Abstract
Background/objective
Nummular headache (NH) is a primary headache disorder characterised by intermittent or continuous scalp pain, affecting a small circumscribed area of the scalp. As there are limited data in the literature on NH, we conducted this review to evaluate demographic characteristics and factors associated with complete resolution of the headache, and effectiveness of treatment options.
Methods
We performed a systematic review of cases reported through PubMed database, using Preferred Reporting Items for Systematic Reviews and Meta-Analyses protocol and ‘nummular headache’, ‘coin-shaped headache’ and ‘coin-shaped cephalalgia’ keywords. Analysis was performed by using χ2 test and Wilcoxon rank-sum test. For individual interventions, the response rate (RR%) of the treatment was calculated.
Results
We analysed a total of 110 NH cases, with median age 47 years and age of pain onset 42 years. Median duration to make correct diagnosis was 18 months after first attack. The median intensity of each attack was 5/10 on verbal rating scale over 4 cm diameter with duration of attack <30 min. Patients with NH had median three attacks per day with frequency of 9.5 days per month. 40 (57.97%) patients had complete resolution of the headache after treatment. Patients with complete resolution were younger, more likely to be female, and were more likely to have diagnosis within year. Patients with complete resolution more likely to have received treatment with onabotulinum toxin A (botulinum toxin type A (BoNT-A)), and gabapentin compared with patients without complete resolution. Most effective interventions were gabapentin (n=34; RR=67.7%), non-steroidal anti-inflammatory drugs (NSAIDs) (n=32; RR=65.6%), BoNT-A (n=12; RR=100%) and tricyclic antidepressant (n=9; RR=44.4%).
Conclusion
Younger patients, female sex and early diagnosis were associated with complete resolution. NSAIDs, gabapentin and BoNT-A were most commonly used medications, with significant RRs.
Keywords: nummular headache, coin-shaped headache, coin-shaped cephalalgia, response rate, systematic review, case reports, onabotulinum toxin A, BoNT-A, gabapentin
Introduction
As per International Classification of Headache Disease-3 (ICHD-3), nummular headache (NH) is a primary headache disorder characterised by intermittent or continuous scalp pain of highly variable duration, but often chronic, in a small circumscribed area of the scalp and in the absence of any underlying structural lesion.1 2 Previously, it was known as ‘coin-shaped headache’.1 The estimated incidence in NH is 6.4 per 100 000.3
The pathophysiology of NH is unknown,4 5 and the majority of them arise without any precipitating factor. The signs and symptoms of NH are confined to a small area, suggesting a peripheral local process with no evidence of central mechanism as in migraine or tension type headache.4 The localisation of pain can be to any part of the scalp, but most commonly parietal area is affected.4 6 NH is typically unifocal, with the exception of a few cases of bilateral headache.6 The pain is usually mild to moderate in intensity, rarely severe. The duration is highly variable, lasting from as short as a few seconds to daily and continuous pain. Pain is mostly described as pressure, stabbing or occasionally burning.4 Sensory disturbances like allodynia, hypo/hyperaesthesia, paraesthesia, hyperalgesia and tenderness commonly occur in the affected area of pain.4–8
Patients with mild pain do not require treatment and reassurance is the only intervention needed. However, treatment is warranted in patients with severe pain. Antiepileptic’s and tricyclic antidepressants (TCA) have not been shown to be effective in patients with NH. Analgesics and non-steroidal anti-inflammatory drugs (NSAIDs) have been reported as an effective treatment in 60% of the published cases; especially in cases of acute exacerbation, mild continuous or intermittent pain or as add-on treatment with other drugs.4 In patients with inadequate response to other treatments, botulinum toxin type A (BoNT-A) is reported to be a well-tolerated and effective treatment in few case series5 9 but lacks appropriate sample size. It has been reported that gabapentin is only transiently effective for NH and NH eventually becomes refractory to all standard prophylactic and analgesic therapies.10–12 Small number of case series and prospective studies have reported NH characteristics and its various treatment therapies but limited by duplication of patients data or inadequate availability of individual patients data.3 4 13 To our knowledge, there are no studies that have analysed the individual cases of NH systematically to evaluate the effectiveness of each therapeutic intervention.
The primary aim of this systematic review is to evaluate the demographic characteristics, variation in presentation of NH and effectiveness of therapeutic interventions in individual NH cases published in literature. Our secondary outcomes were to find the characteristics of patients with complete resolution of the headache and effectiveness (response rate (RR)) of the treatment choices used for patients with NH.
Methods
We performed a systematic review of cases reported on NH. We followed the predesigned Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol and PRISMA checklist14 (online supplementary file 1) and standard for reporting the systematic review to the extent of our possibilities.
bmjno-2020-000049supp001.pdf (65.3KB, pdf)
Search strategy
A comprehensive search for case reports and case series on PubMed database was conducted on 30 June 2019 by two independent investigators (AA and SS). The search included case reports, case illustrations, letters reporting human cases and case series from January 2002 to June 2019, by using keywords ‘nummular headache’, ‘coin-shaped headache’ and ‘coin-shaped cephalalgia’.
Definition and classification
NH is a rare kind of primary headache disorder that is defined as, ‘pain of highly variable duration, often chronic pain in a small circumscribed area of the scalp without any underlying cause’. ICHD-3 has described the following diagnostic criteria: (1) continuous or intermittent head pain, (2) exclusively on the scalp with four characteristics of sharply countered, fixed in size and shape, round or elliptical, 1–6 cm in diameter and (3) not met criteria of other headaches of ICHD-3 diagnosis.1
Eligibility criteria
We used the following inclusion criteria to include cases in systematic review: all case reports and case series of NH (1) where diagnosis was confirmed by clinician as described by the author's judgement, (2) where complete data including demographics and personal information were available, and (3) where mimicking differential diagnosis was ruled out to provide a clear picture. We excluded articles that were (1) observational studies, review articles, letters to the editor that were not presenting clinical NH case reports, (2) case reports in any language other than English and (3) observational studies, review articles and case series with duplication of patient’s data.
Selection of studies and data collection
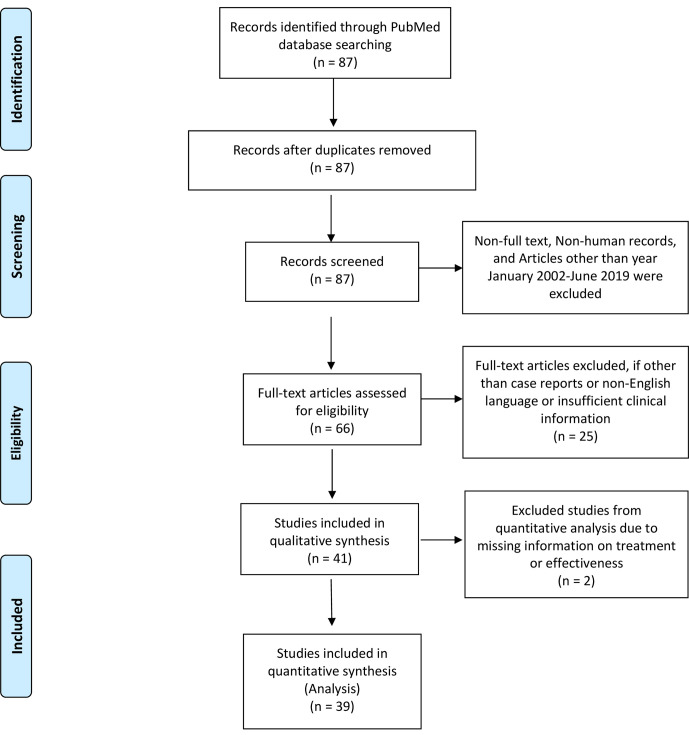
By using this search strategy, a total of 87 articles were identified and screened. We excluded 21 articles which were non-human, non-full text and outside of January 2002–June 2019 publication. Then, both investigators (AA and SS) independently read 66 articles including abstracts and full manuscript, and selected the articles based on inclusion and exclusion criteria. Any disagreement was reviewed by a third investigator (UKP) and disagreement was resolved by consensus. Twenty-five articles that were excluded were not full articles, incomplete information on demographics or headache characteristics, not well defined, non-English language and difficult to comprehend. This left us with 41 case reports and case series, of which 2 were missing treatment given or effectiveness. So, 41 case reports and case series were considered for qualitative and 39 were considered for quantitative analysis (figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of literature search and selection process of nummular headache case reports. From Moher et al.14
All eligible studies were reviewed using a standardised web-based form to collect information. All data were summarised descriptively, including country of the patient, age, sex, age at diagnosis, latency, duration, timing and frequency of attack, characteristic of headache (localisation, region, diameter, quality and intensity of pain, tenderness and exacerbating factors), concomitant symptoms, comorbidities and therapeutic interventions.
Outcomes
The primary outcome of our systematic review of cases is to evaluate the demographic characteristics, variation in presentation of NH and treatment interventions as most cases of NH were initially misdiagnosed for other types of headache. Our secondary outcomes were to find the characteristics of complete resolution versus non-resolution of the headache and effectiveness (RR) of the treatment choices. The complete resolution (no headache with ongoing treatment) versus non-resolution (infrequent headache episodes with ongoing treatment) of the headache pain was decided by the patients’ response noted by the physicians (within case) with the different medicines.
Statistical analysis
We used Microsoft Excel to collect the data of those 110 cases and SAS (V.9.4) software to evaluate the data (online supplementary file 2). Univariate analysis of differences between categorical variables was tested using the χ2 test and analysis of differences of median between continuous variables was tested using Wilcoxon rank-sum test. We used proc means, proc freq, proc npar1way and proc univariate procedures to calculate these numbers. Frequency percentage, median and SE of the cohort were calculated from non-missing data. P value of <0.05 was considered statistically significant. No statistical power calculation was conducted prior to the study and the sample size was based on the available data. For individual interventions, the RR (%) of the treatment was calculated by dividing the number of patients with complete resolution after taking a particular drug to the number of patients who had taken that drug multiplied by 100.
bmjno-2020-000049supp002.pdf (48.7KB, pdf)
Results
We analysed a total of 110 NH published cases which fulfilled the inclusion criteria for this review. Table 1 represents age-based and gender-based distribution of the cohort.
Table 1.
Distribution of the 110 nummular headache cases based on age and gender
| Author; country; year | Number of cases | Age (years) | Gender |
| Liu and Wei; China; 201824 | 3 | 74 | F |
| 46 | M | ||
| 38 | F | ||
| Rodríguez et al; Spain; 20158 | 1 | 14 | F |
| Camacho-Velasquez; Spain; 201625 | 1 | 47 | M |
| Barón et al; Spain; 201526 | 1 | 21 | F |
| López-Ruiz et al; Spain; 201427 | 2 | 67 | M |
| 60 | M | ||
| Iwanowski et al; Poland; 201428 | 1 | 61 | F |
| Kurian and Solomon; USA; 201429 | 2 | 47 | F |
| 49 | F | ||
| López-Mesonero et al; Spain; 201430 | 1 | 41 | F |
| Mulero et al; Spain; 201331 | 3 | 21 | M |
| 45 | M | ||
| 35 | M | ||
| Yin et al; Italy; 201332 | 1 | 52 | M |
| Irimia et al; Spain; 201333 | 1 | 33 | F |
| Danno et al; Japan; 201334 | 3 | 71 | M |
| 57 | F | ||
| 39 | M | ||
| Dai et al; China; 20136 | 1 | 63 | M |
| Herrero-Velázquez et al; Spain; 201335 | 8 | 46 | M |
| 60 | F | ||
| 23 | F | ||
| 43 | M | ||
| 53 | F | ||
| 33 | M | ||
| 54 | F | ||
| 42 | F | ||
| Başağrisi et al; China; 201036 | 1 | 59 | M |
| Yamazaki and Kobatake; Japan; 201137 | 1 | 28 | M |
| Rocha-Filho; Brazil; 201138 | 1 | 52 | M |
| Porta-Etessam et al; Japan; 201039 | 1 | 52 | F |
| Chen et al; Taiwan; 201540 | 1 | 62 | M |
| Guerrero Ángel et al; Spain; 201141 | 6 | 61 | M |
| 71 | F | ||
| 80 | F | ||
| 30 | F | ||
| 33 | M | ||
| 32 | F | ||
| Campbel and Sartori; USA; 201342 | 1 | 47 | F |
| Evans and Pareja; Spain; 200511 | 1 | 57 | F |
| Trucco et al; Italy; 200610 | 1 | 55 | F |
| Evan et al; Spain; 200643 | 1 | 45 | F |
| Trucco et al; Italy; 200744 | 1 | 26 | F |
| Guillem et al; USA; 200745 | 1 | 60 | F |
| Tayeb et al; USA; 200846 | 1 | 47 | M |
| Pareja et al; Spain; 200847 | 5 | 65 | F |
| 50 | F | ||
| 61 | F | ||
| 60 | M | ||
| 34 | F | ||
| Mathew et al; USA; 20089 | 4 | 43 | F |
| 58 | F | ||
| 35 | F | ||
| 47 | F | ||
| Baldacci et al; Italy; 201048 | 1 | 40 | M |
| Dach et al; Spain; 200649 | 3 | 41 | F |
| 29 | M | ||
| 64 | M | ||
| Robbins and Grosberg; USA; 201350 | 1 | 40 | F |
| Alvaro et al; Spain; 200951 | 4 | 67 | M |
| 72 | F | ||
| 50 | F | ||
| 37 | F | ||
| Cuadrado et al; Spain; 200952 | 3 | 28 | M |
| 67 | F | ||
| 51 | M | ||
| Dabscheck and Ian Andrews; Australia; 201053 | 1 | 4 | M |
| Dusitanond et al; USA; 200854 | 5 | 24 | F |
| 30 | F | ||
| 47 | F | ||
| 55 | F | ||
| 59 | F | ||
| Ruscheweyh et al; Germany; 200955 | 6 | 25 | F |
| 39 | M | ||
| 39 | F | ||
| 49 | M | ||
| 24 | M | ||
| 57 | F | ||
| Jiang et al; China; 201956 | 2 | 48 | F |
| 72 | M | ||
| Grosberg et al; USA; 200718 | 1 | 55 | M |
| Pareja et al; Spain; 20043* | 14 | 38 (mean) | 3—Male |
| 11—Female | |||
| Pareja et al; Spain; 20022* | 13 | 50 (mean) | 5—Male |
| 8—Female |
*The data from these studies have considered for the analysis of demographic and headache characteristics but have not considered for analysis of treatment effectiveness due to missing accurate treatment.
Epidemiological and clinical characteristics
There were 108 adults (38% male and 62% female) and 2 children (1 boy and 1 girl) diagnosed with NH. The median age of the study cohort was 47±1.7 (SE) years ranging from 4 to 80 years. The median age of onset of pain in patients was 42±1.8 (SE) years (table 2).
Table 2.
Demographics and clinical characteristics of the patients with nummular headache
| Total number of cases reviewed | n=110 |
| Age group | |
| Adults | 108 (98.18%) |
| Paediatrics | 2 (1.82%) |
| Age (years) (median ±SE; IQR) | 47±1.7 (37.5–61.5) |
| Gender (adults) | |
| Male | 41 (38%) |
| Female | 67 (62%) |
| Age of onset of pain (years) (median ±SE) | 42±1.8 |
| The intensity of pain (VRS 1–10) (median ±SE) | 5±0.2 |
| Latency from the first attack to diagnosis (months; median ±SE) | 18±12.8 |
| Duration of attacks (min) | |
| <30 | 17 (53.13%) |
| 30–120 | 8 (28.13%) |
| >120 | 6 (18.75%) |
| Diameter of the pain (cm; median ±SE) | 4±0.2 |
| Number of attacks per day (median ±SE) | 3±2.1 |
| Frequency (days/month; median ±SE) | 9.5±3.6 |
| Localisation of pain | |
| Unilateral—left | 26 (38.24%) |
| Unilateral—right | 35 (51.47%) |
| Bilateral | 7 (10.29%) |
| Region of brain | |
| Frontal | 17 (21.52%) |
| Temporal | 8 (10.12%) |
| Parietal | 43 (54.43%) |
| Occipital | 11 (13.92%) |
| Quality of pain | |
| Boring | 2 (2.78%) |
| Burning | 9 (12.50%) |
| Electric | 3 (4.17%) |
| Lancinating | 3 (4.17%) |
| Oppressive | 3 (4.17%) |
| Pressure | 32 (44.44%) |
| Pulsating | 2 (2.78%) |
| Sharp | 1 (1.39%) |
| Stabbing | 12 (16.67%) |
| Throbbing | 5 (6.94%) |
| Tenderness | |
| Yes | 24 (35.29%) |
| No | 44 (64.71%) |
| Temporary relief | |
| Yes | 47 (69.12%) |
| No | 21 (30.88%) |
| Total resolution | |
| Yes | 40 (57.97%) |
| No | 29 (42.03%) |
| Therapeutic interventions | 66 |
| Onabotulinum toxin A (BoNT-A) | 12 (18.46%) |
| Triptan | 3 (4.69%) |
| Tricyclic antidepressant (TCA)* | 9 (13.6%) |
| Lamotrigine | 8 (12.31%) |
| Gabapentin | 34 (52.31%) |
| Carbamazepine | 11 (16.92%) |
| Topiramate | 3 (4.69%) |
| Concomitant symptoms | Nausea, vomiting, photophobia, phonophobia, allodynia, hyperaesthesia, tearing, itching eye, bilateral trigeminal hyperalgesia, dizziness, blurred vision, hypoaesthesia, paraesthesia, Hyperalgesia |
| Exacerbating factors | Cough, head movements, valsalva, cough, sneeze, gym activity, physical activity, poor sleep, cold, combing hair |
| Comorbidities | Aneurysm of the temporal artery, aneurysm of occipital artery, occipital neuralgia, coronary artery disease, hypertension, migraine, myasthenia gravis, type 2 diabetes mellitus, chronic tension headache |
Missing data were not considered for the calculation of the frequency percentages.
*TCA includes amitriptyline and nortriptyline.
BoNT-A, botulinum toxin type A; VRS, verbal rating scale (intensity 1=least severe to 10= most severe).
The correct diagnosis of NH was made within 18±12.8 (median ±SE) months after the first episode of headache with median intensity of 5±0.2 (SE) on verbal rating scale (VRS) of 1–10 (intensity: 1=least severe to 10=most severe). The median diameter of pain was 4±0.2 (SE) cm. Out of 32 patients with known duration of attack (pain), 17 (53.13%) patients experienced <30 min of attack, 9 (28.13%) between 30 and 120 min duration and 6 (18.75%) patients had >120 min duration of attack.
Patients with NH in the study had 3±2 (median ±SE) headache attacks per day with frequency of 9.5±3.6 (median ±SE) days per month. The localisation of pain was observed in 68 patients. Out of 68 patients, 26 (38.24%) patients had pain localised to the left side, 35 (51.47%) patients had right side pain and 7 (10.29%) patients had bilateral pain (two separate area). Forty-three (54.43%) patients had parietal area of the brain affected, 17 (21.52%) had frontal region, 11 (13.92%) had occipital region and 8 (10.12%) had temporal region affected. In the study cohort, 32 (44.44%) patients described pain as pressure like, 12 (16.67%) described it as stabbing pain and 9 (12.50%) patients had burning pain. Out of 68 patients who have reported presence or absence of tenderness associated with pain in the study, 24 (35.29%) patients had tenderness with pain.
There were 47 (69.12%) patients in the study with the temporary relief of the symptoms. Forty (57.97%) patients had complete resolution of the headache after treatment. Sixty-six patients in the study had received the known therapeutic interventions and rest 14 patients’ interventions status were not known. In the study, 34 (52.31%) patients were treated with gabapentin, 11 (16.92%) with carbamazepine, 12 (18.46%) with BoNT-A treatment, 3 (4.69%) with triptan, 9 (13.6%) with TCA, 8 (12.31%) with lamotrigine, 3 (4.69%) with topiramate, 2 with metoprolol, 1 with neurotropin, 1 with duloxetin, 1 with pregabalin, 1 with sodium valproate and 2 underwent nerve block. Besides that, 32 patients had tried NSAIDs, 2 tried acetaminophen and 2 tried acupuncture. Most of the patients received two or more combinations of drugs.
Characteristics of the patients with complete resolution after treatment
Table 3 lists the characteristics of patients with NH with and without complete resolution after treatment. Median age of patients with complete resolution was 47±2.5 (SE) years compared with 49±2.9 (SE) years in no-resolution group (p=0.1835). Female gender had higher prevalence of resolution (26 (65%) vs 14 (48.28%); p=0.1648) compared with no resolution, though evidence of significance was weak. Patients with complete resolution were diagnosed early with NH within 12±8.67 (SE) months from the first episode of headache compared with patients with no resolution being diagnosed within 24±32.14 (SE) months from the first headache attack (p=0.0249). There was no difference in intensity of pain and diameter of pain between the complete resolution and no-resolution groups (p=0.6991, p=0.2054, respectively).
Table 3.
Association of characteristics of the nummular headache with complete resolution after treatment
| Characteristics | Resolution (yes) | Resolution (no) | P value |
| Age (years; median ±SE; IQR) | 47±2.5 (33–56) | 49±2.9 (41–63) | 0.1835 |
| Gender | 0.1648 | ||
| Male | 14 (35%) | 15 (51.72%) | |
| Female | 26 (65%) | 14 (48.28%) | |
| Latency from the first attack to diagnosis (months; median ±SE) | 12±8.67 | 24±32.14 | 0.0249 |
| Age of onset of pain (years; median ±SE) | 41±2.73 | 43±2.96 | 0.9337 |
| Intensity of pain (VRS 1–10; median ±SE) | 6±0.25 | 5.5±0.32 | 0.6991 |
| Diameter of the pain (cm; median ±SE) | 4±0.23 | 4±0.30 | 0.2054 |
| Number of attacks per day (median ±SE) | 4±2.9 | 3±2.5 | 0.6191 |
| Frequency (days/month; median ±SE) | 19.5±5.49 | 9.5±1.70 | 0.1659 |
| Duration of attacks (min) | 0.0833 | ||
| <30 | 11 (64.71%) | 5 (38.46%) | |
| 30–120 | 5 (29.41%) | 3 (23.08%) | |
| >120 | 1 (5.88%) | 5 (38.46%) | |
| Temporary relief of headache | <0.0001 | ||
| Yes | 35 (87.50%) | 12 (42.86%) | |
| No | 5 (12.50%) | 16 (57.14%) | |
| Onabotulinum toxin A (BoNT-A) | 0.0024 | ||
| Yes | 12 (30%) | 0 (0%) | |
| No | 28 (70%) | 25 (100%) | |
| Triptan | 0.5554 | ||
| Yes | 1 (2.56%) | 2 (8%) | |
| No | 38 (97.44%) | 23 (92.00%) | |
| Tricyclic antidepressant (TCA)* | 0.1356 | ||
| Yes | 4 (7.50%) | 5 (20%) | |
| No | 37 (92.50%) | 20 (80%) | |
| Lamotrigine | 0.0002 | ||
| Yes | 0 (0%) | 8 (32%) | |
| No | 40 (100%) | 17 (68%) | |
| Gabapentin | 0.1163 | ||
| Yes | 24 (60%) | 10 (40%) | |
| No | 16 (40%) | 15 (60%) | |
| Carbamazepine | <0.0001 | ||
| Yes | 1 (2.50%) | 10 (40%) | |
| No | 39 (97.50%) | 15 (60%) |
Note that all percentages are column percentages to compare characteristics between complete resolution and no-resolution groups.
Missing data were not considered for the calculation of the frequency percentages.
*TCA includes amitriptyline and nortriptyline.
BoNT-A, botulinum toxin type A; VRS, verbal rating scale (intensity 1=least severe to 10=most severe).
Patients with complete resolution had higher prevalence of reported temporary relief of headache compared with patients without resolution (35 (87.50%) vs 12 (42.86%), p<0.0001). Patients treated with BoNT-A and gabapentin had a high prevalence of complete resolution of headache than no resolution (12 (30%) vs 0 (0%), p=0.0024 and 24 (60%) vs 10 (40%); p=0.1163). Lamotrigine and carbamazepine treatment had higher prevalence of no resolution of headache compared with resolution group (8 (32%) vs 0 (0%); p=0.0002 and 10 (40%) vs 1 (2.50%); p<0.0001, respectively).
RR to treatment
Table 4 mentions RR for the interventions. Most common interventions were gabapentin (n=34; RR=67.7%), NSAIDs (n=32; RR=65.6%), BoNT-A (n=12; RR=100%), carbamazepine (n=11; RR=9.09%), TCA (n=9; RR=44.4%) and lamotrigine (n=8; RR=0%). Other less common interventions were triptan (n=3; RR=66.7%), topiramate (n=3; RR=66.7%), acupuncture (n=2; RR=50%), acetaminophen (n=2; RR=50%), nerve block (n=2; RR=0%), neurotropin (n=1; RR=100%), duloxetine (n=1; RR=100%), pregabalin (n=1; RR=0%) and sodium valproate (n=1; RR=0%).
Table 4.
Treatment response of drugs used for nummular headache
| Treatment | Number of cases (n) | Complete resolution (A) | Response rate (A/n)*100 (%) |
| Gabapentin | 34 | 23 | 67.7% |
| NSAIDs | 32 | 21 | 65.6% |
| Onabotulinum toxin A (BoNT-A) | 12 | 12 | 100% |
| Carbamazepine | 11 | 1 | 9.09% |
| Tricyclic antidepressant | 9 | 4 | 44.4% |
| Lamotrigine | 8 | 0 | 0% |
| Topiramate | 3 | 2 | 66.7% |
| Triptan | 3 | 2 | 66.7% |
| Acupuncture | 2 | 1 | 50% |
| Acetaminophen | 2 | 1 | 50% |
| Nerve block | 2 | 0 | 0% |
| Neurotropin | 1 | 1 | 100% |
| Duloxetine | 1 | 1 | 100% |
| Pregabalin | 1 | 0 | 0% |
| Sodium valproate | 1 | 0 | 0% |
| Metoprolol | 2 | 0 | 0% |
NSAID, non-steroidal anti-inflammatory drug.
Discussion
NH has been reported by Pareja et al in the literature since 2002.2 According to a survey, NH comprises 0.25% of all headache consultation.15 According to The International Headache Society’s ICHD-III, the name coin-shaped cephalalgia is defined as NH categorised under primary headaches without an identifiable aetiology, (1) continuous or intermittent head pain, (2) exclusively on the scalp with four characteristics of sharply countered, fixed in size and shape, round or elliptical, 1–6 cm in diameter and (3) not met criteria of other headaches of ICHD-3 diagnosis.16 Unlike migraine, NH is not associated with nausea, vomiting, lacrimation, rhinorrhoea, sound or light sensitivity or focal neurological symptoms.
NH is most commonly present in the middle age group6 17 and the average age of patients in our study group is 47 years with only two paediatric cases. Studies report the predominance of NH in females with a ratio of 1.5–1, consistent with our findings of female to male 0.6/0.4.6 18 NH is most commonly unilateral19 but our study had 10% patients with bilateral pain which is supported by Dai et al review6 with 12% patients with bilateral pain. Pain mostly occurred on the right side and localised to parietal region, consistent with Rammohan et al.17 Nearly half of our study patients had pressure like quality of pain followed by stabbing and burning, with similar results reported by review by Dai et al.6 The average intensity of pain is mild to moderate with an average of 5/10 on VRS. The average pain diameter was 4 cm, findings consistent with other studies which reported 2–6 cm of pain.6 17 20
There are no standard treatment guidelines present for NH, but few drugs have been used for the management of NH. These drugs include NSAIDs, gabapentin, carbamazepine, BoNT-A, triptan, TCA and nerve blocks.4 A study of 21 patients with NH by Zhu et al,21 where 14/21 patients with NH were treated with different therapeutic approaches, concluded that NH can be effectively treated with acupuncture or combining amitriptyline with indomethacin, ibuprofen or carbamazepine. Chirchiglia et al22 reported the successful management of one case of NH by adding palmitoylethanolamide to topiramate. Both of these drugs are used for neuropathic pain and suggest that release of algogenic substances like neurokinins, substance-P and calcitonin gene-related peptide (CGRP) causes inflammation and pain. Due to the involvement of cutaneous branches, the pain is superficial. Use of PAE decreases degeneration of mast cells, prevents alteration of nerve fibres and reduces inflammation. Nerve block is used for the treatment of NH and a study by Dach et al12 showed that blocking greater occipital nerve can relieve pain.
Our study found that gabapentin is the most frequently used therapeutic modality, with an RR of 67.7%. Martins and Abreu5 and Trigo et al23 concluded that gabapentin is the most frequently used medication with RR >50% in NH treatment and most common dose was 800 mg/day. An interesting finding of our study is the 100% treatment response with BoNT-A therapy. In support of our findings, studies by García-Azorín et al13 and Cuadrado et al4 concluded that BoNT-A significantly decreased the frequency of NH and may be a reasonable therapeutic approach for those patients, refractory to gabapentin. Another review study by Dai et al proved the effectiveness of BoNT-A treatment in 9/11 cases.6
The major strength of our study is that the study population analysed was only individual case reports and precisely evaluated the effectiveness of therapeutic interventions. However, our study has some limitations. First, the sample size is small because of lack of reporting, strict exclusion criteria and excluding other prospective studies with no individual patients’ data available. Although this was done to avoid duplicate patients and maintain the quality of article but it further reduced number of patients in the analysis. Second, there were not any randomised controlled studies available to support our study; hence, the evaluated treatment options represent the preferences of the physicians. Third, the treatment response of NH to newer anti-CGRP agents is not known. Nevertheless, given the limited availability of accurate information on this disease, this study shows a relatively large number of patients.
Conclusion
This is the first systematic study to report the effectiveness of treatment options after analysing the individual cases published in literature. The median age of diagnosis of NH was 47 years. Patients with NH had median three attacks per day with frequency of 9.5 days per month. Sixty-nine per cent of patients had temporary relief and 60% of patients had complete resolution of the headache after treatment. Female sex and early diagnosis were associated with complete resolution of NH. NSAIDs, gabapentin and BoNT-A were most commonly used medications, with RRs increasing in that order.
Footnotes
Contributors: UKP conceived of the idea. AA and SS reviewed the literature and collected the data with the help of UKP and PM. UKP and PM performed biostatistics, analysis and formulated the tables. UKP, PM and BC wrote the main draft of the manuscript with support from AK, KA and TK. TK supervised the project.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Headache Classification Committee of the International Headache Society (IHS) The International classification of headache disorders, 3rd edition (beta version). Cephalalgia 2013;33 10.1177/0333102413485658 [DOI] [PubMed] [Google Scholar]
- 2.Pareja JA, Caminero AB, Serra J, et al. Numular headache: a coin-shaped cephalgia. Neurology 2002;58:1678–9. 10.1212/WNL.58.11.1678 [DOI] [PubMed] [Google Scholar]
- 3.Pareja JA, Pareja J, Barriga FJ, et al. Nummular headache: a prospective series of 14 new cases. Headache 2004;44:611–4. 10.1111/j.1526-4610.2004.446011.x [DOI] [PubMed] [Google Scholar]
- 4.Cuadrado ML, López-Ruiz P, Guerrero Ángel L. Nummular headache: an update and future prospects. Expert Rev Neurother 2018;18:9–19. 10.1080/14737175.2018.1401925 [DOI] [PubMed] [Google Scholar]
- 5.Martins IP, Abreu L. Nummular headache: clinical features and treatment response in 24 new cases. Cephalalgia Reports 2018;1:1–8. [Google Scholar]
- 6.Dai W, Yu S, Liang J, et al. Nummular headache: peripheral or central? one case with reappearance of nummular headache after focal scalp was removed, and literature review. Cephalalgia 2013;33:390–7. 10.1177/0333102412474504 [DOI] [PubMed] [Google Scholar]
- 7.Queiroz LP Unusual headache syndromes. Headache 2013;53:12–22. 10.1111/head.12002 [DOI] [PubMed] [Google Scholar]
- 8.Rodríguez C, Herrero-Velázquez S, Ruiz M, et al. Pressure pain sensitivity map of multifocal nummular headache: a case report. J Headache Pain 2015;16:38 10.1186/s10194-015-0523-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathew NT, Kailasam J, Meadors L. Botulinum toxin type A for the treatment of nummular headache: four case studies. Headache 2008;48:442–7. 10.1111/j.1526-4610.2007.00960.x [DOI] [PubMed] [Google Scholar]
- 10.Trucco M, Mainardi F, Perego G, et al. Nummular headache: first Italian case and therapeutic proposal. Cephalalgia 2006;26:354–6. 10.1111/j.1468-2982.2006.01065.x [DOI] [PubMed] [Google Scholar]
- 11.Evans RW, Pareja JA. Nummular headache. Headache 2005;45:164–5. 10.1111/j.1526-4610.2005.05033.x [DOI] [PubMed] [Google Scholar]
- 12.Dach F, Éckeli Álan L., Ferreira KdosS, ÁL Éckeli, KdS F, et al. Nerve Block for the Treatment of Headaches and Cranial Neuralgias - A Practical Approach. Headache 2015;55:59–71. 10.1111/head.12516 [DOI] [PubMed] [Google Scholar]
- 13.García-Azorín D, Trigo-López J, Sierra Álvaro, et al. Observational, open-label, non-randomized study on the efficacy of onabotulinumtoxinA in the treatment of nummular headache: the pre-numabot study. Cephalalgia 2019;39:1818–26. 10.1177/0333102419863023 [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janjua MS, Singh P. Nummular headache. StatPearls. Treasure Island (FL), 2019. [PubMed] [Google Scholar]
- 16.Belvis R, Mas N, Roig C. [Changes introduced into the recent International Classification of Headache Disorders: ICHD-III beta classification]. Rev Neurol 2015;60:81–9. [PubMed] [Google Scholar]
- 17.Rammohan K, Mundayadan SM, Mathew R. Nummular headache: Clinico-epidemiological features in South Indian population. J Neurosci Rural Pract 2016;7:532–6. 10.4103/0976-3147.186984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grosberg BM, Solomon S, Lipton RB. Nummular headache. Curr Pain Headache Rep 2007;11:310–2. 10.1007/s11916-007-0209-1 [DOI] [PubMed] [Google Scholar]
- 19.Schwartz DP, Robbins MS, Grosberg BM. Nummular headache update. Curr Pain Headache Rep 2013;17:340 10.1007/s11916-013-0340-0 [DOI] [PubMed] [Google Scholar]
- 20.Dach F, Éckeli Álan L., Ferreira KdosS, et al. Nerve Block for the Treatment of Headaches and Cranial Neuralgias - A Practical Approach. Headache 2015;55:59–71. 10.1111/head.12516 [DOI] [PubMed] [Google Scholar]
- 21.Zhu K-yun, Huang Y, Zhong S-sheng, et al. [Nummular headache: 21 new cases and therapeutic results]. Zhonghua Yi Xue Za Zhi 2008;88:2935–7. [PubMed] [Google Scholar]
- 22.Chirchiglia D, Della Torre A, Signorelli F, et al. Administration of palmitoylethanolamide in combination with topiramate in the preventive treatment of nummular headache. Int Med Case Rep J 2016;9:193–5. 10.2147/IMCRJ.S106323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trigo J, García-Azorín D, Martinez Pias E, et al. Clinical characteristics of nummular headache and differentiation between spontaneous and posttraumatic variant: an observational study. J Headache Pain 2019;20:34 10.1186/s10194-019-0981-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y, Wei T. First three cases of scalp temperature change in symptomatic areas affected by nummular headache: a case report. BMC Neurol 2018;18:223 10.1186/s12883-018-1231-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Camacho-Velasquez JL Nummular headache associated with linear scleroderma. Headache 2016;56:1492–3. 10.1111/head.12894 [DOI] [PubMed] [Google Scholar]
- 26.Barón J, Rodríguez C, Ruiz M, et al. Atypical nummular headache or circumscribed migraine: the utility of pressure algometry. Pain Research and Management 2015;20:60–2. 10.1155/2015/567072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.López-Ruiz P, Cuadrado M-L, Aledo-Serrano A, et al. Superficial Artery Aneurysms Underlying Nummular Headache - 2 Cases and Proposed Diagnostic Work-Up. Headache 2014;54:1217–21. 10.1111/head.12398 [DOI] [PubMed] [Google Scholar]
- 28.Iwanowski P, Kozubski W, Losy J. Nummular headache in a patient with ipsilateral occipital neuralgia—A case report. Neurol Neurochir Pol 2014;48:141–3. 10.1016/j.pjnns.2013.09.005 [DOI] [PubMed] [Google Scholar]
- 29.Kurian M, Solomon GD. Can temporal course of pain determine patient response to specific medication in nummular headache? Headache 2014;54:1058–61. 10.1111/head.12331 [DOI] [PubMed] [Google Scholar]
- 30.López-Mesonero L, Porta-Etessam J, Ordás CM, et al. Nummular headache in a patient with craniosynostosis: one more evidence for a peripheral mechanism. Pain Medicine 2014;15:714–6. 10.1111/pme.12324 [DOI] [PubMed] [Google Scholar]
- 31.Mulero P, Matarazzo M, Pedraza MI, et al. Nummular headache related to exercise or Valsalva maneuver. clinical characteristics of 3 cases. Headache 2013;53:1167–8. 10.1111/head.12133 [DOI] [PubMed] [Google Scholar]
- 32.Yin H-L, Chui C, Tung W-F, et al. Nummular headache after trans-sphenoidal surgery: a referred pain-based headache syndrome. Neurol Neurochir Pol 2013;47:398–401. 10.5114/ninp.2013.36764 [DOI] [PubMed] [Google Scholar]
- 33.Irimia P, Palma J-A, Idoate MA, et al. Cephalalgia alopecia or nummular headache with trophic changes? a new case with prolonged follow-up. Headache 2013;53:994–7. 10.1111/head.12072 [DOI] [PubMed] [Google Scholar]
- 34.Danno D, Kawabata K, Tachibana H. Three cases of nummular headache effectively treated with Neurotropin(®). Intern Med 2013;52:493–5. 10.2169/internalmedicine.52.9161 [DOI] [PubMed] [Google Scholar]
- 35.Herrero-Velázquez S, Guerrero AL, Pedraza MI, et al. Nummular headache and Epicrania fugax: possible association of Epicranias in eight patients: table 1. Pain Medicine 2013;14:358–61. 10.1111/pme.12022 [DOI] [PubMed] [Google Scholar]
- 36.Man Y-H, Yu T-M, Li L-S, et al. A new variant nummular headache: large diameter accompanied with bitrigeminal hyperalgesia and successful treatment with carbamazepine. Turk Neurosurg 2012;22:506–9. 10.5137/1019-5149.JTN.3960-10.0 [DOI] [PubMed] [Google Scholar]
- 37.Yamazaki Y, Kobatake K. Successful treatment of nummular headache with Neurotropin®. J Headache Pain 2011;12:661–2. 10.1007/s10194-011-0382-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rocha-Filho PAS Nummular headache: two simultaneous areas of pain in the same patient. Cephalalgia 2011;31:874 10.1177/0333102411398156 [DOI] [PubMed] [Google Scholar]
- 39.Porta-Etessam J, Lapeña T, Cuadrado M-L, et al. Multifocal Nummular headache with trophic changes. Headache 2010;50:1612–3. 10.1111/j.1526-4610.2010.01773.x [DOI] [PubMed] [Google Scholar]
- 40.Chen W-H, Li T-H, Lee L-H, et al. Varicella-Zoster virus infection and nummular headache: a possible association with epicranial neuralgia. Intern Med 2012;51:2439–41. 10.2169/internalmedicine.51.7998 [DOI] [PubMed] [Google Scholar]
- 41.Guerrero Ángel L., Cuadrado ML, García-García ME, et al. Bifocal nummular headache: a series of 6 new cases. Headache 2011;51:1161–6. 10.1111/j.1526-4610.2011.01940.x [DOI] [PubMed] [Google Scholar]
- 42.Campbell WW, Sartori RJ. Nummular erythema in a patient with chronic daily headache. Headache 2003;43:1112 10.1046/j.1526-4610.2003.03215.x [DOI] [PubMed] [Google Scholar]
- 43.Evans RW Case studies of uncommon headaches. Neurol Clin 2006;24:347–62. 10.1016/j.ncl.2006.01.006 [DOI] [PubMed] [Google Scholar]
- 44.Trucco M Nummular headache: another case treated with gabapentin. J Headache Pain 2007;8:137–8. 10.1007/s10194-007-0375-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Guillem A, Barriga FJ, Giménez-Roldán S. Nummular headache secondary to an intracranial mass lesion. Cephalalgia 2007;27:943–4. 10.1111/j.1468-2982.2007.01328.x [DOI] [PubMed] [Google Scholar]
- 46.Tayeb Z, Hafeez F, Shafiq Q. Successful treatment of nummular headache with TENS. Cephalalgia 2008;28:897–8. 10.1111/j.1468-2982.2007.01456.x [DOI] [PubMed] [Google Scholar]
- 47.Pareja JA, Cuadrado ML, Fernández-de-las Peñas C, et al. Nummular headache with trophic changes inside the painful area. Cephalalgia 2008;28:186–90. 10.1111/j.1468-2982.2007.01490.x [DOI] [PubMed] [Google Scholar]
- 48.Baldacci F, Nuti A, Lucetti C, et al. Nummular headache dramatically responsive to indomethacin. Cephalalgia 2010;30:1151–2. 10.1177/0333102410361539 [DOI] [PubMed] [Google Scholar]
- 49.Dach F, Speciali J, Eckeli A, et al. Nummular headache: three new cases. Cephalalgia 2006;26:1234–7. 10.1111/j.1468-2982.2006.01197.x [DOI] [PubMed] [Google Scholar]
- 50.Robbins MS, Grosberg BM. Menstrual-related nummular headache. Cephalalgia 2010;30:507–8. 10.1111/j.1468-2982.2009.01947.x [DOI] [PubMed] [Google Scholar]
- 51.Álvaro LC, Garcí JM, Areitio E. Nummular headache: a series with symptomatic and primary cases. Cephalalgia 2009;29:379–83. 10.1111/j.1468-2982.2008.01722.x [DOI] [PubMed] [Google Scholar]
- 52.Cuadrado ML, Valle B, Fernández-de-las-Peñas C, et al. Bifocal nummular headache: the first three cases. Cephalalgia 2009;29:583–6. 10.1111/j.1468-2982.2008.01815.x [DOI] [PubMed] [Google Scholar]
- 53.Dabscheck G, Ian Andrews P. Nummular headache associated with focal hair heterochromia in a child. Cephalalgia 2010;30:1403–5. 10.1177/0333102410368439 [DOI] [PubMed] [Google Scholar]
- 54.Dusitanond P, Young W, Type BT. Botulinum toxin type A's efficacy in nummular headache. Headache 2008;48:1379 10.1111/j.1526-4610.2008.01245.x [DOI] [PubMed] [Google Scholar]
- 55.Ruscheweyh R, Buchheister A, Gregor N, et al. Nummular headache: six new cases and lancinating pain attacks as possible manifestation. Cephalalgia 2010;30:249–53. 10.1111/j.1468-2982.2009.01893.x [DOI] [PubMed] [Google Scholar]
- 56.Jiang L, Li M, Liu Q, et al. Nummular headache: 2 cases with good beta blocker responses and a narrative review. Headache 2019;59:593–602. 10.1111/head.13503 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjno-2020-000049supp001.pdf (65.3KB, pdf)
bmjno-2020-000049supp002.pdf (48.7KB, pdf)