Basilar artery aneurysm and dilative arteriopathy are recognized complications in late-onset Pompe disease (LOPD).1 We present a case of basilar artery aneurysm in infantile Pompe disease (IPD).
The patient, a 9-year-old Hispanic girl with classic IPD, presented at age 3 months with cardiomegaly and a family history positive for IPD. Skin Western blot analysis revealed cross-reactive immunologic material–positive status. GAA mutation analysis revealed c.1802 C>T (p.Ser601Leu), c.1726 G>A (p.Gly576Ser), and c.2065 G>A (p.Glu689Lys) on allele 1, and c.1099 T>C (p.Trp367Arg) mutation on allele 2. At age 5 months, alglucosidase alfa enzyme replacement therapy (ERT, rhGAA; Myozyme; 20 mg/kg every 2 weeks for 56 months, followed by 40 mg/kg every 2 weeks) was initiated. The patient demonstrated remarkable gains until age 5 years, with ability to walk, improved cardiomyopathy, and no need for ventilator support or tube feeding. Between ages 5 and 9 years, she demonstrated phenotypic features of infantile survivors.2
At age 7 years, the patient sustained a closed head injury. Brain computed tomography (CT) revealed a posterior fossa epidural hematoma. Three days after the accident, magnetic resonance angiography/venography (MRA/MRV) demonstrated occlusion of the right sigmoid sinus without evidence of venous infarct in the right temporal lobe. Upon further review, MRA showed a 2-mm, broad-based aneurysm near the origin of the basilar artery (Fig. 1), which, given the lack of a neck, was not amenable to neurointerventional transcatheter occlusion. The patient has remained asymptomatic from this aneurysm with no visual field deficits, dizziness, nausea, vomiting, or sudden-onset speech or motor deficits.
FIGURE 1.
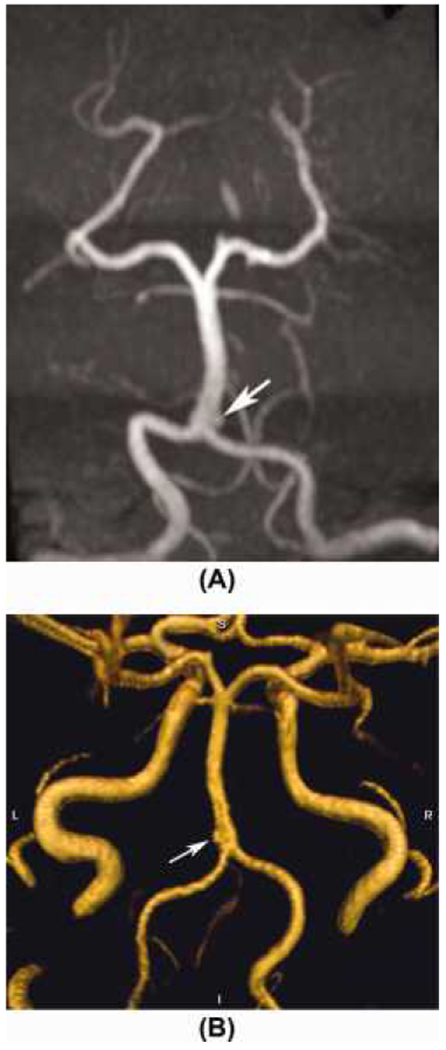
MRA with 3D time-of-flight was performed with (A) minimum-intensity thick slab (as viewed with slight anterior–superior rotation of reconstruction) of the posterior arterial circulation and (B) volume reconstruction of the arterial system at the skull base (as viewed from posterior), both from the axial data set, demonstrating a 2-mm aneurysm (arrows) arising just to the left of the proximal portion of the basilar artery. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
At least 15 cases of basilar artery aneurysm or dilative arteriopathy, as well as cases of thoracic aortic dilation and other signs of diffuse arteriopathy, have been reported in LOPD.1 To date, no similar findings have been reported in IPD. Autopsy reports from both IPD and LOPD patients have shown glycogen accumulation in vascular smooth muscle cells.5 Pathologic studies of cerebral arteries in LOPD patients have demonstrated vacuolation and glycogen-filled vacuoles in smooth muscle cells of cerebral arteries.7 As IPD patients survive longer with ERT, dilative arteriopathy could develop in this population.
In our patient’s case, the location and mechanism of injury made a posttraumatic etiology for the aneurysm highly unlikely, especially given the lack of clinical features predisposing to intracranial aneurysms. Although the basilar artery aneurysm in this case was not amenable to neurointerventional therapy, it is potentially important to identify this finding, as the risk for progression of the aneurysm and the presence of vasculopathy must be considered. Although there are not enough data to support routine MRA in IPD patients, if neuroimaging is conducted for other purposes, it is advisable to specifically evaluate the patient for cerebral vascular malformations.
Although we have presented a basilar artery aneurysm in only 1 IPD patient, and thus cannot prove a link between the 2 conditions, previous experience in LOPD urges clinicians to consider a vascular phenotype, including intracranial aneurysms, as part of the spectrum of clinical findings in IPD, especially as the life expectancy of these infants continues to increase.
Acknowledgments
This project was funded in part by the Lysosomal Disease Network, a part of NIH Rare Diseases Clinical Research Network (RDCRN). Funding and/or programmatic support for this project has been provided by (1U54NS065768-01) from the NINDS and the NIH Office of Rare Diseases Research (ORDR). The views expressed in written materials or publications do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, r organizations imply endorsement by the U.S.
References
- 1.Laforet P, Petiot P, Nicolino M, Orlikowski D, Callaud C, Pelligrini N, et al. Dilative arteriopathy and basilar artery dolichoectasia complicating late-onset Pompe disease. Neurology 2008;70:2063–2066. [DOI] [PubMed] [Google Scholar]
- 2.Prater SN, Banugaria SG, Dearmey SM, Botha EG, Stege EM, Case LE, et al. The emerging phenotype of long-term survivors with infantile Pompe disease. Genet Med 2012;14:800–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sacconi S, Bocquet JD, Chanelet S, Tanant V, Salviati L, Desnuelle C. Abnormalities of cerebral arteries are frequent in patients with late-onset Pompe disease. J Neurol 2010;257:1730–1733. [DOI] [PubMed] [Google Scholar]
- 4.El-Gharbawy AH, Bhat G, Murillo JE, Thurberg BL, Kampmann C, Mengel KE, et al. Expanding the clinical spectrum of late-onset Pompe disease: dilated arteriopathy involving the thoracic aorta, a novel vascular phenotype uncovered. Mol Genet Metab 2011;103:362–366. [DOI] [PubMed] [Google Scholar]
- 5.Thurberg BL, Lynch Maloney C, Vaccaro C, Afonso K, Tsai AC, Bossen E, et al. Characterization of pre- and post-treatment pathology after enzyme replacement therapy for Pompe disease. Lab Invest 2006;86:1208–1220. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi H, Shimada Y, Ikegami M, Kawai T, Sakurai K, Urashima T, et al. Prognostic factors for the late onset Pompe disease with enzyme replacement therapy: from our experience of 4 cases including an autopsy case. Mol Genet Metab 2010;100:14–19. [DOI] [PubMed] [Google Scholar]
- 7.Makos MM, McComb RD, Hart MN, Bennett DR. Alpha-glucosidase deficiency and basilar artery aneurysm: report of a sibship. Ann Neurol 1987;22:629–633. [DOI] [PubMed] [Google Scholar]


