Abstract
Background
Patients with coronavirus disease 2019 (COVID-19) present with diagnostic challenges because COVID-19 can cause varied end-organ failures that mimic respiratory distress of pulmonary origin. Early identification of concurrent complications can significantly alter patient management and course. Point-of-care ultrasound (POCUS) can be particularly useful in helping to differentiate concomitant complications with COVID-19. While lung POCUS findings related to COVID-19 have been published, little guidance exists on how ultrasound can be incorporated into a more comprehensive evaluation of patients under investigation for COVID-19.
Objectives
We devised a pathway called COVUS that incorporates POCUS into the initial evaluation of patients under investigation for COVID-19 to guide diagnosis and management.
Discussion
The pathway was derived based on a review of literature, consensus from the ultrasound faculty, as well as feedback from the entire faculty group at one academic institution with high volumes of patients with COVID-19. The scanning protocol uses a cardiac-first (rather than lung-first) approach to identify potential concomitant organ failure that may immediately alter management.
Conclusions
COVUS aims to maximize identification of the most immediately life-threatening complications while minimizing time at bedside and provider risk of exposure to COVID-19.
Keywords: 2019 novel coronavirus infection, algorithm, bedside technology, cardiomyopathy, point-of-care ultrasound, thromboembolic
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), or coronavirus disease 2019 (COVID-19), presents with clinical heterogeneity (1, 2, 3). While respiratory failure caused by lung injury from COVID-19 continues to be the primary clinical complication, other end-organ failures, such as myocardial injury leading to cardiomyopathy, vascular injury leading to deep venous thrombosis or pulmonary emboli, and exacerbations of existing conditions, are also common complications associated with the disease (1,4,5). Patients with cardiac manifestations and thromboembolic events suffer greater morbidity and mortality than those with isolated pulmonary findings (1,6,7). However, these extrapulmonary complications can present with tachycardia and hypoxia, making it challenging to differentiate from respiratory failure (2). Early identification of concurrent complications can significantly alter patient management and clinical course (7,8). Point-of-care ultrasound (POCUS) can be particularly useful in these circumstances in helping to differentiate or identify concomitant complications in patients with COVID-19. While lung ultrasound findings in patients with COVID-19 have been published, there exists little guidance regarding how ultrasound can be incorporated into a more comprehensive evaluation of patients under investigation for COVID-19 (9, 10, 11, 12, 13). The aim of this novel suggested protocol, called COVUS, is to describe a simple, tailored POCUS pathway for rapidly evaluating organ dysfunction that may change emergent management in persons with suspected COVID-19. The protocol name, COVUS, originated from a combination of COVID and POCUS. This protocol was developed through an iterative process in situ by the ultrasound faculty at an academic emergency department (ED) with high case volumes of COVID-19 in one of the first global epicenters of the pandemic. The protocol intends to assess for severe cardiopulmonary manifestations of COVID-19 while minimizing provider exposure risk.
Discussion
The COVUS protocol guides clinicians in performing a POCUS examination in patients under investigation (PUIs) for COVID-19 by using a sequence of binary questions to rapidly risk stratify and direct interventions. By protocolizing POCUS in these patients, clinicians can perform an expeditious POCUS examination and minimize their exposure to PUIs.
Derivation and Rationale
As COVID-19 ravaged populations worldwide, New York City became one of the first epicenters (14). As of July 2020, New York City had >200,000 patients with COVID-19 and > 18,000 people had died because of COVID-19 (15). Approximately 14% of the total patients with COVID-19 in New York City were treated at Columbia University Medical Center. The virus not only affected our patient population, but also had a significant impact on health care workers (14). One recent study found that >33% of health care providers who received testing in a large New York City health care system tested positive for COVID-19 (14). We now also know that greater viral load is associated with greater disease severity (16).
Patients with COVID-19 commonly exhibit a range of symptoms, including cough, dyspnea, chest pain, fatigue, or respiratory distress (2). The initial management of these patients centers around stabilization of the patients’ respiratory status. Concomitant cardiac complications cannot be differentiated by physical examination alone, because they can masquerade as respiratory distress and failure. However, these unidentified cardiac complications can have significant implications for management (8). Studies from Europe and Asia have shown that >33% of patients with COVID-19 have cardiac complications and suffer from greater morbidity and mortality (4,6,7). In addition, multiple emerging studies have revealed that cardiac involvement may be far more common than previously thought (17,18). Fortunately, earlier diagnosis and timely management may help reduce future morbidity and mortality (4,6,8).
Our Ultrasound Division developed this pathway to help guide triage of patients suspected of having COVID-19. We have 19 ultrasound faculty, which make up >15% of the entire ED faculty population. POCUS has been well established to improve morbidity and mortality in clinical uncertainty, especially in patients with undifferentiated dyspnea or shock (19). COVUS draws from previously established protocols and aims to provide a targeted comprehensive cardiopulmonary picture to guide resuscitation of PUIs for COVID-19, while simultaneously minimizing time at bedside to decrease possible viral exposure to the provider.
The pathway was derived based on existing evidence in the published literature as well as clinical experience. We developed this protocol partly in response to the overwhelming concentration of lung POCUS in COVID-19 literature. We focused on organ systems that could make the biggest difference in emergent management. As such, we had initially discussed only incorporating cardiac POCUS into the clinical evaluation of PUIs to minimize exposure as the pulmonary findings are relatively stereotyped (9,11,12). However, we have witnessed 2 of our PUIs for COVID-19 with other pulmonary complications, such as pneumothorax and empyema. These pathologies can be easily and rapidly diagnosed by POCUS with minimal additional exposure to the provider, and therefore lung POCUS was included in the COVUS pathway to assess pulmonary complications, to establish a baseline for inpatient teams, as well as to provide a more comprehensive evaluation of PUIs. However, we felt that a cardiac-first approach was more critical than the lung POCUS examination alone because it has the potential to provide more timely information regarding underlying concomitant pathologies that require more emergent intervention.
We presented our pathway during an online departmental meeting and circulated the pathway through our departmental email. The Emergency Ultrasound Division was available to answer any questions about the pathway throughout the pandemic.
Scanning Protocol
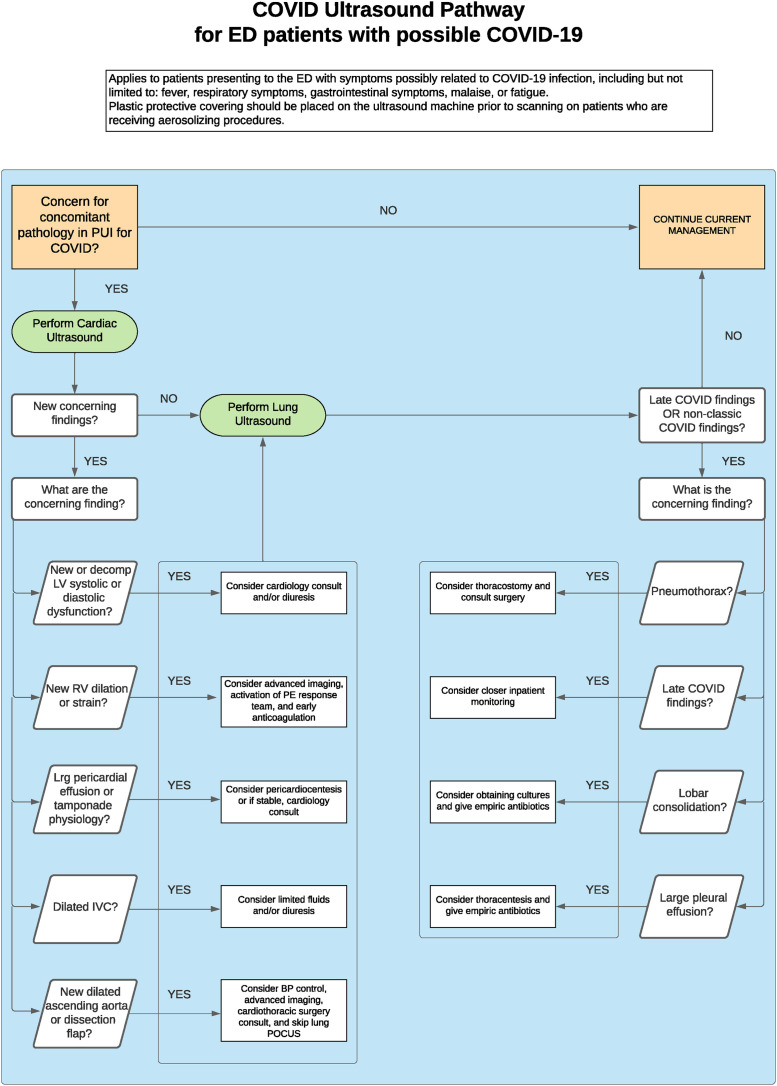
COVUS is appropriate when clinicians are concerned for concurrent organ injury in patients who present with COVID-19–like symptoms (Figure 1 ). Because of the personal risk of COVID-19 exposure while scanning, we left the inclusion criteria for performing COVUS to the discretion of the treating clinician. In COVUS, an initial cardiac POCUS is performed to evaluate for any emergent or urgent treatable causes. COVUS includes the 4 standard cardiac windows as well as the inferior vena cava (IVC) for the cardiac assessment: parasternal long axis view, parasternal short axis view, apical-4 chamber view, subxiphoid view, and longitudinal view of the IVC. The COVUS pathway uses only 1 transducer, the phased array transducer, for the entirety of the study to minimize materials exposure and for ease of postscan disinfection of the device (20,21).
Figure 1.
COVUS pathway for the diagnosis and management of PUI for COVID-19. ED = emergency department; IVC = inferior vena cava; LV = left ventricle; RV = right ventricle; PE = pulmonary embolism; PUI = patients under investigation; BP = blood pressure; POCUS = point-of-care ultrasound.
The cardiac POCUS evaluates for gross and urgent abnormalities by focusing on the 5 Es of emergency physician–performed focused cardiac ultrasound as proposed by Kennedy Hall et al. (22). For expeditious evaluation, we advocate for a qualitative visual estimate of each parameter. This protocol evaluates for ejection (left ventricular systolic and diastolic dysfunction), equality (right ventricular size and function), effusion (pericardial effusion, with or without tamponade physiology), exit (aortic root diameter), and entrance (IVC collapsibility) (22). Probable cardiac complications found in patients with COVID-19 can be found in Table 1 .
Table 1.
COVUS Applications and Sonographic Findings
| COVUS | Suggested Views | Potential Findings in COVID-19 |
|---|---|---|
| Cardiac | Parasternal long, parasternal short, apical 4-chamber, subxiphoid, and IVC | Decreased ejection fraction (consider cardiomyopathy, myocarditis); dilated IVC (consider left or right heart failure); dilated RV (consider pulmonary embolism) |
| Lungs | Bilateral anterior, bilateral axillary, and bilateral posterior (use lawnmower technique for assessment) | Early findings: focal B-lines and disrupted or thickened pleural line |
| Late findings: coalesced B-lines, small peripheral consolidations (with or without air bronchograms), and small pleural effusions |
COVID-19 = coronavirus disease 2019; COVUS = combination of COVID and point-of-care ultrasound; IVC = inferior vena cava; RV = right ventricle.
If there is any evidence of acute cardiac pathology, clinicians are encouraged to manage the patient accordingly, which may include additional imaging, such as computed tomography, consultation with other subspecialty services, and admission to a higher level of care for closer inpatient monitoring (4,6,7). The flow chart in Figure 1 shows the relative urgency of each POCUS examination and suggested interventions based on these findings.
If there is no acute cardiac pathology identified, the lung POCUS increases in value and therefore becomes more essential in evaluation. COVUS lung POCUS evaluates the extent of COVID-19 lung involvement as well as for other possible pulmonary pathologies. Using the same phased array transducer, clinicians evaluate the anterior, midaxillary, and posterior lung fields bilaterally using the lawnmower technique (23). Early lung ultrasound findings in patients with COVID-19 include coarse pleural lines and patchy focal B-lines (9,11). Late lung ultrasound findings in patients with COVID-19 include coalescent B-lines, subpleural consolidations with or without air bronchograms, and small pleural effusions (9,11). These probable lung findings in patients with COVID-19 are outlined in Table 1.
Pulmonary pathology in patients with COVID-19 appears as a multifocal process and often involves multiple lung fields (9, 10, 11). If there is any evidence of late lung pathology, the clinician should strongly consider admission for closer inpatient monitoring. Patients should also be evaluated for additional pathologies, including pneumothoraces, large pleural effusions, lobar consolidations, and empyemas. These manifestations are uncommon in patients with COVID-19 and if identified may suggest alternative or coexisting complications that should be managed accordingly (9,11).
Limitations
COVUS was developed in a single urban academic center with high volumes of critically ill patients with COVID-19. This protocol is limited in the identification of all possible COVID-19 complications, but targets the most immediately potentially life-threatening complications. We recognize that this pathway may not be feasible or the best fit for all practice settings because it was designed by and for emergency physicians with experience in integrating POCUS into their clinical management. The potential for practice variability exists as we did not impose firm guidelines as to when to perform COVUS. For example, some of our providers used COVUS for almost all PUIs, whereas others only performed COVUS for patients with abnormal vital signs. While we do not present any outcome data with regard to this element, practice variability may influence and potentially bias outcomes based on heterogenous inclusion criteria. While our approach allowed a realistic in situ description of the implementation of this approach in our ED, future work instituting more standardized inclusion criteria would allow greater uniformity of the sample population.
Conclusions
Patients presenting to the ED with COVID-19–like symptoms present a clinical challenge to clinicians because the varied manifestations of this relatively new disease process are continually being discovered. As a result, the disposition and management plan for such patients from the ED can often be complicated and may result in significant concurrent pathologies being overlooked. Our goal was to provide emergency physicians with a rapid and intuitive use of POCUS, whose results may significantly alter the course of the patient's therapy. Similar to the RUSH protocol that was designed to aid in the diagnostic challenge of undifferentiated hypotension to tailor therapy, our pathway aims to guide undifferentiated complications of patients presenting with COVID-19 with a focus on organs that may require immediate change in management (24).
While the COVUS pathway does not introduce any new imaging modalities and is largely derived from existing protocols, it differs from other COVID protocols in that it advances a cardiac-first approach, uses a single transducer, and advocates for a lawnmower technique for lung POCUS in lieu of recording individual lung fields with separate videos. COVUS focuses on the most vital systems affected by COVID-19, namely the heart, lungs, and IVC (25,26).
Some COVID POCUS protocols only focus on lung ultrasound, which may overlook common cardiac complications (10,18). Other protocols propose scanning the entire body, which we felt would be too time consuming and unnecessarily increase exposure for providers (25). We considered incorporating other POCUS modalities, such as the evaluation of deep venous thrombosis in the lower extremities. However, without evidence of right heart strain or end-organ failure and injury, identification of a deep venous thrombosis would not lead to clinically significant changes in management in the emergent setting. Our institution has been routinely anticoagulating patients with elevated D-dimer and other inflammatory markers. These anticoagulation recommendations exist for most patients hospitalized for COVID-19 (27). Pulmonary findings not consistent with classic COVID-19 may lead to additional therapeutic procedures, such as antibiotics or even surgery. The aim of the COVUS pathway is to identify problems that may require urgent intervention in addition to diagnosis of COVID-19 infection. The pathway also considers provider and equipment exposure. The longer clinicians remain at the bedside, the higher the risk for infection transmission. In addition, a greater number of required transducers means a more tedious postscanning cleaning processes. The pathway attempts to balance comprehensiveness with expedience; we hope to achieve maximum determination of associated pathology that may significantly alter management while maintaining minimal risk of infectious spread.
Thus far by using the COVUS protocol, anecdotally, our clinicians have found new cardiomyopathies, submassive pulmonary emboli, and other significant findings that acutely changed management in patients with suspected COVID-19. In our experience, the COVUS pathway has provided our clinicians with a quick, real-time bedside screening tool for the assessment and treatment of PUIs.
Future Directions
We have started to prospectively collect data on the effect of COVUS in patient management in the ED. Future work involving application of COVUS across a diverse set of clinical settings and practice environments will help inform clinicians on the applicability of COVUS in their department. Our hope is that by sharing our initial experience with this pathway, we may jumpstart a broader investigation on the applications of POCUS in the evaluation and management of COVID-19 in the acute care community.
Footnotes
Reprints are not available from the authors.
References
- 1.Fried J.A., Ramasubbu K., Bhatt R., et al. The variety of cardiovascular presentations of COVID-19. Circulation. 2020;141:1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kakodkar P., Kaka N., Baig M.N. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19) Cureus. 2020;12:e7560. doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W.-J., Ni Z.-Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo T., Fan Y., Chen M., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikdeli B., Madhavan M.V., Jimenez D., et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonow R.O., Fonarow G.C., O’Gara P.T., Yancy C.W. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5:751–753. doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 7.Arentz M., Yim E., Klaff L., et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur Heart J. 2021;42:206. doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peng Q.-Y., Wang X.-T., Zhang L.-N. Chinese Critical Care Ultrasound Study G. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46:849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soldati G., Smargiassi A., Inchingolo R., et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID-19: a simple, quantitative, reproducible method. J Ultrasound Med. 2021;40:1413–1419. doi: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manivel V., Lesnewski A., Shamim S., Carbonatto G., Govindan T. CLUE: COVID-19 lung ultrasound in emergency department. Emerg Med Australas. 2020;32:694–696. doi: 10.1111/1742-6723.13546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lepri G., Orlandi M., Lazzeri C., et al. The emerging role of lung ultrasound in COVID-19 pneumonia. Eur J Rheumatol. 2020;7(suppl 2):S129–S133. doi: 10.5152/eurjrheum.2020.2063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Federation for Ultrasound in Medicine and Biology Safety Committee. Abramowicz J.S., Akiyama I., et al. World Federation for Ultrasound in Medicine and Biology position statement: how to perform a safe ultrasound examination and clean equipment in the context of COVID-19. Ultrasound Med Biol. 2020;46:1821–1826. doi: 10.1016/j.ultrasmedbio.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moscola J., Sembajwe G., Jarrett M., et al. Prevalence of SARS-CoV-2 Antibodies in Health Care Personnel in the New York City Area. JAMA. 2020;324:893–895. doi: 10.1001/jama.2020.14765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.New York City Department of Health Website COVID-19: Data. https://www1.nyc.gov/site/doh/covid/covid-19-data.page Available at:
- 16.Zheng S., Fan J., Yu F., et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020;369:m1443. doi: 10.1136/bmj.m1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang L., Zhao P., Tang D., et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13:2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puntmann V.O., Carerj M.L., Wieters I., et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69:e27–e54. doi: 10.1016/j.annemergmed.2016.08.457. [DOI] [PubMed] [Google Scholar]
- 20.American College of Emergency Physicians Website ACEP COVID-19 field guide: ultrasound cleaning. https://www.acep.org/corona/covid-19-field-guide/work-safety/ultrasound-cleaning/ Available at:
- 21.American College of Emergency Physicians Website American College of Emergency Physicians policy statement: guideline for ultrasound transducer cleaning and disinfection. https://www.acep.org/globalassets/new-pdfs/policy-statements/guideline-for-ultrasound-transducer-cleaning-and-disinfection.pdf Available at:
- 22.Kennedy Hall M., Coffey E.C., Herbst M., et al. The “5Es” of emergency physician-performed focused cardiac ultrasound: a protocol for rapid identification of effusion, ejection, equality, exit, and entrance. Acad Emerg Med. 2015;22:583–593. doi: 10.1111/acem.12652. [DOI] [PubMed] [Google Scholar]
- 23.Saraogi A. Lung ultrasound: present and future. Lung India. 2015;32:250–257. doi: 10.4103/0970-2113.156245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perera P., Mailhot T., Riley D., Mandavia D. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am. 2010;28:29–56. doi: 10.1016/j.emc.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Sikachi R., Agrawal A. Whole body point-care ultrasound for COVID-19: a multi-system approach to a multi-system disease. Anaesthesia. 2020;75:1114–1115. doi: 10.1111/anae.15087. [DOI] [PubMed] [Google Scholar]
- 26.Fox S., Dugar S. Point-of-care ultrasound and COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc019. [DOI] [PubMed] [Google Scholar]
- 27.Barnes G.D., Burnett A., Allen A., et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020;50:72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]