Abstract
OBJECTIVE:
It is common among medical students to falsely attribute bodily sensations/symptoms and holds a belief of having a medical illness with varying level of conviction. We studied and compared this condition known as “medical student syndrome”, a type of hypochondriasis, between preclinical and clinical years students.
METHODOLOGY:
This research was a descriptive study where a total of 100 students were approached and were asked to complete a short form of health anxiety inventory (SHAI) which has Cronbach's alpha 0.855. No personal identifiers were included in the study questionnaires. All statistical analyses were performed using the SPSS statistical software package (IBM SPSS Statistics Version 23, SPSS Inc., Chicago, IL, USA).
RESULTS:
The response rate among participants was 88% (42 from preclinical and 48 from clinical years of training). Health-related anxiety (SHAI main section score ≥ 18) was found in 14.77% of students with a higher proportion in preclinical than clinical, 16.66% and 13.04%, respectively. The difference was not significant between the two groups (χ2 = 0.429 [1], P = 0.766). Students having medical professional in family had lower rate of health-related anxiety, χ2 (1, n = 88) = 0.228, P = 0.633. The association between family or personal history of psychiatry or medical illness was not significant with SHAI scores. No relation was noted between current health anxiety (SHAI score) and the number of visits to the doctor per year before entering the medical course (χ = 0.174, P = 0.112).
CONCLUSION:
Every seventh medical student was found to have health-related anxiety. It was not affected by personal and family history of either psychiatric or medical illness.
Keywords: Education, health-related anxiety, hypochondriasis, medical students
Introduction
It is common for medical students to experience anxiety related to their health and hold a belief of having a medical illness with varying levels of conviction. This condition has been described in the literature as “medical student syndrome'’ or “medical student disease”. It is thought to arise due to false attribution of bodily sensations/symptoms to the illness being studied by students during their medical training. It is considered a type of hypochondriasis, a kind of health anxiety disorder. Compared to students of other streams, medical students are considered more prone to this condition.[1] However, the opposite finding has also been reported by other studies which found a lower rate of health-related anxiety in medical students compared to non-medical students.[2]
Studies have reported that health-related anxiety is more common in the early years and reduces as clinical exposure starts during later years of medical training,[3,4,5] which may be the reason behind the lower prevalence of health anxiety found in few studies involving final-year students.
Medical students are considered the vulnerable population because of as nature of the level of competence competition faced by them at different levels and nature of training. There is abundance of studies in medical students exploring the level of stress and problems of psychiatric disorders. However, these studies have used instrument or tools for anxiety assessment which does not reliably differentiate pathological anxiety. It is known that stress, to a certain extent, can work as “Eustress” and enhance performance.[6] Therefore, it is important to differentiate between “Distress” and “Eustress.” Unlike other anxiety measuring tools, Health Anxiety Inventory can reliably differentiate hypochondriacal concerns from anxiety associated with physical illness and other anxiety disorders.[7,8]
A short version of this tool known as SHAI has been applied both in normal and medically ill population. It has also been used in the student population and found reliable in differentiating between normal anxiety and abnormal health-related anxiety.
There are only a few studies which explored health anxiety in the medical students in India and assessed the effect of clinical exposure on health anxiety during medical training. Therefore, it was worth exploring and comparing health anxiety between preclinical and clinical years of medical trainees in India.
Methodology
A cross-sectional descriptive study was conducted among medical students in North India. One hundred students are enrolled for the MBBS course each year in our institute. The names of 100 preclinical students (MBBS batch 2017) and 100 clinical students (MBBS batch 2015) were arranged in alphabetical order and listed as serial number 1–100 in two separate lists. The first group was from junior MBBS batch who are yet to expose to clinical posting, while another group was of intern students doing rotational clinical Posting in different medical branches. Every alternate student (serial number 1, 3, 5, and so on) from the list of each batch (50 from preclinical years and 50 clinical years) was approached for the participation in the study. Students were informed that they can pick up the form from and return into a box placed in the common facility area of their residential campus. No personal identifiers were included in the questionnaires. There was no way for either data collector or data analyzer or other investigators to know the identity of any individual response. This anonymous approach of data collection ensured that participants respond to the questionnaire with their free will and without the worry of being identified and judged based on their response.
Each student completed the short form of health anxiety inventory (SHAI) with the following additional questions: personal history of psychiatric illness, personal history of medical illness, family history of medical illness, family history of psychiatric illness, and the presence of medical professional(s) in the family.
Statistical analyses
All statistical analyses were performed using the SPSS statistical software package (IBM SPSS Statistics Version 23, SPSS Inc., Chicago, IL, USA). Mann–Whitney U-test was used to compare the score of individual items of SHAI. One-way ANOVA was used to analyze multiple categorical variables between the two groups. Independent sample t-test was used to find the difference in the mean score of continuous variable such as mean age. The mean total score of SHAI between the two groups was analyzed by both Independent sample t-test and Mann–Whitney U-test.
Ethical consideration
The institutional ethic committee approved the study (Letter No – AIIMS/IEC/19/637). Participants were given the contact number of mental health specialist in case they feel the need to consult for health-related anxiety.
Short health anxiety inventory
It is a shorter version of the original health anxiety inventory and has 18 items. SHAI[8] consists of two factors assessing (a) the perceived likelihood of becoming seriously ill (“illness likelihood”), main section, and (b) the perceived negative consequences of being seriously ill (“negative consequences”).
It has been reliably used in both the general population including students and anxiety disorder patients.[9] Its internal reliability has been proven to be from good to excellent (Cronbach's alpha = 0.87–0.95) in the student population.[9,10,11,12]
Each item in the scale has four choices from a to d and generates the score from 0 to 3, respectively, for each response. Significant health anxiety is indicted by a score of 18 or above in the main part of the scale and has been used in both clinical practice and previous research studies.[13,14]
Results
The response rate among participants was 88%, 42 students from preclinical and 48 from clinical years of training.
Figure 1 shows that the distribution of SHAI score was normally distributed (skewness: 0.264, kurtosis: 0.523, and P value on Shapiro–Wilk test: 0.058). Reliability statistics analysis found SHAI to have good internal consistency (Cronbach's alpha: 0.855) and acceptable item-total correlation (Cronbach's alpha: 0.748).
Figure 1.
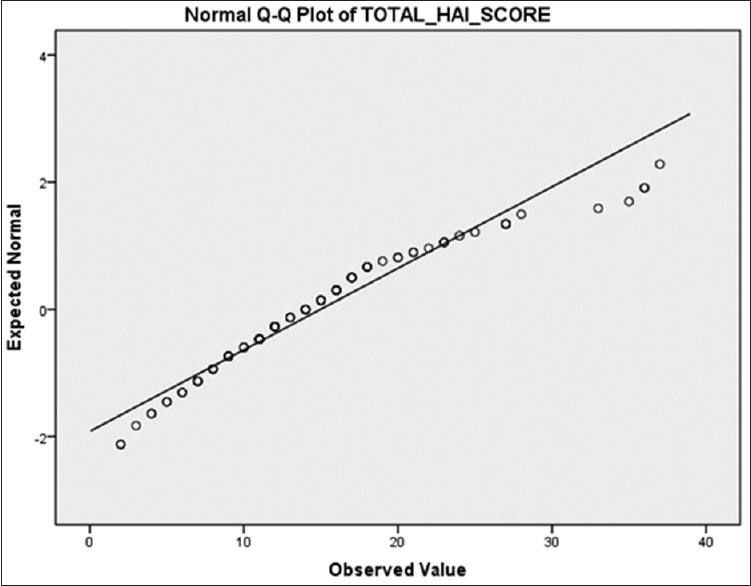
Normal Q–Q plot of short form of health anxiety inventory total score
MBBS students in preclinical years have higher SHAI total and main section scores [Table 1]. In the negative consequence section, clinical students have higher scores. However, the difference in SHAI scores (total, main section score, or negative consequence section) between the two groups was not statistically significant, P = 0.242, 0.299, and 0.730, respectively.
Table 1.
Short health anxiety inventory score: comparison between preclinical and intern students
| SHAI | Preclinical | Internship | Mean difference | Independent Sample test | Mann- Whitney U-test | |||
|---|---|---|---|---|---|---|---|---|
| t | P | Mean rank | U | P | ||||
| Main section (illness likelihood) | 12.45±5.731 | 11.28±6.748 | 1.170±1.341 | 0.872 | 0.385 | 47.45a | 842 | 0.299 |
| 41.80b | ||||||||
| Negative consequence section | 3.12±1.941 | 3.13±2.257 | −0.011±0.451 | −0.025 | 0.980 | 45.46a | 925 | 0.730 |
| 43.62b | ||||||||
| Total (main + negative consequences) | 15.57±6.833 | 14.41±8.635 | 1.158±1.671 | 0.693 | 0.490 | 47.83a | 826 | 0.242 |
| 41.46b | ||||||||
SHAI=Short form of health anxiety inventory a = Preclinical, b = Intern
Health-related anxiety (SHAI main section score ≥ 18) was found in 14.77% with a higher proportion in preclinical students than clinical, 16.66% and 13.04%, respectively. The difference was not significant between the two groups (χ2 = 0.429 [1], P = 0.766).
Table 2 shows individual items of SHAI, which indicates a statistically significant difference in item no 3 (bodily sensation), 4 (resisting the thoughts of illness), and 9 (thinking about an illness) with P = 0.012, 0.049, and 0.018, respectively. Scores of other items in SHAI did not differ between the two groups of students.
Table 2.
Comparison of 18 items of short health anxiety inventory between preclinical and intern students
| Items in SHAI (1- 18) | Median | Mean Ranka | Mean Rankb | U | P |
|---|---|---|---|---|---|
| Worry about health | 1 | 46.45 | 42.72 | 884 | 0.381 |
| Aches/pains | 1 | 47.07 | 42.15 | 858 | 0.330 |
| Bodily sensations | 1 | 51.15 | 38.42 | 686.500 | 0.012 |
| Thoughts of illness | 1 | 49.63 | 39.82 | 750.500 | 0.049 |
| Afraid of serious illness | 1 | 45.32 | 43.75 | 931.500 | 0.750 |
| Images of myself being ill | 0 | 44.60 | 44.41 | 962 | 0.970 |
| Difficulty taking my mind off thoughts about my health | 0 | 45.02 | 44.02 | 944 | 0.836 |
| Initially relieved but the worries sometimes return later | 0 | 43.49 | 45.42 | 923.500 | 0.659 |
| Think of illness | 1 | 50.52 | 39.00 | 713 | 0.018 |
| Bodily sensation or change what I means | 1 | 45.44 | 43.64 | 926.500 | 0.714 |
| Risk of developing serious illness | 1 | 44.06 | 44.90 | 947.500 | 0.869 |
| Have a serious illness | 1 | 45.48 | 43.61 | 925 | 0.701 |
| Unexplained bodily sensation | 1 | 42.11 | 46.68 | 865.500 | 0.368 |
| Worry about health | 1 | 40.17 | 48.46 | 784 | 0.098 |
| Enjoying things in life | 1 | 47.98 | 41.33 | 820 | 0.192 |
| Serious illness chance of medicine to cure | 1 | 41.79 | 46.98 | 852 | 0.297 |
| Illness would ruin aspect of life | 1 | 43.21 | 45.27 | 912 | 0.623 |
| Serious illness and feel of loss of dignity | 0 | 45.74 | 43.37 | 914 | 0.623 |
aPreclinical, bIntern. SHAI=Short form of health anxiety inventory
On comparison of avoidance section of short health anxiety inventory [Table 3], no statistically significant difference was found in avoidance items except “avoid visiting a hospital for other reason” which was more common in preclinical (median = 2) than clinical students (median = 0), U = 713.5, P = 0.025. Reassurance seeking from family members for health anxiety was significantly more common in preclinical students (median = 4) than their seniors in clinical posting, (median = 2), U = 713.5, P = 0.015. No statistically significant difference was found in other reassurance items [Table 4].
Table 3.
Comparison of avoidance items of short health anxiety inventory between preclinical and intern students
| Avoidance items in SHAI | Median | Mean ranka | Mean rankb | U | P |
|---|---|---|---|---|---|
| Consulting your family doctor | 2 | 44.67 | 44.35 | 959 | 0.951 |
| Visiting a friend in hospital | 0 | 48.65 | 40.71 | 791.500 | 0.084 |
| Visiting a relative in hospital | 0 | 48.80 | 40.58 | 785.500 | 0.096 |
| Going to hospital for treatment | 1 | 43.67 | 45.26 | 931 | 0.756 |
| Talking about illness | 1 | 42.65 | 46.18 | 888.500 | 0.496 |
| Reading about illness | 0 | 44.43 | 44.57 | 963 | 0.974 |
| Visiting the hospital for other reasons | 1 | 50.51 | 39.01 | 713.500 | 0.025 |
| Watching TV program about illness | 1 | 48.89 | 40.49 | 781.500 | 0.107 |
| Listening to radio program about illness | 1 | 46.38 | 42.78 | 887 | 0.496 |
| Thinking about illness | 2 | 42.85 | 46.01 | 896.500 | 0.554 |
aPreclinical, bIntern. SHAI=Short form of health anxiety inventory
Table 4.
Comparison of reassurance items of short health anxiety inventory between preclinical and intern students
| Reassurance items in SHAI | Median | Mean ranka | Mean rankb | U | P |
|---|---|---|---|---|---|
| Friend | 4 | 46.25 | 42.90 | 892.500 | 0.530 |
| Family | 4 | 51.27 | 38.32 | 681.500 | 0.015 |
| Reading books | 4 | 47.90 | 41.39 | 823 | 0.221 |
| Checking body for changes | 4 | 49.42 | 40.01 | 759.5 | 0.074 |
| Family doctor | 3.5 | 43.00 | 45.87 | 903 | 0.590 |
| Nurses | 0 | 45.10 | 43.96 | 941 | 0.820 |
| Hospital outpatient clinic | 4 | 48.36 | 40.98 | 804 | 0.168 |
| Hospital casualty | 2 | 47.36 | 41.89 | 846 | 0.296 |
aPreclinical, bIntern. SHAI=Short form of health anxiety inventory
Students with a personal history of psychiatric illness obtained higher SHAI scores, but the association was not significant when tested on one-way ANOVA test (F [1, 83] = 0.753, P = 0.703). The association between family history of psychiatry or medical illness was also not statistically significant with SHAI score [Table 5].
Table 5.
Personal and family history of psychiatric and medical illness and medical professional in the family by short form of health anxiety inventory scores
| Variable | SHAI Score, Mean±SD | F | P* |
|---|---|---|---|
| Personal history of psychiatric illness | 14.97±7.804 | 0.354 | 0.703 |
| Personal history of medical illness | 14.99±7.917 | 0.753 | 0.388 |
| Family history of medical illness | 14.97±7.804 | 0.055 | 0.947 |
| Family history of psychiatric illness | 14.97±7.804 | 0.302 | 0.740 |
| Medical professional in family | 14.99±7.917 | 0.851 | 0.359 |
*One-way ANOVA, P value significant at 0.05. SD=Standard deviation, SHAI=Short form of health anxiety inventory
Students having a medical professional in the family had a lower rate of health-related anxiety (SHAI main section score =18) than those who did not have any medical professional in the family, though the difference was not statistically significant, χ2 (1, n = 88) = 0.228, P = 0.633.
This study found that medical students with high SHAI score had more tendency to visit family doctors (ρ = 0.368, P = 0.001), nurses (ρ = 0.451, P = 0.001), hospital outpatient clinic (ρ = 0.419, P = 0.001), hospital casualty n (ρ = 0.327, P = 0.002), and reading books for reassurance (ρ = 0.358, P = 0.001).
There was no correlation between SHAI score and the number of visits to the doctor per year before entering the medical course (ρ = 0.174, P = 0.112).
Discussion
Our study found that every seventh medical student was suffering from health-related anxiety, more in preclinical student than those in clinical posting. In both the groups, health anxiety was more than among the general population as reported previously.[15] It could be the result of limited knowledge of the medical disorder and a higher chance of misinterpretation of normal physiological variation and bodily changes in medical students.[16]
Earlier studies among medical students in India and other countries have also reported a higher prevalence of stress and anxiety up to 80%.[17,18,19,20,21,22,23,24] However, previous studies have used the instruments which are not able to identify pathological anxiety from anxiety usually found in medical students. For example, the study by Singh and Jha administered the Comprehensive Anxiety Test to assess anxiety among medical students.[18] Test item response had only two choices yes or no and had items measuring academic-related anxiety (not health-related anxiety) like “Do you have the fear of being unsuccessful even after thorough preparations?” Another tool commonly used in many studies to assess medical students’ stress and anxiety is Depression Anxiety Stress Scales (DASS).[25] It has the items which seem to be extraneous with respect to health anxiety assessment. For example, the item 14 in DASS-42 “I found myself getting impatient when I was delayed in any way [e.g., lifts, traffic lights, being kept waiting)]” does not seem to assess any dimension of health-related anxiety.
Recent studies in medical students of Saudi Arabia and Pakistan have found the prevalence of health anxiety approximately similar to our study, 17.4% and 11.9%, respectively.[14,26] While the former used Hypochondria/Health Anxiety Questionnaire, the later applied SHAI.
These findings are similar to a recent study conducted among 513 medical students in a developing country in which 11.9% scored =18 on SHAI main section score. However, the authors didn't find any significant effect of the academic year on the presence of significant hypochondriacal fears related to health among medical students.[14]
Our study found that anxiety among clinical year students regarding their health compared to preclinical students is not statically significant. A recent comparative study among medical students of Taif University found a statistically significant difference in health anxiety between the student of preclinical and clinical years (21% vs. 14%, P = 0.028).[26] However, other studies were not able to prove any significant association between anxiety and stage of training (preclinical or clinical).[4,5,14] They have reported that health anxiety reduced as the student advances in medical training, but the effect was not significant.
A cross-sectional study in medical students of a Brazilian university has found the higher rates of anxiety in students in the first half of the course than in the second half. However, the difference was not statistically significant.[5]
A study in medical students of Guy's, King's, and St Thomas’ School of Medicine (GKT) in London in the year 2004 found a statistically significant difference in health anxiety between year 1 and 4 of the medical course.[2] However, the study has also found that medical students were less health anxious compared to English and Law students, (F = 30.257, P < 0.001).
A recent meta-analysis among health science students in China has found that the pooled prevalence of hypochondriacal symptoms was 28% (95% confidence interval = 19.0%–38.0%) with raw prevalence ranging from 15% to 55%.[16] There is no significant effect of the study year on health illness anxiety. It is important to note that six of seven studies included in the meta-analysis used the Minnesota Multiphasic Personality Inventory-Hypochondriasis scale (MMPI-Hs). Most of the items in the scale are focused on somatic symptoms and bodily sensation. Each item in the scale elicits true or false response rather than grading the possibility on an ordinal or Likert scale. MMPI-Hs has been found to overestimate hypochondriacal concerns in the medically ill population. Unlike MMPI-Hs, SHAI used in our study can reliably differentiate hypochondriacal concerns from anxiety due to medical illness or other anxiety disorders.[11]
Lower prevalence of health anxiety found in our study could be the result of the structure of the medical course and teaching methods used for MBBS trainees. An integrated teaching approach covers all aspects of a disorder at one time reducing the chance for the students to speculate about the likelihood of being ill based on symptoms and bodily sensations.
Lower prevalence of health anxiety seen in our study among students having a medical professional in their family is concordant with previous studies.[7,8] This study found that medical students with a high SHAI score had more tendency to visit doctors (ρ = 0.368, P = 0.001). Reading books for reassurance seeking was more commonly reported by those obtained higher SHAI score. A similar relation was also seen by Eastin et al. while exploring the effects of health anxiety on information-seeking and health-care utilization behaviors.[27] They noted that a positive interaction revealed a significant positive interaction between health anxiety levels, health information seeking online, and visiting a doctor (β = 0.19, t = 4.25, R2= 0.06, P < 0.05) on regression analysis. A possible motivation for students could be a resolution or elimination of the ambiguities regarding their health after information seeking and medical consultation.
Limitations
The sample size is small. The design of this study was cross-sectional and correlational, which precludes causal inferences, for example, worry, body vigilance, and fear of cardiovascular symptoms that are uniquely related to health anxiety; it cannot be determined from these data whether such factors are a cause or consequence of health anxiety.
Conclusions
Our study found that every seventh medical student was suffering from health-related anxiety. Clinical year students were less anxious regarding their health compared to preclinical students, although the difference in SHAI score did not reach the level of statistical significance. Lower prevalence of health anxiety was seen in students having a medical professional in their family. Medical students with a higher degree of health anxiety were more likely to visit health professionals. Counseling programs if implemented at the beginning of the medical course can help students to develop coping skills to deal with health anxiety. The additional approach, already adopted by a few medical schools, is early clinical exposure during medical training via integrated teaching involving both preclinical and clinical medical teachers. Future longitudinal and dynamic studies can further explore medical students’ hypochondriacal concerns at multiple points during medical training and assess its impact on various aspects of medical students’ functioning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are thankful to medical students of Batch 2017 and Batch 2015 of All India Institute of Medical Sciences, Rishikesh, India.
References
- 1.Mahendran S, Jothipriya A. A comparative study on 2nd year syndrome among dental medical and nursing students. Int J Curr Adv Res. 2017;6:2954–7. [Google Scholar]
- 2.Singh G, Hankins M, Weinman JA. Does medical school cause health anxiety and worry in medical students? Med Educ. 2004;38:479–81. doi: 10.1046/j.1365-2929.2004.01813.x. [DOI] [PubMed] [Google Scholar]
- 3.Moss-Morris R, Petrie KJ. Redefining medical students’ disease to reduce morbidity. Med Educ. 2001;35:724–8. doi: 10.1046/j.1365-2923.2001.00958.x. [DOI] [PubMed] [Google Scholar]
- 4.Saravanan C, Wilks R. Medical students’ experience of and reaction to stress: The role of depression and anxiety. ScientificWorldJournal. 2014;2014:737382. doi: 10.1155/2014/737382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tabalipa FO, de Souza MF, Pfützenreuter G, Lima VC, Traebert E, Traebert J. Prevalence of anxiety and depression among medical students. Rev Brasil Educ Mé. 2015;39:388–94. [Google Scholar]
- 6.Teigen KH. Yerkes-Dodson – A law for all seasons. Theory Psychol. 1994;4:525–47. [Google Scholar]
- 7.Abramowitz JS, Deacon BJ, Valentiner DP. The short health anxiety inventory: Psychometric properties and construct validity in a non-clinical sample. Cognit Ther Res. 2007;31:871–83. doi: 10.1007/s10608-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med. 2002;32:843–53. doi: 10.1017/s0033291702005822. [DOI] [PubMed] [Google Scholar]
- 9.Alberts NM, Hadjistavropoulos HD, Jones SL, Sharpe D. The Short Health Anxiety Inventory: A systematic review and meta-analysis. J Anxiety Disord. 2013;27:68–78. doi: 10.1016/j.janxdis.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Wheaton MG, Deacon BJ, McGrath PB, Berman NC, Abramowitz JS. Dimensions of anxiety sensitivity in the anxiety disorders: Evaluation of the ASI-3. J Anxiety Disord. 2012;26:401–8. doi: 10.1016/j.janxdis.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Fergus TA, Valentiner DP. The short health anxiety inventory and multidimensional inventory of hypochondriacal traits: A comparison of two self-report measures of health anxiety. Cogn Thera Res. 2011;35:566–74. [Google Scholar]
- 12.Sulkowski ML, Mancil TL, Jordan C, Reid A, Chakoff E, Storch EA. Validation of a classification system of obsessive-compulsive spectrum disorder symptoms in a nonclinical sample. Psychiatry Res. 2011;188:65–70. doi: 10.1016/j.psychres.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 13.The IAPT Data Handbook: Guidance on Recording and Monitoring Outcomes to Support Local Evidence-Based Practice. Version 2.0. London: IAPT; 2011. [Google Scholar]
- 14.Zahid MF, Haque A, Aslam M, Aleem NA, Hussain S, Fahad H, et al. Health-related anxiety and hypochondriacal concerns in medical students: A cross-sectional study from Pakistan. Teach Learn Med. 2016;28:252–9. doi: 10.1080/10401334.2016.1155459. [DOI] [PubMed] [Google Scholar]
- 15.Sunderland M, Newby JM, Andrews G. Health anxiety in Australia: Prevalence, comorbidity, disability and service use. Br J Psychiatry. 2013;202:56–61. doi: 10.1192/bjp.bp.111.103960. [DOI] [PubMed] [Google Scholar]
- 16.Meng JJ, Li T, Zhang L, Li SQ, Yang J, Yuan H. The analysis of hypochondriac state of medical students and its influencing factors. China Higher Med Educ. 2017;12:1–2. [Google Scholar]
- 17.Hunter RC, Lohrenz JG, Schwartzman AE. Nosophobia and hypochondriasis in medical students. J Nerv Ment Dis. 1964;139:147–52. doi: 10.1097/00005053-196408000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Singh I, Jha A. Anxiety, optimism and academic achievement among students of private medical and engineering colleges: A comparative study. J Educ Dev Psychol. 2013;3:222–33. [Google Scholar]
- 19.Mehanna Z, Richa S. Prevalence of anxiety and depressive disorders in medical students. Transversal study in medical students in the Saint-Joseph University of Beirut. Encephale. 2006;32:976–82. doi: 10.1016/s0013-7006(06)76276-5. [DOI] [PubMed] [Google Scholar]
- 20.Yusoff MS, Abdul Rahim AF, Baba AA, Ismail SB, Mat Pa MN, Esa AR. Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian J Psychiatr. 2013;6:128–33. doi: 10.1016/j.ajp.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 21.Lupo MK, Strous RD. Religiosity, anxiety and depression among Israeli medical students. Isr Med Assoc J. 2011;13:613–8. [PubMed] [Google Scholar]
- 22.Inam SN, Saqib A, Alam E. Prevalence of anxiety and depression among medical students of private university. J Pak Med Assoc. 2003;53:44–7. [PubMed] [Google Scholar]
- 23.Rab F, Mamdou R, Nasir S. Rates of depression and anxiety among female medical students in Pakistan. East Mediterr Health J. 2008;14:126–33. [PubMed] [Google Scholar]
- 24.Mancevska S, Bozinovska L, Tecce J, Pluncevik-Gligoroska J, Sivevska-Smilevska E. Depression, anxiety and substance use in medical students in the Republic of Macedonia. Bratisl Lek Listy. 2008;109:568–72. [PubMed] [Google Scholar]
- 25.Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br J Clin Psychol. 2003;42:111–31. doi: 10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- 26.Althagafi SS, AlSufyani MH, Shawky OA, Afifi OK, Alomairi N, Masoodi I. The health anxiety in medical students, a comparative study from Taif University: Medical student's syndrome revisited. Br J Med Pract. 2019;12:a003. [Google Scholar]
- 27.Eastin MS, Guinsler NM. Worried and wired: Effects of health anxiety on information-seeking and health care utilization behaviors. Cyberpsychol Behav. 2006;9:494–8. doi: 10.1089/cpb.2006.9.494. [DOI] [PubMed] [Google Scholar]


