of total attendances) vs. 17 March 2019 to 21 April 2019: n=59 (0.2% total attendances) 9 Feb 2020 to 16 March vs. 2020: n=64 (0.2% total) |
Hospital presentations only
Only includes first 36 days of distancing measures. Peer reviewed |
Table 6. Summary of studies assessing suicide rates.
| Authors | Geography | Data used | Conclusions | Comments/Limitations |
|---|---|---|---|---|
| Acharya et al., 2020 | Nepal | News reports of police data on suicides
in Nepal 2019–2020 |
April 2020-mid July 2020: 1233 suicide deaths
Feb-March 2020: 414 suicide deaths. Report 414 suicides /month pre-lockdown vs. 559/month after lockdown (a 35% rise) |
Paper uses newspaper reporting of police suicide
statistics as primary source of data, so may not be reliable. Letter to editor, probably not peer reviewed |
| Calderon-Anyosa & Kaufman, 2020 | Peru | Suicide deaths reported by the Peruvian
National Death Information System between 1st January 2017 and 28th June 2020. |
Interrupted Time Series (ITS) analysis.
Suicide deaths fell sharply in males and females from the start of the lockdown period (March 16 2020) |
Authors used appropriate time series methods
Only 80% of all deaths are registered by the Peruvian National Death Information System. It is unclear whether cause of death assignment is time-lagged in Peru. Pre-print. Not peer reviewed |
| Isumi et al., 2020 | Japan | Suicide statistics published by the
Ministry of Health, Labor and Welfare for children (aged <20 years) Jan 2018-May 2020 |
Investigated the impact of school closures (March–
May 2020) by comparing these months with the same period in 2018 and 2019 using Poisson regression. In 2018 and 2019, suicide rates tend to increase from March to May; however, suicide rates from March to May in 2020 appeared to decrease slightly. Compared to March to May 2018 and 2019, no strong evidence of an increase in suicide rates during these months in 2020 (the school closure period): Incidence rate ratio =1.15, (95% CI 0.81 to 1.64). |
Analysis did not account for possible underlying
temporal trends in suicide using time-series approaches. Publicly available national statistics. Possibly too short a timespan to assess impact on child suicides. Suicides among children and adolescents reportedly peak at the beginning of school semesters in Japan, suicide rates may have increased when school restarted in June 2020. Peer reviewed |
| Pokhrel et al., 2021 | Nepal | News reports of police data on suicides
in Nepal 2019–2020 |
Report a 25% rise in suicide deaths in the lockdown
period (after mid-March 2020) compared to pre- lockdown. 1647 suicides between mid-March 2020 and 27 June 2020. |
Data derived from newspaper reporting of police
suicide statistics as primary source of data, so may not be reliable. Letter, may not have been peer reviewed. |
| Poudel et al., 2020; | Nepal | News reports of police data on suicides
in Nepal 2019–2020 |
Report a 20% rise in suicide deaths In the first month
of lockdown (from 24 March) (487 suicides vs. 410 in mid-February to mid-March 2020). Since the start of lockdown up to 6 June, there were 1,227 suicides (16.5/day) compared to 5,785 (15.8/day) in the same period in 2019 |
Data derived from newspaper reporting of police
suicide statistics as primary source of data, so may not be reliable. Peer reviewed |
| Sakelliadis et al., 2020 | Greece | Autopsies carried out at the University
of Athens March 17th–April 15th 2019 vs. March 17th–April 15th 2020 (the first month of lockdown |
Total autopsies - 125 in 2019 ; 105 in 2020. The
number of suicides and undetermined deaths were similar in 2019 vs. 2020: suicides: 6 (2019) vs 4 (2020); deaths of undetermined intent 4 (2019) vs. 5 (2020). |
Small numbers of deaths.
Possible changes / delays in death investigation during COVID-19? Peer reviewed |
| Singh et al., 2020 | Nepal | News reports of police data on suicides
in Nepal 2019–2020 |
Suicide deaths rose by 20% in Nepal during period
of Covid-19. Within the first 74 days of lockdown on average 16.5 people per day died by suicide vs. 15.8 per day in 2019 |
Paper uses newspaper reporting of police suicide
statistics as primary source of data, so may not be reliable. Letter, may not have been peer reviewed. |
| Tanaka & Okamoto, 2020 | Japan | Suicide statistics (all ages) published
by the Ministry of Health, Labor and Welfare. July 2016 – June 2020 |
Compared Use Feb-Jun 2020 (COVID period) vs. and
Feb-Jun 2016–19 (pre-COVID). Suicides fell by 13.5% (95% CI -17.5 to -9.5%) in the COVID period. Decline is greatest in males and in adults compared to children (<20 years) and older people (>70 years). No evidence of an adverse effect on students during school closure (rates fell). |
Publicly available national statistics. The authors cite
the Japanese government’s "generous subsidies, reduced working hours, and fewer school sessions" as possible explanations for lack of adverse effect. Pre-print. Not peer reviewed. |
| Ueda et al., 2021 | Japan | Suicide statistics (all ages) published
by the Ministry of Health, Labor and Welfare. Jan 2017-August 2020 |
During the state of emergency (April-May 2020),
suicides declined by 20%. By August suicide numbers were 7.7% higher than the average for August 2016–19. The largest rises were in females (mean of 532 suicides in August 2017–19 vs. 651 in 2020). Similar trajectories in all age groups, but the largest rise was in those aged <40 years (63% higher in 2020 vs 2017–19). Groups of greatest concern: students (47% rise in university student suicides August 2020 vs August 2017–19) and housekeepers. |
Authors speculate greater rise in women could be
because they largely worked in the sectors most affected by pandemic related closure (retail and travel) The analysis did not account for possible underlying temporal trends in suicide using time-series approaches. the authors compare the percentage change in a single month in 2020 vs figures for the same month in 2017–19. Pre-print. Not peer reviewed |
Study populations
Sample sizes ranged from two individuals in a number of case series ( Kapilan, 2020; Mamun et al., 2020b; Pirnia et al., 2020; Sahoo et al., 2020) to 60 million Twitter posts ( Saha et al., 2020). Most studies included both male and female participants, except the studies reported by Wu et al. (2020a) and Sade et al. (2020) which were conducted in pregnant women.
Outcomes
Seven of the 24 case series (described in 25 papers) focused on a mix of outcomes including suicide attempts (n=2), suicide deaths (n=14) and suicidal thoughts (n=1). Of the 15 cross-sectional surveys five assessed suicidal thoughts alone, others collected data on various combinations of suicidal/self-harming behaviour or thoughts. A range of validated questionnairres were used to assess suicidal thoughts ( Table 2). Five surveys used the single item from PHQ-9 ‘Have you had thoughts that you would be better off dead or of hurting yourself in some way’ over the last 2 weeks. Wang et al. (2020b) assessed responses to this question in a symptom network analysis.
Summary of study findings: Case series
We identified 24 case series of suicide attempts and suicide deaths ( Table 1). Fourteen (58.3%) of these used news reports as their data source ( Bhuiyan et al., 2020; Boshra et al., 2020; Dsouza et al., 2020; Griffiths & Mamun, 2020; Kapilan, 2020; Kar et al., 2020; Mamun & Ullah, 2020; Mamun et al., 2020a; Mamun et al., 2020b; Rahman et al., 2020; Rajkumar, 2020; Shiob et al., 2020; Syed et al., 2020; Thakur & Jain, 2020) and are unlikely to be representative of general population suicide rates. Several overlap in terms of the information used, such as two letters to the editor about celebrity suicides in India ( Kar et al., 2020; Mamun et al., 2020b), and many lack detailed information about the range of contributing factors. Whilst most case series focused on suicdes in the general population, some focussed on specific groups, such as psychiatric patients (e.g. Jolly et al., 2020), healthcare professions (e.g. Kapilan et al., 2020), patients with COVID-19 (e.g. Nalleballe et al., 2020), couple suicides ( Griffiths & Manun, 2020) and alcohol-related deaths (e.g. Ahmed et al., 2020).
Many reasons for COVID-19 related suicide or suicide attempts were suggested in the case series with conclusions often derived from a journalist’s report of the death. Contributory factors reported included fear of contracting the disease or of passing it on to others, reactive psychoses, financial or economic issues, loneliness and isolation due to quarantine, stress among health professionals, the uncertainty around when the pandemic would end, misinterpretation of fever as COVID-19, contracting COVID-19, an inability for migrants to return home, frustration and the stigma of a (possibly perceived) positive result, which resulted in harassment or victimisation by others in the community. In the largest case series from India (n=72 suicide deaths), Dsouza et al. (2020) reported that the most commonly occurring antecedents to suicide were fear of infection (n=21) and financial crisis (n=19). Two studies reported specifically on the consequences of alcohol withdrawal due to lockdowns ( Ahmed et al., 2020; Syed et al., 2020).
In the USA, four case reports described stressors for adolescents which include inability to see friends, arguments with parents, unresolvable misunderstandings over social media, academic stress, and feelings of isolation ( Jolly et al., 2020). In a case series of adults across three hospitals in Doha, Qatar, three patients (out of 50 patients with COVID-19 receiving a psychiatric diagnosis) self-harmed as a reaction to the pandemic ( Iqbal et al., 2020). A study of TriNetX records of people with COVID-19 (n=40,469) found that 0.2% (62 individuals) had suicidal thoughts recorded, although clinicians may not have systematically asked about suicidality ( Nalleballe et al., 2020).
Summary of study findings: Cross-sectional surveys and cohort study
There were 13 articles describing cross-sectional surveys / cohort studies of two or more waves or one wave surveys where comparisons were explicitly made with appropriate pre-pandemic measures; or included comparative data between COVID-19 positive individuals and unaffected comparison individuals ( Table 2). Six studies present repeat survey data, with measures recorded during, as well as before, the pandemic ( Hamm et al., 2020; Hamza et al., 2021; Raifman et al., 2020; Winkler et al., 2020; Wu et al., 2020b; Zhang et al., 2020). Raifman et al. (2020) compared two nationally representative samples of US adults (one from 2017/18 and one from 2020 during the COVID-19 pandemic) using different survey methodologies. They found that suicidal ideation had increased more than fourfold in low-income households, particularly in those with difficulty paying rent, job loss and loneliness. Similarly, Winkler et al. (2020) reported on a repeated, robustly-sampled, nationally representative survey in the Czech Republic using baseline data from 2017 and found that suicide risk, as measured by the Mini International Neuropsychiatric Interview, increased from 3.9% in November 2017 to 11.9% in May 2020. Both Raifman et al. (2020) and Winkler et al. (2020) used somewhat different data collection approaches before and during the pandemic. Two other studies from China ( Wu et al., 2020b; Zhang et al., 2020) reported increases in relevant outcomes during the pandemic compared with before. The cohort study by Zhang et al. (2020) reported increases seen in nonsuicidal self-injury (NSSI), suicidal thoughts, suicidal plans, and suicide attempts in primary and secondary school children pre- compared with post-pandemic. Neither Hamm et al., 2020 (trial participants with depression aged >60years) nor Hamza et al., 2021 (students) found clear evidence of increased risk of suicidal ideation (older adults) or NSSI (students) during the pandemic.
Three additional articles, other than Raifman et al., 2020 and Winkler et al., 2020, reported cross-sectional surveys in the general population. Two of these used web based recruitment ( Iob et al., 2020; Sueki & Ueda, 2020) with non-probability quota sampling or weighting, and one ( Wang et al., 2020b) used a Chinese online platform providing functions similar to Qualtrics. Participants were COVID-19 patients in three studies ( Wang et al., 2020a; Wu et al., 2020a; Zhao et al., 2020). Wang et al. (2020a) and Zhao et al. (2020) both reported higher levels of suicide-related outcomes in COVID-19 patients than general population (compared with the general population recruited through social media or from literature reports). In a general population sample that included people who reported having been diagnosed with COVID-19, Iob et al. (2020) found suicide/self-harm thoughts were more common in those with a COVID-19 diagnosis than in those not affected (33% vs 17%); likewise for suicide attempts (14% vs. 5%). Two surveys were conducted in university student populations ( Debowska et al., 2020; Hamza et al., 2020) from 11 universities, with predominantly female respondents. No statistical evidence of a rise in suicidal thoughts or self-injury was found over a number of waves of data collection. Surveys were targeted at specific populations in a further three studies ( Table 2): depressed patients ( Hamm et al., 2020); pregnant women ( Wu et al., 2020b); and school children ( Zhang et al., 2020).
Summary of study findings: Social media platform posts
Two studies ( Table 3) assessed posts on social media platforms, looking at Reddit ( Low et al., 2020; 50% USA users) and Twitter in the USA ( Saha et al., 2020). Both studies show marked increases in the proportion of postings related to suicidal thoughts and behaviours, and Low et al’s analysis of Reddit data identified a new cluster of posts about self-harm during the pandemic.
Summary of study findings: Modelling studies
We identified six studies ( Table 4) that have used modelling approaches to forecast the potential impact of the pandemic on future suicide rates ( Bhatia, 2020a; Bhatia, 2020b; Kawohl & Nordt, 2020; McIntyre & Lee, 2020a; McIntyre & Lee, 2020b; Moser et al., 2020). Three estimated the impact of the pandemic on suicide in the USA ( Bhatia, 2020a; Bhatia, 2020b; McIntyre & Lee (2020a), while others assessed the impact on suicide in Canada ( McIntyre & Lee, 2020b), Switzerland ( Moser et al., 2020) and worldwide ( Kawohl & Nordt, 2020).
The models suggest between a 1% rise ( Kawohl & Nordt, 2020, globally) and a 145% rise ( Moser et al., 2020, in Switzerland) in suicide deaths. Each was based on different assumptions, but the models largely focused on the well-characterised impact on suicide rates of periods of economic recession and rises in unemployment ( Chang et al., 2013; Stuckler et al., 2009). Unemployment rates are predicted to rise as a result of a post-pandemic recession, due to measures to control the spread of the virus on the wider economy and loss of work as many businesses have been forced to shut down.
Only one study modelled the effects of physical distancing measures on suicide rates ( Moser et al., 2020); it did this by using suicide rates in prisoners in group or single cells as a model for lockdown in a group or in isolation. The prison population is exposed to multiple other risk factors for suicide (e.g. increased prevalence of mental illness, substance misuse and low socioeconomic position) ( Humber et al., 2011; Rivlin et al., 2010), and this, coupled with the distinct differences between prison incarceration and the adoption of home quarantine procedures during the pandemic, means this model is likely to overestimate the potential impact of physical distancing measures on suicide risk in the general population.
Summary of studies’ findings: Service utilisation studies
We identified 20 service utilisation studies. Four of these addressed the impact of COVID-19 on suicidal thoughts only, thirteen included suicide attempts and/or self-harm, one suicidal thoughts, attempts and self-harm ( McAndrew et al., 2020), one suicide threats and suicides in progress ( Lersch, 2020), while in one the precise nature of the suicidal outcome was unclear ( Sheridan et al., 2021) ( Table 5). Most studies were conducted in the US (5) and the UK (4), three in Australia, two in Ireland and one study in each of the following countries: France, Greece, Israel, Italy, Portugal, and Spain.
Across the studies focusing on suicidal thoughts, the methodologies varied from studies of presentations to health/mental health services to callers/visits to a website, with wide-ranging sample sizes, from 1668 ( Titov et al., 2020) to 90 ( Sade et al., 2020); the latter including a specific sample of pregnant women. The studies showed either a reduction ( Chen et al., 2020; Hernandez-Calle et al., 2020; Smalley et al., 2021) or no change ( Sade et al., 2020; Titov et al., 2020) in presentations to health/mental health services or self-reported suicidal thoughts, with the majority making comparisons to the same time in 2019. The eleven studies examining the impact of COVID-19 on self-harm/suicide attempts used a variety of methodologies, including accessing data from health/mental health services, trauma registries, community-based services, emergency call services and the prison service. Where reported, the sample sizes ranged from 18,646 ( Walker et al., 2020) to 30 ( Olding et al., 2021). Eight studies reported a decrease in self-harm/suicide attempts during the first months of the COVID-19 pandemic ( Capuzzi et al., 2020; Chen et al., 2020; Goncalves-Pinho et al., 2021; Hewson et al., 2020; McIntyre et al., 2020; Pignon et al., 2020; Rajput et al., 2020; Walker et al., 2020). In two of these studies – both with somewhat longer post lockdown follow-up periods of 3–5 months ( Chen et al., 2020; McIntyre et al., 2020) – presentations had returned to pre-lockdown levels by the end of follow-up. Three studies reported an increase in self-harm / suicide attempts (Karakasi et al., 2020; Olding et al., 2021; Rhodes et al., 2020).
Pignon et al. (2020) reported a 54.8% decrease in overall psychiatric emergency consultations and a 42.6% decrease in self-harm/suicide attempts during the first 4 weeks of the lockdown in France compared with the same period in 2019. Likewise, Gonçalves-Pinho et al. (2020) identified a 55.6% decrease in presentations of “suicide and intentional self-inflicted injury” to a metropolitan psychiatric emergency department in Portugal in the period 19 th March to 2 nd May between 2019 and 2020. McIntyre et al. (2020) reported a 35% reduction in self-harm presentations to a general hospital in March-April 2020 in Ireland compared with the same period in 2017–2019; however presentations returned to pre-pandemic levels by the end of May. Another study in Ireland ( Mcandrew et al., 2020) also reported a reduction in psychiatric emergency presentations to the emergency department but no change in the proportion of presentations with suicidal thoughts or self-harm. In a study conducted by Hewson et al. (2020) in 31 prisons in the UK between February and April 2020, self-harm incidents decreased by one third between February and April 2020.
In contrast, whilst Olding et al. (2021) reported a reduction in the incidence of all types of penetrating trauma presenting to a UK hospital during the early period of lockdown, the number of self-harm presentations increased slightly (albeit on the basis of very low event counts). A similar pattern was identified by Karakasi et al. (2020a) in Greece, where between March and May 2020 a significant reduction was observed in individuals presenting as emergencies at hospital for psychiatric examination (the number of presentations for suicide attempts was 7 compared with 5 in the same period in 2019). Capuzzi et al. (2020) reported a rise in self-harm / suicide attempts as a proportion of total emergency department presentations in Italy, but this rise in the proportion of cases was in the context of falls in the absolute numbers of cases, set against reductions in total emergency department attendances.
A study of emergency police calls in Detroit, USA, (Lersch et al., 2020) showed that the number of general mental health calls declined after the onset of the pandemic in that city, while calls relating to suicides in progress remained relatively stable over the 4 year period. Calls involving suicide threats declined inversely to the increase in COVID-19 infections, although the authors noted some ‘hotspots’ within the city for both infection rates and suicide threats. A study of 31 prisons in the UK found that after lockdown there were fewer implementations of Assessment, Care in Custody and Teamwork (ACCT) processes to initiate care- plans for prisoners considered at risk of self-harm or suicide ( Hewson et al., 2020).
Summary of study findings: impact of COVID-19 on suicide rates
Nine reports, based on data from four countries – Greece, Japan, Nepal and Peru – describe changes in suicide rates in relation to the onset of COVID-19 and national lockdowns. A challenge with interpreting all the reports is the uncertainty over the extent to which official recording of suicides may have been affected by disruptions in death investigation and reporting due to COVID-19, although this is more likely to lead to under-estimation than over-estimation of suicide rates. Only one of the studies ( Calderon-Anyosa & Kaufman, 2020) used appropriate time series to take account of underlying temporal trends in suicide when comparing the COVID-19 period with earlier years/months.
The four reports from Nepal ( Acharya et al., 2020; Pokhrel et al., 2021; Poudel & Sedhai, 2020; Singh et al., 2020) were all based on news reports of police data on suicides, rather than on data obtained directly from Nepalese authorities and did not describe the strengths and weakness of the police data. They report between a 20% (Poudel & Sedhai, 2020) and 35% ( Acharya et al., 2020) rise in suicide in the first 3 months after lockdown compared with either preceding months or a similar period the previous year. These are marked rises, but without longer time series data it is not possible to determine the extent to which these were COVID-19 related or a possible continuation of pre-existing adverse trends. Three reports, based on Japan’s timely national suicide statistics, describe recent trends in Japanese suicide rates ( Tanaka & Okamoto, 2020 pre-print, Tanaka & Okamoto, 2021, final version; Isumi et al., 2020; Ueda et al., 2021). The most recent of these, using data up to October 2020, indicate that 14% falls in Japanese suicides in the early months of the pandemic (Feb-June 2020), were reversed during the second outbreak (July to October, 2020) increasing by 16% ( Tanaka & Okamoto, 2021). Increases in suicide rates were higher in females (especially housewives) and children and adolescents. Similarly compared with August in 2017–19, figures for August 2020 were increased by 7.7%, with rises particularly in females and people aged <40 years ( Ueda et al., 2021). An early report (data up to May 2020) provided some reassurance about the impact of public health measures/school closures on suicide rates in children (<20 years) in Japan ( Isumi et al., 2020). However, more recent data ( Ueda et al., 2021) flags a concerning rise amongst students and young (<40 years) people, particularly females. The numbers of deaths in the autopsy study from Athens ( Sakelliadis et al., 2020) is too small to reach any conclusion about the impact on suicide in Greece. Calderon-Anyosa’s (2020) study of suicide in Peru is reassuring, though details of potential impacts of COVID-19 on death registration in Peru are not provided.
Other studies
The three other studies investigated various risk groups, using case control and mixed methods approaches. Son et al. (2020) interviewed students from a single US university about the impacts of the pandemic on their mental health; some students described suicidal thoughts and the challenges they faced, one linked suicidal thoughts to being confined at home with their family and another to study-related difficulties. Cai et al. (2020) compared suicidal thoughts in Chinese medical workers dealing with COVID-19 patients and those not in contact with such patients. They found no evidence of increased levels of suicidal thoughts amongst those in contact with COVID patients. Lastly, Evans et al. (2020) studied the pandemic-related stresses felt by Australian families in free text responses to a questionnaire. One respondent, a father with three children described the extreme financial distress they faced with “our three businesses closing, we are eligible for none of the government support due to a tax debt and are looking at bankruptcy and selling our home as the only option. Both of us have had thoughts of suicide" (Quote from father of 3 children). ( Evans et al., 2020)
Discussion
Seventy-eight articles were included in this review, 49 more than in our review of studies published up to 7 th June 2020. All were based on observational studies. The majority of studies were case series or service utilisation studies from across the world. No studies were based on populations from sub-saharan Africa. Almost half of the articles did not appear to have been peer-reviewed, consisting mainly of pre-prints published before peer review, or research letters that may not have been peer-reviewed. In contrast to the last update ( John et al., 2020c) in which no studies reported on the change in incidence of suicide or suicidal behaviour after the onset of the pandemic compared with beforehand, we identified nine papers in this update, presenting data on studies from four countries which investigated the impact of COVID-19 on suicide rates. To date, the highest quality data come from Japan which utilises suicide records covering the entire population; these data indicate that the impact of COVID-19 on suicides rates may change over time and have varying effects on different sections of the population. Analysis of data from Peru used appropriate analytic techniques and reported a fall in suicides following the onset of the pandemic during the months March to September ( Calderon-Anyosa & Kaufman, 2020). Methodological limitations and the availability of data for only four countries limit our ability to assess the early impact of COVID-19 on suicide rates in this update.
Evidence published following our cut-off date for inclusion in this iteration of the review indicates there was no rise in suicide rates in the early months of the pandemic in high income countries ( John et al., 2020a). Since our 19 th October search, a further 13 studies analysing suicide trends in ten countries or regions within countries (Australia, Austria, Germany, Greece, Japan; Korea, Norway, Sweden, Thailand and the USA) have been published ( Ando & Furuichi, 2020; Bray et al., 2021: Deisenhammer & Kemmler, 2021; Faust et al., 2020; Karakasi et al., 2021; Ketphan et al., 2020; Kim, 2021; Leske et al., 2021; Mitchell & Li, 2021; Qin & Mehlum, 2021; Radeloff et al., 2020 and Radeloff et al., 2021; Rück et al., 2020; Vandoros et al., 2020). Four of these use appropriate time-series modelling approaches to control for underlying trends ( Leske et al., 2021, Australia; Faust et al., 2020, USA; Vandoros et al., 2020, Greece; Ando et al., 2020, Japan) – these report either no change or a fall in suicide deaths in the early months of the pandemic, although in keeping with Tanaka & Okamoto (2020); Tanaka & Okamoto (2021) and Ueda et al.’s (2021) analysis for Japan, Ando et al. (2020) report a rise in suicides in Japan since July associated with increased unemployment . In keeping with concerns from Nepal, data from Thailand’s Department of Mental Health indicate suicide numbers have risen during the pandemic ( Ketphan et al., 2020). Data from Connecticut, USA on suicides during the 10 weeks of stringent lockdown measures in the state indicate that whilst suicide rates fell during this period, the proportion of suicides amongst minority ethnic groups rose, highlighting the possibility that the pandemic may be having a disproportionately greater adverse impact on minority groups ( Mitchell & Li., 2021). A concern supported by a recent analysis from Maryland, USA. ( Bray et al., 2021).
The majority of the 13 included cross-sectional surveys were subject to methodological flaws in sampling methods and use of validated instruments. Nonetheless, there is evidence from at least three countries (China, Czech Republic and USA) of increases in suicidal/self-harm thoughts in the general population during the pandemic compared with pre-pandemic levels. Two robustly sampled general population, nationally representative cross-sectional surveys with pre pandemic baseline data from 2017/18 reported a three to four fold increase in suicide risk ( Winkler et al., 2020) and suicidal thoughts in low-income households ( Raifman et al., 2020), but differences in data collection approaches (i.e. face-to-face vs. on-line) may bias comparisons. Recent studies, with repeat measures of mental health outcomes since the start of the pandemic, also point to rising levels of suicidal thoughts during the pandemic ( O’Connor et al., 2020).
The review included 20 service utilisation studies (compared with only three in the previous update), the majority of which identified a drop in frequency of emergency department contacts for suicidal thoughts, behaviours and self-harm. An increase in contacts to a mental health digital platform was identified in one study ( Titov et al., 2020), but with no changes in contacts for suicidal thoughts. There have been several recently published service utilisation studies (Carr et al., 2020; Hawton et al., 2020a; Jollant et al., 2020) which reiterate and extend these findings. Jollant et al. (2020) report a 8.5% decrease in hospitalisation for self-harm, greater in females than males, in France in January to August 2020 compared with the same period in 2019. There was also an increase in use of some more lethal methods (firearms / jumping/ drowning) as well as a rise in in-hospital deaths and ITU admissions. Carr et al. (2020) report a 30% fall in consultations for self-harm in April to June 2020 in primary care and secondary care in the UK, the former a setting not explored in currently included studies. They highlight that the treatment gap for depression and anxiety was greater in working age adults, for practice populations in deprived areas, and for self-harm. A limitation of all studies based on hospital presentations is that they may not reflect community prevalence of suicidal thoughts and behaviours. This may be a particular issue if people were deterred from presenting to hospital because of fears of either over-burdening already stretched healthcare systems or of contracting the virus in these settings themselves. That said, those who present to services may be able to give some insight into whether COVID-19-related concerns are important. In one UK study, ‘stay-at-home’ related issues contributed to around half of cases, more so in males than females. The most frequent COVID-related factors were mental health issues, including new and worsening disorders, cessation, reduction or transformation of services (including absence of face-to-face support), isolation and loneliness, reduced contact with key individuals, disruption to normal routine, and entrapment ( Hawton et al., 2020b).
Modelling studies that aimed to predict the impact of the pandemic on national or global suicide rates produced widely differing estimates of the likely impact and most focused on predictions based on previous studies of the impact of changes in unemployment levels on suicide. These differences between model estimates were partly due to differences in modelling assumptions, which are themselves in turn associated with considerable uncertainty. Given the methodological limitations, the uncertainty of assumptions about how the economies of individual countries will be affected, as well as international differences in financial supports given to businesses and people out of work, these predictive exercises can at best only provide a guide as to where action and available suicide prevention strategies should be directed.
Studies of social media posts potentially provide another insight into the impact of the COVID-19 pandemic on suicide risk and have the potential to provide more-or-less real time assessments of changes in risk. The two studies we identified ( Low et al., 2020; Saha et al., 2020) reported heightened levels of suicide-related posting/suicidality. However, there are several limitations to this approach making these studies hard to interpret, including: self-selecting biases in respect of who contributes to these fora (and when); the unit of analysis being posts/tweets rather than individuals so multiple posts may be from the same individual; and the dissemination of misinformation; the demographic and clinical characteristics of the people making the posts are unknown; and whether comments reflect their own distress or more general concerns is uncertain.
It is also not clear whether mentions of suicide on social media posts map to actual rates of suicidal thoughts in the community and whether this changes in particular contexts and over time. The nature of the relationship (if any) between social media reports and behavioural change in the context of suicide needs to be better understood. Insights derived from such approaches may help deepen our understanding of the mental health challenges of the pandemic and how these may change over time. Future research could usefully try to segment the posts by individuals and sociodemographics to explore changes in sub-groups. Another potentially useful approach to assessing the impact on COVID-19 on population mental health and suicide risk is analysis of Google trends data ( Jacobsen et al., 2020; Knipe et al., 2020; Rana, 2020; Sinyor et al., 2020), but we excluded such studies from our review as we think that search data constitute an even weaker proxy for population mental health.
We identified 25 case series of suicide attempts and suicide deaths, 14 based on news stories in India, Bangladesh and Pakistan. Given the relatively low quality of case series in the hierarchy of evidence, often reflecting small numbers and selection bias, but more importantly the lack of comparator data, drawing any reliable inferences from these studies is inherently flawed. Furthermore, news reports report a non-representative sample of suicide deaths and often derive their information from bystanders and witnesses who are unlikely to know the full circumstances of the death ( Khan et al., 2009). However, in parts of the world without reliable suicide incidence data they may be the only source of information ( Khan & Hyder, 2006). Nevertheless, these studies highlight circumstances surrounding apparently COVID-19-related suicides and flag the potential importance of factors such as economic difficulties, fear of the disease, alcohol withdrawal and social isolation even in young people and children.
Only 14% (11/78) included studies specifically focussed on children and young people. An early report (data up to May 2020) provided some reassurance about the impact of public health measures/school closures on suicide rates in children (<20 years) in Japan ( Isumi et al., 2020). However, more recent data ( Tanaka & Okamoto, 2021; Ueda et al., 2021) flags a concerning rise amongst students and young ((<40 years) people, particularly females and children and adolescents during the second wave of the pandemic and school closure. Three were cross-sectional surveys with attendant methodological flaws. Two surveys were conducted in university student populations ( Debowska et al., 2020; Hamza et al., 2021) in 11 universities with predominantly female respondents. No statistical evidence of a rise in suicidal thoughts or self-injury was found over a number of waves of data collection. Wang et al’s (2020) network analysis of symptoms of anxiety and depression in young people highlighted an increasing connection between ‘too much worry’ and suicidal thoughts. It is challenging to assess how generalisable these findings from China are to other countries and other phases of the pandemic. If generalisable, it could point to some treatment targets that are more central to suicide risk, but this is not yet clear. Zhang et al’s (2020) cohort study reported pre-pandemic comparison data, with increases seen in NSSI, suicidal thoughts, suicidal plans and suicide attempts in primary and secondary school children post-pandemic. However the sampling frame was poorly reported so representativeness of the sample is challenging to assess. Only one of the service utilisation studies focussed on this age group ( Sheridan et al., 2021) but this was based in a single tertiary centre; although another study of a broader age range included them ( Walker et al., 2020). There were two case series focussed on children and young people ( Jefsen et al., 2020b; Jolly et al., 2020). The stressors identified for adolescents included the inability to see friends, arguments with parents, unresolvable arguments via social media, academic stress and feelings of isolation ( Jolly et al., 2020).
Only three included studies focussed on frontline healthcare staff. Two were case series (Kapilan et al., 2020; Rahmen et al., 2020) based on news reports of six or eight nurses deaths (i.e. there is potential duplication of reports of the same deaths). Factors reported as associated with deaths included: fear they had become infected; positive test result; being in quarantine; fearful of becoming infected; and “ extreme stress and mental disturbance”. The third, a case control study, reported that the prevalence of suicidal thoughts was no higher in medical staff who were in direct contact with COVID-19 patients, compared to those who had no direct contact ( Cai et al., 2020).
Strengths and limitations
The literature exploring COVID-19 and suicide deaths, suicidal behaviours, self-harm and suicidal thoughts is expanding rapidly. Since our last review end-date (i.e. between 7 th June 2020 to 19 th October 2020) we identified a further 4156 potentially eligible studies. While most of the published evidence that we identified in this update had important limitations there was a marked improvement in study quality compared with our last update. Importantly, a large volume of the literature remains not peer reviewed; some reports are pre-prints, so this may change, but a number are research letters. All included studies remain observational in design and thus potentially prone to multiple sources of bias (e.g., recall bias, selection bias, confounding).
A number of the studies included in this update used non-probability samples e.g. convenience samples of volunteers recruited via the Internet. Such studies tend to attract volunteers who have access to the internet, are already engaged in research or have an interest in the topic. When assessing suicidal thoughts and behaviours, those in most distress or with co-existing mental illness, as well as older people, may be less likely to participate. Therefore prevalence estimates and associations observed among healthy volunteers may not reflect associations that would be seen in representative samples ( Pierce et al., 2020). However, such study designs potentially provide potentially valuable information at the very early stages of a health crisis, where the timeliness of studies to inform policy and practice is important and repeated cross sectional studies provide valuable evidence about changing levels of population mental health and risk factors (e.g. O’Connor et al., 2020; Raifman et al., 2020). More consistent reporting of sampling frames, repeat survey and the use of validated measures will ensure they make a more meaningful contribution to the evidence base.
There is a paucity of research focussing or reporting on ethnic minorities within populations, children and young people, the bereaved and frontline health and social care staff, which needs to be addressed. Synthesis of findings across studies, and both between and within countries, is confounded by the timing of data collection; differences between studies may be due not only to methodological differences, but also differences in the extent and stringency of public health prevention measures (physical distancing), economic disruption and COVID-19 infection rates in the any population at the time data are collected. A final limitation of the review is that, due to resource limitations, we excluded grey literature (e.g. Fancourt & Steptoe, 2020; National Child Mortality Database, 2020)
Implications
There is thus far no clear evidence of an increase in suicidal behaviour or self-harm associated with the pandemic, nor with the measures taken to curb the spread of COVID-19, although signals from some repeated population surveys and suicide trend data from Nepal and Japan are concerning. There are suggestions of increased risk in people who have been infected with COVID-19, in line with findings from studies showing increased risk of mental health problems in survivors of COVID-19 ( Taquet et al., 2021). Declines in levels of hospital presentation for suicidal behaviour may reflect a real decline in suicidal behaviours early in the pandemic perhaps due to the recognised impact of periods of acute stress / national crisis (e.g. wars) on suicide rates or unmet need in the community, with people cautious about overburdening clinical services or of their own risk of contracting COVID-19 ( John et al., 2020a). There is a relative lack of high quality studies to inform prevention in Low and Middle Income Countries and in disadvantaged groups, although studies point to an emerging risk in the latter ( Mitchell & Li., 2021). There are, as yet, no studies that assess the effectiveness of strategies to reduce the risk of suicide deaths, suicidal behaviours, self-harm and suicidal thoughts, resulting from the COVID-19 pandemic; such research is urgently required.
Our living review provides a regular synthesis of the most up-to-date research evidence to guide public health and clinical policy to mitigate the impact of COVID-19 on risk of suicidality. However, the rapid growth of research in this area necessarily makes the reporting of the large volume of included studies brief. Therefore in the future we plan to publish timely updates focussed on specific topics like suicide rates, for instance, or in specific populations such as children and adolescents, those with confirmed COVID-19 or healthcare workers. Our future updates will also focus on studies investigating suicide deaths, suicide attempts and self-harm. We will no longer include studies: with suicidal thoughts and “suicide risk” as outcomes; modelling studies (since these have been superseded by studies based on suicide deaths) and those based on social media posts (because of the lack of evidence for diagnoses and self-selecting biases in respect of who contributes to these).
Dissemination of information
This living review, along with further updates, will be published via F1000Research. This review was registered on PROSPERO, with ID CRD42020183326. The protocol is available. All further data are publicly available via our Harvard Dataverse repository including all results of the continuous evidence surveillance and screening. Findings from the review will be widely disseminated through conference presentations, policy briefings, peer-reviewed publications, a project website ( https://covid19-suicide-lsr.info/), and traditional and social media outlets.
Study status
We are currently searching and screening on a daily basis.
Ethics and dissemination
Since this is a systematic review, ethical approval is not required.
Data availability
Underlying data
Harvard Dataverse: Full review data for: "The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review". https://doi.org/10.7910/DVN/7WZXZK (John & Schmidt, 2020)
This project contains the following underlying data:
- Screening_snapshot.csv (Screening progress for literature published before June 7th)
Extended data
Harvard Dataverse: Full review data for: "The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review". https://doi.org/10.7910/DVN/7WZXZK (John & Schmidt, 2020)
This project contains the following extended data:
LSR update tables and figures.docx (Tables and figures from this publication)
PRISMA.doc
Data regarding the Protocol are available via our Harvard Dataverse repository for the protocol
Harvard Dataverse: Underlying data for: The impact of the Covid-19 pandemic on suicidal behaviour: a living systematic review protocol. https://doi.org/10.7910/DVN/9JYHLS ( John et al., 2020b)
That project contains the following extended data:
Search.docx (additional information about the searches, including full search strategies)
Data extraction sheet/ study report
Prisma.pdf (the PRISMA-P statement)
Prospero registration
Reporting guidelines
Harvard Dataverse: PRISMA checklist for ‘The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: a living systematic review’ https://doi.org/10.7910/DVN/7WZXZK (John & Schmidt, 2020)
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Software availability
The development version of the software for automated searching is available from Github: https://github.com/mcguinlu/COVID_suicide_living.
Archived source code at time of publication: http://doi.org/10.5281/zenodo.3871366 (McGuinness & Schmidt, 2020)
License: MIT
Funding Statement
This work was supported by Swansea University and the University of Bristol. DG, BKO, JPTH are supported by the NIHR Bristol Biomedical Research Centre [IS-BRC-1215-20011]. JPTH and EE are suported by the NIHR Applied Research Collaboration West. LAMcG is by the NIHR through a NIHR Doctoral Research Fellowship [DRF-2018-11-ST2-048]. LS is supported by the NIHR through a NIHR Systematic Reviews Fellowship [RM-SR-2017-09-028]. AJ and CO are supported by the Swansea University Cochrane Satellite for Suicide and Self-Harm Prevention. AJ is supported by the National Centre for Mental Health [HCRW-CA04] NK and RW are supported by the NIHR Greater Manchester Patient Safety Translational Research Centre [PSTRC-2016-003].
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; peer review: 1 approved
References
- Acharya SR, Shin YC, Moon DH: COVID-19 outbreak and suicides in Nepal: Urgency of immediate action. Int J Soc Psychiatry. 2020; 0020764020963150. 10.1177/0020764020963150 [DOI] [PubMed] [Google Scholar]
- Ahmed S, Khaium MO, Tazmeem F: COVID-19 lockdown in India triggers a rapid rise in suicides due to the alcohol withdrawal symptoms: Evidence from media reports. Int J Soc Psychiatry. 2020;66(8):827–829. 10.1177/0020764020938809 [DOI] [PubMed] [Google Scholar]
- Akl EA, Meerpohl JJ, Elliott J, et al. : Living systematic reviews: 4. Living guideline recommendations. J Clin Epidemiol. 2017;91:47–53. 10.1016/j.jclinepi.2017.08.009 [DOI] [PubMed] [Google Scholar]
- Ando M, Furuichi M: The impact of COVID-19 employment shocks on suicide and safety net use: An early-stage investigation*. medRxiv. 2020. 10.1101/2020.11.16.20232850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Bond AE, Daruwala SE, et al. : Suicidal Ideation Among Individuals Who Have Purchased Firearms During COVID-19. Am J Prev Med. 2021;60(3):311–317. 10.1016/j.amepre.2020.10.013 [DOI] [PubMed] [Google Scholar]
- Bhatia R: Predictions of Covid-19 Related Unemployment On Suicide and Excess Mortality in the United States. medRxiv. 2020a. 10.1101/2020.05.02.20089086 [DOI] [Google Scholar]
- Bhatia R: Predictions of Covid-19 Related Unemployment On Suicide and Excess Mortality in the United States. medRxiv. 2020b. 10.1101/2020.05.02.20089086v3 [DOI] [Google Scholar]
- Bhuiyan AI, Sakib N, Pakpour AH, et al. : COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int J Ment Health Ad. 2020;1–6. 10.1007/s11469-020-00307-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boshra SN, Islam MM: The Status and Risk Factors of COVID-19 Related Suicides in Bangladesh. medRxiv. 2020a. Reference Source [Google Scholar]
- Boshra SN, Islam MM, Griffiths MD: The demography and apparent risk factors of COVID-19-related suicides in Bangladesh in a seven-month period of the pandemic. medRxiv. 2020b. 10.1101/2020.08.11.20171272 [DOI] [Google Scholar]
- Bray MJC, Daneshvari NO, Radhakrishnan I, et al. : Racial Differences in Statewide Suicide Mortality Trends in Maryland During the Coronavirus Disease 2019 (COVID-19) Pandemic. JAMA Psychiatry. 2021;78(4):444–447. 10.1001/jamapsychiatry.2020.3938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschmann C, Tsokos M: Corona-associated suicide - Observations made in the autopsy room. Leg Med (Tokyo). 2020a;46:101723. 10.1016/j.legalmed.2020.101723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschmann C, Tsokos M: Corona-associated suicide - Observations made in the autopsy room. Leg Med (Tokyo). 2020b;46:101723. 10.1016/j.legalmed.2020.101723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q, Feng H, Huang J, et al. : The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J Affect Disord. 2020;275:210–215. 10.1016/j.jad.2020.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderon-Anyosa RJC, Kaufman JS: Impact of COVID-19 lockdown policy on homicide, suicide, and motor vehicle deaths in Peru. medRxiv. 2020. 10.1101/2020.07.11.20150193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capuzzi E, di Brita C, Caldiroli A, et al. : Psychiatric emergency care during Coronavirus 2019 (COVID 19) pandemic lockdown: results from a Department of Mental Health and Addiction of northern Italy. Psychiatry Res. 2020;293:113463. 10.1016/j.psychres.2020.113463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SS, Stuckler D, Yip P, et al. : Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013;347:f5239. 10.1136/bmj.f5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang YH, Chang SS, Hsu CY, et al. : Impact of Pandemic on Suicide: Excess Suicides in Taiwan During the 1918-1920 Influenza Pandemic. J Clin Psychiatry. 2020;81(6):20l13454. 10.4088/JCP.20l13454 [DOI] [PubMed] [Google Scholar]
- Chen S, Jones PB, Underwood BR, et al. : The early impact of COVID-19 on mental health and community physical health services and their patients' mortality in Cambridgeshire and Peterborough, UK. J Psychiatr Res. 2020;131:244–254. 10.1016/j.jpsychires.2020.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung Y, Chau PH, Yip PS: A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psychiatry. 2008;23(12):1231–1238. 10.1002/gps.2056 [DOI] [PubMed] [Google Scholar]
- Cox J, Holden J, Sagovsky R: Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Debowska A, Horeczy B, Boduszek D, et al. : A repeated cross-sectional survey assessing university students' stress, depression, anxiety, and suicidality in the early stages of the COVID-19 pandemic in Poland. Psychol Med. 2020;1–4. 10.1017/S003329172000392X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks JJ, Higgins JPT, Altman DG, et al. : Analysing data and undertaking meta-analyses. Cochrane handbook for systematic reviews of interventions. 2nd ed.: John Wiley & Sons,2019. 10.1002/9781119536604.ch10 [DOI] [Google Scholar]
- Deisenhammer EA, Kemmler G: Decreased suicide numbers during the first 6 months of the COVID-19 pandemic. Psychiatry Res. 2021;295:113623. 10.1016/j.psychres.2020.113623 [DOI] [PubMed] [Google Scholar]
- Dragovic M, Pascu V, Hall T, et al. : Emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia. Australas Psychiatry. 2020;28(6):627–631. 10.1177/1039856220960673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dsouza DD, Quadros S, Hyderabadwala ZJ, et al. : Aggregated COVID-19 suicide incidences in India: Fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020;290:113145. 10.1016/j.psychres.2020.113145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JH, Synnot A, Turner T, et al. : Living systematic review: 1. Introduction-the why, what, when, and how. J Clin Epidemiol. 2017;91:23–30. 10.1016/j.jclinepi.2017.08.010 [DOI] [PubMed] [Google Scholar]
- Elliott JH, Turner T, Clavisi O, et al. : Living systematic reviews: an emerging opportunity to narrow the evidence-practice gap. PLoS Med. 2014;11(2):e1001603. 10.1371/journal.pmed.1001603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Mikocka-Walus A, Klas A, et al. : From " It Has Stopped Our Lives" to " Spending More Time Together Has Strengthened Bonds": The Varied Experiences of Australian Families During COVID-19. Front Psychol. 2020;11:588667. 10.3389/fpsyg.2020.588667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D, Steptoe A: COVID-19 social study.2020. Reference Source [Google Scholar]
- Faust JS, Shah SB, Du C, et al. : Suicide Deaths during the Stay-at-Home Advisory in Massachusetts. medRxiv. 2020. 10.1101/2020.10.20.20215343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay I, Gilmore I: Covid-19 and alcohol—a dangerous cocktail. BMJ. 2020;369:m1987. 10.1136/bmj.m1987 [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Pantoula E, Siamouli M, et al. : Development of the Risk Assessment Suicidality Scale (RASS): a population-based study. J Affect Disord. 2012;138(3):449–457. 10.1016/j.jad.2011.12.045 [DOI] [PubMed] [Google Scholar]
- Gonçalves-Pinho M, Mota P, Ribeiro J, et al. : The Impact of COVID-19 Pandemic on Psychiatric Emergency Department Visits - A Descriptive Study. Psychiatr Q. 2021;92(2):621–631. 10.1007/s11126-020-09837-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths MD, Mamun MA: COVID-19 suicidal behavior among couples and suicide pacts: Case study evidence from press reports. Psychiatry Res. 2020;289:113105. 10.1016/j.psychres.2020.113105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D, Appleby L, Arensman E, et al. : Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. 10.1016/S2215-0366(20)30171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamm ME, Brown PJ, Karp JF, et al. : Experiences of American older adults with pre-existing depression during the beginnings of the covid-19 pandemic: A multicity, mixed-methods study. Am J Geriatr Psychiatry. 2020;28(9):924–932. 10.1016/j.jagp.2020.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza CA, Ewing L, Heath NL, et al. : When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Can Psychol. 2021;62(1):20–30. 10.1037/cap0000255 [DOI] [Google Scholar]
- Hawton K, Casey D, Bale E, et al. : Self-harm during the early period of the COVID-19 Pandemic in England: comparative trend analysis of hospital presentations. medRxiv. 2020a. 10.1101/2020.11.25.20238030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Lascelles K, Brand F, et al. : Self-harm and the COVID-19 pandemic: a study of factors contributing to self-harm during lockdown restrictions. medRxiv. 2020b. 10.1101/2020.12.04.20244129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Marzano L, Fraser L, et al. : Reporting on suicidal behaviour and COVID-19-need for caution. Lancet Psychiatry. 2021;8(1):15–17. 10.1016/S2215-0366(20)30484-3 [DOI] [PubMed] [Google Scholar]
- Hernández-Calle D, Martínez-Alés G, Mediavilla R, et al. : Trends in psychiatric emergency department visits due to suicidal ideation and suicide attempts during the CoViD-19 pandemic in Madrid, Spain. J Clin Psychiatry. 2020;81(5):20l13419. 10.4088/JCP.20l13419 [DOI] [PubMed] [Google Scholar]
- Hewson T, Green R, Shepherd A, et al. : The effects of COVID-19 on self-harm in UK prisons. BJPsych Bull. 2020;1–3. 10.1192/bjb.2020.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, O'Connor RC, Perry VH, et al. : Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humber N, Piper M, Appleby L, et al. : Characteristics of and trends in subgroups of prisoner suicides in England and Wales. Psychol Med. 2011;41(11): 2275–2285. 10.1017/S0033291711000705 [DOI] [PubMed] [Google Scholar]
- Iob E, Steptoe A, Fancourt D: Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatr. 2020;217(4):543–546. 10.1192/bjp.2020.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal Y, Al Abdulla MA, Albrahim S, et al. : Psychiatric presentation of patients with acute SARS-CoV-2 infection: a retrospective review of 50 consecutive patients seen by a consultation-liaison psychiatry team. BJPsych Open. 2020;6(5):e109. 10.1192/bjo.2020.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isumi A, Doi S, Yamaoka Y, et al. : Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110(Pt 2):104680. 10.1016/j.chiabu.2020.104680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob S, Mwagiru D, Thakur I, et al. : Impact of societal restrictions and lockdown on trauma admissions during the COVID‐19 pandemic: a single‐centre cross‐sectional observational study. ANZ J Surg. 2020;90(11):2227–2231. 10.1111/ans.16307 [DOI] [PubMed] [Google Scholar]
- Jacobson NC, Lekkas D, Price G, et al. : Flattening the Mental Health Curve: COVID-19 Stay-at-Home Orders Are Associated With Alterations in Mental Health Search Behavior in the United States. JMIR Ment Health. in press. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefsen OH, Rohde C, NØrremark B, et al. : COVID‐19‐related self‐harm and suicidality among individuals with mental disorders. Acta Psychiatr Scand. 2020a;142(2):152–153. 10.1111/acps.13214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefsen OH, Rohde C, NØrremark B, et al. : Editorial Perspective: COVID‐19 pandemic‐related psychopathology in children and adolescents with mental illness. J Child Psychol Psychiatry. 2020b. 10.1111/jcpp.13292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John A, Eyles E, Mcguinness LA, et al. : The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: protocol for a living systematic review [version 1; peer review: 1 approved, 1 approved with reservations] F1000Research. 2020b;9:644. 10.12688/f1000research.24274.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John A, Okolie C, Eyles E, et al. : The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: a living systematic review [version 1; peer review: 1 approved]. F1000Res. 2020c;9:1097. 10.12688/f1000research.25522.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John A, Pirkis J, Gunnell DG, et al. : Trends in suicide during the covid-19 pandemic. BMJ. 2020a;371:m4352. 10.1136/bmj.m4352 [DOI] [PubMed] [Google Scholar]
- Joiner TE, Pfaff JJ, Acres JG: A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behav Res Ther. 2002;40(4):471–81. 10.1016/s0005-7967(01)00017-1 [DOI] [PubMed] [Google Scholar]
- Jolly TS, Batchelder E, Baweja R: Mental Health Crisis Secondary to COVID-19-Related Stress: A Case Series From a Child and Adolescent Inpatient Unit. Prim care companion CNS disord. 2020;22(5):20l02763. 10.4088/PCC.20l02763 [DOI] [PubMed] [Google Scholar]
- Kapilan N: Suicides cases among nurses in India due to COVID-19 and possible prevention strategies. Asian J Psychiatr. 2020;54:102434. 10.1016/j.ajp.2020.102434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kar SK, Arafat SY, Ransing R, et al. : Repeated celebrity suicide in India during COVID-19 crisis: An urgent call for attention. Asian J Psychiatr. 2020;53:102382. 10.1016/j.ajp.2020.102382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakasi MV, Kevrekidis DP, Pavlidis P: The Role of the SARS-CoV-2 Pandemic on Suicide Rates: Preliminary Study in a Sample of the Greek Population. Am J Forensic Med Pathol. 2021;42(1):99- 100. 10.1097/PAF.0000000000000598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakasi MV, Zaoutsou A, Theofilidis A, et al. : The impact of the SARS‐CoV‐2 pandemic on psychiatric emergencies in northern Greece: preliminary study on a sample of the Greek population. Psychiatry Clin Neurosci. 2020a;74(11):613–615. 10.1111/pcn.13136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavoor AR, Chakravarthy K, John T: Remote consultations in the era of COVID-19 pandemic: Preliminary experience in a regional Australian public acute mental health care setting. Asian J Psychiatr. 2020;51:102074. 10.1016/j.ajp.2020.102074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawohl W, Nordt C: COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. 10.1016/S2215-0366(20)30141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketphan O, Juthamanee S, Racal SJ, et al. : The mental health care model to support the community during the COVID-19 pandemic in Thailand. Belitung Nurs J. 2020;6:152–156. 10.33546/bnj.1193 [DOI] [Google Scholar]
- Khan MM, Ahmed A, Khan SR: Female suicide rates in Ghizer, Pakistan. Suicide Life Threat Behav. 2009;39(2):227–230. 10.1521/suli.2009.39.2.227 [DOI] [PubMed] [Google Scholar]
- Khan MM, Hyder AA: Suicides in the developing world: Case study from Pakistan. Suicide Life Threat Behav. 2006;36(1):76–81. 10.1521/suli.2006.36.1.76 [DOI] [PubMed] [Google Scholar]
- Killgore WD, Cloonan SA, Taylor EC, et al. : Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020a;293:113390. 10.1016/j.psychres.2020.113390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AM: The short-term impact of the COVID-19 outbreak on suicides in Korea. Psychiatry Res. 2021;295:113632. 10.1016/j.psychres.2020.113632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S, Warren N, McMahon L, et al. : Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369;m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, Glenn CR: Assessing the functions of non-suicidal self-injury: Psychometric properties of the Inventory of Statements About Self-injury (ISAS). J Psychopathol Behav Assess. 2009;31(3):215–219. 10.1007/s10862-008-9107-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knipe D, Evans H, Marchant A, et al. : Mapping population mental health concerns related to COVID-19 and the consequences of physical distancing: a Google trends analysis [version 2; peer review: 2 approved] Wellcome Open Res. 2020;5:82. 10.12688/wellcomeopenres.15870.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lersch KM: COVID-19 and Mental Health: An Examination of 911 Calls for Service. Policing: A Journal of Policy and Practice. 2020;14(4):1112– 1126. 10.1093/police/paaa049 [DOI] [Google Scholar]
- Leske S, Kõlves K, Crompton D, et al. : Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2021;8(1):58–63. 10.1016/S2215-0366(20)30435-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low DM, Rumker L, Talkar T, et al. : Natural Language Processing Reveals Vulnerable Mental Health Support Groups and Heightened Health Anxiety on Reddit During COVID-19: Observational Study. J Med Internet Res. 2020;22(10):e22635. 10.2196/22635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E: Covid-19: EU states report 60% rise in emergency calls about domestic violence. BMJ. 2020;369:m1872. [DOI] [PubMed] [Google Scholar]
- Mamun MA, Chandrima RM, Griffiths MD: Mother and son suicide pact due to COVID-19-related online learning issues in Bangladesh: An unusual case report. Int J Ment Health Addict. 2020a;1–4. 10.1007/s11469-020-00362-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun MA, Syed NK, Griffiths MD: Indian celebrity suicides before and during the COVID-19 pandemic and their associated risk factors: Evidence from media reports. J Psychiatr Res. 2020b;131:177–179. 10.1016/j.jpsychires.2020.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun MA, Ullah I: COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? – The forthcoming economic challenges for a developing country. Brain Behav Immun. 2020;87:163–166. 10.1016/j.bbi.2020.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAndrew J, O’Leary J, Cotter D, et al. : Impact of initial COVID-19 restrictions on psychiatry presentations to the emergency department of a large academic teaching hospital. Ir J Psychol Med. 2020;1–8. 10.1017/ipm.2020.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre A, Tong K, McMahon E, et al. : Covid-19 and its effect on emergency presentations to a tertiary hospital with self-harm in Ireland. Ir J Psychol Med. 2020;1–7. 10.1017/ipm.2020.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre RS, Lee Y: Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020a;19(2):250–251. 10.1002/wps.20767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre RS, Lee Y: Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020b;290:113104. 10.1016/j.psychres.2020.113104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell TO, Li L: State-Level Data on Suicide Mortality During COVID-19 Quarantine: Early Evidence of a Disproportionate Impact on Racial Minorities. Psychiatry Res. 2021;295:113629. 10.1016/j.psychres.2020.113629 [DOI] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, et al. : Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser DA, Glaus J, Frangou S, et al. : Years of life lost due to the psychosocial consequences of COVID-19 mitigation strategies based on Swiss data. Eur Psychiatry. 2020;63(1):e58. 10.1192/j.eurpsy.2020.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan R, Sterne JA, Higgins JP, et al. : A new instrument to assess Risk of Bias in Non-randomised Studies of Exposures (ROBINS-E): Application to studies of environmental exposure Global Evidence Summit. Cape Town.2017. Reference Source [Google Scholar]
- Morin CM, Belleville G, Bélanger L, et al. : The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalleballe K, Onteddu SR, Sharma R, et al. : Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav Immun. 2020;88:71–74. 10.1016/j.bbi.2020.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Child Mortality Database: Child Suicide Rates during the COVID-19 Pandemic in England: Real-time Surveillance.2020. Reference Source [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, et al. : Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19(3):309–317. 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- O'Connor RC, Wetherall K, Cleare S, et al. : Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2020;1–8. 10.1192/bjp.2020.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olding J, Zisman S, Olding C, et al. : Penetrating trauma during a global pandemic:changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon. 2021;19(1):e9–e13. 10.1016/j.surge.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, McManus S, Jessop C, et al. : Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020;7(7):567–568. 10.1016/S2215-0366(20)30237-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignon B, Gourevitch R, Tebeka S, et al. : Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. MedRxiv. 2020a. 10.1101/2020.05.19.20095901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignon B, Gourevitch R, Tebeka S, et al. : Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin Neurosci. 2020b;74:557–559. 10.1111/pcn.13104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirnia B, Dezhakam H, Pirnia K, et al. : Grief of COVID-19 is a mental contagion, first family suicide in Iran. Asian J Psychiatr. 2020;54:102340. 10.1016/j.ajp.2020.102340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel S, Sedhai YR, Atreya A: An increase in suicides amidst the coronavirus disease 2019 pandemic in Nepal. Med Sci Law. 2021;61(2):161–162. 10.1177/0025802420966501 [DOI] [PubMed] [Google Scholar]
- Poudel K, Subedi P: Impact of COVID-19 pandemic on socioeconomic and mental health aspects in Nepal. Int J Soc Psychiatry. 2020;66(8):748–755. 10.1177/0020764020942247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin P, Mehlum L: National observation of death by suicide in the first 3 months under COVID-19 pandemic. Acta Psychiatr Scand. 2021;143(1):92–93. 10.1111/acps.13246 [DOI] [PubMed] [Google Scholar]
- Radeloff D, Papsdorf R, Uhlig K, et al. : Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. medRxiv. 2020. 10.1101/2020.10.21.20187419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radeloff D, Papsdorf R, Uhlig K, et al. : Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. 2021;30:E16. 10.1017/S2045796021000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Plummer V: COVID-19 related suicide among hospital nurses; case study evidence from worldwide media reports. Psychiatry Res. 2020;291:113272. 10.1016/j.psychres.2020.113272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman J, Ettman CK, Dean L, et al. : Economic precarity, social isolation, and suicidal ideation during the COVID-19 pandemic. medRxiv. 2020. 10.1101/2020.10.05.20205955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar RP: Suicides related to the COVID-19 outbreak in India: a pilot study of media reports. Asian J Psychiatr. 2020;53:102196. 10.1016/j.ajp.2020.102196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajput K, Sud A, Rees M, et al. : Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg. 2020;1–6. 10.1007/s00068-020-01507-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rana U: Elderly Suicides in India: An Emerging Concern during COVID-19 Pandemic. Int Psychogeriatr. 2020;32(10):1251–1252. 10.1017/S1041610220001052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger MA, Stanley IH, Joiner TE: Suicide Mortality and Coronavirus Disease 2019—A Perfect Storm? JAMA Psychiatry. 2020;77(11):1093–1094. 10.1001/jamapsychiatry.2020.1060 [DOI] [PubMed] [Google Scholar]
- Rhodes HX, Petersen K, Biswas S: Trauma trends during the initial peak of the COVID-19 pandemic in the midst of lockdown: experiences from a rural trauma center. Cureus. 2020;12(8):e9811. 10.7759/cureus.9811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivlin A, Hawton K, Marzano L, et al. : Psychiatric disorders in male prisoners who made near-lethal suicide attempts: case–control study. Br J Psychiatry. 2010;197(4):313–319. 10.1192/bjp.bp.110.077883 [DOI] [PubMed] [Google Scholar]
- Rohde C, Jefsen OH, Nørremark B, et al. : Psychiatric Symptoms Related to the COVID-19 Pandemic. medRxiv. 2020. 10.1101/2020.04.16.20067744 [DOI] [PubMed] [Google Scholar]
- Rück C, Mataix-cols D, Malki K, et al. : Will the COVID-19 pandemic lead to a tsunami of suicides? A Swedish nationwide analysis of historical and 2020 data. medRxiv. 2020. 10.1101/2020.12.10.20244699 [DOI] [Google Scholar]
- Sade S, Sheiner E, Wainstock T, et al. : Risk for depressive symptoms among hospitalized women in high-risk pregnancy units during the COVID-19 pandemic. J Clin Med. 2020;9(8):2449. 10.3390/jcm9082449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha K, Torous J, Caine ED, et al. : Psychosocial Effects of the COVID-19 Pandemic: Large-scale Quasi-Experimental Study on Social Media. J Med Internet Res. 2020;22(11):e22600. 10.2196/22600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahoo S, Rani S, Parveen S, et al. : Self-harm and COVID-19 Pandemic: An emerging concern – A report of 2 cases from India. Asian J Psychiatr. 2020;51:102104. 10.1016/j.ajp.2020.102104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakelliadis EI, Katsos KD, Zouzia EI, et al. : Impact of Covid-19 Lockdown on Characteristics of Autopsy Cases in Greece. Comparison between 2019 and 2020. Forensic Sci Int. 2020;313:110365. 10.1016/j.forsciint.2020.110365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan DC, Cloutier R, Johnson K, et al. : Where have all the emergency paediatric mental health patients gone during COVID-19? Acta Paediatr. 2021;110(2):598–599. 10.1111/apa.15537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoib S, Nagendrappa S, Grigo O, et al. : Factors associated with COVID-19 outbreak-related suicides in India. Asian J Psychiatr. 2020;53:e102223. 10.1016/j.ajp.2020.102223 [DOI] [PubMed] [Google Scholar]
- Singh R, Baral KP, Mahato S: An urgent call for measures to fight against increasing suicides during COVID-19 pandemic in Nepal. Asian J Psychiatr. 2020;54:102259. 10.1016/j.ajp.2020.102259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinyor M, Spittal MJ, Niederkrotenthaler T: Changes in Suicide and Resilience-related Google Searches during the Early Stages of the COVID-19 Pandemic. Can J Psychiatry. 2020;65(10):741–743. 10.1177/0706743720933426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smalley CM, Malone DA, Meldon SW, et al. : The impact of COVID-19 on suicidal ideation and alcohol presentations to emergency departments in a large healthcare system. Am J Emerg Med. in press 2021.41:237–238. 10.1016/j.ajem.2020.05.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son C, Hegde S, Smith A, et al. : Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. J Med Internet Res. 2020;22(9):e21279. 10.2196/21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, et al. : ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuckler D, Basu S, Suhrcke M, et al. : The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. 2009;374(9686):315–323. 10.1016/S0140-6736(09)61124-7 [DOI] [PubMed] [Google Scholar]
- Sueki H: Development of a short form of the suicidal ideation scale. Suicide Prevention & CrisisIntervention. 2019;39(2):94–101. Reference Source [Google Scholar]
- Sueki H, Ueda M: Short-term effect of the COVID-19 pandemic on suicidal ideation: A prospective cohort study. PsyArXiv. 2020. 10.31234/osf.io/3jevh [DOI] [Google Scholar]
- Syed NK, Griffiths MD: Nationwide suicides owing to alcohol withdrawal symptoms during COVID-19 pandemic: A review of cases from media reports. J Psychiatr Res. 2020;130:289–291. 10.1016/j.jpsychires.2020.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T, Okamoto S: Suicide during the COVID-19 pandemic in Japan. medRxiv. 2020. 10.1101/2020.08.30.20184168 [DOI] [Google Scholar]
- Tanaka T, Okamoto S: Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021;5(2):229–238. 10.1038/s41562-020-01042-z [DOI] [PubMed] [Google Scholar]
- Taquet M, Luciano S, Geddes JR, et al. : Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. 10.1016/S2215-0366(20)30462-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur V, Jain A: COVID 2019-suicides: A global psychological pandemic. Brain Behav Immun. in press 2020;88:952–953. 10.1016/j.bbi.2020.04.062 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Titov N, Staples L, Kayrouz R, et al. : Rapid report: Early demand, profiles and concerns of mental health users during the coronavirus (COVID-19) pandemic. Internet Interv. 2020;21:100327. 10.1016/j.invent.2020.100327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turecki G, Brent DA, Gunnell D, et al. : Suicide and suicide risk. Nat Rev Dis Primers. 2019;5(1):74. 10.1038/s41572-019-0121-0 [DOI] [PubMed] [Google Scholar]
- Ueda M, Nordström R, Matsubayashi T: Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health (Oxf). 2021;fdab113. 10.1093/pubmed/fdab113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdés-Florido MJ, López-Díaz Á, Palermo-Zeballos FJ, et al. : Reactive psychoses in the context of the COVID-19 pandemic: clinical perspectives from a case series. Rev Psiquiatr Salud Ment. 2020;13(2):90–94. 10.1016/j.rpsm.2020.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandoros S, Theodorikakou O, Katsadoros K, et al. : No evidence of increase in suicide in Greece during the first wave of Covid-19. medRxiv. 2020. 10.1101/2020.11.13.20231571 [DOI] [Google Scholar]
- Walker LE, Heaton HA, Monroe RJ, et al. : Impact of the SARS-CoV-2 Pandemic on Emergency Department Presentations in an Integrated Health System. Mayo Clin Proc. 2020;95(11):2395–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang R, Li J, Mei J, et al. : Research on the suicide risk, sleep, psychological status and influencing factors of coronavirus disease 2019 patients.Lanzhou University/CNKI ID: czh-359.2020a. Reference Source [Google Scholar]
- Wang Y, Hu Z, Feng Y, et al. : Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. 2020b;25(12):3140–3149. 10.1038/s41380-020-00881-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman IM: The impact of epidemic, war, prohibition and media on suicide: United States, 1910-1920. Suicide Life Threat Behav. 1992;22(2):240–254. [PubMed] [Google Scholar]
- Winkler P, Formanek T, Mlada K, et al. : Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol Psychiatr Sci. 2020;29:e173. 10.1017/S2045796020000888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong TW, Gao Y, Tam WWS: Anxiety among university students during the SARS epidemic in Hong Kong. Stress Health. 2007;23(1):31–35. 10.1002/smi.1116 [DOI] [Google Scholar]
- Worldometers: Covid-19 Coronavirus Pandemic.2020; [Accessed 07/06/2020]. Reference Source [Google Scholar]
- Wu C, Hu X, Song J, et al. : Mental health status and related influencing factors of COVID-19 survivors in Wuhan, China. Clin Transl Med. 2020a;10(2):e52. 10.1002/ctm2.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Zhang C, Liu H, et al. : Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. 2020b;223(2):240.e1–240.e9. 10.1016/j.ajog.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Q, Hu C, Feng R, et al. : Investigation of the mental health of patients with novel coronavirus pneumonia. Chinese Journal of Neurology. 2020; (12):E003–E003. 10.3760/cma.j.cn113694-20200220-00102 [DOI] [Google Scholar]
- Zhang L, Zhang D, Fang J, et al. : Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2021482. 10.1001/jamanetworkopen.2020.21482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zortea TC, Brenna CTA, Joyce M, et al. : The Impact of Infectious Disease-Related Public Health Emergencies on Suicide, Suicidal Behavior, and Suicidal Thoughts. Crisis. 2020;1–14. 10.1027/0227-5910/a000753 [DOI] [PMC free article] [PubMed] [Google Scholar]