Abstract
INTRODUCTION:
The pandemic caused by novel coronavirus (severe acute respiratory syndrome coronavirus 2) in Wuhan, China, in December 2019 is a highly contagious disease. The World Health Organization has declared the outbreak of coronavirus diseases (COVID-19) as a global public health emergency. Currently, the research on novel coronavirus is still in the primary stage. The aim of this study is to assess the knowledge and awareness on COVID-19 disease and related infection control measures among the dental fraternity in Visakhapatnam – the smart city.
METHODS:
A total of 808 dentists from the Visakhapatnam region completed a questionnaire-based survey on the knowledge, awareness, and infection control measures related to COVID-19 infection. The questionnaire was tailored from the guidance and information for health-care workers issued by the US Centers for Disease Control and Prevention. Suitable sampling method was used for the collection of data and the distribution of responses was presented as percentages. Explanatory statistics were performed for all groups and subgroups based on the percentage of correct responses. Individual pair-wise comparisons were done using the Chi-square test for the percentage of correct responses.
RESULTS:
A total of 825 participated in the survey, of which 808 dentists completely answered the survey, and the response rate was 98%. Among the respondents, males and females are 46.8% and 53.2%, respectively. There was a statistically significant difference for all the questions solicited, among age groups (P = 0.001, 0.001) and occupation (P = 0.001, 0.001, 0.004). Private practitioners seem to more awareness compared to teaching faculty, undergraduates, and postgraduates, as they have answered correctly (>70%) for almost all the questions.
CONCLUSION:
The inputs from the survey help us throw some light and fill up lacunae where required. There is a strong need to implement periodic educational interventions and training programs on infection control practices for COVID-19 among dentists in particular. The information from this survey helps us to make necessary changes in implementing periodic educational webinars and stress on areas where necessary, which is important for the dental fraternity for protecting themselves and shielding our society from COVID-19.
Keywords: Awareness, COVID-19, questionnaire, survey
Introduction
Viruses of the family Coronaviridae possess a single-strand, positive-sense RNA genome ranging from 26 to 32 kb in length.[1] Coronaviruses have been identified in several avian hosts,[2,3] as well as in various mammals, including camels, bats, masked palm civets, mice, dogs, and cats. Novel mammalian coronaviruses are now regularly identified.[1] For example, an HKU2-related coronavirus of bat origin was responsible for a fatal acute diarrhea syndrome in pigs in 2018.[4] Among several coronaviruses that are pathogenic to humans, most are associated with mild clinical symptoms,[1] with two main variations: severe acute respiratory syndrome coronavirus (SARS-CoV), a novel beta-coronavirus that emerged in Guangdong, Southern China, in November 2002[5] and resulted in more than 8000 human infections and 774 deaths in 37 countries during 2002–2003[6] and Middle East respiratory syndrome coronavirus (MERS-CoV), which was first detected in Saudi Arabia in 2012[7] and was responsible for 2494 laboratory-confirmed cases of infection and 858 fatalities since September 2012 including 38 deaths following a single introduction into South Korea.[8,9]
Regarding pathophysiology and virulence mechanisms of CoVs, SARS-CoV-2 have associations and obstruct the function of nonstructural proteins (nsps) and structural proteins. For example, the research highlighted that nsp is able to wedge the host immune response. Among functions of structural proteins, the envelope has a vital job in virus pathogenicity as it stimulates viral association and discharge.[10,11]
Deep sequencing studies and laboratory investigations have identified the culprit as a new strain of COV.[10] Initially, this virus was named as 2019-nCoV. However, the International Committee on Taxonomy of Viruses named it as the SARS-CoV-2 virus.[11] On February 11, 2020, the World Health Organization (WHO) directly announced the disease caused by this virus as coronavirus disease-2019 (COVID-19). The repeated outbreaks of CoVs indicate a severe public threat. This report suggested the chances of animal-to-human and human-to-human transmission of newly emerged CoVs. The undergoing changes in the ecology and climates of the specific regions in the world make future emergence of such infections more likely.[10,11]
This disease was noted as a pandemic on March 11, 2020, with global spread and affecting thousands of people. Most of the evidence for this disease comes from the epidemiological findings from China, Korea, Italy, the USA, and the United Kingdom. The information from these countries has helped the researchers and drawn inference for the rest of the world.[12]
After the Chinese, Italy, and the USA, now the time had come for India. India has confirmed its first case of coronavirus on January 30.
With this mode of transmission, among the health-care workers, dentists are more prone and have the highest risk of being infected. The hypothesis assumed was that there is no change regarding knowledge and awareness on coronavirus spread among dental fraternities.
The objective of this study is to assess the knowledge and awareness of COVID-19 disease and its related infection control practices among dentists in the city of Visakhapatnam, Andhra Pradesh (India). This was a questionnaire-based survey and was tailored from the guidance and information for health-care workers issued by the US Centers for Disease Control and Prevention (CDC).
Methods (Study Design, Sampling and Sample Size, Collection of Data, and Statistical Analysis)
A pilot study was done on 20 dentists, the reliability of the questionnaire was checked, and the Cronbach's alpha value was 0.8. Before commencing the survey, consent was obtained from all the participants in the Visakhapatnam region. Participants were informed of the information sought before including them in this study. The participants were assured of confidentiality. The survey was prepared in the online form (Google Docs) and was sent to 825 potential responders who included undergraduate and postgraduate students and teaching faculty and private practitioners. The period of the survey was from March 31, 2020, to April 12, 2020, and a total of 808 responders completed the survey with a response rate of 97.93%. The inclusion criteria for the study, especially for the teaching faculty and postgraduates, were those are concerned only to academics and not practicing outside the institution.
The self-administered questionnaire consisting of 16 questions based on knowledge, awareness, and infection control measures related to COVID-19 disease among the dentists. The questionnaire also has questions related to hand hygiene techniques described by the WHO, which were used to test the contributor's knowledge.
A convenient sampling method was used for data collection, and the distribution of responses was presented as frequency and percentages. Subgroups were classified on the basis of gender, age (18–25 years, 25–35 years, and above 35 years), and profession (undergraduate, postgraduate students, and teaching faculty from a teaching institute and private practitioners).
Statistical analysis
The data were tabulated in Excel and descriptive statistics were performed. The software used for the statistical analysis was SPSS version 20, Armonk, NY:IBM Corp for inferential for inferential statistics and Cronbach's alpha. Statistical test used was Chi-square test and the level of significance was set at 0.05 (P = 0.05).
Results
A total of 825 participated in the survey, of which 808 dentists completely answered the survey, and the response rate was 98%. The majority of the responders were from the age group of 25–35 years (52.40%), followed by 18–25 years (30.20%) and above 35 years (17.5%). Approximately 53.20% of the responders were female and 46.80% were male, 58.90% of the responders were private practitioners, 28% were undergraduates, 7.2% were postgraduates, and 5.9% were teaching faculty [Figures 1-3].
Figure 1.
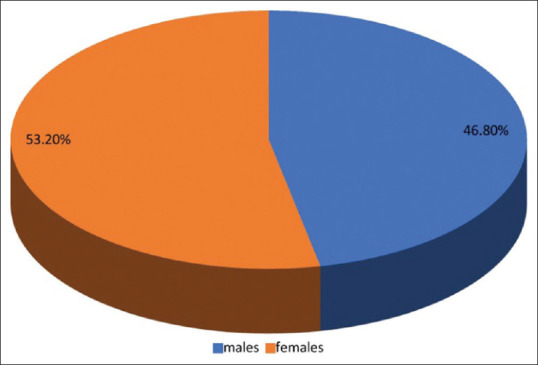
Percentage of males and females participated in the study
Figure 3.
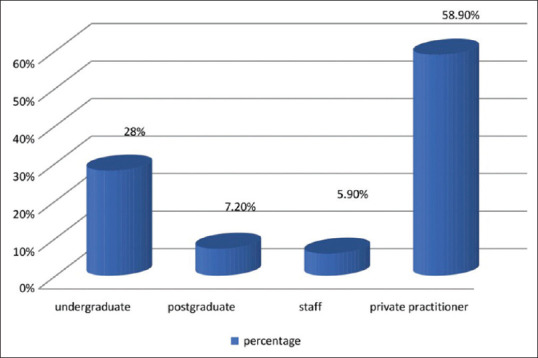
Percentage of responders among the profession
Figure 2.
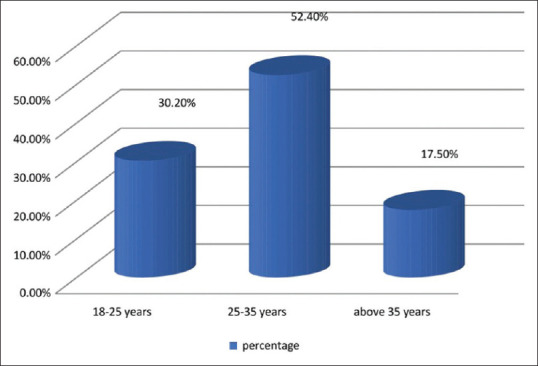
Percentage of the age of the participants
When considering the gender, 71.2% of the males and 62.3% of the females believe that the origin of coronavirus is from the bats, i.e., the response between the genders was statistically significant (P < 0.001). When the question arises that supportive care is the only treatment of choice to treat coronavirus, there is a mixed response from the participants, 52.6% of females and 39.4% of males agreed that supportive care is the only treatment of choice which was statistically significant (P = 0.001). A statistically significant number of males and females believed that COVID-19 symptoms will appear in between 2 and 14 days (P = 0.012). Interestingly, a low percentage of males (20%) and (females (9.1%) said that flu vaccination is helpful in preventing coronavirus spread, and the difference between the gender is statistically significant (P = 0.001). For the other questions asked, there was no statistically significant difference between the males and females (P > 0.05) [Table 1].
Table 1.
Questions versus gender
| Question | Gender | P | |
|---|---|---|---|
| Males | Females | ||
| Do you think that the coronavirus is originated from bats? | |||
| Yes | 269 (71.2) | 268 (62.3) | 0.000* |
| No | 19 (5) | 58 (13.5) | |
| Maybe | 90 (23.8) | 104 (24.2) | |
| COVID-19 is transmitted through air, contact, and fecal- oral routes? | |||
| Yes | 343 (90.7) | 386 (89.8) | 0.895 |
| No | 18 (4.8) | 23 (5.3) | |
| Maybe | 17 (4.5) | 21 (4.9) | |
| Do you think COVID-19 leads to pneumonia, respiratory failure, and death? | |||
| Yes | 353 (93.4) | 404 (94) | 0.871 |
| No | 12 (3.2) | 11 (2.6) | |
| Maybe | 13 (3.4) | 15 (3.4) | |
| Do you think dentists are more prone to get infected with the coronavirus? | |||
| Yes | 353 (93.4) | 406 (94.4) | 0.753 |
| No | 4 (1.1) | 5 (1.2) | |
| Maybe | 21 (5.6) | 19 (4.4) | |
| Do you agree that supportive care is the only treatment of choice for COVID-19? | |||
| Strongly disagree | 9 (2.4) | 5 (1.2) | 0.000* |
| Disagree | 5 (1.3) | 18 (4.2) | |
| Neutral | 171 (45.2) | 138 (32.1) | |
| Agree | 149 (39.4) | 226 (52.6) | |
| Strongly agree | 44 (11.6) | 43 (10) | |
| Which type of masks are more protective to COVID-19 | |||
| N95 masks | 361 (95.5) | 407 (94.7) | 0.075 |
| Surgical masks | 14 (3.7) | 11 (2.6) | |
| Cloth masks | 3 (0.8) | 12 (2.8) | |
| Do you think that there is any impact of social distancing on prevention of coronavirus spread? | |||
| Yes | 368 (97.4) | 404 (94) | 0.060 |
| No | 3 (0.8) | 6 (1.4) | |
| Maybe | 7 (1.9) | 20 (4.7) | |
| Do you think the hand hygiene and covering of the mouth and face can help in the prevention of COVID-19 transmission? | |||
| Yes | 350 (92.6) | 397 (92.3) | 0.397 |
| No | 6 (1.6) | 3 (0.7) | |
| Maybe | 22 (5.8) | 30 (7.0) | |
| Do you think the COVID-19 symptoms will appear in between 2 and 14 days only? | |||
| Yes | 298 (78.8) | 302 (70.2) | 0.012 |
| No | 29 (7.7) | 56 (13.0) | |
| Maybe | 51 (13.5) | 72 (16.7) | |
| Do you think COVID-19 is fatal? | |||
| Yes | 272 (72.0) | 287 (66.7) | 0.262 |
| No | 43 (11.4) | 55 (12.8) | |
| Maybe | 63 (16.7) | 88 (20.5) | |
| Do you think COVID-19 is more fatal for immunocompromised persons? | |||
| Yes | 353 (93.4) | 404 (94.6) | 0.555 |
| No | 8 (2.1) | 5 (1.2) | |
| Maybe | 17 (4.5) | 18 (4.2) | |
| Do you think flu vaccination is helpful in preventing coronavirus spread? | |||
| Yes | 76 (20.1) | 39 (9.1) | 0.000 |
| No | 84 (22.2) | 145 (33.7) | |
| Maybe | 218 (57.7) | 246 (57.2) | |
| Finally, do you think hand sanitization in regular intervals will prevent coronavirus spread? | |||
| Yes | 333 (88.1) | 362 (84.2) | 0.200 |
| No | 7 (1.9) | 7 (1.6) | |
| Maybe | 38 (10.1) | 61 (14.2) | |
*As P ≤ 0.05, it means it is significant; if it is more than 0.05, it is not significant. COVID-19=Coronavirus diseases
A statistically significant difference (P = 0.001, 0.001) was seen in all the questions asked between the age groups (18–25, 25–35, >35 years) [Table 2].
Table 2.
Questions versus age
| Question | Age | P | ||
|---|---|---|---|---|
| 18- 25 | 25- 35 | Above 35 | ||
| Do you think that the coronavirus is originated from bats? | ||||
| Yes | 79 (32.4) | 340 (80.4) | 118 (83.7) | 0.001* |
| No | 61 (25.0) | 14 (3.3) | 2 (1.4) | |
| Maybe | 104 (42.6) | 69 (16.3) | 21 (14.9) | |
| COVID-19 is transmitted through air, contact, and fecal- oral routes? | ||||
| Yes | 199 (81.6) | 400 (94.6) | 130 (92.2) | 0.001* |
| No | 22 (9.0) | 12 (2.8) | 7 (5.0) | |
| Maybe | 23 (9.4) | 11 (2.6) | 4 (2.8) | |
| Do you think COVID-19 leads to pneumonia, respiratory failure, and death? | ||||
| Yes | 222 (91.0) | 403 (95.3) | 132 (93.6) | 0.001 |
| No | 8 (3.3) | 12 (2.8) | 3 (2.1) | |
| Maybe | 14 (5.7) | 8 (1.9) | 6 (4.3) | |
| Do you think dentists are more prone to get infected with the coronavirus? | ||||
| Yes | 208 (85.2) | 416 (98.3) | 135 (95.7) | 0.000 |
| No | 6 (2.5) | 3 (0.7) | 0 (0.0) | |
| Maybe | 30 (12.3) | 4 (0.9) | 6 (4.3) | |
| Do you agree that supportive care is the only treatment of choice for COVID-19? | ||||
| Strongly disagree | 7 (2.9) | 4 (0.9) | 3 (2.1) | 0.000* |
| Disagree | 16 (6.6) | 6 (1.4) | 1 (0.7) | |
| Neutral | 92 (37.7) | 211 (49.9) | 6 (4.3) | |
| Agree | 108 (44.3) | 176 (41.6) | 91 (64.5) | |
| Strongly agree | 21 (8.6) | 26 (6.1) | 40 (28.4) | |
| Which type of masks are more protective to COVID-19 | ||||
| N95 masks | 215 (88.1) | 413 (97.6) | 140 (99.3) | 0.000* |
| Surgical masks | 14 (5.7) | 10 (2.4) | 1 (0.7) | |
| Cloth masks | 15 (6.1) | 0 (0.0) | 0 (0.0) | |
| Do you think that there is any impact of social distancing on prevention of coronavirus spread? | ||||
| Yes | 227 (93.0) | 413 (97.6) | 132 (93.6) | 0.000* |
| No | 9 (3.7) | 0 (0.0) | 0 (0.0) | |
| Maybe | 8 (3.3) | 10 (2.4) | 9 (6.4) | |
| Do you think the hand hygiene and covering of the mouth and face can help in prevention of COVID-19 transmission? | ||||
| Yes | 200 (82) | 415 (98.1) | 132 (93.6) | 0.000* |
| No | 9 (3.7) | 0 (0.0) | 0 (0.0) | |
| Maybe | 35 (14.3) | 8 (1.9) | 9 (6.4) | |
| Do you think the COVID-19 symptoms will appear in between 2 and 14 days only? | ||||
| Yes | 125 (51.2) | 359 (84.9) | 116 (82.3) | 0.000* |
| No | 52 (21.3) | 19 (4.5) | 14 (9.9) | |
| Maybe | 67 (27.5) | 45 (10.6) | 11 (7.8) | |
| Do you think COVID-19 is fatal? | ||||
| Yes | 134 (54.9) | 335 (79.2) | 90 (63.8) | 0.000* |
| No | 31 (12.7) | 26 (6.1) | 41 (29.1) | |
| Maybe | 79 (32.4) | 62 (14.7) | 10 (7.1) | |
| Do you think COVID-19 is more fatal for immunocompromised persons? | ||||
| Yes | 220 (90.5) | 412 (97.4) | 125 (89.9) | 0.000* |
| No | 7 (2.9) | 0 (0.0) | 6 (4.3) | |
| Maybe | 16 (6.6) | 11 (2.6) | 8 (5.8) | |
| Do you think flu vaccination is helpful in preventing coronavirus spread? | ||||
| Yes | 15 (6.1) | 74 (17.5) | 26 (18.4) | 0.000* |
| No | 144 (59.0) | 49 (11.6) | 36 (25.5) | |
| Maybe | 85 (34.8) | 300 (70.9) | 79 (56.0) | |
| Finally, do you think hand sanitization in regular intervals will prevent coronavirus spread? | ||||
| Yes | 157 (64.3) | 406 (96.0) | 132 (93.6) | 0.000* |
| No | 9 (3.7) | 3 (0.7) | 2 (1.4) | |
| Maybe | 78 (32.0) | 14 (3.3) | 7 (5.0) | |
COVID-19=Coronavirus diseases
While considering the occupation, the undergraduates, teaching faculty, postgraduates, and private practitioners showed a statistically significant difference for all the questions that were requested (P = 0.001, 0.001, 0.004) [Table 3]. Thus, the null hypothesis assumed that there is no difference between the groups that are rejected.
Table 3.
Questions versus occupation
| Question | Occupation | P | |||
|---|---|---|---|---|---|
| Undergraduate student | Faculty | Postgraduate student | Private practitioner | ||
| Do you think that the coronavirus is originated from bats? | |||||
| Yes | 74 (32.7) | 15 (31.2) | 33 (56.9) | 415 (87.2) | 0.001* |
| No | 58 (25.7) | 8 (16.7) | 8 (13.8) | 3 (0.6) | |
| Maybe | 94 (41.6) | 25 (52.1) | 17 (29.3) | 58 (12.2) | |
| COVID-19 is transmitted through air, contact, and fecal- oral routes? | |||||
| Yes | 179 (79.2) | 36 (75.0) | 50 (86.2) | 464 (97.5) | 0.000* |
| No | 22 (9.7) | 7 (14.6) | 6 (10.3) | 6 (1.3) | |
| Maybe | 25 (11.1) | 5 (10.4) | 2 (3.4) | 6 (1.3) | |
| Do you think COVID-19 leads to pneumonia, respiratory failure and death? | |||||
| Yes | 205 (90.7) | 44 (91.7) | 57 (98.3) | 451 (94.7) | 0.001 |
| No | 4 (1.8) | 1 (2.1) | 0 (0.0) | 18 (3.8) | |
| Maybe | 17 (7.5) | 3 (6.2) | 1 (1.7) | 7 (1.5) | |
| Do you think dentists are more prone to get infected with the corona virus? | |||||
| Yes | 208 (92.0) | 41 (85.4) | 52 (89.7) | 458 (96.2) | 0.004 |
| No | 4 (1.8) | 0 (0.0) | 2 (3.4) | 3 (0.6) | |
| Maybe | 14 (6.2) | 7 (14.6) | 4 (6.9) | 15 (3.2) | |
| Do you agree that supportive care is the only treatment of choice for COVID-19? | |||||
| Strongly disagree | 10 (4.4) | 0 (0.0) | 0 (0.0) | 4 (0.8) | 0.000* |
| Disagree | 16 (7.1) | 7 (14.6) | 0 (0.0) | 0 (0.0) | |
| Neutral | 74 (32.7) | 10 (20.8) | 23 (39.7) | 202 (42.4) | |
| Agree | 97 (42.9) | 24 (50.0) | 27 (46.6) | 227 (47.7) | |
| Strongly agree | 29 (12.8) | 7 (14.6) | 8 (13.8) | 43 (9.0) | |
| Which type of masks are more protective to COVID-19 | |||||
| N95 masks | 206 (91.2) | 44 (91.7) | 51 (87.9) | 467 (98.1) | 0.000* |
| Surgical masks | 12 (5.3) | 2 (4.2) | 2 (3.4) | 9 (1.9) | |
| Cloth masks | 8 (3.5) | 2 (4.2) | 5 (8.6) | 0 (0.0) | |
| Do you think that there is any impact of social distancing on prevention of coronavirus spread? | |||||
| Yes | 215 (95.1) | 47 (97.9) | 52 (89.7) | 458 (96.2) | 0.000* |
| No | 5 (2.2) | 0 (0.0) | 4 (6.9) | 0 (0.0) | |
| Maybe | 6 (2.7) | 1 (2.1) | 2 (3.4) | 18 (3.8) | |
| Do you think the Hand hygiene and covering of mouth and 2se can help in prevention of COVID-19 transmission? | |||||
| Yes | 193 (85.4) | 39 (81.2) | 55 (94.8) | 460 (96.6) | 0.000* |
| No | 8 (3.5) | 1 (2.1) | 0 (0.0) | 0 (0.0) | |
| Maybe | 25 (11.1) | 8 (16.7) | 3 (5.2) | 16 (3.4) | |
| Do you think the COVID-19 symptoms will appear in between 2 and 14 days only? | |||||
| Yes | 118 (52.2) | 28 (58.3) | 36 (62.1) | 418 (87.8) | 0.000* |
| No | 48 (21.2) | 11 (22.9) | 10 (17.2) | 16 (3.4) | |
| Maybe | 60 (26.5) | 9 (18.8) | 12 (20.7) | 42 (8.8) | |
COVID-19=Coronavirus diseases
Discussion
From the time of its outburst in Wuhan in December 2019, the COVID-19 disease has had a torrential influence globally. The documentation and separation of suspected cases from the community is the most imperative step in restricting the blowout of COVID-19.
According to the US CDC, a “close contact” is defined as: “being within approximately 6 feet (2 m) of a COVID-19 case for a prolonged period of time or having direct contact with infectious secretions of a COVID-19 case”. Likewise, several additional significant explanations have been stipulated and issued by the CDC.[13] This group (dentists) has the highest risk of potential contact with the virus because they will be having near-patient interaction at some point in the health-care setting and consequently at risk of contracting and smattering the contagion.
Mixed response was noted about the supportive care among participants, it might be due to more exposure to the media which constantly updates on the current disease symptoms and treatment.
Appropriate hand sanitization practices play an important job in stopping the blowout of infection. The WHO gave the “Five Moments of hand hygiene” explains vital instants. Two simple procedures to sterile hands are handwashing and hand rubbing. The CDC advocates alcohol-based hand rub in maximum circumstances. However, the question in our survey was focused on hand hygiene, and covering of the mouth will prevent the spreading of infection.[13]
Practicing proper hand hygiene is important because of the transmission of the 2019-nCoV through the fecal–oral route. Specifically, the dental professionals should wash their hands before the patient examination, before dental procedure, after touching the patient, after touching the surroundings and equipment without disinfection, after touching the oral cavity, ruptured skin or wound, blood, fluid secretion, and excrement. Hand disinfection is suggested even for patients.[13] The N95 respirator is chosen over the face mask when exposed to aerosols. Appropriate discarding of the used masks and hand sanitization should be performed. In the present study, majority of the participants answered that N95 masks are protective against COVID-19. This result is also in accordance with the guidelines given by the CDC where N95 masks are more protective against coronavirus spread.[13] When the question arises about the appearance of symptoms in the infected patients, the modest percentage, i.e., 78.8% of males and 70.2% of females, believed that COVID-19 symptoms will appear in between 2 and 14 days only, which is in accordance with CDC.[13] Among all the age groups, major proportion stated that immunocompromised patients are at the highest risk to COVID 19. This increased awareness can be attributed to added social responsibility and experience as age increases and constantly updating themselves about the disease.[14,15,16]
Interestingly, a low percentage, 20% of males and 9.1% of females, said that flu vaccination is helpful in preventing coronavirus spread, similarly conveyed in the situation report by WHO that flu vaccination has no role in controlling the coronavirus spread.[17] On the other hand, 88.1% of males and 84.2% of females trusted that hand sanitization in regular intervals will prevent coronavirus spread, similarly reported in the recent study by Modi et al. stating that the hand sanitization at regular intervals can prevent the spread of COVID-19.[15]
To the best of our information, I think, this might be the first study that assesses the knowledge and awareness of COVID-19 among dentists, especially involving undergraduate students, postgraduates, faculty, and private practitioners in Visakhapatnam, India. This survey is one of its kinds, in the way that dental fraternity is one of the high-risk groups to Covid-19 which can be due to aerosols and directly contacting the mouth being the primary source of infection. It is always important to understand the disease as a whole and be well informed before treating a patient. This survey aims to assess their awareness for the same. The results from the survey help to create awareness in the areas lacking behind. Moreover, the responses in the survey were evaluated based the current information available; our understanding of the disease is never static and constantly evolving. It is always important for us to keep us updated with the current standards and regulations as broadcasted by the WHO.
The present position stresses urgent improvement of plans to inhibit infection among high-risk people including preexposure and postexposure prophylaxis. Several medicines comprising antivirals and antimalarials are under experimental condition. Testing of hydroxychloroquine in vitro showed to have some antiviral action against SARS-CoV-2 and can be used as a chemoprophylaxis for health-care professionals. Scientific examinations for the management of COVID-19 pneumonia with hydroxychloroquine are on-going and outcomes of the same will be observed carefully in the upcoming dates.
Limitations of the study
The study cannot be generalized to the entire dental fraternity as the survey was done on a group of dentists in the Visakhapatnam region
Follow-up surveys (or) surveys with large sample have to be done
There are chances of observational error.
Conclusion
The inputs from the survey show that there is a strong need to implement periodic educational interventions and training programs on infection control practices for COVID-19 among dentists in particular. Conducting regular educational webinars with customary guidelines and contents to create more awareness among dental fraternity is important for them to stay safe and protect our society from this COVID-19. It is also essential to keep ourselves well appointed both mentally and physically to fight against such pandemics. These instances helped us to follow an improved hygiene for the welfare of our lives as well as the nation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24:490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cavanagh D. Coronavirus avian infectious bronchitis virus. Vet Res. 2007;38:281–97. doi: 10.1051/vetres:2006055. [DOI] [PubMed] [Google Scholar]
- 3.Ismail MM, Tang AY, Saif YM. Pathogenicity of turkey coronavirus in Turkeys and chickens. Avian Dis. 2003;47:515–22. doi: 10.1637/5917. [DOI] [PubMed] [Google Scholar]
- 4.Zhou P, Fan H, Lan T, Yang XL, Shi WF, Zhang W, et al. Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin. Nature. 2018;556:255–8. doi: 10.1038/s41586-018-0010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peiris JS, Guan Y, Yuen KY. Severe acute respiratory syndrome. Nat Med. 2004;10:S88–97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan-Yeung M, Xu RH. SARS: Epidemiology. Respirology. 2003;8 Suppl:S9–14. doi: 10.1046/j.1440-1843.2003.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367:1814–20. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 8.Lee J, Chowell G, Jung E. A dynamic compartmental model for the Middle East respiratory syndrome outbreak in the Republic of Korea: A retrospective analysis on control interventions and superspreading events. J Theor Biol. 2016;408:118–26. doi: 10.1016/j.jtbi.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JY, Kim YJ, Chung EH, Kim DW, Jeong I, Kim Y, et al. The clinical and virological features of the first imported case causing MERS-CoV outbreak in South Korea, 2015. BMC Infect Dis. 2017;17:498. doi: 10.1186/s12879-017-2576-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418–23. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD. Features, Evaluation and Treatment Coronavirus (COVID-19) Treasure Island, FL: Stat Pearls Publishing; 2020. [PubMed] [Google Scholar]
- 12.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frequently Asked Questions About Hand Hygiene for Healthcare Personnel Responding to COVID-2019. 2020. [Last accessed on 2020 Apr 20]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/infectioncontrol/hcphand-hygiene-faq.html .
- 14.European Centre for Disease Prevention and Control. Rapid Risk Assessment: Outbreak of Acute Respiratory Syndrome Associated with a Novel Coronavirus, Wuhan, China. First Update – 22 January 2020. Stockholm: ECDC; 2020. [Google Scholar]
- 15.Modi PD, Nair G, Uppe A, Modi J, Tuppekar B, Gharpure AS, et al. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: A questionnaire-based survey. Cureus. 2020;12:e7514. doi: 10.7759/cureus.7514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Modi PD, Kumar P, Solanki R, Modi J, Chandramani S, Gill N. Hand hygiene practices among Indian medical undergraduates: A questionnaire-based survey. Cureus. 2017;9:e1463. doi: 10.7759/cureus.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coronavirus Disease 2019 (COVID-19) Situation Report (WHO) – 46 Data as Reported by National Authorities by 10AM CET; 06 March, 2020 [Google Scholar]


